ABSTRACT
Objectives
This article, the second in a two-part series, continues the discussion of inferior alveolar nerve lateralization/transposition for dental implant placement. The aim of this article is to review the scientific literature and clinical reports in order to analyse the neurosensory complications, risks and disadvantages of lateralization/transposition of the inferior alveolar nerve followed by implant placement in an edentulous atrophic posterior mandible.
Material and Methods
A comprehensive review of the current literature was conducted according to the PRISMA guidelines by accessing the NCBI PubMed and PMC databases, as well as academic sites and books. The articles were searched from January 1997 to July 2014. Articles in English language, which included adult patients between 18 - 80 years of age who had minimal residual bone above the mandibular canal and had undergone inferior alveolar nerve (IAN) repositioning, with minimum 6 months of follow-up, were included.
Results
A total of 21 studies were included in this review. Ten were related to IAN transposition, 7 to IAN lateralization and 4 to both transposition and lateralization. The IAN neurosensory disturbance function was present in most patients (99.47% [376/378]) for 1 to 6 months. In total, 0.53% (2/378) of procedures the disturbances were permanent.
Conclusions
Inferior alveolar nerve repositioning is related to initial transient change in sensation in the majority of cases. The most popular causes of nerve damage are spatula-caused traction in the mucoperiosteal flap, pressure due to severe inflammation or retention of fluid around the nerve and subsequent development of transient ischemia, and mandibular body fracture.
Keywords: alveolar bone atrophy, dental implants, fifth cranial nerve injury, jaw surgery, mandibular nerve, paresthesia
INTRODUCTION
Rehabilitation of edentulous atrophic posterior mandibles by inferior alveolar nerve (IAN) lateralization (IANL) or transposition (IANT), followed by implant placement, demonstrates many advantages; however, it also carries with it some disadvantages, such as neurosensory disturbance (ND) [1,2]. The major clinical difficulty associated with IANT is temporary or permanent dysfunction of the nerve, which patients reported as altered sensation of the lower lip and chin. Some of the symptoms of ND may involve loss of sensation in lower lip and chin; loss of sensation due to stretching of the IAN and disturbed sensation due to vascular damage [2]. Since this surgery is delicate, it is best performed under a general anaesthesia to eliminate patient movement and to maximise access [1].
Diagnostic methods of ND that have been used by different authors include: light touch (LT), two-point discrimination (2-PD), pain test (PT), pin-prick sensation test and brush stroke direction (BSD) method [3-6].
The literature also presents several cases of mandibular fracture as a result of IANL and IANT followed by implant placement in an edentulous atrophic posterior mandible [7,8]. IANL and IANT are techniques that have been used for more than 20 years with good survival and survival rates [23]. This is sometimes the only possible procedure to help patients to obtain a fixed prosthesis, especially in edentulous atrophic posterior mandibles.
The aim of this article is to review the scientific literature and clinical reports in order to analyse the neurosensory complications, risks and disadvantages of inferior alveolar nerve lateralization or transposition followed by implant placement in edentulous atrophic posterior mandible.
MATERIAL AND METHODS
IAN damage during lateralization and transposition definition
IAN damage during IANL is defined as damage to the neurovascular bundle after performing lateral reflection of the IAN. The damage or complication may occur due to exerting too much traction with a small contact area instrument upon the neurovascular bundle during its extraction from the canal or nerve traction during surgery, which may lead to ischemia of the neurosensory bundle [5].
IAN damage during IANT is defined as the damage to the neurosensory bundle after performing incisive nerve transaction. The damage is, first of all, due to the transaction itself, which disconnects the anterior region of the mandible from the neurovascular bundle, which means that no innervations will remain to the anterior teeth (if they are present). Other complications that may occur due to IANT include oedema, hematoma or chronic compression after surgery [6]. The technique involves extending the medial edge of the osteotomy medial to the mental foramen and removing the outer cortex in one piece. This creates a large bone segment that is difficult to manipulate and that has its axis of rotation within the mental nerve area. As a result, permanent mental nerve neurosensory disturbance is a serious risk with this approach [10].
Definition of ND diagnostic methods
LT test is performed in order to investigate lower lip and chin sensation. Static light touch with a soft feather or a cotton-tipped applicator is performed on the chin and lip regions. The patient needs to tell the practitioner when he/she feels a light touch and to show the exact location. The results are compared with a control site [3-6].
BSD test, in which the same feather or cotton-tipped applicator is used as in LT. This time, however, a dynamic stroke movement is performed from left to right and then from right to left. The patient needs to identify the direction of the stroke [3-6].
2-PD test is performed using sharp callipers. With the patient’s eyes closed, the distance between two points of the callipers is increased until the patient can feel the callipers’ points as two separate points of contact [3-6].
PT/Pin-prick sensation test is done by using a sharp explorer. The result is positive when the patient can differentiate between pressure pain (done with a blunt tip that measures the same diameter as the explorer) and the pain caused by a sharp explorer [3-6].
Protocol and registration
The review is registered in international prospective register of systematic reviews ‘PROSPERO’ [11]. The protocol can be accessed at: http://www.crd.york.ac.uk/prospero/display_record.asp?ID=CRD42015016357#.VMt78Z1FAyY
Registration number: CRD42015016357.
Eligibility criteria
Types of publication
The review included studies, case reports, clinical trials conducted on humans. Studies were published in English between January 1997 and July 2014, and included a minimum of 6 months of follow-up. Letters and PhD theses were excluded, as well as abstracts, reviews and studies on animals.
Information sources
The information source was the MEDLINE (NCBI PubMed and PMC) database and other scientific electronic databases.
Search
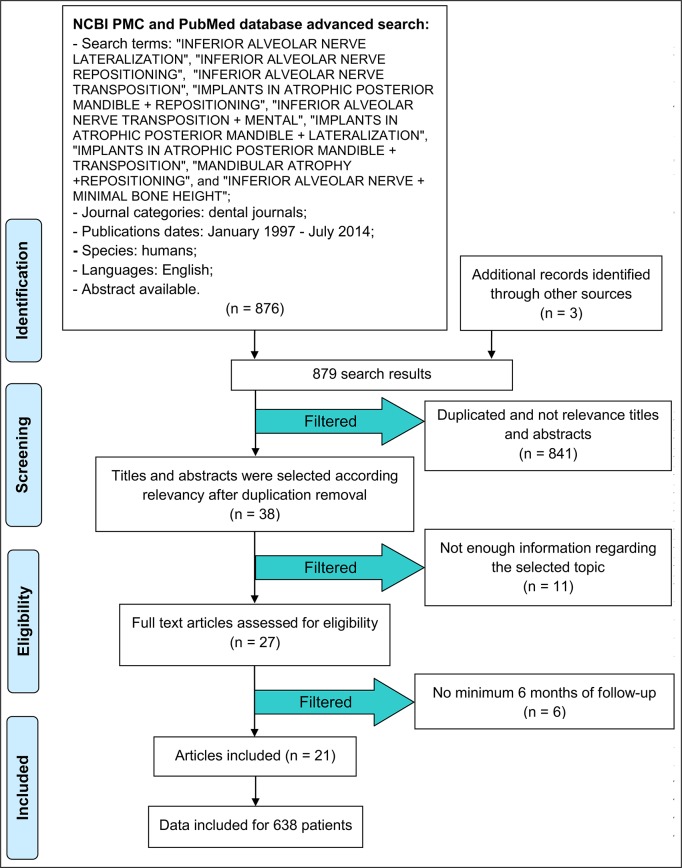
According to the PRISMA guidelines, an electronic search was conducted using the MEDLINE (NCBI PubMed and PMC) database to locate articles concerning IAN lateralization or IAN transposition and implant placement in an edentulous atrophic posterior mandible. The search terms used were: “INFERIOR ALVEOLAR NERVE LATERALIZATION”, ”INFERIOR ALVEOLAR NERVE REPOSITIONING”, ”INFERIOR ALVEOLAR NERVE TRANSPOSITION”, ”IMPLANTS IN ATROPHIC POSTERIOR MANDIBLE + REPOSITIONING”, ”INFERIOR ALVEOLAR NERVE TRANSPOSITION + MENTAL”, ”IMPLANTS IN ATROPHIC POSTERIOR MANDIBLE + LATERALIZATION”, ”IMPLANTS IN ATROPHIC POSTERIOR MANDIBLE + TRANSPOSITION”, ”MANDIBULAR ATROPHY + REPOSITIONING”, and ”INFERIOR ALVEOLAR NERVE + MINIMAL BONE HEIGHT”. Due to the low number of relevant articles and to ensure the sensitivity of the systemic review process, articles were searched from January 1997 to July 2014. Bibliographies of the selected articles were also manually searched. Titles derived from this broad search were independently screened by two authors based on the inclusion criteria. Disagreements were resolved by discussion. Full reports were obtained for all the studies that were deemed eligible for inclusion in this paper. Figure 1 illustrates the flow diagram of the present article selection according to PRISMA guidelines [12].
Figure 1.
PRISMA flow diagram.
Study selection
Inclusion and exclusion criteria
Inclusion criteria for the selection were:
Articles regarding to IANL and IANT procedures;
All article types in English;
Clinical reports with minimum 6 months follow-up;
Studies on adult (between ages 18 and 80) human beings, with no immunologic diseases, uncontrolled; diabetes mellitus, osteoporosis, or other contraindicating systemic conditions.
Exclusion criteria for the selection were:
Clinical reports with no minimum 6 months of follow-up;
Not enough information regarding the selected topic;
Studies on animals;
Studies of patients with immunologic diseases, uncontrolled diabetes mellitus, osteoporosis or other contraindicating systemic conditions;
Studies of adolescents (under 18 years of age) and elderly people (over 80).
Article review and data extraction
Article review and data extraction was performed according to a PRISMA flow diagram (Figure 1).
The search displayed 876 results from the NCBI PMC and PubMed databases and 3 results from other sources (dental-tribune.com, acta.tums.ac.ir, hindawi.com/journals). A total of 879 search results were screened. Preliminary exclusion was made by duplication and relevancy (n = 841). A total of 38 titles and abstracts were selected according to relevancy after the removal of duplications. Exclusion was made by information amount regarding the selected topic (n = 11). Twenty-seven articles were examined. Another exclusion was made based upon follow-up time (n = 6). Finally, 21 articles were included in the systematic review. Data was included for 638 patients.
Population selection
Studies of adult human beings between ages 18 and 80 years of age with minimal residual bone above the mandibular canal, in which IANL and IANT + implant placement had been performed, were selected.
Data collection process
Data was independently extracted from reports in the form of variables according to the aim and themes of the present review as listed below.
Risk of bias assessment
Risk of bias (e.g., lack of information or selective reports on variables of interest) was assessed at the study level. The risks were indicated as lack of precise information of interest in each individual study that can blind the reader from particular information about the examined samples. The Cochrane Collaboration tool for assessing risk of bias [13] was used to assess bias across the studies that could affect cumulative evidence.
RESULTS
Study selection
The search displayed 876 results from the NCBI PMC and PubMed databases and 3 results from other sources (dental-tribune.com, acta.tums.ac.ir, hindawi.com/journals). A total of 879 search results were screened. Preliminary exclusion was made by duplication and relevancy (n = 841). A total of 38 titles and abstracts were selected according to relevancy after duplication removal. Exclusion was made according to information amount regarding the selected topic (n = 11). Twenty-seven full text articles assessed for eligibility. During the eligibility stage, articles that did not meet the inclusion and exclusion criteria were filtered as follows: no minimum 6 months of follow-up (n = 6). In the end, 21 articles were included in the systematic review. Data was included for 638 patients (Figure 1).
Study characteristics
A total of 21 studies were included in this review. Ten were related to IANT, 7 to IANL and 4 to both IANT and IANL (Table 1).
Table 1.
Description of studies included in the review
| Study | Year of publication | Procedure performed | Number of patients |
|---|---|---|---|
| Morrison et al. [1] | 2002 | Transposition | 12 |
| Chrcanovic et al. [2] | 2009 | Transposition | 15 |
| Kan et al. [3] | 1997 | Lateralization | 10 |
| Transposition | 5 | ||
| Khajehahmadi et al. [4] | 2013 | Lateralization | 10 |
| Transposition | 11 | ||
| Ferrigno et al. [6] | 2005 | Transposition | 15 |
| Karlis et al. [7] | 2003 | Transposition | 1 |
| Kan et al. [8] | 1997 | Transposition | 1 |
| Peleg et al. [10] | 2002 | Lateralization | 10 |
| Del Castillo Pardo et al. [14] | 2008 | Lateralization | 1 |
| Proussaefs [15] | 2005 | Transposition | 1 |
| Hashemi [16] | 2005 | Lateralization | 11 |
| Vasconcelos et al. [17] | 2008 | Transposition | 1 |
| Hashemi [18] | 2010 | Lateralization | 87 |
| Lorean et al. [19] | 2013 | Transposition and reposition | 57 |
| Gasparini et al. [20] | 2014 | Transposition | 35 |
| Quantius [21] | 2010 | Lateralization | 70 |
| Barbu et al. [23] | 2014 | Lateralization | 7 |
| Dal Ponte et al. [24] | 2011 | Transposition | 1 |
| Vetromilla et al. [25] | 2014 | Lateralization | 125 |
| Transposition | 150 | ||
| Suzuki et al. [26] | 2012 | Lateralization | 1 |
| Proussaefs [27] | 2005 | Transposition | 1 |
Risk of bias within studies
Data supplied was checked for the following risks of bias within the selected studies: low number of patients (10 or fewer); ND examined by less than 2 methods; random selection of patients; exact post-operative outcomes not indicated for each patient. Any discrepancies or unusual patterns were checked with the study investigator. After analysing of the risk of bias (Table 2), we found that 10 authors [3,7,8,14,15,17,23,24,26,27] used a low number (< 10) of patients (it was decided in this review that < 10 will indicate a low number of patients), while 9 authors [1,2,4,6,10,16,18-20] used 10 or more patients. Nine authors [2,7,10,14,15,18,23,24,27] used only one ND evaluation method. For example, Peleg et al. [10] used only the pin-prick sensation test. Six authors [1,3,4,6,19,20] used 2 or more methods of ND evaluation. For example, Kan et al. [3] performed ND evaluation using LT, BSD and 2-PD test. Meanwhile, 4 authors [8,16,17,26] failed to mention the ND evaluation method. Diagnostic methods of ND that have been used by different authors include: LT, 2-PD, PT, pin-prick sensation test and BSD method. Eight authors [2-4,16,17,24,26,27] selected the patients randomly. Four authors [2,4,19,23] did not indicate the exact post-operative outcomes for each patient.
Table 2.
Assesment of the risks of bias
| Study | Low number of patients (10 or fewer) |
ND examined by less than 2 methods |
Random selection of patients |
Exact post-operative outcomes were not indicated for each patient |
|---|---|---|---|---|
| Morrison et al. [1] | - | - | - | - |
| Chrcanovic et al. [2] | - | + | + | + |
| Kan et al. [3] | + | - | + | - |
| Khajehahmadi et al. [4] | - | - | + | + |
| Ferrigno et al. [6] | - | - | - | - |
| Karlis et al. [7] | + | + | - | - |
| Kan et al. [8] | + | Not mentioned | - | - |
| Peleg et al. [10] | - | + | - | - |
| Del Castillo Pardo et al. [14] | + | + | - | - |
| Proussaefs [15] | + | + | - | - |
| Hashemi [16] | - | Not mentioned | + | - |
| Vasconcelos et al. [17] | + | Not mentioned | + | - |
| Hashemi [18] | - | + | - | - |
| Lorean et al. [19] | - | - | - | + |
| Gasparini et al. [20] | - | - | - | - |
| Barbu et al. [23] | + | + | - | + |
| Dal Ponte et al. [24] | + | + | + | - |
| Suzuki et al. [26] | + | Not mentioned | + | - |
| Proussaefs [27] | + | + | + | - |
ND = neurosensory disturbances.
Results of individual studies
Results of individual studies are shown in Table 3.
Table 3.
Results of individual studies
| Study |
Number of IANL and IANT procedures |
Number of implants placed |
Implant survival rate | Results |
|---|---|---|---|---|
|
Morrison et al. [1] |
20 IANT | 30 | 100% | All patients had initial change in sensation for about one month. 80% of the sites had returned to normal. 4 patients (4 sites in total) had persistent change in sensation. Each also said that the abnormality did not disturb to daily activities. According to objective tests, all sites were normal. 1 patient had painful unilateral dysesthesia for 3 months, in the end, had normal sensation. |
|
Chrcanovic et al. [2] |
18 IANT | 25 | 88% | All patients had initial paresthesia with complete recovery of the sensitivity within 6 months. |
| Kan et al. [3] |
5 IANT 10 IANL |
64 | 93.8% |
For IANL - ND by LT was 16.7%, by BSD 16.7% and by 2-PD test it was 25%. Total ND was 33.3%. For IANT - ND by LT was 66.7%, by BSD 33.3% and by 2-PD it was 55.6%. Total ND was 77.8%. Combined data from both techniques (IANL, IANT) by 2-PD test showed normal function in 61.9% of sites, diminished function in 33.33%, and no function in 4.8%. ND in IANT was bigger that in IANL. |
| Khajehahmadi et al. [4] |
14 IANT 14 IANL |
65 | 100% |
For IANT - vitality test showed negative results at 1 week, 1, 3, 6, 12 months follow-up. All had normal values at 1 week before operation. For IANL - only 2 patients (20%) had negative vitality test results for anterior teeth at 1 week follow-up. In both groups, deep numbness of lower lip was observed at 1 week follow-up. After 3 months, lip sensation by 2-PD and static LT was normal in both groups who continued to have hyperesthesia. At 12 months follow-up, the abnormal lip sensation persisted. |
| Ferrigno et al. [6] | 19 IANT | 46 | 95.7% |
ND (registered by LT, PT and 2-PD tests) detected was 15.8% (3/19) by LT test, 15.8% (3/19) by PT, and 21% (4/19) by 2-PD test. Total ND was 21.1% (4/19). 9 patients had sensory recovery immediately after local anaesthesia. 10 patients had ND: in 6 cases, a total return of sensation within 1 month, 2 patients did not completely recover until 6 months post-op, 1 patient did not completely recover until 12 months post-op, and 1 patient was still experiencing ND. |
| Karlis et al. [7] | 1 IANT | 2 | 0% | 4 weeks post-op patient had pain and moderate oedema on the operated site, and paresthesia on right lower lip and chin. Panoramic X-ray showed radiolucency around posterior implant with no displaced linear fracture through inferior mandibular border. First, closed reduction with maxillo-mandibular fixation was done. After 1 week, open reduction + debridement and internal rigid fixation including removal of both implants was done. Iliac bone graft was placed in the operated site. Normal healing observed after 6 weeks. 6 months later, paresthesia was persisted. |
| Kan et al. [8] | 1 IANT | 3 | 33.33% | 3 weeks post-op patient complained of pain in the operated site, clinical examination revealed mandibular body fracture at the two anterior implants area. 2 anterior implants were removed, open reduction + internal fixation with titanium mesh tray was done. Fracture healed without further complications. |
| Peleg et al. [10] | 10 IANL | 23 | 100% | 4 patients had sensory recovery immediately after local anaesthesia. 6 patients had hypoesthesia immediately post-op. 5 patients had a total return of sensation during 3 - 4 weeks. 1 patient had a complete recovery after 6 weeks. None of the patients experienced permanent ND. |
| Del Castillo Pardo et al. [14] |
1 IANL | 3 | 100% | Immediately post-op, the patient reported slight paresthesia of left half of the lower lip for few weeks. 6 months after implant placement, lip sensitivity was fully normal, and the patient had no paresthesia or neuralgias. |
| Proussaefs [15] | 1 IANT | 5 | 100% | The patient had only a transient hyperesthesia for 3 months. |
| Hashemi [16] | 11 IANL | - | - | Few complications were detected and IAN function presented in all patients. The average time for temporary anaesthesia was 7.3 days and after 3.3 months, in average, there was a complete recovery of the IAN. |
|
Vasconcelos et al. [17] |
1 IANT | 2 | 100% | Complete recovery of the sensitivity 7 months post-op. |
| Hashemi [18] | 110 IANL | - | - |
The patients had ND in the first week follow-up: anaesthesia in 81 sites, hypoesthesia in 9 sites, burning in 9 sites, pain in 8 sites, pinching in 2 sites and tickling in 1 site. At 1 month follow-up, ND disappeared in 81 sites (74%). ND was in 12 sites: tickling in 8 sites, burning in 5 and pain in 4. At the end of first month, 9 sites of hypoesthesia returned to normal. At the end of second month, 95 sites returned to normal and ND remained in 15 sites: hypoesthesia in 8 and tickling in 7. After 3 months, ND was reported in 6 sites: hypoesthesia in 3 and tickling in 3. At the end of 6 months the ND was in 3 sites with tickling. 82 patients (94%) were satisfied with the results. The most common ND was anaesthesia (81 sites); least common was pinching (2 sites). |
| Lorean et al. [19] |
68 IANL 11 IANT |
232 | 99.57% | 4 patients reported prolonged transient ND immediately post-op (5% of operations). The duration of post surgical ND was for 1 - 6 months, while in other cases for 0 - 4 weeks only. No permanent neural damage. No post-op sensibility of the anterior lower teeth. |
| Gasparini et al. [20] |
49 IANT | - | - | Complications were in 6 cases: 1 case (2.8%) of transient anaesthesia and 5 cases (14.3%) of transient hypoesthesia (spontaneously resolving after 6 months). Among the hypoesthesia cases, 4 were of discriminative type and 1 of thermal type (cold). After 6 months there was a remission of symptoms. |
| Barbu et al. [23] | 11 IANL | 32 | 100% | All patients had transient ND for 2 months. No permanent ND was detected. |
| Dal Ponte et al. [24] |
1 IANT | 2 | 100% | During 7 postoperative days the patient had paresthesia of lower lip with some tingling feeling. Laser applications were performed in the region to help sensitivity recovery. |
| Suzuki et al. [26] | 1 IANL | 2 | 100% | Patient had partial loss of sensitivity of right lower lip 7 days post-op, which was completely improved at 1 month follow-up. The results after loading were satisfactory. |
| Proussaefs [27] | 1 IANT | 2 | 100% | Transient hyperesthesia for 3 months was reported. 3 years post-loading revealed no clinical signs of pathosis (i.e., mobility, probing depth < 3 mm, pain, BOP) |
ND = neurosensory disturbances; LT = light touch; 2-PD = two point discrimination; PT = pain test; IANL = inferior alveolar nerve lateralization; IANT = inferior alveolar nerve transposition.
DISCUSSION
It was difficult to compare or organise ND and treatment results because different authors provided different information regarding the IANL and IANT results and outcomes. For example, Del Castillo Pardo et al. [14] and Proussaefs [15] wrote regarding the results of ND and relied only on subjective methods, such as questioning the patients about pain sensation or any other abnormal sensation, without performing any additional objective ND evaluation methods, while others (Ferrigno et al. [6]) used the following objective methods to evaluate ND in addition to subjective questioning: 2-PD, PT and LT. In other studies (Hashemi [16], Vasconcelos et al. [17] and Kan et al. [8]), meanwhile, no ND evaluation method was mentioned. In addition, some authors (Hashemi [18]) described only the ND evaluation of the IAN after the treatment, but failed mention the implant survival rate, while others (Kan et al. [3]) described both the ND and the implant survival rate. It was found, during our current review, that implant survival rate in the examined literature was relatively high (88% - 100%) except for two case reports, which presented a case regarding mandibular fracture as a complication of IANT and placement of endosseous implants. The first one is Karlis et al. [7]. In this case, both implants, which were placed during the procedure, were ultimately removed; therefore, the implant survival rate was 0%. The second case, presented by Kan et al. [8] showed an implant survival rate of 33.33% due to the removal of 2 out of 3 implants placed (Table 3).
We found, based upon the current selected literature, that the most popular procedure is IANL. We calculated that 62.2 % (235/378) of all the operations performed utilised IANL, and 37.8% (143/378) utilised IANT. Implant survival rates of 100% have been determined in 10 studies from the selected literature. Lorean et al. [19] showed an implant survival rate of 99.57%, Ferrigno et al. [6] showed an implant survival rate of 95.7%, Kan et al. [3] survival rate was 93.8%, and Chrcanovic et al. [2] showed an 88% implant survival rate. Three of the studies (Hashemi [16], Hashemi [18], Gasparini et al. [20]) we reviewed failed to mention either the number of implants placed or the implant survival rate (Table 3). Concerning the materials/techniques that are available in order to fill the space following IANL or IANT and implant placement, several methods are available, as mentioned in our previous part 1 article: repositioning the bony window that was removed or the bony window can be crushed and mixed with an allograft or xenograft. The mucoperiosteal flap is then sutured. Peleg et al. [10], demineralised freeze dried bone allograft (DFDBA) was placed between the implant and the inferior alveolar neurovascular bundle in order to avoid any direct contact between the two, protecting the neurovascular bundle from any mechanical or thermal trauma. A collagen membrane was placed lateral to the neurovascular bundle. Another option, as mentioned in Hassani et al. study [5], is to place a collagen membrane between the implant and the nferior alveolar neurovascular bundle. The advantage of bone over a membrane is that if proper healing occurs in the area, the contact area of implant and bone will increase. Regarding the implant type, non-treaded dental implants are indicated during IANL and IANT in order to avoid the risk of IAN paresthesia which can occur from direct contact between the IAN and the sharp implant threads [10].
The risks, complications and disadvantages of IANL and IANT
IANT is not currently considered a safe method; for that reason, it has received little consideration as a surgical technique for pre-prosthetic preparation of atrophic alveolar ridges in edentulous patients. Nevertheless, some authors have continued to analyse the validity of this surgical technique, especially in evaluating the residual functionality of the IAN following IANT. The reported risk of damage to the IAN ranges between 33% and 87%; however, in Gasparini et al. clinical study [20], only a 2.8% risk of anaesthesia and a 13.4% risk of hypoesthesia were documented. In another study, Bernd Quantius [21] observed temporary irritation of the mental nerve, appearing as paresthesia in 90% of the patients, but these irritations disappeared completely within 8 weeks. Certainly, IANT is associated with more risk than other jaw preparation techniques for implant-prosthetic rehabilitation; but, in some cases, IANT is the only method that allows implant-prosthetic rehabilitation with better outcomes, predictability and low biological cost for the patient.
Reconstructive methods and implant-prosthetic strategies for the edentulous mandible in Cawood and Howell [22] classes V and VI are different, including short implants, regenerative techniques, autologous, homologous, or heterologous inlay or onlay bone grafts, and osteodistraction. However, each of these methods is connected with a certain amount of risks [20]. The major risk and postoperative complications of this surgical procedure (as with any surgery whereby a peripheral nerve is moved from its physiological site) is irritation of the inferior neurovascular bundle, with resultant ND to IAN and its terminal branches. These may include: hypoesthesia (partial loss of sensitivity), paresthesia (abnormal response to stimuli), hyperesthesia (hypersensitivity to all stimuli, except for special senses), transient anaesthesia and numbness, as well as temporary or permanent dysfunction of the lower lip and chin (loss of sensation of its terminal incisive branch). This is of no consequence for people who are edentulous in the anterior mandible, but it may cause some disturbance to residual dental and periodontal sensibility in any remaining anterior teeth. In addition, damage to IAN can result in ND in the mental nerve [1].
IANT is likely to be the most traumatic manoeuvre for the nerve. 10 - 17% traction is enough for the fibres to temporarily lose their conduction ability. A spatula-caused traction in the mucoperiosteal flap can lead to nerve twisting, even in areas far from the inured nerve. Therefore, more severe stretch damage may result in partial lesions of the axons and their myelin sheaths. This may lead to loss of sensibility as a result of stretching of the nerve [2].
Functional recovery depends on the nervous fibres’ regeneration ability and speed, which may vary between 1 to 3 mm a day [2]. Vascular damage can also jeopardise nerve function and recovery and may also cause loss of sensibility. Inferior alveolar artery revascularization initiates the regeneration process. Blood arterial pressure helps maintain the canal size and promotes bone remodelling at the surgical site (with no appropriate revascularization, the canal becomes obstructed in about 12 months after surgery). Nerve regeneration goes hand in hand with bone remodelling by directing the growth of the nerve proximal stump toward the distal end of the injured nerve, thus preventing random growth. The process of nerve regeneration after compression or less severe crush injuries usually requires several weeks to 6 months; if there is no sensory recovery during this time, permanent loss of continuity in the nerve trunk should be expected [2].
Other complications/risks after this procedure include mandibular fracture at the operation site (the area of the bony window). The mandible is weakened by the removal of the buccal corticalis, and the simultaneous crestal implantation makes the mandible more susceptible to masticatory forces. Therefore, there is significant loss of structural integrity when a portion of the buccal cortex is removed during the lateralization procedure and combination with the placement of multiple implants can contribute to a potential fracture [1,2,17,19,21,23].
Other complications include implant loss, haemorrhage (result from transaction of the neurovascular bundle) and osteomyelitis [24]. Therefore, it is important for the clinician to perform a through surgical risk assessment, because the major reason for using this technique is to prevent IAN damage. In addition, this procedure is technically difficult and requires adequate experience. The surgeon should have adequate experience, sufficient anatomical knowledge and necessary skills to fully manage preoperative and postoperative complications.
Limitations
The main limitations of this review were that 10 authors [3,7,8,14,15,17,23,24,26,27] used a low number (< 10) of patients (it was decided in this review that < 10 will indicate a low number of patients), nine authors [2,7,10,14,15,18,23,24,27] used only one ND evaluation method and 4 authors [8,16,17,26] failed to mention the ND evaluation method. Eight authors [2-4,16,17,24,26,27] selected the patients randomly. Four authors [2,4,19,23] did not indicate the exact post-operative outcomes for each patient.
CONCLUSIONS
Inferior alveolar nerve repositioning is related with initial change in sensation in majority of cases for 1 to 6 months. The most popular causes of inferior alveolar nerve damage are; spatula-caused traction in mucoperiosteal flap, pressure due to severe inflammation or retention of fluid around the nerve trunk and subsequent development of transient ischemia, and mandibular body fracture. 99.47% (376/378) of procedures presented in this review, showed neurosensory disturbances and complications which were transient, while only 0.53% (2/378) of procedures demonstrate permanent neurosensory disturbances.
Acknowledgments
ACKNOWLEDGMENTS AND DISCLOSURE STATEMENTS
The authors report no conflicts of interest related to this study.
REFERENCES
- 1.Morrison A, Chiarot M, Kirby S. Mental nerve function after inferior alveolar nerve transposition for placement of dental implants. J Can Dent Assoc. 2002 Jan;68(1):46-50. [PubMed]
- 2.Chrcanovic BR, Custódio AL. Inferior alveolar nerve lateral transposition. Oral Maxillofac Surg. 2009 Dec;13(4):213-9. Review. [DOI] [PubMed]
- 3.Kan JY, Lozada JL, Goodacre CJ, Davis WH, Hanisch O. Endosseous implant placement in conjunction with inferior alveolar nerve transposition: an evaluation of neurosensory disturbance. Int J Oral Maxillofac Implants. 1997 Jul-Aug;12(4):463-71. [PubMed]
- 4.Khajehahmadi S, Rahpeyma A, Bidar M, Jafarzadeh H. Vitality of intact teeth anterior to the mental foramen after inferior alveolar nerve repositioning: nerve transpositioning versus nerve lateralization. Int J Oral Maxillofac Surg. 2013 Sep;42(9):1073-8. [DOI] [PubMed]
- 5.Hassani A, Motamedi MHK, Saadat S. Inferior alveolar nerve transpositioning for implant placement. Oral Maxillofac Surg. 2013 Jun;26. URL: http://cdn.intechopen.com/pdfs/44588/InTech-Inferior_alveolar_nerve_transpositioning_for_implant_placement.pdf. [DOI]
- 6.Ferrigno N, Laureti M, Fanali S. Inferior alveolar nerve transposition in conjunction with implant placement. Int J Oral Maxillofac Implants. 2005 Jul-Aug;20(4):610-20. [PubMed]
- 7.Karlis V, Bae RD, Glickman RS. Mandibular fracture as a complication of inferior alveolar nerve transposition and placement of endosseous implants: a case report. Implant Dent. 2003;12(3):211-6. [DOI] [PubMed]
- 8.Kan JY, Lozada JL, Boyne PJ, Goodacre CJ, Rungcharassaeng K. Mandibular fracture after endosseous implant placement in conjunction with inferior alveolar nerve transposition: a patient treatment report. Int J Oral Maxillofac Implants. 1997 Sep-Oct;12(5):655-9. [PubMed]
- 9.Fernández Díaz JÓ, Naval Gías L. Rehabilitation of edentulous posterior atrophic mandible: inferior alveolar nerve lateralization by piezotome and immediate implant placement. Int J Oral Maxillofac Surg. 2013 Apr;42(4):521-6. [DOI] [PubMed]
- 10.Peleg M, Mazor Z, Chaushu G, Garg AK. Lateralization of the inferior alveolar nerve with simultaneous implant placement: a modified technique. Int J Oral Maxillofac Implants. 2002 Jan-Feb;17(1):101-6. [PubMed]
- 11.Chien PF, Khan KS, Siassakos D. Registration of systematic reviews: PROSPERO. BJOG. 2012 Jul;119(8):903-5. [DOI] [PubMed]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336-41. [DOI] [PubMed]
- 13.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Wiley, 2008:187-241. URL: http://www.cochrane.org/cochrane-interventions-handbook.
- 14.Del Castillo Pardo de Vera JL, Chamorro Pons M, Cebrián Carretero JL. Repositioning of the inferior alveolar nerve in cases of severe mandibular atrophy. a clinical case. Med Oral Patol Oral Cir Bucal. 2008 Dec 1;13(12):E778-82. [PubMed]
- 15.Proussaefs P. Inferior alveolar nerve transposing in a situation with minimal bone height: a clinical report. J Oral Implantol. 2005;31(4):180-5. [DOI] [PubMed]
- 16.Hashemi HM. A modified technique of inferior alveolar nerve repositioning: results in 11 patients. Acta Med Iran. 2006;44(4): 273-6. URL: http://acta.tums.ac.ir/index.php/acta/article/viewFile/3131/2817.
- 17.Vasconcelos Jde A, Avila GB, Ribeiro JC, Dias SC, Pereira LJ. Inferior alveolar nerve transposition with involvement of the mental foramen for implant placement. Med Oral Patol Oral Cir Bucal. 2008 Nov 1;13(11):E722-5. [PubMed]
- 18.Hashemi HM. Neurosensory function following mandibular nerve lateralization for placement of implants. Int J Oral Maxillofac Surg. 2010 May;39(5):452-6. [DOI] [PubMed]
- 19.Lorean A, Kablan F, Mazor Z, Mijiritsky E, Russe P, Barbu H, Levin L. Inferior alveolar nerve transposition and reposition for dental implant placement in edentulous or partially edentulous mandibles: a multicenter retrospective study. Int J Oral Maxillofac Surg. 2013 May;42(5):656-9. [DOI] [PubMed]
- 20.Gasparini G, Boniello R, Saponaro G, Marianetti TM, Foresta E, Torroni A, Longo G, Azzuni C, Cervelli D, Pelo S. Long term follow-up in inferior alveolar nerve transposition: our experience. Biomed Res Int. 2014;2014:170602. [DOI] [PMC free article] [PubMed]
- 21.Quantius B. Lateralization of the inferior alveolar nerve. Report. Implants. 2010 Mar. URL: http://www.dentaltribune.com/printarchive/download/document/14688/file/70fe9b6c8636972986229d4aeb1a1e76_18-21.pdf.
- 22.Cawood JI, Howell RA. A classification of the edentulous jaws. Int J OralMaxillofac Surg. 1988 Aug;17(4):232-6. [DOI] [PubMed]
- 23.Barbu HM, Levin L, Bucur MB, Comaneanu RM, Lorean A. A modified surgical technique for inferior alveolar nerve repositioning on severely atrophic mandibles: case series of 11 consecutive surgical procedures. Chirurgia (Bucur). 2014 Jan-Feb;109(1):111-6. [PubMed]
- 24.Dal Ponte GL, Toledo GL, Toledo-Filho JL, Marzola C, Pastori CM, Zorzetto DL, Capelari MM. Lateralization and transposition use of the inferior alveolar nerve before the advent of short implants. Surgery and Maxillofacial Traumatology sponsored by the Hospital Association of Bauru - Base Hospital and the Brazilian College of Oral and Maxillofacial Surgery and Traumatology. URL: http://www.actiradentes.com.br/revista/2011/textos/35RevistaATO-Use_of_Lateralization_and_transposition-2011.pdf.
- 25.Vetromilla BM, Moura LB, Sonego CL, Torriani MA, Chagas OL Jr. Complications associated with inferior alveolar nerve repositioning for dental implant placement: a systematic review. Int J Oral Maxillofac Surg. 2014 Nov;43(11):1360-6. [DOI] [PubMed]
- 26.Suzuki D, Bassi AP, Lee HJ, Alcântara PR, de Sartori IM, Luvizuto ER, Faco EF, Faot F. Inferior alveolar nerve lateralization and implant placement in atrophic posterior mandible. J Craniofac Surg. 2012 Jul;23(4):e347-9. [DOI] [PubMed]
- 27.Proussaefs P. Vertical alveolar ridge augmentation prior to inferior alveolar nerve repositioning: a patient report. Int J Oral Maxillofac Implants. 2005 Mar-Apr;20(2):296-301. [PubMed]