Abstract
Background
Arthritis of the PIP joint is a debilitating condition commonly treated with arthroplasty. The pyrolytic carbon (pyrocarbon) implant has been developed for PIP joint arthroplasty in these patients. This prospective outcomes study will evaluate the outcomes and complications of the pyrocarbon implant for the PIP joint.
Methods
Consecutive candidates for PIP joint arthroplasty with pyrocarbon implant were prospectively evaluated. Functional measurements and the Michigan Hand Outcomes Questionnaire (MHQ) were administered pre-operatively and at 3, 6 and 12 months postoperatively. Pre-operative means and 12-month post-operative means for all functional measures were compared using paired t-tests and nonparametric Wilcoxon signed-rank sum test, and effect size was reported for MHQ.
Results
Fourteen patients treated with 21 implants enrolled in the study. At the 12-month follow-up period, mean active arc of motion (AAM) was 38°, decreasing slightly from the pre-operative value. Mean grip strength improved from 11.3 kg to 15.1 kg, although the difference was not statistically significant. Mean key pinch values improved significantly from 6.6 kg pre-operatively to 9.2 kg at the 12-month follow-up time (p=0.03). Jebsen-Taylor test scores showed improvement, although not significantly. Changes in all MHQ domains showed high effect size. Complications were minimal. Three patients experienced squeaking of the implant and three patients experienced dislocation of the pyrocarbon joint.
Conclusions
The pyrocarbon implant for PIP joint arthroplasty shows encouraging results, primarily in patient satisfaction and pain relief, but is associated with complications related to implant dislocations, which required prolonged treatment with external fixators.
Keywords: Proximal interphalangeal joint, pyrolytic carbon, implant arthroplasty, arthroplasty outcomes
According to the Centers for Disease Control and Prevention, rheumatic disease is one the most prevalent chronic illnesses in the country and is the leading cause of disability among U.S. adults. (1) The proximal interphalangeal (PIP) joint of the hand is often affected. In a 2006 community-based study (N = 3327) by the Arthritis Research Institute of America, approximately 18% of those over the age of 40 demonstrated radiographic evidence of PIP joint osteoarthritis (OA). (2) By the year 2030, a projected 40 million people aged 65 years and older will have arthritis. (1) The social and economic costs of arthritis pose a substantial healthcare burden that is likely to rise as longevity increases and the population ages
Treatment of PIP joint arthritis remains a difficult problem. Current treatment choices include medication, arthroplasty and fusion. Many patients can live with the pain, deformity, and weakness if it is not disabling. When pain becomes refractory to medications and weakness affects day-to-day activities, surgical treatment is often necessary to maintain reasonable hand function. Because most of the active arc of motion for the finger starts at the metacarpophalangeal joint (MCP), fusion of the PIP joint is generally acceptable. Although fusion can reliably decrease pain, the loss of motion of the PIP joint, particularly for the ulnar two digits, hinders hand performance because it creates difficulty in power grip. (3)
The silicone-type implant has been used for MCP and PIP joint arthroplasty for the past 40 years. However, this type of implant is not anatomic and implant fracture and dislocation, inflammatory synovitis, joint deformity, heterotopic bone formation, erosive reaction to implant debris, and loss of motion are quite common. (4–12) It has been estimated that silicone-type implant arthroplasty is associated with a 19% complication rate. (4) Advances in small joint arthroplasty demand innovative, anatomic implant designs that are analogous to the advances in hip and knee arthroplasty.
Recent development of a surface replacing implant using a novel material, pyrolytic carbon, appears to be promising and is gaining popularity for PIP joints of the fingers. Pyrolytic carbon is a synthetic material that is wear-resistant and biocompatible - unique properties that make it especially useful for small joint prostheses. (2) While most of the published literature using the pyrocarbon implant has thus far focused on the MCP joint, (4, 13–18) this will be one of the few prospective studies to evaluate the outcomes and complication rates for this type of implant for the PIP joint. Additionally, this study established an a priori protocol by applying physical measurements, a test that simulated activities of daily living (the Jebsen-Taylor Test), and a validated patient-rated outcomes assessment by using the Michigan Hand Outcomes Questionnaire (MHQ). The specific aim of this study is to assess outcomes and complication rates of a consecutive series of patients undergoing PIP joint arthroplasty using the pyrocarbon implant.
Materials and Methods
Consecutive candidates for PIP joint arthroplasty with the pyrocarbon implant (Ascension Orthopedics, Austin, TX) were approached by a research associate regarding study participation following their decision to undergo the procedure. The primary indication for the procedure was intractable pain in the PIP joint. Study inclusion criteria included age of 18 years or older, the ability to read and write in English and the cognitive ability to complete the outcome assessments. Every patient who presented during the study period met the inclusion criteria and was successfully recruited. Written informed consent was obtained from each patient. This study was approved by the University of Michigan Medical School Institutional Review Board.
Functional Assessment
Functional measurements, grip strength, key pinch strength and active arc of motion (AAM), were assessed pre-operatively and at 3, 6 and 12 months post-operatively. Grip and pinch strength were measured by a research associate with a Jamar dynamometer (Sammons Preston Rolyan, Bolingbrook, IL) and a pinch gauge (B&L Engineering, Tustin CA), respectively. AAM was measured by an independent certified hand therapist. The Jebsen-Taylor test, a validated measure of hand function that simulates activities of daily living (ADLs),(19) was also administered at each follow-up visit. We excluded the writing portion of the Jebsen-Taylor test because writing ability is dependent on hand dominance, and prior studies have reported difficulty interpreting this portion of the test. (19, 20)
Patient-rated Assessment
The Michigan Hand Outcomes Questionnaire (MHQ) was administered pre-operatively and at 3, 6 and 12 months post-operatively. The MHQ is a self-administered instrument that measures six health-status domains that are important to patients with hand disorders: (1) overall hand function, (2) ADLs, (3) pain, (4) work performance, (5) aesthetics, and (6) patient satisfaction. (21) The responsiveness, reliability, and validity of the MHQ have been proven for a variety of common hand conditions. (22–26)
Statistical Analysis
Means and standard deviations for functional data were calculated for each follow-up time point. For grip strength and key pinch strength, the percent of the contralateral hand was also calculated. The resulting percentage was adjusted for the 10% increase in strength of the dominant hand, per the standard method to correct for hand dominance. (27) Pre-operative means and 12-month post-operative means for all measures were compared using paired t-tests. Because normality could not be established, if a statistically significant change was detected by the paired t-test, the significance was confirmed with the comparable nonparametric Wilcoxon signed-rank sum test. In these cases, both p-values are reported. Significance was set at p-value of 0.05.
Means and standard deviations were also calculated for overall MHQ score and for all subscales. Improvement from pre-operative to 12-month post-operative scores was determined with effect size; an effect size of 0.2 was defined as small, 0.5 as medium and 0.8 as a large effect, based on Cohen’s criteria. (28) All data analysis was done using SAS 9.1 (SAS Institute, Cary, NC) statistical analysis software.
Surgical Technique
The surgical technique has been described previously by the senior author (KCC) and will be briefly outlined. (3)
Preoperative Examination/Imaging
Three views of the hand are essential to evaluate the structural integrity of the small joints of the hand. Occasionally, CT scan of the joints may be necessary to assess the condition of the articular cartilage to determine if arthroplasty is warranted versus capsular/ligament release.
PIP Joint Approach
The procedure is performed under tourniquet control with the patient in the supine position. The PIP joint is approached using a lazy-S incision on the dorsum of the joint. This incision provides wide exposure of the joint. After the arthroplasty, the lazy-S incision can be closed by recruiting lateral skin to decrease tension on the skin flap during flexion of the PIP joint. There are two incisions to expose the extensor mechanism. The widest exposure is a chevron incision that detaches the extensor tendon proximally while the central tendon remains inserted distally. The tendon is reflected distally and the entire joint is fully exposed. This exposure must be performed cautiously because the subsequent tendon repair may stretch out during therapy, resulting in an extension lag. The senior author’s preference is a tendon splitting incision that will maintain the tendon integrity. This incision requires traction of the split extensor tendon during the surgical procedure, but the tendon can be closed in a side-to-side fashion that will not stretch out during therapy.
Step 1: Preparation of the Proximal Phalanx
A starter awl is placed through the interval between the condyles of the head of the PIP joint to create a medullary canal. The medullary canal is centered at the axis of the proximal phalanx using an alignment awl and an alignment guide. After creating the medullary canal in the proximal phalanx, a vertical cutting guide is placed over the head of the proximal phalanx, and a saw is used to cut the proximal phalanx just proximal to the head of the condyles. This vertical proximal osteotomy is made 1–2mm distal from the attachment of the collateral ligaments. A series of broaches are sequentially inserted into the proximal phalanx, starting with a no. 10 broach and increasing to the largest broach that can be accommodated within the medullary canal. The broach must be fully inserted into the medullary canal to fully accommodate the implant. An oblique cutting guide is then placed into the cut proximal phalanx to complete the volar oblique osteotomy. The proximal phalanx is now ready to accommodate the trial proximal phalanx implant. The pyrocarbon implant is press-fit, and cement is not used.
Step 2: Preparation of the Middle Phalanx
A small oval bur is used to remove the articular surface of the middle phalanx and create a gentle trough that can accommodate the middle phalanx implant. Bone is not resected from the middle phalanx. The medullary canal is broached sequentially to obtain the largest implant that can be accommodated within the medullary cavity. After adequate placement of the trial implant with the PIP joint moving smoothly, the implant is press-fit into the medullary cavity. If the implant is excessively tight, additional bone should be resected from the proximal phalanx. The extensor tendon is closed and the finger is splinted in full extension.
Postoperative Care
The joint should be kept in extension for 3 weeks after the operation to consolidate the soft tissue support. One week after the operation, an 8-week program of flexion and extension exercises are started in a dynamic splint. A static resting splint can be worn at night for 2 months after the therapy protocol is completed.
Results
Between November 2004 and July 2008, 21 PIP joint arthroplasty with pyrocarbon implant procedures were performed on 14 patients. Ten patients had single procedures and 4 patients had multiple procedures. In patients with multiple procedures, the mean duration between procedures was 41 weeks. Each procedure was performed separately because of the technical difficulty associated with this procedure and the possibility of dislocation. One pyrocarbon implant replaced an existing silicone implant and one procedure was performed after the patient had an unsuccessful microvascular toe joint transfer because of limited motion and deviation of joint, which hindered the other fingers. The demographic information is presented in Table 1.
Table 1.
Patient Demographic Data
| Number of procedures | 21 |
| Number of patients | 14 |
| Gender distribution (F/M) | 9/5 |
| Age (range) | 54 (34–72) |
| Female (range) | 58 (52–63) |
| Male (range) | 47 (34–72) |
| Etiology | |
| Osteoarthritis | 10 |
| Post-traumatic Arthritis | 3 |
| Psoriatic Arthritis | 1 |
| Laterality of procedure | |
| Right | 11 |
| Left | 10 |
| Digit involved | |
| Index | 6 |
| Middle | 9 |
| Ring | 5 |
| Little | 1 |
Functional Outcomes
Functional outcomes data are presented in Table 2. Pre-operative functional data are available for 13 patients. Nine patients provided 3 and 6 month data and 6 patients supplied 12 month functional data. Given that there are very few prospective studies of PIP joint arthroplasty with pyrocarbon implants, we felt it was necessary to publish our results despite some patients not reaching all follow-up points at the time of writing. With the increasing popularity of this implant design, the outcomes and complication rate of this procedure in a prospective cohort study design will provide high level of evidence data to guide surgeons and patients on whether to choose this procedure for arthritic PIP joints. Patients are continued to be recruited and followed in this prospective longitudinal series.
Table 2.
Functional Outcomes Data
| Pre-operative ± SD | 3 months ± SD | 6 months ± SD | 12 months ± SD | t-test p-value | Wilcoxon signed-rank test p-value* | |
|---|---|---|---|---|---|---|
| Grip strength (kg) | 11.3 ± 9.9 | 19.0 ± 18.5 | 22.5 ± 20.7 | 15.1 ± 12.9 | 0.53 | 0.56 |
| Grip strength, % of contralateral hand | 53.0 ± 20.1 | 85.3 ± 47.7 | 64.3 ± 26.0 | 66.3 ± 26.4 | 0.62 | 0.88 |
| Key pinch (kg) | 6.6 ± 2.8 | 7.4 ± 2.8 | 8.8 ± 3.2 | 9.2 ± 2.9 | 0.006 | 0.03 |
| Key pinch, % of contralateral hand | 84.9 ± 18.7 | 88.0 ± 16.4 | 88.2 ± 11.8 | 98.8 ± 9.2 | 0.05 | 0.06 |
| Jebsen-Taylor score (seconds) | 33.7 ± 6.6 | 39.8 ± 4.0 | 29.1 ± 4.8 | 27.8 ± 2.7 | 0.03 | 0.06 |
| Active Arc of Motion (degrees) | 40 ± 17 | 45 ± 15 | 47 ± 19 | 38 ± 18 | 0.64 | 0.88 |
p-value calculated using paired t-tests and Wilcoxon signed rank sum test for nonparametric paired samples comparing pre-operative mean and 12-month means (significance at p< 0.05)
Grip strength improved post-operatively, but decreased slightly at the 12-month follow-up point. Grip strength as a percentage of the contralateral hand followed a similar pattern. Key pinch strength showed little change between the pre-operative and 6-month visits, but had a significant increase over pre-operative measurement at 12 months (t-test p=0.006; Wilcoxon signed-rank test p=0.03). As a percentage of the contralateral hand, key pinch strength remained essentially unchanged until the 6–12 month period, when it showed a marked increase. Jebsen-Taylor test scores improved steadily over the study period.
AAM data were available for 20 joints pre-operatively, 12 joints at 3 months, 11 joints at 6 months and 10 joints at 12 months. There was no meaningful change in AAM over the study period. This is not unusual; only one out of eight previous studies of PIP arthroplasty using the pyrocarbon implant have demonstrated a significant increase in post-operative AAM (11, 29–31)
Patient-rated Outcomes
MHQ data were available for 13 patients pre-operatively, for 10 patients at 3 months and 6 months and for 6 patients at 12 months. All domains of the MHQ showed large effect sizes (effect size >0.8), indicating that pyrocarbon implant arthroplasty improves many aspects of patients’ lives. (Figure 1, Table 3) Among those showing the largest effects were Pain (effect size=3.5), Satisfaction (effect size=2.3) and Aesthetics (effect size=2.2). All domains, with the exception of Work, demonstrated their biggest jump in score between the pre-operative point and the 3-month follow-up point. This indicates that patients observed improvement quite early in the recovery period. Despite no improvement in motion or grip strengths, patients reported increased Satisfaction 12 months following surgery (effect size=2.3). This signifies that decreased pain, a more aesthetically pleasing hand and an increased ability to perform ADLs are more important to patients than increased AAM or grip strength.
Figure 1.
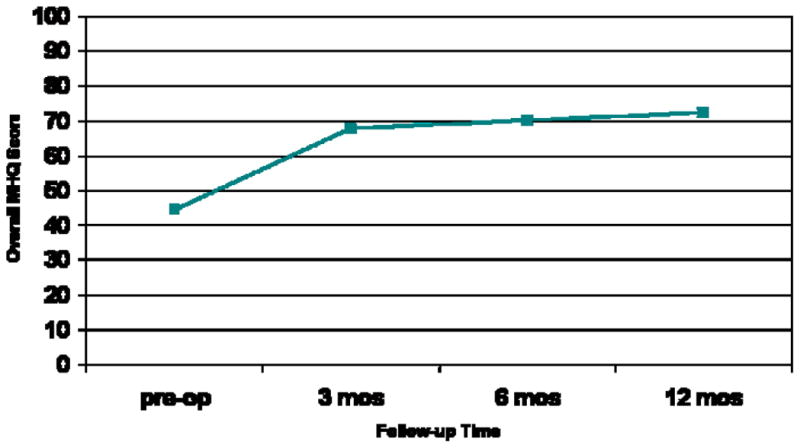
Mean overall MHQ score by time points.
Table 3.
Michigan Hand Outcomes Questionnaire (MHQ) Data#
| Domain | Pre-operative ± SD | 3 months ± SD | 6 months ± SD | 12 months ± SD | Effect size¥ |
|---|---|---|---|---|---|
| Overall | 45 ± 11 | 68 ± 15 | 70 ± 16 | 72 ± 15 | 2.3 |
| Function | 54 ± 16 | 75 ± 11 | 77 ± 12 | 67 ± 16 | 0.9 |
| ADL§ | 57 ± 20 | 72 ± 25 | 78 ± 18 | 81 ± 17 | 1.5 |
| Work | 56 ± 21 | 65 ± 30 | 72 ± 23 | 77 ± 19 | 1.3 |
| Pain | 66 ± 13 | 33 ± 23 | 39 ± 21 | 22 ± 19 | 3.5 |
| Aesthetics | 34 ± 21 | 55 ± 24 | 63 ± 29 | 70 ± 21 | 2.2 |
| Satisfaction | 32 ± 12 | 65 ± 19 | 70 ± 21 | 61 ± 31 | 2.3 |
The MHQ domains are based on a scale of 0 to 100. For all domains except pain a higher score indicates better performance. For the pain domain a lower score indicates less pain
The effect size is defined as (mean2 − mean1)/(Standardized Response Mean). For example for the Overall MHQ score effect size = (72 − 45)/(11.9) = 2.3. Effect size of 0.2 is small, 0.5 is medium and 0.8 is large.
Activities of Daily Living
Complications
There were few complications seen during the study period. Three patients experienced dislocation of the pyrocarbon joint. The first, a right index finger, presented 13 days after surgery with this complication. The second, a left middle finger, presented 6 days after surgery. The third, which presented 5 days post-surgery, was a right ring finger. This patient previously had 3 pyrocarbon implants placed without complications. All three joints were reduced and stabilized with 6 to 8 weeks of external fixation and the ligamentous support tightened sufficiently to avoid problems with dislocation. Three additional patients experienced intermittent squeaking of the pyrocarbon joint. Joint squeaking was most pronounced during finger flexion, but was not associated with any pain. It was postulated that the stress on the implant may be responsible for this implant. (11) None of the patients had any other complaints and all three were satisfied with the results.
Patient Reports
Case 1
A 63-year-old right hand dominant teacher with a long history of osteoarthritis (OA) affecting multiple joints of the hands had previously had PIP joint arthroplasty using a silicone implant on the right index finger. The implant became dislocated, which caused finger deviation and reduced function. (Figure 2) She had also developed pain in the right index PIP joint, on which she chose to have pyrocarbon arthroplasty. Her recovery was unremarkable (Figure 3) and she was so pleased with the results she opted to have pyrocarbon arthroplasty on the left middle PIP joint and to have the silicone implant in the left index PIP joint replaced with a pyrocarbon implant. Unfortunately, the ligamentous support of the left index finger was not suitable for the pyrocarbon implant and the joint was fused. (Figure 4) Following these two procedures, the patient’s recovery was again unremarkable and she is scheduled to have a pyrocarbon implant placed in the left ring finger PIP joint as well.
Figure 2.
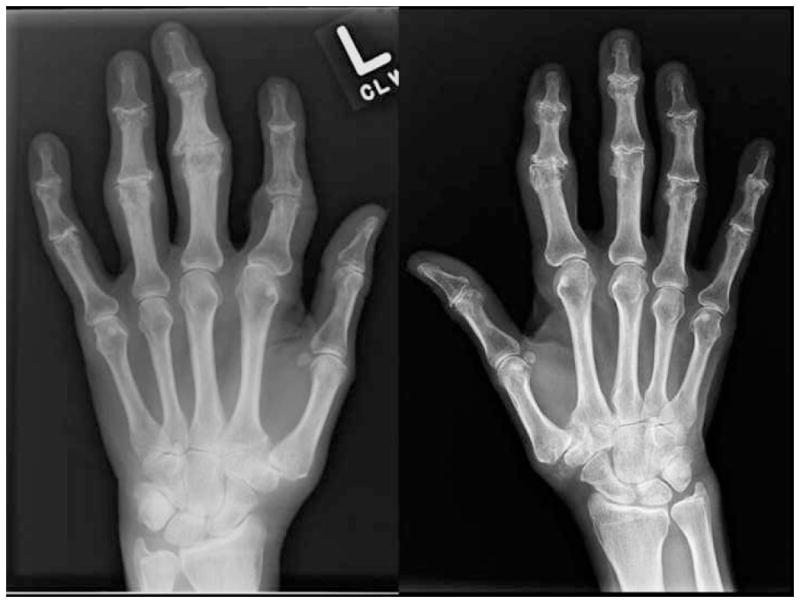
63-year-old female with a long history of osteoarthritis. Note the silicone implant and deformity of the left index PIP joint (left x-ray). The osteoarthritic PIP joints in the right index (right x-ray) and left middle fingers will be replaced by pyrocarbon implants.
Figure 3.
Right index PIP pyrocarbon joint.
Figure 4.

Left hand, placement of pyrocarbon implant in left middle PIP joint, and removal of silicone implant and fusion of left index PIP joint.
Case 2
A 37-year-old right hand dominant photographer with a 10-year history of psoriatic arthritis presented with long-standing left middle finger pain. Six days after pyrocarbon arthroplasty, it was noted that the joint had become dislocated. (Figure 5) Ligament support is crucial in this unconstrained two-piece implant design and the loss of joint space should be a clear sign that the ligaments would not be sufficiently strong to support this implant after joint resection. An external fixator was placed the next day. One week following surgery, the joint was stable and there were no problems with the external fixator. (Figure 6) Four days later, the external fixator became infected and had to be exchanged with a new one over the opposite side of the finger. After 8 weeks of external fixation to allow tightening of the reconstructed collateral ligaments, the joint was stable. (Figure 7) The patient reported no problems and good motion at the 12-month follow-up visit. For patients with unstable PIP joints due to insufficient soft tissue support, dislocation can occur and these patients are best treated with fusion.
Figure 5.

35-year-old male with dislocated left middle PIP pyrocarbon joint.
Figure 6.

Stabilized left middle PIP joint with external fixator.
Figure 7.

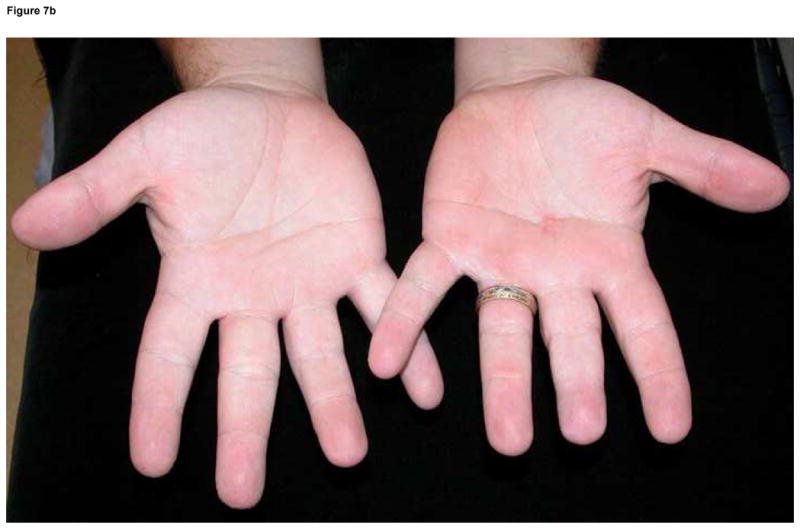

Figure 7a. Stable and mobile left middle PIP joint.
Figures 7b & 7c. Extension (b) and flexion (c) views showing good motion of the left middle PIP joint
Discussion
Treatment for PIP joint arthritis has been an ongoing challenge for hand surgeons. PIP fusion has been the conventional treatment for the index and middle fingers because these two digits require stability for fine pinch, in contrast to the ring and little fingers that require motion for power grip. Loss of motion after fusion can be unacceptable for patients who require mobility from the PIP joint to maintain its functional use.
The production of the silicone prosthesis in the 1960s strongly contributed to the progress of small joint arthroplasty. The silicone implant has since been the standard of treatment for PIP joint arthroplasty. Although this treatment has been shown to eliminate pain, it is prone to implant fracture and dislocation. (5) A recent meta-analysis of treatment for post-traumatic arthritis in PIP joints showed that the use of silicone implants and vascularized toe joint implants were associated with high rates of surgical revision (18% and 29%, respectively) and mediocre AAM (approximately 44° and 37°, respectively). (4) Disappointing outcomes associated with these traditional procedures emphasize the great need for more effective and less complication-prone implant designs.
Pyrocarbon implants are the latest technology in the field and show potential for treating a variety of PIP pathologies including arthritis, ankylosis, instability, deformity, and acute trauma. (32) The prosthesis is a bicondylar total joint that facilitates flexion-extension motion. (33) It is unconstrained and uncemented and requires minimal bone resection, allowing the preservation of the collateral ligaments for joint stabilization. (30, 34) The unconstrained design employs a ball-and-socket configuration that permits excellent movement and prevents subluxation of the joint. Additionally, the stem of the prosthesis complements the finger anatomy and fills the medullary canal. (33) This is thought to disperse forces generated along the bone-implant interface, which preserves surrounding tissue and assures fixation. (34) The actual pyrolytic carbon is a synthetic coating that is applied to a portion of preshaped graphite by heating a hydrocarbon gas. Pyrolytic carbon has been shown to be biocompatible and extremely durable via more than 10 million patient-years of experience with the material as a component of artificial heart valves. (11, 17, 18, 34–36) Because the pyrocarbon implant better matches the joint mechanics of the fingers and the physiologic characteristics of the joint environment, it is believed to have a longer implant life with superior function. (37–39)
The pyrocarbon device was designed to mirror the anatomic construct of the finger to achieve better outcomes with fewer complications. As such, it has become the preferred implant for OA-related arthroplasty. In March 2002, the U.S. FDA approved the implant under the Humanitarian Device Exemption to market the product as a Humanitarian Use Device. This designation allows the implant to be used extensively without the intensive effectiveness testing that other devices must undergo. The pyrocarbon implant’s unique synthetic properties and excellent mimicry of natural joint movements makes it an exciting development in the area of small joint arthroplasty.
The MCP joint is particularly well suited for the pyrocarbon implant because the strong ligamentous supports provided by the intermetacarpal and tight collateral ligaments assure implant stability for arthroplasty. (3) The favorable anatomy of this joint is reflected by high satisfaction rates of those who have received the pyrocarbon implant for osteoarthritic MCP joint conditions. (4, 13–16, 18) However, for rheumatoid arthritis (RA) involving the MCP joint, the senior author is reluctant to use the pyrocarbon implant because the unconstrained nature of the implant coupled with the ligament laxity associated with RA can lead to recurrent ulnar drift and dislocation.
The pyrocarbon implant has not been applied as widely for the PIP joint because of the potential for dislocation due to the tenuous ligamentous support for this hinge-type joint. When indicated, however, the senior author has employed this implant design for the PIP joints and has obtained satisfactory results. An arthritic PIP joint causing Boutonniere’s deformity with joint destruction may be contraindicated for the use of this implant because the amount of bone resection would be excessive and the removal of the collateral ligaments will destabilize the joint. For patients with joint destruction associated with Swan-neck deformity, on the other hand, the amount of bone resected is modest and the pyrocarbon implant may be indicated to achieve better flexion of the fingers to improve grip.
While the mean post-surgical AAM ranges between a modest 38°–45°, the mean MHQ Satisfaction scores range from 65–70, which may seem comparatively high considering the functional outcomes were not exceptional. In the authors’ opinion, it is likely that the ability to maintain satisfactory motion and to avoid fusion is adequate for patients to be satisfied in spite of minimal AAM gains. The AAM with the pyrocarbon implant in this series is comparable to the gains typically seen with the silicone implant. However, long-term functional outcomes are still unknown. There is hope that the pyrocarbon implant’s biomechanical advantage over the silicone implant will translate into increased longevity with fewer long-term complications, which would be especially useful for the ring and little fingers because of their need for power grip and motion.
Because it is a newer technology, the pyrolytic carbon implant has not been well investigated. To date, only eight studies of pyrolytic carbon arthroplasty for the PIP joint have been published. Stutz et al. in 2005, retrospectively evaluated the outcomes of 13 pyrolytic PIP joint procedures between 9–12 months after surgery. (40) Of note is the significant improvement in AAM from 51° preoperatively to 77° postoperatively along with an 80% reduction in pain based on the visual analog scale. (40) Schulz et al., in 2005, reviewed the results of 20 patients with a follow-up period ranging from 6 months to 2.5 years. (41) An analysis of radiographs indicated signs of periprosthetic cysts, osteophytes, and loosening of the proximal and distal components of the implant in some patients - short-term complications commonly seen with the silicone prosthesis. (4–12) Range of motion varied greatly, but patient satisfaction was high.
In 2006, Tuttle et al. published a retrospective review of 18 pyrolytic carbon PIP joint arthroplasty procedures on 8 patients with an average follow-up period of 13 months. (30) The authors achieved an increased AAM in 9 joints but a decreased AAM in 9 joints, although changes were insignificant. Complete pain relief was obtained in 8 of the joints, but complications included joint contracture, joint dislocation, residual deformity, and squeaking of the implants. Herren et al. in 2006, conducted a prospective study of 17 pyrolytic carbon implants followed for an average of 20.5 months. (31) Implant migration was discovered in 8 of the joints, which corresponded to a statistically insignificant decrease in AAM and grip strength.
In 2006, Nunley et al. reported the first prospective study, on 5 young patients (mean age: 40 yrs) who suffered from posttraumatic arthritis. (29) After seeing no improvement in DASH score and pain ratings, the authors concluded the pyrolytic carbon implant was ineffective and stopped using it altogether. (29) In 2007, Meier et al. reported retrospectively on 24 pyrolytic carbon PIP prostheses, with an average follow-up period of 15 months. (42) Complications included one case of infection, two dislocations, five cases of distal component migration, and four cases of proximal component migration. Nonetheless, 80% of patients were satisfied with the outcome of the operation. (42) Bravo et al. in 2007, retrospectively studied a total of 50 PIP joints treated with pyrocarbon implants with a minimum follow-up period of 2 years. (11) They documented significant improvements in pinch strength and pain ratings, but insignificant improvements in AAM and grip strength. They reported overall increased patient satisfaction, and nearly 80% of patients stated that they would undergo the procedure again. (11) Branam et al. in 2007 compared the silicone implant to the pyrocarbon implant in a retrospective review of 41 arthroplasty procedures in 22 patients. (43) This study was the first to directly compare outcomes between the pyrocarbon and silicone implants. Achieved AAM was 62° in the silicone group and 66° in the pyrolytic carbon group. Eleven of 20 joints in the silicone group and 4 of 19 joints in the pyrolytic carbon group had a coronal plane deformity, de ned by angulation of the PIP joint greater than or equal to 10°. The pyrocarbon group had fewer complications than the silicone group, which was statistically significant. (43)
Our analysis of 21 procedures over a 44 month period is mostly consistent with previous reports. There was a statistically significant improvement in key pinch but an insignificant improvement in grip strength. We report an average AAM of 38°, which is essentially unchanged from our preoperative values. The Jebsen-Taylor test score improved over the observation period. MHQ data reveal a large effect size (effect size >0.8) for all domains. Patients reported the largest postoperative improvement in Pain and Satisfaction, followed by Aesthetics. The data suggest that the improved pain relief despite minimal functional gain is enough to increase overall patient satisfaction scores. We will continue to follow these patients and monitor their x-rays to detect changes and screen for abnormalities.
The pyrocarbon implant does not seem to confer any significant functional advantages when compared to the silicone prosthesis. Stutz et al. appear to be the only group that has achieved a significant improvement in post-operative AAM, which may be credited to their intensive post-operative therapy aimed at stretching the tendon early to obtain optimal movement. (40) Whether these encouraging results will be consistently reproduced in future studies remains to be seen. However, our MHQ data show that overall patient-rated satisfaction can still be realized despite meager functional gains. To this end, the pyrocarbon implant seems to be an effective way to reduce pain without sacrificing AAM.
This study has several limitations. The most obvious limitation is the small sample size. We feel that this does not affect the conclusions, however. Although a small number of patients were available to be recruited into this study, every patient who was eligible was recruited. We employed a prospective study design, which few currently published studies have employed, that applied two validated measures of hand function, the Michigan Hand Outcomes Questionnaire and the Jebsen-Taylor test. In addition, this is the only published to include multiple follow-up time-points. Considering the paucity of data regarding outcomes after pyrocarbon PIP joint arthroplasty, the data can be useful to surgeons and patients when contemplating this increasingly popular procedure.
PIP joint arthroplasty using the pyrocarbon implant is a demanding procedure involving complex technical sequences. While the data suggest that pyrolytic carbon delivers excellent in vivo durability and biomechanics, there is no convincing data thus far to support the use of this prosthesis over the traditional silicone implant for the OA PIP joint. The pyrolytic carbon implant suffers from short-term complications similar to that of the silicone implant; dislocation is not uncommon and functional improvements based on physical tests are marginal at best. Our data with the pyrocarbon implant show encouraging results, namely in patient satisfaction and pain relief, but are not compelling. The advantages of the pyrolytic carbon design must be weighed against the cost (est. $2800 per implant) (Ascension Orthopedics, Austin, TX, personal communication), the technical challenge, and the limited long-term experience with this device. Prospective outcomes studies with long-term follow-up periods may shed light on whether this new technology is warranted. The evolution of PIP joint arthroplasty will depend heavily on the research and development of improved implant materials and designs, in consideration with practical surgical techniques that will sustain long-term benefits to the patient.
Acknowledgments
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Dr. Kevin C. Chung).
The authors wish to thank Jeanne Riggs, CHT, who performed the hand therapy and measurements for patients in this study.
Footnotes
Financial disclosure statement: The authors have no other financial interest in any of the products, devices, or drugs mentioned in this manuscript.
References
- 1.Centers for Disease Control Prevention. Projected prevalence of self-reported arthritis or chronic joint symptoms among persons aged >65 years - United States 2005–2030. MMWR. 2003;52:489–491. [PubMed] [Google Scholar]
- 2.Wilder FV, Barrett JP, Farina EJ. Joint-specific prevalence of osteoarthritis of the hand. Osteoarthritis Cartilage. 2006;14:953–957. doi: 10.1016/j.joca.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 3.Chung KC. Implant arthroplasty using pyrocarbon implant. In: Chung KC, editor. Operative Techniques: Hand and Wrist Surgery. 1. Philadelphia, PA: Saunders/Elsevier; 2007. pp. 607–630. [Google Scholar]
- 4.Squitiere L, Chung KC. A systematic review of outcomes and complications of vascularized toe joint transfer, silicone arthroplasty and pyrocarbon arthroplasty for post-traumatic joint reconstruction of the finger. Plast Reconstr Surg. doi: 10.1097/PRS.0b013e31816aa0b3. in press. [DOI] [PubMed] [Google Scholar]
- 5.Foliart DE. Swanson silicone finger joint implants: a review of the literature regarding long-term complications. J Hand Surg. 1995;20A:445–449. doi: 10.1016/S0363-5023(05)80104-2. [DOI] [PubMed] [Google Scholar]
- 6.Pellegrini VD, Jr, Burton RI. Osteoarthritis of the proximal interphalangeal joint of the hand: arthroplasty or fusion? J Hand Surg. 1990;15A:194–209. doi: 10.1016/0363-5023(90)90096-a. [DOI] [PubMed] [Google Scholar]
- 7.Hage JJ, Yoe EP, Zevering JP, et al. Proximal interphalangeal joint silicone arthroplasty for posttraumatic arthritis. J Hand Surg. 1999;24A:73–77. doi: 10.1053/jhsu.1999.jhsu24a0073. [DOI] [PubMed] [Google Scholar]
- 8.Ashworth CR, Hansraj KK, Todd AO, et al. Swanson proximal interphalangeal joint arthroplasty in patients with rheumatoid arthritis. Clin Orthop Relat Res. 1997:34–37. [PubMed] [Google Scholar]
- 9.Takigawa S, Meletiou S, Sauerbier M, et al. Long-term assessment of Swanson implant arthroplasty in the proximal interphalangeal joint of the hand. J Hand Surg. 2004;29A:785–795. doi: 10.1016/j.jhsa.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Beckenbaugh RD, Dobyns JH, Linscheid RL, et al. Review and analysis of silicone-rubber metacarpophalangeal implants. J Bone Joint Surg. 1976;58A:483–487. [PubMed] [Google Scholar]
- 11.Bravo CJ, Rizzo M, Hormel KB, et al. Pyrolytic carbon proximal interphalangeal joint arthroplasty: results with minimum two-year follow-up evaluation. J Hand Surg. 2007;32A:1–11. doi: 10.1016/j.jhsa.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 12.Stanley JK, Evans RA. What are the long term follow-up results of silastic metacarpophalangeal and proximal interphalangeal joint replacements? Br J Rheumatol. 1992;31:839. doi: 10.1093/rheumatology/31.12.839. [DOI] [PubMed] [Google Scholar]
- 13.Parker WL, Rizzo M, Moran SL, et al. Preliminary results of nonconstrained pyrolytic carbon arthroplasty for metacarpophalangeal joint arthritis. J Hand Surg [Am] 2007;32:1496–1505. doi: 10.1016/j.jhsa.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Hilker A, Miehlke RK, Schmidt K. Prosthetics of metacarpophalangeal joints. Z Rheumatol. 2007;66:366–375. doi: 10.1007/s00393-007-0193-1. [DOI] [PubMed] [Google Scholar]
- 15.Nunez VA, Citron ND. Short-term results of the Ascension pyrolytic carbon metacarpophalangeal joint replacement arthroplasty for osteoarthritis. Chir Main. 2005;24:161–164. doi: 10.1016/j.main.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 16.Fayaz HC, Beckenbaugh RD, An KN, et al. The Arthur Vick Award: kinematics of the metacarpophalangeal joint after surface replacement arthroplasty. Z Orthop Unfall. 2007;145:199–206. doi: 10.1055/s-2007-965173. [DOI] [PubMed] [Google Scholar]
- 17.Cook SD, Beckenbaugh RD, Redondo J, et al. Long-term follow-up of pyrolytic carbon metacarpophalangeal implants. J Bone Joint Surg. 1999;81A:635–648. doi: 10.2106/00004623-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Beckenbaugh RD. Arthroplasty of the metacarpophalangeal joint using pyrocarbonate implants. Orthopade. 2003;32:794–797. doi: 10.1007/s00132-003-0519-x. [DOI] [PubMed] [Google Scholar]
- 19.Jebsen RH, Taylor N, Trieschmann RB, et al. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50:311–319. [PubMed] [Google Scholar]
- 20.Sharma S, Schumacher HRJ, McLellan AT. Evaluation of the Jebsen hand function test for use in patients with rheumatoid arthritis. Arthritis Care Res. 1994;7:16–19. doi: 10.1002/art.1790070105. [DOI] [PubMed] [Google Scholar]
- 21.Chung KC. Michigan Hand Outcomes Questionnaire. 2008 http://sitemaker.umich.edu/mhq/overview.
- 22.Chung KC, Kotsis SV, Kim HM. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg. 2004;29A:646–653. doi: 10.1016/j.jhsa.2004.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kotsis SV, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder and Hand questionnaire in carpal tunnel surgery. J Hand Surg. 2005;30A:81–86. doi: 10.1016/j.jhsa.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Kotsis SV, Lau FH, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg. 2007;32A:84–90. doi: 10.1016/j.jhsa.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Chung KC, Hamill JB, Walters MR, et al. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42:619–622. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Chung KC, Pillsbury MS, Walters MR, et al. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg. 1998;23A:575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 27.Petersen P, Petrick M, Connor H, et al. Grip strength and hand dominance: challenging the 10% rule. Am J Occup Ther. 1989;43:444–447. doi: 10.5014/ajot.43.7.444. [DOI] [PubMed] [Google Scholar]
- 28.Cohen J, editor. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 29.Nunley RM, Boyer MI, Goldfarb CA. Pyrolytic carbon arthroplasty for posttraumatic arthritis of the proximal interphalangeal joint. J Hand Surg. 2006;31A:1468–1474. doi: 10.1016/j.jhsa.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 30.Tuttle HG, Stern PJ. Pyrolytic carbon proximal interphalangeal joint resurfacing arthroplasty. J Hand Surg. 2006;31A:930–939. doi: 10.1016/j.jhsa.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 31.Herren DB, Schindele S, Goldhahn J, et al. Problematic bone fixation with pyrocarbon implants in proximal interphalangeal joint replacement: short-term results. J Hand Surg [Br] 2006;31:643–651. doi: 10.1016/j.jhsb.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 32.Rizzo M, Beckenbaugh RD. Proximal interphalangeal joint arthroplasty. J Am Acad Orthop Surg. 2007;15:189–197. doi: 10.5435/00124635-200703000-00009. [DOI] [PubMed] [Google Scholar]
- 33.The Medical Advisory Secretariat. Health technology scientific literature and policy review. Ministry of Health and Long-Term Care; 2004. Pyrocarbon finger joint implant. [Google Scholar]
- 34.Sears EA, Chung KC. Arthroplasty procedures in the hand. In: Chung KC, editor. Atlas of Reconstructive Surgery. 1. Philadelphia, PA: Elsevier, pending publication; [Google Scholar]
- 35.Leuer LH, Gross JM, Johnson KM. Material properties, biocompatibility, and wear resistance of the Medtronic pyrolytic carbon. J Heart Valve Dis. 1996;5 (Suppl 1):S105–109. [PubMed] [Google Scholar]
- 36.Haubold AD. On the durability of pyrolytic carbon in vivo. Med Prog Technol. 1994;20:201–208. [PubMed] [Google Scholar]
- 37.Uchiyama S, Cooney WP, 3rd, Linscheid RL, et al. Kinematics of the proximal interphalangeal joint of the finger after surface replacement. J Hand Surg. 2000;25A:305–312. doi: 10.1067/jhsu.2000.jhsu25a0305. [DOI] [PubMed] [Google Scholar]
- 38.Linscheid RL, Murray PM, Vidal MA, et al. Development of a surface replacement arthroplasty for proximal interphalangeal joints. J Hand Surg. 1997;22A:286–298. doi: 10.1016/S0363-5023(97)80165-7. [DOI] [PubMed] [Google Scholar]
- 39.Kobayashi K, Terrono AL. Proximal interphalangeal joint arthroplasty of the hand. J Am Soc Surg Hand. 2006;3:219–226. [Google Scholar]
- 40.Stutz N, Meier R, Krimmer H. Pyrocarbon prosthesis for finger interphalangeal joint replacement. Experience after one year. Unfallchirurg. 2005;108:365–369. doi: 10.1007/s00113-004-0891-y. [DOI] [PubMed] [Google Scholar]
- 41.Schulz M, Muller-Zimmermann A, Behrend M, et al. Early results of proximal interphalangeal joint replacement with pyrolytic carbon prosthesis (Ascension) in idiopathic and post-traumatic arthritis. Handchir Mikrochir Plast Chir. 2005;37:26–34. doi: 10.1055/s-2005-837533. [DOI] [PubMed] [Google Scholar]
- 42.Meier R, Schulz M, Krimmer H, et al. Proximal interphalangeal joint replacement with pyrolytic carbon prostheses. Oper Orthop Traumatol. 2007;19:1–15. doi: 10.1007/s00064-007-1192-8. [DOI] [PubMed] [Google Scholar]
- 43.Branam BR, Tuttle HG, Stern PJ, et al. Resurfacing arthroplasty versus silicone arthroplasty for proximal interphalangeal joint osteoarthritis. J Hand Surg [Am] 2007;32:775–788. doi: 10.1016/j.jhsa.2007.04.006. [DOI] [PubMed] [Google Scholar]



