Abstract
Objectives
After reading this article (part I of II), the participant should be able to: 1. Describe the history of tendon transfer procedures. 2. List and understand the principles and biomechanics of tendon transfers. 2. Describe the anatomy and function of the radial nerve in the forearm and hand. 3. Describe the indications, benefits, and drawbacks for various tendon transfer procedures performed for radial nerve palsy.
Summary
This article reviews the history of tendon transfer procedures, and describes the principles and biomechanics behind them. It also discusses the anatomy and clinical findings of radial nerve palsy, and the tendon transfer procedures used to treat it.
Keywords: Tendon, transfer, paraplegia, brachial plexus, paraplegia, radial nerve palsy
Definition
A tendon transfer procedure relocates the insertion of a functioning muscle-tendon unit (MTU) in order to restore lost movement and function at another site.
History
The polio epidemics that occurred in 19th century Europe contributed to the development of tendon transfer procedures. Poliomyelitis, a viral illness that attacks anterior horn motor neurons, results in varying degrees of paralysis. Many of the first tendon transfer procedures were devised in order to improve ambulation in polio patients.
Further advances followed World Wars I and II. Prior to these wars, most tendon transfer procedures were confined to the lower extremity. World Wars I and II resulted in large groups of patients with upper extremity injuries that could benefit from tendon transfer procedures.1 This led to the expansion and refinement of their use in the upper extremity.
Indications
The most common indication for upper extremity tendon transfer procedures is a peripheral nerve injury that has no potential to improve.2 This includes nerve injuries that are physically irreparable such as root avulsions, nerve injuries that do not recover after direct nerve repair or grafting, or failed nerve transfers. In addition, tendon transfer procedures are often indicated when peripheral nerve injuries present so late that muscle reinnervation is impossible due to motor end-plate fibrosis.
Other common indications include loss of muscle or tendon following trauma, central neurologic deficits such as spinal cord injuries and cerebral palsy,3 and tendon ruptures in patients with rheumatoid arthritis. Other rarer disorders, including poliomyelitis and leprosy, can result in disability that may benefit from a tendon transfer procedure.
It should be noted that other treatment options can sometimes be used in place of, or in combination with tendon transfer procedures to improve upper extremity function. These include non-operative modalities such as static and dynamic splinting, or operations such as tendon grafting, tenodesis, arthrodesis, nerve transfer, and free functional muscle transfer. The role of these other treatment options should be carefully evaluated in all potential tendon transfer candidates.
Principles of Tendon Transfer Procedures
The principles of successful tendon transfer procedures have been identified and refined over the last century. They are 1) supple joints prior to transfer, 2) soft tissue equilibrium, 3) donor of adequate excursion, 4) donor of adequate strength, 5) expendable donor, 6) straight line of pull, 7) synergy, and 8) single function per transfer.
Supple joints prior to transfer
The joint that the tendon transfer will move must have maximum passive range of motion prior to the procedure. A tendon transfer procedure will fail if the joint has become stiff. Often, aggressive therapy is required to achieve and maintain a supple joint before performing a tendon transfer procedure. If contracture release is necessary, it should be performed prior to the tendon transfer procedure, and should be followed by intensive therapy to maintain range of motion. Because immobilization is required after a tendon transfer procedure to allow healing of the tendon juncture, contracture release should not be performed at the same time.
Soft tissue equilibrium
The principle of soft tissue equilibrium refers to the idea that a tendon transfer should pass through a healthy bed of tissue that is free from inflammation, edema, and scar.4 This is necessary to allow the tendon to glide freely and to minimize adhesions. Following a soft tissue injury, the surgeon must allow enough time to pass for the inflammation and edema to fully subside. If the planned tendon transfer must pass through an area of severely scarred tissue, the scar should be excised and replaced with a flap, or an alternative transfer through a healthier bed should be considered.
Donor of adequate excursion
The excursion or maximum linear movement of the transferred MTU should be adequate to achieve the desired hand movement. This means that the transferred MTU should have an excursion similar to that of the tendon which it is replacing. In adults, wrist flexors and extensors have approximately 33 mm of excursion. The extrinsic finger extensors have about 50 mm of excursion, and the extrinsic finger flexors have about 70 mm of excursion.5 Most of the time, a donor MTU with adequate excursion will be available for transfer. However, in some situations none of the available donor MTU’s have the required excursion. In these cases, the tenodesis effect can often be used to augment the excursion of the transferred tendon. For example, when a wrist flexor is transferred to restore finger extension, the excursion of the wrist flexor (33 mm) is insufficient to achieve complete finger extension (50 mm). However, if the patient flexes the wrist during finger extension, the tenodesis effect tightens the finger extensors, resulting in greater finger extension.
Donor of adequate strength
The principle of choosing a donor MTU with adequate strength means that the MTU to be transferred must be strong enough to achieve the desired movement, but at the same time, should not be too strong. A donor MTU that is too weak will have inadequate movement and function, while a donor that is too strong will result in imbalanced movement and inappropriate posture at rest. When evaluating potential donor MTU’s, it is easiest to compare their relative strength as opposed to absolute strength.2 The flexor carpi radialis (FCR), wrist extensors, finger flexors, and pronator teres (PT) all have a relative strength of 1. The brachioradialis (BR) and flexor carpi ulnaris (FCU) are stronger, and have a relative strength of 2. Finger extensors are weaker and have a relative strength of 0.5. The abductor pollicis longus (APL), extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and palmaris longus (PL) are all weaker still, with relative strengths of 0.1.
Expendable donor
The principle of using an expendable MTU as a donor means that there must be another remaining muscle that can continue to adequately perform the transferred MTU’s original function. It does no good to restore a given movement if another equally important movement is lost in the process. Fortunately there is a fair amount of redundancy in the upper extremity. For example, the wrist has three extensors, the extensor carpi ulnaris (ECU), the extensor carpi radialis longus (ECRL), and the extensor carpi radialis brevis (ECRB). If all three are functional, one or two of the extensors can be transferred. Although wrist extension will be weakened, it will not be lost as long as there is one remaining extensor. When evaluating potential donor MTU’s for transfer, one must be mindful of the weakness, loss of movement, or imbalance that might occur following the transfer.
Straight line of pull
Tendon transfer procedures are most effective if there is a straight line of pull. This is because direction changes diminish the force that the transferred MTU is able to exert on its insertion. A change in direction of just 40 degrees will result in a clinically significant loss of force. For example, a PT to ECRB transfer is commonly used to restore wrist extension in patients with radial nerve palsy. This transfer can be performed in an end-to-side or end-to-end fashion. Assuming that all other factors are equal, the end-to-end transfer will result in better function and force transfer than the end-to-side transfer, because the line of pull is straighter. However, with some tendon transfer procedures, a direction change is unavoidable or even necessary. In these cases, the tendon should be passed around a fixed, smooth structure that can act as a pulley.
Synergy
The principle of synergy refers to the fact that certain muscle groups usually work together to perform a function or movement. Wrist flexion and finger extension are synergistic movements that often occur simultaneously during normal activity. When one flexes the wrist, the fingers automatically extend. Wrist extension and finger flexion are similarly synergistic. Finger flexion and extension, however, do not normally occur together and are not synergistic movements. Transferring a wrist flexor to restore finger extension adheres to the principle of synergy, whereas using a finger flexor to provide finger extension does not. A synergistic transfer is preferable, although sometimes a non-synergistic transfer is the only available option.6
Single function per transfer
The final principle is that a single tendon should be used to restore a single function. Transfer of one MTU to restore multiple functions will result in compromised strength and movement.7 The exception to this rule is that a single MTU can be used to restore the same movement in more than one digit. For example, the FCU cannot be used to power wrist and finger extension, or to power finger extension and thumb abduction. However, it can be used to power the extension of all four fingers.
It is important to remember these principles when evaluating a patient for a tendon transfer procedure. Although adherence to these principles does not guarantee success, ignoring them invites failure.
Biomechanics
There are many biomechanical factors that affect the ability of a transferred tendon to move a joint. However, there are four main concepts that are especially important: MTU excursion, MTU force-generating ability, the moment arm, and the tension at which the transfer is set. The importance of adequate MTU excursion and the use of the tenodesis effect to augment excursion have been discussed above.
Force-generating ability
The amount of force that an MTU can generate is directly proportionate to the physiologic cross-sectional area (PCSA) of the muscle belly.8 For example, the force-generating ability of the brachioradialis is approximately twice that of the FCR. Most of this difference is due to the greater PCSA of the brachioradialis. There are other architectural characteristics that affect a muscle’s force-generating ability, although to a lesser degree. For example, the orientation of muscle fibers relative to the long axis of the MTU, called the pennation angle, affects how much force can be generated. Muscle fibers that are oriented obliquely relative to the long axis of the MTU are less effective in generating force than muscle fibers that are oriented nearly parallel to the long axis. For example, the relatively weak interossei muscles of the hand have a high pennation angle.
The moment arm
The moment arm of a tendon transfer is an important determinant of how much movement will occur and how strong the movement will be.9 The moment arm is in turn determined by how far away the tendon line of action is from the joint axis of rotation. The closer the tendon line of action is to the joint axis of rotation, the smaller is the moment arm. The further the tendon line of action is from the joint axis of rotation, the greater the moment arm. A tendon inserted close to the joint will have a small moment arm as the joint moves, resulting in an increased arc of motion at the expense of strength. A tendon insertion placed farther from the joint will have a greater moment arm as the joint moves, resulting in stronger movement, but with a more limited arc of motion. It should be remembered that the moment arm is not a static value, but changes as the joint is moved, and the relationship between the joint and the tendon is altered. Choosing the appropriate moment arm requires balancing the requirements for range of motion and strength of movement.
Tension of the transfer
Finally, the amount of passive tension at which the tendon transfer procedure is set is one of the most critical aspects of the operation. In order to achieve maximum force generation, the muscle must be set at an optimum degree of tension. The ideal tension really depends upon the amount of actin-myosin overlap that occurs at different muscle lengths. Unfortunately, the surgeon cannot feel when maximum actin-myosin overlap occurs, because it does not correlate with maximum passive tension. In practical terms, the MTU should be set at a tension as close as possible to its preoperative resting tension. This determination was made Freehafer et al., who used intraoperative electrical stimulation to determine the ideal tension at which to set the transfer.10 However, it is certainly preferable to set a tendon transfer too tightly rather than too loosely. The tendon transfer juncture tends to relax and lengthen postoperatively, and a transfer that is set with inadequate tension will not improve with time.
Radial Nerve Palsy
Anatomy
Proximal to the elbow, the radial nerve lies adjacent to posterior surface of the humerus where it innervates the triceps muscle. As it courses distally, it pierces the lateral intermuscular septum and descends between the brachialis and the brachioradialis muscles. It often provides motor innervation to the brachialis, which also receives innervation from the musculocutaneous nerve. Still proximal to the elbow, it innervates the brachioradialis and the ECRL. At the lateral epicondyle, it bifurcates into a deep motor branch, the posterior interosseous nerve (PIN), and a superficial sensory branch. It is at this level that it innervates the ECRB. The branch to the ECRB may come from the main nerve prior to bifurcation into the PIN and the superficial sensory branch. The superficial sensory branch travels between the brachioradialis (BR) and the ECRL muscle bellies, rising into the subcutaneous tissue between the BR and ECRL tendons about 9 cm proximal to the radial styloid. It provides sensibility to the dorsoradial aspect of the hand and the dorsal aspect of the thumb, index, and middle fingers. The PIN divides into multiple branches, running deep and innervating the supinator. Its branches innervate the extensor digitorum communis (EDC), the extensor digiti quinti (EDQ), and the ECU. It then sends branches to the APL, EPB, EPL, and extensor indicis proprius (EIP). The EIP is the last muscle to be innervated. The PIN terminates in the wrist capsule volar to the 4th extensor compartment.
Clinical Findings
Radial nerve palsy results in debilitating motor dysfunction of the hand. The patient loses the ability to extend the wrist, fingers and thumb, movements that are essential for functional grasp. In addition, the patient loses grip strength because he cannot stabilize the wrist during power grip. Fortunately, the loss of cutaneous sensibility in the radial nerve distribution is well tolerated.
A high radial nerve palsy is defined as an injury proximal to the elbow. Wrist, finger (MCPJ), and thumb extension, as well as thumb abduction are lost. Low radial nerve palsy, defined as an injury to the PIN, occurs distal to the elbow. Wrist extension is preserved because the more proximally innervated ECRL remains intact. If the PIN is injured proximally, ECU function may be lost, resulting in radial deviation with wrist extension. If the injury to the PIN is more distal, ECU function is preserved and wrist extension remains balanced.
Tendon transfer procedures
There are three main goals when treating radial nerve palsy. They include restoration of finger (MCPJ) extension, restoration of thumb extension, and in cases of high radial nerve palsy, restoration of wrist extension.
The most accepted method for restoring wrist extension after high radial nerve injury is the PT to ECRB transfer. If recovery of the radial nerve is not expected, the transfer should be performed in an end-to-end fashion, meaning that the ECRB tendon is transected and the cut end of the PT tendon sutured to it (Figure 1). This creates a direct line of pull, and a more efficient transfer. However, if the radial nerve has been repaired and ECRB reinnervation is expected in the future, the transfer should be performed in an end-to-side fashion, with the cut PT tendon sutured to the side of the intact ECRB tendon (Figure 2). If performed early, this transfer acts as an internal splint that stabilizes the wrist while the nerve is recovering. Because the ECRB is left intact, it can resume wrist extension once it regains function.
Figure 1.
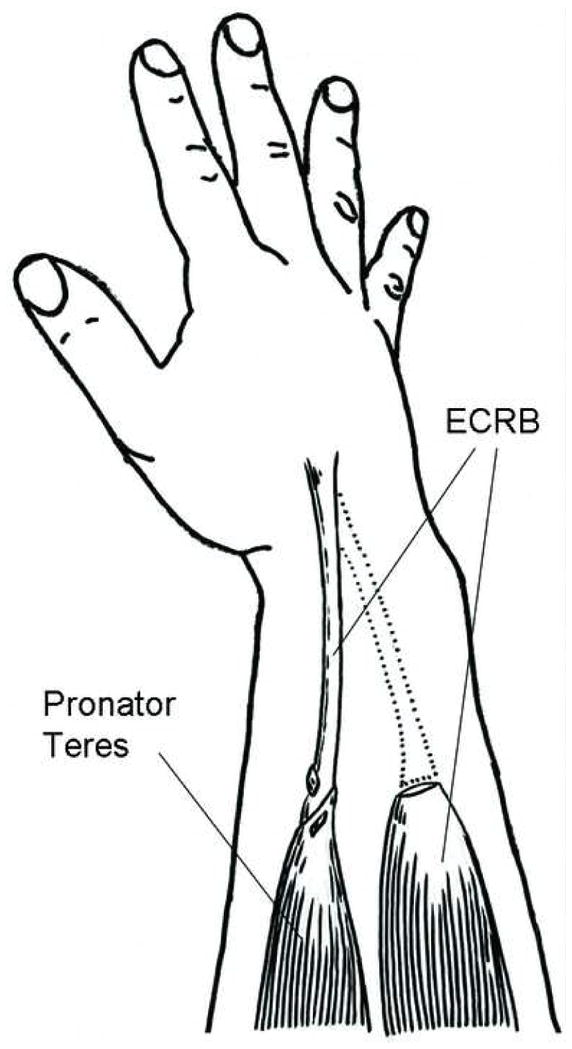
PT to ECRB transfer, end-to-end, to restore wrist extension.
Figure 2.
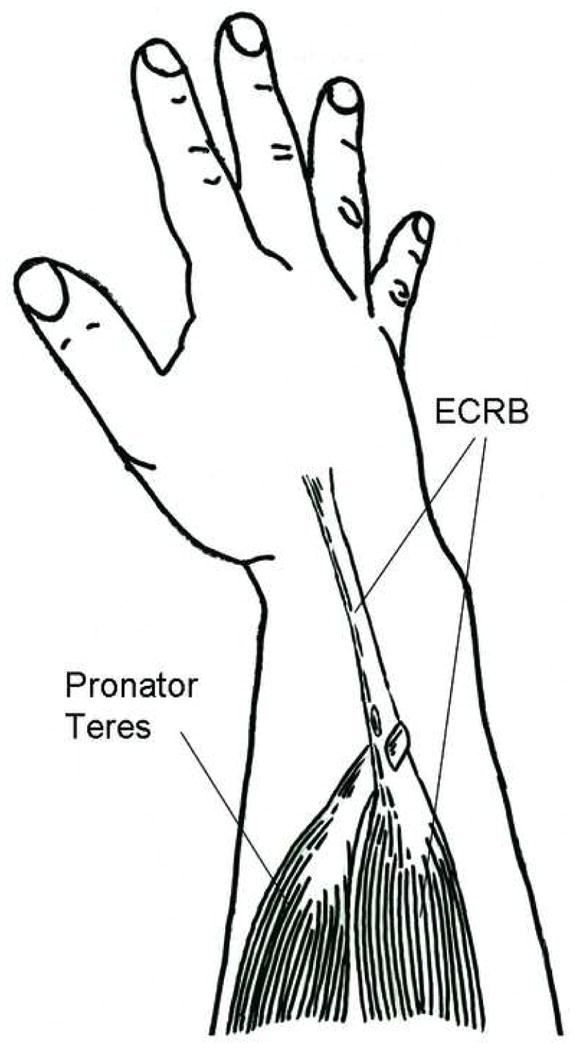
PT to ECRB transfer, end-to-side, to restore wrist extension.
Many different tendons can be transferred to the EPL to restore thumb extension. The palmaris longus (PL) or the ring finger flexor digitorum superficialis (FDS) are used most often. When the ring FDS is used, it can be split and inserted into both the EPL and the EIP, allowing concomitant thumb and index finger extension. Although this transfer seems to violate the principle of using a single tendon to perform a single movement, in reality it does not. Concomitant thumb and index finger extension is a composite movement that is useful in precision manipulation, and can be considered a single function. When the PL is used as a motor, the EPL is usually rerouted volarly to meet the PL in a direct line of pull (Figure 3). This results in abduction of the thumb as well as IPJ extension.
Figure 3.
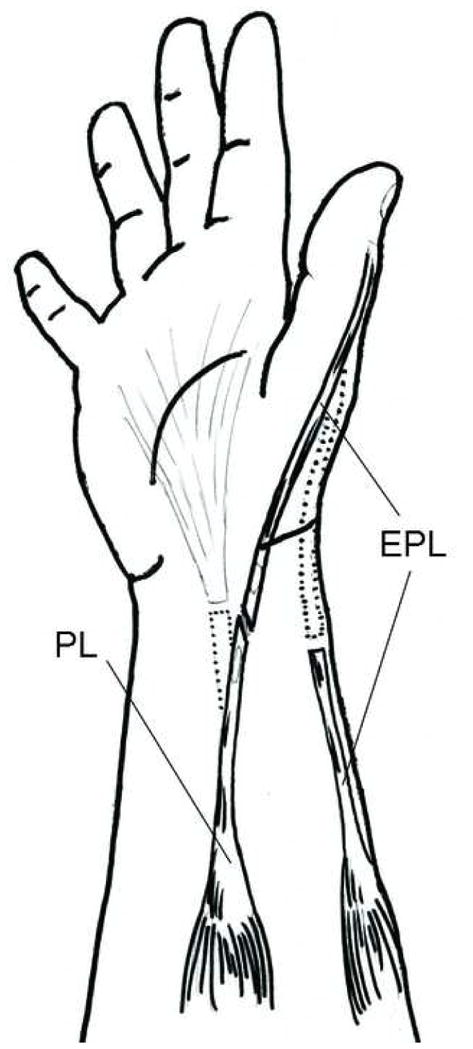
PL to EPL transfer to restore thumb extension.
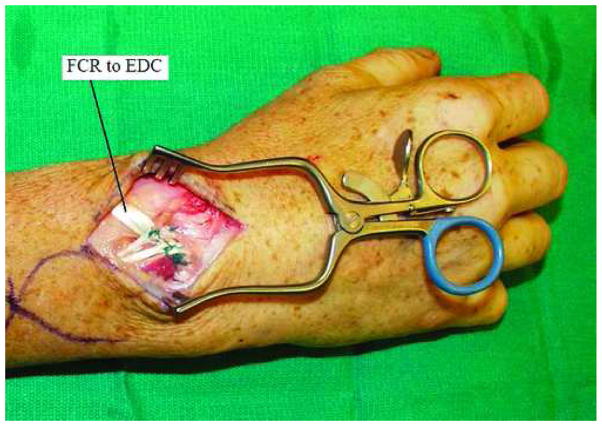
Finger MCPJ extension can be re-established by transferring the FCR (Figure 4), FCU (Figure 5), or FDS tendon to the EDC. In the early 1900’s, Jones popularized the used of the FCU to restore MCPJ extension.11, 12 However, there are a number of drawbacks to using the FCU. For one, it sacrifices the only remaining ulnar-sided wrist motor. This results in radial deviation of the wrist, particularly in cases of low radial nerve palsy in which the ECRL remains intact. In addition, ulnar deviation with wrist flexion is lost when the FCU is sacrificed. This is an important wrist motion, and is essential for activities such as hammering and throwing. For these reasons, the FCR (Brand)13 and FDS (Boyes)14 transfers are also often used. Neither the FCR nor the FDS transfer results in radial deviation of the wrist or loss of ulnar deviation with wrist flexion. In addition, the FDS transfer has the advantage of having better excursion than the other two transfers. The main disadvantage of the FDS transfer is that powering MCPJ extension with a finger flexor is not synergistic, and motor re-education after the transfer is difficult.
Figure 4.
FCR to EDC transfer to restore finger MCP extension.
Figure 5.
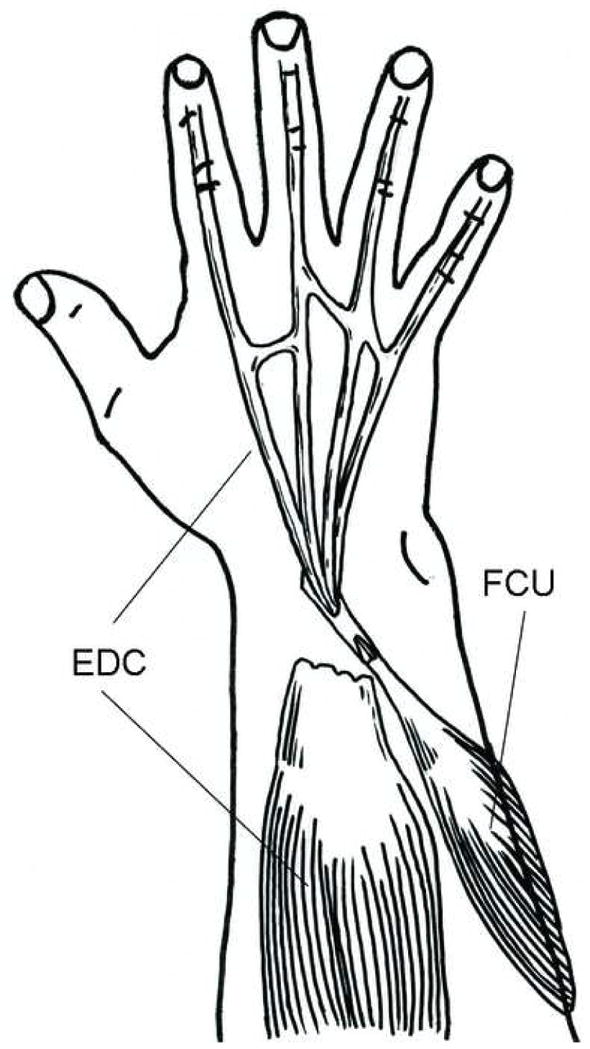
FCU to EDC transfer to restore finger MCP extension.
Three main patterns of tendon transfer procedures for radial nerve palsy have emerged over the last century: the FCR transfer (Brand), the FCU transfer, and the superficialis transfer (Boyes). All three transfers use the PT to ECRB transfer to restore wrist extension, but vary in the transfers used to restore finger and thumb extension. The FCR transfer involves an FCR to EDC transfer to restore finger extension and a PL to EPL transfer to restore thumb extension. The FCU transfer is identical except that the FCU is used to power the EDC instead of the FCR. The superficialis transfer is quite different from the other two. The ring finger FDS is transferred to the EPL and EIP to provide thumb and index finger extension. The middle finger FDS is used to power the EDC to all four fingers, restoring finger extension (Figures 6 and 7). In addition, the FCR can be transferred to the APL and EPB to restore independent planar abduction of the thumb.15 Each of these transfers has been shown to have good and reliable results in various published series. There is no comparison showing one to be definitively better than another.
Figure 6.
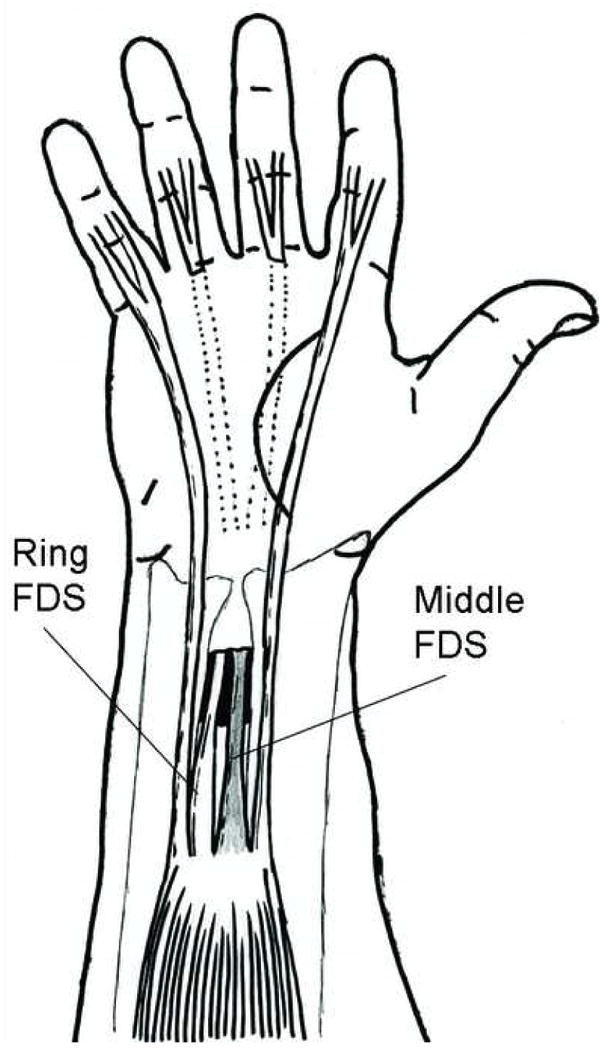
Middle and ring finger FDS passed through interosseous membrane.
Figure 7.
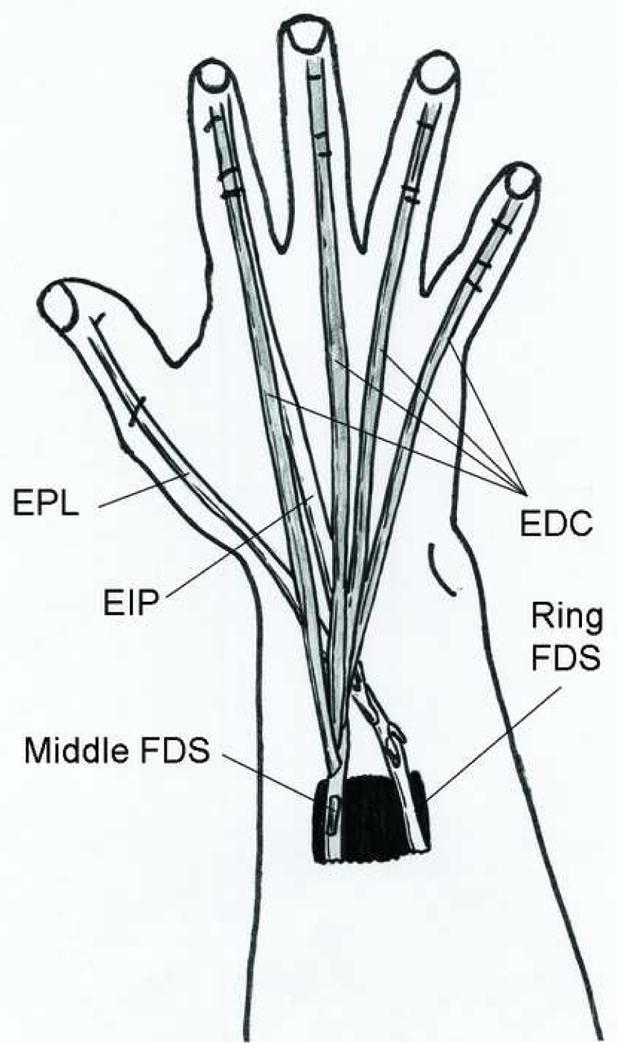
Middle finger FDS to EDC, ring finger FDS to EPL and EIP.
A fourth and final tendon transfer procedure deserves mention: the Merle d’Aubigne procedure. Like the above procedures, it involves a PT to ECRB (and ECRL) transfer. The FCU is used to power the EPL and EDC together. In addition, the PL is transferred to the EPB and APL to provide thumb abduction. This alternative procedure for treating radial nerve palsy has also been shown to be a reliable procedure with good outcomes.16
Technical Considerations
The PT to ECRB transfer should be performed by dividing the PT at its distal insertion, routing it subcutaneously and superficial to the brachioradialis, around the radial border of the forearm. It should be inserted end-to-end or end-to-side on the ECRB. Although the Boyes’ superficialis transfer describes an insertion on the ECRB and ECRL, this can cause too much radial deviation, and should be avoided.
When the FCU or FCR is used to power the EDC, the donor MTU should be divided as distally as possible at the wrist. The FCR is generally routed in the subcutaneous plane around the radial border of the forearm, while the FCU is routed around the ulnar border of the forearm. The four EDC tendons should be divided just distal to their musculotendinous junction, and woven into the FCU or FCR. This should be done proximal to the extensor retinaculum, to keep gliding as smooth as possible, and to prevent the bow-stringing occurs if the extensor retinaculum is divided.
If the PL is used to power the EPL, it should be divided as distally as possible at the wrist and retracted into the forearm. The EPL should be divided proximally, near its musculotendinous junction. The EPL should then be taken out of the third extensor compartment and transposed radial to Lister’s tubercle. This allows a straighter line of pull from the PL to the EPL. It also allows the transfer to provide some radial abduction of the thumb in addition to extension.
If the FDS transfer is performed, the FDS tendons should be divided between the A1 and A2 pulleys, just before spliting at Camper’s chiasm. The superficialis tendons of the ring and middle fingers can be passed either around the ulnar and radial borders of the wrist respectively, or through an opening in the interosseous membrane, made proximal to the pronator quadratus. If this route is used to reach the dorsal aspect of the wrist, the opening should be made as large as possible, so that the superficialis tendons pass easily.
Postoperative Care and Rehabilitation
Regardless of which procedure is performed, the patient should be placed in an above elbow splint or cast postoperatively. The elbow should be flexed at ninety degrees, the forearm pronated, and the wrist extended at thirty degrees. This takes tension off the PT to ECRB transfer. The thumb should be abducted and extended, and the MCPJ’s of the fingers extended, to take tension off the transfers to the EDC and the EIP. The IPJ’s of the fingers should be left free. The postoperative splint can be change at 1–2 weeks for a wound check and to refit the splint. At four weeks post-operatively, a thermoplastic splint should be fabricated. During the first four weeks after surgery, it is important to maintain range of motion of the shoulder and the IPJ’s of the fingers.
At four weeks mobilization begins. During weeks four to six, exercises will focus on mobilization of single joints, while keeping tension off the transfer. For example, elbow flexion and extension will be performed while keeping the wrist and fingers extended and the forearm pronated. Wrist flexion and extension will be performed while keeping the fingers extended, and the elbow flexed. Finger MCP flexion and extension will be performed with the elbow flexed and the finger IP joints extended. Mobilization will begin with active ROM and advance to gentle passive ROM. The splint should be worn when not performing prescribed exercises. During the sixth week, the therapist will begin to focus on activating the muscles used in the tendon transfer, and will begin muscle retraining. It is still important during this period to prevent simultaneous flexion of the wrist and fingers, so as not to place excessive tension on the transfers. Electrical stimulation and biofeedback may be performed to assist with retraining. At eight weeks postoperatively, strengthening exercises are begun, and the splint can be weaned off. Full activity is resumed at twelve weeks.17
References
- 1.Green DP. Radial Nerve Palsy. In: Green DP, Hotchkiss RN, Pederson WC, editors. Green’s Operative Hand Surgery. 4. Vol. 2. New York: Churchill Livingstone; 1999. pp. 1481–1496. [Google Scholar]
- 2.Richards RR. Tendon Transfers for Failed Nerve Reconstruction. In: Mackinnon SE, editor. Clinics in Plastic Surgery: Peripheral Nerve Surgery. Vol. 30. Philadelphia: W.B. Saunders Company; 2003. pp. 223–246. [DOI] [PubMed] [Google Scholar]
- 3.Van Heest AE, House JH, Cariello C. Upper extremity surgical treatment of cerebral palsy. J Hand Surg [Am] 1999 Mar;24(2):323–330. doi: 10.1053/jhsu.1999.0323. [DOI] [PubMed] [Google Scholar]
- 4.Boyes JH. Tendon Transfers in the Hand; Paper presented at: Medicine of Japan in 1959, Proc 15th Gen Assembly Japan Med Cong; 1959. [Google Scholar]
- 5.Boyes JH. Selection of a donor muscle for tendon transfer. Bull Hosp Joint Dis. 1962 Apr;23:1–4. [PubMed] [Google Scholar]
- 6.Littler JW. Restoration of Power and Stability in the Partially Paralyzed Hand. In: Converse JM, editor. Reconstructive Plastic Surgery. 2. Philadelphia: W.B. Saunders Company; 1977. pp. 3266–3280. [Google Scholar]
- 7.Scuderi C. Tendon Transfers for Irreperable Radial Nerve Paralysis. Surg Gynecol Obstet. 1949;88:643–651. [PubMed] [Google Scholar]
- 8.Lieber RL, Jacobson MD, Fazeli BM, Abrams RA, Botte MJ. Architecture of selected muscles of the arm and forearm: anatomy and implications for tendon transfer. J Hand Surg [Am] 1992 Sep;17(5):787–798. doi: 10.1016/0363-5023(92)90444-t. [DOI] [PubMed] [Google Scholar]
- 9.Brand PW. Biomechanics of tendon transfer. Orthop Clin North Am. 1974 Apr;5(2):205–230. [PubMed] [Google Scholar]
- 10.Freehafer A, Hunter P, Keith M. Determination of muscle-tendon unit properties during tendon transfer. Journal of Hand Surgery. 1979;4(4):331–339. doi: 10.1016/s0363-5023(79)80069-6. [DOI] [PubMed] [Google Scholar]
- 11.Jones R. On suture of nerves, and alternative methods of treatment by transplantation of tendon. British Medical Journal. 1916;1:641–643. doi: 10.1136/bmj.1.2888.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones R. Tendon transplantation in cases of musculospiral injuries not amenable to suture. American Journal of Surgery. 1921;35:333–335. [Google Scholar]
- 13.Brand PW. Tendon transfers in the forearm. In: Flynn JE, editor. Hand Surgery. 2. Baltimore: Williams & Wilkins; 1975. pp. 189–200. [Google Scholar]
- 14.Chuinard RG, Boyes JH, Stark HH, Ashworth CR. Tendon transfers for radial nerve palsy: use of superficialis tendons for digital extension. J Hand Surg [Am] 1978 Nov;3(6):560–570. doi: 10.1016/s0363-5023(78)80007-0. [DOI] [PubMed] [Google Scholar]
- 15.Boyes JH. Tendon transfers for radial palsy. Bull Hosp Joint Dis. 1960;21:97–105. [Google Scholar]
- 16.Kruft S, Von Heimburg D, Reill P. Treatment of irreversible lesion of the radial nerve by tendon transfer: indication and long term results of the Merle d’Aubigne procedure. Plastic and Reconstructive Surgery. 1997;100(3):610–616. doi: 10.1097/00006534-199709000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds C. Preoperative and postoperative management of tendon transfers after radial nerve injury. In: Mackin E, Callahan A, Skirven T, Schneider L, Osterman A, editors. Rehabilitation of the hand and upper extremity. 5. Vol. 1. St. Louis: Mosby; 2002. pp. 821–831. [Google Scholar]