Abstract
Objective
Determine the relative influence of patient's resuscitation preferences on periviable delivery management.
Methods
Surveyed 295 obstetrician-gynecologists about managing periviable preterm premature rupture of membranes. Across 10 vignettes, we systematically varied gestational age; occupation; method of conception; and resuscitation preference. Physicians rated their likelihood (0-10) of proceeding with induction, steroids, and cesarean. Data were analyzed via conjoint analysis.
Results
205 physician responses were included. Median ratings for management decisions were: induction 1.89; steroids 5.00; cesarean for labor 3.89; cesarean for distress 4.11. Gestational age had the greatest influence on physician ratings across all decisions (importance values ranging from 72.6-86.6), followed by patient's resuscitation preference (range= 9.3-21.4).
Conclusion
Gestational age is weighted more heavily than patients’ resuscitation preferences in obstetricians’ decision-making for periviable delivery management. Misalignment of antenatal management with parental resuscitation preferences may adversely affect periviable outcomes. Interventions are needed to facilitate more patient-centered decision-making in periviable care.
Introduction
When periviable delivery occurs, families and physicians face the difficult challenge of making high-stakes, ethically complex ‘end-of-life decisions’ at the beginning of a child's life. Given the high rates of mortality and morbidity among periviable neonates,1 pediatric and obstetrical professional organizations suggest that decision-making at the limits of viability should be preference-sensitive and subject to shared decision-making.2,3 This means that providers should make management decisions that take into account not only patients’ clinical characteristics, but also parents’ resuscitation preferences. Failing to do so risks undermining parents’ autonomy and potentiating decisional regret.
Several studies have explored the attitudes and role of neonatologists in counseling families about resuscitation and extreme prematurity.4-8 However, obstetricians play an important and understudied role in counseling parents.3,9 Moreover, antenatal management decisions regarding steroid administration and mode of delivery have been shown to impact periviable outcomes.10-12
Nevertheless, little research has explored the factors that influence obstetrical management decision-making in the setting of periviability. Because a previous qualitative study reported that obstetricians felt that patients’ resuscitation preferences were central to periviable delivery management decision-making,9 the primary aim of this study is to quantitatively determine the relative influence of parental resuscitation preferences on obstetrical decision-making for periviable deliveries. As a secondary aim, we evaluate the relative influence of a patients’ clinical and sociodemographic characteristics on obstetrical decision-making.
Methods
Study Population
With approval from the Indiana University Institutional Review Board, we recruited a convenience sample of 295 practicing obstetricians from the exhibit hall of the American College of Obstetricians and Gynecologists 61st Annual Clinical Meeting in New Orleans, LA from May 5-8, 2013. General Obstetrician-Gynecologists (OB/GYN) and Maternal Fetal Medicine (MFM) specialists practicing in the United States were included. Physicians in ‘Gyn-only’ practice settings or Gyn subspecialties (Reproductive Endocrinology and Infertility, Uro-gynecology, or Gyn-Oncology) were excluded.
Study Design
Conjoint analysis is a regression-based analytic technique traditionally used in marketing studies to evaluate how product characteristics (i.e., “attributes”) influence consumer decision-making, typically purchase decisions. Recently, these techniques have been applied to study patients’ and physicians’ health care preferences and decision-making.13,14 To do so, study participants are presented with multiple scenarios in which attributes of a medical situation and/or ‘patient’ are systematically varied. For ‘ratings-based’ conjoint analyses, participants are then asked to indicate their likelihood of pursuing a course of action (e.g. administering a vaccine) based on a given combination of attributes. This likelihood rating serves as the outcome of interest, and is modeled as a function of the case attributes using standard regression methods.15
For the purposes of this study, obstetricians received a survey containing 10 clinical case vignettes, along with a demographics questionnaire. Each vignette described a patient presenting with preterm premature rupture of membranes (PPROM) at the threshold of viability with a fetus in breech presentation. Four selected patient characteristics, or attributes, were systematically varied across vignettes, with each attribute having 2 or 3 levels: 1. Gestational Age and Estimated Fetal Weight (levels: 22 1/7 & 494g vs 23 1/7 & 582g vs 24 1/7 & 676g); 2. Occupation (levels: corporate manager vs janitor); 3. Fertility History/Method of Conception (levels: IVF vs spontaneous conception); and 4. Patient Resuscitation Preference (levels: resuscitate vs comfort care vs undecided). Study participants were randomly assigned on a 1:1 basis to receive a set of vignettes in which all patients were described as White or a set in which all patients were described as Black.16 A full-factorial design, which presents every possible combination of patient characteristics, would have required each participant to read and respond to 36 separate scenarios. This would be too lengthy and repetitive for participants; therefore, we utilized a fractional factorial conjoint design. This design, generated based on the orthogonal design algorithms of Addelman,17 using commercially available software (SPSS ORTHOPLAN), was comprised of a representative subset of 9 case profiles. An additional ‘dummy’ case was also included for a total of 10 case vignettes. The instrument took 10-15 minutes to complete in its entirety. Respondents were entered in a raffle and received a gift card as compensation. Of the 295 returned surveys, 90 were excluded from the final analysis because the survey was incomplete or the respondent did not meet study inclusion criterion.
Vignette Development
The clinical case vignette was developed in consultation with a multidisciplinary team of experts (prominent OB/GYN physician researchers, neonatologists, and ethicists). The vignette's patient attributes were determined based on qualitative interviews with OB/GYN physicians regarding factors that influenced their counseling and management of periviability.9 Estimated fetal weights corresponding to the 50%ile were calculated for each GA of interest using the fetal weight estimation developed by Shepard et. al.18 An actual weight was provided in grams, as opposed to the percentile, because we suspected that some providers might utilize weight ‘cut-offs’, or thresholds, in decision-making independent from, or in addition to, GA. Occupations were selected based upon occupational prestige scores,19 occupational status,20 and field-tested occupations subjectively identified as “working class” and “upper-middle class.”21 The vignette, attributes, and levels are described in detail in Appendix A.
Outcomes
After reading each vignette, participants were asked to provide likelihood ratings for 4 decisions. Using an 11-point scale from 0 (Definitely would not) to 10 (Definitely would), they reported their likelihoods of planning to 1) Offer induction 2) Order steroids 3) Perform cesarean section if labor progresses and 4) Perform cesarean section for signs of fetal distress. We included cesarean in labor and for fetal distress as separate outcomes because, while we suspected that the two responses would be consistent, we thought it useful to empirically test and quantify the relationship. While these 4 outcomes do not represent an exhaustive list of management considerations, they were identified as ‘preference-sensitive’ decisions because there is equivocal and/or insufficient data to dictate one ‘correct’ management strategy. Obstetricians have also described deferring to parents’ resuscitation preferences to guide these kinds of decisions.9
Data Analysis
Univariate statistics were utilized to describe the study population as well as provide summary statistics on obstetricians’ likelihood ratings for each of the four decisions of interest (offer induction, order steroids, perform cesarean section for labor, perform cesarean section for distress). For each decision, differences in distributions of the likelihood ratings by vignette were tested using Friedman's test. As for the conjoint analysis, for each vignette, the 4 decision ratings were modeled as a function of the 4 case attributes using standard regression methods. We initially conducted stratified conjoint analyses for White and Black patient vignettes. Results did not vary by patient race in these stratified analyses; therefore, final analyses were conducted in aggregate. A full-profile, ratings-based conjoint analysis was used to evaluate the influence of patient attributes on obstetrical decision-making. This regression analysis breaks the overall likelihood rating (utility) into parts depending on the relative importance of each attribute's levels. These ‘part-worth utilities,’ which are simply beta weights from the regression model, measure how the obstetricians value a particular patient attribute in the context of their management decisions. For example, the likelihood rating for performing CD for distress attributed to GA would be broken into parts based on each of the levels—22, 23, 24 weeks—chosen for this attribute. Positive values are assigned to the levels of GA that are associated with a higher relative likelihood/preference for performing CD for distress. The part-worth utilities for each attribute sum to zero. In addition to part-worth utilities, importance values are also calculated from the regression model, which reflect the percent of total variability in utility accounted for by each attribute. The attributes with the largest part-worth utility ranges (highest – lowest) are the most important in determining preference. Modeling was performed using the SPSS v.21 Conjoint Module.
Results
Study Population
A total of 205 obstetricians were eligible for inclusion in the final analysis. They were 64.9% female, 92.2% Ob/Gyn Generalists and 4.4% were MFMs. See Table 1 for a complete description of the study participants.
Table 1.
Provider characteristics (N=205)
| Provider Characteristic | N(%) |
|---|---|
| Age | 44 (mean); 27-76 (range) |
| # of Years Since Residency | 12.5 (mean); 0-48 (range) |
| # of Periviable Deliveries (last 6 mos.) | 6 (mean); 0-100 (range) |
| Specialty | |
| OB/GYN Generalist | 189 (92.2) |
| Maternal Fetal Medicine (MFM) | 9 (4.4) |
| Other | 3 (1.5) |
| Missing | 4 (2.0) |
| Sex | |
| Male | 70 (34.1) |
| Female | 133 (64.9) |
| Missing | 2 (1.0) |
| Race/Ethnicity | |
| White | 110 (53.7) |
| Black | 54 (26.3) |
| Asian | 25 (12.2) |
| Other | 12 (5.9) |
| Missing | 4 (2.0) |
| Practice Region | |
| Northeast | 61 (29.8) |
| Southeast | 51 (24.9) |
| Midwest | 37 (18.0) |
| West | 32 (15.6) |
| Southwest | 16 (7.8) |
| Missing | 8 (3.9) |
| Practice Setting | |
| Private Practice | 72 (35.1) |
| Health Maintenance Organization | 9 (4.4) |
| Hospital-owned Practice | 56 (27.3) |
| University-based | 49 (23.9) |
| Other | 12 (5.9) |
| Missing | 7 (3.4) |
| Supervise Residents | |
| Yes | 114 (55.6) |
| No | 87 (42.4) |
| Missing | 4 (2.0) |
Likelihood Ratings
Across vignettes, median ratings for each management decision were as follows: induction 1.89; steroids 5.00; cesarean for labor 3.89; cesarean for distress 4.11. For each management decision, the distributions of the likelihood ratings were significantly different across vignettes (p-value < 0.001 for each outcome). Clear and consistent patterns in likelihood ratings are noted for GA and resuscitation preferences (see Table 2). In order to highlight these patterns, we present both mean and median ratings in the table, as the means provide additional support of the interplay between GA and preference. Obstetricians were unlikely to offer induction to patients facing periviable PPROM (overall median=1.89). Obstetricians were most likely to offer induction at lower gestational ages, and at every GA, they were more likely to do so when patients preferred to pursue comfort care rather than resuscitation. However, even among 22 week scenarios with parents pursuing comfort measures, the median rating was only 3.00. Steroids were likely (median rating >5) to be ordered for all 24 week scenarios regardless of parental resuscitation preferences, but only for the 23 week scenarios in which resuscitation was desired were steroids more likely to be ordered than not to be ordered (median=6.00). In fact, at 22 weeks, participants were highly unlikely to order steroids regardless of parental preference (median=0.00). Overall, obstetricians were not likely to offer cesarean—neither in the setting of labor nor fetal distress—for breech periviable neonates (median=3.89 and 4.11, respectively). However, in 24 week scenarios, cesarean was likely to be offered for laboring breech neonates regardless of parental resuscitation preference (range=7.00-10.00); likewise in the case of fetal distress (range=8.00-10.00). Medians were noted to be polarized at the 22 and 24 week extremes. For example, among 24 week scenarios, obstetricians rated a high likelihood of ordering steroids and performing cesarean for labor and fetal distress with all median ratings exceeding 7 across vignettes. Conversely, at 22 weeks, they were highly unlikely to perform these interventions (all medians=0.00). Occupation and fertility history did not show consistent trends in the manner that GA and parental preference did. Moreover, practice patterns did not vary by patient race.
Table 2.
Decision ratings for each vignettea (0=Definitely would not; 10=Definitely would)
| Offer Induction | Mean | Median (IQR) | Vignette | GA | Resuscitation Preference | Occupation | Conception |
|---|---|---|---|---|---|---|---|
| Most likely | 4.4 | 3.0 (0, 10.0) | 2 | 22+1 | comfort | janitor | IVF |
| 3.8 | 1.0 (0, 9.0) | 5 | 22+1 | uncertain | marketing | planned | |
| 3.5 | 1.0 (0, 8.0) | 9 | 22+1 | resuscitation | marketing | planned | |
| 3.3 | 1.0 (0, 7.5) | 1 | 23+1 | comfort | marketing | planned | |
| 2.9 | 1.0 (0, 5.0) | 7 | 23+1 | uncertain | janitor | planned | |
| 2.3 | 0.0 (0, 3.0) | 3 | 23+1 | resuscitation | marketing | IVF | |
| 1.5 | 0.0 (0, 1.0) | 4 | 24+1 | comfort | marketing | planned | |
| 1.1 | 0.0 (0, 1.0) | 6 | 24+1 | uncertain | marketing | IVF | |
| Least likely | 0.9 | 0.0 (0, l.0) | 8 | 24+1 | resuscitation | janitor | planned |
| Order Steroids | Mean | Median (IQR) | Vignette | GA | Resuscitation Preference | Occupation | Conception |
|---|---|---|---|---|---|---|---|
| Most likely | 9.6 | 10.0 (10.0, 10.0) | 8 | 24+1 | resuscitation | janitor | planned |
| 9.5 | 10.0 (10.0, 10.0) | 6 | 24+1 | uncertain | marketing | IVF | |
| 8.8 | 10.0 (9.0, 10.0) | 4 | 24+1 | comfort | marketing | planned | |
| 5.6 | 6.0 (1.0, 10.0) | 3 | 23+1 | resuscitation | marketing | IVF | |
| 4.8 | 5.0 (0, 10.0) | 7 | 23+1 | uncertain | janitor | planned | |
| 4.4 | 3.0 (0, 9.0) | 1 | 23+1 | comfort | marketing | planned | |
| 2.0 | 0.0 (0, 2.5) | 9 | 22+1 | resuscitation | marketing | planned | |
| 1.7 | 0.0 (0, 1.0) | 5 | 22+1 | uncertain | marketing | planned | |
| Least likely | 1.6 | 0.0 (0, 1.0) | 2 | 22+1 | comfort | janitor | IVF |
| CD for Labor | Mean | Median (IQR) | Vignette | GA | Resuscitation Preference | Occupation | Conception |
|---|---|---|---|---|---|---|---|
| Most likely | 7.9 | 10.0 (6.5, 10.0) | 8 | 24+1 | resuscitation | janitor | planned |
| 7.3 | 9.0 (5.0, 10.0) | 6 | 24+1 | uncertain | marketing | IVF | |
| 6.0 | 7.0 (2.0, 10.0) | 4 | 24+1 | comfort | marketing | planned | |
| 4.6 | 4.0 (0, 8.0) | 3 | 23+1 | resuscitation | marketing | IVF | |
| 3.4 | 2.0 (0, 5.5) | 7 | 23+1 | uncertain | janitor | planned | |
| 2.7 | 1.0 (0, 5.0) | 1 | 23+1 | comfort | marketing | planned | |
| 1.9 | 0.0 (0, 3.0) | 9 | 22+1 | resuscitation | marketing | planned | |
| 1.4 | 0.0 (0, 1.0) | 5 | 22+1 | uncertain | marketing | planned | |
| Least likely | 1.0 | 0.0 (0, 1.0) | 2 | 22+1 | comfort | janitor | IVF |
| CD for Distress | Mean | Median (IQR) | Vignette | GA | Resuscitation Preference | Occupation | Conception |
|---|---|---|---|---|---|---|---|
| Most likely | 8.8 | 10.0 (9.0, 10.0) | 8 | 24+1 | resuscitation | janitor | planned |
| 8.2 | 10.0 (7.0, 10.0) | 6 | 24+1 | uncertain | marketing | IVF | |
| 6.7 | 8.0 (4.0, 10.0) | 4 | 24+1 | comfort | marketing | planned | |
| 4.9 | 5.0 (1.0, 10.0) | 3 | 23+1 | resuscitation | marketing | IVF | |
| 3.7 | 3.0 (0, 6.0) | 7 | 23+1 | uncertain | janitor | planned | |
| 2.8 | 1.0 (0, 5.0) | 1 | 23+1 | comfort | marketing | planned | |
| 2.0 | 0.0 (0, 3.0) | 9 | 22+1 | resuscitation | marketing | planned | |
| 1.4 | 0.0 (0, 1.0) | 5 | 22+1 | uncertain | marketing | planned | |
| Least Likely | 1.0 | 0.0 (0, 1.0) | 2 | 22+1 | comfort | janitor | IVF |
Distributions of ratings were significantly different across all decisions (all p<.001 based on Friedman's test).
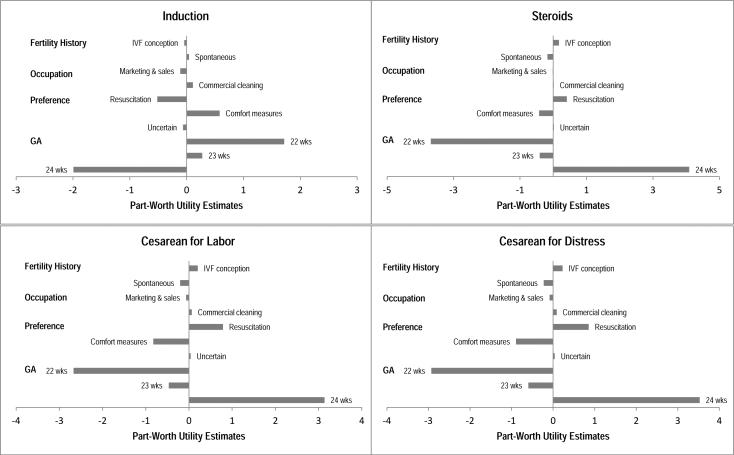
Conjoint analysis results
Table 3 depicts the summary importance rankings. For steroids administration and mode of delivery, GA was the most important factor driving decision-making, followed by resuscitation preference, fertility history, and occupation. For induction, GA and patient preference were also of greatest importance; however, this was followed by occupation then fertility history. Across the four management decisions, importance values for GA ranged from 72.6-86.6. Interestingly, patient resuscitation preference importance values were close to 20 for induction, and mode of delivery, but were only 9.3 for steroids, suggesting that steroid administration was not as sensitive to resuscitation preferences as the other categories. Figure 1 shows the part-worth utility estimates across attributes for each outcome. The strongest physicians preferences (largest utilities) were observed for ordering steroids in 24 week patients compared to 22 and 23 week patients (utility=4.09) and performing cesarean section for labor and distress in the 24 week patient (utilities=3.14 and 3.53, respectively).
Table 3.
Importance values for each management decision (N=205)
| INDUCTION | |
|---|---|
| Attribute | Importance Value |
| GA | 72.55 |
| Preference | 21.44 |
| Occupation | 4.35 |
| Fertility History | 1.66 |
| STEROIDS | |
|---|---|
| Attribute | Importance Value |
| GA | 86.55 |
| Preference | 9.28 |
| Fertility History | 3.84 |
| Occupation | 0.33 |
| CESAREAN FOR LABOR | |
|---|---|
| Attribute | Importance Value |
| GA | 72.96 |
| Preference | 20.27 |
| Fertility History | 5.13 |
| Occupation | 1.64 |
| CESAREAN FOR DISTRESS | |
|---|---|
| Attribute | Importance Value |
| GA | 73.15 |
| Preference | 19.81 |
| Fertility History | 5.12 |
| Occupation | 1.93 |
Figure 1.
Part-worth utility estimates across attributes are presented, stratified by management decision. Part-worth utilities represent the relative weights given to each level of an attribute. Positive values are assigned to the levels with the greatest preference. The part-worth utilities for each attribute sum to zero.
Discussion
An obstetrician's ‘willingness to intervene’ has been shown to impact neonatal outcomes for extremely low birth-weight and periviable neonates.11,12 Therefore, it is important to understand the factors that influence obstetrical management decision-making. To that end, we set out to examine obstetrical decision-making for periviable delivery management, and specifically, to quantify the degree to which obstetrical decision-making is influenced by parental resucitation preferences. We found that GA was the primary driver of obstetrical decision-making, with parental resuscitation preference playing a secondary role. Patient sociodemographic characteristics played a relatively small role.
These findings are somewhat inconsistent with results of previous qualitative work. Obstetricians have previously reported that their decision-making was primarily influenced by patients’ resuscitation preferences--even describing a ‘do-everything default’ attributed to the perception that every patient wanted ‘everything done.’9 However, in this study we found that, when explicitly provided with a patient's resuscitation preference, patient preference was, in fact, not the primary driver of decision-making. One explanation for this discrepancy may lie in institutional norms or policies that utilize GA ‘cut-offs’ to dictate plans of care. It is noteworthy, however, that patient preference played an important, if secondary, role. This confirms the notion that obstetrical decision-making is ‘preference sensitive’ in this setting. We also noted that patient preference played a lesser role in steroid decision-making, which may suggest that obstetricians perceive a stronger evidence-base to guide steroid administration, making it less sensitive to parental preference.
Our study has several limitations. First, as a convenience sample of providers, these results cannot be generalized to all obstetricians. Furthermore, because the obstetricians were in attendance at the Annual Clinical Meeting, obstetrical generalists and community practitioners may be overrepresented. It is important to examine the practices patterns of a community-based sample of obstetricians given that the majority of providers practicing on the ‘front-lines’ and making consultation and transfer decisions are generalists. However, because periviable deliveries occur infrequently, many community-based obstetricians may rarely see these patients, and thus, lack the experience or the facility support to manage these deliveries without consultation or transfer. Therefore, one could argue for future studies that focus more narrowly on generalists and MFMs practicing at academic centers or settings with level III NICUs, as these providers are likely to have the greatest experience with and more direct impact upon periviable outcomes and care. In addition, this study focused on a selected subset of patient characteristics. Future studies should examine parity, maternal age, social support, and pregnancy intendedness or desiredness. Finally, we found that inductions are not readily offered in the periviable period—even among patients desiring comfort care. However, we failed to ascertain whether providers practiced in institutions that prohibited induction of labor at these gestational ages. Institutional policies on induction should be considered in any further efforts to understand physician-practice patterns.
In closing, our findings raise several important questions. To what extent should obstetrical decision-making be sensitive to patients’ preferences? Should patients be given options at 22 weeks; should they have no options after 24? Should we be concerned that inductions are not being offered at 22 weeks to patients desiring comfort care? These are challenging questions, given that long-term neurodevelopmental outcomes are not dramatically improved as gestational age increases from 22 weeks to 24 weeks.1,22 Despite obstetricians’ apparent reliance on GA to guide clinical practice, periviable outcomes are sufficiently poor that one could argue that parental preference should be of primary importance. The American Academy of Pediatrics (AAP) offers the following guidance to the pediatric community:
“When a good outcome is considered very unlikely, the parents should be given the choice of whether resuscitation should be initiated, and clinicians should respect their preference. . . .” (Batton. Peds, 2009).23
To that end, a recent executive summary of a joint pediatric and obstetrical workshop also emphasizes the importance of patient-centered counseling in periviable care for obstetricians as well as neonatologists.3 If obstetrcians and neonatologists attend to parental preference differentially,8 with obstetricians attending more staunchly to GA thresholds, we potentially face a discordance in management planning across specialties—e.g. 23 week neonates are being resuscitated having not received steroids and/or 24 week neonates being delivered by cesarean when parents desire comfort measures. To optimize periviable care, obstetricians and neonatologists alike must be attentive to both the likelihood of a ‘good outcome’ and the parents’ valuation of what a ‘good outcome’ entails. To this end, clarifying issues such as parents’ resuscitation preferences; their thresholds for disability; or their understanding of suffering, is as critical as prognosticating survival.24 This type of values and/or attitudes elicitation would help to align management plans with parental preferences and allow for more coordinated multidisciplinary care. Moving forward, interventions are needed to facilitate values elicitation, promote shared decision-making, and ensure patient-centered periviable care.
Acknowledgements
This publication was made possible in part by Grant Number KL2 TR000163 (A. Shekhar, PI) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award.
Appendix A
Vignette
The patient is a 32 year old {Black OR White} G1P0 now at [GA+] who presents to L&D with confirmed PPROM. Her medical, surgical, and family histories are negative. She denies tobacco, alcohol or drug use, and she [Occupation]. This pregnancy was the result of [Fertility History]. The pregnancy has been uncomplicated. Her prenatal labs, quad screen, and anatomy scan were all normal. She is not contracting or dilated. Her exam is negative for vaginal bleeding and shows no signs of infection. Fetal status is reassuring. Today's ultrasound reveals a female fetus in breech presentation with an EFW of [+EFW] and an AFI of 5.1. The patient has been counseled by the NICU [resuscitation preference].
Attributes and Levels:
| Attribute | # of Levels | Levels |
|---|---|---|
| Gestational Age (GA) + 50%ile Estimated Fetal Weight (EFW) | 3 | • 22+1/7 weeks gestational age, 494g • 23+1/7 weeks gestational age, 582g • 24+1/7 weeks gestational age, 676g |
| Occupation | 2 | • works in corporate marketing and sales as a manager • works in commercial cleaning as a janitor |
| Fertility history/Method of conception | 2 | • a planned, spontaneous conception. She is dated by a 9 wk scan consistent with her LMP. • an IVF conception. She is dated by her Day 3 transfer date. |
| Preference/Plan of care | 3 | • and is planning to pursue resuscitation of the neonate • and is planning to pursue comfort measures only for the neonate • but remains overwhelmed & uncertain about whether to resuscitate the neonate |
Footnotes
Conflict of Interest
The authors report no relevant conflicts of interest.
References
- 1.Kaempf JW, Tomlinson MW, Campbell B, Ferguson L, Stewart VT. Counseling pregnant women who may deliver extremely premature infants: medical care guidelines, family choices, and neonatal outcomes. Pediatrics. 2009 Jun;123(6):1509–1515. doi: 10.1542/peds.2008-2215. [DOI] [PubMed] [Google Scholar]
- 2.Batton B, Burnett C, Verhulst S, Batton D. Extremely preterm infant mortality rates and cesarean deliveries in the United States. Obstetrics and gynecology. 2011 Jul;118(1):43–48. doi: 10.1097/AOG.0b013e318221001c. [DOI] [PubMed] [Google Scholar]
- 3.Raju TN, Mercer BM, Burchfield DJ, Joseph GF. Periviable birth: executive summary of a Joint Workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. J Perinatol. 2014 May;34(5):333–342. doi: 10.1038/jp.2014.70. [DOI] [PubMed] [Google Scholar]
- 4.Doron MW, Veness-Meehan KA, Margolis LH, Holoman EM, Stiles AD. Delivery Room Resuscitation Decisions for Extremely Premature Infants. Pediatrics. 1998 Sep 1;102(3):574–582. doi: 10.1542/peds.102.3.574. 1998. [DOI] [PubMed] [Google Scholar]
- 5.Bastek TK, Richardson DK, Zupancic JA, Burns JP. Prenatal consultation practices at the border of viability: a regional survey. Pediatrics. 2005 Aug;116(2):407–413. doi: 10.1542/peds.2004-1427. [DOI] [PubMed] [Google Scholar]
- 6.Sanders MR, Donohue PK, Oberdorf MA, Rosenkrantz TS, Allen MC. Perceptions of the limit of viability: neonatologists' attitudes toward extremely preterm infants. J Perinatol. 1995 Nov-Dec;15(6):494–502. [PubMed] [Google Scholar]
- 7.Partridge JC, Freeman H, Weiss E, Martinez AM, Kilpatrick S. Delivery room resuscitation decisions for extremely low birthweight infants in California. J Perinatol. 2001 Jan-Feb;21(1):27–33. doi: 10.1038/sj.jp.7200477. [DOI] [PubMed] [Google Scholar]
- 8.Martinez AM, Weiss E, Partridge JC, Freeman H, Kilpatrick S. Management of extremely low birth weight infants: perceptions of viability and parental counseling practices. Obstet Gynecol. 1998 Oct;92(4 Pt 1):520–524. doi: 10.1016/s0029-7844(98)00285-3. [DOI] [PubMed] [Google Scholar]
- 9.Tucker Edmonds B, Krasny S, Srinivas S, Shea J. Obstetric decision-making and counseling at the limits of viability. Am J Obstet Gynecol. 2012 Mar;206(3):248, e241–245. doi: 10.1016/j.ajog.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Carlo WA, McDonald SA, Fanaroff AA, et al. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22 to 25 weeks' gestation. JAMA. 2011 Dec 7;306(21):2348–2358. doi: 10.1001/jama.2011.1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bottoms SF, Paul RH, Iams JD, et al. Obstetric determinants of neonatal survival: influence of willingness to perform cesarean delivery on survival of extremely low-birth-weight infants. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. Am J Obstet Gynecol. 1997 May;176(5):960–966. doi: 10.1016/s0002-9378(97)70386-7. [DOI] [PubMed] [Google Scholar]
- 12.Malloy MH. Impact of Cesarean Section on Neonatal Mortality Rates Among Very Preterm Infants in the United States, 2000-2003. Pediatrics. 2008 Aug 1;122(2):285–292. doi: 10.1542/peds.2007-2620. 2008. [DOI] [PubMed] [Google Scholar]
- 13.Zimet GD, Mays RM, Sturm LA, Ravert AA, Perkins SM, Juliar BE. Parental attitudes about sexually transmitted infection vaccination for their adolescent children. Archives of pediatrics & adolescent medicine. 2005;159(2):132. doi: 10.1001/archpedi.159.2.132. [DOI] [PubMed] [Google Scholar]
- 14.Hendrix KS, Meslin EM, Carroll AE, Downs SM. Attitudes About the Use of Newborn Dried Blood Spots for Research: A Survey of Underrepresented Parents. Academic Pediatrics. 2013;13(5):451–457. doi: 10.1016/j.acap.2013.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orme BK. Getting started with conjoint analysis. Research Publishers, LLC; 2006. [Google Scholar]
- 16.Laskey AL, Stump TE, Perkins SM, Zimet GD, Sherman SJ, Downs SM. Influence of Race and Socioeconomic Status on the Diagnosis of Child Abuse: A Randomized Study. The Journal of Pediatrics. 2012;160(6):1003–1008. e1001. doi: 10.1016/j.jpeds.2011.11.042. 6// [DOI] [PubMed] [Google Scholar]
- 17.Addelman S. Symmetrical and asymmetrical fractional factorial plans. Technometrics. 1962;4(1):47–58. [Google Scholar]
- 18.Shepard MJ, Richards VA, Berkowitz RL, Warsof SL, Hobbins JC. An evaluation of two equations for predicting fetal weight by ultrasound. Am J Obstet Gynecol. 1982 Jan 1;142(1):47–54. doi: 10.1016/s0002-9378(16)32283-9. [DOI] [PubMed] [Google Scholar]
- 19.Nakao K, Treas J. Updating occupational prestige and socioeconomic scores: How the new measures measure up. Sociological methodology. 1994:1–72. [Google Scholar]
- 20.Nam CB, Boyd M. Occupational status in 2000; over a century of census-based measurement. Population Research and Policy Review. 2004;23(4):327–358. [Google Scholar]
- 21.Jackman MR. The Subjective Meaning ofSocial Class Identification inthe United States. Public Opinion Quarterly. 1979;43(4):443–462. [Google Scholar]
- 22.Hintz SR, Kendrick DE, Wilson-Costello DE, et al. Early-childhood neurodevelopmental outcomes are not improving for infants born at <25 weeks' gestational age. Pediatrics. Jan;127(1):62–70. doi: 10.1542/peds.2010-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Batton DG. Clinical report--Antenatal counseling regarding resuscitation at an extremely low gestational age. Pediatrics. 2009 Jul;124(1):422–427. doi: 10.1542/peds.2009-1060. [DOI] [PubMed] [Google Scholar]
- 24.Boss RD, Donohue PK, Roter DL, Larson SM, Arnold RM. “This is a decision you have to make”: using simulation to study prenatal counseling. Simulation in healthcare : journal of the Society for Simulation in Healthcare. 2012 Aug;7(4):207–212. doi: 10.1097/SIH.0b013e318256666a. [DOI] [PubMed] [Google Scholar]