Abstract
Early intervention for potentially serious disorder is a fundamental feature of healthcare across the spectrum of physical illness. It has been a major factor in the reductions in morbidity and mortality that have been achieved in some of the non-communicable diseases, notably cancer and cardiovascular disease. Over the past two decades, an international collaborative effort has been mounted to build the evidence and the capacity for early intervention in the psychotic disorders, notably schizophrenia, where for so long deep pessimism had reigned. The origins and rapid development of early intervention in psychosis are described from a personal and Australian perspective. This uniquely evidence-informed, evidence-building and cost-effective reform provides a blueprint and launch pad to radically change the wider landscape of mental health care and dissolve many of the barriers that have constrained progress for so long.
Key Words: Early intervention, psychosis, prevention, service reform
Although the efficacy of modern treatments in psychiatry is comparable with those in general medicine (Leucht et al., 2012), the reductions in mortality and morbidity seen in cancer and cardiovascular disease over recent decades have proven more elusive in serious mental disorders, such as schizophrenia and other psychoses (Insel, 2010). The conventional wisdom is that such progress must await the discovery of new dramatically more effective treatments based on target mechanisms; however, this has not been the main reason for the improved outcome in the main medical disease categories. Prevention has played a role in reducing the incidence of cardiovascular disease and some cancers, and some new therapeutic strategies have emerged recently; however, early diagnosis and the sustained and sophisticated delivery of existing therapies have been the decisive factors in improving outcomes. Yet across the world, even in the most developed countries, only a small minority of people with mental illness obtain access to evidence-based care, and even then, typically only after prolonged delays (Organization for Economic Co-operation and Development, 2014). The human and economic consequences of this neglect are enormous (Bloom et al., 2011), especially because mental disorders largely begin in young people on the threshold of productive life (Insel and Fenton, 2005). However, the opportunity to save lives, restore and safeguard futures, and strengthen the global economy are equally huge and beckoning (The Economist, 2014). The evidence-based reform of early intervention in psychosis represents a blueprint and launch pad to radically change the landscape and dissolve many of the barriers that have constrained effective mental health care for so long.
ORIGINS
Mental disorders have always been misunderstood, heavily stigmatized, and until recently, actively hidden from public gaze. Even well-intentioned 19th century attempts to make progress through the asylum movement and the development of a descriptive diagnostic system ended up reinforcing these destructive forces. Nowhere is this better illustrated than in the phenomenon of dementia praecox, later schizophrenia, which was deliberately associated conceptually by Emil Kraepelin and his contemporaries with an essentially hopeless future. Although these were serious illnesses and at the time there was no effective treatment, this was a serious conceptual and strategic mistake, and the corrosive pessimism it reinforced was to cloud and impede the care of people with psychosis for over a century. There were early challenges to this orthodoxy. For example, the American social psychiatrist Harry Stack Sullivan stated: “I feel certain that many incipient cases might be arrested before the efficient contact with reality is suspended, and a long stay in institutions made necessary” (Sullivan, 1927, pp. 106–107).
The facts began to get in the way of the Kraepelinian paradigm, with recovery proving more possible in schizophrenia than had been allowed (Bleuler et al., 1976). However, even the advent of effective antipsychotic drugs, developed in the 1950s, and the rise of an embryonic and hopeful community psychiatry, failed to sweep away this pessimism. It was not to be until the 1980s that the focus would turn to the early stages of psychotic illness and the notion of early diagnosis would become a realistic proposition. Initially, this was driven by a research agenda, which correctly proposed that studying first-episode patients free of the many confounding variables that were present in chronic and multiepisode samples would shed more light on etiological questions. However, the establishment of streamed, or discrete, early psychosis programs starkly revealed the clinical imperatives, both from a harm reduction perspective and an opportunity for reductions in premature death and disability and more complete functional recovery. This was certainly our own experience at Royal Park Hospital in Melbourne, where in 1984, we established a 10-bed clinical research unit for first-episode psychosis patients (Copolov et al., 1989; McGorry, 1985). We immediately saw that their clinical needs were very different from those of older multiepisode patients and that the drug and psychosocial therapies offered to the latter ranged from off-key to completely inappropriate or even harmful. These mostly young patients were typically propelled into a hospital after a prolonged period of untreated psychosis as a result of a suicidal crisis or behavioral disturbance, usually with police involvement. They were terrified by their surroundings and the confrontation in the admission ward with an acutely disturbed cohort of much older chronically mentally ill patients. Deep pessimism regarding their future was communicated to them on every level, especially by psychiatrists and nursing staff true to the Kraepelinian traditions of the time and also by the compelling, yet illusory, evidence of the chronicity of the illness that surrounded them in the form of their older copatients (Cohen and Cohen, 1984). These acute units were dangerous places. Not only were their fellow patients disorganized, frightened, and often aggressive, this was also the era of rapid neuroleptization and the drug-naïve first-episode patients were at risk of receiving at least 10 times, if not 30 times, more medication than they needed. Their families were equally shattered by these experiences. Our task was simple. First, we had to reduce or prevent the harm that they were exposed to by separating them from the longer-term patients and the toxic messages and treatments that were draining hope and optimism for the future and find the minimally effective dose of antipsychotics that would result in remission with no, or minimal, side effects. Second, we had to develop and evaluate psychosocial interventions for both patients and families that were truly relevant for their stage of illness and psychosocial development (McGorry, 1992). This task was made possible by doubling our early psychosis bed numbers and creating what was called the “Recovery Program,” anticipating a later international recovery movement aimed at increasing optimism for people living with established illness (Gagne et al., 2007). Psychosocial group programs, early cognitive therapy strategies, and family interventions were explored. Ultimately, we also hoped to find ways to reduce the destructive delays in accessing care and to provide care predominantly in the community. Some of these aspirations would take time and additional resources and required an incubation period (1984–1991) in what we termed our clinical laboratory (McGorry et al., 1996; McGorry and Jackson, 1999). At least one other group, and perhaps others, in the 1980s, led by Marco Merlo in Bern, had recognized the value of creating a streamed, or separate, inpatient space for first-episode patients.
We and most of the new early psychosis programs that followed in the 1990s defined first- episode psychosis and early psychosis as including all psychotic disorders, although in some centers and jurisdictions, psychotic mood disorders were excluded and the focus was on schizophrenia spectrum disorders. I personally disagreed with this approach, for a number of reasons. Some of these were simply practical, as it is so often difficult to separate these two groups in terms of syndrome clarity especially early on and because schizophrenia and bipolar disorder in particular are “late phenotypes,” which manifest and even require a substantial course of illness before the diagnosis can be securely affixed. Second, excluding psychotic mood disorders was problematic because of long-standing doubts regarding the validity of the Kraepelinian dichotomy, which have amplified over the past two decades, and also the mostly similar and overlapping treatment needs of the patients and families.
“A Stitch in Time…”
With this as our new slogan, in 1991–1992, we designed and received new State government funding for a fully fledged model of care called EPPIC (Early Psychosis Prevention and Intervention Centre), which added several community-based components to our streamed inpatient unit and reversed the whole orientation of the program to one of early detection and community-based care with inpatient care as a back-up and last resort (McGorry, 1993; McGorry et al., 1996). A key element was a mobile early psychosis assessment and detection team whose goal was to reduce the duration of untreated psychosis (DUP) and ensure engagement with care was a positive and safe experience wherever possible. Key research had, by this time, indicated that prolonged DUP was common and associated with a wide range of negative immediate consequences as well as worse longer-term outcomes (Loebel et al., 1992; Wyatt, 1991). Other new features were a recovery-oriented outpatient group program and a case management system guaranteeing secure tenure in the service for 2 years after diagnosis. At the time, and indeed still in most of Australia and elsewhere, standard services merely discharged patients back to primary care once the first acute episode had responded, allowing repeat access only once a severe relapse occurred. Within 12 months of EPPIC's opening, a special clinic for subthreshold and potentially prodromal patients was established nearby in a low-stigma adolescent health setting (Phillips et al., 2002; Yung et al., 1995).
The synergy with clinical research continued as a program grant from the Victorian Health Promotion Foundation established the Early Psychosis Research Centre in 1991 and enabled us to conduct our first clinical trials of psychosocial interventions (cognitively oriented psychotherapy for early psychosis) (Jackson et al., 1998, 2001), study the pathways to initial care (Lincoln et al., 1998), and operationally define the prodromal or at-risk mental state through a series of prospective studies (Yung and McGorry, 1996; Yung et al., 2003, 2006). To provide an alternative to hospitalization, we created an extended-hours home treatment capacity to augment the early detection team's capacity and funded this by reducing our inpatient beds from 21 to 14. In the early 1990s, we did not expect or anticipate that early intervention in psychosis would become a sufficient basis for international system reform, as indeed it subsequently did, but felt that, if a cross-diagnostic and developmentally sophisticated approach in young people, aged from early to mid teen to late twenties, were adopted, this might be a stronger platform for a more sustainable paradigm shift. Blending the logic of early intervention with the developmental paradigm, between 1994 and 1996, we were successful in integrating and remodeling an existing older adolescent program with EPPIC to create a complementary early intervention program for non-psychotic young people. This later formed the basis of our more extensive youth mental health reform strategy from 2002 (McGorry, 1996; McGorry et al., 2013).
“An Idea Whose Time Has Come…”
The growing research interest in first-episode psychosis, which began at Northwick Park in London (Crow et al., 1986) and Hillside hospital in New York (Kane et al., 1982; Lieberman et al., 1992) and the seminal paper by Wyatt (1991)focusing on the destructive impact of treatment delay, created a context for exponential growth in early psychosis. This growth was not only in early psychosis research but also in the development of novel, stage-specific interventions and models of care. It is often said with the benefit of hindsight of an idea that has spread that “it's time had come.” However, many such ideas fail to flourish and spread. Powerful ideas must also be “stage-managed” or translated into reality, a process that requires many additional ingredients to mere vision or creativity. Key among these is the demonstration that the idea can work and be sustained in a real-world setting and that it can subsequently be scaled up in many other locations. This aspect, and how research evidence is vital in sustaining the spread of the idea, will be discussed further below. Knowledge of the EPPIC program in Melbourne reached Max Birchwood, a clinical psychologist and an already prominent schizophrenia researcher, who was also beginning to focus on young people with recent-onset psychosis in Birmingham, United Kingdom. He spent a period of sabbatical leave in Melbourne in 1993/1994 in the early phase of EPPIC's development, during which he helpfully characterized the period of illness after the onset of psychosis as the “critical period” (Birchwood and Macmillan, 1993). This notion of a period of maximum vulnerability and virulence of the illness gave a clear logic to why such patients should not be rapidly discharged from the specialist service and should rather be retained within expert specialized early psychosis care in the community for some 2 to 5 years to maximize recovery and limit the risk of relapse and disability. On his return to the United Kingdom, with the support of key health administrators, key clinicians, and consumer/family allies, he established a similar early psychosis clinical program in North Birmingham, which, along with the LEO service at the Institute of Psychiatry in London, developed independently by Paddy Power, Tom Craig, and Phillipa Garety (Power et al., 2007), ultimately provided the blueprint for the national scaling up of early intervention for psychosis under the Blair government in the late 1990s and early 2000s. The Initiative to Reduce the Impact of Schizophrenia project, an activist coalition triggered and inspired by an English general practitioner (GP), Dr David Shiers, whose daughter Mary had developed a psychotic disorder and had received standard care of poor quality in both child and adolescent mental health services (CAMHS) and adult mental health services, and comprising clinical academics (Max Birchwood and Jo Smith), clinicians, and uniquely, senior health executives (Anthony Sheehan and John Mahoney), was a potent influence in bringing about these reforms in the United Kingdom, with which the leadership of EPPIC (myself and Jane Edwards) closely collaborated. David Shiers and Jo Smith subsequently shared national leadership within the National Health Service of the impressive upscaling of early intervention services within the wider mental health reforms of the Blair government during the 2000s. The latter were inspired and engineered by Anthony Sheehan and John Mahony, who had previously piloted these reforms with Birchwood and others in the “clinical laboratory” of North Birmingham.
Another key relationship at that time was forged when Thomas McGlashan, a leading US psychiatrist and schizophrenia researcher, visited Australia in 1994. He was told about the EPPIC initiative by his hosts in another state and decided to make a detour to visit our program. By that stage, we had not only established our early detection and community care system for first-episode psychosis but also were now operating the PACE clinic, a special service in an adolescent health setting for young people with subthreshold psychotic or prodromal symptoms and a need for care. We had already demonstrated that these help-seeking “ultra-high risk” patients were at substantially increased risk of early transition to psychosis. McGlashan was disillusioned, through his work at the once renowned Chestnut Lodge sanitorium in Washington, DC, with the diminishing returns of treating established psychotic illness. Influenced by Wyatt's (1991) paper on DUP and key Norwegian colleagues who had shown that very long DUPs were the norm in first-episode psychosis, even within the advanced health system of Norway, he was planning a sabbatical in Stavanger. He had been engaged by a progressive Norwegian group in Stavanger, led by the visionary chief psychiatrist of the region, Dr Jan Olav Johanessen, to design a research project to test the value of reducing treatment delay. We were introduced to the Stavanger group by McGlashan, and this led to an international symposium with a small number of kindred spirits (including the innovative Ian Falloon, who had explored early intervention on a local scale in rural England in the 1980s) on early intervention in Stavanger in 1995, a special issue of Schizophrenia Bulletin, and a major symposium at the American Psychological Association in New York in 1996. The Scandinavian Tidlig Intervensjon ved Funksjonell Psykose study, one of the major building blocks of evidence in early intervention, was the legacy of this period. In the late 1990s, McGlashan was also responsible for introducing the prodromal focus to the US research environment by establishing the Prevention through Risk Identification, Management and Education clinic at Yale, by adapting the Australian criteria for ultra-high risk for psychosis, and also by modifying the original assessment instrument developed by Alison Yung and our group, the Comprehensive Assessment of At-Risk Mental States (Yung et al., 2005), to become the Structured Interview for Prodromal Symptoms (Miller et al., 2003).
From a long-term perspective, however, a major catalytic event for early intervention occurred in Melbourne, also in 1996, subsequently leading to the establishment of the International Early Psychosis Association (IEPA). EPPIC hosted a major satellite conference following the Collegium Internationale Neuro-Psychopharmacologicum congress held in June of that year, which made it possible to bring together 10 of the leading early psychosis researchers of that era together in one place. We had already held a national early psychosis conference in 1994, and we hopefully named the 1996 meeting, which was attended by more than 600 participants, “Verging on Reality: The First International Early Psychosis Conference.” The keynote papers were later published in a supplement to the British Journal of Psychiatry in 1998, and the meeting proposed and commenced the formation of the IEPA, which was finalized at Stratford-on-Avon at the inaugural UK National Early Psychosis Conference in 1997. There have now been a total of nine International Early Psychosis conferences, in Australia, the United Kingdom, Europe, the United States, Canada, and Japan, with attendances rivaling those seen at the major international schizophrenia meetings. The success of this holistic venture, which spans neuroscience through clinical care, psychotherapy, consumer partnership and engagement, health services, and economics, has been due to a shared vision, coalescing in many places, and with many innovative and inspiring leaders working together in a mutually supportive and collaborative manner over many years. A commitment to evidence-based health care has been a vital pillar for the sustainability of the reform that has accompanied this research-led momentum. Yet ironically, the evidence-based medicine paradigm has been misused at times to question the value of this change in approach, constantly raising the bar for justifying overdue reform, while protecting a dysfunctional status quo from such scrutiny and standards. In fact, much of the more definitive evidence has actually flowed from reform initially based on indicative and best available evidence, consumer and carer dissatisfaction with the poor quality of the status quo, and the face validity of early intervention. Innovation always requires an initial leap of faith that can be validated or discarded on the basis of results. Reform is always necessary to obtain more solid evidence, which conversely is critical in changing course when indicated. That is in fact what has occurred over the past two decades as early intervention for psychosis has weathered early storms and matured.
The scientific literature in early psychosis has expanded exponentially over the past 20 years, and many textbooks have appeared as well (some examples include Addington et al., 2008; Chan et al., 2014; Edwards and McGorry, 2002; French et al., 2010; Fusar-Poli et al., 2012, 2013; Hegelstad et al., 2012; Jackson and McGorry, 2009; Marshall et al., 2005; McGorry, 2002, 2005, 2010, 2011b; McGorry et al., 2010, 2008a, 2009, 2012; 2008b; McGorry and Jackson, 1999; Nordentoft et al., 2014; Van Der Gaag et al., 2013; Yung et al., 2007). The neurobiology of onset is much better understood, and the evidence base for optimal treatment and culture of care is much stronger. More than 60 nations are represented at IEPA conferences now, and hundreds of early psychosis services, first-episode, and prodromal centers have been developed in many countries. These have typically been locally led initiatives and vary in terms of fidelity to a core or optimal model; however, some nations have scaled up services more systematically, some even with widespread or full national coverage. England and Denmark are the best examples of this, although Hong Kong and Canada, especially Ontario, have also been very strong.
CURRENT STATE OF PLAY
Australia
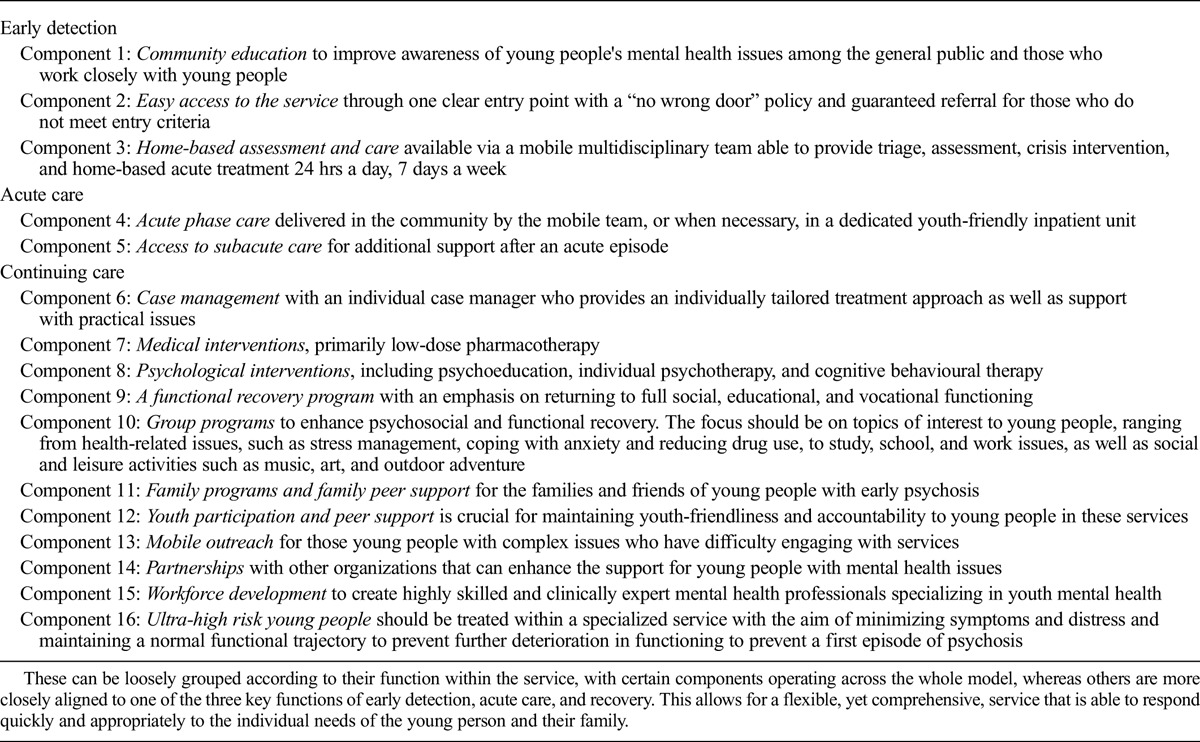
At EPPIC and, later, Orygen, we have continued our research in the neurobiology of onset, much of this in collaboration with Christos Pantelis and his colleagues (McGorry et al., 2014a) and a series of clinical trials and cohort studies aimed at innovation, improving the effectiveness of treatment and service models. In 2003, the State of Victoria added modest, yet discrete, early psychosis case management teams to all adult mental health services, although this was a limited reform that omitted many of the components of a fully fledged early psychosis service. Elsewhere in Australia, reform remained piecemeal until recently, when the Australian Federal government decided to embrace further mental health reform and make early intervention and youth mental health a centerpiece. To complement the growing range of enhanced primary mental health care services for young people under the headspace brand (a further $197 million and 30 new centers announced in 2011—a nationwide program that began in 2005 and that will be in 100 communities by 2016), eight substantial early psychosis services were funded in 2011 and are gradually taking shape in every state and territory with a total funding base of $222 m. These are based on a blueprint derived from an international and national review of evidence and best practice (Orygen Youth Health Research Centre, 2011). The model comprises 16 discrete elements (Table 1), which have been carefully operationalized and will be monitored for fidelity (Hughes et al., 2014). Crucially, the new model includes provision for a cohort of ultra-high risk or potentially prodromal cases and is nested within community-based clusters of the headspace enhanced primary care model for young people.
TABLE 1.
The Core Components of a Specialized Early Psychosis Service
England
The English reforms have been extensive but, despite the development of a national program implementation guide, are somewhat variable in design and quality. For an early intervention model, they seem to have been oddly positioned behind, rather than in front of, the ubiquitous yet poorly evidence-based generic community mental health teams, with the result that DUP remained very long and entry depended on referral from a community mental health team or CAMHS in most cases. It has been shown, for example, that the strongest predictor of a long DUP is ever having been treated in a CAMHS service (Birchwood et al., 2013), where psychosis onset seems to be particularly poorly recognized and treated. Even requiring a GP referral is an unnecessary barrier to access in our experience in Australia, so a secondary barrier to access in addition to the GP is not surprisingly a major one. Nevertheless, the UK reforms have been carefully evaluated from an economic perspective and have been shown to be highly cost-effective (McCrone et al., 2010) as in Australia (Mihalopoulos et al., 2009). Over the past 5 years, there have been extensive cuts to mental health services in England, which, despite the demonstrated capacity of early intervention services to save money, have resulted in the absorption of a number of early intervention services into the generic care system. At the time of writing, with an election approaching, the UK national government has moved to reinvest modestly in early intervention once again, and is considering a broader youth mental health approach in some regions.
Canada
Ontario established a large number of early intervention services in the 2000s following the success of the Prevention and Early Psychosis Program service in London led by Ashok Malla and Ross Norman, the Centre for Addiction and Mental Health first-episode service in Toronto led by Robert Zipursky, and later the Ottawa first-episode program led by Paul Roy. Other provinces, notably Alberta (Jean and Don Addington), British Columbia (Bill McEwen and Karen Tee), and later, Quebec (Ashok Malla), have also established major beachheads for early psychosis care and research but not yet province-wide services. Like Australia, and funded through a unique partnership model of investment from the Canadian Institutes for Health Research and the Graham Boeckh Foundation, Canada is moving to focus research and potentially clinical care more broadly around the needs of young people aged 12 to 25 years with the full range of mental disorders (http://tramcan.ca/).
Denmark
The OPUS model, which, under the leadership of Merete Nordentoft and her colleagues, was the largest demonstration project providing hard evidence for the effectiveness of early psychosis care, has been scaled up across Denmark in recent years, and is being complemented by the establishment of the Australian-inspired headspace model in six locations so far. Extensive research has also been conducted within the OPUS framework.
Norway
The Stavanger group, who showed in the seminal Tidlig Intervensjon ved Funksjonell Psykose project that reducing DUP had long-term benefits for outcome, continues to promote the value of reducing DUP across Norway, stigma reduction, and prodromal research; however, streamed early psychosis services have not yet been a feature of the reforms in Norway.
The Netherlands
Great innovation in research in relation to the boundaries of psychosis and the early stages of illness has been driven through a number of leading Dutch research centers, from Amsterdam (Linszen, De Haan), Maastricht (Van Os), Utrecht (Kahn), and Groningen (Wunderink). However, definitive service reforms are reported to have been hampered by recent cuts.
Germany
The original work of Gerd Huber and his colleagues, notably Joachim Klosterkoetter, and later Stephan Ruhrmann, Frauke Schulze-Lutter, and Andreas Bechdolf, provided an alternative conception of the psychopathology of the prepsychotic stage of illness and evidence in relation to prediction and treatment. In Mannheim, Heinz Häfner and Anita Riecher mapped the onset phase of psychosis with the IRAOS: Instrument for the Retrospective Assessment of the Onset of Schizophrenia and showed the wide time window available for early intervention (Häfner et al., 1992). Other German centers, notably Düsseldorf (Gaebel), also contributed to first episode research.
Asia
Early psychosis programs have been flourishing and producing key research evidence for over a decade in Singapore (Early Psychosis Intervention Program, EPIP) and Hong Kong (Early Assessment Service for Young People with Early Psychosis, EASY) under the leadership of Siow Ann Chong and Eric Chen, respectively. Despite limited resources, better outcomes, reduced suicide rates, and cost savings have already been demonstrated in contrast to traditional services. In Japan (Masafumi Mizuno) and Korea (Young-Chul Chung, Sung-Wan Kim), there are also centers for early psychosis research.
United States
The United States has been a key leader in first-episode research, especially neurobiological research; however, because of the limitations of the US health care system, service reform has been piecemeal until recently. The highly influential and landmark Hillside program, led originally by John Kane, subsequently by Jeffrey Lieberman, and later by Nina Schooler, Barbara Cornblatt (who pioneered the RAPP clinic for clinical high risk cases), and Delbert Robinson, has been an international research leader since the early 1980s. Oregon (Tamara Sale and colleagues) has been the pioneer in service reform, with a statewide commitment to early psychosis care for several years, based on the Early Assessment and Support Alliance model, and more recently, Californian projects have come to fruition, although in a poorly standardized way. California also hosts several key early psychosis centers at University of California, San Francisco (Vinogradov, Loewy), University of California, Davis (Carter), University of California, San Diego (Cadenhead), and University of California, Los Angeles (Cannon, Nuechterlein). In fact, very many US academic centers carry out early psychosis research; however, it is only now that evidence-informed system reform is being driven through National Institute of Mental Health (NIMH) funding of the recovery after an initial schizophrenia episode project, which is testing whether enhancing first-episode psychosis care can improve outcomes (https://raiseetp.org/), and new Federal funding to seed new reform across 44 states with “set-aside” funds from Congress in January 2014. This is incremental research and reform, but pragmatic within the US health care context. North American Prodrome Longitudinal Study (NAPLS) project, led by Ty Cannon, which has integrated the multiple North American prodromal clinics, of which the prevention through risk identification, management and education clinic at Yale was the first, into a coherent research network catalyzed and funded by NIMH is a key platform for new evidence at the subthreshold phase of illness. The role of Robert Heinssen in assembling and nurturing these national research collaborations and the leadership of the current NIMH director, Thomas Insel, have been absolutely crucial in ensuring that early intervention has been placed at the apex of the US mental health research agenda and furthermore is being realized. In a perverse yet positive twist, the recent shooting tragedies in the United States have focused attention and funding on the need to respond more effectively to emerging mental disorders in young people and have added moral force to the logic and evidence supporting early intervention and sustained care.
Other European nations to have made significant research contributions and reforms in early psychosis include Ireland, led by the late Eadbhard O'Callaghan at DETECT; Italy through Programma 2000, led by Anna Meneghelli and Angelo Cocchi; and finally, in Switzerland at multiple sites (Merlo, Riecher, Conus, Simon, and Berger).
RESISTANCE TO REFORM: GENUINE SKEPTICS OR MERCHANTS OF DOUBT?
When one surveys the landscape of premature death, preventable suffering and multiple risks, the blighted lives and the recoveries against the odds, often despite the often harmful, poor quality and at best patchy care offered in most traditional settings for psychotic illness and contrasts this with the effectiveness and cost-effectiveness of expert care for early psychosis when it is provided and sustained, one might wonder why it has not been scaled up even more rapidly and why a small cadre of critics, especially in parts of the “anglosphere,” has fiercely resisted its advance. Whereas the safety of screening and proactive early treatment in cancer and elsewhere has been debated in a logical fashion, the debates concerning early intervention in psychosis have taken on a more strident and, at times, emotional even personal tone (e.g., Frances, 2011). Why should this be the case?
The human mind, and particularly its vicissitudes and dysfunctions, is an extraordinarily complex domain and inhabits the crossroads of many scientific disciplines and philosophical traditions. As a field of medicine, psychiatry has struggled to mature, emerging from the ideas and clinical models of the 19th century only very recently. Continuing funding neglect and its consequences have fueled reductionism and false dichotomies in research and clinical care, and the living memory and continuing experience of suffering and iatrogenesis, the insecurity, and to some extent tribalism, within the mental health professions, notably psychiatry, have undermined the process of maturation of our field and the creation of confidence and public trust. Unholy alliances and crusades readily form in the face of complex and genuine dilemmas and threaten to inhibit reasonable practical stepping stones to solutions, or at least progress. We witnessed these culture wars writ large as the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, was developed and launched (Greenberg, 2013; Maj, 2013).
Skepticism and debate are of course crucial scientific processes to guide and safeguard effective reform. However, extreme or excessive skepticism, especially in relation to a reform with strong face validity, should prompt an analysis of motives because vested interests and ideological groups have been known to misuse science to undermine valid change and reform (Oreskes and Conway, 2010). In some parts of the world, notably the United Kingdom and Australia, yet less so in others (Canada, Asia, Western Europe), we have seen intense skepticism expressed toward early intervention, particularly when the momentum shifted from pure research studies and boutique clinics to serious investment in new early psychosis services. To a great extent, this is understandable in the context of the wholesale neglect of the mental health care of even people with severe and persistent illnesses. Clinicians working in these underfunded and low-morale cultures of care, barely beyond the shadows of the asylum, genuinely feel that much more must be done to effectively treat and relieve the suffering of their patients and their families, especially when this neglect is leading to the criminalization of the mentally ill and the re-warehousing of people with severe mental illnesses in prisons. They fear early intervention will divert scarce, finite, and precious resources from these neglected patients to notionally less deserving patients, often citing the experience of the 1960s, where this did in fact occur in the United States. However, this is so obviously a false dichotomy. The fundamental fallacy that these well-intentioned, yet essentially simplistic, emotion-based critiques promote is that this is a zero sum game. Unlike our colleagues in cancer and other noncommunicable disease areas, they have somehow embraced the notion that substantial growth and parity in funding for mental health care are not an achievable goal and that only one focus, palliation, should be pursued. In fact, even when a zero sum game is clearly not the scenario, as in Australia in 2011, when $2.2 billion of new funding was injected into the national mental health budget across a wide range of targets, we still witnessed intense, albeit focal, resistance from some academic psychiatrists to any new resources being allocated to early intervention, even when substantial new funding was allocated at the same time to services for people with enduring mental illness (Castle, 2012; Frances, 2011; McGorry, 2011a, 2012).
The dichotomy is false for another even more compelling reason. The evidence that early intervention actually saves money in all kinds of ways means that it is almost certainly part of the solution in relation to funding secure longer-term care for the seriously and persistently mentally ill (McCrone et al., 2010; Mihalopoulos et al., 2009). The notion that patients with prolonged and severe mental illness should receive sole priority until their care is truly optimal is part of the mantra of the cadre of critics, yet it is not a principle that would survive in cancer and cardiovascular medicine. Here, we do not see the trivialization of the needs of those in earlier stages or with less severe or persistent forms of illness as the “worried well” or the fanning of fears of labeling and overtreatment (the latter being mostly a consequence of underfunding, poor cultures, low skill levels, and biological reductionism). In cancer, we simply do not see palliative care being pitted against early diagnosis. The threat of a potentially lethal illness is taken very seriously, and a manageable number of false positives is accepted as a reasonable price to pay for saving lives. Perhaps, the definition of the point when a genuine need for assessment and professional care is more challenging in the mental health sphere than in physical medicine; however, such a tipping point undoubtedly exists, is now being better defined, and as long as safe forms of intervention and stigma-free cultures of care are an initial option in a sequential treatment approach, the principle should be the same as in physical medicine. It is important that these conversations, debates, dilemmas, and choices are able to be faced honestly and openly in the light of the facts and the evidence and that they are not buried, distorted, or hijacked by ideologues, vested interests, sensational and irresponsible media, or even misguided humanitarians. These complex scientific and sociological forces must be understood, recognized, and responded to quite differently on their merits within the cycle of innovation and reform.
Innovation is a vital ingredient if we are to dispel the “soft bigotry of low expectations” and the palliative mindset of traditional mental health care. Innovation has been likened to an orchid, exquisitely sensitive to the context and environment (Brooks et al., 2011; Rogers, 1962), and we need to understand the innovation cycle as it applies in other fields. Innovation involves new thinking, new models, new treatments—all of which we desperately need. Innovators and early adopters need to be nurtured as we seek progress in mental health care. Late adopters need to be respected, listened to, persuaded, and convinced on the basis of logic and scientific evidence wherever possible. However, as referred to already, we have seen intense and personal critiques of early intervention from another more desperate group known as the “laggards.” The critiques have come from opposite ends of the ideological spectrum—from the world of antipsychiatry and psychological reductionists on the one hand, who seek to scare the public that more harm than good will be visited on them by an overreaching, dystopian, and biologically reductionist psychiatry, or on the other, from within traditional academic psychiatry, uneasily supported by a phalanx of late adopter mainstream clinicians, who insist that the needs of those with long-term illnesses must be fully addressed before the uncharted and doubtful territory of early diagnosis should be explored. The agenda of the antipsychiatrists is all too clear, although, often, their techniques of misrepresentation, fear-mongering, and personal and reputational attack may be hard to accept. However, the defense with an odd fervor of a failing status quo, which does regrettably rely excessively on medications and seriously neglects evidence-based psychosocial care by some academic psychiatrists, misusing the evidence card to demand impossible standards of proof for any change, is harder to accept (e.g., Burns, 2005). The common feature of these critiques is to go beyond reasonable skepticism to seek to introduce doubt into the minds of the public and policymakers about reforms that have great potential value. Doubt is their product; they are “merchants of doubt” (Oreskes and Conway, 2010).
THE NEXT WAVE OF REFORM: BEYOND PSYCHOSIS
The clinical epidemiology of the onset of mental disorders is more or less the mirror image of that seen in physical illness, with 75% of mental and substance use disorders emerging for the first time by age 25 years. Some of these disorders, notably neurodevelopmental disorders, and some behavioral and anxiety disorders, commence in childhood before the age of 12 years. However, the dominant and potentially persistent and disabling mental and substance use disorders of adult life are by far the major source of health burden during adolescence and emerging adulthood, and yet there has not only been no systematic approach to examining prevention, early diagnosis, and treatment. Worse still, until recently, there has been no sense of urgency to do much at all to intervene to improve their course and outcome. As Gunn (2004) characterized it, this is a form of self-harm that our society inflicts on itself. This obviously has to change.
A conceptual underpinning of this change is the wider application of early intervention beyond psychosis to all disorders and particularly, but not only, in young people. Although there has been exponential expansion of research and clinical activity in early psychosis in recent years, there was little evidence of this trend in other major diagnostic domains, even those such as mood, eating, personality, and substance use disorders, with a similar age of onset. In 2007, to stimulate scientific and clinical interest in early intervention, a new journal was established by Blackwell (subsequently Wiley and Sons), Early Intervention in Psychiatry. Several years on, there has been some growth in early intervention beyond psychosis; however, progress remains slow. Early Intervention in Psychiatry has established itself as a strong international journal, with a rising impact factor and moving to six issues per annum, as the official journal of the IEPA. The latter international association resolved in 2014 to progressively broaden its own focus from psychosis and severe mood disorders to the full range of mental disorders.
This conceptual framework may be difficult to progress given the siloed nature of psychiatric research and organization of specialist clinical care. However, buttressed by more flexible research and diagnostic approaches such as the Research Domain Criteria (Insel et al., 2010) and clinical staging (McGorry, 2007a), a cross-diagnostic focus for early intervention sits alongside a new wave of service reforms in youth mental health in a small number of countries (McGorry et al., 2013, 2014b). These reforms aim to create a comprehensive fully integrated youth mental health service stream for young people that offers seamless mental health care from puberty to mature adulthood up to around 25 years of age, with soft transitions at either boundary with child and older adult mental health care. Such a vertically integrated system embraces the reality of dynamic biopsychosocial development and recognizes the complexity of the challenges faced by young people as they become independent adults, as well the burden of disease imposed on this age group by mental ill-health. It responds by blurring the distinctions and borders between the tiers of primary and specialist care in recognition of the complexity of the presentation of much of the mental ill-health apparent in young people, allowing a flexible and appropriate response for each individual (McGorry et al., 2013, 2014b).
The foundations for reform in mental health must be built on the principles of demonstrable need and capacity to benefit and evidence informed care, including indicative evidence of value for better health outcomes and value for money, which, given the timing of morbidity, is likely to trump almost any other domain of health and social care (McGorry, 2007b; McGorry et al., 2011). Youth mental health is emerging as a new professional field, and evidence will be created as the field evolves. However, we can be optimistic here, not the least because of the success of the early psychosis paradigm, which has not only provided proof-of-concept for early intervention but also has largely driven the current transformation of psychiatry toward a more preventive and personalized focus, analogous to the approach now widespread in physical medicine. The dilemma now is whether health policymakers and planners in different parts of the world pursue a conservative approach and continue to build early psychosis systems in parallel with, or within, mainstream mental health care or leapfrog to a reform that is more ambitious, definitive, and sustainable. My view and prediction are that early psychosis reform will prove to be an insufficient paradigm for radical reform of our systems of mental health care and that a much more inclusive and cross-diagnostic youth mental system to deliver early intervention for all mental disorders is what is now required in all developed countries and, arguably, low- and middle-income countries as well. Early intervention, the keystone of preemptive psychiatry, should now be explored across the full diagnostic spectrum, and this exciting new field promises human, economic, and public health benefits on a much larger scale than could have been envisioned in psychiatry even a decade ago.
ACKNOWLEDGMENTS
This article contains a personal and somewhat ethnocentric perspective (and certainly not an exhaustive review of the evidence) on three decades of hard-won progress in early intervention, and the author takes full responsibility for the views expressed as well as for the inevitable omissions and flaws. However, the progress described is the fruit of an international team effort, and the author acknowledges the extraordinary leadership, innovation and dedication of all of his colleagues at EPPIC and Orygen over several decades. Special appreciation is due to Henry Jackson, Jane Edwards, Alison Yung, Kerryn Pennell, John Moran, Andrew Chanen, Helen Herrman, Heather Stavely, Paddy Power, Peter Burnett, Shona Francey, Dianne Albiston, Eoin Killackey, Christos Pantelis, Lisa Phillips, Barnaby Nelson, and to Bruce Singh and David Copolov. Many others have made key contributions too, including many colleagues, notably Paddy Power, Philippe Conus, Gregor Berger, Andrew Thompson, Rick Fraser, and Martin Lambert, who have all returned to Europe to lead their own early intervention centers. The author sincerely appreciates the creativity, collegiality, trust, and friendship of an array of international colleagues who have enabled this field to flourish in pursuit of a vastly better deal for people with early psychosis and their families and become a template and vehicle for more widespread reform in mental health care. Thanks are also due to our critics who have strengthened our resolve and the quality of our endeavors. Finally, the author is extremely grateful to Sherilyn Goldstone, PhD, for her expert assistance in preparing the manuscript.
DISCLOSURE
Professor McGorry is the executive director of Orygen: the National Centre of Excellence in Youth Mental Health, is editor in chief of Early Intervention in Psychiatry, and also led the design and implementation of headspace, Australia's nationwide model of enhanced youth mental health primary care. He is currently a director of the headspace Board.
Professor McGorry has received grant funding from the Colonial Foundation and the National Health and Medical Research Council of Australia, NARSAD, the Stanley Foundation, and the Australian and Victorian governments. He has also received past unrestricted grant funding from Janssen-Cilag, Astra Zeneca, Bristol-Meyer-Squibb, Eli Lilly and Pfizer, and honoraria for consultancy and teaching from Janssen-Cilag, Eli Lilly, Pfizer, Astra Zeneca, Roche, and Lundbeck.
REFERENCES
- Addington JF, Francey SM, Morrison AP. ( 2008) Working with people at high risk of developing psychosis. New York, NY: Wiley. [Google Scholar]
- Birchwood M, Connor C, Lester H, Patterson P, Freemantle N, Marshall M, Fowler D, Lewis S, Jones P, Amos T, Everard L, Singh SP. ( 2013) Reducing duration of untreated psychosis: Care pathways to early intervention in psychosis services. Br J Psychiatry. 203: 58– 64. [DOI] [PubMed] [Google Scholar]
- Birchwood M, Macmillan F. ( 1993) Early intervention in schizophrenia. Aust N Z J Psychiatry. 27: 374– 378. [DOI] [PubMed] [Google Scholar]
- Bleuler M, Huber G, Gross G, Schuttler R. ( 1976) Long-term course of schizophrenic psychoses. Joint results of two studies. Nervenarzt. 47: 477– 481. [PubMed] [Google Scholar]
- Bloom DE, Cafiero ET, Jane-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, Fiegl AB, Mowafi M, Pandya A, Prettner K, Rosenberg L, Seligman B, Stein A, Weinstein C. ( 2011) The global economic burden of non-communicable disease. Geneva, Switzerland: World Economic Forum. [Google Scholar]
- Brooks H, Pilgrim D, Rogers A. ( 2011) Innovation in mental health services: What are the key components of success? Implement Sci. 6: 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns TA. ( 2005) What evidence is needed for service reforms in mental health care? BMJ. 331: 586.16166109 [Google Scholar]
- Castle DJ. ( 2012) The truth, and nothing but the truth, about early intervention in psychosis. Aust N Z J Psychiatry. 46: 10– 13. [DOI] [PubMed] [Google Scholar]
- Chan SK, So HC, Hui CL, Chang WC, Lee EH, Chung DW, Tso S, Hung SF, Yip KC, Dunn E, Chen EY. ( 2014) 10-year outcome study of an early intervention program for psychosis compared with standard care service. Psychol Med. Published online ahead of print. [DOI] [PubMed] [Google Scholar]
- Cohen P, Cohen J. ( 1984) The clinician's illusion. Arch Gen Psychiatry. 41: 1178– 1182. [DOI] [PubMed] [Google Scholar]
- Copolov DL, McGorry PD, Keks N, Minas IH, Herrman HE, Singh BS. ( 1989) Origins and establishment of the schizophrenia research programme at Royal Park Psychiatric Hospital. Aust N Z J Psychiatry. 23: 443– 451. [DOI] [PubMed] [Google Scholar]
- Crow TJ, MacMillan JF, Johnson AL, Johnstone EC. ( 1986) A randomised controlled trial of prophylactic neuroleptic treatment. Br J Psychiatry. 148: 120– 127. [DOI] [PubMed] [Google Scholar]
- Edwards J, McGorry PD. ( 2002) Implementing early intervention in psychosis: A guide to establishing early psychosis services. London, England: Martin Dunitz. [Google Scholar]
- Frances A. ( 2011) DSM 5 in distress. Psychology Today. Retrieved from http://www.psychologytoday.com/blog/dsm5-in-distress/201105/australias-reckless-experiment-in-early-intervention. [Google Scholar]
- French D, Shiers D, Smith J, Reed M, Rayne M. ( 2010) Promoting recovery in early psychosis: A practice manual. London, England: Wiley Blackwell. [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Barale F, Caverzasi E, McGuire P. ( 2012) Predicting psychosis: A meta-analysis of evidence. Arch Gen Psychiatry. 69: 220– 229. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rossler A, Schultze-Lutter F, Keshavan M, Wood S, Ruhrmann S, Seidman LJ, Valmaggia L, Cannon T, Velthorst E, De Haan L, Cornblatt B, Bonoldi I, Birchwood M, McGlashan T, Carpenter W, McGorry P, Klosterkotter J, McGuire P, Yung A. ( 2013) The psychosis high-risk state: A comprehensive state-of-the-art review. JAMA Psychiatry. 70: 107– 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagne C, White W, Anthony WA. ( 2007) Recovery: A common vision for the fields of mental health and addictions. Psychiatr Rehab J. 31: 32– 37. [DOI] [PubMed] [Google Scholar]
- Greenberg G. ( 2013) The book of woe: The DSM and the unmaking of psychiatry. New York, NY: Blue Rider Press. [Google Scholar]
- Gunn J. ( 2004) Foreword. In Bailey S, Dolan M. (Eds), Adolescent forensic psychiatry. London, England: Arnold, xi. [Google Scholar]
- Häfner H, Riecher-Rossler A, Hambrecht M, Maurer K, Meissner S, Schmidtke A, Fatkenheuer B, Loffler W, van der Heiden W. ( 1992) IRAOS: An instrument for the assessment of onset and early course of schizophrenia. Schizophr Res. 6: 209– 223. [DOI] [PubMed] [Google Scholar]
- Hegelstad WT, Larsen TK, Auestad B, Evensen J, Haahr U, Joa I, Johannesen JO, Langeveld J, Melle I, Opjordsmoen S, Rossberg JI, Rund BR, Simonsen E, Sundet K, Vaglum P, Friis S, McGlashan T. ( 2012) Long-term follow-up of the TIPS early detection in psychosis study: Effects on 10-year outcome. Am J Psychiatry. 169: 374– 380. [DOI] [PubMed] [Google Scholar]
- Hughes F, Stavely H, Simpson R, Goldstone S, Pennell K, McGorry P. ( 2014) At the heart of an early psychosis centre: The core components of the 2014 Early Psychosis Prevention and Intervention Centre model for Australian communities. Australas Psychiatry. 22: 228– 234. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. ( 2010) Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. Am J Psychiatry. 167: 748– 751. [DOI] [PubMed] [Google Scholar]
- Insel TR. ( 2010) Rethinking schizophrenia. Nature. 468: 187– 193. [DOI] [PubMed] [Google Scholar]
- Insel TR, Fenton WS. ( 2005) Psychiatric epidemiology: It's not just about counting anymore. Arch Gen Psychiatry. 62: 590– 592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson H, McGorry P, Edwards J, Hulbert C, Henry L, Francey S, Maude D, Cocks J, Power P, Harrigan S, Dudgeon P. ( 1998) Cognitively-oriented psychotherapy for early psychosis (COPE). Preliminary results. Br J Psychiatry. 172: 93– 100. [PubMed] [Google Scholar]
- Jackson H, McGorry P, Henry L, Edwards J, Hulbert C, Harrigan S, Dudgeon P, Francey S, Maude D, Cocks J, Power P. ( 2001) Cognitively oriented psychotherapy for early psychosis (COPE): A 1-year follow-up. Br J Clin Psychology. 40: 57– 70. [DOI] [PubMed] [Google Scholar]
- Jackson HJ, McGorry PD. ( 2009) The recognition and management of early psychosis: A preventive approach, (2nd ed). Cambridge, United Kingdom: Cambridge University Press. [Google Scholar]
- Kane JM, Rifkin A, Quitkin F, Nayak D, Ramos-Lorenzi J. ( 1982) Fluphenazine vs placebo in patients with remitted, acute first-episode schizophrenia. Arch Gen Psychiatry. 39: 70– 73. [DOI] [PubMed] [Google Scholar]
- Leucht S, Hierl S, Kissling W, Dold M, Davis JM. ( 2012) Putting the efficacy of psychiatric and general medicine medication into perspective: Review of meta-analyses. Br J Psychiatry. 200: 97– 106. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Alvir JM, Woerner M, Degreef G, Bilder RM, Ashtari M, Bogerts B, Mayerhoff DI, Geisler SH, Loebel A, Levy DC, Hinrichson G, Szymanski S, Chakos M, Koreen A, Borenstein M, Kane JM. ( 1992) Prospective study of psychobiology in first-episode schizophrenia at Hillside Hospital. Schizophr Bull. 18: 351– 371. [DOI] [PubMed] [Google Scholar]
- Lincoln C, Harrigan S, McGorry PD. ( 1998) Understanding the topography of the early psychosis pathways. An opportunity to reduce delays in treatment. Br J Psychiatry. 172: 21– 25. [PubMed] [Google Scholar]
- Loebel AD, Lieberman JA, Alvir JM, Mayerhoff DI, Geisler SH, Szymanski SR. ( 1992) Duration of psychosis and outcome in first-episode schizophrenia. Am J Psychiatry. 149: 1183– 1188. [DOI] [PubMed] [Google Scholar]
- Maj M. ( 2013) Adherence to psychiatric treatments and the public image of psychiatry. World Psychiatry. 12: 185– 186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. ( 2005) Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: A systematic review. Arch Gen Psychiatry. 62: 975– 983. [DOI] [PubMed] [Google Scholar]
- McCrone P, Craig TK, Power P, Garety PA. ( 2010) Cost-effectiveness of an early intervention service for people with psychosis. Br J Psychiatry. 196: 377– 382. [DOI] [PubMed] [Google Scholar]
- McGorry PD. ( 1985) The Aubrey Lewis Unit: The origins, development and first year of operation of the clinical research unit and Royal Park Psychiatric Hospital. Dissertation for membership of the Royal Australian and New Zealand College of Psychiatrists. Melbourne, Australia: The Royal Australian and New Zealand College of Psychiatrists. [Google Scholar]
- McGorry PD. ( 1992) The concept of recovery and secondary prevention in psychotic disorders. Aust N Z J Psychiatry. 26: 3– 17. [DOI] [PubMed] [Google Scholar]
- McGorry PD. ( 1993) Early Psychosis Prevention and Intervention Centre. Australas Psychiatry. 1: 32– 34. [DOI] [PubMed] [Google Scholar]
- McGorry PD. ( 1996) The Centre for Young People's Mental Health: Blending epidemiology and developmental psychiatry. Australas Psychiatry. 4: 243– 247. [Google Scholar]
- McGorry PD. ( 2002) The recognition and optimal management of early psychosis: An evidence-based reform. World Psychiatry. 1: 76– 83. [PMC free article] [PubMed] [Google Scholar]
- McGorry PD. ( 2005) Early intervention in psychotic disorders: Beyond debate to solving problems. Br J Psychiatry. 48: s108– s110. [DOI] [PubMed] [Google Scholar]
- McGorry PD. ( 2007a) Issues for DSM-V: Clinical staging: A heuristic pathway to valid nosology and safer, more effective treatment in psychiatry. Am J Psychiatry. 164: 859– 860. [DOI] [PubMed] [Google Scholar]
- McGorry PD. ( 2007b) The Specialist Youth Mental Health Model: Strengthening the weakest link in the public mental health system. Med J Aust. 187: S53– S56. [DOI] [PubMed] [Google Scholar]
- McGorry PD. ( 2010) Evidence, early intervention and the tipping point. Early Interv Psychiatry. 4: 1– 3. [DOI] [PubMed] [Google Scholar]
- McGorry PD. ( 2011a) Australia's mental health reform: Timely intervention and social inclusion. Psychology Today. Retrieved from http://www.psychologytoday.com/blog/dsm5-in-distress/201105/australias-reckless-experiment-in-early-intervention. [Google Scholar]
- McGorry PD. ( 2011b) Pre-emptive intervention in psychosis: Agnostic rather than diagnostic. Aust N Z J Psychiatry. 45: 515– 519. [DOI] [PubMed] [Google Scholar]
- McGorry PD. ( 2012) Truth and reality in early intervention. Aust N Z J Psychiatry. 46: 313– 316. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Bates T, Birchwood M. ( 2013) Designing youth mental health services for the 21st century: Examples from Australia, Ireland and the UK. Br J Psychiatry. 54: s30– s35. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Edwards J, Mihalopoulos C, Harrigan SM, Jackson HJ. ( 1996) EPPIC: An evolving system of early detection and optimal management. Schizophr Bull. 22: 305– 326. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Goldstone SD, Parker AG, Rickwood DJ, Hickie IB. ( 2014a) Cultures for mental health care of young people: An Australian blueprint for reform. Lancet Psychiatry. 1: 559– 568. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Jackson HJ. ( 1999) The recognition and management of early psychosis: A preventive approach. Cambridge, United Kingdom: Cambridge University Press. [Google Scholar]
- McGorry PD, Johanessen JO, Lewis S, Birchwood M, Malla A, Nordentoft M, Addington J, Yung A. ( 2010) Early intervention in psychosis: Keeping faith with evidence-based health care. Psychol Med. 40: 399– 404. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Keshavan M, Goldstone S, Amminger P, Allott K, Berk M, Lavoie S, Pantelis C, Yung A, Wood S, Hickie I. ( 2014b) Biomarkers and clinical staging in psychiatry. World Psychiatry. 13: 211– 223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGorry PD, Killackey E, Yung A. ( 2008a) Early intervention in psychosis: Concepts, evidence and future directions. World Psychiatry. 7: 148– 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGorry PD, Nelson B, Amminger GP, Bechdolf A, Francey SM, Berger G, Riecher-Rossler A, Klosterkotter J, Ruhrmann S, Schultze-Lutter F, Nordentoft M, Hickie I, McGuire P, Berk M, Chen EY, Keshavan MS, Yung AR. ( 2009) Intervention in individuals at ultra high risk for psychosis: A review and future directions. J Clin Psychiatry. 70: 1206– 1212. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Nelson B, Goldstone S. ( 2012) Providing care to young people with emerging risk of psychosis: Balancing potential risks and benefits. Clin Pract. 9: 669– 682. [Google Scholar]
- McGorry PD, Purcell R, Goldstone S, Amminger GP. ( 2011) Age of onset and timing of treatment for mental and substance use disorders: Implications for preventive intervention strategies and models of care. Curr Opin Psychiatry. 24: 301– 306. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Yung AR, Bechdolf A, Amminger P. ( 2008b) Back to the future: predicting and reshaping the course of psychotic disorder. Arch Gen Psychiatry. 65: 25– 27. [DOI] [PubMed] [Google Scholar]
- Mihalopoulos C, Harris M, Henry L, Harrigan S, McGorry P. ( 2009) Is early intervention in psychosis cost-effective over the long term? Schizophr Bull. 35: 909– 918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, McFarlane W, Perkins DO, Pearlson GD, Woods SW. ( 2003) Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: Predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 29: 703– 715. [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Rasmussen JO, Melau M, Hjorthoj CR, Thorup AA. ( 2014) How successful are first episode programs? A review of the evidence for specialised assertive early intervention. Curr Opin Psychiatry. 27: 167– 172. [DOI] [PubMed] [Google Scholar]
- Oreskes N, Conway E. ( 2010) Merchants of doubt. London, England: Bloomsbury Publishing. [Google Scholar]
- Organization for Economic Co-operation and Development ( 2014) Making mental health count. Paris, France: Organization for Economic Co-operation and Development. [Google Scholar]
- Orygen Youth Health Research Centre ( 2011) Early Psychosis Feasibility Study Report. Canberra, Australia: National Advisory Council on Mental Health and Department of Health and Ageing. [Google Scholar]
- Phillips LJ, Leicester SB, O'Dwyer LE, Francey SM, Koutsogiannis J, Abdel-Baki A, Kelly D, Jones S, Vay C, Yung AR, McGorry PD. ( 2002) The PACE Clinic: Identification and management of young people at ‘ultra’ high risk of psychosis. J Psychiatr Pract. 8: 255– 269. [DOI] [PubMed] [Google Scholar]
- Power P, McGuire P, Iacoponi E, Garety P, Morris E, Valmaggia L, Grafton D, Craig T. ( 2007) Lambeth Early Onset and Outreach and support in South London services. Early Interv Psychiatry. 1: 97– 103. [DOI] [PubMed] [Google Scholar]
- Rogers EM. ( 1962) Diffusion of innovations (5th ed). New York: Simon and Schuster. [Google Scholar]
- Sullivan HS. ( 1927) The onset of schizophrenia. Am J Psychiatry. 84: 105– 134. [DOI] [PubMed] [Google Scholar]
- The Economist ( 2014) Mental health and integration. London, England: The Economist. [Google Scholar]
- Van Der Gaag M, Smit F, Bechdolf A, French P, Linszen D, Yung AR, McGorry PD. ( 2013) Preventing a first episode of psychosis: Meta-analysis of randomised controlled prevention trials of 12 month and medium-term follow-ups. Schizophr Res. 149: 56– 62. [DOI] [PubMed] [Google Scholar]
- Wyatt RJ. ( 1991) Neuroleptics and the natural course of schizophrenia. Schizophr Bull. 17: 325– 351. [DOI] [PubMed] [Google Scholar]
- Yung AR, Killackey E, Hetrick SE, Parker AG, Schultze-Lutter F, Klosterkoetter J, Purcell R, McGorry PD. ( 2007) The prevention of schizophrenia. Int Rev Psychiatry. 19: 633– 646. [DOI] [PubMed] [Google Scholar]
- Yung AR, McGorry PD. ( 1996) The initial prodrome in psychosis: Descriptive and qualitative aspects. Aust N Z J Psychiatry. 30: 587– 599. [DOI] [PubMed] [Google Scholar]
- Yung AR, McGorry PD, McFarlane CA, Patton GC. ( 1995) The Pace Clinic: Development of a clinical service for young people at high risk of psychosis. Australas Psychiatry. 3: 345– 349. [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, McGorry PD. ( 2003) Psychosis prediction: 12-month follow up of a high-risk (‘prodromal’) group. Schizophr Res. 60: 21– 32. [DOI] [PubMed] [Google Scholar]
- Yung AR, Stanford C, Cosgrave E, Killackey E, Phillips L, Nelson B, McGorry PD. ( 2006) Testing the ultra high risk (prodromal) criteria for the prediction of psychosis in a clinical sample of young people. Schizophr Res. 84: 57– 66. [DOI] [PubMed] [Google Scholar]
- Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, Francey SM, Cosgrave EM, Killackey E, Stanford C, Godfrey K, Buckby J. ( 2005) Mapping the onset of psychosis: The Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 39: 964– 971. [DOI] [PubMed] [Google Scholar]


