Abstract
Background
Lowering the diagnostic threshold for troponin is controversial because it may disproportionately increase the diagnosis of myocardial infarction in patients without acute coronary syndrome. We assessed the impact of lowering the diagnostic threshold of troponin on the incidence, management, and outcome of patients with type 2 myocardial infarction or myocardial injury.
Methods
Consecutive patients with elevated plasma troponin I concentrations (≥50 ng/L; n = 2929) were classified with type 1 (50%) myocardial infarction, type 2 myocardial infarction or myocardial injury (48%), and type 3 to 5 myocardial infarction (2%) before and after lowering the diagnostic threshold from 200 to 50 ng/L with a sensitive assay. Event-free survival from death and recurrent myocardial infarction was recorded at 1 year.
Results
Lowering the threshold increased the diagnosis of type 2 myocardial infarction or myocardial injury more than type 1 myocardial infarction (672 vs 257 additional patients, P < .001). Patients with myocardial injury or type 2 myocardial infarction were at higher risk of death compared with those with type 1 myocardial infarction (37% vs 16%; relative risk [RR], 2.31; 95% confidence interval [CI], 1.98-2.69) but had fewer recurrent myocardial infarctions (4% vs 12%; RR, 0.35; 95% CI, 0.26-0.49). In patients with troponin concentrations 50 to 199 ng/L, lowering the diagnostic threshold was associated with increased healthcare resource use (P < .05) that reduced recurrent myocardial infarction and death for patients with type 1 myocardial infarction (31% vs 20%; RR, 0.64; 95% CI, 0.41-0.99), but not type 2 myocardial infarction or myocardial injury (36% vs 33%; RR, 0.93; 95% CI, 0.75-1.15).
Conclusions
After implementation of a sensitive troponin assay, the incidence of type 2 myocardial infarction or myocardial injury disproportionately increased and is now as frequent as type 1 myocardial infarction. Outcomes of patients with type 2 myocardial infarction or myocardial injury are poor and do not seem to be modifiable after reclassification despite substantial increases in healthcare resource use.
Keywords: Myocardial infarction, Outcomes, Troponin, Type 2
Clinical Significance.
-
•
Lowering the diagnostic threshold for troponin preferentially increases the number of patients identified with type 2 myocardial infarction or myocardial injury.
-
•
Patients reclassified as having type 2 myocardial infarction or myocardial injury remained in the hospital for longer and were more likely to undergo cardiac investigations but, in contrast to type 1 myocardial infarction, were discharged without additional cardiac therapies and clinical outcomes remained poor and unchanged.
The Universal Definition of Myocardial Infarction proposes a classification for patients with myocardial infarction based on cause to accommodate more sensitive markers of myocardial necrosis.1 The classification differentiates between type 1 myocardial infarction, due to thrombosis of an atherosclerotic plaque, and type 2 myocardial infarction, due to an imbalance of myocardial blood supply and demand that may arise in many acute medical and surgical conditions. The expert consensus further defines evidence of myocardial necrosis in the absence of clinical evidence of myocardial ischemia as myocardial injury. Although this classification has been used in recent clinical trials to refine clinical outcomes,2–4 type 2 myocardial infarction and myocardial injury are difficult to distinguish or diagnose definitively, and the frequency in clinical practice and implications of these diagnoses are uncertain.5,6
After improvements in assay performance, a sensitive troponin assay was introduced into our institution.7,8 The validation and subsequent implementation of this assay provided an opportunity to assess the impact of lowering the diagnostic threshold on the incidence, management, and clinical outcome of patients with type 2 myocardial infarction and myocardial injury.
Materials and Methods
Study Population
We identified consecutive patients admitted to our regional cardiac center (Royal Infirmary, Edinburgh, UK), with plasma cardiac troponin I concentrations ≥50 ng/L irrespective of clinical presentation during the validation and implementation of a contemporary sensitive troponin assay. We report a prespecified analysis from a published cohort study evaluating the impact of implementation of a contemporary sensitive troponin assay on patients with suspected acute coronary syndrome.7 In this analysis, we include all patients in whom troponin was measured as part of routine clinical care whether or not they presented with suspected acute coronary syndrome.
Clinical characteristics as described previously,7 including the primary presenting symptom, referral to specialist cardiology services, cardiac investigations, percutaneous or surgical coronary revascularization, and the use of medical therapies, were obtained through “TrakCare” (InterSystems Corp, Cambridge, Mass), an electronic patient record system used by all hospitals in the National Health Service (NHS), Lothian, United Kingdom. Exclusion criteria included patients admitted for elective nonemergency procedures, patients resident outside of Lothian, and those with incomplete hospital records.
Troponin Assay
Plasma troponin I concentrations were measured using the ARCHITECTSTAT assay (Abbott Laboratories, Abbott Park, Ill). The study was divided into 2 phases: validation and implementation. Although plasma troponin was measured using the reformulated sensitive assay throughout both phases, only concentrations above our previous diagnostic threshold (≥200 ng/L) were reported in the validation phase, whereas concentrations above the revised diagnostic threshold (≥50 ng/L) were reported during the implementation phase.7
Classification of Myocardial Infarction
Patients were classified as having a type 1 myocardial infarction when myocardial necrosis occurred in the context of an isolated presentation with suspected acute coronary syndrome with chest pain or evidence of myocardial ischemia on the electrocardiogram.1 Patients with symptoms and signs of myocardial ischemia on the electrocardiogram that were thought to be due to increased oxygen demand or decreased supply (eg, tachyarrhythmia, hypotension, or anemia) and myocardial necrosis were classified as having a type 2 myocardial infarction. Myocardial injury was defined as evidence of myocardial necrosis in the absence of any clinical features of myocardial ischemia. Myocardial infarction presenting as a sudden unexpected cardiac death (type 3) after percutaneous coronary intervention (type 4) and coronary artery bypass grafting (type 5) were also defined. Each case was reviewed and classified independently by 2 cardiologists, and any discrepancies were resolved by consensus through in-depth review of source data. A total of 400 consecutive patients were classified by 2 internal medicine physicians to determine the generalizability of classification.
Outcomes
Clinical outcomes were identified using national and local population registries, the General Register of Scotland and TrakCare, respectively. The primary outcomes were recurrent type 1 myocardial infarction and all-cause mortality at 1 year. Recurrent myocardial infarction was defined as admission with chest pain or ST-segment deviation of ≥0.5 mm with evidence of myocardial necrosis using plasma troponin concentrations of ≥50 ng/L as the diagnostic threshold. Secondary outcomes were coronary revascularization, stroke, gastrointestinal bleeding,9 and length of stay.
Statistical Analysis
Summary clinical statistics were compared by type of myocardial infarction and between implementation and validation phases using chi-square, Fisher exact, Student t, and Mann-Whitney U tests where appropriate. Agreement for the classification of myocardial infarction was estimated using Cohen's kappa. Cox regression models were used to explore competing risks. Cause-specific hazard ratios were estimated for type 1 versus type 2 myocardial infarction and myocardial injury for time to death and time to recurrent myocardial infarction separately with adjustment for age and sex. Analyses were performed in SPSS (IBM Version 20.0.0; New York, NY) and R (Version 2.14.2, Vienna, Austria).
Results
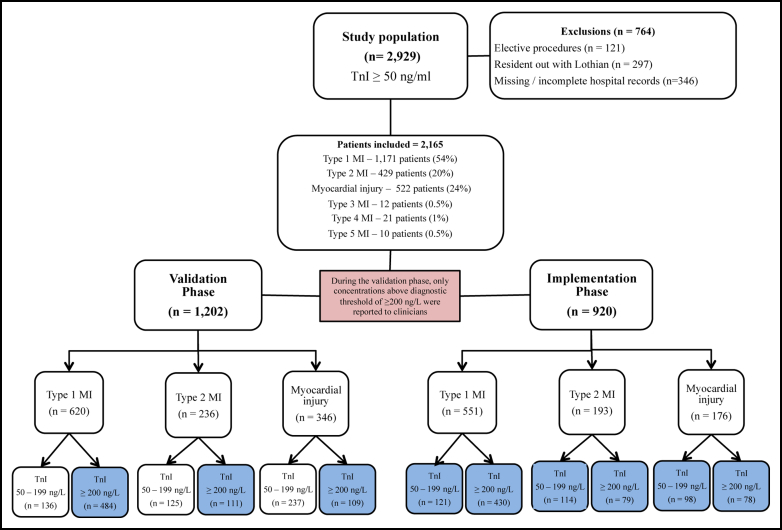
We identified 2929 patients with a peak plasma troponin concentration ≥50 ng/L, of whom 764 met the exclusion criteria (Online Figure 1); 1171 patients (54%) were classified with type 1 myocardial infarction, 429 patients (20%) were classified with type 2 myocardial infarction, 522 patients (24%) were classified with myocardial injury, and 43 patients (2%) were classified with type 3 to 5 myocardial infarction. There was excellent agreement between cardiologists (κ = 0.92; 95% confidence interval [CI], 0.89-0.95) and internal medicine physicians (κ = 0.87, 95% CI, 0.82-0.93) for the classification of myocardial infarction.
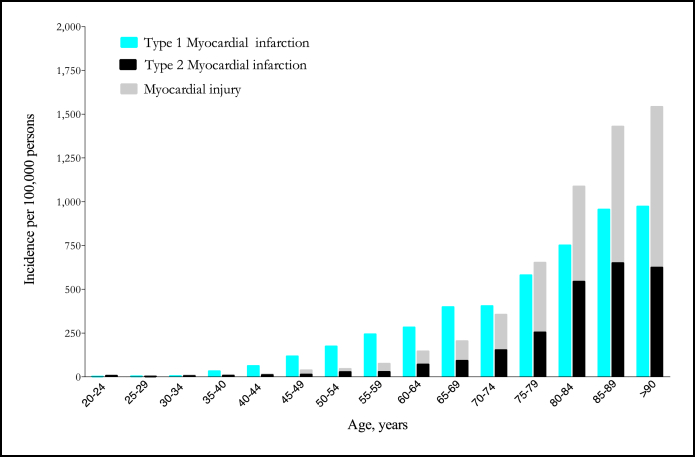
Lowering the diagnostic threshold from 200 to 50 ng/L identified an additional 257 patients with type 1 myocardial infarction, 239 patients with type 2 myocardial infarction, and 335 patients with myocardial injury: a 22%, 56%, and 64% increase, respectively (P < .001). The incidence rate for type 1 myocardial infarction, type 2 myocardial infarction, and myocardial injury increased with age (Figure 1).10
Figure 1.
Incidence rate of type 1 myocardial infarction, type 2 myocardial infarction, and myocardial injury per 100,000 persons in Lothian stratified by age. The incidence rate was estimated as the number of events during the total 12-month period divided by the mid-year population estimates for that age-specific stratum.10 Patients aged <75 years had a higher incidence of type 1 than type 2 myocardial infarction or myocardial injury (124 vs 60 per 100,000 persons), whereas the reverse was true for patients aged ≥75 years (750 vs 1008 per 100,000 persons).
Clinical Characteristics
Compared with patients with type 1 myocardial infarction, patients with type 2 myocardial infarction or myocardial injury were older, had worse renal function, and were more likely to be female (Table 1). Ninety-seven percent of patients with type 1 myocardial infarction had a physician diagnosis of acute coronary syndrome, whereas patients with type 2 myocardial infarction or myocardial injury had a wide range of alternative clinical diagnoses (Online Figure 2). The majority of patients with type 2 myocardial infarction presented with chest pain and had a clear alternative primary diagnosis. Patients with myocardial injury were more likely to present with dyspnea, syncope, or confusion. The most common conditions predisposing to type 2 myocardial infarction or myocardial injury were tachyarrhythmia, heart failure, and respiratory disorders (Table 1).
Table 1.
Baseline Characteristics of Patients with Type 1 Myocardial Infarction, Type 2 Myocardial Infarction, and Myocardial Injury
| Type 1 MI (n = 1171) | Type 2 MI (n = 429) | Myocardial Injury (n = 522) | |
|---|---|---|---|
| Age, y | 68 (14) | 75 (14) | 76 (13) |
| Male sex, (%) | 709 (61%) | 222 (52%) | 260 (50%) |
| Presenting symptom, n (%) | |||
| Ischemic chest pain | 1041 (89%) | 217 (51%) | 0 (0%) |
| Dyspnea | 45 (4%) | 80 (19%) | 172 (33%) |
| Collapse/syncope | 21 (2%) | 31 (7%) | 94 (18%) |
| Falls | 18 (2%) | 40 (9%) | 86 (17%) |
| Confusion | 2 (0%) | 15 (4%) | 23 (4%) |
| Palpitations | 2 (0%) | 4 (1%) | 18 (3%) |
| Abdominal pain | 6 (1%) | 6 (1%) | 12 (2%) |
| Cardiac arrest | 14 (1%) | 0 (0%) | 3 (1%) |
| Medical history, n (%) | |||
| Ischemic heart disease | 497 (45%) | 191 (45%) | 186 (36%) |
| Myocardial infarction | 231 (24%) | 109 (26%) | 107 (21%) |
| Stroke | 92 (8%) | 48 (11%) | 86 (17%) |
| Peripheral vascular disease | 85 (8%) | 29 (7%) | 39 (8%) |
| Previous PCI | 153 (15%) | 17 (4%) | 23 (5%) |
| Previous CABG | 62 (6%) | 30 (7%) | 32 (6%) |
| Risk factors, n (%) | |||
| Current smoker | 380 (34%) | 62 (15%) | 73 (14%) |
| Hypertension | 533 (48%) | 254 (59%) | 303 (59%) |
| Hyperlipidemia | 539 (49%) | 177 (42%) | 202 (39%) |
| Diabetes mellitus | 185 (17%) | 93 (22%) | 96 (19%) |
| Biochemistry | |||
| Hemoglobin, mg/dL | 13.3 (2.0) | 12.1 (2.5) | 12.0 (2.2) |
| Creatinine, mg/dL | 1.2 (0.7) | 1.5 (1.2) | 1.4 (1.4) |
| GFR, mL/min | 69 (26) | 56 (30) | 52 (33) |
| GFR <30 mL/min, % | 89 (8%) | 67 (16%) | 125 (24%) |
| Cholesterol, mg/dL | 185 (50) | 166 (51) | 171 (53) |
| Troponin, ng/L | 2420 (270-15,230) | 140 (70-660) | 130 (60-390) |
| Change in troponin ≥20% | 432 (86%) | 41 (65%) | 41 (79%) |
| Electrocardiography, no (%) | |||
| ST elevation | 427 (38%) | 40 (10%) | 3 (1%) |
| ST depression | 207 (18%) | 152 (36%) | 0 (0%) |
| T-wave inversion | 125 (11%) | 97 (23%) | 13 (3%) |
| Medication on admission, no (%) | |||
| Aspirin | 418 (50%) | 222 (56%) | 244 (54%) |
| Clopidogrel | 100 (12%) | 25 (6%) | 26 (6%) |
| ß-blockers | 257 (31%) | 101 (26%) | 111 (25%) |
| ACE inhibitors | 300 (36%) | 136 (34%) | 158 (35%) |
| Statins | 384 (47%) | 156 (40%) | 191 (42%) |
| Warfarin | 35 (4%) | 38 (10%) | 52 (12%) |
| Proton pump inhibitors | 188 (24%) | 127 (33%) | 135 (30%) |
Values are mean (standard deviation), median (interquartile range), and counts (%).
Conversion factor to SI Units as follows: hemoglobin = 10, creatinine = 88.4, cholesterol = 0.0259.
ACE = angiotensin-converting enzyme; CABG = coronary artery bypass grafting; GFR = glomerular filtration rate; MI = myocardial infarction; PCI = percutaneous coronary intervention; TIMI = Thrombolysis in Myocardial Infarction.
Peak troponin concentrations were higher in patients with type 1 myocardial infarction at 2420 ng/L compared with 140 ng/L and 130 ng/L in patients with type 2 myocardial infarction and myocardial injury, respectively. The majority of patients had a ≥20% change in troponin concentration on serial sampling, and this was similar across all groups. Patients with type 1 myocardial infarction were more likely to have ST-segment elevation on the electrocardiogram, whereas ST-segment depression and T-wave inversion were more common in patients with type 2 myocardial infarction and myocardial injury. The clinical characteristics of patients with type 1 and type 2 myocardial infarction did not differ between the validation and implementation phases (data not shown).
Management During Index Admission
Compared with type 1 myocardial infarction, patients with type 2 myocardial infarction or myocardial injury were less likely to be referred to cardiology services, to undergo inpatient coronary angiography and revascularization, and to be discharged on secondary preventative therapies (P < .01 for all) (Table 2). The median duration of hospital stay was double in patients with type 2 myocardial infarction (median [interquartile range]; 7 [2-17] days) and myocardial injury (10 [4-23] days) compared with type 1 myocardial infarction (4 [2-7] days; P < .001) (Table 2).
Table 2.
Management and Outcomes of Patients with Type 1 Myocardial Infarction, Type 2 Myocardial Infarction, and Myocardial Injury
| Type 1 MI (n = 1171) | Type 2 MI (n = 429) | Myocardial Injury (n = 522) | P Value/RR Type 1 Versus Type 2‖ | P Value/RR Type 2 Versus Myocardial Injury¶ | |
|---|---|---|---|---|---|
| Management, n (%), median (IQR) | |||||
| Cardiology referral | 1004 (87%) | 181 (43%) | 146 (29%) | <.001 | <.001 |
| Length of stay, median days (IQR) | 4 (2-7) | 7 (2-17) | 10 (4-23) | <.001 | <.001 |
| Investigations, n (%) | |||||
| Echocardiography | 340 (30%) | 122 (29%) | 117 (23%) | .535 | .042 |
| Exercise tolerance test | 29 (3%) | 1 (0%) | 0 (0%) | .003 | .451 |
| Angiography | 744 (65%) | 31 (7%) | 19 (4%) | <.001 | .012 |
| Coronary revascularization, n (%) | |||||
| PCI | 564 (49%) | 1 (0%) | 3 (1%) | <.001 | .632 |
| CABG | 56 (5%) | 3 (1%) | 3 (1%) | <.001 | .999 |
| Medications on discharge, n (%) | |||||
| Aspirin | 910 (90%) | 166 (49%) | 192 (49%) | <.001 | .835 |
| Clopidogrel | 831 (80%) | 48 (14%) | 38 (9%) | <.001 | .052 |
| Dual antiplatelet therapy | 789 (76%) | 26 (7%) | 26 (6%) | <.001 | .547 |
| ß-blockers | 660 (63%) | 124 (36%) | 114 (28%) | <.001 | .02 |
| ACE inhibitors | 735 (71%) | 135 (39%) | 159 (39%) | <.001 | .999 |
| Statins | 884 (85%) | 152 (44%) | 190 (46%) | <.001 | .442 |
| Warfarin | 35 (3%) | 52 (15%) | 61 (15%) | <.001 | .965 |
| Proton pump inhibitors | 304 (29%) | 135 (39%) | 150 (37%) | .001 | .508 |
| Outcomes, n (%) | |||||
| Recurrent MI∗ | 141 (12%) | 24 (6%) | 18 (3%) | .46 (0.31-0.71) | .62 (0.34-1.12) |
| Death | 187 (16%) | 134 (31%) | 193 (37%) | 1.95 (1.61-2.37) | 1.19 (0.99-1.42) |
| Recurrent MI/death | 280 (24%) | 144 (34%) | 203 (39%) | 1.40 (1.19-1.66) | 1.16 (0.98-1.38) |
| Gastrointestinal bleeding† | 20 (2%) | 11 (3%) | 7 (1%) | 1.50 (0.73-3.11) | .52 (0.21-1.34) |
| Stroke‡ | 24 (2%) | 11 (3%) | 22 (4%) | 1.25 (0.61-2.53) | 1.64 (0.81-3.35) |
| Coronary revascularization§ | 95 (8%) | 5 (1%) | 5 (1%) | .14 (0.06-0.35) | .82 (0.24-2.82) |
ACE = angiotensin-converting enzyme; CABG = coronary artery bypass grafting; IQR = interquartile range; MI = myocardial infarction; PCI = percutaneous coronary intervention; RR = relative risk.
Recurrent type 1 myocardial infarction.
Includes type II–V bleeding as defined in the recent consensus statement.11
Defined as stroke by the attending physician.
Coronary revascularization includes both percutaneous coronary intervention and coronary artery bypass grafting.
Type 1 myocardial infarction as referent.
Type 2 myocardial infarction as referent.
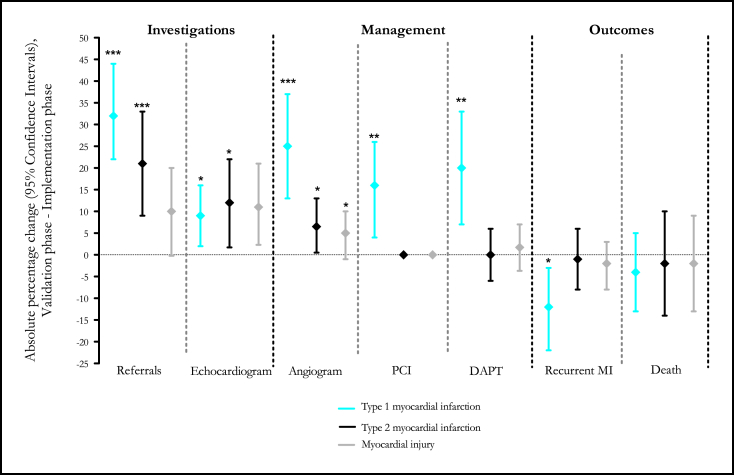
In patients with troponin concentration of 50 to 199 ng/L and type 1 myocardial infarction, lowering the diagnostic threshold increased the number of patients referred for a specialist opinion, further investigations, and treatments for myocardial infarction (P < .01 for all) (Figure 2, Online Table 1). Lowering the diagnostic threshold also increased the number of patients with type 2 myocardial infarction or myocardial injury referred to the cardiologists for further investigation, although the proportion of patients referred was less than for type 1 myocardial infarction and the use of therapies for myocardial infarction was unchanged.
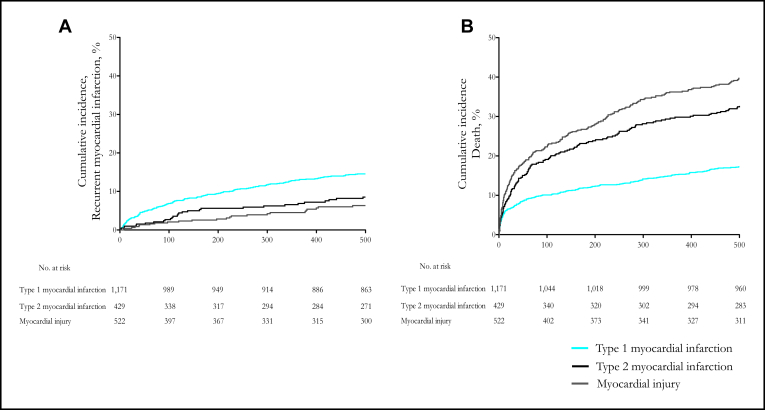
Figure 2.
Cumulative incidence of (A) recurrent myocardial infarction and (B) death in patients with type 1 myocardial infarction, type 2 myocardial infarction, and myocardial injury. Compared with patients with type 1 myocardial infarction, patients with type 2 myocardial infarction or myocardial injury were less likely to be readmitted with myocardial infarction, but were more likely to die at 1 year. In comparison with patients with type 1 myocardial infarction, more patients with type 2 myocardial infarction (16% vs 31%; hazard ratio [HR], 1.62; 95% CI, 1.30-2.04) and myocardial injury (16% vs 37%; HR, 1.87, 95% CI, 1.52-2.30) were dead, but fewer had recurrent myocardial infarction (12% vs 6%; HR, 0.40, 95% CI, 0.26-0.62 and 12% vs 3%; HR, 0.24; 95% CI, 0.15-0.40, respectively) at 1 year. HR presented after adjustment for age and sex with type 1 myocardial infarction as referent.
Clinical Outcomes
Compared with patients with type 1 myocardial infarction, patients with type 2 myocardial infarction were more likely to die (16% vs 37%; relative risk [RR], 1.95; 95% CI, 1.61-2.37) but less likely to have recurrent myocardial infarction (12% vs 6%; RR, 0.46; 95% CI, 0.31-0.71) (Figure 3). Similar risk ratios were obtained for patients with myocardial injury with a higher proportion dead at 1 year (16% vs 37%; RR, 2.36; 95% CI, 1.99-2.81) and fewer recurrent myocardial infarcts (12% vs 4%; RR, 0.29; 95% CI, 0.18-0.46). Similar cause-specific hazards ratio were seen after adjusting for age and sex for both recurrent myocardial infarction and death (Figure 3).
Figure 3.
Change in the investigation, management, and clinical outcomes of patients with type 1 myocardial infarction, type 2 myocardial infarction, and myocardial injury after implementation of a sensitive troponin assay. In patients with troponin concentrations of 50 to 199 ng/L and type 1 myocardial infarction, lowering the diagnostic threshold increased referrals for a specialist opinion, further investigation, and treatments for myocardial infarction (P < .01 for all). For patients with type 2 myocardial infarction and myocardial injury, similar patterns were seen, although the absolute magnitude was smaller. In patients with type 1 myocardial infarction, lowering the diagnostic threshold was associated with a significant reduction in recurrent myocardial infarction (absolute risk reduction, 12%; 95% CI, 3-23), whereas outcomes in patients with type 2 myocardial infarction and myocardial injury remained unchanged. DAPT = dual antiplatelet therapy; MI = myocardial infarction; PCI = percutaneous coronary intervention. *P < .05. ** P < .01. ***P < .001.
In patients with troponin concentration of 50 to 199 ng/L, lowering the diagnostic threshold was associated with a reduction in recurrent myocardial infarction (24% vs 12%; RR, 0.48; 95% CI, 0.27-0.88) in patients with type 1 myocardial infarction, but not in patients with type 2 myocardial infarction or myocardial injury (Figure 2, Online Table 1). Similar reductions were observed for death and recurrent myocardial infarction in patients with type 1 myocardial infarction (31% vs 20%; RR, 0.64; 95% CI, 0.41-0.99), but no change was observed in patients with type 2 myocardial infarction (31% vs 27%; RR, 0.87; 95% CI, 0.59-1.30) or myocardial injury (40% vs 34%; RR, 0.84, 95% CI, 0.61-1.15).
Discussion
The frequency and clinical implications of type 2 myocardial infarction and myocardial injury in clinical practice are uncertain. We have systematically evaluated all patients with elevated plasma troponin concentrations admitted to a regional cardiac center during the validation and implementation of a sensitive troponin assay and have made a number of important and novel observations. First, type 2 myocardial infarction or myocardial injury is as common as type 1 myocardial infarction in clinical practice irrespective of the threshold for diagnosis. The incidence of type 2 myocardial infarction or myocardial injury increases with age and is more common than type 1 myocardial infarction in patients aged ≥75 years. Second, patients with type 2 myocardial infarction or myocardial injury have worse clinical outcomes than patients with type 1 myocardial infarction, with 1 in 3 patients dead at 1 year. Third, lowering the diagnostic threshold preferentially increases the number of patients identified with type 2 myocardial infarction or myocardial injury. Indeed, for every additional patient reclassified with type 1 myocardial infarction, we identified 3 patients with type 2 myocardial infarction or myocardial injury. Finally, patients reclassified as type 2 myocardial infarction or myocardial injury remained in the hospital longer and underwent more cardiac investigations but, in contrast to type 1 myocardial infarction, were discharged without additional cardiac therapies and clinical outcomes remained poor and unchanged.
The Universal Definition makes a distinction between type 2 myocardial infarction and causes of elevations in plasma troponin resulting in myocardial injury, such as renal failure, heart failure,12 sepsis,13,14 and myopericarditis,15 and defines myocardial infarction, regardless of pathobiology, as evidence of myocardial necrosis in the presence of clinical symptoms and signs of myocardial ischemia.16,17 However, it is clinically challenging to distinguish between patients with type 2 myocardial infarction and myocardial injury because there remains considerable overlap between these 2 clinical entities.5,6 The consensus document does not provide specific criteria on how to differentiate between these entities in clinical practice, and our analysis represents one of the first attempts to do so in consecutive hospitalized patients. Thus, our frequency data may differ from those of others who may have applied a different criteria to define type 1 myocardial infarction and may or may not have had a category for myocardial injury. Accordingly, the frequency of type 2 myocardial infarction in our study of 20% (429/2165) was lower than in the only previous reports in which the frequency was 30% (64/701 patients)18 and 26% (144/553 patients)19 in unselected hospitalized patients with elevated troponin concentrations. Our analysis is novel in that we distinguish between patients with type 2 myocardial infarction and myocardial injury, and differences in classification may explain the lower rates of type 2 myocardial infarction in our cohort. Perhaps it is not surprising that type 2 myocardial infarction has been reported to be less frequent (2%-5%) in highly selected populations with myocardial infarction from randomized controlled trials or registries of patients admitted to cardiac units.4,11,20 Our patients were widely distributed across medical and surgical specialties, and it is likely that selection bias has underestimated the true prevalence of type 2 myocardial infarction in these studies.
One of the main strengths of our study is that we identified a group of patients admitted during the validation period in whom plasma troponin concentrations of 50 to 199 ng/L were reported as normal. This allowed us to assess the impact of implementation of a sensitive troponin assay on the management and clinical outcome of these patients. Lowering the diagnostic threshold for myocardial infarction increased the use of appropriate investigations and treatments in patients with type 1 myocardial infarction. This was associated with a reduction in recurrent myocardial infarction and death consistent with our previous report.7 In contrast, there was no improvement in the clinical outcome of patients with type 2 myocardial infarction or myocardial injury despite increased referral to cardiology services and subsequent additional invasive and noninvasive investigations. Approximately one third of patients with type 2 myocardial infarction were dead at 1 year. These findings are consistent with those of Saaby et al,21 who observed mortality rates that were 2-fold higher in patients with type 2 myocardial infarction compared with type 1 myocardial infarction. Of note, despite more patients being identified as having type 2 myocardial infarction after lowering the diagnostic threshold, the majority of these patients did not receive additional therapies for coronary heart disease. This may represent a missed opportunity to improve outcomes, and further prospective studies are required to define the optimal management of patients with type 2 myocardial infarction.
The increased frequency of type 2 myocardial infarction or myocardial injury is likely to be even more marked with the development of the next-generation high-sensitivity troponin assays that will permit further lowering of the diagnostic threshold for myocardial infarction.22-24 These assays are likely to identify an even greater and more disproportionate number of patients with myocardial injury or type 2 myocardial infarction. However, this must not detract from the substantial benefits that high-sensitivity assays will confer for diagnosing patients with type 1 myocardial infarction.25,26 This underlines the need to provide additional guidance on how to distinguish between myocardial infarction and myocardial injury.27
We believe there remains scope for clarification of the diagnostic criteria for type 2 myocardial infarction and that this is necessary to help clinicians adopt the proposed classification. Acute myocardial injury should be the initial diagnosis in all patients with troponin elevations due to supply–demand imbalance, including those with chest pain or evidence of myocardial ischemia. This would be in keeping with many other organ systems, such as acute liver or kidney injury, where similar elevations in tissue enzymes or biomarkers confer major prognostic value but are not disease specific. In our opinion, type 2 myocardial infarction classification should be used exclusively in patients in whom coronary artery disease has contributed to myocardial injury and there may be opportunities to improve outcomes through medical therapy or coronary revascularization. Selection of patients for further investigation will depend on the mechanism of myocardial injury and the patient's probability of having coronary artery disease.5
Study Limitations
Despite our careful attempts to classify patients, we were reliant on investigations performed by attending clinicians. Although agreement between our adjudicating cardiologists and internal medicine physicians was excellent, we accept that a small proportion of patients with type 2 myocardial infarction or myocardial injury may have been misclassified. Furthermore, we were unable to differentiate between acute and chronic myocardial injury in many patients because serial samples were requested at the discretion of the clinical team and were not routinely obtained in patients without suspected acute coronary syndrome.
Conclusions
We have demonstrated that type 2 myocardial infarction and myocardial injury are now as common as type 1 myocardial infarction in clinical practice. With the use of a sensitive troponin assay, we identified 3 patients with type 2 myocardial infarction or myocardial injury for every patient reclassified with type 1 myocardial infarction. Although this was associated with better treatment and outcomes in patients with type 1 myocardial infarction, patients with type 2 myocardial infarction or myocardial injury underwent more investigations and used additional cardiac services without altering their poor clinical outcome.
Footnotes
Funding: British Heart Foundation Intermediate Fellowship (FS/10/024/28266) and Clinical Research Fellowship (SS/CH/09/002).
Conflict of Interest: ASVS, SW, and NLM have received honoraria for Abbott Diagnostics, and NLM has acted as a consultant for Beckman-Coulter and Abbott Diagnostics. ASJ has consulted for most of the major diagnostic companies.
Authorship: All authors had access to the data and played a role in writing this manuscript.
ASVS and DAM have contributed equally.
Appendix
Online Figure 1.
CONSORT diagram of study population stratified by infarct type and study phase. Consecutive patients with plasma troponin I concentrations ≥50 ng/L were identified irrespective of clinical presentation during the validation (February 1, 2008, to July 31, 2008) and implementation (February 1, 2009, to July 31, 2009) of a contemporary sensitive troponin I assay (n = 2929). Exclusion criteria were limited to patients admitted for elective nonemergency procedures, patients who were resident outside of Lothian, and patients with incomplete hospital records. The remaining 2165 patients were classified with type 1 to 5 myocardial infarction or myocardial injury. Although plasma troponin was measured using a reformulated sensitive assay throughout both phases, only concentrations above a diagnostic threshold of 200 ng/L were reported in the validation phase, whereas concentrations above a revised diagnostic threshold of 50 ng/mL were reported during the implementation phase. MI = myocardial infarction.
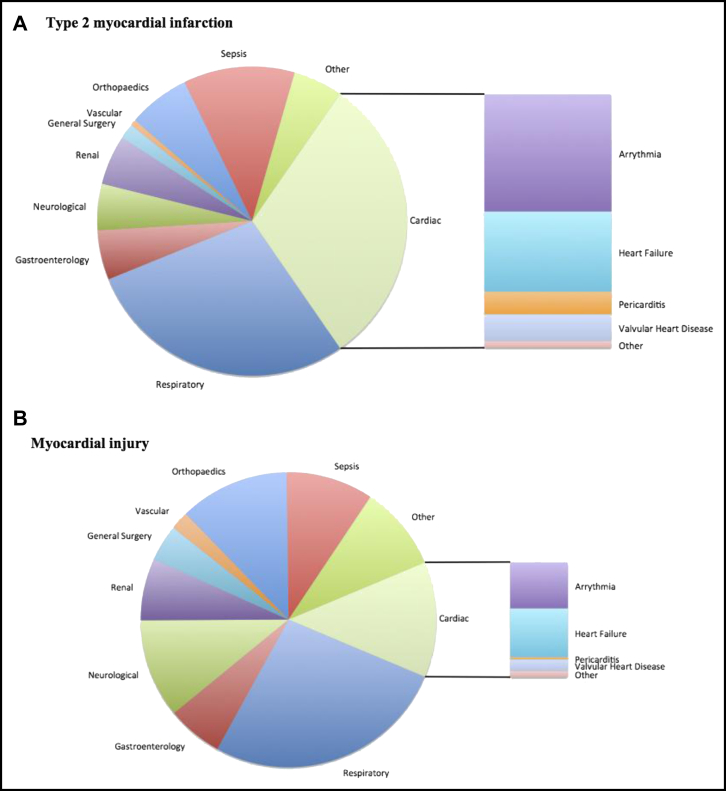
Online Figure 2.
Primary diagnosis of patients with type 2 myocardial infarction and myocardial injury. Patients classified with (A) type 2 myocardial infarction or (B) myocardial injury were a heterogeneous group presenting to a wide range of medical and surgical specialties. Most patients with type 2 myocardial infarction had a cardiac or respiratory diagnosis, with heart failure and arrhythmias the most common cause of elevated troponin concentrations.
Online Table 1.
Clinical Investigations, Management, and Outcomes in Patients with Troponin Concentration Between 50 and 199 ng/L in Patients with Type 1 Myocardial Infarction, Type 2 Myocardial Infarction, and Myocardial Injury
| Validation (n = 136) | Implementation (n = 121) | P Value/Relative Risk‖ (95% CI) | Validation (n = 125) | Implementation (n = 114) | P Value/Relative Risk‖ (95% CI) | Validation (n = 237) | Implementation (n = 98) | P Value/Relative Risk‖ (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|
| Cardiology referral | 67 (50%) | 96 (83%) | <.001 | 31 (26%) | 53 (48%) | .001 | 40 (18%) | 27 (28%) | .043 |
| Investigations, n (%) | |||||||||
| Echocardiography | 6 (4%) | 16 (13%) | .014 | 19 (15%) | 31 (27%) | .023 | 28 (12%) | 23 (24%) | .007 |
| Exercise tolerance test | 6 (4%) | 3 (2%) | >.99 | 1 (1%) | 0 (0%) | .999 | 0 (0%) | 0 (0%) | – |
| Angiography | 36 (27%) | 60 (52%) | <.001 | 3 (3%) | 10 (9%) | .032 | 2 (1%) | 5 (5%) | .025 |
| Coronary revascularization, n (%) | |||||||||
| PCI | 19 (14%) | 34 (30%) | .005 | 1 (1%) | 0 (0%) | .999 | 0 (0%) | 0 (0%) | – |
| CABG | 7 (5%) | 3 (3%) | 1.00 | 1 (1%) | 1 (1%) | .999 | 0 (0%) | 0 (0%) | .376 |
| Medications on discharge, n (%) | |||||||||
| Aspirin | 91 (73%) | 95 (85%) | .038 | 52 (47%) | 53 (54%) | .366 | 92 (47%) | 35 (43%) | .595 |
| Clopidogrel | 53 (43%) | 75 (63%) | .002 | 10 (9%) | 11 (11%) | .628 | 8 (4%) | 7 (9%) | .124 |
| Dual antiplatelet therapy | 47 (38%) | 65 (58%) | .003 | 6 (6%) | 5 (5%) | .896 | 4 (2%) | 3 (4%) | .418 |
| ß-blockers | 68 (55%) | 67 (60%) | .511 | 37 (34%) | 37 (37%) | .573 | 50 (25%) | 23 (28%) | .572 |
| ACE-inhibitors | 64 (52%) | 76 (68%) | .017 | 39 (36%) | 45 (46%) | .141 | 70 (35%) | 38 (47%) | .072 |
| Statins | 82 (57%) | 85 (76%) | .150 | 42 (38%) | 49 (50%) | .100 | 95 (48%) | 31 (38%) | .130 |
| Warfarin | 9 (5%) | 7 (6%) | .770 | 18 (17%) | 17 (17%) | .923 | 26 (13%) | 15 (19%) | .263 |
| Proton pump inhibitors | 23 (23%) | 51 (46%) | .001 | 41 (38%) | 33 (33%) | .488 | 60 (31%) | 30 (37%) | .299 |
| 12-mo outcomes, n (%) | |||||||||
| Recurrent MI∗ | 33 (24%) | 14 (12%) | .48 (0.27-0.88) | 10 (8%) | 8 (7%) | .88 (0.36-2.14) | 13 (6%) | 3 (3%) | .56 (0.19-1.92) |
| Death | 19 (14%) | 12 (10%) | .71 (0.36-1.40) | 34 (27%) | 29 (25%) | .94 (0.61-1.43) | 86 (36%) | 33 (34%) | .93 (0.67-1.28) |
| Recurrent MI/death | 42 (31%) | 24 (20%) | .64 (0.41-0.99) | 39 (31%) | 31 (27%) | .87 (0.59-1.30) | 95 (40%) | 33 (34%) | .84 (0.61-1.15) |
| Gastrointestinal bleeding† | 2 (2%) | 3 (3%) | 1.67 (0.29-9.92) | 2 (2%) | 2 (2%) | 1.10 (0.16-7.66) | 3 (1%) | 4 (4%) | 3.22 (0.73-14.14) |
| Stroke‡ | 2 (2%) | 1 (1%) | .56 (0.05-6.12) | 2 (2%) | 3 (3%) | 1.10 (0.23-5.32) | 13 (6%) | 3 (3%) | .56 (0.16-1.92) |
| Coronary revascularization§ | 17 (13%) | 15 (12%) | .99 (0.51-1.90) | 1 (1%) | 1 (1%) | 1.10 (0.07-17.32) | 4 (2%) | 0 (0%) | – |
Values are mean (standard deviation), median (interquartile range), and counts (%).
ACE = angiotensin-converting enzyme; CABG = coronary artery bypass grafting; MI = myocardial infarction; PCI = percutaneous coronary intervention.
Recurrent type 1 myocardial infarction.
Includes type 2–V bleeding as defined in the recent consensus statement.11
Defined as stroke by the attending physician.
Coronary revascularization includes both percutaneous coronary intervention and coronary artery bypass grafting.
RRs comparing implementation phase with validation phase as the reference group.
References
- 1.Thygesen K., Alpert J.S., Jaffe A.S. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 2.Morrow D.A., Wiviott S.D., White H.D. Effect of the novel thienopyridine prasugrel compared with clopidogrel on spontaneous and procedural myocardial infarction in the Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel-Thrombolysis in Myocardial Infarction 38: an application of the classification system from the universal definition of myocardial infarction. Circulation. 2009;119:2758–2764. doi: 10.1161/CIRCULATIONAHA.108.833665. [DOI] [PubMed] [Google Scholar]
- 3.Bonaca M.P., Wiviott S.D., Braunwald E. American College of Cardiology/American Heart Association/European Society of Cardiology/World Heart Federation universal definition of myocardial infarction classification system and the risk of cardiovascular death: observations from the TRITON-TIMI 38 trial. Circulation. 2012;125:577–583. doi: 10.1161/CIRCULATIONAHA.111.041160. [DOI] [PubMed] [Google Scholar]
- 4.White H.D., Reynolds H.R., Carvalho A.C. Reinfarction after percutaneous coronary intervention or medical management using the universal definition in patients with total occlusion after myocardial infarction: Results from long-term follow-up of the occluded artery trial (OAT) cohort. Am Heart J. 2012;163:563–571. doi: 10.1016/j.ahj.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alpert J.S., Thygesen K.A., White H.D., Jaffe A.S. Diagnostic and therapeutic implications of type 2 myocardial infarction: review and commentary. Am J Med. 2014;127:105–108. doi: 10.1016/j.amjmed.2013.09.031. [DOI] [PubMed] [Google Scholar]
- 6.Sandoval Y., Smith S.W., Thordsen S.E., Apple F.S. Supply/demand type 2 myocardial infarction: Should we be paying more attention? J Am Coll Cardiol. 2014;63:2079–2087. doi: 10.1016/j.jacc.2014.02.541. [DOI] [PubMed] [Google Scholar]
- 7.Mills N.L., Churchhouse A.M., Lee K.K. Implementation of a sensitive troponin I assay and risk of recurrent myocardial infarction and death in patients with suspected acute coronary syndrome. JAMA. 2011;305:1210–1216. doi: 10.1001/jama.2011.338. [DOI] [PubMed] [Google Scholar]
- 8.Mills N.L., Lee K.K., McAllister D.A. Implications of lowering threshold of plasma troponin concentration in diagnosis of myocardial infarction: cohort study. BMJ. 2012;344:e1533. doi: 10.1136/bmj.e1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehran R., Rao S.V., Bhatt D.L. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the bleeding academic research consortium. Circulation. 2011;123:2736–2747. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 10.Mid-2009 population estimates for Scotland: Population estimates by sex, age and administrative area. Available at: http://www.gro-scotland.gov.uk/statistics/theme/population/estimates/mid-year/index.html. Accessed June 4, 2014.
- 11.Stein G.Y., Herscovici G., Korenfeld R. Type-II myocardial infarction–patient characteristics, management and outcomes. PLoS One. 2014;9:e84285. doi: 10.1371/journal.pone.0084285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peacock W.F., De Marco T., Fonarow G.C. Cardiac troponin and outcome in acute heart failure. N Engl J Med. 2008;358:2117–2126. doi: 10.1056/NEJMoa0706824. [DOI] [PubMed] [Google Scholar]
- 13.Newby L.K., Rodriguez I., Finkle J. Troponin measurements during drug development-considerations for monitoring and management of potential cardiotoxicity: an educational collaboration among the cardiac safety research consortium, the duke clinical research institute, and the us food and drug administration. Am Heart J. 2011;162:64–73. doi: 10.1016/j.ahj.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Markou N., Gregorakos L., Myrianthefs P. Increased blood troponin levels in ICU patients. Curr Opin Crit Care. 2011;17:454–463. doi: 10.1097/MCC.0b013e3283491f0d. [DOI] [PubMed] [Google Scholar]
- 15.Newby L.K., Ohman E.M. Troponins in pericarditis: Implications for diagnosis and management of chest pains patients. Eur Heart J. 2000;21:798–800. doi: 10.1053/euhj.1999.2056. [DOI] [PubMed] [Google Scholar]
- 16.Chin C.W., Shah A.S., McAllister D.A. High-sensitivity troponin I concentrations are a marker of an advanced hypertrophic response and adverse outcomes in patients with aortic stenosis. Eur Heart J. 2014;35:2312–2321. doi: 10.1093/eurheartj/ehu189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah A.S., Chin C.W., Vassiliou V. Left ventricular hypertrophy with strain and aortic stenosis. Circulation. 2014;130:1607–1616. doi: 10.1161/CIRCULATIONAHA.114.011085. [DOI] [PubMed] [Google Scholar]
- 18.Javed U., Aftab W., Ambrose J.A. Frequency of elevated troponin I and diagnosis of acute myocardial infarction. Am J Cardiol. 2009;104:9–13. doi: 10.1016/j.amjcard.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Saaby L., Poulsen T.S., Hosbond S. Classification of myocardial infarction: frequency and features of type 2 myocardial infarction. Am J Med. 2013;126:789–797. doi: 10.1016/j.amjmed.2013.02.029. [DOI] [PubMed] [Google Scholar]
- 20.Szymański F.M., Karpiński G., Płatek A.E. Clinical characteristics, aetiology and occurrence of type 2 acute myocardial infarction. Kardiol Pol. 2014;72:339–344. doi: 10.5603/KP.a2013.0284. [DOI] [PubMed] [Google Scholar]
- 21.Saaby L., Poulsen T.S., Diederichsen A.C. Mortality rate in type 2 myocardial infarction: observations from an unselected hospital cohort. Am J Med. 2014;127:295–302. doi: 10.1016/j.amjmed.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 22.Shah A.S., Newby D.E., Mills N.L. High sensitivity cardiac troponin in patients with chest pain. BMJ. 2013;347:f4222. doi: 10.1136/bmj.f4222. [DOI] [PubMed] [Google Scholar]
- 23.Jaffe A.S., Apple F.S., Morrow D.A., Lindahl B., Katus H.A. Being rational about (im)precision: a statement from the Biochemistry Subcommittee of the Joint European Society of Cardiology/American College of Cardiology Foundation/American Heart Association/World Heart Federation Task Force for the Definition of Myocardial Infarction. Clin Chem. 2010;56:941–943. doi: 10.1373/clinchem.2010.143958. [DOI] [PubMed] [Google Scholar]
- 24.Apple F.S., Collinson P.O. Analytical characteristics of high-sensitivity cardiac troponin assays. Clin Chem. 2012;58:54–61. doi: 10.1373/clinchem.2011.165795. [DOI] [PubMed] [Google Scholar]
- 25.Keller T., Zeller T., Ojeda F. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA. 2011;306:2684–2693. doi: 10.1001/jama.2011.1896. [DOI] [PubMed] [Google Scholar]
- 26.Reichlin T., Irfan A., Twerenbold R. Utility of absolute and relative changes in cardiac troponin concentrations in the early diagnosis of acute myocardial infarction. Circulation. 2011;124:136–145. doi: 10.1161/CIRCULATIONAHA.111.023937. [DOI] [PubMed] [Google Scholar]
- 27.Haaf P., Drexler B., Reichlin T. High-sensitivity cardiac troponin in the distinction of acute myocardial infarction from acute cardiac non-coronary artery disease. Circulation. 2012;126:31–40. doi: 10.1161/CIRCULATIONAHA.112.100867. [DOI] [PubMed] [Google Scholar]