Abstract
BACKGROUND
The authors investigated the prevalence, determinants of, and disparities in any perceived unmet need for 8 supportive services (home nurse, support group, psychological services, social worker, physical/occupational rehabilitation, pain management, spiritual counseling, and smoking cessation) by race/ethnicity and nativity and how it is associated with perceived quality of care among US patients with lung cancer.
METHODS
Data from a multiregional, multihealth system representative cohort of 4334 newly diagnosed patients were analyzed. Binomial logistic regression models adjusted for patient clustering.
RESULTS
Patients with any perceived unmet need (9% overall) included 7% of white–US-born (USB), 9% of white–foreign-born (FB), 13% of black-USB, 8% of Latino-USB, 24% of Latino-FB, 4% of Asian/Pacific Islander (API)-USB, 14% of API-FB, and 11% of “other” patients (P <.001). Even after controlling for demographic and socioeconomic factors, health system and health care access, and need, black-USB, Latino-FB, and Asian-FB patients were more likely to perceive an unmet need than white-USB patients by 5.1, 10.9, and 5.6 percentage points, respectively (all P<.05). Being younger, female, never married, uninsured, a current smoker, or under surrogate care or having comorbidity, anxiety/depression, or a cost/insurance barrier to getting tests/treatments were associated with any unmet need. Patients with any unmet need were more likely to rate care as less-than-“excellent” by 13 percentage points than patients with no unmet need (P<.001).
CONCLUSIONS
Significant disparities in unmet supportive service need by race/ethnicity and nativity highlight immigrants with lung cancer as being particularly underserved. Eliminating disparities in access to needed supportive services is essential for delivering patient-centered, equitable cancer care.
Keywords: lung cancer, patient-centered care, health care disparities, underserved populations, immigrants, supportive care
INTRODUCTION
Lung cancer is the leading cause of cancer mortality among women and men in the United States, causing >160,000 deaths in 2012 and representing an estimated 28% of all cancer deaths; this toll in mortality is more than breast, prostate, colon, and pancreatic cancer combined.1 Despite improvements in early detection and treatment, the majority of patients are diagnosed at an advanced stage of disease when treatment options are limited and the 1-year relative survival rate is 43% and the 5-year relative survival rate is 16%.1
Lung cancer is stressful for patients and their caregivers, stigmatizing and limiting patients’ social interaction and deterring them from seeking needed support.2,3 It is associated with greater distress4 and depression5 and a greater risk of death from suicide and cardiovascular deaths6 than other cancers. Psychosocial care is critical for those patients experiencing multiple sources of stress associated with the diagnosis, treatment, and psychosocial impact of the disease. Such care may be salient for underserved patients coping with additional socioeconomic and health care barriers and relevant for understanding social disparities in cancer care.7,8
Patients with lung cancer who are racial/ethnic minorities experience poorer survival9,10; are less likely to receive appropriate, timely treatment11–15 and hospice care16; and are more likely to hold misconceptions regarding treatment and hospice care17 than non-Hispanic whites. For example, black and Hispanic patients were reported to have lower 5-year relative survival rates (14.1% and 14.9%) than white patients (17.7%) between 2002 and 2006.10 The effects of nativity on care may be masked by aggregate racial/ethnic data.18 Immigrants experience worse access and a poorer quality of care than their US-born counterparts19; they are less likely to receive some cancer therapies and to rate their cancer care as “excellent” even after accounting for language and experiences of interpersonal care.7,8
As a vital component of supportive and palliative care, psychosocial support can ease suffering and improve experiences of care, quality of life, and survival.20–24 To address the often unmet psychosocial needs of patients, the Institute of Medicine boldly advanced a new standard of care urging the integrated delivery of needed psychosocial health services with routine oncology care.20 Providing information and resources to cope with emotions (eg, support groups) and manage illness and behavioral interventions (eg, smoking cessation) were emphasized as integral to holistic cancer care. Hospital cancer programs seeking accreditation must now adhere to recently revised standards of the American College of Surgeons Commission on Cancer promoting patient-centered care by requiring access to needed psychosocial and rehabilitation services.25
Psychosocial care is critical for patients with lung cancer experiencing a complex array of supportive care needs and a greater number of unmet needs than other patients with cancer.26–29 Needs may be unperceived (eg, if patients are unaware of services)30 or, even when perceived, remain unmet.31 Unmet needs can be defined as “differences between services judged necessary to deal appropriately with health problems and services actually received”32 and may be greater among socially disadvantaged groups.
To our knowledge, limited knowledge exists regarding the extent and impact of perceived unmet need for supportive services among US patients with lung cancer. Identifying underserved populations of patients with cancer is a research priority.20 Eliminating racial/ethnic disparities in unmet need for supportive services is also critical because racial/ethnic minorities are projected to shoulder a steeply increasing and unequal burden of incident lung cancer.33 To address gaps in knowledge and inform population-based efforts to equitably deliver patient-centered cancer care, we assessed the prevalence, determinants of, and disparities in perceived unmet needs for supportive services by race/ethnicity and nativity and how it is associated with the perceived quality of cancer care in a multiregional, multihealth system representative cohort of newly diagnosed US patients with lung cancer.
Conceptual Framework
Determining which inequalities/differences in care constitute a cancer inequity/disparity is essential34 but often debated, as policymakers, researchers, and clinical leaders strive to understand whether they are unnecessary, avoidable, unfair, or unjust. Charged with assessing racial/ethnic disparities in health care not attributable to known factors including access, the Institute of Medicine defined them as “not due to access-related factors or clinical needs, preferences, and appropriateness of intervention” while recognizing that access-related factors such as socioeconomic status (SES) often affect the quality of care and are correlated with race and ethnicity.35 Drawing on this definition to unpack racial/ethnic differences driven by nativity, we applied intersectional theory. It posits that multiple identities of social inequality (eg, race and class) are not experienced separately but simultaneously and interact on multiple levels of power and privilege with not just additive but multiplicative effects on health and access to social resources including health care.36 Jointly considering race/ethnicity and nativity as such can help to identify populations at risk of receiving a lower quality of care for lung cancer.18 Thus, we define a racial/ethnic-nativity disparity in perceived unmet need for supportive services as the unadjusted differences across groups defined by their race/ethnicity and nativity. In the context of studying a sick population with severe psychosocial needs, the unadjusted differences, which include differences attributed to access and additional health/clinical needs, reflect inequities. To identify determinants of unmet need for services, the Behavioral Model of Health Services Use provides a theoretical framework explaining service use as a function of contextual and individual-level predisposing characteristics (eg, demographics), enabling or impeding factors (eg, wealth, regular source of care), and perceived (eg, self-rated health) and evaluated (eg, stage of cancer) need for services.37
MATERIALS AND METHODS
Data Source and Study Population
We analyzed data from a geographically and racially diverse cohort of patients who were newly diagnosed with invasive lung cancer and participating in the Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium, a large population-based and health system-based study of cancer care sponsored by the National Cancer Institute (NCI). The study sample, population, recruitment, and data collection procedures are detailed elsewhere.38,39 Patients aged ≥ 21 years were contacted within 4 months of diagnosis between September 2003 and December 2005 in multiple regions (Alabama, Iowa, Los Angeles County, Northern California) and health systems (5 integrated health care delivery systems in the NCI-funded Cancer Research Network [CRN] and 15 Veterans Health Administration hospitals). Black, Latino, and Asian/Pacific Islander (API) patients were over-sampled to increase statistical power for studying racial/ethnic variations. Recruitment materials and surveys were translated into Spanish, Mandarin, and Cantonese, and experienced bilingual interviewers recruited and interviewed patients (or, for patients who were too ill to participate or those who had died, a surrogate [ie, a relative/household member familiar with their care]). The American Association for Public Opinion Research response rate was 49%,40 and the final cohort was representative of newly diagnosed patients in the United States.39 Information from medical records or cancer registries supplemented the survey data. Institutional Review Boards at each study site approved the study protocol. Patients or their surrogates provided informed consent to participate in the study. The analytic design of the current study was approved by the Institutional Review Boards of Harvard Medical School and the Harvard School of Public Health.
Measures
The following outcomes were assessed in this study: 1) perceived unmet need for supportive services (any vs none), defined as responding “yes” to at least 1 of 8 needed services: “Which of these practitioners or services do you believe you needed but did not receive?…“a. Have a nurse come to your home? b. Join a support group?; c. See a psychiatrist, psychologist, or mental health worker?; d. See a social worker?; e. See a physical or occupational therapist for rehabilitation?; f. See a pain management expert?; g. Talk with a pastoral counselor, such as a chaplain, minister, priest, or rabbi about your lung cancer?; h. Participate in a class or program to help you stop smoking?’; and 2) perceived quality of care (excellent vs less-than-excellent indicated by very good/good/fair/poor), assessed from “Overall, how would you rate the quality of your health care since your diagnosis of lung cancer?”
The main independent variable, race/ethnicity-nativity, (white–US-born [USB], white–foreign-born [FB], black-USB, Latino-USB, Latino-FB, API-USB, API-FB, and other) was defined from 3 items: 1) “Are you of Latino or Hispanic origin?”; 2) “Which of the following would you use to describe yourself? Would you describe yourself as Native Hawaiian, Other Pacific Islander, American Indian, Alaska Native, Asian, Black, African American, or White? Or more than 1 of these?”; and 3) “In what country were you born?” Small sample sizes limited disaggregating the “other” category (Native Americans [n =36], multiracial [n =119], and other/unknown [n =67]), disaggregating Asians and PI (n =17), and the heterogeneous API and Latino groups by ethnicity. Approximately two-thirds of Latino-USB (69%) and Latino-FB (65%) patients reported being of Mexican descent, whereas API-USB patients reported most commonly Japanese (50%) or Chinese (30%) ethnicity and API-FB patients reported most typically Chinese (47%) or Filipino (28%) ethnicity.
Analyses controlled for covariates theorized by the Behavioral Model and available in CanCORS data. Demographic factors included age, gender, marital status, and limited English proficiency (LEP), defined as responding in a non-English language or reporting speaking English “somewhat,” “a little,” or “not at all.” SES measures included education, annual household income, and wealth, a single measure of time able to sustain living at one’s current address and standard of living upon loss of all household income (<1 month, 1 month-2 months, 3 months-6 months, 7 months-12 months, and >1 year).
Health care access measures included continuity of any public/private health insurance coverage (assessed with detailed questions regarding the type of coverage from varied sources and any gaps in coverage within the last 12 months), having a primary doctor, and any cost-related/insurance-related barrier in receiving care (defined as reporting “yes” to “Were there any tests or treatments that your doctor recommended for you for lung cancer that you did not get because of problems with insurance coverage or because you were unable to pay for them?”).
We controlled for health maintenance organization (HMO) enrollment and study site, 2 contextual factors, to account for geographical/regional and health system differences. Perceived and evaluated need measures included self-rated health; surrogate respondent; collaborative stage of cancer at the time of diagnosis extracted from medical records or, if missing, from the cancer registry41; smoking status; any comorbidity (myocardial infarction, congestive heart failure, stroke, chronic lung disease, and diabetes); and anxiety/depression assessed using an item from the European Quality of Life-5 Dimensions.42 Analyses for perceived quality of care also controlled for perceived discrimination in cancer care, reporting “worse than” to the question “Would you say that you received medical care that was better than, about the same as, or worse than other patients with lung cancer?”
Statistical Analyses
Analyses were conducted with CanCORS core data (version 1.14) and full patient survey data (version 1.11) using Stata statistical software (version 11.0; StataCorp, College Station, Tex). After excluding patients who completed a brief survey that did not assess patient experiences of care, the final study cohort included 4334 patients. Item non-response was rare (range, 0.6% for perceived quality of care and 0.7% for perceived unmet need to 5% for stage of cancer at the time of diagnosis) except for wealth (32%), driven by surrogate responses. Bivariate comparisons were tested with the Pearson’s chi-square and Fisher’s exact tests.
Because not all patients may perceive a need and assuming that all patients who used services perceived a need for them, we computed the proportion of need in each racial/ethnic-nativity group that was “unmet”: number with any unmet service need/(number with any unmet service need + number using any service and with no unmet service need). We also examined the distribution of unmet need for each type of service among patients reporting any unmet need by race/ethnicity-nativity.
Analyses were conducted on a multiply-imputed data set created by the CanCORS Statistical Coordinating Center to address item nonresponse using sequential regression multiple imputation.43 Sequential regression multiple imputation accommodates complex missing data and iteratively imputes values when data are missing at random by specifying separate conditional models for each missing variable regressed on all observed and imputed variables.43
To estimate the unadjusted and adjusted effects of race/ethnicity-nativity with perceived unmet need, binomial logistic regression models were specified and parameters were estimated44 with cluster-correlated Huber-White sandwich/robust standard errors45 adjusting for patient clustering within 10 study sites (4 regional sites, 5 Cancer Research Network sites, VA; clusters ranged from 26 to 933 patients) before and after sequentially controlling for demographic and socioeconomic factors, health care access and health system, and need. We modeled: the log odds of any perceived unmet need for patient i in cluster j, ln(pij/1−pij) = β · Xij in which pij represents the patient’s probability of any perceived unmet need, Xij represents the patient’s vector of covariates, and β is a vector of regression coefficients representing the log odds of any unmet need for the covariates. Similarly, we estimated the adjusted effect of perceived unmet need on perceived quality of care while controlling for perceived discrimination in care. We found no evidence of a lack of fit using the Hosmer and Lemeshow (H-L) goodness-of-fit test and acceptable discrimination using the c-statistic for the full models of unmet need (H-L chi-square, 6.21; P =.62 [c-statistic, 0.75]) and quality of care (H-L chi-square, 7.14; P =.52; [c-statistic, 0.72]).
To help interpret results, using regression risk analysis,46 we computed the predictive margins (average model-adjusted predicted probabilities conditional on all observations being in a category) for each race/ethnicity-nativity group and the average marginal effects (difference in average model-adjusted predicted probability conditional on all observations being in a category and average predicted probability conditional on all observations being in the reference category) holding model covariates constant with standard errors calculated using the delta method. All significance tests were 2-sided with α=.05.
RESULTS
Table 1 shows sample characteristics by race/ethnicity-nativity and differences compared with white-USB patients. Black-USB and Latino-FB patients were more likely to report the lowest levels of education, income, and wealth. API-FB patients were younger and reported lower levels of income. Black-USB, Latino-FB, and API-FB patients were less likely to be continuously insured with a primary doctor. Latino-FB patients were more likely to report a cost/insurance barrier to getting care and not be enrolled in a HMO. Black-USB patients were less likely and white-FB patients were more likely to be diagnosed at an earlier stage of disease. White-FB, Latino, and API patients were less likely to have ever been smokers. Approximately one-half of all patients reported moderate/extreme anxiety/depression.
TABLE 1.
Characteristics of Newly Diagnosed US Patients With Lung Cancer in the Cancer Care Outcomes Research and Surveillance Consortium (%)
| All, n=4334 | White-USB, n=3034 | White-FB, n=132 | Black-USB, n=496 | Latino-USB, n=131 | Latino-FB, n=120 | API-USB, n=54 | API-FB, n=145 | |
|---|---|---|---|---|---|---|---|---|
| Male | 58 | 56 | 55 | 65a | 50a | 58 | 52 | 71a |
| Age, y <55 | 12 | 10 | 8b | 16 | 14 | 17 | 9 | 23a |
| 55–64 | 25 | 24 | 20 | 31 | 21 | 23 | 28 | 21 |
| 65–74 | 34 | 35 | 25 | 29 | 37 | 33 | 22 | 34 |
| >75 | 30 | 31 | 47 | 24 | 28 | 28 | 41 | 23 |
| LEP | 3 | 0 | 4 | 0 | 4 | 49a | 7a | 30a |
| Marital status: Married/cohabiting | 61 | 61 | 58 | 49 | 64 | 68 | 72 | 78a |
| Widowed/divorced/separated | 35 | 36 | 39 | 42 | 33 | 29 | 26 | 19 |
| Never married | 4 | 3 | 2 | 10 | 3 | 3 | 2 | 3 |
| Education: <High school | 23 | 19 | 14a | 35a | 42a | 58a | 9a | 26a |
| High school/GED | 60 | 64 | 54 | 54 | 52 | 30 | 63 | 39 |
| College graduate | 17 | 17 | 33 | 11 | 6 | 12 | 28 | 36 |
| Income: <$20,000 | 35 | 31 | 30 | 53a | 37 | 51a | 17c | 44b |
| $20,000–<$40,000 | 34 | 35 | 31 | 27 | 38 | 32 | 33 | 21 |
| $40,000–<$60,000 | 16 | 17 | 21 | 11 | 15 | 12 | 20 | 19 |
| ≥$60,000 | 15 | 16 | 18 | 9 | 11 | 6 | 30 | 15 |
| Wealth: <1 mo | 16 | 15 | 5c | 20a | 17 | 18b | 6b | 11 |
| 1–2 mo | 10 | 10 | 9 | 13 | 11 | 17 | 9 | 12 |
| 3–6 mo | 10 | 9 | 11 | 12 | 7 | 8 | 11 | 10 |
| 7–12 mo | 8 | 7 | 12 | 10 | 12 | 7 | 9 | 11 |
| >1 y | 25 | 27 | 25 | 16 | 21 | 12 | 33 | 21 |
| Missing data | 32 | 32 | 37 | 29 | 32 | 39 | 32 | 34 |
| Health insurance–primary doctor: Insured 12 mo, primary doctor | 87 | 89 | 93 | 78a | 88 | 70a | 93 | 77b |
| Uninsured | 2 | 2 | 3 | 4 | 5 | 5 | 0 | 2 |
| Enrolled in HMO | 24 | 24 | 37b | 22 | 24 | 12b | 52a | 19 |
| Cost/insurance barrier getting care | 2 | 2 | 2 | 2 | 3a | 8a | 2 | 3a |
| Study site: CRN | 15 | 16 | 21a | 11a | 5a | 0a | 33a | 5a |
| Northern California | 20 | 17 | 33 | 17 | 41 | 28 | 41 | 59 |
| Alabama | 13 | 12 | 2 | 34 | 0 | 0 | 0 | 1 |
| Los Angeles | 21 | 16 | 35 | 18 | 44 | 71 | 26 | 35 |
| Iowa | 22 | 29 | 5 | 2 | 4 | 0 | 0 | 0 |
| Veterans Affairs | 11 | 10 | 5 | 19 | 5 | 2 | 0 | 0 |
| Surrogate respondent | 43 | 42 | 52c | 42 | 47 | 63a | 46 | 59a |
| Comorbidity | 67 | 69 | 61 | 63b | 70 | 53a | 52a | 46a |
| AJCC cancer stage: I | 21 | 22 | 30c | 17b | 20 | 20 | 13 | 19 |
| II | 8 | 8 | 6 | 8 | 8 | 6 | 4 | 4 |
| III | 27 | 26 | 18 | 30 | 23 | 30 | 26 | 26 |
| IV | 39 | 39 | 36 | 38 | 45 | 38 | 54 | 46 |
| Unknown | 5 | 5 | 10 | 8 | 4 | 6 | 4 | 5 |
| Smoking status: Never | 9 | 6 | 16a | 7 | 12b | 39a | 24a | 36a |
| Current | 14 | 14 | 8 | 16 | 19 | 5 | 0 | 4 |
| Anxiety/depression | 49 | 48 | 47 | 52 | 53 | 56 | 50 | 46 |
Abbreviations: AJCC, American Joint Committee on Cancer; API, Asian/Pacific Islander; CRN, Cancer Research Network; FB, foreign-born; GED, General Educational Development; HMO, health maintenance organization; LEP, Limited English proficiency; USB, US-born. Income refers to annual household income. Wealth was assessed as time able to sustain living at one’s current address and standard of living upon loss of all household income.
P <.001.
P <.01.
P <.05; indicates a statistically significant difference compared with white US-born patients.
Prevalence of Perceived Unmet Need for Supportive Services by Race/Ethnicity-Nativity
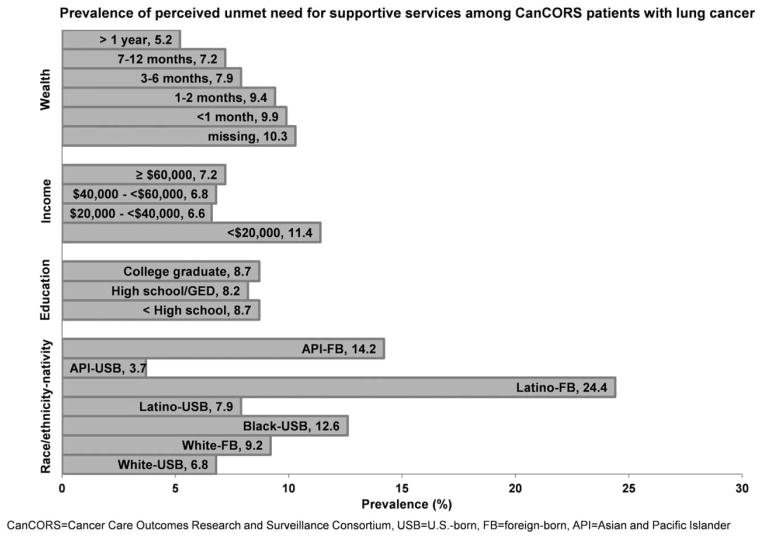
The prevalence of perceived unmet need for supportive services (Fig. 1) was 9% overall with significant disparities by race/ethnicity-nativity (9% of white-FB, 13% of black-USB, 8% of Latino-USB, 24% of Latino-FB, 4% of API-USB, 14% of API-FB, and 11% of “other” patients vs 7% of white-USB patients [P <.001]). Differences by nativity were striking, particularly among Latino and API patients, with immigrants having at least a 3-fold higher prevalence than their USB counterparts. Racial/ethnic disparities were greater among immigrants than among USB patients. The proportion of need that was “unmet” for API-USB, white-FB, Latino-USB, black-USB, API-FB, and Latino-FB patients was 0.06, 0.12, 0.12, 0.17, 0.29, and 0.33, respectively (vs 0.10 for white-USB patients). Significant differences also existed by income and wealth with the prevalence greatest among those with the lowest incomes and wealth.
Figure 1.
Prevalence (shown as percent) of perceived unmet need for supportive services among US patients with lung cancer in the Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium is shown by race/ethnicity-nativity and socioeconomic status. Supportive services studied included home nurse, support group, psychological services, social worker, physical/occupational rehabilitation, pain management, spiritual counseling, and smoking cessation. Income refers to annual household income. Wealth was assessed as time able to sustain living at one’s current address and standard of living upon loss of all household income. Differences across categories are statistically significant at P <.001 for all variables except education. GED indicates General Educational Development.
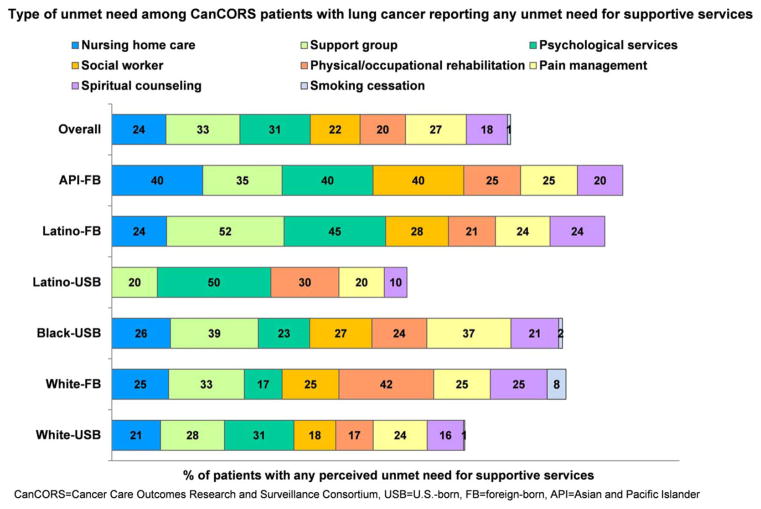
The 3 most commonly cited needs among those with any unmet need (Fig. 2) were for support groups (33%), psychological services (31%), and pain management (27%). Compared with white-USB patients, black-USB, white-FB, Latino-FB, and API-FB patients were more likely to cite unmet need for support groups. Latino-FB and API-FB patients were also more likely to report unmet need for psychological services and more unmet needs (median of 2 unmet needs vs 1 unmet need) than white-USB patients. Support groups and psychological services were among the least used services (4% and 8%, respectively) overall and within all groups (results not shown).
Figure 2.
Type of need for US patients with lung cancer perceiving any unmet need for supportive services in the Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium is shown by race/ethnicity-nativity. Percentages do not add to 100% because patients could report multiple unmet service needs. Results for Asian/Pacific Islander–US-born (API-USB) patients are not reported due to small samples (< 10 patients) in these categories.
Adjusted Probability of Perceived Unmet Need for Supportive Services by Race/Ethnicity-Nativity
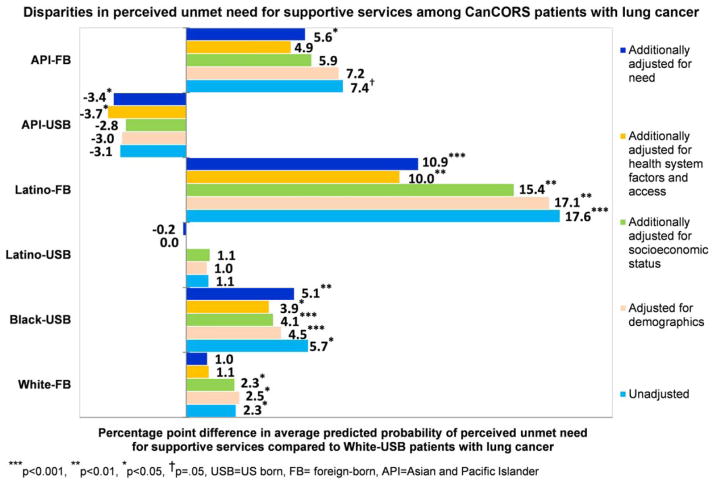
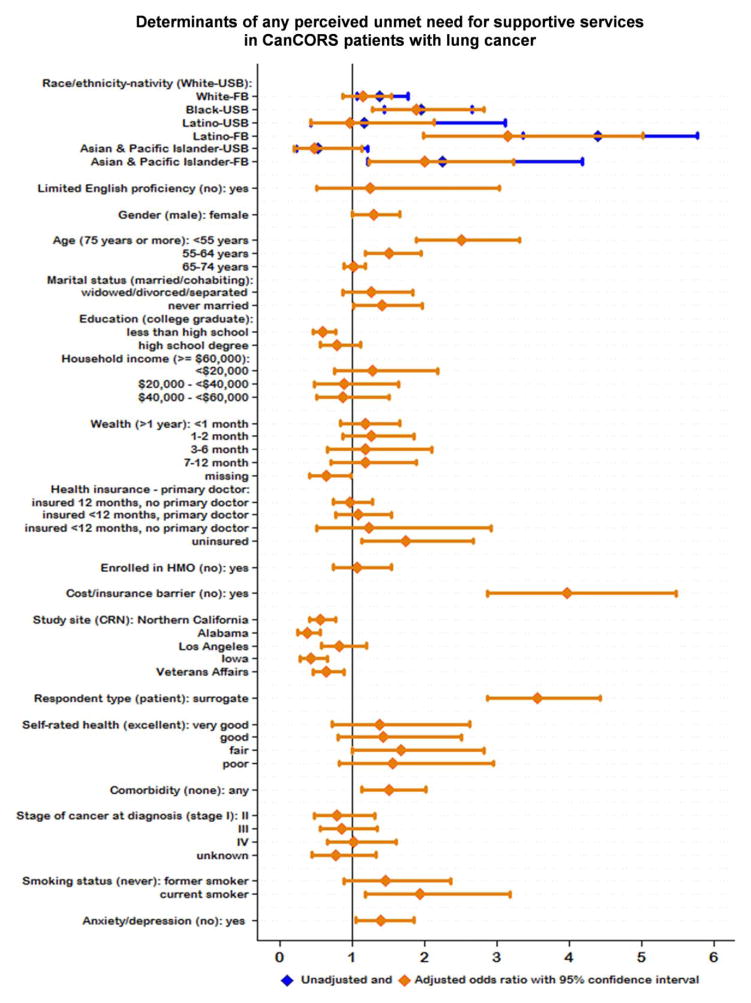
The unadjusted probability of perceived unmet need for white-FB, black-USB, Latino-FB, and API-FB patients was 2.5, 5.7, 17.6, and 7.4 percentage points higher, respectively, than for white-USB patients (all P <.05) (Fig. 3). Controlling for demographic and socioeconomic factors resulted in modest attenuations of the marginal effects whereas health system and health care access resulted in the greatest reductions, particularly for Latino-FB patients. Further controlling for health need increased disparities with the probability of any unmet need for black-USB, Latino-FB, and API-FB patients being 5.1, 10.9, and 5.6 percentage points higher, respectively, than for white-USB patients (all P <.05). Patients who were younger, female, never married, uninsured, had a cost/insurance barrier in getting care, or health needs (being a current smoker, under surrogate care, having comorbidity or anxiety/depression) had significantly greater odds whereas patients in Northern California, Alabama, and Iowa and the Veterans Health Administration and with less than a high school education had significantly lower odds of reporting any unmet need (Fig. 4). Detailed results for the regression models are shown in Table 2.
Figure 3.
Difference in the model-adjusted average predicted probabilities of any perceived unmet need for supportive services for patients in each racial/ethnic-nativity group and white–US-born (USB) patients with lung cancer in the Cancer Care Outcomes Research and Surveillance Consortium is shown. The difference was calculated using average marginal effects or risk differences from logistic regression models with robust standard errors adjusted for patient clustering and holding model covariates constant. For example, on average, a Latino–foreign-born (FB) patient’s probability of having any perceived unmet need is 10.9 percentage points higher than for an otherwise similar white-USB patient holding constant demographics, socioeconomic status, health care access and health system, and need. Supportive services studied included home nurse, support group, psychological services, social worker, physical/occupational rehabilitation, pain management, spiritual counseling, and smoking cessation.
Figure 4.
Odds ratios with 95% confidence intervals are shown for factors associated with perceived unmet need for supportive services among US patients with lung cancer in the Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium. Supportive services studied included home nurse, support group, psychological services, social worker, physical/occupational rehabilitation, pain management, spiritual counseling, and smoking cessation. Reference categories are shown in parentheses. Reference category for health insurance-primary doctor was insured for 12 months with a primary doctor. USB indicates US-born; FB, foreign-born; HMO, health maintenance organization; CRN, Cancer Research Network.
TABLE 2.
Association of Race/Ethnicity-Nativity With Perceived Unmet Need for Supportive Services Among Patients With Lung Cancer in the Cancer Care Outcomes Research and Surveillance Consortium
| %, Unmet need | Unadjusted
|
Model 1
|
Model 2
|
Model 3
|
Model 4
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Race-nativity: White-USBa | 7 | ||||||||||
| White-FB | 9 | 1.38b | (1.07–1.78) | 1.40c | (1.09–1.82) | 1.37b | (1.03–1.80) | 1.17 | (0.89–1.54) | 1.16 | (0.88–1.54) |
| Black-USB | 13 | 1.96d | (1.45–2.66) | 1.74d | (1.31–2.30) | 1.67c | (1.25–2.24) | 1.64b | (1.08–2.49) | 1.90c | (1.28–2.82) |
| Latino-USB | 8 | 1.17 | (0.44–3.12) | 1.15 | (0.44–3.00) | 1.18 | (0.45–3.05) | 1.00 | (0.46–2.17) | 0.97 | (0.44–2.14) |
| Latino-FB | 24 | 4.40d | (3.36–5.78) | 4.32d | (2.24–8.34) | 3.97d | (2.17–7.27) | 2.81d | (1.72–4.60) | 3.16d | (1.99–5.02) |
| API-USB | 4 | 0.53 | (0.23–1.22) | 0.54 | (0.22–1.33) | 0.57 | (0.24–1.37) | 0.46 | (0.17–1.24) | 0.48 | (0.21–1.14) |
| API-FB | 14 | 2.26c | (1.22–4.18) | 2.22b | (1.15–4.31) | 1.99 | (1.00–3.97) | 1.82b | (1.01–3.29) | 2.00c | (1.24–3.23) |
| Limited English proficiency: Noa | 8 | ||||||||||
| Yes | 18 | 2.44b | (1.17–5.08) | 1.02 | (0.32–3.26) | 1.07 | (0.32–3.60) | 1.15 | (0.37–3.55) | 1.25 | (0.52–3.04) |
| Gender: Malea | 8 | ||||||||||
| Female | 9 | 1.17 | (0.95–1.45) | 1.10 | (0.86–1.40) | 1.16 | (0.91–1.49) | 1.12 | (0.87–1.43) | 1.30b | (1.01–1.67) |
| Age: >75 ya | 7 | ||||||||||
| <55 y | 15 | 2.41d | (1.87–3.12) | 2.22d | (1.70–2.90) | 2.45d | (1.80–3.33) | 2.18d | (1.69–2.80) | 2.51d | (1.90–3.32) |
| 55–64 y | 9 | 1.39c | (1.10–1.75) | 1.38b | (1.06–1.80) | 1.51b | (1.08–2.12) | 1.44b | (1.06–1.96) | 1.52c | (1.18–1.95) |
| 65–74 y | 7 | 0.96 | (0.81–1.14) | 0.97 | (0.83–1.13) | 1.03 | (0.87–1.21) | 1.01 | (0.86–1.20) | 1.03 | (0.90–1.18) |
| Marital status: Married/cohabitinga | 7 | ||||||||||
| Widowed, divorced, separated | 10 | 1.38 | (0.99–1.93) | 1.45b | (1.07–1.97) | 1.19 | (0.82–1.74) | 1.18 | (0.81–1.72) | 1.27 | (0.87–1.84) |
| Never married | 14 | 2.06c | (1.34–3.19) | 1.56b | (1.09–2.24) | 1.25 | (0.85–1.82) | 1.28 | (0.88–1.87) | 1.42b | (1.02–1.98) |
| Education: College graduatea | 9 | ||||||||||
| < High school | 9 | 0.99 | (0.74–1.33) | 0.65d | (0.51–0.83) | 0.72c | (0.56–0.91) | 0.60d | (0.46–0.78) | ||
| High school/GED | 8 | 0.93 | (0.76–1.15) | 0.81 | (0.64–1.03) | 0.85 | (0.63–1.13) | 0.80 | (0.57–1.12) | ||
| Income: ≥ $60,000a | 7 | ||||||||||
| < $20,000 | 12 | 1.67b | (1.02–2.72) | 1.63 | (0.93–2.87) | 1.67 | (0.93–2.98) | 1.28 | (0.76–2.18) | ||
| $20,000–$40,000 | 7 | 0.93 | (0.51–1.69) | 1.05 | (0.56–1.99) | 1.07 | (0.57–1.99) | 0.89 | (0.48–1.64) | ||
| $40,000–$59,000 | 7 | 0.94 | (0.53–1.67) | 1.00 | (0.58–1.73) | 0.99 | (0.58–1.70) | 0.88 | (0.51–1.51) | ||
| Wealth: >1 ya | 5 | ||||||||||
| < 1 mo | 10 | 1.97d | (1.39–2.81) | 1.38 | (0.96–1.98) | 1.32 | (0.94–1.86) | 1.18 | (0.84–1.66) | ||
| 1–2 mo | 9 | 1.88c | (1.25–2.82) | 1.36 | (0.93–2.01) | 1.36 | (0.95–1.95) | 1.27 | (0.87–1.86) | ||
| 3–6 mo | 8 | 1.55 | (0.88–2.72) | 1.23 | (0.71–2.11) | 1.21 | (0.72–2.04) | 1.18 | (0.66–2.11) | ||
| 7–12 mo | 7 | 1.41 | (0.88–2.25) | 1.20 | (0.74–1.93) | 1.13 | (0.72–1.78) | 1.18 | (0.72–1.90) | ||
| Missing | 11 | 2.13d | (1.42–3.20) | 1.95d | (1.36–2.80) | 1.90d | (1.39–2.59) | 0.64b | (0.42–0.99) | ||
| Health insurance - primary doctor: Insured 12 mo, primary doctora | 8 | ||||||||||
| Insured 12 mo, no primary doctor | 9 | 1.19 | (0.83–1.70) | 0.91 | (0.67–1.23) | 0.98 | (0.74–1.29) | ||||
| Insured <12 mo, primary doctor | 14 | 1.99d | (1.69–2.33) | 1.12 | (0.85–1.48) | 1.09 | (0.77–1.54) | ||||
| Insured <12 mo, no primary doctor | 18 | 2.59d | (1.70–3.94) | 1.23 | (0.60–2.54) | 1.23 | (0.52–2.93) | ||||
| Uninsured | 21 | 3.20d | (1.85–5.54) | 1.78b | (1.05–3.02) | 1.75c | (1.14–2.68) | ||||
| Enrolled in HMO: Noa | 8 | ||||||||||
| Yes | 10 | 1.19 | (0.76–1.87) | 1.15 | (0.77–1.71) | 1.08 | (0.75–1.55) | ||||
| Cost/insurance barrier getting care: Noa | 8 | ||||||||||
| Yes | 35 | 6.22d | (4.79–8.09) | 4.44d | (3.31–5.97) | 3.97d | (2.87–5.48) | ||||
| Study site: CRNa | 10 | ||||||||||
| Northern California | 8 | 0.76 | (0.55–1.05) | 0.65c | (0.48–0.88) | 0.57d | (0.42–0.77) | ||||
| Alabama | 7 | 0.62c | (0.45–0.86) | 0.52b | (0.32–0.86) | 0.38d | (0.25–0.57) | ||||
| Los Angeles | 12 | 1.19 | (0.86–1.66) | 0.99 | (0.67–1.46) | 0.83 | (0.58–1.20) | ||||
| Iowa | 5 | 0.47d | (0.34–.66) | 0.50c | (0.31–0.80) | 0.43d | (0.28–0.66) | ||||
| Veterans Affairs | 9 | 0.82 | (0.59–1.14) | 0.78 | (0.54–1.15) | 0.65b | (0.47–0.90) | ||||
| Surrogate completed survey: Noa | 6 | ||||||||||
| Yes | 12 | 2.23d | (1.64–3.01) | 3.57d | (2.88–4.43) | ||||||
| Self-rated health: Excellenta | 5 | ||||||||||
| Very good | 7 | 1.39 | (0.76–2.55) | 1.39 | (0.73–2.63) | ||||||
| Good | 8 | 1.73b | (1.01–2.95) | 1.43 | (0.81–2.52) | ||||||
| Fair | 11 | 2.32c | (1.33–4.05) | 1.68 | (1.00–2.82) | ||||||
| Poor | 11 | 2.50c | (1.32–4.72) | 1.57 | (0.83–2.95) | ||||||
| Comorbid conditions: Nonea | 7 | ||||||||||
| One or more | 9 | 1.40b | (1.04–1.87) | 1.52c | (1.14–2.03) | ||||||
| AJCC cancer stage at diagnosis: Ia | 7 | ||||||||||
| II | 6 | 0.91 | (0.61–1.36) | 0.79 | (0.48–1.32) | ||||||
| III | 8 | 1.16 | (0.87–1.54) | 0.86 | (0.56–1.35) | ||||||
| IV | 10 | 1.57c | (1.11–2.20) | 1.03 | (0.66–1.62) | ||||||
| Unknown | 9 | 1.26 | (0.79–2.02) | 0.78 | (0.45–1.34) | ||||||
| Smoking status: Nevera | 8 | ||||||||||
| Former | 8 | 0.97 | (0.55–1.72) | 1.46 | (0.90–2.36) | ||||||
| Current | 12 | 1.57 | (0.99–2.50) | 1.94c | (1.18–3.18) | ||||||
| Anxiety/depression: Nonea | 6 | ||||||||||
| Moderate/extreme | 11 | 1.91d | (1.53–2.39) | 1.40b | (1.05–1.86) | ||||||
| No. | 4334 | 4302 | 4302 | 4301 | 4301 | ||||||
| Log likelihood | −1200.00 | −1182.00 | −1148.00 | −1099.00 | |||||||
| Akaike information criterion, | 2418.00 | 2382.90 | 2313.11 | 2215.47 | |||||||
| Bayesian information criterion | 2475.37 | 2440.20 | 2370.41 | 2272.76 | |||||||
Abbreviations: 95% CI, 95% confidence interval; AJCC, American Joint Committee on Cancer; API, Asian/Pacific Islander; CRN, Cancer Research Network; GED, General Educational Development; FB, foreign-born; HMO, Health Maintenance Organization; OR, odds ratio; USB, US-born.
Note: Perceived unmet need (any vs none) was assessed for 8 supportive services (home nurse, support group, psychological services, social worker, physical/occupational rehabilitation, pain management, spiritual counseling, and smoking cessation). Income refers to annual household income. Wealth was assessed as time able to sustain living at one’s current address and standard of living upon loss of all household income. Comorbid conditions included congestive heart failure, myocardial infarction, stroke, chronic lung disease, and diabetes. Binomial logistic regression models with robust standard errors adjusted for patient clustering and controlled for demographic characteristics (model 1), and additionally for socioeconomic status (model 2), health system and health care access (model 3), and need (model 4) were used.
Reference group.
P <.05.
P <.01.
P <.001.
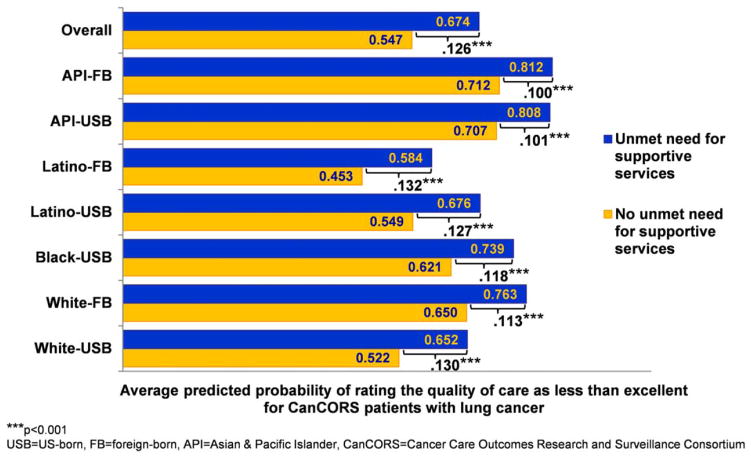
Adjusted Probability of Perceiving Less-Than-Excellent Quality of Care
The predicted probability of perceiving less-than-excellent care for patients with any unmet service need was 12.6 percentage points (95% confidence interval, 7.4 percentage points-17.8 percentage points) higher than otherwise similar counterparts with no unmet need, and at least 10 percentage points higher for all groups (all P <.05; ranging from 10.0 percentage points for API-FB patients to 13.2 percentage points for Latino-FB patients) (Fig. 5). Detailed results for the regression models are shown in Table 3.
Figure 5.
Model-adjusted average predicted probability of perceiving less-than-excellent quality of care is shown for patients with lung cancer in the Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium with and without any unmet need for supportive services. The probability was computed using predictive margins from a logistic regression model with robust standard errors adjusted for patient clustering and holding constant model covariates (demographic factors, socioeconomic status, health care access and health system, need, and perceived discrimination in care). Supportive services studied included home nurse, support group, psychological services, social worker, physical/occupational rehabilitation, pain management, spiritual counseling, and smoking cessation.
TABLE 3.
Marginal Effects on Perceiving the Quality of Care as Less Than Excellent Among Patients With Lung Cancer in the Cancer Care Outcomes Research and Surveillance Consortium
| Unadjusted
|
Model 1, Adjusted
|
Model 2, Adjusted
|
||||
|---|---|---|---|---|---|---|
| OR(95% CI) | Marginal Effect(95% CI) | OR(95% CI) | AME(95% CI) | OR(95% CI) | AME(95% CI) | |
| Race/ethnicity-nativity: white-USBa | ||||||
| White-FB | 1.90b (1.45–2.49) | 0.153b (0.092–0.214) | 1.82b (1.39–2.39) | 0.126b (0.071–0.181) | 1.83b (1.39–2.41) | 0.126b (0.071–0.182) |
| Black-USB | 1.61b (1.38–1.88) | 0.116b (0.078–0.153) | 1.63b (1.42–1.86) | 0.103b (0.075–0.132) | 1.59b (1.37–1.84) | 0.097b (0.066–0.129) |
| Latino-USB | 1.27d (1.06–1.53) | 0.059d (0.014–0.105) | 1.11 (0.90–1.37) | 0.023 (−0.021–0.068) | 1.13 (0.90–1.42) | 0.026 (−0.022–0.074) |
| Latino-FB | 1.49c (1.17–1.91) | 0.098c (0.039–0.157) | 0.79 (0.39–1.61) | −0.051 (−0.203–0.101) | 0.72 (0.36–1.46) | −0.069 (−0.217–0.078) |
| API-USB | 2.20c (1.35–3.61) | 0.185b (0.081–0.289) | 2.42b (1.47–3.99) | 0.180b (0.087–0.274) | 2.45b (1.51–3.99) | 0.182b (0.091–0.273) |
| API-FB | 3.06b (2.15–4.37) | 0.249b (0.185–0.313) | 2.60b (1.93–3.49) | 0.193b (0.140–0.247) | 2.53b (1.89–3.38) | 0.187b (0.135–0.240) |
| Unmet need for supportive services: Nonea | ||||||
| One or more | 2.93b (2.38–3.60) | 0.236b (0.198–0.274) | 1.85b (1.42–2.40) | 0.126b (0.074–0.178) | ||
|
| ||||||
| N | 4,299 | 4,297 | ||||
| Log likelihood | −2604.96 | −2594.24 | ||||
| Akaike information criterion | 5227.92 | 5206.49 | ||||
| Bayesian information criterion | 5285.21 | 5263.78 | ||||
Abbreviations: 95% CI, 95% confidence interval; AME, average marginal effect; API, Asian/Pacific Islander; FB, foreign-born; OR, odds ratio; USB, US-born.
Note: Perceived unmet need was assessed for 8 supportive services (home nurse, support group, psychological services, social worker, physical/occupational rehabilitation, pain management, spiritual counseling, and smoking cessation).
Binomial logistic regression models with robust standard errors adjusted for patient clustering were used.
Model 1 was adjusted for individual demographic characteristics (age, gender, limited English proficiency, and marital status), socioeconomic status (education, income, and wealth), health care access and health system (continuity of health insurance coverage, primary doctor, health maintenance organization enrollment, cost/insurance barrier in obtaining tests/treatment, and study site), need (stage of cancer at diagnosis, self-rated health, comorbid health conditions, anxiety/depression, smoking status, and surrogate respondent), and perceived discrimination in care. Model 2 was in addition adjusted for any perceived unmet need for supportive services.
Reference group.
P <.001.
P <.01.
P <.05.
Sensitivity Analyses
To assess the robustness of results, we performed several sensitivity analyses. First, because surrogate respondents were more likely to report perceived unmet need than self-reporting patients (12% vs 6%; P <.001) and their perceptions may differ from those of patients, we ran models separately adjusting for the surrogate’s relationship (spouse/partner, child, other family, or nonfamily) and frequency of telephone/in-person contact (daily or less than daily) with the patient as well as models stratified by respondent type (patient or surrogate). Controlling for the surrogate’s relationship (95% were family members) and contact (91% reported daily contact), results concerning disparities in unmet need were mostly unchanged. In stratified analyses, disparities persisted for black-USB patients among self-reporting patients and for Latino-FB and API-FB patients among surrogate respondents. Patients with unmet needs remained significantly more likely to rate care as less-than-excellent than otherwise similar counterparts with no unmet need among self-reporting patients and surrogate respondents by 18.3 and 9.1 percentage points, respectively. Second, models including language spoken at home (English vs non-English) and length of stay in the United States (<15 years and ≥15 years vs USB) as proxy measures of acculturation did not substantially alter results. The former was non-significant. The 2 categories of length of stay for immigrants, although significant, did not differ significantly from each other (Wald chi-square, 1.07; P =.30).
DISCUSSION
In a socially and geographically diverse cohort representative of newly diagnosed US patients with lung cancer, approximately 1 in 10 patients reported an unmet need for at least 1 of 8 key supportive services. Significant inequities in access to needed services were found by race/ethnicity-nativity status, signifying inequitable quality of care, between API-FB, black-USB, Latino-FB, white-FB, and white-USB patients. Marked disparities persisted for black-USB, Latino-FB, and API-FB patients even after controlling for demographic and socioeconomic factors, health care access and health system, and need. Unmet need for services had a significant bearing on the perceived quality of care, irrespective of race/ethnicity and nativity, and warrants further study on other patient-reported outcomes (eg, health-related quality of life) and survival. To our knowledge, the current study is the first to describe the prevalence, determinants, and disparities in perceived unmet need for supportive services and how it affects perceived quality of care among US patients with lung cancer.
The findings of the current study underscore the importance of considering nativity jointly with race/ethnicity and, when possible, disaggregating racial/ethnic data by nativity to identify social disparities in cancer care, and subgroups of patients at risk of receiving poor care.18 Nativity status was found to be an important marker of disparities within racial/ethnic groups including white patients. Nativity also highlighted immigrants as a subpopulation among whom racial/ethnic disparities were greater than for USB patients and who were particularly underserved, with approximately 33% of assessed need unmet among Latino-FB and API-FB patients (vs approximately 10% for white-USB and white-FB patients).
Factors underlying differences in unmet need for services varied for different groups and may require different strategies to eliminate disparities. Demographic factors (age, gender, and marital status) were significantly associated with unmet need and accounted for the greatest reduction in the disparity between white-USB and black patients. SES was not found to be significantly associated in adjusted analyses except for education and accounted for modest reductions in observed disparities, mostly for Latino-FB and API-FB patients. Health system and health care access factors accounted for the greatest reduction in the disparity between white-USB and Latino-FB patients, who were most likely to report access barriers. Health-related needs were found to be significantly associated and increased disparities between white-USB patients and Latino-FB, API-FB, and, to a greater extent, black-USB patients, suggesting that the needs of sicker patients may go unmet.
The persistence of disparities affecting black-USB, Latino-FB, and API-FB patients after controlling for LEP, access, and factors that induce disparities is troubling and warrants studying other contextual and institutional factors including service availability. LEP was not found to be associated with unmet need and may reflect the influences of long-term immigrant status (> 80% of FB patients lived in the United States at least 15 years) or geography mitigating language barriers in access. Greater than 90% of study patients with LEP resided in California, which has comprehensive policies in place to serve patients with LEP.47 Data limitations prevented the examination of recent immigrant status with a length of stay of <10 years (n =45 with <10 cases of unmet need) and other aspects of acculturation. These areas need further study in larger samples of Latino, API, and FB patients that enable examining jointly ethnicity and immigration-related and cultural factors including patient and provider attitudes and behaviors toward supportive services (eg, stigma toward using services, providers not facilitating access).
The results of the current study highlight current smokers and patients under the care of surrogates as underserved groups deserving more attention in research and practice. Patients experience substantial social stigma irrespective of their smoking status,2 but current smokers may be particularly underserved. Continued smoking after diagnosis is associated with low social support.48 Smokers may be prone to guilt, self-blame, and denial of their disease; they may hold nihilistic beliefs, experience therapeutic nihilism, and perceive unfair treatment and dissatisfaction with care.3
Surrogates experience a substantial negative toll from medical decision-making.49 We found that patients under surrogate care were also likely to have unmet needs and be immigrants. Latino-FB and API-FB patients with cancer value and rely on family support and caregivers for medical decision-making but also, not wanting to be a burden, have significant informational, psychosocial, and social support needs and desire external support such as support groups.50,51 Nonspouse proxies of surveys also tend to rate care lower but with smaller effects on reports of care (eg, getting needed care).52 The findings of the current study were robust after accounting for the surrogate’s relationship and contact with the patient but assessing to what extent proxy response bias versus greater needs drove the observed results deserves further study.
Improvements in screening, treatment, and survival1,53 and a projected rise in the burden of incident lung cancer on racial/ethnic minorities, particularly Latinos and Asians,33 necessitate systematically monitoring and eliminating disparities in unmet need for supportive services. The current study has important implications for improving the equitable delivery of needed services through financing and care coordination. Inadequate assessment of psychosocial needs and perverse reimbursement policies that pay providers to “give treatments and not hold hands” are major impediments in current cancer care.22 Policies and interventions encouraging systematic assessment at the time of diagnosis and follow-up and reformed reimbursement for supportive services are needed to help ensure that needed services are delivered equitably and in a linguistically and culturally appropriate manner, particularly in community settings serving underserved populations. Although multidisciplinary care teams are essential for the integrated delivery of psychosocial care, patient navigation shows potential as a cost-effective strategy to reduce cancer care disparities.54 It is required for hospital cancer programs to be accredited by the American College of Surgeons to address barriers and disparities in care.25 In a fragmented health care system, patients value lay navigators to provide emotional support and assistance in coordinating cancer care and reduce unmet needs.22,55 Consistent with a recent study demonstrating substantial underuse of psychosocial care among cancer survivors,56 the findings of the current study also support improving access to support groups and psychological services, particularly for racial/ethnic minorities and immigrants.
The findings of the current study should be interpreted in light of some important limitations. First, the 8 services studied, although broad, may have missed specific concerns (eg, financial or transportation needs) and may have resulted in underestimates of unmet service need. Second, we studied unmet need in the initial months after diagnosis, which may not represent subsequent needs. Third, although we studied a large representative cohort and controlled for geographical differences, these findings may have limited generalizability to FB patients in the South and Midwest, who were not well represented in the current study cohort. Fourth, selection bias is likely because some FB subpopulations likely to have LEP (eg, Vietnamese Americans) may have been unable to participate in their preferred language. Fifth, response bias (eg, proxy respondent bias) may have affected the information collected.
In conclusion, the results of the current study demonstrate significant disparities in perceived unmet need for supportive services by race/ethnicity-nativity, which persisted for black-USB, Latino-FB, and API-FB patients after adjusting for varied factors, and highlighted immigrants as being particularly underserved. The most common unmet needs were related to access to support groups and psychological services. Unmet need for supportive services was associated with perceiving less-than-excellent quality of care. Eliminating disparities by race/ethnicity and nativity in access to needed supportive services is essential for delivering high-quality cancer care that is patient-centered and equitable.
Acknowledgments
We are grateful to study participants in the Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium for their responses.
FUNDING SUPPORT
Supported by the Kellogg Health Scholar Program funded by the W.K. Kellogg Foundation, grant P50CA148596 funded by the National Cancer Institute (NCI), and a pilot grant from the Lung Cancer Disparities Center at Harvard University. The Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium was supported by grants from the NCI to the Statistical Coordinating Center (Dana-Farber Cancer Institute [U01CA093344]) and the NCI-supported Primary Data Collection and Research Centers (Harvard Medical School/Northern California Cancer Center [U01CA093324], Dana-Farber Cancer Institute/Cancer Research Network [U01CA093332], RAND/University of California at Los Angeles [U01CA093348], University of Alabama at Birmingham [U01CA093329], University of Iowa [U01CA093339], and University of North Carolina [U01CA093326]) and by a Department of Veterans Affairs grant to the Durham VA Medical Center (CRS 02-164). These sources of support had no role in the conception and design of the current study, analysis or decision to publish.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures apart from the funding sources.
References
- 1.American Cancer Society. Cancer Facts & Figures 2012. Atlanta, GA: American Cancer Society; 2012. [Google Scholar]
- 2.Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. BMJ. 2004;328:1470. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chambers SK, Jeffrey D, Occhipinti S, et al. A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer. 2012;12:184. doi: 10.1186/1471-2407-12-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 5.Carlsen K, Jensen AB, Jacobsen E, Krasnik M, Johansen C. Psychosocial aspects of lung cancer. Lung Cancer. 2005;47:293–300. doi: 10.1016/j.lungcan.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Fang F, Fall K, Mittleman MA, et al. Suicide and cardiovascular death after a cancer diagnosis. N Engl J Med. 2012;366:1310–1318. doi: 10.1056/NEJMoa1110307. [DOI] [PubMed] [Google Scholar]
- 7.Ayanian JZ, Zaslavsky AM, Arora NK, et al. Patients’ experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2010;28:4154–4161. doi: 10.1200/JCO.2009.27.3268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nielsen SS, He Y, Ayanian JZ, et al. Quality of cancer care among foreign-born and US-born patients with lung or colorectal cancer. Cancer. 2010;116:5497–5506. doi: 10.1002/cncr.25546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hardy D, Xia R, Liu CC, Cormier JN, Nurgalieva Z, Du XL. Racial disparities and survival for nonsmall-cell lung cancer in a large cohort of black and white elderly patients. Cancer. 2009;115:4807–4818. doi: 10.1002/cncr.24521. [DOI] [PubMed] [Google Scholar]
- 10.Pulte D, Redaniel MT, Brenner H, Jeffreys M. Changes in survival by ethnicity of patients with cancer between 1992–1996 and 2002–2006: is the discrepancy decreasing? Ann Oncol. 2012;23:2428–2434. doi: 10.1093/annonc/mds023. [DOI] [PubMed] [Google Scholar]
- 11.Bach PB, Cramer LD, Warren JL, Begg CB. Racial differences in the treatment of early-stage lung cancer. N Engl J Med. 1999;341:1198–1205. doi: 10.1056/NEJM199910143411606. [DOI] [PubMed] [Google Scholar]
- 12.Earle CC, Venditti LN, Neumann PJ, et al. Who gets chemotherapy for metastatic lung cancer? Chest. 2000;117:1239–1246. doi: 10.1378/chest.117.5.1239. [DOI] [PubMed] [Google Scholar]
- 13.Lathan CS, Neville BA, Earle CC. The effect of race on invasive staging and surgery in non-small-cell lung cancer. J Clin Oncol. 2006;24:413–418. doi: 10.1200/JCO.2005.02.1758. [DOI] [PubMed] [Google Scholar]
- 14.Shugarman LR, Mack K, Sorbero ME, et al. Race and sex differences in the receipt of timely and appropriate lung cancer treatment. Med Care. 2009;47:774–781. doi: 10.1097/MLR.0b013e3181a393fe. [DOI] [PubMed] [Google Scholar]
- 15.Park ER, Japuntich SJ, Traeger L, Cannon S, Pajolek H. Disparities between blacks and whites in tobacco and lung cancer treatment. Oncologist. 2011;16:1428–1434. doi: 10.1634/theoncologist.2011-0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hardy D, Chan W, Liu CC, et al. Racial disparities in the use of hospice services according to geographic residence and socioeconomic status in an elderly cohort with nonsmall cell lung cancer. Cancer. 2011;117:1506–1515. doi: 10.1002/cncr.25669. [DOI] [PubMed] [Google Scholar]
- 17.Jonnalagadda S, Lin JJ, Nelson JE, et al. Racial and ethnic differences in beliefs about lung cancer care. Chest. 2012;142:1251–1258. doi: 10.1378/chest.12-0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams DR, Kontos EZ, Viswanath K, et al. Integrating multiple social statuses in health disparities research: the case of lung cancer. Health Serv Res. 2012;47(3 pt 2):1255–1277. doi: 10.1111/j.1475-6773.2012.01404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Derose KP, Bahney BW, Lurie N, Escarce JJ. Review: immigrants and health care access, quality, and cost. Med Care Res Rev. 2009;66:355–408. doi: 10.1177/1077558708330425. [DOI] [PubMed] [Google Scholar]
- 20.Adler NE, Page A, editors. Institute of Medicine. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 21.Surbone A, Baider L, Weitzman TS, et al. MASCC Psychosocial Study Group. Psychosocial care for patients and their families is integral to supportive care in cancer: MASCC position statement. Support Care Cancer. 2010;18:255–263. doi: 10.1007/s00520-009-0693-4. [DOI] [PubMed] [Google Scholar]
- 22.Wagner EH, Aiello Bowles EJ, Greene SM, et al. The quality of cancer patient experience: perspectives of patients, family members, providers and experts. Qual Saf Health Care. 2010;19:484–489. doi: 10.1136/qshc.2010.042374. [DOI] [PubMed] [Google Scholar]
- 23.Jacobsen PB, Holland JC, Steensma DP. Caring for the whole patient: the science of psychosocial care. J Clin Oncol. 2012;30:1151–1153. doi: 10.1200/JCO.2011.41.4078. [DOI] [PubMed] [Google Scholar]
- 24.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 25.Commission on Cancer of the American College of Surgeons. Cancer Program Standards 2012, version 1.1: Ensuring Patient-Centered Care. Chicago, IL: American College of Surgeons; 2012. [Google Scholar]
- 26.Hill KM, Amir Z, Muers MF, Connolly CK, Round CE. Do newly diagnosed lung cancer patients feel their concerns are being met? Eur J Cancer Care (Engl) 2003;12:35–45. doi: 10.1046/j.1365-2354.2003.00324.x. [DOI] [PubMed] [Google Scholar]
- 27.Maguire R, Papadopoulou C, Kotronoulas G, Simpson MF, McPhelim J, Irvine L. A systematic review of supportive care needs of people living with lung cancer. Eur J Oncol Nurs. 2012;17:449–464. doi: 10.1016/j.ejon.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 28.Kim YA, Yun YH, Chang YJ, et al. Employment status and work-related difficulties in lung cancer survivors compared with the general population. Ann Surg. 2014;259:569–575. doi: 10.1097/SLA.0b013e318291db9d. [DOI] [PubMed] [Google Scholar]
- 29.Li J, Girgis A. Supportive care needs: are patients with lung cancer a neglected population? Psychooncology. 2006;15:509–516. doi: 10.1002/pon.983. [DOI] [PubMed] [Google Scholar]
- 30.Steele R, Fitch MI. Why patients with lung cancer do not want help with some needs. Support Care Cancer. 2008;16:251–259. doi: 10.1007/s00520-007-0301-4. [DOI] [PubMed] [Google Scholar]
- 31.Acheson RM. The definition and identification of need for health care. J Epidemiol Community Health. 1978;32:10–15. doi: 10.1136/jech.32.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carr W, Wolfe S. Unmet needs as sociomedical indicators. Int J Health Serv. 1976;6:417–430. doi: 10.2190/MCG0-UH8D-0AG8-VFNU. [DOI] [PubMed] [Google Scholar]
- 33.Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009;27:2758–2765. doi: 10.1200/JCO.2008.20.8983. [DOI] [PubMed] [Google Scholar]
- 34.Krieger N, Emmons K, Williams D. Defining, investigating, and addressing cancer inequities: critical issues. In: Koh HK, editor. Toward the Elimination of Cancer Disparities. New York: Springer; 2009. pp. 3–28. [Google Scholar]
- 35.Nelson AR, Smedley BD, Stith AY, editors. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 36.Schulz AJ, Mullings L. Gender, Race, Class, and Health: Intersectional Approaches. 1. San Francisco, CA: Jossey-Bass; 2006. [Google Scholar]
- 37.Andersen R, Davidson P. Improving access to care in America. In: Andersen R, Kominski GF, Rice TH, editors. Changing the US Health Care System: Key Issues in Health Services Policy and Management. 3. San Francisco: Jossey-Bass; 2007. [Google Scholar]
- 38.Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: The Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2004;22:2992–2996. doi: 10.1200/JCO.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 39.Catalano PJ, Ayanian JZ, Weeks JC, et al. Cancer Care Outcomes Research Surveillance Consortium. . Representativeness of participants in the Cancer Care Outcomes Research and Surveillance Consortium relative to the Surveillance, Epidemiology, and End Results program. Med Care. 2013;51:e9–e15. doi: 10.1097/MLR.0b013e318222a711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American Association for Public Opinion Research. Final Dispositions of Case Codes and Outcome Rates for Surveys. 5. Lenexa, KS: American Association for Public Opinion Research; 2008. [Google Scholar]
- 41.American Joint Committee on Cancer. AJCC Cancer Staging Atlas. 1. New York: Springer; 2006. [Google Scholar]
- 42.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43:203–220. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- 43.He Y, Zaslavsky AM, Landrum MB, Harrington DP, Catalano P. Multiple imputation in a large-scale complex survey: a practical guide. Stat Methods Med Res. 2010;19:653–670. doi: 10.1177/0962280208101273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2. New York: John Wiley & Sons Inc; 2000. [Google Scholar]
- 45.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56:645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 46.Kleinman LC, Norton EC. What’s the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009;44:288–302. doi: 10.1111/j.1475-6773.2008.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Youdelman MK. The medical tongue: U.S. laws and policies on language access. Health Aff (Millwood) 2008;27:424–433. doi: 10.1377/hlthaff.27.2.424. [DOI] [PubMed] [Google Scholar]
- 48.Park ER, Japuntich SJ, Rigotti NA, et al. A snapshot of smokers after lung and colorectal cancer diagnosis. Cancer. 2012;118:3153–3164. doi: 10.1002/cncr.26545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154:336–346. doi: 10.7326/0003-4819-154-5-201103010-00008. [DOI] [PubMed] [Google Scholar]
- 50.Lopez-Class M, Perret-Gentil M, Kreling B, Caicedo L, Mandelblatt J, Graves K. Quality of life among immigrant Latina breast cancer survivors: realities of culture and enhancing cancer care. J Canc Educ. 2011;26:724–733. doi: 10.1007/s13187-011-0249-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leng J, Lee T, Sarpel U, et al. Identifying the informational and psychosocial needs of Chinese immigrant cancer patients: a focus group study. Support Care Cancer. 2012;20:3221–3229. doi: 10.1007/s00520-012-1464-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Elliott MN, Beckett MK, Chong K, Hambarsoomians K, Hays RD. How do proxy responses and proxy-assisted responses differ from what Medicare beneficiaries might have reported about their health care? Health Serv Res. 2008;43:833–848. doi: 10.1111/j.1475-6773.2007.00820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.The National Lung Screening Trial Research Team. Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Donaldson EA, Holtgrave DR, Duffin RA, Feltner F, Funderburk W, Freeman HP. Patient navigation for breast and colorectal cancer in 3 community hospital settings: an economic evaluation. Cancer. 2012;118:4851–4859. doi: 10.1002/cncr.27487. [DOI] [PubMed] [Google Scholar]
- 55.Carroll JK, Humiston SG, Meldrum SC, et al. Patients’ experiences with navigation for cancer care. Patient Educ Couns. 2010;80:241–247. doi: 10.1016/j.pec.2009.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Forsythe LP, Kent EE, Weaver KE, et al. Receipt of psychosocial care among cancer survivors in the United States. J Clin Oncol. 2013;31:1961–1969. doi: 10.1200/JCO.2012.46.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]