Abstract
This study aimed to determine the diagnostic accuracy of computed tomography imaging for the diagnosis of chronic thromboembolic pulmonary hypertension (CTEPH). Additionally, the effect of test and study characteristics was explored. Studies published between 1990 and 2015 identified by PubMed, OVID search and citation tracking were examined. Of the 613 citations, 11 articles (n=712) met the inclusion criteria. The patient-based analysis demonstrated a pooled sensitivity of 76% (95% confidence interval [CI]: 69% to 82%), and a pooled specificity of 96% (95%CI: 93% to 98%). This resulted in a pooled diagnostic odds ratio (DOR) of 191 (95%CI: 75 to 486). The vessel-based analyses were divided into 3 levels: total arteries、main+ lobar arteries and segmental arteries. The pooled sensitivity were 88% (95%CI: 87% to 90%)、95% (95%CI: 92% to 97%) and 88% (95%CI: 87% to 90%), respectively, with a pooled specificity of 90% (95%CI: 88% to 91%)、96% (95%CI: 94% to 97%) and 89% (95% CI: 87% to 91%). This resulted in a pooled diagnostic odds ratio of 76 (95%CI: 23 to 254),751 (95%CI: 57 to 9905) and 189 (95%CI: 21 to 1072), respectively. In conclusion, CT is a favorable method to rule in CTEPH and to rule out pulmonary endarterectomy (PEA) patients for proximal branches. Furthermore, dual-energy and 320-slices CT can increase the sensitivity for subsegmental arterials, which are promising imaging techniques for balloon pulmonary angioplasty (BPA) approach. In the near future, CT could position itself as the key for screening consideration and for surgical and interventional operability.
Introduction
Chronic thromboembolic pulmonary hypertension (CTEPH) is a life threatening complication and carries poor diagnosis[1]. It is characterized by obstruction of the large pulmonary arteries by acute and recurrent pulmonary emboli[2]. These changes lead to a progressive elevation of pulmonary arterial pressure (PAP) and pulmonary vascular resistance (PVR) and then subsequent right-sided heart failure[3]. Recent studies suggest that the incidence of CTEPH varies from 1% to 3.8% of patients 2 years after acute pulmonary embolism (APE)[4, 5], and CTEPH has a poor prognosis without surgical intervention[6]. Pulmonary endarterectomy (PEA) and BPA has been demonstrated feasible for the treatment of CTEPH. However, the choice of therapy predominantly depends on the presence of inaccessible distal disease [7]. Therefore, preoperative workup is crucial to determine if it is eligible to perform either PEA or BPA[8]. Ventilation/perfusion (V/Q) lung scintigraphy used to be recommended to differentiate CTEPH from unexplained pulmonary hypertension (PH)[9]. There was consensus among experts that the presence of multiple bilateral perfusion defects with normal ventilation allowed the diagnosis of CTEPH. Nevertheless, some trials have depicted that other types of PH including pulmonary veno-occlusive disease, fibrosing mediastinitis, and sarcomas of the pulmonary arteries may occasionally appear the same abnormalities[10, 11]. Combining with right heart catheterization, selective digital subtraction angiography (DSA) remains the choice of diagnosing CTEPH and assessing the eligibility of surgery[12]. But it's invasive and expensive which makes DSA reluctant to be widely used[13]. With the advent of multidetector-row computed tomography (MDCT), computed tomography (CT) has also being increasingly used in the diagnosis of CTEPH[14]. However, uncertainty still persists about the performance of CT for the diagnosis of CTEPH. Therefore it is necessary to know the diagnostic performance of CT for CTEPH. The aim of the study is to conduct a meta-analysis to clarify the role of CT for CTEPH and furthermore provides guidance to clinicians regarding imaging management of CTEPH.
Materials and Methods
Data Sources and Study Selection
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guideline (S1 Table). We searched the PubMed database and Ovid database for English literature from January 1990 to January 2015 on the diagnostic accuracy of CT for the detection of CTEPH. Both free-text searching and thesaurus terms (Medical Subject Headings terms for Pubmed and EMTREE for OVID) were used. We combined search terms for applied technique (Computed Tomography) and disease (Chronic Thromboembolic Pulmonary Hypertension). The bibliographies of included studies and reference lists were also screened for potentially suitable studies. We included a study if: 1) CT was used as a diagnostic test for CTEPH; 2) Patients were referred for suspected or confirmed CTEPH; 3)DSA and/or V/Q scanning were used as reference standard; 4) absolute numbers of true positive, false positive, true negative, and false negative cases were given, or if these data were derivable from the presented results. A study was eligible regardless of what CT technique was used. Studies were excluded if they were: 1) reviews or case reports; 2) conducted with animals. Two investigators independently performed the screening, and any discrepancy was resolved through discussion or by involving a third reviewer (XK), when necessary.
QUADAS-2 tool was used to assess the quality of studies included. We assumed that only V/Q scanning or DSA could correctly rule in or rule out CTEPH.
Data Extraction
First, identifying information about the study such as first author, journal, and year of publication was extracted (Table 1). Further extracted variables consisted of patient characteristics, technical information and absolute numbers of true negative, true positive, false negative, and false positive test results (Table 2). If available, data were recorded on patient basis and vessel basis (i.e., main + lobar pulmonary arteries and segmental arteries). Two investigators (C.D and M.Z) extracted data independently, and discrepancies were resolved by consensus.
Table 1. Characteristics of included studies 1 .
| Author | Year | Study Size (Male, %) | Mean Age, y | Prevalence (%) | Time Interval | Selection | Slices | Contrast Material | Reference Standard | mPAP | SPAP |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bartalena | 2008 | 39(36.4%) | 59 | 34.6 | 0-86d | Confirmed PH | 16 | Iomeron | V/Q,CTPA | Unclear | Unclear |
| He | 2012 | 49(43%) | 43.3 | 44.7 | 7d | Suspected CTEPH | 16 or 64 | Unclear | DSA | 52.77±18.31 | 1474.66±671.16 |
| Dournes | 2014 | 14(35%) | 67.1 | 35 | 2.0±3.8d | Confirmed PH | DECT | Xenetix 350 | V/Q | Unclear | Unclear |
| Tunariu | 2007 | 85(37.4%) | 42 | 34.8 | 48h-10d | Confirmed PH | Unclear | Unclear | DSA,V/Q,CTPA | Unclear | Unclear |
| Sugiura | 2013 | 16(36%) | 59.2 | 100 | 2d-2w | Suspected CTEPH | 320 | Iomeron | DSA | 42.2±9.9 | 696±274 |
| Reichelt | 2009 | 13(48%) | 59 | 89 | 2d-2w | Suspected CTEPH | 64 | Imeron | DSA,V/Q | 46±8 | 763±345 |
| Ley | 2012 | 13(54.2%) | 58 | 100 | 3d | Suspected CTEPH | 40 or 64 | Imeron | DSA | 42±10 | Unclear |
| Soler | 2011 | 5(55.6%) | 52.8 | 100 | Unclear | Confirmed CTEPH | 4 to 64 | Unclear | DSA | 40±8 | 450±178 |
| Nakazawa | 2011 | 35(67%) | 57.7 | 100 | 2.5d | Suspected CTEPH | DECT | Unclear | DSA | Unclear | Unclear |
| Bergin | 1997 | Unclear | Unclear | 87 | Unclear | Suspected CTEPH | Unclear | Ioversol | DSA | Unclear | Unclear |
| Zhang | 2013 | Unclear | 49 | 100 | 10d | Confirmed CTEPH | 64 | Unclear | DSA | Unclear | Unclear |
1mPAP: mean PAP; sPAP: standard PAP.
Table 2. Absolute numbers of included studies 1 .
| Author | Patient-Based Analysis | Vessel-Based Analysis | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Vessels | Main + Lobar | Segmental | ||||||||||||||||||
| No. | TP | FN | FP | TN | No. | TP | FN | FP | TN | No. | TP | FN | FP | TN | No. | TP | FN | FP | TN | |
| Bartalena | 107 | 35 | 2 | 7 | 63 | |||||||||||||||
| He | 114 | 47 | 4 | 3 | 60 | |||||||||||||||
| Dournes | 40 | 14 | 0 | 2 | 23 | |||||||||||||||
| Tunariu | 227 | 40 | 38 | 1 | 148 | |||||||||||||||
| Sugiura | 1175 | 228 | 29 | 44 | 903 | 344 | 65 | 2 | 8 | 269 | 860 | 163 | 27 | 36 | 634 | |||||
| Reichelt | 724 | 365 | 18 | 23 | 336 | 212 | 109 | 2 | 5 | 96 | 530 | 256 | 16 | 18 | 240 | |||||
| Ley | 639 | 370 | 0 | 1 | 268 | 190 | 91 | 0 | 0 | 99 | 449 | 279 | 0 | 1 | 169 | |||||
| Bergin | 910 | 526 | 124 | 102 | 282 | 188 | 43 | 13 | 11 | 121 | 846 | 483 | 111 | 91 | 161 | |||||
| Soler | 107 | 67 | 73 | 8 | 32 | |||||||||||||||
| Nakazawa | 817 | 686 | 25 | 33 | 98 | |||||||||||||||
| Zhang | 589 | 217 | 51 | 42 | 279 | |||||||||||||||
1 No.: number; TP: true positive; FN: false negative; FP: false positive; TN: true negative.
Statistical Analysis
Based on the results from the derived contingency tables, pooled sensitivity, specificity and DOR were calculated. The generated output of sensitivity and 1-specificity were used for the construction of summary receiver operating characteristic (SROC) curves. Also, the area under the curve (AUC) with 95%CIs was computed. SROC curves would generate a composite statistic which can demonstrate the diagnostic ability of CT[15]. The I2 index was used to test for the heterogeneity between study results, which described the significance of total variation across studies rather than chance[16]. Statistical heterogeneity was defined as an I2 statistic value of >50%. Differences in study characteristics between articles can be a cause of considerable heterogeneity (e.g., the use of different contrast media, PAP and PVR). Therefore, the study characteristics were compared using the meta-regression to test for the sources of heterogeneity. Additionally, pooled estimates were calculated for subgroups of studies that were defined according to specific study characteristics on vessel-based analysis. Furthermore, sensitivity analysis were also performed to assess the reliability and stability of the meta-analysis results. Meta-Disc 1.4 was used for data analysis. Publication bias was examined using Deeks' test[17].
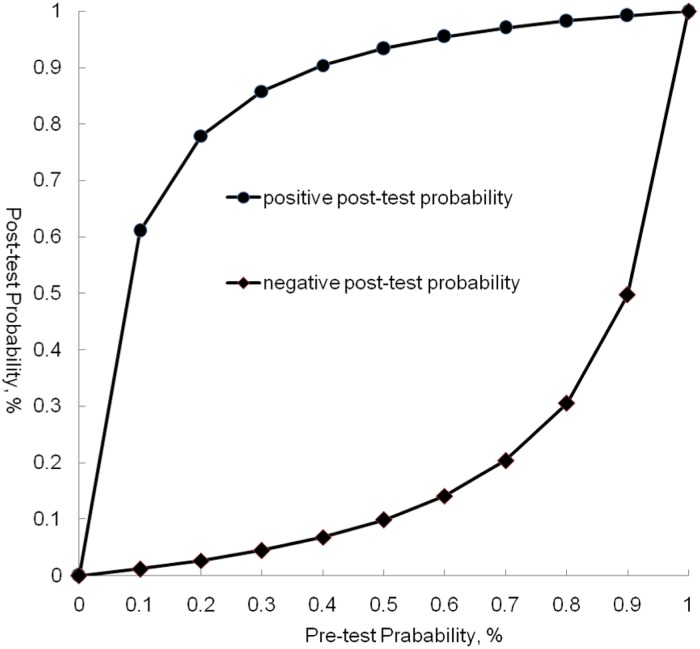
Clinical practice perspectives
Bayes's theorem was used to calculate the post-test probability of CT on patient-based analysis[18]. We presumed that a post-test probability of 85% and 5% was accurate enough to diagnose and exclude CTEPH, respectively[19]. As for vessel-based analysis, positive predictive value (PPV) and negative predictive value (NPV) were computed.
Results
Study Identification
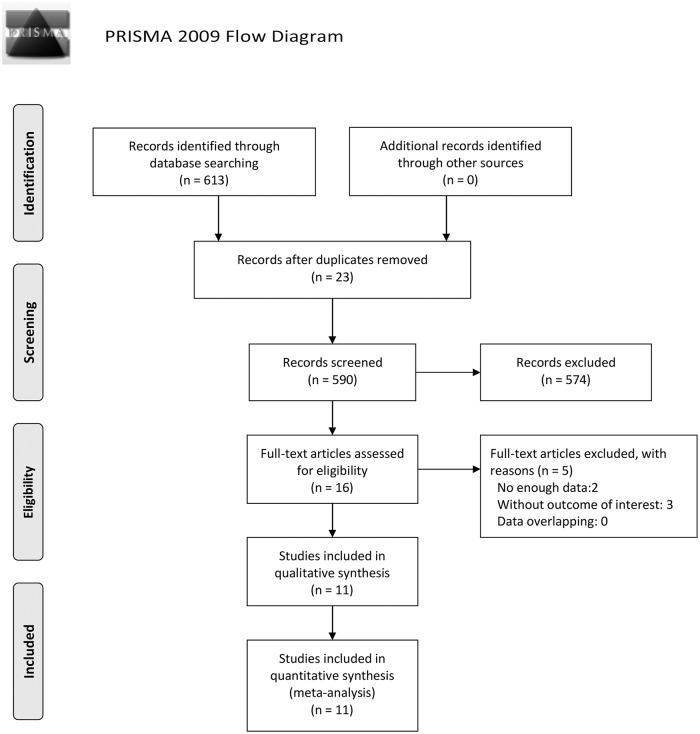
The search process and results were shown in the flow chart in Fig 1. A total of 11 articles met our inclusion criteria: 4 on patient basis and 7 on vessel basis.
Fig 1. Flow Diagram of Literature Search.
Of 613 potentially relevant citations, 11 articles met our inclusion criteria and were included in the meta-analysis.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097
For more information, visit www.prisma-statement.org.
Methodological Quality of Included Studies
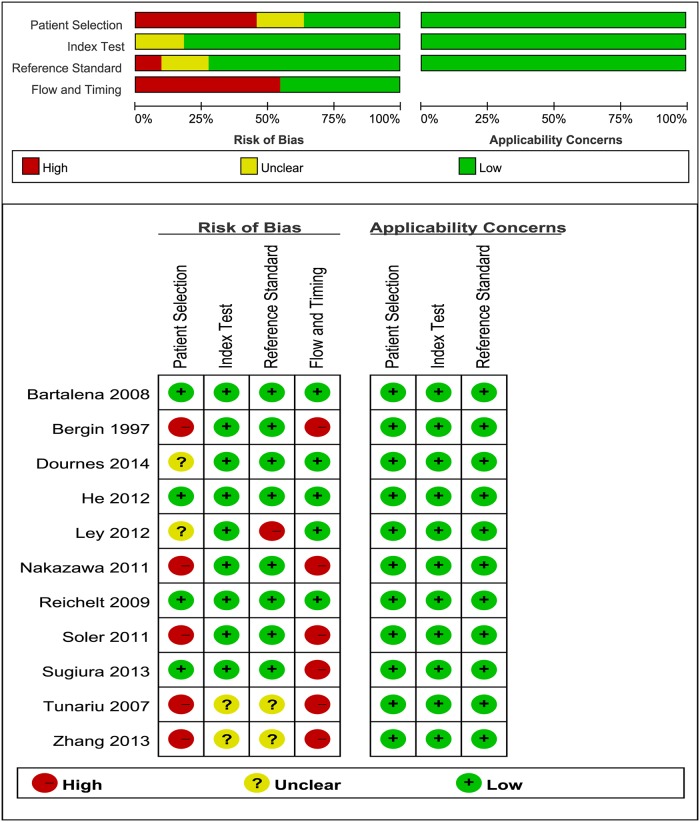
Methodological quality of the studies according to the QUADAS-2 tool was summarized in Fig 2.
Fig 2. Pooled Quality Assessment of Primary Studies.
Study characteristic
Baseline characteristics of patients included in the studies were summarized in Table 1. In total, 11 articles were retrieved [1, 13, 20–28]. Study size ranged from 9 to 227 patients, with a total of 712 subjects, of whom patient-based and vessel-based analyses included 488 and 224 patients, respectively. We observed a mean prevalence of 37% for CTEPH in patient-based studies. The diagnostic performance of two investigators was reported in one study[27]. Since the agreement between the two readers was excellent, we chose values provided by the first reader.
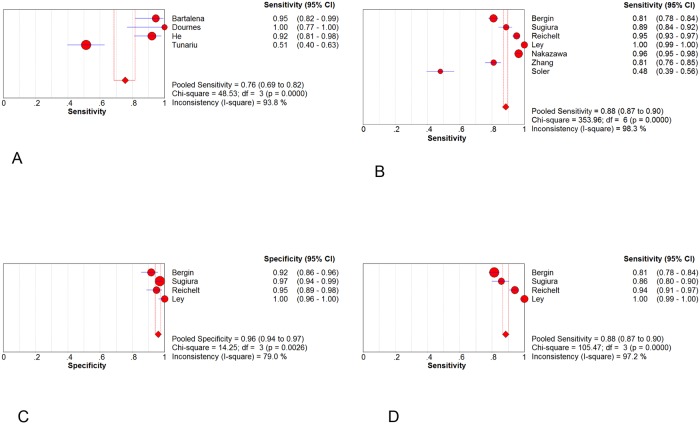
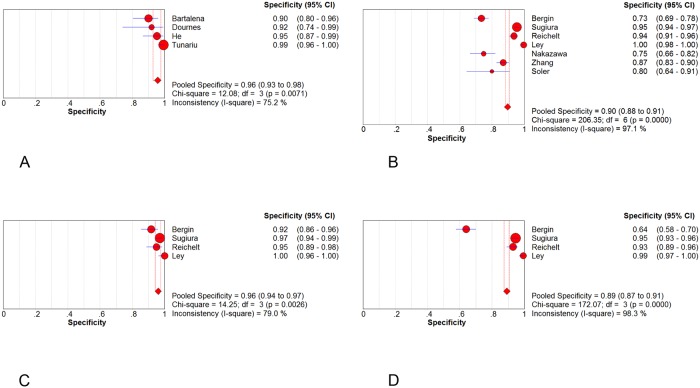
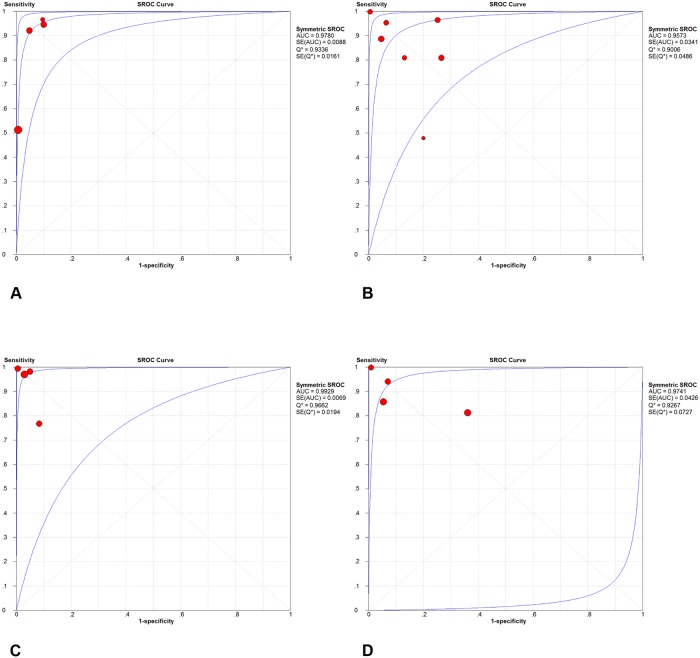
Diagnostic Performance of CT
Forest plots of sensitivity and specificity were shown in Figs 3 and 4. The patient-based analyses demonstrated a moderate sensitivity of 76% (95% CI: 69% to 82%, I2 = 93.8%, p<0.01) and a high specificity of 96% (95%CI: 93% to 98%, I2 = 75.2%, p<0.01). The vessel-based analyses were divided into three levels: total arteries、main+ lobar arteries and segmental arteries. The more peripheral areas the emboli located, the lower the sensitivity and specificity were. The pooled sensitivity were 88% (95%CI: 87% to 90%)、95% (95%CI: 92% to 97%) and 88% (95%CI: 87% to 90%), respectively. And the pooled specificity were 90% (95%CI: 88% to 91%)、96% (95%CI: 94% to 97%) and 89% (95% CI: 87% to 91%), correspondently. SOC curves of CT on both patient and vessel basis were in Fig 5. The area under the curves was 0.9780, 0.9573, 0.9929 and 0.9741, respectively. There was significant heterogeneity across the studies on both patient and vessel basis. Subgroup analyses were performed to explore all possible sources of heterogeneity (Table 3). The analyses revealed no significant effect of study characteristics on the diagnostic performance of CT, except for a lower pooled DOR of CT in poor-quality studies compared with high-quality studies in overall arterials on vessel basis. We classified studies into 2 categories depending upon the methodological quality: high-quality studies (Ref. 19, 23, 24) and poor-quality studies (Ref. 1, 22, 26, 27). A study was judged poor-quality if it was judged "high risk of bias" in 2 or more domains. Additionally, in vessel level, promising CT (320-slices CT and dual-energy CT) demonstrated a higher but non-significant DOR in comparison to routine CT (64 or less slices CT). Sensitivity analysis demonstrated that pooled estimate did not change with exclusion of any 1 study (Table 4). The post-test probability on patient-based analysis showed that CT has a favorable positive post-test probability over a wide range of pre-test probabilities, which can be applied to rule in the disease (Fig 6). The value of PPV and NPV was 90.6% and 87% in total arteries, 92.8% and 97% in main + lobar arteries and 89% and 89% in segmental arteries, respectively.
Fig 3. Forest plots of sensitivity.
Sensitivity in (A) patient basis; (B) total arteries; (C) main + lobar arteries; (D) segmental arteries.
Fig 4. Forest plots of specificity.
Specificity in (A) patient basis; (B) total arteries; (C) main + lobar arteries; (D) segmental arteries.
Fig 5. Summary ROC curve for CT.
Diagnostic performance of CT in (A) patient basis; (B) total arteries; (C) main + lobar arteries; (D) segmental arteries.
Table 3. Subgroup analyses for the diagnostic performance of CT on overall arterials levelc.
| Characteristic | Studies, n | Sensitivity % (95% CI) | Specificity % (95% CI) | DOR (95% CI) | RDOR 1 | p Value |
|---|---|---|---|---|---|---|
| Patient selection | ||||||
| confirmed CTEPH | 2 | 70 (65–74) | 86 (82–90) | 10 (1–78) | 1.00 | |
| suspected CTEPH | 5 | 96 (95–97) | 92 (90–94) | 349 (73–1671) | 35.64 | 0.18 |
| CT technology | ||||||
| Promising CT | 2 | 97(95–98) | 90(87–93) | 268(20–3545) | 1.00 | |
| Routine CT | 4 | 79(76–83) | 90(87–93) | 126(13–1261) | 0.46 | 0.85 |
| Quality | ||||||
| Poor-quality | 4 | 86(84–88) | 85(82–88) | 24(8–75) | 1.00 | |
| High-quality | 3 | 99(96–100) | 97(95–99) | 1604(392–6568) | 0.46 | 0.0139 |
1RDOR: relative diagnostic odds ratio.
Table 4. Sensitivity analysis on both patient and vessel basis.
| Author | Studies, n | Sensitivity%(95%CI) | Specificity%(95% CI) | DOR(95%CI) | p Value |
|---|---|---|---|---|---|
| Patient-based | 4 | 76(69–82) | 96 (93–98) | 191 (75–486) | |
| Excluding Bartalena | 3 | 71 (62–78) | 98 (95–99) | 210 (67–657) | 0.7408 |
| Excluding He | 3 | 79 (60–77) | 96 (93–98) | 170 (53–548) | 0.809 |
| Excluding Dournes | 3 | 74 (66–80) | 96 (93–98) | 184 (69–490) | 0.8774 |
| Excluding Tunariu | 3 | 94 (88–98) | 92 (87–96) | 202 (70–579) | 0.847 |
| Vessel-based | 7 | 88 (87–90) | 90 (88–91) | 76 (23–254) | |
| Excluding Sugiura | 6 | 88 (86–90) | 88 (86–90) | 70 (20–247) | 0.4649 |
| Excluding Reichelt | 6 | 88 (86–89) | 90 (88–92) | 72 (20–258) | 0.6972 |
| Excluding Ley | 6 | 88 (85–89) | 89 (87–91) | 71 (21–241) | 0.1029 |
| Excluding Bergin | 6 | 89 (87–91) | 90 (89–92) | 144 (32–656) | 0.8667 |
| Excluding Soler | 6 | 93 (91–94) | 91 (89–92) | 185 (56–614) | 0.2795 |
| Excluding Nakazawa | 6 | 81 (78–84) | 92 (91–94) | 132 (25–687) | 0.0909 |
| Excluding Zhang | 6 | 90 (88–92) | 92 (90–94) | 171 (29–996) | 0.6446 |
Fig 6. Probabilities of CTEPH after CT on a patient-based level.
The plot showed that CT has a favorable positive post-test probability over a wide range of pre-test probabilities, which can be applied to rule in CTEPH.
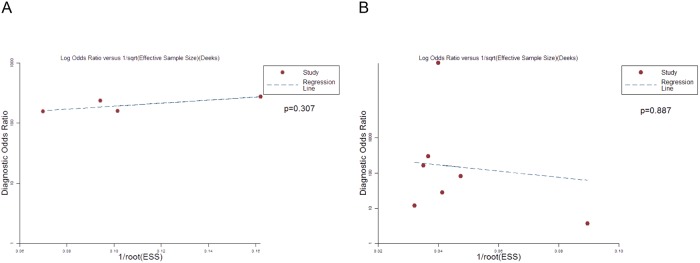
Publication Bias
The effective sample size funnel plot and associated regression test of asymmetry (Deeks 2005) were used to detect publication bias[17]. The results were shown in Fig 7. There was no evidence of publication bias in both patient-based and vessel-based analysis.
Fig 7. Deek’s test to measure the funnel plot asymmetric.
P-values less than 0.05 were considered representative of publication bias. (A) patient basis; (B) total arteries.
Discussion
There are three challenges in imaging of patients with suspected CTEPH: an accurate diagnostic performance of the imaging modality is essential for the presence of CTEPH. It should enable detection of a patient with confirmed CTEPH suitable for PEA with great certainty, and finally, allow the adequate quantification of PH by measuring pulmonary hemodynamics[29]. Several imaging modalities can be applied as diagnostic tools for CTEPH, inclusive of DSA, V/Q lung scintigraphy, multidetector CT angiography and magnetic resonance angiography[2, 30]. Nowadays, invasive pulmonary DSA is a standard diagnostic tool used to assess patients with suspected CTEPH for both establishing the diagnosis and evaluating operability [31, 32]. In contrast to pulmonary DSA, CT is a non-invasive substitute for pulmonary vascular imaging[21]. And it has been found beneficial to determine the causes of PH, affect the selection of surgical methods and predict prognosis after surgery[33]. Accumulating number of articles has focused on the diagnostic accuracy of CT for CTEPH. To the best of our knowledge, this is the first meta-analysis carried out to estimate the role of CT in detection of CTEPH.
Our results indicated a moderate sensitivity and a high specificity of CT for the assessment of CTEPH on patient basis. However, in vessel-based analysis, our meta-analysis revealed both a satisfactory sensitivity and specificity, especially at the main+ lobar artery level. In addition, study quality was identified as a significant source of heterogeneity among studies on vessel-based analysis. And high-quality studies showed a much higher pooled sensitivity of 99% and specificity of 97%, which was considered adequate to confirm and rule out the presence of pulmonary embolism. Whereas patients with acute emboli are practically treated with anticoagulant therapy, regardless of burden of emboli, knowledge of the location and extent of disease in CTEPH helps in the selection of candidates for thromboendarterectomy[27]. Based on this purpose, CT can be used as a good tool for the diagnosis of CTEPH.
A higher but non-significant diagnostic performance was observed for promising CT in comparison with routine CT in overall arterials level. Dual-energy CT has two promising advantages. First, it may be used to provide a “one-stop” diagnostic assessment of CTEPH in anatomy and perfusion without any additional radiation exposure. Small occlusive clots sometimes have a greater influence on oxygenation changes than larger non-occlusive emboli. Lung perfusion imaging can increase the diagnostic performance of CTEPH by identifying those clots in the small vessels, which are difficult to visualize in CTPA. Functional information derived from perfusion imaging can offer a better representation of haemodynamic significance than CTPA alone[34]. Compared with routine CT, dual-energy CT (DECT) can provide an equivalent clinical information about lung perfusion at comparatively low dose. Second, kim et al reported that DECT can be used to differentiate between acute pulmonary thromboembolism and chronic pulmonary thromboembolism through the attenuation value of emboli, which is benefit to choose the correct treatment[35]. Additionally, 320-slices CT scanning can estimate pulmonary artery pressure (PAP) based on interventricular septum (IVS) curvature and evaluate pulmonary hemodynamics in patients with CTEPH[24]. Based on all the aspects mentioned above, DECT and 320-slices CT are promising tools in diagnosing CTEPH.
The sensitivity of the study by Tunariu et al. was much lower than that of the other studies [21]. The reason was thought to be that some patients with subsegmental pulmonary embolism were included in this study[13]. With the emergence of BPA, subsegmental arterials become increasingly important. BPA is implemented as an alternative interventional strategy for patients without surgical potential due to distal pulmonary artery obstructions with surgically inaccessible or comorbid illness[36]. Since studies included in our meta-analysis paid insufficient attention to subsegmental arterials, we can't extracted the data in subsegmental level.
Our meta-analysis has following potential limitations. First, the number of included studies was insufficient. This might reduce the statistical power of meta-analysis. Second, our meta-analysis combined results from trials with different CT techniques, which may lead to bias. Third, patients referred for suspected or confirmed CTEPH may lead to bias although subgroup analysis revealed no significant effect of patient selection. Fourth, the reference standards of included studies referred as DSA or V/Q scanning influence the reliability of the pooled data. Fifth, although subgroup analyses were conducted in overall arterials, some potential factors might be missed such as the contrast agent and the prevalence. Meta-regression wasn't conducted in patient-basis, main+ lobar arterials and segmental arterials because of insufficient trials. Sixth, diagnostic value of CTEPH in subsegmental arterials wasn't evaluated due to lack of data.
In conclusion, CT is a favorable method to rule in CTEPH and to rule out pulmonary endarterectomy (PEA) patients for proximal branches. Furthermore, dual-energy and 320-slices CT can increase the sensitivity for subsegmental arterials, which are promising imaging techniques for balloon pulmonary angioplasty (BPA) approach. In the near future, CT could position itself as the key for screening consideration and for surgical and interventional operability.
Supporting Information
(PDF)
Acknowledgments
We thank all the people who give the help for this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1. Soler X, Hoh CK, Test VJ, Kerr KM, Marsh JJ, Morris TA. Single photon emission computed tomography in chronic thromboembolic pulmonary hypertension. Respirology (Carlton, Vic). 2011;16(1):131–7. Epub 2010/10/06. 10.1111/j.1440-1843.2010.01867.x . [DOI] [PubMed] [Google Scholar]
- 2. Dartevelle P, Fadel E, Mussot S, Chapelier A, Herve P, de Perrot M, et al. Chronic thromboembolic pulmonary hypertension. The European respiratory journal. 2004;23(4):637–48. . [DOI] [PubMed] [Google Scholar]
- 3. Hoey ET, Mirsadraee S, Pepke-Zaba J, Jenkins DP, Gopalan D, Screaton NJ. Dual-energy CT angiography for assessment of regional pulmonary perfusion in patients with chronic thromboembolic pulmonary hypertension: initial experience. AJR American journal of roentgenology. 2011;196(3):524–32. Epub 2011/02/24. 10.2214/ajr.10.4842 . [DOI] [PubMed] [Google Scholar]
- 4. Dentali F, Donadini M, Gianni M, Bertolini A, Squizzato A, Venco A, et al. Incidence of chronic pulmonary hypertension in patients with previous pulmonary embolism. Thrombosis research. 2009;124(3):256–8. 10.1016/j.thromres.2009.01.003 . [DOI] [PubMed] [Google Scholar]
- 5. Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. The New England journal of medicine. 2004;350(22):2257–64. 10.1056/NEJMoa032274 . [DOI] [PubMed] [Google Scholar]
- 6. Lewczuk J, Piszko P, Jagas J, Porada A, Wojciak S, Sobkowicz B, et al. Prognostic factors in medically treated patients with chronic pulmonary embolism. Chest. 2001;119(3):818–23. . [DOI] [PubMed] [Google Scholar]
- 7. Manecke GR Jr,. Anesthesia for pulmonary endarterectomy. Seminars in thoracic and cardiovascular surgery. 2006;18(3):236–42. 10.1053/j.semtcvs.2006.09.005 . [DOI] [PubMed] [Google Scholar]
- 8. Ley S, Kauczor HU, Heussel CP, Kramm T, Mayer E, Thelen M, et al. Value of contrast-enhanced MR angiography and helical CT angiography in chronic thromboembolic pulmonary hypertension. European radiology. 2003;13(10):2365–71. Epub 2003/04/25. 10.1007/s00330-003-1878-8 . [DOI] [PubMed] [Google Scholar]
- 9. Galie N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, Barbera JA, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). European heart journal. 2009;30(20):2493–537. 10.1093/eurheartj/ehp297 . [DOI] [PubMed] [Google Scholar]
- 10. Fedullo PF, Auger WR, Channick RN, Kerr KM, Rubin LJ. Chronic thromboembolic pulmonary hypertension. Clinics in chest medicine. 2001;22(3):561–81. Epub 2001/10/10. . [DOI] [PubMed] [Google Scholar]
- 11. Bailey CL, Channick RN, Auger WR, Fedullo PF, Kerr KM, Yung GL, et al. "High probability" perfusion lung scans in pulmonary venoocclusive disease. American journal of respiratory and critical care medicine. 2000;162(5):1974–8. 10.1164/ajrccm.162.5.2003045 . [DOI] [PubMed] [Google Scholar]
- 12. Pitton MB, Duber C, Mayer E, Thelen M. Hemodynamic effects of nonionic contrast bolus injection and oxygen inhalation during pulmonary angiography in patients with chronic major-vessel thromboembolic pulmonary hypertension. Circulation. 1996;94(10):2485–91. . [DOI] [PubMed] [Google Scholar]
- 13. He J, Fang W, Lv B, He JG, Xiong CM, Liu ZH, et al. Diagnosis of chronic thromboembolic pulmonary hypertension: comparison of ventilation/perfusion scanning and multidetector computed tomography pulmonary angiography with pulmonary angiography. Nuclear medicine communications. 2012;33(5):459–63. Epub 2012/01/21. 10.1097/MNM.0b013e32835085d9 . [DOI] [PubMed] [Google Scholar]
- 14. Rajaram S, Swift AJ, Capener D, Telfer A, Davies C, Hill C, et al. Diagnostic accuracy of contrast-enhanced MR angiography and unenhanced proton MR imaging compared with CT pulmonary angiography in chronic thromboembolic pulmonary hypertension. European radiology. 2012;22(2):310–7. Epub 2011/09/03. 10.1007/s00330-011-2252-x . [DOI] [PubMed] [Google Scholar]
- 15. Rosman AS, Korsten MA. Application of summary receiver operating characteristics (sROC) analysis to diagnostic clinical testing. Advances in medical sciences. 2007;52:76–82. . [PubMed] [Google Scholar]
- 16. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. Journal of clinical epidemiology. 2005;58(9):882–93. 10.1016/j.jclinepi.2005.01.016 . [DOI] [PubMed] [Google Scholar]
- 18. Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. The New England journal of medicine. 1979;300(24):1350–8. 10.1056/NEJM197906143002402 . [DOI] [PubMed] [Google Scholar]
- 19. Kearon C. Diagnosis of pulmonary embolism. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2003;168(2):183–94. [PMC free article] [PubMed] [Google Scholar]
- 20. Ley S, Ley-Zaporozhan J, Pitton MB, Schneider J, Wirth GM, Mayer E, et al. Diagnostic performance of state-of-the-art imaging techniques for morphological assessment of vascular abnormalities in patients with chronic thromboembolic pulmonary hypertension (CTEPH). European radiology. 2012;22(3):607–16. Epub 2011/09/29. 10.1007/s00330-011-2290-4 . [DOI] [PubMed] [Google Scholar]
- 21. Tunariu N, Gibbs SJ, Win Z, Gin-Sing W, Graham A, Gishen P, et al. Ventilation-perfusion scintigraphy is more sensitive than multidetector CTPA in detecting chronic thromboembolic pulmonary disease as a treatable cause of pulmonary hypertension. Journal of nuclear medicine: official publication, Society of Nuclear Medicine. 2007;48(5):680–4. Epub 2007/05/04. 10.2967/jnumed.106.039438 . [DOI] [PubMed] [Google Scholar]
- 22. Dournes G, Verdier D, Montaudon M, Bullier E, Riviere A, Dromer C, et al. Dual-energy CT perfusion and angiography in chronic thromboembolic pulmonary hypertension: diagnostic accuracy and concordance with radionuclide scintigraphy. European radiology. 2014;24(1):42–51. Epub 2013/08/29. 10.1007/s00330-013-2975-y . [DOI] [PubMed] [Google Scholar]
- 23. Nakazawa T, Watanabe Y, Hori Y, Kiso K, Higashi M, Itoh T, et al. Lung perfused blood volume images with dual-energy computed tomography for chronic thromboembolic pulmonary hypertension: correlation to scintigraphy with single-photon emission computed tomography. Journal of computer assisted tomography. 2011;35(5):590–5. Epub 2011/09/20. 10.1097/RCT.0b013e318224e227 . [DOI] [PubMed] [Google Scholar]
- 24. Sugiura T, Tanabe N, Matsuura Y, Shigeta A, Kawata N, Jujo T, et al. Role of 320-slice CT imaging in the diagnostic workup of patients with chronic thromboembolic pulmonary hypertension. Chest. 2013;143(4):1070–7. Epub 2012/10/27. 10.1378/chest.12-0407 . [DOI] [PubMed] [Google Scholar]
- 25. Reichelt A, Hoeper MM, Galanski M, Keberle M. Chronic thromboembolic pulmonary hypertension: evaluation with 64-detector row CT versus digital substraction angiography. European journal of radiology. 2009;71(1):49–54. Epub 2008/05/09. 10.1016/j.ejrad.2008.03.016 . [DOI] [PubMed] [Google Scholar]
- 26. Bartalena T, Oboldi D, Guidalotti PL, Rinaldi MF, Bertaccini P, Napoli G, et al. Lung perfusion in patients with pulmonary hypertension: comparison between MDCT pulmonary angiography with minIP reconstructions and 99mTc-MAA perfusion scan. Invest Radiol. 2008;43(6):368–73. Epub 2008/05/23. 10.1097/RLI.0b013e31816901e2 . [DOI] [PubMed] [Google Scholar]
- 27. Bergin CJ, Sirlin CB, Hauschildt JP, Huynh TV, Auger WR, Fedullo PF, et al. Chronic thromboembolism: diagnosis with helical CT and MR imaging with angiographic and surgical correlation. Radiology. 1997;204(3):695–702. Epub 1997/09/01. 10.1148/radiology.204.3.9280245 . [DOI] [PubMed] [Google Scholar]
- 28. Zhang Z, Guo Y. A comparison between ventilation/perfusion scintigraphy and ctpa in the diagnosis of chronic thromboembolic pulmonary hypertension. Journal of Thoracic Imaging. 2013;28 (5):W94 . [Google Scholar]
- 29. Wirth G, Bruggemann K, Bostel T, Mayer E, Duber C, Kreitner KF. Chronic Thromboembolic Pulmonary Hypertension (CTEPH)—Potential Role of Multidetector-Row CT (MD-CT) and MR Imaging in the Diagnosis and Differential Diagnosis of the Disease. RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2014. Epub 2014/04/24. 10.1055/s-0034-1366425 . [DOI] [PubMed] [Google Scholar]
- 30. Hoeper MM, Mayer E, Simonneau G, Rubin LJ. Chronic thromboembolic pulmonary hypertension. Circulation. 2006;113(16):2011–20. 10.1161/CIRCULATIONAHA.105.602565 . [DOI] [PubMed] [Google Scholar]
- 31. Jamieson SW, Kapelanski DP, Sakakibara N, Manecke GR, Thistlethwaite PA, Kerr KM, et al. Pulmonary endarterectomy: experience and lessons learned in 1,500 cases. The Annals of thoracic surgery. 2003;76(5):1457–62; discussion 62–4. . [DOI] [PubMed] [Google Scholar]
- 32. Auger WR, Channick RN, Kerr KM, Fedullo PF. Evaluation of patients with suspected chronic thromboembolic pulmonary hypertension. Seminars in thoracic and cardiovascular surgery. 1999;11(2):179–90. Epub 1999/06/23. . [DOI] [PubMed] [Google Scholar]
- 33. Coulden R. State-of-the-art imaging techniques in chronic thromboembolic pulmonary hypertension. Proceedings of the American Thoracic Society. 2006;3(7):577–83. Epub 2006/09/12. 10.1513/pats.200605-119LR . [DOI] [PubMed] [Google Scholar]
- 34. Hoey ET, Gopalan D, Ganesh V, Agrawal SK, Qureshi N, Tasker AD, et al. Dual-energy CT pulmonary angiography: a novel technique for assessing acute and chronic pulmonary thromboembolism. Clinical radiology. 2009;64(4):414–9. 10.1016/j.crad.2008.11.007 . [DOI] [PubMed] [Google Scholar]
- 35. Kim SS, Hur J, Kim YJ, Lee HJ, Hong YJ, Choi BW. Dual-energy CT for differentiating acute and chronic pulmonary thromboembolism: an initial experience. The international journal of cardiovascular imaging. 2014;30 Suppl 2:113–20. Epub 2014/08/07. 10.1007/s10554-014-0508-7 . [DOI] [PubMed] [Google Scholar]
- 36. Feinstein JA, Goldhaber SZ, Lock JE, Ferndandes SM, Landzberg MJ. Balloon pulmonary angioplasty for treatment of chronic thromboembolic pulmonary hypertension. Circulation. 2001;103(1):10–3. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.