Abstract
This study sought to assess the relationship between serum concentrations of the soluble ST2 (sST2) and B-type natriuretic peptide (BNP) and investigate the role of sST2 as a prognosticator in patients hospitalized with acute heart failure (HF) and renal insufficiency. sST2 was measured at admission and discharge in 66 patients hospitalized with acute decompensated HF and renal insufficiency (estimated glomerular filtration rate [eGFR] < 90 mL/min/1.73 m2) using a high sensitivity immunoassay. BNP was sampled at the same time and compared to sST2. Demographical, biochemical, and echocardiographic data were also obtained during hospitalization.There were positive correlations between sST2 and BNP levels at admission (r = 0.330, P = 0.007) and at discharge (r = 0.320, P = 0.009) in overall patients. However, there was no correlation between them at each timepoint in patients with severe renal insufficiency (eGFR < 30 mL/min/1.73 m2, n = 17). sST2 level was not changed with the degree of renal function, even though BNP level was much higher in patients with severe renal insufficiency. During 3 month follow-up, 9 (13.6%) died and 16 (24.2%) were readmitted due to HF aggravation.On multivariate analysis, sST2 at discharge was independently associated with death or HF readmission during 3 months after discharge (hazard ratio, 1.038; 95% confidence interval, 1.011-1.066, P = 0.006). In conclusion, sST2 is not affected by renal function compared with BNP in acute HF patients. The measurement of predischarge sST2 can be helpful in predicting short-term outcomes in acute decompensated HF patients with renal insufficiency.
Keywords: ST2 Protein, Human; Natriuretic Peptide, Brain; Heart Failure; Renal Insufficiency
INTRODUCTION
B-type natriuretic peptide (BNP) has been used for risk stratification and prognosis prediction in heart failure (HF) patients. However, the role of BNP seems to be in doubt in patients with renal insufficiency. It is cleared by receptor-mediated proteolysis, enzymatic digestion by neutral endopeptidases, and passive excretion,all of which are affected by renal function (1, 2). Therefore, plasma BNP concentration is elevated in patients with reduced estimated glomerular filtration rate (eGFR) (3, 4). Nonetheless, recent studies have suggested that BNP is also a valuable diagnostic and prognostic biomarker in HF patients with renal insufficiency, just requiring higher diagnostic cut-offs (3, 5). However, there are some risks for confounding effect of BNP in renal insufficiency patients because it may be affected by volume expansion due to renal dysfunction or associated left ventricular (LV) hypertrophy and silent coronary artery disease in which BNP may be elevated (4, 6). Moreover, high concentrations of BNP imply great differences of values according to the changes of clinical situation. Thus, there has been a hurdle of using BNP as a biomarker in real world HF patients with renal insufficiency.
ST2 is a member of interleukin (IL)-1 receptor family and functions as a decoy receptor of IL-33 which has a role in ameliorating myocardial hypertrophy and fibrosis in response to cardiovascular stretch (7, 8). ST2 has two isoforms, a transmembrane and a soluble form, and the latter is known to be a biomarker in several cardiovascular diseases including HF (9, 10). The expression of soluble ST2 (sST2) is regulated by immune inflammatory processes. However, it is not certain whether the level of sST2 might be influenced by renal function. Recent study revealed that sST2 was valuable as a prognostic marker in chronic HF patients with renal insufficiency (11). However, there are few data about the role of sST2 as a predictor of poor prognosis in acute HF patients with impaired renal function. The purpose of this study was to investigate whether sST2 might be correlated with BNP according to renal function and it might be helpful to predict future clinical outcomes compared with BNP in patients hospitalized with acute decompensated HF and renal insufficiency.
MATERIALS AND METHODS
Study population
From March 2013 and January 2014, 77 patients aged over 18 yr and hospitalized with acute decompensated HF were enrolled at theAsan Medical Center in Seoul, Korea. Among them, patients with renal insufficiency (eGFR <90 mL/min/1.73 m2) were included. Patients with end-stage renal disease who required renal replacement therapy were excluded from the study. In addition, patients with rheumatic disease or systemic or localizedinfection were excluded. Finally, a total of 66 patients were analyzed in this study. Demographical, biochemical, and echocardiographic data were obtained during hospitalization. All patients were followed up at least 3 months after discharge.
The measurement of sST2 and BNP levels
Blood samples were collected within 24 hr after admission and before discharge in EDTA-containing tubes. sST2 and BNP levels were analyzed from the same blood sample. sST2 serum concentrations were measured from samples using a high-sensitivity sandwich monoclonal immunoassay (Presage sST2 assay; Critical Diagnostics, San Diego, CA, USA). The antibodies used in the Presage assay were generated from recombinantprotein based on the human cDNA clone for the completesoluble sST2 sequence. BNP serum concentrations were determined using a high-throughput system (ADVIA Centaur CP immunoassay; Siemens Medical Solution Diagnostics, Tarrytown, NY, USA).
Assessment of kidney function
Kidney function was assessed by eGFR (modification of diet in renal disease formula, MDRD, mL/min/1.73 m2). The patients wereclassified into three categories based on their eGFR. Mild renal insufficiency included patients with eGF in 89-60 mL/min/1.73 vm2. Moderate renal insufficiency included progressed patients with eGFR in 59-30 mL/min/1.73 m2. Severe renal insufficiency included pre-dialyzed patients with eGFR <30 mL/min/1.73 m2.
Statistical analysis
All values are expressed as mean±standarddeviation (continuous variables) or as counts and percentages (categorical variables). Continuous variables were compared using thettest or the Mann Whitney U test, and categorical variables were compared using chi-square statistics or Fisher's exact tests. Correlations between sST2 levels and BNP levels at the same timepoints were performed using Pearson's correlation coefficient.
Univariate analysis of the risk factors associated with the development of death or HF readmission within 3 months after hospital discharge was performed using the chi-square statistic and estimates of hazard ratios (HRs) with their 95% confidence intervals (CIs). Multivariate analysis was performed to evaluate the independent risk factors associated with the development of the events and using logistic regression analysis for the dichotomous dependent variables. Forward conditional method was selected for this model. The entry criterion used for the multivariate analysis was P<0.10 as determined by univariate analysis. Receiver operating characteristic (ROC) analyses were also performed to assess optimal sST2 cut points. P values less than 0.05 were considered to indicate statistical significance. All statistical analyses were performed using the SPSS version 17.0 (SPSS Inc., Chicago, IL, USA).
Ethics statement
Patients signed written informed consent before being included, and the study was approved by the institutional review board of the Asan Medical Center (IRB No. 2013-0308).
RESULTS
Baseline characteristics of the study population
A total of 66 patients were enrolled and analyzed. Forty patients were males with a mean age of 66.9±15.0 yr (range: 18-89 yr). LV ejection fraction (EF) at enrollment was 27.5±8.8% and mean eGFR was 46.9±25.1 mL/min/1.73 m2. Seventeen patients (25.8%) had severe renal insufficiency, while 26 patients (39.4%) had moderate renal insufficiency and 23 patients (34.8%) had mild renal insufficiency at admission. The comparisons of baseline characteristics of all patients stratified by renal function are shown in Table 1. Patients with mild renal insufficiency had younger age (68.4±13.4 yr vs. 72.1±8.7 yr vs. 59.9±19.1 yr, P=0.014 for severe vs. moderate vs. mild renal insufficiency) and lower incidence of diabetes (52.9% vs. 57.7% vs. 17.4%, P=0.010) and patients with severe renal insufficiency had lower hemoglobin levels (10.8±2.7g/dL vs. 12.3±2.4g/dL vs. 13.4±2.5 g/dL, P=0.006).
Table 1. Baseline clinical characteristics.
| Characteristics (Unit) | eGFR (mL/min/1.73 m2) | P values | |||
|---|---|---|---|---|---|
| Overall (n=66) | <30 (n=17) | 30-59 (n=26) | 60-89 (n=23) | ||
| Age (yr) | 66.9 ± 15.0 | 68.4 ± 13.4 | 72.1 ± 8.7 | 59.9 ± 19.1 | 0.014 |
| Male | 40 (58.0) | 10 (58.8) | 17 (65.4) | 13 (56.5) | 0.806 |
| Resting heart rate (beats/min) | 95.0 ± 28.5 | 91.7 ± 33.3 | 97.2 ± 25.1 | 95.0 ± 29.5 | 0.833 |
| Mean blood pressure (mmHg) | 98.9 ± 24.8 | 103.4 ± 23.3 | 92.6 ± 22.1 | 102.8 ± 28.1 | 0.251 |
| Body mass index (kg/m2) | 23.0 ± 3.5 | 22.1 ± 2.7 | 23.4 ± 3.7 | 23.1 ± 4.0 | 0.491 |
| NYHA functional class ≥ III | 48 (72.7) | 12 (70.6) | 22 (84.6) | 14 (60.9) | 0.960 |
| Diabetes | 28 (42.4) | 9 (52.9) | 15 (57.7) | 4 (17.4) | 0.010 |
| Hypertension | 38 (57.6) | 12 (70.6) | 14 (53.8) | 12 (52.2) | 0.449 |
| Atrial fibrillation | 21 (31.8) | 7 (41.2) | 9 (34.6) | 5 (21.7) | 0.395 |
| Dyslipidemia | 22 (33.3) | 9 (52.9) | 6 (23.1) | 7 (30.4) | 0.119 |
| Ischemic etiology | 23 (34.8) | 9 (52.9) | 10 (38.5) | 4 (17.4) | 0.058 |
| Dilated cardiomyopathy | 32 (48.5) | 5 (29.4) | 14 (53.8) | 13 (56.5) | 0.185 |
| LV ESD (mm) | 51.1 ± 10.1 | 49.4 ± 7.5 | 51.4 ± 9.9 | 52.1 ± 12.2 | 0.703 |
| LV EDD (mm) | 60.5 ± 8.9 | 60.4 ± 6.7 | 60.0 ± 9.1 | 61.3 ± 10.4 | 0.885 |
| LV EF (%) | 27.5 ± 8.8 | 30.4 ± 8.0 | 26.1 ± 7.4 | 27.0 ± 10.5 | 0.271 |
| Serum creatinine (mg/dL) | 1.96 ± 1.45 | 3.98 ± 1.46 | 1.58 ± 0.36 | 0.91 ± 0.18 | < 0.001 |
| Serum BUN (mg/dL) | 37.7 ± 24.5 | 65.8 ± 27.0 | 35.5 ± 14.1 | 19.4 ± 7.1 | < 0.001 |
| Serum sodium (mM/L) | 136.5 ± 5.7 | 137.0 ± 5.6 | 136.4 ± 5.6 | 136.2 ± 6.2 | 0.912 |
| Hemoglobin (g/dL) | 12.3 ± 2.7 | 10.8 ± 2.7 | 12.3 ± 2.4 | 13.4 ± 2.5 | 0.006 |
| Renin-angiotensin antagonist | 44 (66.7) | 9 (52.9) | 20 (76.9) | 15 (65.2) | 0.260 |
| β blocker | 29 (43.9) | 11 (64.7) | 11 (42.3) | 7 (30.4) | 0.095 |
| Aldosterone antagonist | 9 (13.6) | 1 (5.9) | 5 (19.2) | 3 (13.0) | 0.457 |
Values represent the number (percentages) or mean±standard deviation.eGFR, estimated glomerular filtration rate;NYHA, New York Heart Association; LV ESD/EDD, left ventricular end-systolic/diastolic dimension; EF, Ejection fraction; BUN, Blood urea nitrogen.
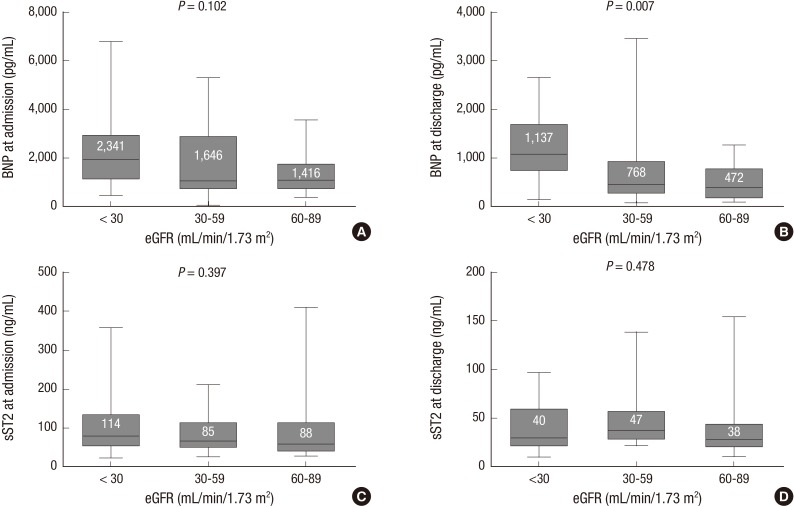
The levels of BNP and sST2 at admission and at discharge according to the degree of renal function
The level of BNP at admission showed a trend toward high concentration in patients with severe renal insufficiency compared to mild or moderate renal insufficiency, which did not achieve statistical difference (Fig. 1A, 2,341.9±1,664.8 pg/mL vs. 1,645.6±1,479.5 pg/mL vs. 1,416.4±898.8 pg/mL, P=0.102 for severe vs. moderate vs. mild renal insufficiency). BNP at discharge was much higher in patients with severe renal insufficiency (Fig. 1B, 1,136.6±654.8 pg/mL vs. 768.1±782.2 pg/mL vs. 472.0±350.5 pg/mL, P=0.007 for severe vs. moderate vs. mild renal insufficiency). However, the level of sST2 was not changed with the degree of renal dysfunction (Fig. 1C, sST2 at admission; 114.1±90.4 ng/mL vs. 84.5±48.0 ng/mL vs. 88.0±81.6 ng/mL, P=0.397 for severe vs. moderate vs. mild renal insufficiency: Fig. 1D, sST2 at discharge; 39.9±23.2 ng/mL vs. 47.1±27.6 ng/mL vs. 37.9±30.5 ng/mL, P=0.478). In addition, there was no relationship between sST2 level and eGFR (r=-0.140, P=0.262 for admission: r=-0.109, P=0.383 for discharge).
Fig. 1. Changes of BNP and sST2 according to the degree of renal function. Box plots of BNP at admission (A) and at discharge (B) according to the degree of renal function and box plots of sST2 at admission (C) and at discharge (D) according to the degree of renal function. The central box represents the values from the lower to the upper quartile, the middle line the median;the whiskers extend to the minimum and maximum values. The value in the box indicates the mean of biomarkers.
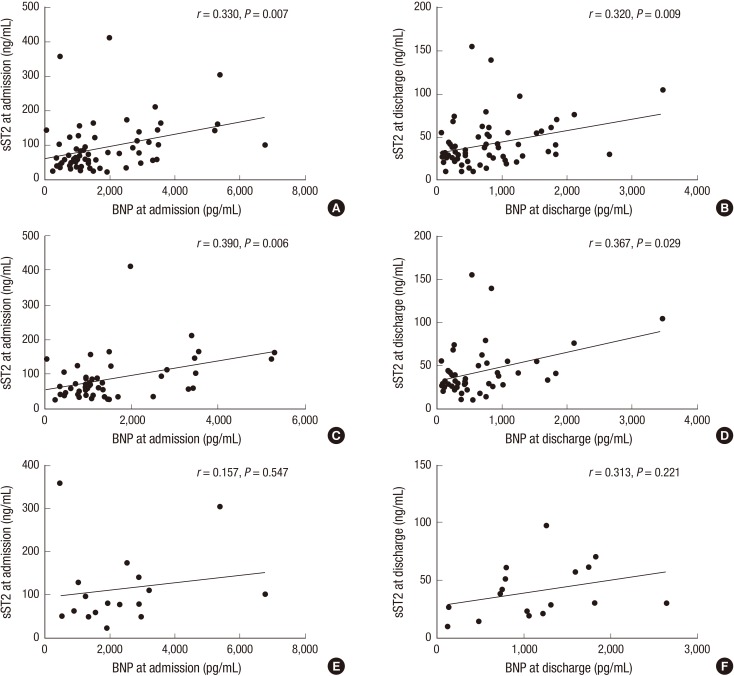
Relationship between sST2 and BNP according to the degree of renal function
There were mild correlations between sST2 and BNP at admission (r=0.330, P=0.007) and at discharge (r=0.320, P=0.009) in total patients (Fig. 2). In addition, there was mild correlation between them in patients with mild to moderate renal insufficiency (eGFR in 89-30 mL/min/1.73 m2, n=49: r=0.390, P= 0.006 for admission: r=0.367, P=0.029 for discharge). However, there was no correlation between them at each timepoint in patients with severe renal insufficiency (eGFR<30 mL/min/1.73 m2, n=17).
Fig. 2. Correlations between sST2 and BNP levels. The correlations between sST2 and BNP levels at admission (A) and at discharge (B) in total patients (n = 66). The correlation between sST2 and BNP levels at admission (C) and at discharge (D) in acute HF patients with mild to moderate renal insufficiency (n = 49). The correlation between sST2 and BNP levels at admission (E) and at discharge (F) in acute HF patients with severe renal insufficiency (n = 17).
Association between sST2 and other clinical parameters
There was no correlation between sST2 and age (r=-0.052, P=0.679 for admission: r=0.083, P=0.507 for discharge). Moreover, there was no correlation between sST2 and body mass index (r=-0.060, P=0.640 for admission: r=0.054, P=0.674 for discharge). In addition, there was no difference in the level of sST2 at admission according to sex (89.2±63.9 ng/mL vs. 99.8±85.8 ng/mL, P=0.591 for male vs. female). However, male patients showed higher sST2 level at discharge than female patients (47.5±30.3 ng/mL vs. 33.7±20.5 ng/mL, P=0.031 for male vs. female). There were no differences in the level of sST2 at admission (117.4±90.2 ng/mL vs. 86.3±81.2 ng/mL vs. 84.6±48.4 ng/mL, P=0.307 for class II vs. III vs. IV) and at discharge (31.3±12.0 ng/mL vs. 46.8±31.4 ng/mL vs. 46.5±30.4 ng/mL, P=0.135 for class I vs. II vs. III) according to NYHA functional class.
sST2 as a prognostic indicator
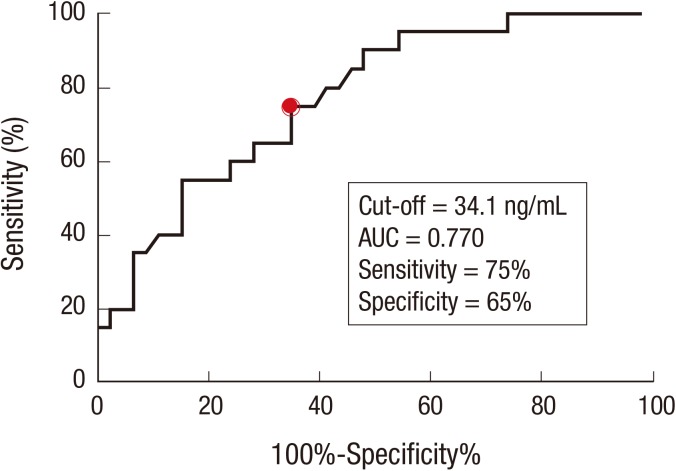
During 3 month follow-up, 9 patients (13.6%) died due to cardiac cause and 16 patients (24.2%) were readmitted due to HF aggravation. According to the degree of renal function, 2 patients (11.8%), 7 patients (26.9%), and no patient (0%) died in severe, moderate, and mild renal insufficiency group, respectively. In addition, 7 patients (41.2%), 5 patients (19.2%), and 4 patients (17.4%) were readmitted due to HF aggravation in severe, moderate, and mild renal insufficiency group, respectively. The results of the univariate analysis showed that BNP at discharge, sST2 at discharge, eGFR, serum creatinine, blood urea nitrogen, and hemoglobin level were significantly associated with the development of death or HF readmission within 3 months after hospital discharge (Table 2). Delta-sST2 and delta-BNP (delta means the value at admission minus the value at discharge) were not related to the development of events. On multivariate analysis, sST2 at discharge and hemoglobin levels were independently associated with death or HF readmission during 3 months after discharge (HR, 1.038; 95% CI, 1.011-1.066, P=0.006 for sST2 at discharge: HR, 0.723; 95% CI, 0.550-0.951, P=0.020 for hemoglobin). ROC analysis showed that the best cut-off value of sST2 at discharge for predicting death or HF readmission was 34.1 ng/mL, which showed a sensitivity of 75% and a specificity of 65% (Fig. 3). When the area under curves of sST2 and BNP at admission and at discharge were compared, sST2 at discharge was superior to other variables to predict outcomes (Table 3). However, net reclassification improvement did not improve when sST2 at discharge was added to the model including BNP at discharge (95% CI -0.097-0.861, P=0.118 for risk as a continuous variable: 95% CI -0.120-0.513, P=0.069 for risk as a categorical variable).
Table 2. Factors associated withthe development of death or HF readmission within 3 months after hospital discharge.
| Variables | Univariateanalsysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | |
| sST2 at admission | 1.008 | 1.000-1.015 | 0.058 | |||
| BNP at admission | 1.000 | 1.000-1.001 | 0.082 | |||
| sST2 at discharge | 1.041 | 1.013-1.070 | 0.004 | 1.038 | 1.011-1.066 | 0.006 |
| BNP at discharge | 1.001 | 1.000-1.002 | 0.009 | |||
| eGFR | 0.974 | 0.951-0.997 | 0.026 | |||
| Serum creatinine | 1.461 | 1.009-2.115 | 0.045 | |||
| Serum BUN | 1.029 | 1.005-1.054 | 0.017 | |||
| Hemoglobin | 0.702 | 0.544-0.906 | 0.006 | 0.723 | 0.550-0.951 | 0.020 |
HR, Hazard ratio; CI, Confidence interval; eGFR, estimated glomerular filtration rate; BUN, Blood urea nitrogen.
Fig. 3. The receiver operating characteristic curve in assessing the diagnostic accuracy of sST2 at discharge for death or heart failure readmission within 3 months after hospital discharge.
Table 3. The area under curves of ST2 and BNP at admission and at discharge to predict death or heart failure readmission within 3 months after hospital discharge.
| Variables | All patients (n=66) | Mild renal insufficiency (n=23) | Moderate renal insufficiency (n=26) | Severe renal insufficiency (n=17) | ||||
|---|---|---|---|---|---|---|---|---|
| AUC (95% CI) | P | AUC (95% CI) | P | AUC (95% CI) | P | AUC (95% CI) | P | |
| sST at admission | 0.680 (0.539-0.821) | 0.024 | 0.825 (0.589-1.000) | 0.077 | 0.667 (0.428-0.905) | 0.169 | 0.614 (0.340-0.888) | 0.435 |
| sST at discharge | 0.761 (0.641-0.882) | 0.001 | 0.965 (0.887-1.000) | 0.011 | 0.778 (0.594-0.961) | 0.022 | 0.629 (0.358-0.899) | 0.380 |
| BNP at admission | 0.600 (0.445-0.754) | 0.210 | 0.456 (0.132-0.781) | 0.811 | 0.703 (0.501-0.904) | 0.095 | 0.543 (0.213-0.872) | 0.770 |
| BNP at discharge | 0.747 (0.627-0.867) | 0.002 | 0.825 (0.636-1.000) | 0.077 | 0.732 (0.535-0.929) | 0.056 | 0.586 (0.296-0.875) | 0.558 |
| Delta-sST2 | 0.549 (0.381-0.717) | 0.535 | 0.333 (0.000-0.867) | 0.363 | 0.565 (0.313-0.817) | 0.590 | 0.564 (0.283-0.846) | 0.661 |
| Delta-BNP | 0.481 (0.316-0.645) | 0.806 | 0.246 (0.000-0.515) | 0.165 | 0.614 (0.385-0.844) | 0.346 | 0.457 (0.141-0.773) | 0.770 |
AUC, Area under curve; CI,Confidence interval; Delta-sST2, sST2 at admission minus sST2 at discharge; Delta-BNP, BNP at admission minus BNP at discharge.
DISCUSSION
In the present study, sST2 levels were not significantly changed according to the degree of renal dysfunction compared with BNP levels. In addition, sST2 levels were correlated with BNP levels with acute HF patients with mild to moderate renal insufficiency, not with severe renal insufficiency. These findings raised the questions whether sST2 might be superior to BNP in predicting prognosis in patients hospitalized with acute decompensated HF and severe renal insufficiency. Our result showed that sST2 at discharge was independently associated with the development of death or HF readmission within 3 months after hospital discharge.
Measurement of BNP levels has been used to establish a diagnosis of HF, especially in an uncertain situation, and determine the level of disease severity in the context of hospitalization with acute decompensated HF (12). However, the elevated plasma levels of BNP have been known to be associated with various cardiac and noncardiac causes. Among them, the change of renal function has been known as one of the confounding factors. Considering the physiological mechanism of BNP clearance, it may be an inevitable result that BNP levels were changed in accordance with renal insufficiency (13). In particular, interpretation of BNP levels may be more complicated in acute HF decompensated event in which changes of renal function is diverse. Even though the confounding of renal insufficiency, BNP levels were thought to be valuable in diagnosing HF and establishing prognosis in patients with renal insufficiency (3, 5). However, the optimum cutpoint for BNP to diagnose HF may be various according to the degree of renal insufficiency and especially greater than in normal renal function suggesting a wide range of values. Moreover, BNP levels may be dependent on volume-related factors in renal insufficiency (14). These concerns make the use of BNP more difficult in acute HF patients with renal insufficiency.
sST2 is a soluble form of the protein ST2 which is an interleukin-1 receptor family member (9). Circulating concentrations of sST2 are elevated in various clinical situations related to inflammation such as systemic lupus erythematosus, asthma, trauma, and septic shock (15, 16). Furthermore, it is released in cardiovascular tissue in response to biomechanical overload in a similar way to BNP secretion (8). Thus, this emerging biomarker has been investigated for the purpose of predicting prognosis. Studies have shown the prognostic role of sST2 in patients withchronic HF or acute myocardial infarction (9, 10). In addition, previous data suggest that sST2 could be prognostically informative in patients with acute HF (17). However, sST2 has not been examined in patients hospitalized with acute HF and combined with renal insufficiency, and there is limited information on their association with existing biomarkers such as BNP levels.
This study evaluated the change in circulating concentrations of sST2 with the degree of renal dysfunction and there were no differences in sST2 levels, even though BNP level was much higher in patients with severe renal insufficiency. A previous investigation showed that sST2 was elevated in chronic kidney disease patients and correlated with disease severity (18). However, this study did not assess cardiac function. Thus, unmeasured cardiac function may confound the association between sST2 levels and severity of renal insufficiency. Controversy still exists regarding the change of sST2 levels according to renal insufficiency. Nevertheless, recent data demonstrated that sST2 levels were not influenced by renal function and its prognostic value was also preserved in chronic HF patients with renal insufficiency (11). Surprisingly, the study results were in close agreement with our results in terms of independency of sST2 levels by renal function and the usefulness for prognosis prediction. However, our study included patients hospitalized with acute HF in which renal function may be changed more dynamically. Besides, we measured both sST2 and BNP levels at two timepoints to estimate their prognostic values in different clinical situations. Our results showed that sST2 levels at discharge were more useful to predict short-term clinical events.
There have been some reports about the role of sST2 in patients hospitalized with acute HF. Rehman and colleagues showed that sST2 at presentation strongly predicted mortality and had synergistic effects with natriuretic peptides (17). Moreover, a few studies investigated the role of serial sampling of sST2 in patients with acute HF. Boisot and colleagues measured sST2 up to 6 days between admission and discharge and showed that a rise in sST2 was related with worst short-term outcomes, independent of natriuretic peptide levels (19). Recently, Breithardt and colleagues showed the change of sST2 levels during the first 48 hr after admission was associated with mortality (20). These results were different from our results highlighting the role of sST2 at discharge. However, data from serial sampling equally indicated that a considerable amount of sST2 at admission changed at discharge and eventually less decrease in sST2 levels during hospitalization was associated with poorer outcomes. Actually, sST2 levels at presentation may be more affected by active inflammation from decompensated HF than at discharge. Besides, mechanical strain of cardiac tissues may be more prominent at admission, especially in patients with severe renal insufficiency because they are usually more vulnerable to volume overload. Therefore, sST2 levels at discharge may reflect hemodynamic stability and decrease in LV filling pressure after acute treatment and predict prognosis more powerfully than sST2 levels at admission or BNP levels. Even though the usefulness of sST2-guided therapy for acute decompensated HF with renal insufficiency is yet to be determined, sST2 levels at discharge may be valuable because it could give reference values for next readmission compared with sST2 levels at presentation.
The number of patients in the study population was relatively small and consisted of subjects from a single center. Thus, small number of subjects may make the role of sST2 statistically insignificant in patients with severe renal insufficiency. In addition, serial measurement of sST2 levels at outpatient department may be more helpful to compare the prognostic power in those patients. However, it may be a field of chronic HF and already shown in a recent study (11). Moreover, it was not analyzed whether patients with renal insufficiency already have chronic kidney disease before hospitalization or not. It may be unavoidable because some patients were diagnosed as de novo HF.
In conclusion, the current study documented that sST2 levels were not affected by renal function compared with BNP in patients hospitalized with acute HF. The measurement of sST2 levels at discharge can be helpful in predicting short-term outcomes in acute decompensated HF patients with renal insufficiency suggesting its informative role compared with BNP levels.
Footnotes
DISCLOSURE: The authors have no relevant financial relationships or potential conflicts of interest to disclose regarding the material discussed in this manuscript.
AUTHOR CONTRIBUTION: Conception and coordination of the study: Kim MS, Kim JJ. Design of ethical issues: Kim MS, Kim JJ. Acquisition of data: Kim MS, Jeong TD, Min WK, Kim JJ. Statistical analysis: Han SB. Manuscript preparation: Kim MS, Han SB, Kim JJ. Manuscript approval: Kim MS, Jeong TD, Han SB, Min WK, Kim JJ.
References
- 1.Levin ER, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med. 1998;339:321–328. doi: 10.1056/NEJM199807303390507. [DOI] [PubMed] [Google Scholar]
- 2.Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007;50:2357–2368. doi: 10.1016/j.jacc.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 3.Anwaruddin S, Lloyd-Jones DM, Baggish A, Chen A, Krauser D, Tung R, Chae C, Januzzi JL., Jr Renal function, congestive heart failure, and amino-terminal pro-brain natriuretic peptide measurement: results from the ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) Study. J Am Coll Cardiol. 2006;47:91–97. doi: 10.1016/j.jacc.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 4.Richards M, Nicholls MG, Espiner EA, Lainchbury JG, Troughton RW, Elliott J, Frampton CM, Crozier IG, Yandle TG, Doughty R, et al. Christchurch Cardioendocrine Research Group; Australia-New Zealand Heart Failure Group. Comparison of B-type natriuretic peptides for assessment of cardiac function and prognosis in stable ischemic heart disease. J Am Coll Cardiol. 2006;47:52–60. doi: 10.1016/j.jacc.2005.06.085. [DOI] [PubMed] [Google Scholar]
- 5.McCullough PA, Duc P, Omland T, McCord J, Nowak RM, Hollander JE, Herrmann HC, Steg PG, Westheim A, Knudsen CW, et al. Breathing Not Properly Multinational Study Investigators. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis. 2003;41:571–579. doi: 10.1053/ajkd.2003.50118. [DOI] [PubMed] [Google Scholar]
- 6.Cataliotti A, Malatino LS, Jougasaki M, Zoccali C, Castellino P, Giacone G, Bellanuova I, Tripepi R, Seminara G, Parlongo S, et al. Circulating natriuretic peptide concentrations in patients with end-stage renal disease: role of brain natriuretic peptide as a biomarker for ventricular remodeling. Mayo Clin Proc. 2001;76:1111–1119. doi: 10.4065/76.11.1111. [DOI] [PubMed] [Google Scholar]
- 7.Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest. 2007;117:1538–1549. doi: 10.1172/JCI30634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinberg EO, Shimpo M, De Keulenaer GW, MacGillivray C, Tominaga S, Solomon SD, Rouleau JL, Lee RT. Expression and regulation of ST2, an interleukin-1 receptor family member, in cardiomyocytes and myocardial infarction. Circulation. 2002;106:2961–2966. doi: 10.1161/01.CIR.0000038705.69871.D9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shimpo M, Morrow DA, Weinberg EO, Sabatine MS, Murphy SA, Antman EM, Lee RT. Serum levels of the interleukin-1 receptor family member ST2 predict mortality and clinical outcome in acute myocardial infarction. Circulation. 2004;109:2186–2190. doi: 10.1161/01.CIR.0000127958.21003.5A. [DOI] [PubMed] [Google Scholar]
- 10.Weinberg EO, Shimpo M, Hurwitz S, Tominaga S, Rouleau JL, Lee RT. Identification of serum soluble ST2 receptor as a novel heart failure biomarker. Circulation. 2003;107:721–726. doi: 10.1161/01.cir.0000047274.66749.fe. [DOI] [PubMed] [Google Scholar]
- 11.Bayes-Genis A, Zamora E, de Antonio M, Galán A, Vila J, Urrutia A, Diez C, Coll R, Altimir S, Lupón J. Soluble ST2 serum concentration and renal function in heart failure. J Card Fail. 2013;19:768–775. doi: 10.1016/j.cardfail.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, et al. American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–e327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 13.Khalifeh N, Haider D, Hörl WH. Natriuretic peptides in chronic kidney disease and during renal replacement therapy: an update. J Investig Med. 2009;57:33–39. doi: 10.2310/JIM.0b013e318194f44b. [DOI] [PubMed] [Google Scholar]
- 14.Tagore R, Ling LH, Yang H, Daw HY, Chan YH, Sethi SK. Natriuretic peptides in chronic kidney disease. Clin J Am Soc Nephrol. 2008;3:1644–1651. doi: 10.2215/CJN.00850208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brunner M, Krenn C, Roth G, Moser B, Dworschak M, Jensen-Jarolim E, Spittler A, Sautner T, Bonaros N, Wolner E, et al. Increased levels of soluble ST2 protein and IgG1 production in patients with sepsis and trauma. Intensive Care Med. 2004;30:1468–1473. doi: 10.1007/s00134-004-2184-x. [DOI] [PubMed] [Google Scholar]
- 16.Dieplinger B, Januzzi JL, Jr, Steinmair M, Gabriel C, Poelz W, Haltmayer M, Mueller T. Analytical and clinical evaluation of a novel high-sensitivity assay for measurement of soluble ST2 in human plasma--the Presage ST2 assay. Clin Chim Acta. 2009;409:33–40. doi: 10.1016/j.cca.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 17.Rehman SU, Mueller T, Januzzi JL., Jr Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol. 2008;52:1458–1465. doi: 10.1016/j.jacc.2008.07.042. [DOI] [PubMed] [Google Scholar]
- 18.Bao YS, Na SP, Zhang P, Jia XB, Liu RC, Yu CY, Mu SH, Xie RJ. Characterization of interleukin-33 and soluble ST2 in serum and their association with disease severity in patients with chronic kidney disease. J Clin Immunol. 2012;32:587–594. doi: 10.1007/s10875-011-9622-7. [DOI] [PubMed] [Google Scholar]
- 19.Boisot S, Beede J, Isakson S, Chiu A, Clopton P, Januzzi J, Maisel AS, Fitzgerald RL. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J Card Fail. 2008;14:732–738. doi: 10.1016/j.cardfail.2008.06.415. [DOI] [PubMed] [Google Scholar]
- 20.Breidthardt T, Balmelli C, Twerenbold R, Mosimann T, Espinola J, Haaf P, Thalmann G, Moehring B, Mueller M, Meller B, et al. Heart failure therapy-induced early ST2 changes may offer long-term therapy guidance. J Card Fail. 2013;19:821–828. doi: 10.1016/j.cardfail.2013.11.003. [DOI] [PubMed] [Google Scholar]