Abstract
Objective
To determine the prevalence of and risk factors for postprandial hypoglycemic symptoms among bariatric surgery patients.
Design and Methods
A questionnaire including the Edinburgh hypoglycemia scale was mailed to patients who underwent either Roux-en-Y gastric bypass (RYGB) or vertical sleeve gastrectomy (VSG) at a single center. Based on the questionnaire, we categorized the patients as having high or low suspicion for post-surgical, postprandial hypoglycemic symptoms.
Results
Of the 1119 patients with valid addresses, 40.2% (N=450) responded. Among the respondents, 34.2% had a high suspicion for symptoms of post-bariatric surgery hypoglycemia. In multivariate analyses, in addition to female sex (p=0.001), RYGB (p=0.004), longer time since surgery (p=0.013), lack of diabetes (p=0.040), the high suspicion group was more likely to report preoperative symptoms of hypoglycemia (p<0.001), compared to the low suspicion group. Similar results were observed when the high suspicion group was restricted to those requiring assistance from others, syncope, seizure with severe symptoms or medically confirmed hypoglycemia (N=52).
Conclusion
One third of RYGB or VSG reported postprandial symptoms concerning for post-surgical hypoglycemia, which was related to the presence of pre-operative hypoglycemic symptoms. Pre-operative screening for hypoglycemic symptoms may identify a group of patients at increased risk of post-bariatric surgery hypoglycemia.
Keywords: Bariatric surgery, gastric bypass, glucose metabolism, treatment outcomes, questionnaire design
Introduction
Bariatric surgery is an effective treatment for obesity, which is associated with a significant reduction in mortality and obesity-related comorbidities such as diabetes and hypertension. 1,2 While the favorable outcomes and safety profile of bariatric surgery has led to its rising utilization in the United States and worldwide, the metabolic and nutritional complications of bariatric surgery are also becoming increasingly recognized.3
Hypoglycemia after bariatric surgery is a metabolic complication associated with inappropriate secretion of insulin and gut hormones, which is particularly associated with Roux-en-Y gastric bypass surgery (RYGB). 4-6 Also known as late dumping syndrome, post-bariatric surgery hypoglycemia differs from the early dumping syndrome in its delayed onset of 1-2 hours after a meal without vasomotor symptoms. 7 Unlike hypoglycemia related to insulinoma or sulfonylurea occurring both at fasting and fed state, post-bariatric surgery hypoglycemia occurs almost exclusively postprandially starting 6 months or greater following surgery. 8 Severe post-bariatric surgery hypoglycemia is rare but potentially devastating with reports of associated seizure, syncope and motor vehicle accidents. 4,5 The mechanism behind post-bariatric surgery hypoglycemia is poorly understood; Several proposed etiologies include 1) presurgical hypertrophy of the β cells leading to their hyperfunction, 2) inappropriate hypersecretion of incretin hormones such as glucagon-like peptide (GLP)-1, 3) abnormality in counterregulatory hormones such as glucagon and 4) rapid improvement in insulin sensitivity after weight loss. 9-11 While most cases can be managed with a low-carbohydrate diet, some cases require medical therapies such as acarbose and diozoxide and extreme cases can require surgical therapies such as partial or total pancreatectomy, reduction of gastric pouch size and reversal of gastric bypass. 5,12-14
Currently, there are limited and contrasting reports regarding the prevalence of post-bariatric surgery hypoglycemia. Severe hypoglycemia after bariatric surgery appears rare, with less than 1% prevalence based on hospitalization records or clinic visits for hypoglycemia leading to neuroglycopenic symptoms such as confusion, syncope and seizure. 12,15 Another study based on the Bariatric Outcomes Longitudinal Database (BOLD) similarly reported less than 0.1% incidence of severe hypoglycemia based on self-report following gastric bypass and even lower incidence after sleeve gastrectomy and gastric banding. 16 In contrast, mild to moderate hypoglycemia appears to be much more common. Up to one third of subjects with a history of RYGB and no history of hypoglycemia developed asymptomatic hypoglycemia during mixed meal challenge or continuous glucose monitoring. 17,18 The discrepancy in the prevalence of post-bariatric surgery hypoglycemia in the literature highlights the need for its further evaluation, including risk factors associated with its development.
In order to determine the prevalence of hypoglycemic symptoms and associated risk factors among bariatric surgery patients, we conducted a questionnaire in patients who underwent Roux-en-Y gastric bypass surgery or vertical sleeve gastrectomy at our bariatric surgery center.
Methods
Subject/ Study Design
Between August 2013 to April 2014 we conducted a mailed survey of 1174 patients who had undergone either RYGB or VSG at the Johns Hopkins Center for Bariatric Surgery between August 2008 and August 2012. The Institutional Review Board of the Johns Hopkins Hospital exempted the study from further review. Consent was assumed by the completion of the questionnaire.
Data Collection
In August 2013, we mailed questionnaires to 1174 subjects with a $2 bill enclosed as incentive. We asked each subject to complete the questionnaire either on paper or online. A total of 55 patients did not have valid addresses and were excluded from the study. Through April 2014, multiple attempts were made to follow up with each subject using 2 additional questionnaire mailings and 2 reminder postcards.
Questionnaire Design
The questionnaire was adapted from Edinburgh hypoglycemia questionnaire, which identified and validated 11 key symptoms underlying hypoglycemia (Supplementary Figure 1). 19 These symptoms include sweating, palpitation, shaking, hunger, confusion, drowsiness, odd behavior, speech difficulty, incoordination, nausea and headache. We asked the respondent “have you felt any of the [above-mentioned] symptoms within 5 hours after eating?” If the respondent answered yes to any of the symptoms, he or she was asked additional questions regarding the onset of symptom(s) in relation to the meal, frequency, previous experience with and awareness of hypoglycemia, prior diagnosis of hypoglycemia and any severe episode of hypoglycemia requiring assistance from others. Respondents were asked whether the symptoms of hypoglycemia were new since the bariatric surgery. We also collected data on bariatric surgery history, current dietary history, presurgical weight, current weight and height of the respondent. Respondents with diabetes were asked to provide further information including the duration of diabetes, current medication and current hemoglobin A1c.
Each respondent who completed the questionnaire was categorized into either a low or high suspicion group for symptoms of post-bariatric hypoglycemia. The group with low suspicion of hypoglycemia symptoms was defined as those with 0-2 postprandial symptoms of hypoglycemia following bariatric surgery, whereas the group with high suspicion of hypoglycemia symptoms was defined as those with 3 or more symptoms of postprandial hypoglycemia following bariatric surgery or a history of requiring assistance, seizure or medical diagnosis of hypoglycemia. We performed two sensitivity analyses based on: i) defining the high suspicion group as those with a history of severe hypoglycemia requiring assistance and or medically confirmed hypoglycemia or ii) those with a history of severe hypoglycemia as above and/or neuroglycopenic symptoms (confusion, drowsiness, odd behavior, speech difficulty or incoordination/clumsiness) after surgery.
Our primary outcome was the percentage of patients who reported high suspicion of symptoms of hypoglycemia following RYGB or VSG.
Statistical analysis
Chi squared or ANOVA tests were used to compare clinical characteristics such as pre-surgery BMI, amount of weight loss following the surgery, diabetes status/duration/severity, prior history of hypoglycemia, dietary pattern and dietary compliance of those in the high versus low suspicion group. To determine factors that were independently associated with post-bariatric surgery hypoglycemic symptoms, we used multivariable logistic regression. The variables with statistically significant difference between the high and low suspicion group were included in the final logistic regression model. All analyses were performed using Stata version 12 (College Station, Tx).
Results
Among 1119 patients with a valid address who were mailed the questionnaire, a total of 450 (40.2%) respondents completed the questionnaire. Demographics and clinical characteristics of the questionnaire respondents are presented in Table 1. The sample was predominantly middle-aged Caucasian women (71.6%) with no prior history of diabetes (64%) who underwent RYGB (78.9%). Respondents (n=450) were somewhat older and more likely to live outside of Baltimore city than non-respondents (n=724) (Supplemental Table 1). Regarding the frequency of each of the 11 key symptoms of hypoglycemia included in the questionnaire, neuroglycopenic symptoms such as confusion, odd behavior and speech difficulty occurred less often compared to autonomic or malaise-related symptoms (Table 2).
Table 1. Characteristics of the Survey Respondents (N=450).
| Mean | SD | |
|---|---|---|
| Age (years) | 50.8 | 11.2 |
| Gender | ||
| Female | 355 (79.0%) | |
| Male | 95 (21.0%) | |
| Race | ||
| Caucasian | 322 (71.6%) | |
| Non-Caucasian | 128 (28.4%) | |
| Type of surgery | ||
| RYGB | 355 (78.9%) | |
| VSG | 95 (21.1%) | |
| Number of years since surgery | 3.3 | 1.3 |
| Excess weight loss since surgery (%) | 80.3 | 25.3 |
| Current BMI (kg/m2)* | 32.6 | 7.4 |
| History of diabetes | 162 (36.0%) | |
| Adherence to diet after surgery** | ||
| Always | 27 (6.1%) | |
| Very often | 161 (36.2%) | |
| Sometimes | 155 (34.8%) | |
| Rarely | 71 (16.0%) | |
| Never | 31 (7.0%) |
RYGB: Roux-en-Y gastric bypass, VSG: vertical sleeve gastrectomy
Excess weight loss was calculated as (preoperative weight – lowest postoperative weight)/ (preoperative weight – ideal weight based on goal BMI of 25 kg/m2)
5 missing,
6 missing
Table 2. The frequency of each of the 11 symptoms of hypoglycemia after bariatric surgery.
| Post-bariatric surgery Symptoms of Hypoglycemia | N (%) | |
|---|---|---|
| Autonomic | Sweating | 147 (32.6%) |
| Palpitation | 101 (22.4%) | |
| Shaking | 162 (36.0%) | |
| Hunger | 105 (23.0%) | |
|
| ||
| Neuroglycopenic | Confusion | 47 (10.4%) |
| Drowsiness | 96 (21.3%) | |
| Odd behavior | 40 (8.0%) | |
| Speech difficulty | 19 (4.2%) | |
| Incoordination | 45 (10.0%) | |
|
| ||
| Malaise | Nausea | 132 (29.3%) |
| Headache | 49 (10.8%) | |
Among the respondents, a total of 34% (154/450) reported symptoms that were highly suspicious for post-bariatric surgery hypoglycemia. Compared to the low suspicion group, the high suspicion group included significantly more females (89.0% versus 74.3%), RYGB surgeries (89.0% versus 73.7%), reported a longer time since surgery (3.6 versus 3.2 years), more excess weight loss (86.5% versus 77.1%), and more moderate to severe preoperative symptoms of hypoglycemia (31.1% versus 16.6%) (Table 3).
Table 3. Characteristics of 450 Individuals by the status of symptoms of hypoglycemia after bariatric surgery.
| High suspicion for hypoglycemia (N=154) |
Low suspicion for hypoglycemia (N=296) |
P-value | |
|---|---|---|---|
| Race | 0.052 | ||
| Caucasian | 119 (77.3%%) | 203 (68.6%) | |
| Non-Caucasian | 35 (22.7%) | 93 (31.4%) | |
| Sex | <0.001 | ||
| Male | 17 (11.0%) | 76 (25.7%) | |
| Female | 137 (89.0%) | 220 (74.3%) | |
| Age (year) | 0.039 | ||
| Mean (SD) | 48.9 (11.3) | 51.2 (11.2) | |
| Type of surgery | <0.001 | ||
| RYGB | 137 (89.0%) | 218 (73.7%) | |
| VSG | 17 (11.0%) | 78 (26.3%) | |
| Years since surgery | 0.002 | ||
| Mean (SD) | 3.6 (1.3) | 3.2 (1.3) | |
| Percent EWL from surgery | <0.001 | ||
| Mean (SD) | 86.5 (22.9) | 77.1 (26.0) | |
| Pre-existing Diabetes | 0.081 | ||
| No | 107 (69.5%) | 181 (61.2%) | |
| Yes | 47 (30.5%) | 115 (38.8%) | |
| Preoperative Weight | 0.143 | ||
| In pound, Mean (SD) | 296.8 (67.4) | 307.3 (74.3) | |
| Dietary adherence* | 0.218 | ||
| Always/ very often | 60 (39.0%) | 128 (44.0%) | |
| Sometimes | 52 (33.8%) | 103 (35.4%) | |
| Never/ seldom | 42 (27.2%) | 60 (20.6%) | |
| Preoperative Symptoms of Hypoglycemia | <0.001 | ||
| None | 73 (47.4%) | 146 (49.3%) | |
| Mild | 33 (21.5%) | 101 (34.1%) | |
| Moderate | 31 (20.1%) | 41 (13.9%) | |
| Severe | 17 (11.0%) | 8 (2.7%) |
The unadjusted results showed female gender (OR=2.8; 95% CI:1.6,4.9), RYGB (OR=2.9, 95% CI:1.6, 5.1), excess weight loss (OR=1.4, 95% CI:1.2, 1.7), a longer time since surgery (OR=1.4, 95% CI:1.1, 1.6), and presence of preoperative symptoms of hypoglycemia (OR=1.3, 95% CI:1.1, 1.6) were each associated with high suspicion for symptoms of post-bariatric hypoglycemia. After multivariable adjustment, our results showed that female gender, RYGB, a longer time since surgery, presence of preoperative symptoms of hypoglycemia and lack of history of diabetes were factors independently associated with high suspicion for symptoms of post-bariatric hypoglycemia (Figure 1A).
Figure 1.
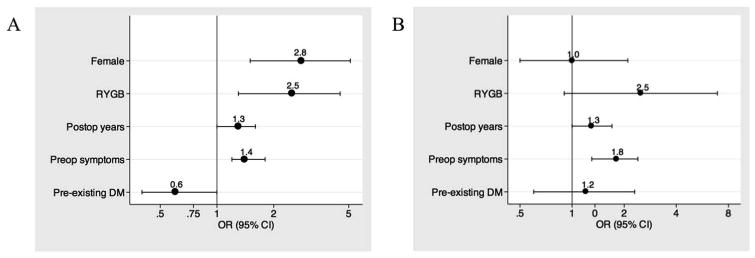
Odds of post-bariatric surgery hypoglycemic symptoms in (A) high suspicion group* (N=154) compared to those not in the high suspicion group and in (B) those with severe or medically confirmed hypoglycemia (N=52) compared to those without such history
*High suspicion group: Those with 3 or more symptoms of hypoglycemia or a history of severe hypoglycemia requiring assistance, seizure or medical diagnosis of hypoglycemia following bariatric surgery
When we defined the high suspicion group as those with a history of severe hypoglycemia requiring assistance (N=35) and/or medically confirmed hypoglycemia (N=32) only, those with pre-operative symptoms of hypoglycemia were still more likely to have post-operative, post-prandial hypoglycemic symptoms (OR, 1.8, 95%CI: 1.3, 2.4) (Figure 1B). While RYGB appeared to confer some increased risk (OR 2.5, 95% CI: 0.9, 6.9), women were no more likely than men to report these symptoms (OR 1.0, 95%CI: 0.5, 2.1). Similar results were seen when the definition of high suspicion was changed to those with a history of severe hypoglycemia and/or neuroglycopenic symptoms (confusion, drowsiness, odd behavior, speech difficulty or incoordination/clumsiness), (N=52) of hypoglycemia after surgery (pre-operative symptoms of hypoglycemia (OR 1.7, 95%CI, 1.3, 2.1), RYGB (OR 2.5, 95% CI 1.3, 4.5)).
Discussion
Post-bariatric surgery hypoglycemia is a complication after bariatric surgery whose prevalence and associated risk factors are incompletely understood. We found that post-bariatric surgery hypoglycemic symptoms affect up to 34% of patients who underwent bariatric surgery and responded to our questionnaire. Our finding is similar to a recent study of 15 RYGB patients, which found asymptomatic hypoglycemia in over a third of these patients using a continuous glucose monitor. 18 A similar study of 6 RYGB patients without any history of hypoglycemia showed that 50% had asymptomatic hypoglycemia on continuous glucose monitor and 60% on mixed meal tolerance test. 17 On the other hand, our finding contrasts with that of studies focused on severe hypoglycemia, which reported less than 1% prevalence of postgastric bypass hypoglycemia based on hospitalization records, clinic visits or large bariatric surgery database for hypoglycemia. 12,15,16 When we restricted our definition to those who reported more severe symptoms of post-prandial hypoglycemia, including those requiring assistance from others, or those with syncope, seizure or medically confirmed hypoglycemia (N=52), we found a prevalence of 11.6%, and that preoperative symptoms of hypoglycemia was the only significant correlate of post-bariatric surgery hypoglycemic symptoms.
The fact that post-bariatric surgery hypoglycemia is often hard to recognize and not systemically monitored among post-bariatric surgery patients suggests that the results of these large database studies based on hospitalization, clinic visit or self-report of hypoglycemia may be an underestimate of the true prevalence. To add to the challenge, post-bariatric surgery hypoglycemia can occur without any symptoms, as demonstrated in studies using the continuous glucose monitor. 17,18 While severe hypoglycemia, which can lead to dangerous clinical consequences such as seizure, syncope and motor vehicle accidents, the clinical relevance of mild or asymptomatic hypoglycemia is less clear. 4,5 However, a recent study showed an increased risk of cardiac arrhythmia during hypoglycemia among insulin-treated patients with type 2 diabetes and another study demonstrated increased healthcare utilization and work-time loss associated with mild to moderate hypoglycemia. 20,21 As we begin to learn the harmful effects of asymptomatic hypoglycemia in addition to well-known harms of more severe hypoglycemia, more systemic screening for hypoglycemia in post-bariatric surgery patients may help clarify its true prevalence.
To our knowledge, this is the first study demonstrating a strong correlation between preoperative symptoms of hypoglycemia and post-bariatric surgery hypoglycemia as shown in our main analysis and confirmed in both of our sensitivity analyses. Interestingly, this association was independent from a history of pre-existing diabetes. Contrary to our expectation, pre-existing diabetes did not confer an elevated risk of post-bariatric surgery hypoglycemia. In fact, our data showed an elevated risk of post-bariatric surgery hypoglycemia among those without diabetes. This finding may suggest a role for screening the patients for symptoms of hypoglycemia prior to bariatric surgery regardless of their diabetes status in order to identify those at an elevated risk of developing post-bariatric surgery hypoglycemia. The presence of preoperative hypoglycemic symptoms may suggest enhanced insulin sensitivity in affected individuals that may later predispose them to the risk of developing further exaggerated insulin response and subsequent hypoglycemia following bariatric surgery.
We found additional clinical factors such as RYGB, female gender and number of years since surgery to be independently associated with symptoms of post-bariatric surgery hypoglycemia. RYGB is strongly correlated with post-bariatric surgery hypoglycemic symptoms in our study in conjunction with the findings of prior studies. 12,15,16,22. The risk of hypoglycemia after VSG is less well established and may be related to the fact that the procedure is new with less longitudinal outcome data. However, short-term data on VSG suggests up to 33% of patients have hypoglycemia upon oral glucose tolerance test postoperatively. 23 Both RYGB and VSG were shown to increase glucose-mediated GLP-1 secretion and to expedite gastric emptying time after surgery, which are thought to play key roles in increasing the risk of post-bariatric surgery hypoglycemia. 24,25. Time since surgery is another correlate of post-bariatric surgery hypoglycemia, confirming the late onset pattern of this phenomenon and the importance of its continued monitor after bariatric surgery.
The strengths of this study are large sample size, inclusion of both RYGB and VSG patients, and use of validated hypoglycemia questionnaire and clinical history of severe hypoglycemia. However, the 40.2% response rate to our questionnaire raises the likelihood of response bias, with more respondents perhaps having more symptoms of hypoglycemia to report. Even with the assumption that none of the non-respondents have symptoms of hypoglycemia, the proportion of patients with high suspicion for symptoms of post-bariatric surgery hypoglycemia would remain significant at 13.7% (154/1119). The respondents tended to be older and live outside Baltimore city, suggesting some socio-economic differences between the respondents and non-respondents (Supplementary Table 1). Due to the retrospective questionnaire design, we required questionnaire respondents to recall various symptoms years after the surgery, including before surgery. This increases the chances of not recognizing or remembering symptoms of hypoglycemia, especially among non-diabetic patients, which may underestimate the prevalence of post-bariatric surgery hypoglycemic symptoms. In addition, we do not have blood glucose data or medical records to confirm the reports of hypoglycemic symptoms, which raises the possibility of overestimating the true prevalence of post-bariatric surgery hypoglycemia, primarily based on symptomatology. The challenge of distinguishing between early and late dumping syndrome may also contribute to overestimating the prevalence of post-bariatric surgery hypoglycemia. However, we used a validated questionnaire, as well as reports of well-validated consequences or proof of hypoglycemia, and performed several sensitivity analyses, which strengthen our results. Finally, the study population was mostly female, middle-aged and Caucasian. While this is similar to many patients undergoing bariatric surgery in the US, our findings may not apply to men or non-Caucasian races.
In conclusion, post-bariatric surgery postprandial hypoglycemic symptoms appear to be common, affecting up to one third of patients who undergo bariatric surgery at our academic institution. The presence of preoperative symptoms of hypoglycemia appears to be the strongest indicator of elevated risk of post-bariatric surgery hypoglycemia regardless of preoperative diabetes status. While our study does not provide adequate evidence to counsel patients with preoperative symptoms of hypoglycemia against undergoing bariatric surgery, it does support the role for screening patients for symptoms of hypoglycemia prior to bariatric surgery in order to identify those at an elevated risk of developing post-bariatric surgery hypoglycemia. In turn, we may be better able to educate these individuals on recognizing hypoglycemic symptoms after surgery and if confirmed to have post-bariatric hypoglycemia, recommend interventions such as low-carbohydrate diet, which is an effective treatment in most cases. 12 Prospective studies that routinely measure blood sugar or collect symptoms real-time are warranted to better understand both the predictors and the clinical impact of post-bariatric surgery hypoglycemia.
Supplementary Material
Supplemental Table 1: Characteristics of the Survey Respondents (N=450) versus Non-responders (N=724)
Supplemental Figure 1: Hypoglycemic Symptoms Questionnaire
What is already known about the subject?
Post-Bariatric surgery hypoglycemia is an increasingly recognized complication associated with inappropriate secretion of insulin and gut hormones.
There are limited and contrasting reports regarding the prevalence of post-bariatric surgery hypoglycemia.
While severe hypoglycemia appears rare, non-severe hypoglycemia affects up to a third of patients who undergo gastric bypass.
What does this study add?
Between 14-34% of patients who underwent RYGB or VSG reported postprandial symptoms highly suspicious for post-bariatric surgery hypoglycemia.
Presence of pre-operative hypoglycemic symptoms was associated with post-bariatric surgery hypoglycemic symptoms.
Pre-operative screening for hypoglycemic symptoms may identify a group of patients at increased risk of post-bariatric surgery hypoglycemia.
Acknowledgments
Drs. Lee, Clark and Brown designed the study and performed data collection and analysis. Olivia Koerner performed data collection and data entry. Drs. Schweitzer, Magnuson and Steele carried out the study. All authors were involved in writing the paper and had final approval of submitted and published versions. The authors would like to thank the staff at the Johns Hopkins Pro Health for their help with questionnaire mail preparation, delivery and receipt, and Eva Kelly, the bariatric database coordinator, who provided access to patient data. This research was supported by Grant Number KL2 (5KL2TR001077-02) as part of the Institute for Clinical and Translational Research Grant from the NIH/NCAT and Julius Edlow MD grant from the Division of Endocrinology, Diabetes and Metabolism, the Johns Hopkins University.
Footnotes
Conflicts of interest: The authors have no competing interests.
References
- 1.Sjostrom L, Peltonen M, Jacobson P, Sjostrom C, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56–65. doi: 10.1001/jama.2011.1914. [DOI] [PubMed] [Google Scholar]
- 2.Courcoulas AP, Christian NJ, Belle SH, Berk P, Flum D, Garcia L, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310(22):2416–2425. doi: 10.1001/jama.2013.280928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J. Trends in use of bariatric surgery, 2003-2008. J Am Coll Surg. 2011;213(2):261–266. doi: 10.1016/j.jamcollsurg.2011.04.030. [DOI] [PubMed] [Google Scholar]
- 4.Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med. 2005;353(3):249–254. doi: 10.1056/NEJMoa043690. [DOI] [PubMed] [Google Scholar]
- 5.Patti ME, McMahon G, Mun EC, Bitton A, Holst J, Goldsmith J, et al. Severe hypoglycaemia post-gastric bypass requiring partial pancreatectomy: Evidence for inappropriate insulin secretion and pancreatic islet hyperplasia. Diabetologia. 2005;48(11):2236–2240. doi: 10.1007/s00125-005-1933-x. [DOI] [PubMed] [Google Scholar]
- 6.Goldfine AB, Mun EC, Devine E, Bernier R, Baz-Hecht M, Jones D, et al. Patients with neuroglycopenia after gastric bypass surgery have exaggerated incretin and insulin secretory responses to a mixed meal. J Clin Endocrinol Metab. 2007;92(12):4678–4685. doi: 10.1210/jc.2007-0918. [DOI] [PubMed] [Google Scholar]
- 7.Tack J, Arts J, Caenepeel P, De Wulf D, Bisschops R. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol. 2009;6(10):583–590. doi: 10.1038/nrgastro.2009.148. [DOI] [PubMed] [Google Scholar]
- 8.Won JG, Tseng HS, Yang AH, et al. Clinical features and morphological characterization of 10 patients with noninsulinoma pancreatogenous hypoglycaemia syndrome (NIPHS) Clin Endocrinol (Oxf) 2006;65(5):566–578. doi: 10.1111/j.1365-2265.2006.02629.x. [DOI] [PubMed] [Google Scholar]
- 9.Korner J, Bessler M, Inabnet W, Taveras C, Holst JJ. Exaggerated glucagon-like peptide-1 and blunted glucose-dependent insulinotropic peptide secretion are associated with roux-en-Y gastric bypass but not adjustable gastric banding. Surg Obes Relat Dis. 2007;3(6):597–601. doi: 10.1016/j.soard.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meier JJ, Butler AE, Galasso R, Butler PC. Hyperinsulinemic hypoglycemia after gastric bypass surgery is not accompanied by islet hyperplasia or increased beta-cell turnover. Diabetes Care. 2006;29(7):1554–1559. doi: 10.2337/dc06-0392. [DOI] [PubMed] [Google Scholar]
- 11.Cummings DE. Endocrine mechanisms mediating remission of diabetes after gastric bypass surgery. Int J Obes (Lond) 2009;33(Suppl 1):S33–40. doi: 10.1038/ijo.2009.15. [DOI] [PubMed] [Google Scholar]
- 12.Kellogg TA, Bantle JP, Leslie DB, Redmond J, Slusarek B, Swan T, et al. Postgastric bypass hyperinsulinemic hypoglycemia syndrome: Characterization and response to a modified diet. Surg Obes Relat Dis. 2008;4(4):492–499. doi: 10.1016/j.soard.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Halperin F, Patti ME, Goldfine AB. Glucagon treatment for post-gastric bypass hypoglycemia. Obesity (Silver Spring) 2010;18(9):1858–1860. doi: 10.1038/oby.2010.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clancy TE, Moore FD, Jr, Zinner MJ. Post-gastric bypass hyperinsulinism with nesidioblastosis: Subtotal or total pancreatectomy may be needed to prevent recurrent hypoglycemia. J Gastrointest Surg. 2006;10(8):1116–1119. doi: 10.1016/j.gassur.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Marsk R, Jonas E, Rasmussen F, Naslund E. Nationwide cohort study of post-gastric bypass hypoglycaemia including 5,040 patients undergoing surgery for obesity in 1986-2006 in sweden. Diabetologia. 2010;53(11):2307–2311. doi: 10.1007/s00125-010-1798-5. [DOI] [PubMed] [Google Scholar]
- 16.Sarwar H, Chapman WH, 3rd, Pender JR, Ivanescu A, Drake A, Pories W, et al. Hypoglycemia after roux-en-Y gastric bypass: The BOLD experience. Obes Surg. 2014;24(7):1120–1124. doi: 10.1007/s11695-014-1260-8. [DOI] [PubMed] [Google Scholar]
- 17.Halperin F, Patti ME, Skow M, Bajwa M, Goldfine AB. Continuous glucose monitoring for evaluation of glycemic excursions after gastric bypass. J Obes. 2011;2011 doi: 10.1155/2011/869536. 869536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Engstrom BE, Sundbrom M, Anders K. Continuous glucose measuring reveals frequent, and mainly unnoticed hypoglycemias after bariatric surgery. American Diabetes Association. 2014 Jun 14; [Google Scholar]
- 19.Deary IJ, Hepburn DA, MacLeod KM, Frier BM. Partitioning the symptoms of hypoglycaemia using multi-sample confirmatory factor analysis. Diabetologia. 1993;36(8):771–777. doi: 10.1007/BF00401150. [DOI] [PubMed] [Google Scholar]
- 20.Chow E, Bernjak A, Williams S, Fawdry R, Hibbert S, Freeman J, et al. Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk. Diabetes. 2014;63(5):1738–1747. doi: 10.2337/db13-0468. [DOI] [PubMed] [Google Scholar]
- 21.Geelhoed-Duijvestijn PH, Pedersen-Bjergaard U, Weitgasser R, Lahtela J, Jensen MM, Ostenson CG. Effects of patient-reported non-severe hypoglycemia on healthcare resource use, work-time loss, and wellbeing in insulin-treated patients with diabetes in seven european countries. J Med Econ. 2013;16(12):1453–1461. doi: 10.3111/13696998.2013.852098. [DOI] [PubMed] [Google Scholar]
- 22.Patti ME, Goldfine AB. Hypoglycaemia following gastric bypass surgery--diabetes remission in the extreme? Diabetologia. 2010;53(11):2276–2279. doi: 10.1007/s00125-010-1884-8. [DOI] [PubMed] [Google Scholar]
- 23.Papamargaritis D, Koukoulis G, Sioka E, Zachari E, Bargiota A, Zacharoulis D, et al. Dumping symptoms and incidence of hypoglycaemia after provocation test at 6 and 12 months after laparoscopic sleeve gastrectomy. Obes Surg. 2012;22(10):1600–1606. doi: 10.1007/s11695-012-0711-3. [DOI] [PubMed] [Google Scholar]
- 24.Laferrere B, Teixeira J, McGinty J, Tran H, Egger J, Colarusso A, et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab. 2008;93(7):2479–2485. doi: 10.1210/jc.2007-2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Braghetto I, Davanzo C, Korn O, Csendes A, Valladares H, Herrera E, et al. Scintigraphic evaluation of gastric emptying in obese patients submitted to sleeve gastrectomy compared to normal subjects. Obes Surg. 2009;19(11):1515–1521. doi: 10.1007/s11695-009-9954-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1: Characteristics of the Survey Respondents (N=450) versus Non-responders (N=724)
Supplemental Figure 1: Hypoglycemic Symptoms Questionnaire


