Abstract
Objective
The purpose of this study was to examine the association of intergenerational education and country of birth with waist circumference, metabolic syndrome, and type-2 diabetes among older adult Latinos in the United States.
Design and Methods
We used cross-sectional data from the Sacramento Area Latino Study on Aging, a cohort of older adult Mexican-American Latinos (mean age=70 years). At baseline, we measured waist circumference and assessed metabolic syndrome and diabetes according to established guidelines (N=1,789). We classified participants as US-born or foreign-born based on self-reported birth country. Participants reported their parents’ education level (≥6 years vs.<6) and their own educational attainment (≥12 years vs.<12).
Results
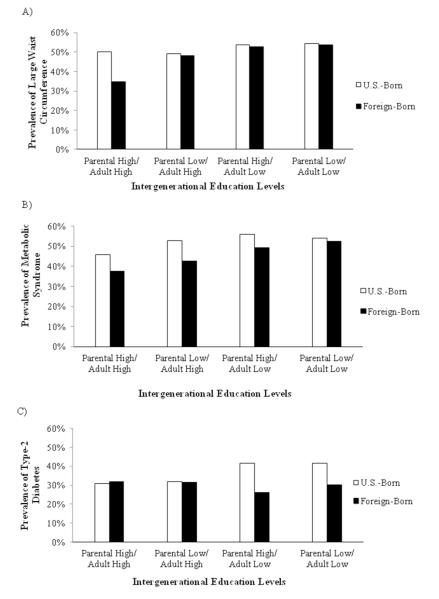
US-born participants who achieved high adult education, regardless of their parents’ education, had 37% lower odds of type-2 diabetes, compared to US-born participants with both low parental and personal education levels (e.g., multivariable-adjusted OR (Parental Low/Adult High)=0.63; 95%CI=0.40, 0.99). Among the foreign-born, only those with both high parental and high personal education levels had 55% lower odds of large waist circumference (OR=0.45; 95%CI=0.23, 0.88), compared to foreign-born participants with both low parental and personal education levels.
Conclusions
Intergenerational exposure to low education levels may increase central obesity and type-2 diabetes differentially among US-born and foreign-born Latinos.
Keywords: Diabetes, Education, Latinos, Nativity, Obesity, Social Mobility
Introduction
Rising obesity rates in older adults (aged 60 years or over) continue to be a major public health challenge for the United States [1]. Higher body mass index and waist circumference are associated with a two-fold increased risk of developing type-2 diabetes [2]. In the US, the incidence of type-2 diabetes doubled in the past decade and is highest among older adults [3]. With cardiovascular and metabolic diseases as the leading causes of death and health care costs in the US [4], the obesity epidemic among older adults has the potential to reduce recent gains in life expectancy in the US.
The obesity epidemic is exacerbated by marked socioeconomic, racial, and ethnic disparities [5], as US minority groups are disproportionately affected by this epidemic [5, 6]. Many Latinos, especially those of Mexican descent, have a higher prevalence of obesity, metabolic syndrome, and type-2 diabetes than non-Latino whites [7-9]. They also tend to experience suboptimal diabetes control and more frequent complications from diabetes [10]. Latinos are heterogeneous with respect to their immigration history (immigrant vs. born in the US) and to their motivation for immigration (e.g., attaining better economic status or education). This heterogeneity contributes to variations in the associations between social factors and health risks such as obesity, metabolic disorders, and type-2 diabetes among Latinos [11, 12].
One gap in the existing literature on the social determinants of obesity, metabolic syndrome, and type-2 diabetes in aging populations is that it has largely involved non-Latino white and black populations [13-21]. Furthermore, obesity, metabolic syndrome, and type-2 diabetes represent the culmination of inflammatory and other pathophysiologic risk factors that develop over long periods of time. Therefore, epidemiologic studies of older populations may miss critical windows of susceptibility in which intergenerational social factors influence long-term health risk. The present study expands the literature on social determinants of cardiovascular and metabolic health by examining how educational attainment across generations (parental education and personal educational attainment) and by country of birth (US-born vs. foreign-born) influences adult waist circumference, metabolic syndrome, and type-2 diabetes in a large epidemiological cohort of older adult Latinos in the US.
Methods
Study population
Participants included in this analysis were from the Sacramento Area Latino Study on Aging (SALSA). SALSA is a prospective cohort study of 1,789 community-dwelling older Mexican Americans residing in California’s Sacramento Valley and aged 60-101 years at baseline in 1998-1999. The study population and the recruitment of SALSA participants have been described elsewhere [22]. During home visits, we collected clinical data on participants and reported health conditions, lifestyle, and socio-demographic factors.
Measures
Assessment of waist circumference
We defined the waist as the midway point between the iliac crest and the lower rib. During baseline examination, we measured waist circumference (in inches) at the level of maximum indentation over the abdomen using a tape passed around the circumference. We identified maximum indentation by asking the participant to bend to one side and place their finger at the point where their body bent.
Assessment of metabolic syndrome and type-2 diabetes
We ascertained baseline metabolic syndrome based on the guidelines of the Third Adult Treatment Panel of the National Cholesterol Education Program [23] whereby participants had to meet at least three of the following five criteria: having abdominal obesity (waist circumference >35inches (88cm) in women; >40 inches (102 cm) in men), high triglycerides (≥150mg/dl), low HDL cholesterol (<50mg/dl in women; <40mg/dl in men), high blood pressure (systolic ≥130mmHg, diastolic ≥85mmHg), and high fasting glucose (≥100mg/dl). We measured glucose and lipid levels from fasting blood, and we measured systolic (SBP) and diastolic (DBP) blood pressure using a digital blood pressure monitor. We ascertained baseline type-2 diabetes as a fasting glucose level ≥126 mg/dl, a self-report of a physician diagnosis, or use of any diabetes medication.
Assessment of educational attainment across generations
We were specifically interested in educational attainment as our measure of socioeconomic status as it is potentially a modifiable risk factor in future populations. We asked SALSA participants to report how many years of school their mother and father completed: we classified maternal and paternal education levels as “low” if they had less than 6 years of education (i.e., did not complete elementary school) or “high” if they had 6 years of education or more (i.e., completed elementary school or beyond). We then chose the highest education of either the mother or the father as an indicator of parental education. We also obtained participants’ own education level by asking them how many years of school they completed: we classified the responses as “low” if they had less than 12 years of education (i.e., did not complete high school) or “high” if they had 12 years of education or more (i.e., completed high school or beyond). In line with prior SALSA publications [22], our choice of the education cut-points was driven by the data distribution in both generations of our SALSA cohort. We then created a four-level education measure representing the participants’ parental level of educational attainment and their own educational attainment as an adult: 1) “Low/Low”: low parental education and low adult education (referent category); 2) “High/Low”: high parental education but low adult education; 3) “Low/High”: low parental education but high adult education; and 4) “High/High”: high parental education and high adult education. These education groupings enabled us to easily translate interpretations about the influence of different levels of education across generations on adult disease outcomes.
Nativity
Nativity was based on participants’ report of their country of birth. Participants were classified as either US-born or foreign-born (in Mexico or another Central or South American country) before migrating to the US. A total of 51.1% of the participants were foreign-born, and nearly all (90%) of the immigrants were born in Mexico.
Other covariates
For foreign-born participants, we calculated “time since migration” as the difference between their age at enrollment in our study and their reported age at migration. We assessed depressive symptoms at baseline using the 20-item Epidemiologic Studies-Depression Scale (CES-D) (range 0 to 60); and we ascertained hypertension based on a self-report of a physician diagnosis, use of antihypertensive medication, a systolic blood pressure >140 mm Hg, and/or a diastolic blood pressure >90 mm Hg.
Statistical Analyses
This is a cross-sectional analysis of intergenerational educational attainment and the prevalence of large waist circumference, metabolic syndrome, and type-2 diabetes at baseline. We first compared baseline characteristics of the participants across the intergenerational four-level education measure using Chi-square tests for categorical variables and t-tests for continuous variables. We then used multivariable logistic regression models to examine the associations between the four-level intergenerational education measure and the prevalence of large waist circumference, metabolic syndrome, and type-2 diabetes. All regression analyses were performed separately for the US-born and foreign-born. At the multivariable level, we adjusted for age and gender and we included potential confounders based on a priori literature as well as the potential confounders’ established associations with education and each of the outcomes of interest. In regression models of the foreign-born, we additionally adjusted for time since migration as a potential confounder. We did not adjust for household income or occupation as they are largely determined by educational attainment and likely lie in the mediating pathway between educational attainment and adult disease. Furthermore, our measure of income was assessed in older age when most participants are retired and thus does not capture wealth or assets.
We performed the following sensitivity analyses. First, we conducted logistic regression models to examine the associations between the four-level intergenerational education measure and the prevalence of individual components of metabolic syndrome, using a separate model for each component. Second, we adjusted for childhood exposures including markers of food deprivation (how often participants did not have enough to eat while growing up) and childhood health (whether any of their siblings died in childhood). Third, to assess the potential for mediation of some of the behavioral risk factors in the pathways of interest, we adjusted for smoking, alcohol consumption, and physical activity. All P values were based on 2-sided tests. Statistical analyses were performed using SAS v.9.2.
Data imputation
Before data imputation, one-fourth of the participants had missing data at any point during the study time, including baseline. To accommodate missing data, a statistical team at the University of Michigan performed a sequential regression multivariate imputation (SRMI) approach for the entire SALSA dataset. This approach was conditioned on all observed variables as predictors, thus providing less biased estimates compared to other approaches such as the list-wise deletion [24]. The statistical team produced five imputations for the SALSA dataset using the Imputation and Variance Estimation Software. We summarized regression analyses using the “MIANALYZE” procedure in SAS. Details of the imputation technique are described elsewhere [22].
Results
Of participants who were born in the US (N=874), 25.2% had both high parental and personal education levels (High/High), 19.3% had parents with low education yet achieved high adult education personally (Low/High, upward social mobility), 22.5% had parents with a high education level but only attained low education levels personally (High/Low, downward social mobility), and 31.4% had both low parental and personal education levels (Low/Low). Of the foreign-born participants (N=908), the majority either had both low parental and personal education levels (48.6% Low/Low) or had parents with high education attainment but only attained low educational levels personally (35.5% High/Low, downward social mobility).
Among the US-born participants (Table 1), 56.6% were females. Mean baseline age was 70.1 years (SD=6.4) and participants completed a mean of 9 years of education (SD=4.9). A total of 37.3% had type-2 diabetes, and more than half had large waist circumference, high triglycerides, high fasting glucose, high blood pressure, and metabolic syndrome. US-born participants with high parental and personal levels of education (High/High) were significantly younger and less likely to have low HDL cholesterol, type-2 diabetes, hypertension, and depressive symptoms.
Table 1.
Distribution of Baseline Sample Characteristics by Intergenerational Education Level, Among the U.S.-born, SALSA (N=874)
| Parental education / adult education | ||||||
|---|---|---|---|---|---|---|
| Overall | High/High N=220 (25.2%) |
Low/High N=169 (19.3%) |
High/Low N=197 (22.5%) |
Low/Low N=274 (31.4%) |
P value | |
| Age at enrollment, mean (SD) | 70.1 (6.4) | 68.4 (5.6) | 68.0 (5.5) | 71.7 (6.8) | 71.3 (6.5) | <0.01 |
| Years of adult education, mean (SD) | 9.6 (4.9) | 14.2 (2.5) | 13.6 (2.2) | 6.3 (3.3) | 5.9 (3.3) | <0.01 |
| Years of parental education, mean (SD) | 5.2 (4.3) | 9.1 (2.9) | 2.2 (1.9) | 8.6 (2.7) | 1.4 (1.9) | <0.01 |
| Females, n (%) | 495 (56.6) | 107 (48.6) | 91 (53.9) | 119 (60.4) | 170 (62.0) | 0.01 |
| Health insurance, n (%) | 852 (97.5) | 216 (98.2) | 163 (96.5) | 190 (96.5) | 269 (98.2) | 0.47 |
| Type 2 diabetes, n (%) | 326 (37.3) | 68 (30.9) | 54 (32.0) | 82 (41.6) | 114 (41.6) | 0.02 |
| Metabolic syndrome, n (%) | 458 (52.4) | 101 (45.9) | 89 (52.7) | 110 (55.8) | 148 (54.0) | 0.18 |
| Large waist circumference, inches, n (%)a | 454 (52.0) | 110 (50.0) | 83 (49.1) | 106 (53.8) | 149 (54.4) | 0.62 |
| High triglycerides, mg/dl, n (%)a | 480 (54.9) | 117 (53.2) | 97 (57.4) | 108 (54.8) | 151 (55.1) | 0.88 |
| Low HDL cholesterol, mg/dl, n (%)a | 284 (32.5) | 58 (26.4) | 44 (26.0) | 77 (39.1) | 98 (35.8) | 0.01 |
| High fasting glucose, mg/dl, n (%)a | 446 (51.0) | 106 (48.2) | 84 (49.7) | 105 (53.3) | 144 (52.6) | 0.68 |
| High Blood pressure, n (%)a | 586 (67.1) | 140 (63.6) | 110 (65.1) | 139 (70.6) | 184 (67.2) | 0.48 |
| Depressive symptoms (0-60), mean (SD) | 8.6 (9.9) | 5.6 (8.2) | 6.7 (8.4) | 9.9 (10.7) | 11.1 (10.6) | <0.01 |
| Hypertension, n (%) | 554 (63.4) | 126 (57.3) | 97 (57.4) | 139 (70.6) | 178 (65.0) | 0.01 |
Abbreviations: HDL, High Density Lipoprotein; SALSA, Sacramento Area Latino Study on Aging.
Large waist circumference is >35inches for women and >40 inches for men; High triglycerides is ≥150mg/dl; Low HDL cholesterol is <50mg/dl for women and <40mg/dl for men; high fasting glucose is ≥100 mg/dl; high blood pressure is SBP ≥130 or DBP≥85.
Among the foreign-born participants (Table 2), 60.2% were females. Mean baseline age was 71.2 years (SD=6.4) and participants completed a mean of 5 years of education (SD=4.7). A total of 29.4% had type-2 diabetes. More than half had large waist circumference, high triglycerides, and high blood pressure. 49.9% had metabolic syndrome. Foreign-born participants with high parental and personal levels of education (High/High) were less likely to have large waist circumference, low HDL cholesterol, and depressive symptoms.
Table 2.
Distribution of Baseline Sample Characteristics by Intergenerational Education Level, Among the Foreign-born, SALSA (N=908)
| Parental education / adult education | ||||||
|---|---|---|---|---|---|---|
| Overall | High/ High N=72 (7.9%) |
Low/ High 54 (6.0%) |
High/ Low 322 (35.5%) |
Low/ Low 441 (48.6%) |
p-value | |
| Age at enrollment, mean (SD) | 71.2 (7.7) | 70.5 (7.4) | 71.3 (8.6) | 71.4 (7.9) | 70.9 (7.2) | 0.74 |
| Years of adult education, mean (SD) | 5.0 (4.7) | 14.4 (3.6) | 13.3 (1.6) | 4.0 (3.1) | 3.2 (3.0) | <0.01 |
| Years of parental education, mean (SD) | 4.8 (4.4) | 9.9 (4.1) | 2.5 (1.8) | 8.5 (2.7) | 1.4 (1.9) | <0.01 |
| Females, n (%) | 547 (60.2) | 40 (55.6) | 32 (59.3) | 194 (60.3) | 270 (61.2) | 0.84 |
| Health insurance, n (%) | 764 (84.1) | 67 (93.1) | 50 (92.6) | 267 (82.9) | 364 (82.5) | 0.04 |
| Type 2 diabetes, n (%) | 267 (29.4) | 23 (31.9) | 17 (31.5) | 84 (26.1) | 133 (30.2) | 0.56 |
| Metabolic syndrome, n (%) | 453 (49.9) | 27 (37.5) | 23 (42.6) | 159 (49.4) | 232 (52.6) | 0.08 |
| Large waist circumference, inches, n (%)a | 467 (51.4) | 25 (34.7) | 26 (48.2) | 170 (52.8) | 237 (53.7) | 0.02 |
| High triglycerides, mg/dl, n (%)a | 467 (51.4) | 39 (54.2) | 27 (50.0) | 153 (47.5) | 237 (53.7) | 0.37 |
| Low HDL cholesterol, mg/dl, n (%)a | 312 (34.4) | 15 (20.8) | 11 (20.4) | 106 (32.9) | 167 (37.9) | <0.01 |
| High fasting glucose, mg/dl, n (%)a | 401 (44.2) | 30 (41.7) | 26 (48.2) | 136 (42.2) | 197 (44.7) | 0.80 |
| High Blood pressure, n (%)a | 628 (69.2) | 46 (63.9) | 37 (68.5) | 228 (70.8) | 305 (69.2) | 0.72 |
| Depressive symptoms (0-60), mean (SD) | 11.3 (11.0) | 8.1 (10.1) | 8.7 (9.1) | 10.7 (10.7) | 12.3 (11.3) | <0.01 |
| Hypertension, n (%) | 556 (61.2) | 35 (48.6) | 37 (68.5) | 192 (59.6) | 281 (63.7) | 0.06 |
Abbreviations: HDL, High Density Lipoprotein; SALSA, Sacramento Area Latino Study on Aging.
Large waist circumference is >35inches for women and >40 inches for men; High triglycerides is ≥150mg/dl; Low HDL cholesterol is <50mg/dl for women and <40mg/dl for men; high fasting glucose is ≥100 mg/dl; high blood pressure is SBP ≥130 or DBP≥85.
For US-born participants, results from multivariable logistic regression models showed a significant education gradient in the prevalence of type-2 diabetes (p<0.05) (Table 3). In fully-adjusted models, US-born participants who achieved high adult education, regardless of their parents’ education, had significantly lower odds of type-2 diabetes (Parental High/Adult High: OR=0.63; 95% CI=0.41, 0.95; Parental Low/Adult High: OR=0.63; 95% CI=0.40, 0.99), compared to participants with both low parental and adult education levels. The education gradients in waist circumference and metabolic syndrome were not significant. Similarly, the education gradients in other components of metabolic syndrome (e.g., low HDL cholesterol and high fasting glucose) were not significant from logistic regression models (data not shown).
Table 3.
Multivariate Logistic Regression Models for the Associations Between Intergenerational Education Level and Prevalence of Large Waist Circumference, Metabolic Syndrome, and Type-2 Diabetes, SALSA.
| US-born | Foreign-bornd | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parental education /adult education (Ref=Low/Low) | Parental education /adult education (Ref=Low/Low) | |||||||||||
| High/ High | Low/ High | High/ Low | High/ High | Low/ High | High/ Low | |||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Large waist | ||||||||||||
| Unadjusted | 0.82 | 0.55, 1.20 | 0.81 | 0.55, 1.21 | 0.88 | 0.56, 1.39 | 0.44 * | 0.24, 0.80 | 0.87 | 0.47, 1.63 | 0.99 | 0.73, 1.34 |
| Adjusteda | 0.90 | 0.59, 1.37 | 0.86 | 0.57,1.31 | 0.89 | 0.56, 1.42 | 0.45 * | 0.23, 0.88 | 0.76 | 0.36, 1.59 | 0.95 | 0.66, 1.38 |
| Metabolic | ||||||||||||
| Unadjusted | 0.76 | 0.51, 1.13 | 1.01 | 0.65, 1.58 | 1.02 | 0.60, 1.72 | 0.52 * | 0.27, 1.00 | 0.79 | 0.34, 1.86 | 0.97 | 0.64, 1.48 |
| Adjustedb | 0.72 | 0.48, 1.08 | 0.90 | 0.57, 1.42 | 0.99 | 0.59, 1.64 | 0.60 | 0.32, 1.11 | 1.01 | 0.48, 2.11 | 0.94 | 0.61, 1.45 |
| Type-2 diabetes | ||||||||||||
| Unadjusted | 0.60 * | 0.41, 0.89 | 0.62 * | 0.41, 0.95 | 0.91 | 0.57, 1.44 | 1.12 | 0.55, 2.28 | 1.16 | 0.53, 2.53 | 0.94 | 0.64, 1.39 |
| Adjustedc | 0.63 * | 0.41, 0.95 | 0.63 * | 0.40, 0.99 | 0.95 | 0.58, 1.55 | 1.18 | 0.56, 2.51 | 1.43 | 0.67, 3.04 | 1.10 | 0.71, 1.69 |
Abbreviations: CI, Confidence Intervals; OR, Odds Ratio; SALSA, Sacramento Area Latino Study on Aging.
P<0.05.
Adjusted for age, gender, diabetes, hypertension, and depressive symptoms.
Adjusted for age, gender, and depressive symptoms.
Adjusted for age, gender, large waist circumference, hypertension, and depressive symptoms.
All models for the foreign-born are adjusted for time since migration to the United States.
For foreign-born participants (Table 3), there was a significant education gradient in the prevalence of large waist circumference (p<0.05). In fully-adjusted logistic regression models, foreign-born participants with both high parental and personal education levels (High/High) had 55% lower odds of having large waist circumference (OR=0.45; 95% CI=0.23, 0.88), compared to participants with both low parental and personal education levels (Low/Low). The education gradient in type-2 diabetes and metabolic syndrome was not statistically significant. Similarly, the education gradients in other components of metabolic syndrome (e.g., low HDL cholesterol and high fasting glucose) were not statistically significant in logistic regression models (data not shown).
As depicted in the figure, the prevalence of large waist circumference was significantly lower for foreign-born participants whose parents’ education was high and who also personally achieved high adult education levels (Parental High/Adult High). On the other hand, the prevalence of type-2 diabetes was significantly lower for US-born participants who achieved high adult education, regardless of their parents’ educational attainment (Parental High/Adult High or Parental Low/Adult High).
Discussion
The findings in our study demonstrate the sizable burden of long-term cardiovascular and metabolic risk associated with patterns of intergenerational educational attainment. Our findings suggest that achieving high adult education confers a 37% lower probability of type-2 diabetes among US-born older adult Latinos, regardless of their parents’ educational attainment. Education, however, does not significantly influence central obesity or metabolic syndrome in US-born Latinos. On the other hand, foreign-born older adult Latinos only benefitted from having both high parental and high adult educational attainment for lower waist circumference-up to a 55% lower odds. A similar association was observed for high education across generation and lower odds of metabolic syndrome among the foreign born, but the confidence interval included the null value. The large advantages conferred by intergenerational education for waist circumference among foreign-born Latinos did not hold for type-2 diabetes risk. Taken in the context of rising obesity prevalence and the growth of the aging Latino population in the US, our study fills an important gap in the literature by providing evidence that there are key periods across the life course, varying according to country of birth, in which parental or personal education may substantially reduce the odds of having large waist circumference and type-2 diabetes.
Factors that may explain the impact of adult educational attainment on the long-term risk of large waist circumference, metabolic syndrome, and type-2 diabetes may include differences in behavioral and psychosocial factors, exposure to stress, and access to health care. For example, lower socioeconomic status has been associated with structural and behavioral risk factors such as lack of access to nutritious food, prevalence of smoking, and inadequate opportunities for physical activity [25-27]. These structural and behavioral risk factors have profound influences on waist circumference, metabolic syndrome, and type-2 diabetes [28]. Furthermore, the stress of living in a low socioeconomic environment has been shown to be associated with dysfunction of the hypothalamic-pituitary-adrenocortical (HPA) axis [29], which in turn is a potential pathway leading to central obesity and dysregulation of insulin sensitivity [30]. Moreover, subjects residing in low socioeconomic environments may be more vulnerable to the negative impact of stressful life events on their health [31].
In addition to the direct influence of participants’ adult educational attainment on health in older age, by including parental education as an exposure, we investigated the hypothesis that a host of early-life experiences may exert influence on the associations observed here. Early-life influences of low parental education may reflect exposure to detrimental environments while growing up, such as poor housing quality, environmental stressors, and a lack of an academically stimulating early-life environment [32, 33]. These early-life exposures likely influence the educational attainment of children and ultimately shape their adult living environment, access to resources, and health behaviors, all of which can influence waist circumference, metabolic syndrome, and type-2 diabetes risk. When we further adjusted, in our sensitivity analysis, for other childhood exposures such as food deprivation and sibling mortality, our main findings were slightly attenuated but conclusions remained the same. The early-life environment may also influence the children’s (i.e., SALSA participants’) motivation for migration and thus the age at migration, which will then impact the types of exposures and likelihood of developing health conditions in the receiving country.
To crudely assess the potential for mediation of some of the behavioral risk factors in the pathways of interest, as a sensitivity analysis, we additionally adjusted for smoking, alcohol use, and physical activity. The associations were only slightly attenuated, suggesting that these factors may be partial mediators but do not fully explain the pathways between education and outcomes of interest. Therefore, other structural factors such as stress related to exposure to discrimination and the safety and availability of walkable neighborhoods and recreational areas should be examined as potential additional mediating factors.
Our findings suggest an association between higher adult education and increased odds of type-2 diabetes among the US-born, and an association between higher education across generations and lower waist circumference among the foreign-born. A similar trend was observed for higher education and lower odds of metabolic syndrome among the foreign born, but it did not reach statistical significance levels in fully-adjusted models. There are several factors that may explain the observed heterogeneity by country of birth. For example, migration, which has been associated with the development of unhealthy behaviors, is likely to induce differing trajectories depending upon place of birth and age at migration. A change in disease risk of immigrating populations has been supported in multiple studies, including Latinos [11]. In our study, the US-born were more likely to have worse cardiovascular risk profile (e.g., high fasting glucose and high triglycerides) and a clustering of risk factors (e.g. metabolic syndrome) than their foreign-born counterparts. In other studies, individuals who never migrated to the US, such as Mexicans of Mexico City reported in the CARMELA study (Cardiovascular Risk Factor Multiple Evaluation in Latin America), showed generally a lower burden of cardiovascular risk factors [34]. Along those lines, it is possible that those born in the US have developed cardiovascular and metabolic risk factors over the life course (i.e., had more exposure time) and thus needed fewer triggers to move on to the development of type-2 diabetes by age 60 (study baseline age). On the other hand, foreign-born individuals may have had less exposure to risk factors given that their time spent in the US has been of a shorter duration. Therefore, foreign-born individuals may be more likely to have developed central obesity by age 60 and less likely to have developed type-2 diabetes, and may only develop it at later ages or across later generations.
The observed association between intergenerational education and central obesity is a key finding for foreign-born Latinos, a group with high obesity rates [35]. Central obesity is a component of metabolic syndrome and a risk factor for developing type-2 diabetes, which represents a more advanced clinical endpoint. Therefore, an early diagnosis of the components of metabolic syndrome, particularly central obesity, can help in designing early interventions targeting lifestyle and behavioral risk factors. While we would have expected to see an association between education and other components of metabolic syndrome, the lack of such associations, especially among the foreign-born, may be due to limited heterogeneity in cardiometabolic risk factors at the lower end of intergenerational education.
Our findings are consistent with prior literature suggesting that socioeconomic exposures influence waist circumference and type-2 diabetes. The majority of prior work, however, focused on non-Latino white and black populations; neglected intergenerational effects of education; and reported inconsistent findings [13, 14, 36, 37]. Similarly, prior work incorporated limited research from studies including older adult Latinos [18-21]. Our findings were consistent with those from the Proyecto VER study of Hispanics aged 40 years old and above, in which adult socioeconomic status was associated with type-2 diabetes [20]. Our results were also consistent with a recent analysis from NHANES that included Mexican Americans and showed an inverse socioeconomic gradient with diabetes [19]. It is important to note that none of these previous studies examined intergenerational effects of socioeconomic status. To our knowledge, there is only one recent study that explored the association between intergenerational education (parental and adult) and obesity among immigrants [38]. However, their study focused on young adults (up to 33 years old); used only BMI as a measure of obesity, as opposed to waist circumference; and examined a heterogeneous Hispanic group – in terms of country of origin – in addition to other racial groups.
In the context of life course determinants of adult disease, our findings suggest that life course theories related to cumulative disadvantage may vary by nativity. Among US-born, our findings suggest a pathway model whereby childhood SES may shape adulthood SES, but adulthood SES is the etiologically relevant exposure for adult disease. Among foreign-born, our findings suggest a cumulative disadvantage model whereby both childhood and adulthood SES together are etiologically relevant exposure periods that influence adult disease. Finally, while the literature suggests that prenatal exposures influence adult disease [39], we did not collect this data in our study and thus could not explore any potential latent effect of these factors on adult disease.
There are a few limitations in our study. First, participants had to survive until age 60 and above to be eligible in this study, which could result in selection bias. Second, parents’ education was self-reported and is therefore subject to recall bias. However, studies have shown that self-report of parental socioeconomic characteristics are valid and generally in high agreement with parent’s report [40]. Furthermore, given the possibility of a differential access to higher education and differences in the quality of education across geographic regions between the US-born and foreign-born, our findings should be interpreted with caution. Third, education may be a marker for other unmeasured factors that influence cardiometabolic disorders such as chronic malnutrition or environmental stressors [33] that were unavailable in this study. Fourth, our relatively small sample size when stratifying subjects into US-born and foreign-born categories, may have reduced our power to identify statistically significant associations for some outcomes. Finally, given the heterogeneity of risk across Latino subgroups, it is important to note that our findings are generalizable to US Latinos who are of Mexican descent. Despite these limitations, to the best of our knowledge, this study is the first to examine the association of intergenerational education and nativity with waist circumference, metabolic syndrome, and type-2 diabetes among older adult Latinos. Furthermore, the current analysis used objective measures of type-2 diabetes and features of metabolic syndrome, rather than self-report, as is common in other studies of Latinos.
In conclusion, the findings from our study fill an important gap in the literature on education across generations and metabolic risk in older adult Latinos, one of the fastest growing aging populations in the US. Our findings suggest the need to further examine the socioeconomic changes occurring across generations of Latinos as immigrants assimilate in the US, and how these factors ultimately influence health outcomes in older age.
What is already known about this subject
Obesity epidemic remains a major public health challenge, and is exacerbated by socioeconomic, racial, and ethnic disparities.
Studies of non-Latino white and black populations have reported inconsistent findings on the role of social factors, education in particular, in shaping obesity and type-2 diabetes outcomes.
Intergenerational economic status has been shown to influence adult health status, but the majority of prior work has neglected intergenerational effects of education, particularly in Latino populations.
What this study adds
Our study population is comprised only of US Latinos who are the fastest growing ethnic minority group in the US and are disproportionately burdened with obesity and type-2 diabetes compared to non-Latino whites and blacks.
For the first time, we evaluate the role of educational attainment across generations on waist circumference, metabolic syndrome, and type-2 diabetes.
Figure 1.
Prevalence of A) large waist circumference, B) metabolic syndrome, and C) type-2 diabetes by intergenerational education levels, for the US-born and foreign-born.
Acknowledgments
Author Contributions: AA developed the aims of the study. AZ and AA analyzed and interpreted the data and drafted the manuscript. MH is the principal investigator of the SALSA study. MH, WR, PG, LG, and EC were involved in critical revision of the manuscript for important intellectual content. All authors had final approval of the submitted and published versions.
Sources of Funding: Dr. Zeki Al Hazzouri was supported by a grant from the NIH, National Institute on Aging (K01AG047273) and the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number KL2TR000143. The SALSA study was funded by a grant from the National Institute on Aging (AG12975).
Footnotes
Competing Interests: None
Contributor Information
Adina Zeki Al Hazzouri, Division of Epidemiology and Population Health, Department of Public Health Sciences, University of Miami, Miami, FL.
Mary Haan, Department of Epidemiology & Biostatistics, School of Medicine, University of California San Francisco, San Francisco, CA.
Whitney R. Robinson, Department of Epidemiology, UNC Gillings School of Global Public Health, University of North Carolina Chapel Hill, NC
Penny Gordon Larsen, Department of Nutrition, UNC Gillings School of Global Public Health, University of North Carolina Chapel Hill, NC.
Lorena Garcia, Department of Public Health Sciences, Division of Epidemiology, UC Davis School of Medicine, Davis, CA.
Erin Clayton, Department of Epidemiology, University of Michigan School of Public Health, Ann Arbor, MI.
Allison E Aiello, Department of Epidemiology, UNC Gillings School of Global Public Health, University of North Carolina Chapel Hill, NC.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA : the journal of the American Medical Association. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vazquez G, Duval S, Jacobs DR, Jr., Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiologic Reviews. 2007;29:115–128. doi: 10.1093/epirev/mxm008. [DOI] [PubMed] [Google Scholar]
- 3.Biggs ML, Mukamal KJ, Luchsinger JA, Ix JH, Carnethon MR, Newman AB, et al. Association between adiposity in midlife and older age and risk of diabetes in older adults. JAMA : the journal of the American Medical Association. 2010;303:2504–2512. doi: 10.1001/jama.2010.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandya A, Gaziano TA, Weinstein MC, Cutler D. More americans living longer with cardiovascular disease will increase costs while lowering quality of life. Health Affairs. 2013;32:1706–1714. doi: 10.1377/hlthaff.2013.0449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA : the journal of the American Medical Association. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 6.Knowlden AP, Sharma M. Systematic review of school-based obesity interventions targeting African American and Hispanic children. Journal of Health Care for the Poor and Underserved. 2013;24:1194–1214. doi: 10.1353/hpu.2013.0129. [DOI] [PubMed] [Google Scholar]
- 7.Umpierrez GE, Gonzalez A, Umpierrez D, Pimentel D. Diabetes mellitus in the Hispanic/Latino population: an increasing health care challenge in the United States. The American journal of the medical sciences. 2007;334:274–282. doi: 10.1097/MAJ.0b013e3180a6efe3. [DOI] [PubMed] [Google Scholar]
- 8.Albrecht SS, Gordon-Larsen P. Ethnic differences in body mass index trajectories from adolescence to adulthood: a focus on Hispanic and Asian subgroups in the United States. PloS one. 2013;8:e72983. doi: 10.1371/journal.pone.0072983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003-2006. National health statistics reports. 2009:1–7. [PubMed] [Google Scholar]
- 10.Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Medical care research and review : MCRR. 2007;64:101S–156S. doi: 10.1177/1077558707305409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morales LS, Leng M, Escarce JJ. Risk of cardiovascular disease in first and second generation Mexican-Americans. Journal of immigrant and minority health / Center for Minority Public Health. 2011;13:61–68. doi: 10.1007/s10903-009-9262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mainous AG, 3rd, Majeed A, Koopman RJ, Baker R, Everett CJ, Tilley BC, et al. Acculturation and diabetes among Hispanics: evidence from the 1999-2002 National Health and Nutrition Examination Survey. Public Health Reports. 2006;121:60–66. doi: 10.1177/003335490612100112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramsay SE, Whincup PH, Morris R, Lennon L, Wannamethee SG. Is socioeconomic position related to the prevalence of metabolic syndrome?: influence of social class across the life course in a population-based study of older men. Diabetes care. 2008;31:2380–2382. doi: 10.2337/dc08-1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chichlowska KL, Rose KM, Diez-Roux AV, Golden SH, McNeill AM, Heiss G. Life course socioeconomic conditions and metabolic syndrome in adults: the Atherosclerosis Risk in Communities (ARIC) Study. Annals of epidemiology. 2009;19:875–883. doi: 10.1016/j.annepidem.2009.07.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leonetti DL, Tsunehara CH, Wahl PW, Fujimoto WY. Educational attainment and the risk of non-insulin-dependent diabetes or coronary heart disease in Japanese-American men. Ethnicity and Disease. 1992;2:326–336. [PubMed] [Google Scholar]
- 16.Maty SC, James SA, Kaplan GA. Life-course socioeconomic position and incidence of diabetes mellitus among blacks and whites: the Alameda County Study, 1965-1999. American Journal of Public Health. 2010;100:137–145. doi: 10.2105/AJPH.2008.133892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and type 2 diabetes in African American and non-Hispanic white women and men: evidence from the Third National Health and Nutrition Examination Survey. American Journal of Public Health. 2001;91:76–83. doi: 10.2105/ajph.91.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maty SC, Everson-Rose SA, Haan MN, Raghunathan TE, Kaplan GA. Education, income, occupation, and the 34-year incidence (1965-99) of Type 2 diabetes in the Alameda County Study. International Journal of Epidemiology. 2005;34:1274–1281. doi: 10.1093/ije/dyi167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karlamangla AS, Merkin SS, Crimmins EM, Seeman TE. Socioeconomic and ethnic disparities in cardiovascular risk in the United States, 2001-2006. Annals of epidemiology. 2010;20:617–628. doi: 10.1016/j.annepidem.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.West SK, Munoz B, Klein R, Broman AT, Sanchez R, Rodriguez J, et al. Risk factors for Type II diabetes and diabetic retinopathy in a mexican-american population: Proyecto VER. American Journal of Ophthalmology. 2002;134:390–398. doi: 10.1016/s0002-9394(02)01595-7. [DOI] [PubMed] [Google Scholar]
- 21.Best LE, Hayward MD, Hidajat MM. Life course pathways to adult-onset diabetes. Social Biology. 2005;52:94–111. [PubMed] [Google Scholar]
- 22.Zeki Al Hazzouri A, Haan MN, Kalbfleisch JD, Galea S, Lisabeth LD, Aiello AE. Life-course socioeconomic position and incidence of dementia and cognitive impairment without dementia in older Mexican Americans: results from the Sacramento area Latino study on aging. American Journal of Epidemiology. 2011;173:1148–1158. doi: 10.1093/aje/kwq483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002:3143–3421. [PubMed] [Google Scholar]
- 24.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27:83–95. [Google Scholar]
- 25.Yang S, Lynch JW, Raghunathan TE, Kauhanen J, Salonen JT, Kaplan GA. Socioeconomic and psychosocial exposures across the life course and binge drinking in adulthood: population-based study. American Journal of Epidemiology. 2007;165:184–193. doi: 10.1093/aje/kwj357. [DOI] [PubMed] [Google Scholar]
- 26.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Social Science and Medicine. 1997;44:809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- 27.Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. American Journal of Preventive Medicine. 2008;34:16–22. doi: 10.1016/j.amepre.2007.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes care. 2007;30:744–752. doi: 10.2337/dc06-1842. [DOI] [PubMed] [Google Scholar]
- 29.Brunner E. Stress and the biology of inequality. Bmj. 1997;314:1472–1476. doi: 10.1136/bmj.314.7092.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brindley DN. Neuroendocrine regulation and obesity. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 1992;16(Suppl 3):S73–79. [PubMed] [Google Scholar]
- 31.Rosmond R, Bjorntorp P. The hypothalamic-pituitary-adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. Journal of Internal Medicine. 2000;247:188–197. doi: 10.1046/j.1365-2796.2000.00603.x. [DOI] [PubMed] [Google Scholar]
- 32.Bradley RH, Corwyn RF, McAdoo HP, Coll CG. The home environments of children in the United States part I: variations by age, ethnicity, and poverty status. Child Development. 2001;72:1844–1867. doi: 10.1111/1467-8624.t01-1-00382. [DOI] [PubMed] [Google Scholar]
- 33.Fernald LC, Neufeld LM, Barton LR, Schnaas L, Rivera J, Gertler PJ. Parallel deficits in linear growth and mental development in low-income Mexican infants in the second year of life. Public Health Nutrition. 2006;9:178–186. doi: 10.1079/phn2005759. [DOI] [PubMed] [Google Scholar]
- 34.Schargrodsky H, Hernandez-Hernandez R, Champagne BM, Silva H, Vinueza R, Silva Aycaguer LC, et al. CARMELA: assessment of cardiovascular risk in seven Latin American cities. The American journal of medicine. 2008;121:58–65. doi: 10.1016/j.amjmed.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 35.Albrecht SS, Diez Roux AV, Kandula NR, Osypuk TL, Ni H, Shrager S. Immigrant assimilation and BMI and waist size: a longitudinal examination among Hispanic and Chinese participants in the multi-ethnic study of atherosclerosis. Obesity. 2013;21:1695–1703. doi: 10.1002/oby.20104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gustafsson PE, Persson M, Hammarstrom A. Life course origins of the metabolic syndrome in middle-aged women and men: the role of socioeconomic status and metabolic risk factors in adolescence and early adulthood. Annals of epidemiology. 2011;21:103–110. doi: 10.1016/j.annepidem.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 37.Parker L, Lamont DW, Unwin N, Pearce MS, Bennett SM, Dickinson HO, et al. A lifecourse study of risk for hyperinsulinaemia, dyslipidaemia and obesity (the central metabolic syndrome) at age 49-51 years. Diabetic medicine : a journal of the British Diabetic Association. 2003;20:406–415. doi: 10.1046/j.1464-5491.2003.00949.x. [DOI] [PubMed] [Google Scholar]
- 38.Albrecht SS, Gordon-Larsen P. Socioeconomic gradients in body mass index (BMI) in US immigrants during the transition to adulthood: examining the roles of parental education and intergenerational educational mobility. Journal of Epidemiology and Community Health. 2014 doi: 10.1136/jech-2014-203814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barker DJ, Forsen T, Uutela A, Osmond C, Eriksson JG. Size at birth and resilience to effects of poor living conditions in adult life: longitudinal study. Bmj. 2001;323:1273–1276. doi: 10.1136/bmj.323.7324.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ridolfo H, Maitland A. Factors that influence the accuracy of adolescent proxy reporting of parental characteristics: a research note. Journal of adolescence. 2011;34:95–103. doi: 10.1016/j.adolescence.2010.01.008. [DOI] [PubMed] [Google Scholar]