Abstract
Background
The triage nurse is involved in the early identification of the most severe patients at emergency department (ED) presentation. However, clinical criteria alone may be insufficient to identify them correctly. Measurement of capillary lactate concentration at ED presentation may help to discriminate these patients. The primary objective of this study was to identify the prognostic value of capillary lactate concentration measured by the triage nurse among patients presenting to the ED.
Methods
This was a prospective observational study, performed in the ED of a university hospital. At ED presentation, capillary lactate measurement was performed by the triage nurse among patients presenting with a clinical criteria of systemic inflammatory response syndrome (SIRS). Clinical variables usually used to determine severity were collected at presentation. Twenty-eight-day mortality and MEDS score were recorded.
Results
One hundred seventy-six patients with clinical SIRS presented to the ED. Median age was 72 years, and 28-day mortality was 16%. Capillary lactate at ED presentation was significantly higher among 28-day non-survivors than among survivors (5.7 mmol.L−1 [3.2 to 7.4] vs 2.9 mmol.L−1 [1.9 to 5.2], p = 0.003). A score based on mottling and capillary lactate concentration >3.6 mmol.L−1 was significantly associated with 28-day mortality (area under curve, AUC = 0.75), independently of the MEDS score (AUC = 0.79) for the prediction of 28-day mortality (AUC global model 0.87).
Conclusions
A high capillary lactate concentration measured by the triage nurse among patients presenting to the ED with clinical SIRS is associated with a high risk of death. A score calculated by the triage nurse, based on mottling and capillary lactate concentration, appears to be useful for identifying the most severe patients.
Keywords: Systemic inflammatory response syndrome, Capillary lactate, Prognosis, Triage tool
Background
The triage nurse is involved in the early identification of the most severe patients at Emergency Department (ED) presentation in order to avoid delaying treatment, to orientate patients towards the appropriate structure, and finally, to improve their prognosis [1-4]. However, clinical criteria alone can be insufficient for the triage nurse to correctly identify the most severe patients at initial presentation to the ED [5,6]. The Mortality in Emergency Department Sepsis (MEDS) score is validated for the evaluation of prognosis in patients admitted to the ED with systemic inflammatory response syndrome (SIRS) or sepsis. However, it requires a clinical diagnosis by the doctor and includes the results of biological data [7,8]. It is well established that plasma concentration of lactate is associated with the risk of death in critically ill patients [9-19], but since it requires venous or arterial blood puncture and then the time of analysis, its measurement is available only after patient care has been initiated [20]. On the contrary, capillary lactate measurement can be performed by the nurse immediately at presentation and may help to stratify patient according to their severity [21]. In addition, it is well established that there is a good correlation between plasma and capillary lactate concentrations [20]. The primary objective of this study was to evaluate the prognostic value of capillary lactate concentration among patients presenting to the ED with a clinical criteria of SIRS. Secondary objectives were to identify variables collected by the nurse at ED presentation that were associated with 28-day mortality and to build a prognostic score integrating capillary lactate concentration.
Methods
Study population
Adult patients presenting to the ED between November 2008 and May 2009 in a large, regional university hospital were screened immediately by the triage nurse. Inclusion criteria were: age 18 years or more and presence clinical SIRS defined by at least two criteria among the following: temperature <36°C or >38°C, heart rate >90 bpm, and respiratory rate >20/min [21]. Exclusion criteria were: traumatic injury and voluntary intoxication.
Data collection
As part of usual practice, the following variables were prospectively collected by the triage nurse at ED presentation: age, sex, temperature (°C), Glasgow Coma Score, respiratory rate, SpO2, heart rate (bpm), and noninvasive assessment of blood pressure with an adjusted device according to body weight (systolic arterial pressure (mmHg), mean arterial pressure (mmHg), and diastolic arterial pressure (mmHg)). In addition, after a short educational program for the study, nurses recorded the following additional variables: presence of mottling on lower limbs, capillary refilling time on the foot (s), clinical criteria of SIRS as previously defined, and point of care capillary lactate concentration from a finger stick (Lactate Pro®, Arkray Factory, Shiga, Japan) at the same time as capillary blood glucose measurement. Doctors were blinded from capillary lactate measurement. Therapy in the ED are the following: antibiotic use, volume of vascular filling (L), catecholamine use, oxygen flow (L/min), and hospitalization after ED admission. Length of stay (days) and the final diagnosis at the end of hospitalization were recorded. Mortality at 28 days was recorded by a phone call to the patient, their family, or their general practitioner. MEDS score at ED admission was calculated [8].
Statistical analysis
Quantitative variables are presented as median [interquartile range, IQR]. Qualitative variables are presented as number (percentage). Comparisons between qualitative variables were assessed using Fisher’s exact test or the chi-square test as appropriate. Comparisons between quantitative variables were assessed using the Wilcoxon test. A p value of <0.05 was considered statistically significant. A subgroup analysis was performed in the subgroup of patients presenting to the ED without hypotension. Receiver operating characteristic (ROC) curve analysis was performed to calculate the optimal cutoff values for capillary refilling time and capillary lactates to detect mortality. Because of the limited number of patients in comparison to the number of variables studied, we decided to focus on the prognostic value of mottling, capillary refilling time, and capillary lactates. Multiple logistic regression analysis was performed to evaluate whether these three variables were independently associated with 28-day mortality. Results are presented as odds ratios (OR) with 95% confidence interval (CI). A score was constructed, including the presence or absence of mottling, and two classes of capillary lactates, according to the threshold previously identified by the ROC curve analysis. Survival after ED presentation according to this score was estimated using the Kaplan-Meier analysis. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Patient consent
The study was approved by the ethics committee of Besançon University Hospital. Written informed consent was obtained from all patients before inclusion in the study. In the most severe patients who were unable to provide consent, written consent was obtained from the patient’s family.
Results
Study population
One hundred seventy-six patients with clinical criteria of SIRS at ED presentation were included in the study. The characteristics of the patients at ED presentation and the description of SIRS criteria are shown in Tables 1 and 2, respectively. Eighteen patients (10%) presented to the ED with systolic arterial pressure <90 mmHg and/or mean arterial pressure <65 mmHg. Mortality at 28 days was 16% (29/176). Capillary lactate concentration was available in 175 out of 176 patients.
Table 1.
Baseline characteristics of the study population at emergency department presentation
| Variable | n = 176 |
|---|---|
| Age (years) | 72 [56 to 82] |
| Sex male | 89 (51) |
| Temperature | 37.3 [36.4 to 38.3] |
| Glasgow Coma Score | 15 [15] |
| Ventilatory rate (bpm) | 25 [22 to 30] |
| SpO2 (%) | 96 [93 to 98] |
| Heart rate (bpm) | 106 [93 to 117] |
| Systolic arterial pressure (mmHg) | 134 [111 to 159] |
| Systolic arterial pressure <90 mmHg | 18 (10) |
| Mean arterial pressure (mmHg) | 92 ([77 to 108]) |
| Diastolic arterial pressure (mmHg) | 72 ([61 to 85]) |
| Capillary refilling time (s) | 1 ([1]) |
| Presence of mottling | 24 (14) |
| Capillary lactates (mmol.L−1)a | 3.3 [2.0 to 5.8] |
| Length of hospitalization (days) | 7 [2-13] |
| 28-day mortality | 29 (16) |
| MEDS score | 6 [5-11] |
| Therapy in the ED after admission | |
| Antibiotic therapy | 91 (52) |
| Volume vascular filling (L) | 0.5 [0.5 to 1.5] |
| Catecholamine use | 9 (5) |
| Oxygen flow (L/min) | 0 [0 to 3] |
| Hospitalization after ED admission | 150 (85) |
| Final diagnosis | |
| Pneumonia | 63 (36) |
| Digestive disease | 29 (15) |
| Cardiovascular disease | 22 (13) |
| Neurological disease | 15 (9) |
| Urinary disease | 10 (6) |
| Cardiac arrest | 2 (1) |
| Other diagnosis | 35 (20) |
Numbers are n (%), median [interquartile range]. aAvailable in 175 out of 176 patients.
Table 2.
Characteristics of the systemic inflammatory response syndrome
| Variable | n = 176 |
|---|---|
| SIRS criteria | |
| Temperature <36°C or >38°C | 92 (53) |
| Heart rate >90 bpm | 146 (83) |
| Ventilatory rate >20 | 155 (88) |
| Number of SIRS criteria | |
| 2 out of 3 | 135 (77) |
| 3 out of 3 | 41 (23) |
Numbers are n (%); SIRS, systemic inflammatory response syndrome.
Univariate analysis
Univariate analysis of the relation between variables recorded by the triage nurse at ED presentation and 28-day mortality is presented in Table 3. Non-survivors at 28 days were older; had lower admission temperature, Glasgow coma score, systolic arterial pressure, mean arterial pressure, diastolic arterial pressure, and SpO2; more frequently had presence of mottling; had a longer capillary refilling time; and had a higher capillary lactate concentration than 28-day survivors (all p < 0.05). There was a positive correlation between the capillary lactate concentration measured at presentation and the volume of vascular filling administered in the ED (R = 0.26, p = 0.0005). ROC curve analysis identified a threshold of 2 s for capillary refilling time and 3.6 mmol.L−1 for capillary lactate concentration as best predicting 28-day mortality (area under curve (AUC) 0.66 for each).
Table 3.
Univariate analysis of the variables at ED presentation according to 28-day mortality
| Survivors at 28 days | Non-survivors at 28 days | p | |
|---|---|---|---|
| n = 147 | n = 29 | ||
| Age (years) | 66 [51 to 81] | 79 [69 to 83] | 0.004 |
| Sex male | 70 (48) | 19 (66) | 0.10 |
| Temperature (°C) | 37.4 [36.5 to 38.4] | 36.9 [35.6 to 37.8] | 0.046 |
| Glasgow Coma Score | 15 [15] | 14 [11 to 15] | <0.0001 |
| Heart Rate (bpm) | 105 [95 to 116] | 106 [91 to 120] | 0.85 |
| Systolic arterial pressure (mmHg) | 137 [113 to 160] | 113 [88 to 150] | 0.04 |
| Systolic blood pressure <90 mmHg | 10 (7) | 8 (28) | 0.003 |
| Mean arterial pressure (mmHg) | 96 [80 to 109] | 86 [69 to 98] | 0.03 |
| Diastolic arterial pressure (mmHg) | 74 [62 to 86] | 63 [56 to 79] | 0.04 |
| Ventilatory rate (bpm) | 25 [22 to 30] | 29 [24 to 31] | 0.10 |
| SpO2 (%) | 96 [94 to 98] | 95 [90 to 96] | 0.02 |
| Capillary refilling time (s) | 1 [1 to 1] | 1 [1 to 3] | 0.0001 |
| Presence of mottling | 11 (7) | 13 (45) | <0.0001 |
| Capillary lactates | 2.9 [1.9 to 5.2] | 5.7 [3.2 to 7.4] | 0.003 |
Numbers are n (%), median [interquartile range].
Logistic regression analysis
The results of logistic regression analysis of mottling, capillary refilling time, and capillary lactate concentration to predict 28-day mortality are shown in Table 4.
Table 4.
Logistic regression analysis to predict 28-day mortality in patients presenting to the ED with clinical SIRS
| Variables | Simple logistic regression | Multiple logistic regression | ||
|---|---|---|---|---|
| OR | P | OR | P | |
| Capillary refilling time | <0.0001 | 0.013 | ||
| ≤2 s | 1 | 1 | ||
| >2 s | 18.9 [5.4 to 66.7] | 6.6 [1.5 to 29.4] | ||
| Mottling | <0.0001 | 0.014 | ||
| Absence | 1 | 1 | ||
| Presence | 10 [3.9 to 26.3] | 4.4 [1.35 to 14.5] | ||
| Capillary lactates | 0.003 | 0.019 | ||
| ≤3.6 mmol/L | 1 | 1 | ||
| >3.6 mmol/L | 3.8 [1.6 to 9.1] | 3.2 [1.2 to 8.4] | ||
OR, odds ratio [confidence interval 95%].
By simple logistic regression, capillary refilling time >2 s, presence of mottling, and capillary lactate concentration >3.6 mmol.L−1 were all significantly associated with 28-day mortality (OR [CI 95%] = 18.9 [5.4 to 66.7], OR [CI 95%] = 10 [3.9 to 26.3], and OR [CI 95%] = 3.8 [1.6 to 9.1], respectively). By multiple logistic regression, capillary refilling time >2 s, presence of mottling, and capillary lactates >3.6 mmol.L−1 were independently associated with 28-day mortality (OR = 6.6 [1.5 to 29.4], OR = 4.4 [1.35 to 14.5], and OR = 3.2 [1.2 to 8.4], respectively).
Score based on mottling and capillary lactates
Since capillary lactate concentration and mottling at presentation were independently associated with 28-day mortality, a score based on the presence or absence of mottling, and capillary lactate concentration ≤3.6 mmol.L−1 or >3.6 mmol.L−1 was built (Table 5). Mortality at 28 days was 6%, 19%, and 67% among patients with score of 0, 1, or 2, respectively (p < 0.0001). Among the 157 patients presenting to ED without hypotension (i.e., systolic arterial pressure ≥90 mmHg and mean arterial pressure ≥65 mmHg), 28-day mortality was 6%, 17%, and 56% for a score of 0, 1, or 2, respectively (p = 0.0005).
Table 5.
Nurse hypoperfusion score in patients with clinical SIRS at ED presentation
| Definition of score | 28-day mortality | ||||
|---|---|---|---|---|---|
| Overall SIRS | p | SIRS without hypotension | p | ||
| Absence of mottling and capillary lactates ≤3.6 mmol/L | 0 point | 5/85 (6) | <0.0001 | 5/84 (6) | 0.0005 |
| Presence of mottling or capillary lactates >3.6 mmol/L | 1 point | 14/75 (19) | 11/64 (17) | ||
| Presence of mottling and capillary lactates >3.6 mmol/L | 2 points | 10/15 (67) | 5/9 (56) | ||
Survival after ED presentation according to this score was estimated using the Kaplan-Meier method (Figure 1, log-rank p < 0.0001). The characteristics of the patients at ED presentation according to the score are presented in Table 6. Care intensity in the ED according to the score is presented in Table 7. The higher the score, the higher the volume of vascular filling, the higher the oxygen flow, and the more frequent the catecholamine use. The AUC for the score and for the MEDS score were 0.75 and 0.79, respectively. Multiple logistic regression analysis showed that the two scores were independent for the prediction of 28-day mortality (AUC of the global model = 0.87).
Figure 1.
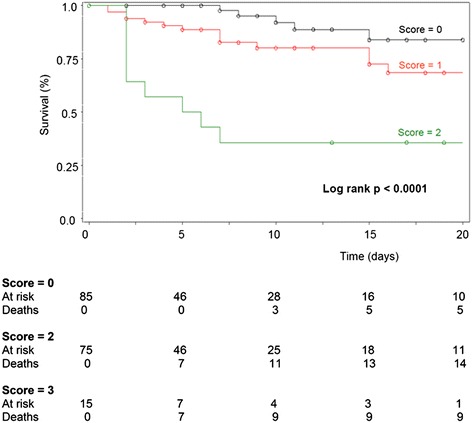
Survival after ED presentation based on mottling and capillary lactates estimated using the Kaplan-Meier method. Kaplan-Meier survival curve of patients with clinical SIRS at emergency department presentation according to the nurse hypoperfusion score. Vertical axis represents estimated probability of survival. Horizontal axis represents time in days after emergency department admission. Censored observations, corresponding to patient survivors that were lost of follow-up, are represented by circles.
Table 6.
Characteristics of the patients at ED presentation according to the nurse hypoperfusion score
| Score = 0 | Score = 1 | Score = 2 | |
|---|---|---|---|
| n | 85 | 75 | 15 |
| Age (years) | 75 [56–83] | 66 [53 to 79] | 79 [61 to 85] |
| Temperature (°C) | 37.3 [36.7 to 38.3] | 37.4 [36.4 to 38.3] | 36.5 [35.3 to 38.2] |
| Glasgow Coma Score | 15 [15 to 15] | 15 [14 to 15] | 14 [8 to 15] |
| Heart Rate (bpm) | 102 [95 to 112] | 108 [94 to 117] | 95 [76 to 120] |
| Systolic arterial pressure (mmHg) | 142 [121 to 163] | 130 [104 to 156] | 110 [85 to 143] |
| Mean arterial pressure (mmHg) | 96 [85 to 112] | 92 [73 to 106] | 73 [60 to 103] |
| Diastolic arterial pressure (mmHg) | 75 [64 to 88] | 71 [58 to 83] | 59 [46 to 81] |
| Ventilatory rate (bpm) | 25 [22 to 29] | 25 [22 to 30] | 30 [21 to 34] |
| SpO2 (%) | 96 [94 to 98] | 96 [94 to 98] | 96 [91 to 98] |
| Capillary refilling time (s) | 1 [1 to 1] | 1 [1 to 1] | 3 [1 to 3] |
Numbers are median [interquartile range].
Table 7.
Care intensity in the ED according to the nurse hypoperfusion score calculated at ED presentation
| Score = 0 | Score = 1 | Score = 2 | p | |
|---|---|---|---|---|
| n | 85 | 75 | 15 | |
| Oxygen flow (L/min) | 0 [0 to 2] | 2 [0 to 3] | 3 [1 to 6] | 0.006 |
| Vascular filling (L) | 0.5 [0.5 to 1] | 0.9 [0.5 to 1.5] | 1.5 [0.5 to 2.5] | 0.0002 |
| Catecholamine use | 0 (0) | 5 (7) | 4 (27) | <0.0001 |
| Antibiotic therapy | 38 (45) | 41 (55) | 11 (73) | 0.09 |
Numbers are median [interquartile range], n (%).
Discussion
The main result of this study is that a high capillary lactate concentration measured by the triage nurse at ED presentation among patients with clinical criteria of SIRS is associated with a high risk of death. This study reinforces the role of the triage nurse.
To the best of our knowledge, this is the largest study evaluating the prognostic value of capillary lactate concentration at ED presentation in terms of the number of patients included. Only one study has specifically studied the prognostic value of capillary lactate at ED admission. Seoane et al., in their prospective study of 79 patients with critical illness, identified that a capillary lactate concentration of >2.35 mmol.L−1 was associated with mortality [20]. In the present study, we identified a cutoff of 3.6 mmol.L−1 that best predicted 28-day mortality (OR = 3.8 [1.6 to .1], p = 0.003). This cutoff is close to the cutoff of 4 mmol.L−1 recommended to identify patients with severe sepsis [2].
Measuring capillary lactate concentration may help to identify patients with altered microcirculation. Indeed, in our study, 90% of patients presented to the ED without hypotension but with increased capillary lactate concentration. Among the variables collected by the triage nurse, we found that the capillary refilling time was associated with 28-day mortality, with an optimal cutoff of 2 s (OR = 18.9 [5.4 to 66.7], p < 0.0001). However, only 8% of patients had a capillary refilling time >2 s. Intuitively, one could imagine that an elevated capillary refilling time provides the same information as the presence of mottling or increased lactate concentration. However, interestingly, presence of mottling, capillary lactate concentration >3.6 mmol.L−1, and capillary refilling time >2 s were independent of each other for the identification of 28-day non-survivors.
A score integrating capillary lactate concentration with a cutoff of 3.6 mmol.L−1, and presence or absence of mottling, appears to be a useful tool for determining severity of disease in these patients. Mortality at 28 days was 6%, 19%, and 67% among patients with a score 0, 1, or 2, respectively (p < 0.0001). This nurse hypoperfusion score presents several advantages.
Firstly, it can be calculated by a nurse and not necessarily by a doctor. Secondly, it can be obtained immediately at patient presentation, avoiding the time delay engendered by admission procedures, arterial or venous blood puncture, and the time required for laboratory analyses. Indeed, it has been demonstrated that the time required for capillary lactate assessment was significantly shorter than that needed for arterial or venous lactate assessment [20]. Thirdly, this score does not take into account variables that are clearly associated with patient’s severity. Indeed, coma, hypotension, or acute respiratory failure are clinically obvious, and these patients are immediately oriented towards a medical doctor. On the contrary, our score takes into account variables that could reflect occult tissue hypoperfusion, even in patients with normal vital signs. Indeed, the score was strongly associated with 28-day mortality, even after restricting the analysis to patients presenting to the ED without hypotension (Table 5). Analysis of the patient’s characteristics at ED presentation according to the three classes of the score showed that the median systolic or mean arterial pressure, the median SaO2, and the median Glasgow Coma Score were all within normal range (Table 6). Since all the patients had clinical criteria of SIRS, it can be observed that median heart and ventilatory rates were increased. Furthermore, a recent study showed that some patients do not have increased plasma lactate concentration despite an unfavorable outcome including vasopressor-dependant septic shock [22]. There is thus a likely benefit to be gained from using such a composite score that integrates both capillary lactate dosage and clinical signs of hypoperfusion. Although promising, these results are preliminary, in view of the sample size. The utility of such a score needs to be evaluated prospectively in a large cohort of patients.
The MEDS score is the most validated prognostic score among patients admitted to the ED with sepsis or SIRS [7,8,23]. Its calculation requires the intervention of a medical doctor for the evaluation of fatal disease and diagnoses of pneumonia and septic shock, and it is also necessary to wait for the results of biological analyses for leucocyte and platelet counts. Therefore, the MEDS score cannot be calculated by a nurse and cannot be calculated immediately at patient presentation. Two findings of the present study deserve to be underlined. Firstly, the AUC for our microcirculatory dysfunction score was similar to the AUC of the MEDS score for predicting 28-day mortality (0.75 and 0.79, respectively), suggesting that our score is efficient for discriminating the most severe patients. Secondly, multiple logistic regression analysis showed that the two scores were independent of each other for the prediction of 28-day mortality, suggesting that they give different information regarding prognosis (AUC of the global model 0.87). Finally, these two scores could be complementary, with one performed by the triage nurse at patient presentation and the second calculated by the doctor after admission and evaluation of the patient.
Improving patient triage is a matter of importance, in particular, in case of high affluence to the ED, a situation where there is a risk of underestimating severity due to lack of time and means. In this setting, reinforcing the role and the performance of the triage nurse may help the medical doctor to allocate the appropriate care to the patients. In the present study, the nurse did not inform the medical doctor of capillary lactate concentration. However, the score calculated by the triage nurse at presentation was associated with care intensity in the ED. It remains to be evaluated whether taking the results of the nurse hypoperfusion score into account might improve the patient’s prognosis. For example, patients presenting to the ED with a score of 0, with an expected 28-day mortality risk of 6%, could be oriented to usual care. On the contrary, those with a score of 1 or 2, with an expected 28-day mortality risk ranging between 19% and 67%, should be immediately evaluated by an intensive care specialist and oriented towards an ICU. By avoiding delay in the first precious hours of care, for example, the golden hour for initiation of antibiotic therapy, such a strategy could considerably improve the prognosis of patients presenting to the ED.
This study has several limitations. First, this was a monocentric study. It is necessary to evaluate the interest and limits of the nurse hypoperfusion score in a large multicentric study, and in particular, to compare it with the MEDS score. Second, during the study period, consecutive patients presenting to the ED were not all included. Indeed, triage nurses who did not participate to the short educational program did not participate to the study. Third, arterial or venous lactate concentration was not measured in all patients, and therefore, a correlation between capillary and plasma lactate concentration was not available. However, a recent study has found a good correlation between capillary and plasma lactate concentrations [20].
Conclusions
In conclusion, a high capillary lactate concentration measured by the triage nurse among patients presenting to the ED is associated with a high risk of death. A score based on mottling and capillary lactate concentration, calculated by the triage nurse, appears to be useful to identify the most severe patients.
Acknowledgements
We are indebted to the triage nurses of the emergency department of the Besançon University Hospital for the clinical data collection and capillary lactate measurement. The authors thank Fiona Ecarnot (EA3920, University Hospital Besancon, France) for the editorial assistance.
Abbreviation
- ED
emergency department
Footnotes
Cyril Manzon and Gaël Piton contributed equally to this work.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CM and GC participated in the design of the study. GP performed the statistical analysis. CM, GC, and GP drafted the manuscript. LB, OB, GB, and TD reviewed the manuscript and consistently improved its content. All authors read and approved the final manuscript.
Contributor Information
Cyril Manzon, Email: cyril.manzon@hotmail.fr.
Loïc Barrot, Email: lbarrot@chu-besancon.fr.
Guillaume Besch, Email: gbesch@chu-besancon.fr.
Olivier Barbot, Email: olivbarbot@gmail.com.
Thibaut Desmettre, Email: tdesmettre@chu-besancon.fr.
Gilles Capellier, Email: gilles.capellier@univ-fcomte.fr.
Gaël Piton, Email: gpiton@chu-besancon.fr.
References
- 1.Jones AE, Puskarich MA. The surviving sepsis campaign guidelines 2012: update for emergency physicians. Ann Emerg Med. 2014;63(1):35–47. doi: 10.1016/j.annemergmed.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal S, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 4.Perman SM, Goyal M, Gaieski DF. Initial emergency department diagnosis and management of adult patients with severe sepsis and septic shock. Scand J Trauma Resusc Emerg Med. 2012;20:41. doi: 10.1186/1757-7241-20-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berger T, Green J, Horeczko T, Hagar Y, Garg N, Suarez A, et al. Shock index and early recognition of sepsis in the emergency department: pilot study. West J Emerg Med. 2013;14(2):168–74. doi: 10.5811/westjem.2012.8.11546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolf L. Early recognition and treatment of the septic patient in the emergency department. J Emerg Nurs JEN Off Publ Emerg Dep Nurses Assoc. 2012;38(2):195–7. doi: 10.1016/j.jen.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Sankoff JD, Goyal M, Gaieski DF, Deitch K, Davis C, Sabel A, et al. Validation of the Mortality in Emergency Department Sepsis (MEDS) score in patients with the systemic inflammatory response syndrome (SIRS) Crit Care Med. 2008;36(2):421–6. doi: 10.1097/01.CCM.0B013E3181611F6A0. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates D, et al. Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med. 2003;31(3):670–5. doi: 10.1097/01.CCM.0000054867.01688.D1. [DOI] [PubMed] [Google Scholar]
- 9.Moomey CB, Jr, Melton SM, Croce MA, Fabian T, Proctor K. Prognostic value of blood lactate, base deficit, and oxygen-derived variables in an LD50 model of penetrating trauma. Crit Care Med. 1999;27(1):154–61. doi: 10.1097/00003246-199901000-00044. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro NI, Howell MD, Talmor D, Nathanson L, Lisbon A, Wolfe R, et al. Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med. 2005;45(5):524–8. doi: 10.1016/j.annemergmed.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Howell MD, Donnino M, Clardy P, Talmor D, Shapiro N. Occult hypoperfusion and mortality in patients with suspected infection. Intensive Care Med. 2007;33(11):1892–9. doi: 10.1007/s00134-007-0680-5. [DOI] [PubMed] [Google Scholar]
- 12.Trzeciak S, Dellinger RP, Chansky ME, Arnold R, Schorr C, Milcarek B, et al. Serum lactate as a predictor of mortality in patients with infection. Intensive Care Med. 2007;33(6):970–7. doi: 10.1007/s00134-007-0563-9. [DOI] [PubMed] [Google Scholar]
- 13.Gatien M, Stiell I, Wielgosz A, Ooi D, Lee J. Diagnostic performance of venous lactate on arrival at the emergency department for myocardial infarction. Acad Emerg Med Off J Soc Acad Emerg Med. 2005;12(2):106–13. doi: 10.1111/j.1553-2712.2005.tb00844.x. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan LJ, Kellum JA. Initial pH, base deficit, lactate, anion gap, strong ion difference, and strong ion gap predict outcome from major vascular injury. Crit Care Med. 2004;32(5):1120–4. doi: 10.1097/01.CCM.0000125517.28517.74. [DOI] [PubMed] [Google Scholar]
- 15.Meregalli A, Oliveira RP, Friedman G. Occult hypoperfusion is associated with increased mortality in hemodynamically stable, high-risk, surgical patients. Crit Care Lond Engl. 2004;8(2):R60–5. doi: 10.1186/cc2423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levraut J, Ichai C, Petit I, Ciebiera JP, Perus O, Grimaud D. Low exogenous lactate clearance as an early predictor of mortality in normolactatemic critically ill septic patients. Crit Care Med. 2003;31(3):705–10. doi: 10.1097/01.CCM.0000045561.85810.45. [DOI] [PubMed] [Google Scholar]
- 17.Levy B, Sadoune LO, Gelot AM, Bollaert PE, Nabet P, Larcan A. Evolution of lactate/pyruvate and arterial ketone body ratios in the early course of catecholamine-treated septic shock. Crit Care Med. 2000;28(1):114–9. doi: 10.1097/00003246-200001000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler J, et al. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32(8):1637–42. doi: 10.1097/01.CCM.0000132904.35713.A7. [DOI] [PubMed] [Google Scholar]
- 19.Jansen TC, van Bommel J, Mulder PG, Rommes J, Schieveld S, Bakker J. The prognostic value of blood lactate levels relative to that of vital signs in the pre-hospital setting: a pilot study. Crit Care Lond Engl. 2008;12(6):R160. doi: 10.1186/cc7159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seoane L, Papasidero M, De Sanctis P, Posadas-Martinez L, Soler S, Rodriguez M. Capillary lactic acid validation in an ED. Am J Emerg Med. 2013;31(9):1365–7. doi: 10.1016/j.ajem.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 21.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. 1992. Chest. 2009;136(5 Suppl):e28. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 22.Dugas AF, Mackenhauer J, Salciccioli JD, Cocchi M, Gautam S, Donnino M. Prevalence and characteristics of nonlactate and lactate expressors in septic shock. J Crit Care. 2012;27(4):344–50. doi: 10.1016/j.jcrc.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shapiro NI, Howell MD, Talmor D, Donnino M, Ngo L, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score predicts 1-year mortality. Crit Care Med. 2007;35(1):192–8. doi: 10.1097/01.CCM.0000251508.12555.3E. [DOI] [PubMed] [Google Scholar]


