Introduction and Background
The secondary neuroinflammatory response has attracted increasing attention in experimental stroke research.1 Analyses of immunologic mechanisms after acute stroke have been performed in the hope of identifying key pathomechanisms that contribute to secondary infarct growth and can be modulated to benefit a large proportion of stroke patients. Among a variety of pathophysiologic mechanisms, including microglial activation, brain leukocyte invasion, and secretion of pro-inflammatory factors, lymphocytes have been uncovered as the key leukocyte subpopulation that determines the neuroinflammatory outcome. Several studies have shown that pro-inflammatory lymphocytes, such as TH1, TH17, and γδ T-cells, worsen stroke outcome, and that blocking of their brain invasion is neuroprotective.2-4 Contrary to pro-inflammatory lymphocytes, regulatory T-cells (Treg) and B-cells (Breg) have been characterized as disease-limiting protective cells;5 in particular, in primary inflammatory diseases of the central nervous system (CNS). The discovery of the important role of Treg in other T-cell-driven pathologies has initiated productive research efforts on the role of Treg, including in ischemic brain injury, over the past years. However, due to the complex function of regulatory cells in immune homeostasis and disease, as well as partially divergent findings using different stroke models, uncertainty has emerged about the pathophysiologic function of regulatory lymphocytes in stroke.6-8 This article will comprehensively review current findings on regulatory lymphocytes in brain ischemia models and discuss potential reasons for the observed discrepancies.
Treg as Modulators of Post-Stroke Neuroinflammation
The immune system has evolved several regulatory mechanisms, including cell depletion, anergy, and unresponsiveness to autoantigens, to prevent damage of endogenous tissues due to an overshooting immune reaction. The presence of Treg actively suppressing autoimmune reactivity is one of the key mechanisms preserving immune homeostasis and limiting inflammatory collateral damage.9 Depletion of CD25+CD4+ Treg naturally arising in the immune system induces autoimmune diseases, and reconstitution of this cell population prevents disease development.10 A lack of Treg has been shown to be a primary cause of autoimmune diseases in humans.11 In addition to sustaining autotolerance, Treg are also involved in suppressive control of a broad spectrum of immune responses, including those against autologous tumor cells,12 allergens,13 and organ transplantation.14 Although Treg might be simplistically defined as immunosuppressive T-cells, several phenotypically and functionally distinct Treg subpopulations have been defined, such as induced Treg populations, Tr1, TH3, and various others.15 Yet, the best investigated population of Treg are CD4+CD25+Foxp3+ naturally occurring Treg, which are physiologically produced in the thymus as a mature cell population.16
While it is still unknown at which specific site Treg act as immunomodulators after stroke, their kinetics and magnitude of brain infiltration have been characterized in several studies using models of experimental middle cerebral artery occlusion (MCAO). The brain invasion of lymphocytes after murine focal brain ischemia was already observed more than two decades ago.17 One of the first studies systematically analyzing brain leukocyte invasion of brain homogenates after transient brain ischemia (filament-induced MCAO resulting in large hemispheric lesions) by flow cytometry was performed by Gelderblom et al.18 In this study, only a very low number of CD25+Foxp3+ Treg at a frequency of less than 5% of all CD4+ T-cells was observed within the first week after transient ischemia. In contrast, using a permanent MCAO model, we detected substantial T-cell and Treg counts in the ischemic hemisphere, with Foxp3+ Treg constituting ~20% of all CD4+ cells.19 This is consistent with the previous observation that distal permanent occlusion induces a significantly stronger neuroinflammatory reaction with manifold higher T-cell counts in the ischemic hemisphere than in proximal transient occlusion models.20 A more recent study by Stubbe et al investigated cerebral Treg up to 1 month after large hemispheric lesions.21 Although they detected only negligible amounts of Foxp3+ early after MCAO, substantial Treg invasion occurred 14 and 30 days after MCAO. Additionally, the percentage of Treg within the Thelper cell population was increased in brains after stroke compared with peripheral lymphatic organs.21
Despite their delayed recruitment in the brain, Treg have been found, in both depletion and therapeutic paradigms (see below), to influence stroke outcomes within the first days after ischemia. Such early effects prior to a considerable degree of Treg invasion into the brain prompts a rational assumption that Treg might have an early function in the ischemic brain by targeting cells in the peripheral immune system. In accordance with this assumption, delayed deletion of Treg by antibodies or in inducible Foxp3-knockout (Foxp3-KO) mice at 3 days after MCAO failed to alter stroke outcome.21, 22 Hence, although the definite site of action for Treg after stroke is still unsolved, currently available data suggest that Treg have an immunomodulatory function within the first 3 days after stroke when they still remain outside of the CNS. Potential peripheral functions of Treg might include suppression of peripheral effector T-cell activation, inhibition of autoantigen-specific clonal expansion, or priming of transendothelial effector T-cell migration via currently unknown mechanisms. An additional – probably non-immunologic – function of Treg has been proposed for the development of secondary microthrombosis in models of transient mechanical vascular occlusion (TMVO), which was termed thromboinflammation.23 This concept of thromboinflammatory infarct progression proposes an interaction of Treg with platelets and the activated endothelium as an independent mechanism of Treg function.
Treg Depletion in Experimental Brain Ischemia
Depletion of the Treg population is a common experimental paradigm to investigate the functional role of Treg in brain ischemia in several publications. Methodologically, two principally different approaches have been used to deplete Treg: antibody-mediated cell lysis, using CD25-specific antibodies; or the use of transgenic mice with a diphtheria toxin receptor (DTR) transgene under the control of the Foxp3 promoter for inducible Treg depletion. Using Treg-depletion paradigms, about half of the experiments performed revealed an increase in infarct volume,19, 22, 24 while the other half did not detect any effect on stroke outcome,19, 21, 22, 25, 26 and one study even observed a reduction of infarct size in Treg-deficient mice23 (Table 1).
Table 1.
Summary of studies investigating Treg depletion paradigms
| Study | Model | Lesion (% hemisphere) |
Latest endpoint |
Depletion model |
Depletion efficacy |
Outcome on infarct vol. |
|---|---|---|---|---|---|---|
| Liesz et al., 200919 |
Distal, permanent |
≈ 10% | 7d | 1) Anti- CD25 |
90% | Increased |
| 2) Adoptive cell transfer |
n.a. | |||||
| Liesz et al., 201322 |
Distal, permanent |
≈ 10% | 7d | Foxp3-KO | 85% | Increased |
| 30min transient | ≈ 10% | 7d | Anti-CD25 | 90% | Increased | |
| Xie et al.24 | Rats: 90min transient |
≈ 40% | 3d | Anti-CD25 | 65% | Increased |
| Liesz et al., 200919 |
90min transient | ≈ 55% | 7d | Anti-CD25 | 90% | No effect |
| Ren et al.25 | 60min transient | ≈ 55% | 3d | Foxp3-KO | 90% | No effect |
| Li et al. 201326 | 60min transient | ≈ 50% | 3d | Anti-CD25 | 90% | No effect |
| Stubbe et al.21* |
30min transient | ≈ 50% | 27d | Anti-CD25 | 75% | No effect |
| Liesz et al., 201322 |
60min transient | ≈ 50% | 3d | Foxp3-KO | 85% | No effect |
| Kleinschnitz et al.23 |
60min transient | ≈ 55% | 7d | Foxp3-KO | 90% | Reduced |
depletion 3d after MCAO induction; in all other studies: pretreatment or acute depletion
This discrepancy triggered an intense debate on the biological role of Treg in stroke and led to the denomination of Treg as a “double-edged sword” in acute brain injury.27-29 Of note, inconsistencies cannot be attributed to the various depletion paradigms used, since transgenic mouse models have been used on both sides of the “efficacy spectrum”. However, in each of the three publications reporting genetic depletion of Treg, a different inducible Foxp3-KO mouse line has been used: Ren et al25 used the original Foxp3DTR mouse,30 Liesz et al22 the Foxp3.LuciDTR.4 mouse line,31 and Kleinschnitz et al23 the DEREG mouse.32 Each of these DTR-transgene-mediated Foxp3-deletion models are derived from different transgene constructs. Moreover, they vary regarding the efficacy of Treg depletion and the respective diphtheria toxin treatment protocols. Although most studies reported Treg-depletion efficacy of more than 80%, individual extent of Treg-depletion differs considerably (cp. Table 1) and most studies did not investigate organ-specific Treg-depletion, the kinetics of depletion and reconstitution of the Treg population. In contrast, it is apparent that the stroke models utilized, and more precisely the resulting volume of the ischemic lesion, do indeed predict the functional role of Treg in depletion paradigms.
Both studies from Liesz et al found an increase in stroke volume after Treg depletion only in small permanent ischemia lesion models, but not after extensive infarction induced by transient MCAO.19, 22 A recent study by Xie et al also described larger infarct volumes after antibody-mediated Treg depletion in a rat model of moderate brain ischemia.24 In contrast, all studies describing unaltered19, 21, 22, 25, 26 or even improved23 outcome after Treg depletion were performed in transient mechanical occlusion models causing extensive brain lesions.
The immunologic effects of Treg depletion on the neuroinflammatory outcome after stroke have unfortunately been addressed in only a small number of the above studies. All three studies detecting an exacerbation of stroke outcome after Treg depletion also measured an associated increase in neuroinflammatory biomarkers.19, 22, 24 The most robust findings included an increase in leukocyte brain invasion, particularly of distinct lymphocyte subpopulations, and an increase in pro-inflammatory cytokine secretion, such as tumor necrosis factor α, interleukin (IL)-1β, IL-12, and interferon γ. Among the studies using models of extensive brain injury with no effect of Treg depletion on stroke outcome, only one study has investigated neuroimmunologic readouts with correspondingly unaltered inflammatory markers.21 In contrast, the study by Kleinschnitz et al investigating the role of Treg in thromboinflammation and stroke progression has detected a detrimental role of Treg in mediating post-stroke neurodegeneration, independent of their immunologic function.23 Interestingly, “wannabe Treg” without immunomodulatory function were still able to exert their impact on stroke progression without affecting neuroinflammatory markers, supporting the hypothesis of non-immunologic functions of Treg after stroke.
Therapeutic Enhancement of Treg Function in Brain Ischemia
Despite the obvious and still unresolved discrepancies arising from studies investigating the effects of Treg depletion, a rapidly increasing number of reports have tested Treg augmentation for stroke therapy. These studies have investigated very different approaches to increase Treg numbers and/or function. The most intuitive approach might be the adoptive cell transfer of purified Treg to wild-type animals to increase circulating Treg numbers. The second most widely used approach was the administration of a CD28 superagonist (CD28SA), which induces in vivo expansion of Treg and amplification of their suppressive function. In addition, histone deacetylase (HDAC) inhibition and treatment with a mammalian target of rapamycin (mTOR) inhibitor have previously been shown to boost Treg by increasing Foxp3 expression in T-cells. A pathomechanistically very different approach used in earlier studies was the paradigm of “mucosal immunization” with mucosal administration of cerebrovascular antigens, such as myelin oligodendrocyte glycoprotein or selectins, which induce the expansion of autoantigen-specific Treg33, 34.
Out of 15 independent experiments reported in 13 studies, 13 found an improvement in stroke outcome22, 24, 26, 33-39, while two described an increase in infarct volume when using two independent Treg-targeted therapies.23, 40 This discrepancy cannot be easily explained by the therapeutic paradigm used, since the methods of adoptive Treg transfer into wild-type mice and the CD28SA treatment utilized in the two studies showing an exacerbation of lesion volume were also tested in three or more other experiments that showed an improved outcome (Table 2).
Table 2.
Studies investigating Treg-targeted therapeutic approaches (by treatment and outcome)
| Study | Model | Lesion (% hemisphere) |
Latest endpoint |
Treatment paradigm |
Outcome on infarct volume |
|---|---|---|---|---|---|
| Chen et al.36 | Rats: distal, permanent |
≈ 20% | 48h | Mucosal immunization |
Reduced |
| Gee et al.33 | Rats: 3h transient |
Infarct vol. NA* |
28d | Mucosal immunization |
Reduced (Behavior) |
| Ishibashi et al.34 | Rats: distal, permanent |
≈ 20% | 28d | Mucosal immunization |
Reduced |
| Li et al. 201326 | Rats: 2h transient |
≈ 40% | 3d | Adoptive transfer |
Reduced |
| Mouse: 60min transient |
≈ 35% | 3d | Adoptive transfer |
Reduced | |
| Li et al., 201338 | Mouse: 60min transient |
≈ 35% | 3d | Adoptive transfer |
Reduced |
| Li et al., 201437 | Mouse: 60min transient |
≈ 35% | 3d | Adoptive transfer |
Reduced |
| Brea et al.35 | Rat: transient | ≈ 30% | 28d | Adoptive transfer |
Reduced |
| Liesz et al. 201322 | Mouse: distal, permanent |
≈ 10% | 7d | HDACi | Reduced |
| Brea et al.35 | Rat: transient | ≈ 30% | 10d | CD28SA | Reduced |
| Na et al.39 | Mouse: distal, permanent |
≈ 10% | 7d | CD28SA | Reduced |
| Mouse: 60min transient |
≈ 50% | 3d | CD28SA | Reduced | |
| Xie et al.24 | Rats: 90min transient |
≈ 45% | 28d | mTOR Inh. | Reduced |
| Kleinschnitz et al.23 |
Mouse: 60min transient |
≈ 55% | 3d | Adoptive transfer |
Increased |
| Schuhmann et al.40 |
Mouse: 60min transient |
≈ 40% | 3d | CD28SA | Increased |
this study analyzed behavioral deficits as the primary outcome and did not report infarct volume
Again, it appears that stroke severity might predict the net biologic effect of Treg: out of the 13 experiments detecting an overall benefit of therapeutically enhancing Treg numbers and/or function, only two have reported infarct volumes in the control group of more than 40% of the ipsilesional hemisphere, while the other studies deployed models that induce only small- to moderate-sized lesions. Surprisingly however, the two studies,39, 40 in which the identical CD28SA has been used in very similar stroke models reported opposing results. Na et al described reduced infarct volumes and an improved functional outcome following treatment with the CD28SA,39 while Schuhmann et al described a significant worsening of stroke, indicating the presence of other confounding factors independent of lesion volume to Treg function.40
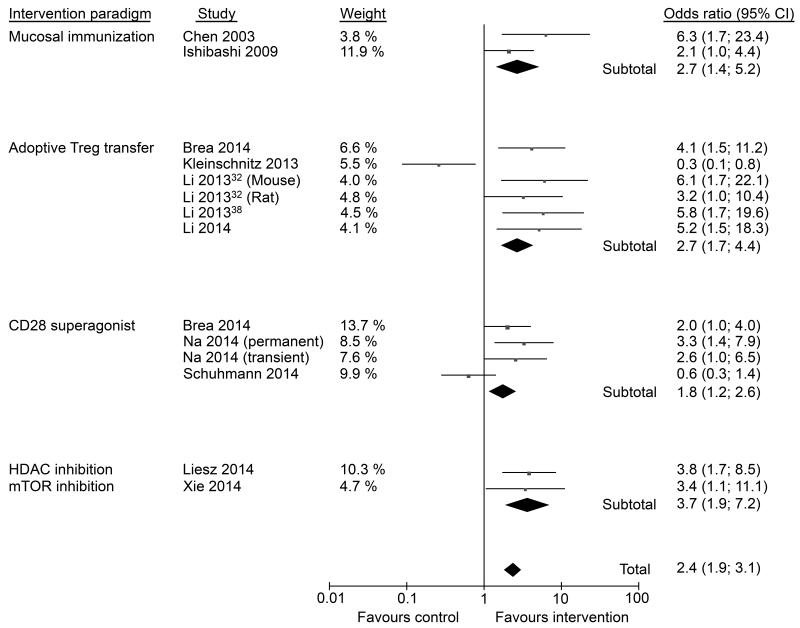
We have performed a Meta-analysis in order to more precisely estimate the efficacy of Treg-targeted therapeutic approaches in experimental stroke models. For this purpose, all studies that investigated interventions with the aim to modulate Treg (defined at least by CD25- or Foxp3-expressing CD4+ T-cells) numbers and/or Treg function in models of experimental brain ischemia were included in the analysis. The studies were clustered by the respective treatment paradigm: mucosal immunization,34, 36 adoptive Treg transfer,23, 26, 35, 37,38 CD28SA,35, 39, 40 and others (i.e. HDAC inhibition22 and mTOR inhibition24). Effect size estimates (odds ratio) were calculated and the forest plot illustrated using RevMan software (version 5.3).
The overall effect size estimation revealed an odds ratio favoring the respective intervention for each interventional paradigm and for all studies in total (Figure 1). However, a large heterogeneity between the included studies regarding study design, experimental model, and species (rat and mice) has to be taken into account. In addition, several studies did not report sufficient information to assure quality according to the Stroke Therapy Academic Industry Roundtable (STAIR) recommendations. Therefore, the number of studies investigating Treg interventions needs to be increased to more robustly estimate a realistic effect size. Also, the publication of negative results has to be encouraged to avoid a publication bias in such an emerging research field.
Figure 1. Forest plot for meta-analysis of regulatory T-cell (Treg)-targeted therapies in experimental stroke.
The meta-analysis includes all published studies until December 2014 investigating Treg (at least characterized by CD25- and/or Foxp3-expressing CD4+ cells) in rodent stroke models. Odds ratios were calculated using inverse variance in a fixed effects model. CI, confidence interval.
Mechanisms of Treg Function in Post-Stroke Neuroinflammation
Basic immunologic research on Treg function has identified several mechanisms by which Treg suppress immune reactions.41 These can be mainly divided into mechanisms acting on lymphocyte activation and mechanisms inhibiting antigen-presenting cells. While most of these mechanisms can be recognized using in vitro model systems, the contribution of individual mechanisms, such as different anti-inflammatory cytokines or cell–cell contact-dependent suppression, is highly diverse among in vivo disease models. The most prominent mechanisms of Treg function in vivo are the secretion of anti-inflammatory cytokines (IL-10, tumor growth factor β (TGF-β), expression of immunosuppressant molecules (CTLA-4, CD39, PD-1), consumption of vital cytokines (IL-1, IL-2) and the secretion of cytolytic molecules (granzymes, perforin).5
In the context of experimental brain ischemia, several studies have demonstrated that IL-10 is a critical neuroprotective cytokine regulating post-stroke neuroinflammation.42-45 The main sources of cerebral IL-10 are Treg, Breg, and microglia/monocytes. The property of IL-10 as an important tissue protective effector mechanism of Treg46 was verified in some of the previous stroke studies.19, 22, 47 Accordingly, strategies increasing lymphocyte-derived IL-10 production22, 39, 44, 48 or therapeutic IL-10 administration42, 45, 49 have been shown to improve stroke outcome. In addition, alternative Treg-related mechanisms have been found to act in ischemic brains, such as the expression of TGF-β and IL-3524 as well as a role of Treg in the PD-1/PD-L1 pathway. However, whereas the immune regulatory function of PD-1 limits ischemic brain lesions and blood-brain barrier damage,37 PD-L1 appears to have an opposing, i.e. detrimental, effect in stroke.50 Pro-inflammatory lymphocytes and brain-resident microglia/macrophages have been characterized as the main target cells for the immunosuppressive effect of Treg after brain injury19, 22, 26. The beneficial effect of Treg at later stages of ischemic stroke was frequently related to the reduced invasion of T-cells,19, 26 suppression of effector T-cell proliferation,22 suppressed cytokine production,24, 26, 34 reduced microglia/monocyte activation,19 or a priming towards a M2-like microglial phenotype.24 In contrast, studies reporting an exacerbation of stroke by Treg-targeted therapies during the very early stage23, 40 found an association of increased lesion volumes with amplified cerebral immune cell accumulation.40 However, evidence exists that the deleterious effects observed with Treg in these two studies might be independent of their immunologic function, but rather attributable to an impact on secondary microthrombosis (thrombo-inflammation).23
Other Regulatory Lymphocyte Subpopulations: Breg and CD8+CD122+ Treg
Some of the previous studies have investigated a potential regulatory function of B-cells and detected an increase in stroke lesions in B-cell-depleted mice,51 while other reports could not confirm this observation.52, 53 While the adoptive transfer of B-cells to lymphocyte-deficient Rag−/− did not affect outcome in the early phase after stroke,53 subsequent studies reported substantial IL-10 production by B-cells and neuroprotective effects of transferring wild-type, but not IL-10-deficient, B-cells to limit stroke severity.44, 51, 54 Further studies revealed that the transferred IL-10+ B-cells included roughly equal proportions of several known Breg subtypes, including the B10, T2-MZ, and B1a subpopulations. In addition, it was observed in one study that transferred B-cells had systemic immunomodulatory effects and mitigated splenic atrophy and induced Treg populations.55 It was further demonstrated that direct transfer of IL-10-secreting B-cells into the striatum limited stroke lesions.56 A more recent experiment confirmed a potentially neuroprotective function of regulatory IL-10-producing B-cells after stroke by inducing CD8+CD122+ Treg and ameliorating post-stroke neuroinflammation.57 Taken together, the findings of previous studies not observing a major role for B-cells in the acute phase after stroke and more recent reports of a neuroprotective function of Breg in later secondary neuroinflammatory response might support an immunoregulatory effect of IL-10-secreting B-cells and their induction of CD8+CD122+ Treg at later stages of post-stroke neuroinflammation. Considering the previously observed differences in natural Treg function between stroke models, it will be of interest for future studies to also investigate such a differential role for other regulatory lymphocytes, such as Breg and CD8+CD122+ Treg.
Tregs in the Peripheral Immune System After Stroke
Acute brain ischemia induces profound alterations of the peripheral immune reaction, encompassing peripheral immune activation in the acute phase after brain injury58 and features of an immunosuppressive syndrome in the later phase.59 In addition to the effect of Treg in directly modulating local neuroinflammation within the brain, they also play a role in altering the peripheral immune response after stroke. A consistent finding in the subacute phase after extensive experimental stroke is that cellular immunosuppression and splenic atrophy are accompanied by a relative expansion of Treg in the spleen and blood.60, 61 However, regulatory T-cells themselves do not contribute to the exacerbation of post-stroke immunosuppression.38, 62 Interestingly, a recent report even suggested that the adoptive transfer of Treg on the one side reduced the systemic inflammatory reaction in the early phase after stroke, while on the other it also ameliorated the extent of immunosuppression (i.e. lymphopenia) in the later phase.38 This finding of a dualistic role of Treg in systemic immunity when comparing the acute with subacute phases after stroke is well in line with the concept that the initial over-activation of the peripheral immune system might result in an immunosuppression syndrome.63 The potent homeostatic function of Treg might help to suppress the initial systemic inflammation, thereby attenuating the subsequent immune disturbances, such as activation-induced lymphopenia and exhaustion of antigen-presenting cells.
In addition, a recent study has detected the expansion of Foxp3+ natural Treg in the bone marrow of mice after extensive brain ischemia.64 It was proposed that this myeloid Treg expansion is related to sympathetic stress signaling after brain ischemia. However, whether this observation of myeloid Treg is functionally related to the previously observed alterations in bone marrow monocyte populations63 and hematopoiesis65 after stroke is currently unknown.
Only very few studies have investigated regulatory T-cells in patients suffering from acute brain ischemia. Understandably, these studies have focused on peripheral immune effects after stroke by investigating blood samples of patients with different stroke entities. The first study specifically analyzing Treg function after stroke by Hug et al. has found that Treg function is preserved in the context of post-stroke immunosuppression in contrast to the dysfunction of effector cell populations such as circulating monocytes or helper T-cells. 66 In contrast, a second study has found reduced suppressive capacities of post-stroke Treg in female but not male stroke patients, proposing sex-specific effects on post-stroke peripheral immunity. 67 This difference between the studies could be explained by differing patient characteristics in terms of comorbidities and stroke severity. While the latter study has detected a robust increase of Treg cell counts after stroke in accordance with experimental studies, another report has shown the opposite. Li et al. reported a significant reduction of peripheral Treg in stroke patients. 68 In contrast to the previous studies investigating post-stroke effects on peripheral Treg function, a report by Wigren et al., analyzed the association of Treg counts in a cohort of 700 participants of the Malmö Diet and Cancer study with the prospective incidence of stroke. While low Treg counts at baseline were associated with an increased risk of myocardial infarction this association was not present for stroke. 69 Overall, clinical data is supporting the experimental finding of substantial peripheral immunomodulation after stroke, which is also affecting the Treg population, yet, specific changes might depend on stroke entity, severity and patient characteristics.
Potential Reasons for the Discrepancies on Treg Function in Post-Stroke Neuroinflammation
Thromboinflammation and Secondary Microthrombosis
The commonly used model of transient MCAO using intraluminal filaments (a model that was used in the two studies detecting a deleterious role of Treg in stroke23, 40) can be described as a TMVO model with prompt revascularization. One prominent and distinct feature of this model is the occurrence of delayed neuronal damage due to microthrombosis and thromboinflammation.70 In contrast, secondary microthrombosis was not observed in rodents and non-human primates with gradual reperfusion.71 The occurrence of microthrombosis/thromboinflammation in stroke patients is currently still elusive. Although the distinct factors contributing to the development of thromboinflammation in TMVO are still unclear, several potential mechanisms could be assumed: the extent of endothelial activation induced by the reperfusion, the speed of filament retraction and prompt versus gradual reperfusion, and the occlusion time. Finally, these at-first-sight minor methodological differences might finally have a major pathophysiologic impact by the presence or absence of secondary thrombosis. In the case of microthrombosis after prompt revascularization, the cascade of endothelial activation, thromboinflammation, and microvascular dysfunction not only leads to secondary ischemic infarct progression, but might also induce vascular inflammation and an alteration of the neuroinflammatory response to brain ischemia per se.
The Impact of Lesion Volume and Reperfusion on Stroke Immunology
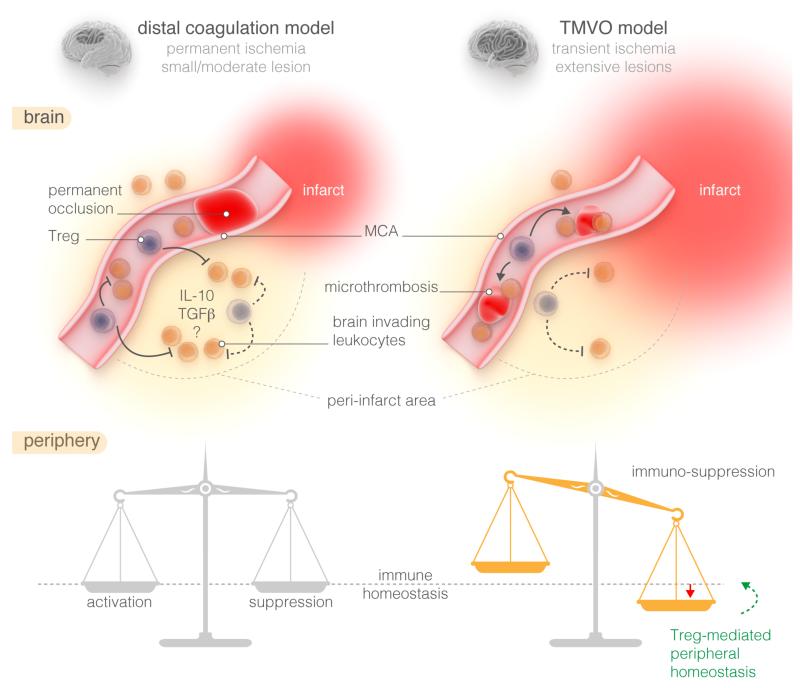
As noted above, it seems that lesion size and/or reperfusion might be relevant confounders of secondary neuroinflammation. It is well acknowledged that the phenomenon of post-stroke peripheral immunosuppression occurs in stroke patients and animal stroke models only after extensive brain tissue injury.59, 61, 72, 73 While mice and humans with substantial brain lesions develop lymphopenia and alterations of the monocyte population, small ischemic injuries induce only a minor immunomodulation, but no immunosuppressive syndrome. Whereas, to the best of our knowledge, the impact of peripheral immunosuppression after major stroke on secondary neuroinflammation has not been systematically investigated until now, it is conceivable that peripheral immune alterations might also affect central neuroinflammation. Indeed, a previous study performing a face-to-face comparison of the extent of cerebral leukocyte invasion, microglial activation, and cytokine secretion in three common models of brain ischemia of differing lesion size detected crucial differences among models with a manifold stronger inflammatory reaction in small permanent ischemia models than in extensive hemispheric lesions after transient MCAO.20 Moreover, a more recent study has investigated the neuroinflammatory reaction in the acute phase (<24h) after transient or permanent malignant infarctions induced by the filament model. The authors detected significantly less leukocyte brain infiltration after transient ischemia, as it was used in the majority of studies analyzed in this review, compared to permanent proximal MCA occlusion.74 Therefore, it is plausible that Treg have an inferior role in stroke models with only minor bystander inflammation compared with the critical role of Treg in lesion models with an over-shooting immune reaction (Figure 2). However, it is currently still unclear if these detrimental differences in neuroinflammatory response are indeed related to factors such as lesion volume, reperfusion and localization or are merely an epiphenomenon due to technical aspects of the particular stroke model (i.e. differences in skull trepanation, surgical wound, pain, and food intake).
Figure 2. Proposed mechanism of differential regulatory T-cell (Treg) function in permanent/small-lesion versus transient mechanical vascular occlusion (TMVO)/extensive-lesion models.
The schematic diagram illustrates the discrepancy of the observed role of Treg in brain (upper panels) versus peripheral immune system (lower panels) in models of permanent ischemia with small- to moderate-sized lesions or after extensive brain lesions in TMVO models. Permanent occlusion of the distal middle cerebral artery (MCA; left panels) induces a strong neuroinflammatory reaction, but preserves peripheral immune homeostasis with only minor immunomodulation. In this context, Treg have a primary role in inhibiting an overshooting inflammatory reaction mediated by pro-inflammatory leukocytes. It is assumed that this immunosuppressive function of Treg takes place in the periphery even before brain invasion. In contrast, TMVO models with extensive brain injuries (right panels) have less pronounced neuroinflammation, but induce an immunosuppressive phenotype of the peripheral immune system. Here, Treg have only a minor function in suppressing the neuroinflammatory response, and might even have a non-immunologic function in the manifestation of secondary microthrombosis and thromboinflammation. The principal role of Treg in TMVO models seems rather to be in ameliorating immune disturbances by inhibiting initial immunologic activation or over-activation and later immunosuppression, thereby preserving homeostatic systemic immune function. IL-10, interleukin 10; TGFβ, tumor growth factor β.
Milieu-Dependent Treg Function
Moreover, the above-stated methodologic differences, including the presence of microthrombosis/thromboinflammation, induction of peripheral immune alterations, and the extent of neuroinflammation, might have a direct impact on the functional properties of natural Treg. It is known from other disease paradigms that Treg function in vivo might by particularly dependent on the immunologic milieu. For example, in cancer research, this phenomenon – very much akin to stroke immunology – has been termed the “Janus-faced function of Treg”.75, 76 In addition, the currently predominant perception of neuroinflammation after acute brain injury and particularly stroke research as too much of a bad thing should be revisited. Several elegant reports by the groups of Michal Schwartz and Jonathan Kipnis have established the concept of “protective autoimmunity” (see Schwartz and Raposo77 for a recent review of the concept). This concept ascribes secondary inflammation as a generally physiologic and protective mechanism in which too much immune activation as well as immunosuppression might be deleterious. Accordingly, in certain situations of acute brain lesions and neurodegeneration models – determined by the time-dependent inflammatory milieu of the brain during disease progression, both Treg depletion as well as its augmentation might negatively affect the outcome.78-80 Therefore, the very specific properties of the stroke model used and targeted mechanism of Treg function have to be carefully investigated before considering Treg in a potentially oversimplified view as good or bad immune cells after stroke.
Quo Vadis: Treg in Stroke – Open Questions and Required Experiments
As comprehensively reported above, rapidly accumulating data by a number of studies in the last few years have clearly indicated a pathophysiological role for Treg in the secondary neuroinflammation as well as more remote effects in the vasculature and the peripheral immune system after stroke. Yet, some controversies are still unresolved and important questions not been addressed so far: What is the contribution of lesions size, location and reperfusion to post-stroke neuroinflammation – and what is the pathophysiological basis for the immunological differences between stroke subtypes? Where is the primary site of Treg-function – in the peripheral immune system by preserving immune homeostasis or in the CNS suppressing neuroinflammation? Which of the diverse Treg-targeted immunotherapeutic approaches is most effective and clinically relevant?
While further exploratory studies will be needed to address these questions - such as comparing stroke models and intervention paradigms in one laboratory face-to-face approaches instead of compiling data sets from different models, laboratories, treatment and analysis strategies – the next step in Treg-targeted research for stroke will be to proceed from exploratory studies to confirmatory research in order to pave the way for potential translation.81 As for other emerging research areas that are challenged by preclinical controversies, collaborative research efforts with rigorous guidelines for study design, conductance and analysis will be necessary to resolve current controversies on the role of Treg and particularly their use as immunotherapeutic targets for treating brain ischemia.82
Conclusion
Taken together, it can be well acknowledged that Treg constitute a highly potent cell population that is capable of modulating various immunologic pathways. Yet, their functional role in acute brain injuries might be much more complicated and diverse than currently appreciated. Although a meta-analysis of currently published Treg-targeted immunotherapies might indicate an overall neuroprotective function of Treg, at least during the later stages of infarct development, their role during the very acute phase is much less clear, and we need first to better understand their distinct function in diverse settings of secondary neuroinflammation before promoting Treg-targeted cell therapies for clinical testing. Therefore, we should be careful with generalizations of findings from different animal stroke models that critically differ in their inflammatory response. Instead we should use this vast variability and the distinct properties of the commonly used stroke models as a chance to investigate, in more detail, the spectrum of neuroinflammation in this highly diverse disease. Not only in stroke models, but certainly also in stroke patients, the impact of neuroinflammation might crucially differ depending on stroke subtype, localization, time pattern, and comorbidities. This individualized view on post-stroke inflammatory mechanisms is still in its infancy, but will ultimately be inevitable for a future personalized stroke immunotherapy that has to stratify patients that might potentially benefit from immune-targeted approaches.
Acknowledgments
Sources of Funding
This work was supported by grants from the German Research Foundation (DFG), project LI2534/1-1 to A.L. and the collaborative research center 688, project A13 and KL2323/6-1 to C.K.; a grant from the American Heart Association (13SDG14570025) to X.H.; and a NIH grant (1RO1 NS075887) to H.O.
Footnotes
Disclosures
The authors have nothing to declare.
References
- 1.Iadecola C, Anrather J. The immunology of stroke: From mechanisms to translation. Nat Med. 2011;17:796–808. doi: 10.1038/nm.2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shichita T, Sugiyama Y, Ooboshi H, Sugimori H, Nakagawa R, Takada I, et al. Pivotal role of cerebral interleukin-17-producing gammadeltat cells in the delayed phase of ischemic brain injury. Nat Med. 2009;15:946–950. doi: 10.1038/nm.1999. [DOI] [PubMed] [Google Scholar]
- 3.Gelderblom M, Weymar A, Bernreuther C, Velden J, Arunachalam P, Steinbach K, et al. Neutralization of the il-17 axis diminishes neutrophil invasion and protects from ischemic stroke. Blood. 2012;120:3793–3802. doi: 10.1182/blood-2012-02-412726. [DOI] [PubMed] [Google Scholar]
- 4.Liesz A, Zhou W, Mracsko E, Karcher S, Bauer H, Schwarting S, et al. Inhibition of lymphocyte trafficking shields the brain against deleterious neuroinflammation after stroke. Brain. 2011;134:704–720. doi: 10.1093/brain/awr008. [DOI] [PubMed] [Google Scholar]
- 5.Sakaguchi S, Miyara M, Costantino CM, Hafler DA. Foxp3+ regulatory t cells in the human immune system. Nat Rev Immunol. 2010;10:490–500. doi: 10.1038/nri2785. [DOI] [PubMed] [Google Scholar]
- 6.Schabitz WR. Regulatory t cells in ischemic stroke: Helpful or hazardous? Stroke. 2013;44:e84. doi: 10.1161/STROKEAHA.113.002228. [DOI] [PubMed] [Google Scholar]
- 7.Xu X, Li M, Jiang Y. The paradox role of regulatory t cells in ischemic stroke. TheScientificWorldJournal. 2013;2013:174373. doi: 10.1155/2013/174373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen S, Wu H, Klebe D, Hong Y, Zhang J, Tang J. Regulatory t cell in stroke: A new paradigm for immune regulation. Clinical & developmental immunology. 2013;2013:689827. doi: 10.1155/2013/689827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sakaguchi S. Regulatory t cells: Key controllers of immunologic self-tolerance. Cell. 2000;101:455–458. doi: 10.1016/s0092-8674(00)80856-9. [DOI] [PubMed] [Google Scholar]
- 10.Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic self-tolerance maintained by activated t cells expressing il-2 receptor alpha-chains (cd25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol. 1995;155:1151–1164. [PubMed] [Google Scholar]
- 11.Ochs HD, Ziegler SF, Torgerson TR. Foxp3 acts as a rheostat of the immune response. Immunol Rev. 2005;203:156–164. doi: 10.1111/j.0105-2896.2005.00231.x. [DOI] [PubMed] [Google Scholar]
- 12.Baecher-Allan C, Anderson DE. Regulatory cells and human cancer. Seminars in cancer biology. 2006;16:98–105. doi: 10.1016/j.semcancer.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Chatila TA. Role of regulatory t cells in human diseases. The Journal of allergy and clinical immunology. 2005;116:949–959. doi: 10.1016/j.jaci.2005.08.047. quiz 960. [DOI] [PubMed] [Google Scholar]
- 14.Battaglia M, Roncarolo MG. Induction of transplantation tolerance via regulatory t cells. Inflammation & allergy drug targets. 2006;5:157–165. doi: 10.2174/187152806778256052. [DOI] [PubMed] [Google Scholar]
- 15.Jiang H, Chess L. Regulation of immune responses by t cells. N Engl J Med. 2006;354:1166–1176. doi: 10.1056/NEJMra055446. [DOI] [PubMed] [Google Scholar]
- 16.Shevach EM, DiPaolo RA, Andersson J, Zhao DM, Stephens GL, Thornton AM. The lifestyle of naturally occurring cd4+ cd25+ foxp3+ regulatory t cells. Immunol Rev. 2006;212:60–73. doi: 10.1111/j.0105-2896.2006.00415.x. [DOI] [PubMed] [Google Scholar]
- 17.Schroeter M, Jander S, Witte OW, Stoll G. Local immune responses in the rat cerebral cortex after middle cerebral artery occlusion. J Neuroimmunol. 1994;55:195–203. doi: 10.1016/0165-5728(94)90010-8. [DOI] [PubMed] [Google Scholar]
- 18.Gelderblom M, Leypoldt F, Steinbach K, Behrens D, Choe CU, Siler DA, et al. Temporal and spatial dynamics of cerebral immune cell accumulation in stroke. Stroke. 2009;40:1849–1857. doi: 10.1161/STROKEAHA.108.534503. [DOI] [PubMed] [Google Scholar]
- 19.Liesz A, Suri-Payer E, Veltkamp C, Doerr H, Sommer C, Rivest S, et al. Regulatory t cells are key cerebroprotective immunomodulators in acute experimental stroke. Nat Med. 2009;15:192–199. doi: 10.1038/nm.1927. [DOI] [PubMed] [Google Scholar]
- 20.Zhou W, Liesz A, Bauer H, Sommer C, Lahrmann B, Valous N, et al. Postischemic brain infiltration of leukocyte subpopulations differs among murine permanent and transient focal cerebral ischemia models. Brain Pathol. 2013;23:34–44. doi: 10.1111/j.1750-3639.2012.00614.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stubbe T, Ebner F, Richter D, Engel O, Klehmet J, Royl G, et al. Regulatory t cells accumulate and proliferate in the ischemic hemisphere for up to 30 days after mcao. J Cereb Blood Flow Metab. 2013;33:37–47. doi: 10.1038/jcbfm.2012.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liesz A, Zhou W, Na SY, Hammerling GJ, Garbi N, Karcher S, et al. Boosting regulatory t cells limits neuroinflammation in permanent cortical stroke. J Neurosci. 2013;33:17350–17362. doi: 10.1523/JNEUROSCI.4901-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleinschnitz C, Kraft P, Dreykluft A, Hagedorn I, Gobel K, Schuhmann MK, et al. Regulatory t cells are strong promoters of acute ischemic stroke in mice by inducing dysfunction of the cerebral microvasculature. Blood. 2013;121:679–691. doi: 10.1182/blood-2012-04-426734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xie L, Sun F, Wang J, Mao X, Xie L, Yang SH, et al. Mtor signaling inhibition modulates macrophage/microglia-mediated neuroinflammation and secondary injury via regulatory t cells after focal ischemia. J Immunol. 2014;192:6009–6019. doi: 10.4049/jimmunol.1303492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ren X, Akiyoshi K, Vandenbark AA, Hurn PD, Offner H. Cd4+foxp3+ regulatory t-cells in cerebral ischemic stroke. Metab Brain Dis. 2011;26:87–90. doi: 10.1007/s11011-010-9226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li P, Gan Y, Sun BL, Zhang F, Lu B, Gao Y, et al. Adoptive regulatory t-cell therapy protects against cerebral ischemia. Ann Neurol. 2013;74:458–471. doi: 10.1002/ana.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kleinschnitz C, Wiendl H. Con: Regulatory t cells are protective in ischemic stroke. Stroke. 2013;44:e87–88. doi: 10.1161/STROKEAHA.113.001268. [DOI] [PubMed] [Google Scholar]
- 28.Hu X, Li P, Chen J. Pro: Regulatory t cells are protective in ischemic stroke. Stroke. 2013;44:e85–86. doi: 10.1161/STROKEAHA.113.001267. [DOI] [PubMed] [Google Scholar]
- 29.Urra X, Cervera A, Villamor N, Planas AM, Chamorro A. Harms and benefits of lymphocyte subpopulations in patients with acute stroke. Neuroscience. 2009;158:1174–1183. doi: 10.1016/j.neuroscience.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 30.Kim JM, Rasmussen JP, Rudensky AY. Regulatory t cells prevent catastrophic autoimmunity throughout the lifespan of mice. Nat Immunol. 2007;8:191–197. doi: 10.1038/ni1428. [DOI] [PubMed] [Google Scholar]
- 31.Suffner J, Hochweller K, Kuhnle MC, Li X, Kroczek RA, Garbi N, et al. Dendritic cells support homeostatic expansion of foxp3+ regulatory t cells in foxp3.Lucidtr mice. J Immunol. 2010;184:1810–1820. doi: 10.4049/jimmunol.0902420. [DOI] [PubMed] [Google Scholar]
- 32.Lahl K, Loddenkemper C, Drouin C, Freyer J, Arnason J, Eberl G, et al. Selective depletion of foxp3+ regulatory t cells induces a scurfy-like disease. J Exp Med. 2007;204:57–63. doi: 10.1084/jem.20061852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gee JM, Kalil A, Thullbery M, Becker KJ. Induction of immunologic tolerance to myelin basic protein prevents central nervous system autoimmunity and improves outcome after stroke. Stroke. 2008;39:1575–1582. doi: 10.1161/STROKEAHA.107.501486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ishibashi S, Maric D, Mou Y, Ohtani R, Ruetzler C, Hallenbeck JM. Mucosal tolerance to e-selectin promotes the survival of newly generated neuroblasts via regulatory t-cell induction after stroke in spontaneously hypertensive rats. J Cereb Blood Flow Metab. 2009;29:606–620. doi: 10.1038/jcbfm.2008.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brea D, Agulla J, Rodriguez-Yanez M, Barral D, Ramos-Cabrer P, Campos F, et al. Regulatory t cells modulate inflammation and reduce infarct volume in experimental brain ischaemia. Journal of cellular and molecular medicine. 2014;18:1571–1579. doi: 10.1111/jcmm.12304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen Y, Ruetzler C, Pandipati S, Spatz M, McCarron RM, Becker K, et al. Mucosal tolerance to e-selectin provides cell-mediated protection against ischemic brain injury. Proc Natl Acad Sci U S A. 2003;100:15107–15112. doi: 10.1073/pnas.2436538100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li P, Mao L, Liu X, Gan Y, Zheng J, Thomson AW, et al. Essential role of program death 1-ligand 1 in regulatory t-cell-afforded protection against blood-brain barrier damage after stroke. Stroke. 2014;45:857–864. doi: 10.1161/STROKEAHA.113.004100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li P, Mao L, Zhou G, Leak RK, Sun BL, Chen J, et al. Adoptive regulatory t-cell therapy preserves systemic immune homeostasis after cerebral ischemia. Stroke. 2013;44:3509–3515. doi: 10.1161/STROKEAHA.113.002637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Na SY, Mracsko E, Liesz A, Hunig T, Veltkamp R. Amplification of regulatory t cells using a cd28 superagonist reduces brain damage after ischemic stroke in mice. Stroke. 2014;46:212–20. doi: 10.1161/STROKEAHA.114.007756. [DOI] [PubMed] [Google Scholar]
- 40.Schuhmann MK, Kraft P, Stoll G, Lorenz K, Meuth SG, Wiendl H, et al. Cd28 superagonist-mediated boost of regulatory t cells increases thrombo-inflammation and ischemic neurodegeneration during the acute phase of experimental stroke. J Cereb Blood Flow Metab. 2014;35:6–10. doi: 10.1038/jcbfm.2014.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shevach EM. Review mechanisms of foxp3 + t regulatory cell-mediated suppression. Immunity. 2009;30:636–645. doi: 10.1016/j.immuni.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 42.Spera PA, Ellison JA, Feuerstein GZ, Barone FC. Il-10 reduces rat brain injury following focal stroke. Neurosci Lett. 1998;251:189–192. doi: 10.1016/s0304-3940(98)00537-0. [DOI] [PubMed] [Google Scholar]
- 43.Grilli M, Barbieri I, Basudev H, Brusa R, Casati C, Lozza G, et al. Interleukin-10 modulates neuronal threshold of vulnerability to ischaemic damage. Eur J Neurosci. 2000;12:2265–2272. doi: 10.1046/j.1460-9568.2000.00090.x. [DOI] [PubMed] [Google Scholar]
- 44.Bodhankar S, Chen Y, Vandenbark AA, Murphy SJ, Offner H. Il-10-producing b-cells limit cns inflammation and infarct volume in experimental stroke. Metab Brain Dis. 2013;28:375–386. doi: 10.1007/s11011-013-9413-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liesz A, Bauer A, Hoheisel JD, Veltkamp R. Intracerebral interleukin-10 injection modulates post-ischemic neuroinflammation: An experimental microarray study. Neurosci Lett. 2014;579:18–23. doi: 10.1016/j.neulet.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 46.O’Garra A, Vieira PL, Vieira P, Goldfeld AE. Il-10-producing and naturally occurring cd4+ tregs: Limiting collateral damage. J Clin Invest. 2004;114:1372–1378. doi: 10.1172/JCI23215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frenkel D, Huang Z, Maron R, Koldzic DN, Hancock WW, Moskowitz MA, et al. Nasal vaccination with myelin oligodendrocyte glycoprotein reduces stroke size by inducing il-10-producing cd4+ t cells. J Immunol. 2003;171:6549–6555. doi: 10.4049/jimmunol.171.12.6549. [DOI] [PubMed] [Google Scholar]
- 48.Frenkel D, Huang Z, Maron R, Koldzic DN, Moskowitz MA, Weiner HL. Neuroprotection by il-10-producing mog cd4+ t cells following ischemic stroke. J Neurol Sci. 2005;233:125–132. doi: 10.1016/j.jns.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 49.Strle K, Zhou JH, Shen WH, Broussard SR, Johnson RW, Freund GG, et al. Interleukin-10 in the brain. Crit Rev Immunol. 2001;21:427–449. [PubMed] [Google Scholar]
- 50.Bodhankar S, Chen Y, Vandenbark AA, Murphy SJ, Offner H. Pd-l1 enhances cns inflammation and infarct volume following experimental stroke in mice in opposition to pd-1. Journal of neuroinflammation. 2013;10:111. doi: 10.1186/1742-2094-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ren X, Akiyoshi K, Dziennis S, Vandenbark AA, Herson PS, Hurn PD, et al. Regulatory b cells limit cns inflammation and neurologic deficits in murine experimental stroke. J Neurosci. 2011;31:8556–8563. doi: 10.1523/JNEUROSCI.1623-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yilmaz G, Arumugam TV, Stokes KY, Granger DN. Role of t lymphocytes and interferon-gamma in ischemic stroke. Circulation. 2006;113:2105–2112. doi: 10.1161/CIRCULATIONAHA.105.593046. [DOI] [PubMed] [Google Scholar]
- 53.Kleinschnitz C, Schwab N, Kraft P, Hagedorn I, Dreykluft A, Schwarz T, et al. Early detrimental t-cell effects in experimental cerebral ischemia are neither related to adaptive immunity nor thrombus formation. Blood. 2010;115:3835–3842. doi: 10.1182/blood-2009-10-249078. [DOI] [PubMed] [Google Scholar]
- 54.Offner H, Hurn PD. A novel hypothesis: Regulatory b lymphocytes shape outcome from experimental stroke. Transl Stroke Res. 2012;3:324–330. doi: 10.1007/s12975-012-0187-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bodhankar S, Chen Y, Vandenbark AA, Murphy SJ, Offner H. Treatment of experimental stroke with il-10-producing b-cells reduces infarct size and peripheral and cns inflammation in wild-type b-cell-sufficient mice. Metab Brain Dis. 2014;29:59–73. doi: 10.1007/s11011-013-9474-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen Y, Bodhankar S, Murphy SJ, Vandenbark AA, Alkayed NJ, Offner H. Intrastriatal b-cell administration limits infarct size after stroke in b-cell deficient mice. Metab Brain Dis. 2012;27:487–493. doi: 10.1007/s11011-012-9317-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bodhankar S, Chen Y, Lapato A, Vandenbark AA, Murphy SJ, Saugstad JA, et al. [Accessed February 26, 2015];Regulatory cd8+cd122+ t-cells predominate in cns after treatment of experimental stroke in male mice with il-10-secreting b-cells. Metab Brain Dis. 2014 doi: 10.1007/s11011-014-9639-8. published online ahead of print December 25, 2014. http://link.springer.com/article/10.1007/s11011-014-9639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Offner H, Subramanian S, Parker SM, Afentoulis ME, Vandenbark AA, Hurn PD. Experimental stroke induces massive, rapid activation of the peripheral immune system. J Cereb Blood Flow Metab. 2006;26:654–665. doi: 10.1038/sj.jcbfm.9600217. [DOI] [PubMed] [Google Scholar]
- 59.Meisel C, Schwab JM, Prass K, Meisel A, Dirnagl U. Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci. 2005;6:775–786. doi: 10.1038/nrn1765. [DOI] [PubMed] [Google Scholar]
- 60.Offner H, Subramanian S, Parker SM, Wang C, Afentoulis ME, Lewis A, et al. Splenic atrophy in experimental stroke is accompanied by increased regulatory t cells and circulating macrophages. J Immunol. 2006;176:6523–6531. doi: 10.4049/jimmunol.176.11.6523. [DOI] [PubMed] [Google Scholar]
- 61.Liesz A, Hagmann S, Zschoche C, Adamek J, Zhou W, Sun L, et al. The spectrum of systemic immune alterations after murine focal ischemia: Immunodepression versus immunomodulation. Stroke. 2009;40:2849–2858. doi: 10.1161/STROKEAHA.109.549618. [DOI] [PubMed] [Google Scholar]
- 62.Irmler IM, Gajda M, Kamradt T. Amelioration of experimental arthritis by stroke-induced immunosuppression is independent of treg cell function. Ann Rheum Dis. 2014;73:2183–2191. doi: 10.1136/annrheumdis-2013-204148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liesz A, Dalpke A, Mracsko E, Antoine DJ, Roth S, Zhou W, et al. Damp signaling is a key pathway inducing immune modulation after brain injury. The Journal of Neuroscience. 2015;35:583–98. doi: 10.1523/JNEUROSCI.2439-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang J, Yu L, Jiang C, Fu X, Liu X, Wang M, et al. Cerebral ischemia increases bone marrow cd4(+)cd25(+)foxp3(+) regulatory t cells in mice via signals from sympathetic nervous system. Brain Behav Immun. 2015;43:172–183. doi: 10.1016/j.bbi.2014.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Courties G, Herisson F, Sager H, Heidt T, Ye Y, Ying W, et al. Ischemic stroke activates hematopoietic bone marrow stem cells. Circ Res. 2015;116:407–17. doi: 10.1161/CIRCRESAHA.116.305207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hug A, Liesz A, Muerle B, Zhou W, Ehrenheim J, Lorenz A, et al. Reduced efficacy of circulating costimulatory cells after focal cerebral ischemia. Stroke. 2011;42:3580–6. doi: 10.1161/STROKEAHA.111.620948. [DOI] [PubMed] [Google Scholar]
- 67.Yan J, Read SJ, Henderson RD, Hull R, O’Sullivan JD, McCombe PA, et al. Frequency and function of regulatory t cells after ischaemic stroke in humans. J Neuroimmunol. 2012;243:89–94. doi: 10.1016/j.jneuroim.2011.12.019. [DOI] [PubMed] [Google Scholar]
- 68.Li Q, Wang Y, Yu F, Wang YM, Zhang C, Hu C, et al. Peripheral th17/treg imbalance in patients with atherosclerotic cerebral infarction. International journal of clinical and experimental pathology. 2013;6:1015–1027. [PMC free article] [PubMed] [Google Scholar]
- 69.Wigren M, Bjorkbacka H, Andersson L, Ljungcrantz I, Fredrikson GN, Persson M, et al. Low levels of circulating cd4+foxp3+ t cells are associated with an increased risk for development of myocardial infarction but not for stroke. Arteriosclerosis, thrombosis, and vascular biology. 2012;32:2000–2004. doi: 10.1161/ATVBAHA.112.251579. [DOI] [PubMed] [Google Scholar]
- 70.Hossmann KA. The two pathophysiologies of focal brain ischemia: Implications for translational stroke research. J Cereb Blood Flow Metab. 2012;32:1310–1316. doi: 10.1038/jcbfm.2011.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gauberti M, Martinez de Lizarrondo S, Orset C, Vivien D. Lack of secondary microthrombosis after thrombin-induced stroke in mice and non-human primates. Journal of thrombosis and haemostasis: JTH. 2014;12:409–414. doi: 10.1111/jth.12487. [DOI] [PubMed] [Google Scholar]
- 72.Chamorro A, Meisel A, Planas AM, Urra X, van de Beek D, Veltkamp R. The immunology of acute stroke. Nature reviews. Neurology. 2012;8:401–410. doi: 10.1038/nrneurol.2012.98. [DOI] [PubMed] [Google Scholar]
- 73.Liesz A, Ruger H, Purrucker J, Zorn M, Dalpke A, Mohlenbruch M, et al. Stress mediators and immune dysfunction in patients with acute cerebrovascular diseases. PLoS One. 2013;8:e74839. doi: 10.1371/journal.pone.0074839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chu HX, Kim HA, Lee S, Moore JP, Chan CT, Vinh A, et al. Immune cell infiltration in malignant middle cerebral artery infarction: Comparison with transient cerebral ischemia. J Cereb Blood Flow Metab. 2014;34:450–459. doi: 10.1038/jcbfm.2013.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Levings MK, Allan S, d’Hennezel E, Piccirillo CA. Functional dynamics of naturally occurring regulatory t cells in health and autoimmunity. Adv Immunol. 2006;92:119–155. doi: 10.1016/S0065-2776(06)92003-3. [DOI] [PubMed] [Google Scholar]
- 76.Danese S, Rutella S. The janus face of cd4+cd25+ regulatory t cells in cancer and autoimmunity. Current medicinal chemistry. 2007;14:649–666. doi: 10.2174/092986707780059599. [DOI] [PubMed] [Google Scholar]
- 77.Schwartz M, Raposo C. Protective autoimmunity: A unifying model for the immune network involved in cns repair. The Neuroscientist: a review journal bringing neurobiology, neurology and psychiatry. 2014;20:343–358. doi: 10.1177/1073858413516799. [DOI] [PubMed] [Google Scholar]
- 78.Walsh JT, Zheng J, Smirnov I, Lorenz U, Tung K, Kipnis J. Regulatory t cells in central nervous system injury: A double-edged sword. J Immunol. 2014;193:5013–5022. doi: 10.4049/jimmunol.1302401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kipnis J, Schwartz M. Controlled autoimmunity in cns maintenance and repair: Naturally occurring cd4+cd25+ regulatory t-cells at the crossroads of health and disease. Neuromolecular Med. 2005;7:197–206. doi: 10.1385/NMM:7:3:197. [DOI] [PubMed] [Google Scholar]
- 80.Kipnis J, Mizrahi T, Hauben E, Shaked I, Shevach E, Schwartz M. Neuroprotective autoimmunity: Naturally occurring cd4+cd25+ regulatory t cells suppress the ability to withstand injury to the central nervous system. Proc Natl Acad Sci U S A. 2002;99:15620–15625. doi: 10.1073/pnas.232565399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kimmelman J, Mogil JS, Dirnagl U. Distinguishing between exploratory and confirmatory preclinical research will improve translation. PLoS biology. 2014;12:e1001863. doi: 10.1371/journal.pbio.1001863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dirnagl U, Hakim A, Macleod M, Fisher M, Howells D, Alan SM, et al. A concerted appeal for international cooperation in preclinical stroke research. Stroke. 2013;44:1754–1760. doi: 10.1161/STROKEAHA.113.000734. [DOI] [PMC free article] [PubMed] [Google Scholar]