Abstract
Background and purpose
Hospital costs associated with atrial fibrillation (AFib) among stroke patients have not been well-studied, especially among people younger than 65 years. We estimated the AFib-associated hospital costs in U.S. patients aged 18-64 years.
Methods
We identified hospital admissions with a primary diagnosis of ischemic stroke from the 2010-2012 MarketScan Commercial Claims and Encounters inpatient datasets, excluding those with capitated health insurance plans, aged <18 or >64, missing geographic region, hospital costs below the 1st or above 99th percentile, and having carotid intervention (N=40,082). We searched the data for AFib and analyzed the costs for non-repeat and repeat stroke admissions separately. We estimated the AFib-associated costs using multivariate regression models controlling for age, sex, geographic region, and Charlson comorbidity index.
Results
Of the 33,500 non-repeat stroke admissions, 2,407 (7.2%) had AFib. Admissions with AFib cost $4,991 more than those without AFib ($23,770 vs. $18,779). For the 6,582 repeat stroke admissions, 397 (6.0%) had AFib. The costs were $3,260 more for those with AFib than those without ($24,119 vs. $20,929). After controlling for potential confounders, AFib-associated costs for non-repeat stroke admissions were $4,905, representing 20.6% of the total costs for the admissions. Both the hospital costs and the AFib-associated costs were associated with age, but not sex. AFib-associated costs for repeat stroke admissions were not significantly higher than for non-AFib patients, except for those aged 55-64 ($3,537).
Conclusions
AFib increased the hospital cost of ischemic stroke substantially. Further investigation on AFib-associated costs for repeat stroke admissions is needed.
Keywords: Hospital cost, ischemic stroke, atrial fibrillation, hospital admission
INTRODUCTION
The prevalence of stroke, the fourth leading cause of death in the United States and a leading cause of long-term severe disability,1-2 is expected to increase dramatically in the coming years, owing to the aging population and increasing stroke survival rate.3 Stroke is one of the most expensive chronic diseases to treat, and the costs are projected to increase rapidly.3-7 For example, the estimated direct medical cost alone was $18.8 billion in 2008.4 An even higher costs of $28.3 billion were projected for 2010 (in 2008 dollars), which would increase 238% between 2010 and 2030.6 Furthermore, the prevalence of stroke increases with age. Over two-thirds of stroke hospitalizations occur in those aged 65 and older, i.e., the nation’s Medicare recipients.8-10 Thus, stroke has been and will continue to be a significant public health problem in the United States. Because of the large aging population and the strong link between age and stroke, epidemiologic and economic research has focused on the population aged 65 and older. Yet, some studies have shown that the prevalence of stroke is increasing among younger adults.11-12 Investigation of the health and economic burden of stroke among those younger than 65 years is needed to guide public health interventions.
Atrial fibrillation (AFib) is a serious and common health condition, affecting between 2.5 million and 6 million Americans, and is associated with a 4- to 5-fold increased risk of ischemic stroke.13-14 It is an independent risk factor for ischemic stroke severity, recurrent stroke, and mortality associated with stroke.13-17 Prevention of ischemic stroke in patients with AFib is potentially effective in reducing the disability and economic burden associated with stroke. In fact, many investigators have explored the cost-effectiveness of stroke prevention among patients with AFib.18-24 The role of AFib in the economic burden of stroke is still unknown, although many researchers have investigated the economic burden of both stroke and AFib separately.5-9, 25-31 Identifying AFib-associated economic burden among ischemic stroke patients could guide decision makers in resource allocations for developing public health programs. This information can also be valuable to researchers in the field, especially to those investigating cost-effective strategies for stroke prevention among patients with AFib. In this study, we estimated the AFib-associated hospital costs among ischemic stroke patients aged 18-64 years.
METHODS
Study population
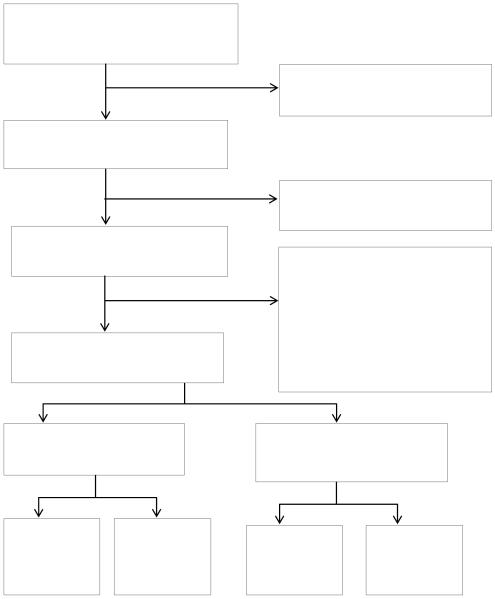
Using the 2010-2012 MarketScan Commercial Claims and Encounters inpatient data set, we identified all hospitalizations with a primary diagnosis of ischemic stroke (International Classification of Diseases, Ninth Revision [ICD-9] codes 433, 434, 436). In each year, the data contained inpatient information on more than 1 million hospital admissions for privately insured patients, mainly for patients 64 years or younger, with comprehensive and high-quality coding of medical conditions and of hospital costs based on payments received by providers.32 It has been used by many researchers in estimating the economic burden of various health conditions, including cardiovascular disease. 28, 33-36 Because of the relatively low prevalence of stroke and AFib in adults younger than 65 years, we pooled 3 years of MarketScan data to increase our sample size for this analysis. In selecting the study sample (N=40,082, Figure 1), we excluded: 1) patients younger than 18 because of extremely low prevalence of stroke and AFib, and patients older than 64 because the extremely small number of these patients in this data set; 2) admissions with a capitated health insurance plan because their costs did not reflect the medical services they received; 3) missing geographic region information because region is a major controlling variable in our study; 4) hospitalizations with a cost below the 1st or above 99th percentiles to reduce the influence of extreme values on the cost estimates; and 5) patients with an accompanying procedure code for carotid intervention (ICD-9 procedure codes 38,02, 38.12, 00.61, 00.63) because this study focused on the cost of acute stroke rather than an elective surgical procedure.
Figure 1.
Study population selection process, 2010-2012 MarketScan Commercial Claims and Encounters Database Inpatient Admissions
1An admission was a non-repeat stroke admission if it was the only admission for a patient during the study period of 2010-2012; otherwise, it was classified as a repeat stroke admission.
Among the stroke admissions, we searched the data for AFib including atrial flutter (ICD-9 427.31 and 427.32).29 Our main outcome measure was the total hospital costs (total payments received by providers), including the costs for physician services, all diagnostic tests, therapeutics, supplies, and room fees during the stay. We evaluated the impact of AFib on the costs by length of stay (LOS). The average LOS was 5.2 days for patients with AFib and 3.9 days for patients without AFib. Therefore, we used 5 days as the cut point for our analysis. We controlled for age, sex, urbanization, geographic region, and Charlson Comorbidity Index (CCI). The CCI measured the likelihood of death or serious disability in the subsequent year by diagnosis codes for up to 18 different diseases to control the effects of disease severity and comorbidities on the costs.37-38
Statistical analysis
We conducted univariate comparison of the hospital costs between the hospitalizations with and without AFib by Wilcoxon two-sample test. Then, we specified various multivariate regression models to derive the AFib-associated costs. Because the data were at the hospital admission level rather than patient level, a patient included in the study might have multiple admissions during the study period. To estimate AFib-associated costs for initial stroke and recurrent stroke separately, we identified patients with non-repeat stroke admissions for ischemic stroke and analyzed the costs separately from those of repeat stroke admissions. An admission was classified as a non-repeat stroke admission if it was the only admission for a patient during the study period of 2010-2012; otherwise, it was classified as a repeat stroke admission. However, we were unable to confirm initial or recurrent stroke status due to the limitations of the data. We estimated the regression models using ordinary least squares for non-repeat stroke admissions, and mixed-effects with repeated-measure approaches for repeat stroke admissions.39-40 All statistical analyses were performed using SAS version 9.3 (Cary, NC: SAS Institute, Inc., Cary, NC).
RESULTS
We identified 40,082 hospital admissions with a primary diagnosis of ischemic stroke from 2010-2012 in the MarketScan data files, of which 33,500 (2,407 [7.2%] with AFib, and 31,093 without AFib) were non-repeat stroke admissions and 6,582 (397 [6.0%] with AFib, and 6,185 without AFib) were repeat stroke admissions (Figure 1). Compared to patients without AFib, a higher percentage of patients with AFib were older, male, residing in the Northeast, and had a longer LOS (Table 1). For non-repeat stroke admissions, the mean costs were $19,138, and they were $4,991 (p<0.001) higher for patients with AFib than those without AFib (Table 2). This significant difference existed among all population groups by age, sex, urbanicity, geographic regions, and LOS. The largest differences were among patients aged 18-54 ($5,439) and those who resided in the West ($6,367). For repeat stroke admissions, the mean costs were $21,126. Although the costs were higher for admissions with AFib than those without, the differences were not statistically significant for repeat stroke admissions among most population groups.
Table 1.
Characteristics of patients with a primary diagnosis of ischemic stroke, 2010-2012 MarketScan Commercial Claims and Encounters Database Inpatient Admissions
| Total, %1 | Without AFib, % | With AFib, % | P-value | |
|---|---|---|---|---|
|
| ||||
|
Non-repeat Stroke
Admissions2 |
N=33,500 | N=31,093 | N=2,407 | |
| Age (years) | ||||
| 18-54 | 41.5 | 42.7 | 25.6 | <0.001 |
| 55-64 | 58.5 | 57.3 | 74.4 | <0.001 |
|
| ||||
| Average Age (years) | 54.3 | 54.0 | 57.4 | <0.001 |
|
| ||||
| Male | 58.3 | 57.7 | 66.1 | <0.001 |
|
| ||||
| Urban | 82.1 | 81.9 | 83.8 | 0.018 |
|
| ||||
| Region3 | ||||
| Northeast | 17.0 | 16.6 | 21.9 | <0.001 |
| North Central | 27.0 | 27.2 | 25.1 | 0.025 |
| South | 44.0 | 44.4 | 38.1 | <0.001 |
| West | 12.1 | 11.8 | 15.0 | <0.001 |
|
| ||||
| Charlson Comorbidity Index | 3.2 | 3.2 | 3.3 | 0.014 |
| (CCI) mean score | ||||
|
| ||||
| Length of Stay (LOS) | ||||
| <5 days | 72.4 | 72.6 | 57.1 | <0.001 |
| ≥5 days | 27.6 | 26.4 | 42.9 | <0.001 |
|
| ||||
| Average LOS (days) | 4.1 | 4.0 | 5.2 | <0.001 |
|
| ||||
| Repeat Stroke Admissions | N=6,582 | N=6,185 | N=397 | |
|
| ||||
| Age | ||||
| 18-54 | 43.0 | 44.3 | 26.4 | <0.001 |
| 55-64 | 57.0 | 55.7 | 73.6 | <0.001 |
|
| ||||
| Average Age (years) | 54.1 | 53.8 | 57.5 | <0.001 |
|
| ||||
| Male | 57.0 | 56.7 | 62.2 | 0.003 |
|
| ||||
| Urban | 82.2 | 82.2 | 81.9 | 0.847 |
|
| ||||
| Region | ||||
| Northeast | 22.3 | 22.1 | 26.4 | 0.042 |
| North Central | 27.0 | 27.0 | 28.0 | 0.667 |
| South | 41.9 | 42.2 | 37.8 | 0.083 |
| West | 8.7 | 8.7 | 7.8 | 0.520 |
|
| ||||
| CCI mean score | 3.4 | 3.4 | 3.6 | 0.070 |
|
| ||||
| LOS | ||||
| <5 days | 57.9 | 58.4 | 50.4 | 0.002 |
| ≥5 days | 42.1 | 41.6 | 49.6 | 0.002 |
|
| ||||
| Average LOS (days) | 6.5 | 6.5 | 6.8 | 0.451 |
All values are percentages unless otherwise indicated.
An admission was a non-repeat stroke admission if it was the only admission for a patient during the study period of 2010-2012; otherwise, it was classified as a repeat stroke admission.
Northeast region includes Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York, and Pennsylvania; North Central region includes Illinois, Indiana, Michigan, Ohio, Wisconsin, Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, and South Dakota; South region includes are Washington D.C., Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia, Alabama, Kentucky, Mississippi, Tennessee, Arkansas, Louisiana, Oklahoma, and Texas; West region includes Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming, Alaska, California, Hawaii, Oregon, and Washington.
Table 2.
Mean hospital costs (2012 $) of patients with a primary diagnosis of ischemic stroke, by atrial fibrillation (AFib) status, 2010-2012 MarketScan Commercial Claims and Encounters Database Inpatient Admissions
| Total | Without AFib | With AFib | Mean Difference Between with AFib and without AFib (p-value) |
|
|---|---|---|---|---|
|
| ||||
|
Non-repeat Stroke
Admissions1 |
N=33,500 | N=31,093 | N=2,407 | |
| Total | 19,138 | 18,779 | 23,770 | 4,991 (< 0.001) |
|
| ||||
| Age (years) | ||||
| 18-54 | 19,710 | 19,469 | 24,908 | 5,439 (<0.001) |
| 55-64 | 18,732 | 18,263 | 23,379 | 5,116 (<0.001) |
|
| ||||
| Sex | ||||
| Male | 19,194 | 18,786 | 23,802 | 5,016 (<0.001) |
| Female | 19,058 | 18,769 | 23,709 | 4,939 (<0.001) |
|
| ||||
| Metropolitan Statistical Area | ||||
| Yes | 19,489 | 19,128 | 24,047 | 4,920 (<0.001) |
| No | 17,531 | 17,199 | 22,332 | 5,133 (<0.001) |
|
| ||||
| Region2 | ||||
| Northeast | 19,757 | 19,341 | 23,841 | 4,500 (<0.001) |
| North Central | 18,773 | 18,473 | 22,969 | 4,496 (<0.001) |
| South | 17,962 | 17,685 | 22,133 | 4,448 (<0.001) |
| West | 23,365 | 22,796 | 29,163 | 6,367 (<0.001) |
|
| ||||
| Length of Stay (LOS) | ||||
| <5 days | 14,322 | 14,203 | 16,314 | 2,111 (<0.001) |
| ≥5 days | 31,798 | 31,558 | 33,704 | 2,147 (=0.014) |
|
| ||||
| Repeat Stroke | N=6,582 | N=6,185 | N=397 | |
| Admissions | ||||
|
| ||||
| Total | 21,126 | 20,929 | 24,199 | 3,269 (=0.002) |
|
| ||||
| Age (years) | ||||
| 18-54 | 21,634 | 21,487 | 25,471 | 3,985 (=0.053) |
| 55-64 | 20,741 | 20,487 | 23,741 | 3,254 (=0.007) |
|
| ||||
| Sex | ||||
| Male | 21,228 | 20,850 | 26,582 | 5,732 (<0.001) |
| Female | 20,992 | 21,033 | 20,273 | −759 (=0.643) |
|
| ||||
| Metropolitan Statistical Area | ||||
| Yes | 21,744 | 21,623 | 23,640 | 2,017 (=0.087) |
| No | 18,270 | 17,716 | 26,719 | 9,003 (<0.001) |
|
| ||||
| Region | ||||
| Northeast | 22,525 | 22,398 | 24,164 | 1,765 (=0.391) |
| North Central | 20,785 | 20,546 | 24,383 | 3,837 (=0.041) |
| South | 19,584 | 19,388 | 23,002 | 3,615 (=0.028) |
| West | 26,037 | 25,842 | 29,444 | 3,602 (=0.439) |
|
| ||||
| LOS | ||||
| <5 days | 13,912 | 13,899 | 14,157 | 259 (=0.727) |
| ≥5 days | 31,042 | 30,786 | 34,393 | 3,607 (=0.058) |
An admission was a non-repeat stroke admission if it was the only admission for a patient during the study period of 2010-2012; otherwise, it was classified as a repeat stroke admission.
Northeast region includes Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York, and Pennsylvania; North Central region includes Illinois, Indiana, Michigan, Ohio, Wisconsin, Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, and South Dakota; South region includes are Washington D.C., Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia, Alabama, Kentucky, Mississippi, Tennessee, Arkansas, Louisiana, Oklahoma, and Texas; West region includes Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming, Alaska, California, Hawaii, Oregon, and Washington.
After controlling for potential confounders, AFib increased the hospital costs by $4,905 (p<0.001) for non-repeat stroke admissions, which is about 20.6% of the total hospital costs for patients with AFib (Table 3). AFib increased the costs of non-repeat stroke admissions by $5,084 (p<0.001) for patients aged 18-54 years and $4,854 (p<0.001) for patients aged 55-64 years. The increased costs associated with AFib were similar by sex ($4,902 for men and $4,898 for women; both p<0.001). Admissions with LOS <5 days had $1,909 (p<0.001) higher costs for those with AFib compared to those without AFib. The cost increase associated with AFib was not statistically significant for admissions with a LOS ≥5 days. For repeat stroke admissions, AFib had a statistically significant effect on the hospital costs for patients aged 55-64 years only (mean cost increased by $3,537, p=0.005) (Table 3).
Table 3.
Atrial fibrillation associated hospital costs (2012 $) for patients with a primary diagnosis of ischemic stroke, 2010-2012 MarketScan Commercial Claims and Encounters Database Inpatient Admissions1
| Population Group | Non-repeat Stroke Admissions2
(p-value) |
Repeat Stroke Admissions (p-value) |
|---|---|---|
| Total | 4,905 (<0.001) |
3,315 (0.341) |
|
| ||
| Age: | ||
| 18-54 | 5,084 (<0.001) |
4,118 (0.537) |
| 55-64 | 4854 (<0.001) |
3,537 (0.005) |
|
| ||
| Sex: | ||
| Male | 4,902 (<0.001) |
5,785 (0.497) |
| Female | 4,898 (<0.001) |
−422 (0.894) |
|
| ||
| Length of Stay (LOS): | ||
| <5 days | 1,909 (<0.001) |
207 (0.785) |
| >=5 days | 2,238 (0.010) |
3,525 (0.489) |
Note:
Controlling variables are age, sex, metropolitan statistical area, region, Charlson Comorbidity Index score, and years.
An admission was a non-repeat stroke admission if it was the only admission for a patient during the study period of 2010-2012; otherwise, it was classified as a repeat stroke admission.
DISCUSSION
Our study may be the first comprehensive examination of the impact of AFib on hospital costs of ischemic stroke patients in a younger stroke population. After controlling for potential confounders, we found that AFib increased hospital costs for non-repeat ischemic stroke admissions by $4,905, accounting for 20.6% of the total hospital costs of admissions with AFib. Although not directly comparable, this cost difference for stroke admissions with AFib was lower than that derived by Kim et al. ($5,218),29 based on 2004-2006 MarketScan data. Using propensity score-matched subjects, Kim and colleagues compared inpatient costs between AFib and non-AFib patients aged 20 and older for all patients (i.e., without focusing on stroke patients). Their propensity score-matching technique improved their cost estimate, but deriving incremental costs by univariate comparison without further controlling for potential confounders might have led to an overestimate of the AFib-associated costs. Using all patients (i.e., not limited to stroke or ischemic stroke patients) as their study subjects might also have overestimated the AFib-associated cost.
By focusing on ischemic stroke patients, we further found that both the costs of hospitalizations and the costs associated with AFib were higher in the younger age (18-54 years) group compared to those aged 55-64 years. These findings are new and may have important public health implications. For example, while research and public health efforts have focused on stroke management and prevention among those aged 65 years or older,8, 9, 27, 31 stroke interventions such as AFib management among younger adults, as well as older adults, may have a greater economic impact. The higher costs associated with AFib suggests that stroke with AFib may be more severe than stroke without this disorder,13, 15-17 or it may reflect the added costs of diagnosis and treatment of previously undiagnosed AFib. Our findings may also suggest that younger patients aged 18-54 with AFib-associated stroke were treated more aggressively than older patients aged 55-64 years old. 41, 42
Regardless of AFib status, overall hospital costs were similar for male and female patients. Moreover, the AFib-increased costs were also similar by sex ($4,902 for male and $4,898 for female patients). This suggests that economically, AFib equally affected men and women. The hospital costs were higher for patients from urban areas compared to rural areas. It was clearly higher for patients from the West than from the other three regions of the United States. These geographic variations deserve further investigation. Another interesting finding was that for repeat admissions, the impact of AFib on the hospital costs was not statistically significant, except for patients aged 55-64. This may be due to the large cost variations among these admissions, as shown by the insignificant cost differences between AFib and non-AFib admission in Table 2. These issues deserve further exploration.
Our findings had several limitations. First, we selected the hospital admissions with a primary diagnosis of ischemic stroke for the cost analysis. This helped us to derive accurate estimates of the costs of ischemic stroke associated with AFib, but we might have missed stroke cases where acute stroke was listed as a secondary diagnosis. Indeed, there is a need to explore AFib-associated costs for those with a secondary diagnosis of stroke because a large proportion of stroke patients have stroke listed as a secondary diagnosis.28 Similarly, we did not include admissions with a primary diagnosis of AFib. This certainly led to a lower estimated cost associated with AFib.
Second, as with all studies that rely on medical records, the issue of coding error must also be considered. Although misdiagnosis issues have been investigated in the literature, how this issue would affect the costs in our study is unknown.43-45 Furthermore, AFib is often asymptomatic or clinically undetected; thus, AFib-associated stroke may be substantially underestimated.14 In addition, we may have missed AFib cases that were not identified during the hospital stays. A recent study found that 30-day ECG monitoring identified AFib in 5 times as many cryptogenic stroke patients compared to the standard 24-hour ECG monitoring post-stroke. A high proportion of cryptogenic stroke is later found to be associated with AFib.46
Third, although we distinguished repeat stroke admissions during the 3-year study period from non-repeat stroke admissions, we could not confirm initial stroke admission from recurrent stroke admission status. It is possible that some of the non-repeat stroke admissions were for a recurrent stroke. Because there was no way to confirm whether an admission was truly an initial or recurrent stroke admission, we were unable to further refine our analysis. Additionally, using CCI might not be sufficient to control for the impact of health conditions and stroke severely. Clinical information such as procedures and details cost categories are needed to shed more light on the AFib associated costs.
Finally, our study sample only contained patients aged 18-64 years with non-capitated private insurance plans, and thus the costs might be influenced by insurance reimbursement rate. The estimated hospital costs might be slightly higher than that of U.S. general population because it was an insured population.47 We expected that this did not severely bias the estimation of AFib associated costs. While the prevalence of Afib in the younger population was much lower than in the 65 years and older population, we were not looking at total national burden of AFib and stroke. In addition to missing the stroke cases for patients without health insurance, with a capitated health insurance plan and government insurance coverage, we were unable to investigate the hospital costs among people older than 65 years. Because both stroke and AFib are strongly associated with age, investigating the relationship between stroke and AFib in the elderly population would be useful for policy makers in planning for a rapidly aging population. Despite these limitations, our cost estimates are valuable inputs for cost-effectiveness models such as comparing medical cost savings from high-quality anticoagulation services and patient home-testing of anticoagulation levels by AFib status or age groups.
CONCLUSIONS
We found that among non-repeat admissions for ischemic stroke, the hospital costs were substantial and varied by age and geographic area, and that AFib was an important contributor to the costs. Overall, AFib increased the hospital costs of ischemic stroke patients substantially across all age and sex groups. Particularly, both mean hospital costs and AFib-associated costs were higher for younger patients (aged 18-54 years) than older patients (aged 55-64 years) among non-repeat stroke admissions. Among repeat stroke admissions, AFib-associated costs were not statistically higher except for patients aged 55-64 years. These findings can help to identify future research areas such as the need for separately examining the health and economic burden of initial and recurrent strokes, or evaluating cost-effectiveness of interventions for AFib and stroke prevention and control.
Acknowledgments
Sources of funding: None
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention (CDC).
There is no potential conflict of interest related to any part of this article.
References
- 1.Heron M. Deaths: leading cause for 2009. 2012;61(7) National Vital Statistics Reports. Available at http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_07.pdf, Accessed April 13, 2013. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Prevalence and most common causes of disability among adults, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–426. [PubMed] [Google Scholar]
- 3.Demaerschalk BM, Hwang HM, Leung G. US cost burden of ischemic stroke: a systematic literature review. Am J Manag Care. 2010;16:525–533. [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality Total expenses and percent distribution for selected conditions by source of payment: United States, 2008. Medical Expenditure Panel Survey Household Component Data. http://meps.ahrq.gov/data_stats/tables_compendia_hh_interactive.jsp?_SERVICE=MEPSSocket0&_PROGRAM=MEPSPGM.TC.SAS&File=HCFY2008&Table=HCFY2008%5FCNDXP%5FC&_Debug=. Accessed March 16, 2015.
- 5.Brown DL, Boden-Albala B, Langa KM, Lisabeth LD, Fair M, Smith MA, et al. Projected costs of ischemic stroke in the United States. Neurology. 2006;67:1390–1395. doi: 10.1212/01.wnl.0000237024.16438.20. [DOI] [PubMed] [Google Scholar]
- 6.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowits MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 7.Wier LM, Andrews RM. The National Hospital Bill: The most expensive conditions by payer, 2008. Agency for Healthcare Research and Quality; Rockville, MD: Mar, 2011. HCUP Stat Brief #107. [PubMed] [Google Scholar]
- 8.Buntin BM, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after post acute care for stroke and hip fracture. Med Care. 2010;48:776–784. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee WC, Christensen MC, Joshi AV, Pashos CL. Long-term cost of stroke subtypes among Medicare beneficiaries. Cerebrovasc Dis. 2007;23:57–65. doi: 10.1159/000096542. [DOI] [PubMed] [Google Scholar]
- 10.Hall MJ, Levant S, DeFrances CJ. Hospitalization for stroke in U.S. hospitals, 1989-2009. National Center for Health Statistics; Hyattsville, MD: 2012. NCHS data brief, no 95. [Google Scholar]
- 11.George MG, Tong X, Kuklina EV, Labarthe DR. Trends in stroke hospitalizations and associated risk factors among children and young adults, 1995-2008. Ann Neurol. 2011;70:713–21. doi: 10.1002/ana.22539. [DOI] [PubMed] [Google Scholar]
- 12.Arntz RM, van Alebeek ME, Synhaeve NE, Brouwers PJ, van Dijk GW, Gons RA, et al. Observational Dutch young symptomatic stroke study (ODYSSEY): Study rational and protocol of a multicenter prospective cohort study. BMC Neurol. 2014;14:55. doi: 10.1186/1471-2377-14-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines. Circulation. 2006;114:e257–e354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 14.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hohnloser SH, Duray GZ, Baber U, Halperin JL. Prevention of stroke in patients with atrial fibrillation: current strategies and future directions. Europ Heart J Suppl. 2008;10(Supplement H):H4–H10. [Google Scholar]
- 16.Marini C, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke. 2005;36:1115–1119. doi: 10.1161/01.STR.0000166053.83476.4a. [DOI] [PubMed] [Google Scholar]
- 17.Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, et al. Stroke severity in atrial fibrillation: the Framingham study. Stroke. 1996;27:1760–1764. doi: 10.1161/01.str.27.10.1760. [DOI] [PubMed] [Google Scholar]
- 18.Singh SM, Micieli A, Wijeysundera HC. Economic evaluation of percutaneous left atrial appendage occlusion, dibigatran, and warfarin for stroke prevention in patients with nonvalvular atrial fibrillation. Circulation. 2013:2411–2423. doi: 10.1161/CIRCULATIONAHA.112.000920. [DOI] [PubMed] [Google Scholar]
- 19.Kamel H, Johnston C, Easton JD, Kim AS. Cost-effectiveness of dabigatran compared with warfarin for stroke prevention in patients with atrial fibrillation and prior stroke or transient ischemic attack. Stroke. 2012;43:881–883. doi: 10.1161/STROKEAHA.111.641027. [DOI] [PubMed] [Google Scholar]
- 20.Shah SV, Gage BF. Cost-effectiveness of dabigatran for stroke prophylaxis in atrial fibrillation. Circulation. 2011;123:2562–2570. doi: 10.1161/CIRCULATIONAHA.110.985655. [DOI] [PubMed] [Google Scholar]
- 21.Freeman JV, Zhu RP, Owens DK, Garber AM, Hutton DW, Go AS, et al. Cost-effectiveness of dabigatran compared with warfarin for stroke prevention in atrial fibrillation. Ann Intern Med. 2011;154:1–11. doi: 10.7326/0003-4819-154-1-201101040-00289. [DOI] [PubMed] [Google Scholar]
- 22.Sorensen SV, Kansal AR, Connolly S, Peng S, Linnehan J, Bradley-Kennedy C, et al. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and system embolism in atrial fibrillation: A Canadian payer perspective. Thromb Haemost. 2011;105:908–919. doi: 10.1160/TH11-02-0089. [DOI] [PubMed] [Google Scholar]
- 23.Sorensen SV, Dewilde S, Singer DE, Goldhaber SZ, Monz BU, Plumb JM. Cost-effectiveness of warfarin: trial versus “real world” stroke prevention in atrial fibrillation. Am Heart J. 2009;157:1064–1073. doi: 10.1016/j.ahj.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 24.Gustafsson C, Asplund K, Britton M, Norrving B, Olsson B, Marke LA. Cost-effectiveness of primary stroke prevention in atrial fibrillation: Swedish national perspective. Br Med J. 1992;305:1457–1460. doi: 10.1136/bmj.305.6867.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qureshi AI, Suri FK, Nasar A, Kirmani JF, Ezzeddin MA, Divani AA, et al. Changes in cost and outcome among US patients with stroke hospitalized in 1990 to 1991 and those hospitalized in 2000 to 2001. Stroke. 2007;38:2180–2184. doi: 10.1161/STROKEAHA.106.467506. [DOI] [PubMed] [Google Scholar]
- 26.Di Carlo A. Human and economic burden of stroke. Age and Ageing. 2009;38:4–5. doi: 10.1093/ageing/afn282. [DOI] [PubMed] [Google Scholar]
- 27.Brinjiki W, Rabinstein AA, Cloft HJ. Hospitalization costs for acute ischemic stroke patients treated with intravenous thrombolysis in the United States are substantially higher than Medicare payments. Stroke. 2012;43:1311–1133. doi: 10.1161/STROKEAHA.111.636142. [DOI] [PubMed] [Google Scholar]
- 28.Wang G, Zhang Z, Ayala C, Dunet DO, Fang J, George MG. Costs of hospitalization for stroke patients aged 18-64 years in the United States. J Stroke Cerebrovasc Dis. 2014;23:861–865. doi: 10.1016/j.jstrokecerebrovasdis.2013.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4:313–320. doi: 10.1161/CIRCOUTCOMES.110.958165. [DOI] [PubMed] [Google Scholar]
- 30.Ringborg A, Niewlaat R, Lindgren P, Jonsson B, Fidan D, Moggioni AP, et al. Costs of atrial fibrillation in five European countries: results from the Euro Heart Survey on atrial fibrillation. Europace. 2008;10:403–411. doi: 10.1093/europace/eun048. [DOI] [PubMed] [Google Scholar]
- 31.Lee W, Lamas G, Balu S, Spalding J, Wang Q, Pashos CL. Direct treatment cost of atrial fibrillation in the elderly American population: a Medicare perspective. J Med Economics. 2008;11:281–298. doi: 10.3111/13696990802063425. [DOI] [PubMed] [Google Scholar]
- 32.Danielson E. Health research data for the real world: The MarketScan databases. (January 2014 white paper) http://truvenhealth.com/Portals/0/Users/031/31/31/PH_13434%200314_MarketScan_WP_web.pdf. Accessed 7/24/2014.
- 33.Menzin J, Wygant G, Hauch O, Jackel J, Friedman M. One year costs of ischemic heart disease among patients with acute coronary syndromes: findings from a multiemployer claims database. Curr Med Res Opin. 2008;24:461–468. doi: 10.1185/030079908x261096. [DOI] [PubMed] [Google Scholar]
- 34.Kahende JW, Woollery TA, Lee CW. Assessing medical expenditures on smoking-related diseases, 1996-2001. Am J Health Behav. 2007;31:602–611. doi: 10.5555/ajhb.2007.31.6.602. [DOI] [PubMed] [Google Scholar]
- 35.Wang J, Zhang Z, Ayala C. Hospitalization costs associated with hypertension as a secondary diagnosis among insured patients aged 18-64 years. Am J Hypertens. 2010;23:275–281. doi: 10.1038/ajh.2009.241. [DOI] [PubMed] [Google Scholar]
- 36.Wang G, Zhang Z, Ayala C, Wall HK, Fang J. Costs of heart failure-related hospitalizations in patients aged 18-64 years. Am J Manag Care. 2010;16:769–776. [PubMed] [Google Scholar]
- 37.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbiditiy in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 38.Zhang JX, Rathouz PJ, Chin MH. Comorbidity and the concentration of healthcare expenditures in older patients with heart failure. J Am Geriatr Soc. 2003;52:476–482. doi: 10.1046/j.1532-5415.2003.51155.x. [DOI] [PubMed] [Google Scholar]
- 39.Nichols GA, Bell TJ, Pedula KL, O’Keeffe-Rosetti CR. Medical care costs among patients with established cardiovascular disease. Am J Manag Care. 2010;16:e86–e93. [PubMed] [Google Scholar]
- 40.Mandell DS, Quevara JP, Rpstain AL, Hadley TR. Economic grand rounds: medical expenditures among children with psychiatric disorders in a Medicaid population. Psychiatr Serv. 2003;54:465–467. doi: 10.1176/appi.ps.54.4.465. [DOI] [PubMed] [Google Scholar]
- 41.Asdaghi N, Butcher KS, Hill MD. Risk and benefits of thrombolysis in the elderly. Int J Stroke. 2012;7:142–149. doi: 10.1111/j.1747-4949.2011.00744.x. [DOI] [PubMed] [Google Scholar]
- 42.Saposnik G, Guzik AK, Reeves M, Ovbiagele B, Johnston SC. Stroke prognostication using age and NIH stroke scale: SPAN-100. Neurology. 2013;80:21–28. doi: 10.1212/WNL.0b013e31827b1ace. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Benesch C, Witter DM, Jr, Wilder AL, Duncan PW, Samsa GA, Matchar DB. Inaccuracy of the International Classification of Disease (ICD-9-CM) in identifying the diagnosis of ischemic cerebrovascular disease. Neurology. 1997;49:660–664. doi: 10.1212/wnl.49.3.660. [DOI] [PubMed] [Google Scholar]
- 44.Rinaldi R, Vignatelli L, Galeotti M, Azzimodi G, de Carolis P. Accuracy if ICD-9 in identifying ischemic stroke in general hospital of Lugo di Romagna (Italy) Neurol Sci. 2003;24:65–69. doi: 10.1007/s100720300074. [DOI] [PubMed] [Google Scholar]
- 45.Thigpen J, Dillon CS, Forster K, Henault L, Quinn EK, Tripodis G, et al. Using international classification of diseases ninth revision codes overestimates the frequency of true stroke. JACC. 2013;61:E299. [Google Scholar]
- 46.Gladston DJ, Spring M, Dorian P, Panzov V, Thorpe KE, Hall J, et al. Atrial fibrillation in patients with crytogenic stroke. N Engl J Med. 2041;370:2467–2477. doi: 10.1056/NEJMoa1311376. [DOI] [PubMed] [Google Scholar]
- 47.Aizcorbe A, Liebman E, Pack S, Cutler DM, Chernew ME, Rosen AB. Measuring health care costs of individuals with employer-sponsored health insurance in the U.S.:A comparison of survey and claims data. Statistical Journal of the IAOS. 2012;28:43–51. doi: 10.3233/SJI-2012-0743. [DOI] [PMC free article] [PubMed] [Google Scholar]