Abstract
The number of falls and/or accidental injuries associated with cellular phone use during walking is growing rapidly. Understanding the effects of concurrent cell phone use on human gait may help develop safety guidelines for pedestrians. It was shown previously that older adults had more pronounced dual-task interferences than younger adults when concurrent cognitive task required visual information processing. Thus, cell phone use might have greater impact on walking stability in older than in younger adults. This study examined gait stability and variability during a cell phone dialing task (phone) and two classic cognitive tasks, the Paced Auditory Serial Addition Test (PASAT) and Symbol Digit Modalities Test (SDMT). Nine older and seven younger healthy adults walked on a treadmill at four different conditions: walking only, PASAT, phone, and SDMT. We computed short-term local divergence exponent (LDE) of the trunk motion (local stability), dynamic margins of stability (MOS), step spatiotemporal measures, and kinematic variability. Older and younger adults had similar values of short-term LDE during all conditions, indicating that local stability was not affected by the dual-task. Compared to walking only, older and younger adults walked with significantly greater average mediolateral MOS during phone and SDMT conditions but significantly less ankle angle variability during all dual-tasks and less knee angle variability during PASAT. The current findings demonstrate that healthy adults may try to control foot placement and joint kinematics during cell phone use or another cognitive task with a visual component to ensure sufficient dynamic margins of stability and maintain local stability.
Keywords: dual-task, gait, cell phone, dynamic stability, margins of stability
Introduction
The number of falls and/or accidental injuries associated with cellular phone use during walking has been increasing [1]. Using a cell phone while driving was evidenced to increase the risk of motor vehicle collisions [2]. Currently, most states ban text messaging and a number of states prohibit drivers from using hand-held cell phones [2]. Although walking is thought to be a more automatic motor task compared to driving, cell phone use may cause cognitive distraction, reduced visual attention to the environment, and altered physical demands such as reduced arm swinging and altered head orientation [3]. Distraction from cell phone use was shown to affect pedestrian behavior, for example, reducing situation awareness and increasing unsafe pedestrian behavior while crossing the street [4]. However, few studies have examined the impact of cell phone use on gait [3, 5]. Previous studies showed reduced walking speed, increased lateral deviation from a straight line and greater variation in lateral foot placement when using a cell phone [3, 5]. Those results suggest that walking stability might be compromised during cell phone use, which would lead to an increased risk of falls. Thus, a better understanding of the effects of cell phone use on walking stability may help develop safety guidelines for pedestrians.
The effects of cell phone use on gait stability can be estimated by employing a dual-task walking paradigm. During dual-task walking, subjects are usually required to perform an attention demanding task while walking [6]. Growing evidence demonstrates that walking is not a fully automated motor activity but requires executive function, attention, and the ability to adapt to environmental complexity [7]. When performing two tasks simultaneously, each of which requires a certain level of attention, the total attention required may exceed the total information processing capacity of an individual and thus, lead to a negative influence on the performance of either task [6]. Previous studies showed that both healthy younger and older adults reduced their walking speed and increased gait variability while performing a cognitive task [8, 9]. In addition, the changes in performance during dual-task walking were strongly associated with an increased risk of falls in older adults and neurologically impaired individuals [10]. It was also shown that older adults had more pronounced dual-task interferences than younger adults when the cognitive task required visual information processing [11, 12]. Thus, cell phone use may have greater impact on walking stability in older adults than in younger adults. However, increased gait variability was often used as an index of reduced stability and walking speed, a confounding factor for gait variability [13], was not controlled in those studies. It is not clear if the increased gait variability during dual-tasking resulted from the reduced walking speed or reflected reduced stability.
Altered physical demands associated with the cell phone manipulation such as reduced arm swinging and altered head orientation may also play an important role in modifying walking performance in addition to cognitive distractions. Arm swinging was suggested to help stabilize the body and enhance lateral balance during walking [14]. It has been shown that the vertical ground reaction moment and the rate of metabolic energy consumption during walking increased when arm swinging was eliminated [14, 15]. Thus, reducing arm swinging due to cell phone manipulation might reduce walking stability or result in energetically costly stabilization strategies such as increasing trunk muscle activation or adjusting step width [14]. Moreover, during the cell phone use, the gaze is somewhat fixed to the phone and the head position is tilted downward in relation to the direction of walking, which may increase variations of sensory signals from the vestibular and/or visual system for controlling balance during walking [16].
The purpose of this study was to investigate how people maintain walking stability during a cell phone dialing task. Specifically, we would like to explore the effects of dual-tasking on subjects’ local dynamic stability [13] and dynamic margins of stability [17]. To control walking speed during dual-tasking, we examined treadmill walking. We compared the cell phone dialing task with two classic cognitive tasks, the Paced Auditory Serial Addition Test [18] and Symbol Digit Modalities Test [19], which challenge auditory working memory and visual information processing speed, respectively. During the PASAT, subjects were auditorily presented a single digit number every two seconds and were instructed to add each new digit to the one immediately prior to it. During the SDMT, subjects were instructed to hold a letter size of testing paper with both hands while reading the symbols, thus eliminating arm swinging and resulting in an altered head orientation similar to the cell phone dialing task. We also compared older and younger adults to examine the age-related changes in dual-task walking. We hypothesized that both healthy younger and older adults would show reduced walking stability during the cell phone dialing task and the two cognitive tasks compared to walking only. We expected to see greater dual-tasking effects on walking stability in older adults than in younger adults. We also expected to see that the cell phone dialing task and SDMT would have greater effects on gait compared to the PASAT because these two tasks would lead to altered physical demands in addition to cognitive distraction.
Methods
Subjects
Seven healthy younger (five female, age: 20.4±2.2 years) and nine older subjects (seven female, age: 61.1±10.0 years) gave written informed consent to participate in this study. Both universities’ Institutional Review Boards approved the protocol.
Experimental protocol
All subjects walked on a treadmill at their self-selected speed (younger subjects: 1.11±0.15 m/s, older subjects: 1.07±0.27 m/s) and under four different conditions: walking only, while performing the Paced Auditory Serial Addition Test (PASAT), a cellular phone dialing task (phone) and Symbol Digit Modalities Test (SDMT). During the PASAT, subjects were presented a single digit number by way of audio recording every two seconds and asked to add the most recent number to the number just presented, thereby disregarding their own verbal response and inhibiting the tendency to maintain a running total [18]. During the phone dialing task (phone), subjects were visually presented a series of ten-digit phone numbers one at a time and asked to dial the numbers on a standard flip phone (Motorola Razor) with both hands. During the SDMT [19], subjects were provided with a reference key where nine different symbols correspond to the numbers 1 through 9, followed by a list of 110 symbols on a letter size page held by the subject. Subjects were asked to rapidly state the number associated with each symbol in the order presented [19]. These tasks were chosen to include a more ecological task as well as traditional tasks known to assess different but partially overlapping elements of cognition. Each walking trial was tested for two minutes and in a pseudo-randomized order.
Data acquisition and analysis
Kinematics and ground reaction forces were recorded while subjects walked on an instrumented treadmill (1200 Hz, Bertec Corp., Columbus, OH, USA). The 3-D kinematic data were recorded using an 8-camera video system (60Hz, Motion Analysis Corporation, Santa Rosa, CA, USA) with reflective markers attached on the feet, legs, pelvis, trunk, and over the C7 vertebra. Commercial software (Visual3D, C-Motion Inc., Germantown, MD, USA) was used for the initial data processing.
We quantified local stability by computing short-term local divergence exponents (LDE) of the trunk motion based on the reconstructed state spaces of C7 vertebral marker movement [13, 20]. This local stability measure quantifies the sensitivity of the human locomotor system to the naturally occurring small perturbation during walking [21]. Techniques to quantify local stability are well established [22, 23]. Briefly, we extracted and analyzed the first 90 continuous strides of each trial because it was the minimum number of continuous strides across trials. We then re-sampled the data to 9,000 total data samples, approximately 100 data samples per stride [22]. Delay embedded state spaces were reconstructed independently from the mediolateral, anteroposterior, and vertical velocities of non-filtered C7 vertebral marker data using the original data and their time delayed copies [20]:
| (1) |
where S(t) is the 5-dimensional state vector, v(t) is the original 1-dimensional C7 vertebral marker velocity data, and τ is the time delay. We used fixed time delays of 30, 25, and 15 data samples for the mediolateral (ML), anteroposterior (AP), and vertical (VT) directions, respectively, for all trials [23]. LDE quantified how quickly neighboring movement trajectories in a state space diverge over time. We first identified nearest neighbors and calculated the logarithmic Euclidean distances between neighboring trajectories in the state space as a function of time. The logarithmic divergences were then averaged over all pairs of initial nearest neighbors. Short-term LDE was estimated from the slope of a linear least-squares fit to the average logarithmic divergence curve between 0 and the 1st stride [21]. A positive and larger value of LDE indicates the locomotor system is more unstable, diverging from the neighboring trajectories at a faster rate [23].
We quantified dynamic margins of stability (MOS) by computing the distances between the extrapolated center of mass (XCOM) positions and the boundaries of the base of support [17]. The XCOM position was calculated as:
| (2) |
where COM and are the position and velocity of the COM, respectively, and , where g is 9.81m/s2 and is taken as the height of the COM position during quiet standing. We computed mediolateral MOS (MOSML) as the lateral distance between the XCOM and the 5th metatarsal marker of the leading foot at heel strike. Anteroposterior MOS (MOSAP) was computed as the anteroposterior distance between the XCOM and the front toe marker of the leading foot at heel strike.
We also examined gait variability to determine if the increased gait variability during the dual-task overground walking shown previously [8] resulted from reduced walking speed or reflected reduced stability. We computed the standard deviation of step width, length and time. We also calculated mean standard deviation (meanSD) of the lower-limb joint motions and C7 marker positions for each trial. The meanSD of the C7 marker positions quantifies the overall variability of subjects’ displacements (i.e., drift) on the treadmill [13].
Statistics
We performed Mann-Whitney U tests and Friedman’s tests to test for the between-subject (i.e., two groups) and within-subject differences (i.e., four conditions), respectively, in the dependent variables (i.e., local stability of the trunk motion, margins of stability, step measures, and variability of gait kinematics). For the small sample size, we chose the nonparametric methods because the validity of this approach does not crucially depend on the normality assumption. We set the significance level at p<0.05. If a condition effect was detected, we used Wilcoxon signed rank tests to discriminate differences between walking only and each of the dual-task conditions (i.e., walking only vs. PASAT, walking only vs. phone, and walking only vs. SDMT) with Bonferroni’s correction (adjusted α=0.017). We performed all statistical analyses using SPSS version 22 (IBM Corp., Armonk, NY, USA).
Results
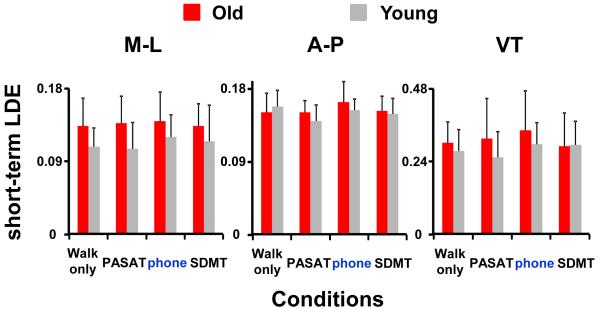
Both older and younger subjects had similar values of short-term local divergence exponents (LDE) during dual-task conditions compared to walking only, indicating that local stability was not affected by the dual-task conditions (Fig. 1). For the mediolateral C7 movements, there was no significant group (Mann-Whitney U test, p=0.079) or condition effect (Friedman’s test, p=0.878). Older subjects showed a trend to have slightly greater values of short-term LDE, indicating more locally unstable, for mediolateral C7 movements compared to younger subjects. For the anteroposterior or vertical C7 movements, there were also no group (AP: p=0.478, VT: p=0.415) or condition effects (AP: p=0.160, VT: p=0.233).
Figure 1.
Short-term LDE, indicating local stability of the C7 vertebral marker movement, in the mediolateral (M-L), anteroposterior (A-P), and vertical (VT) directions for older (red bars) and younger (grey bars) subjects. Error bars represent 1 STD. Note that a larger value of short-term LDE indicates more instability of the trunk motion represented by the C7 vertebral marker velocity profile.
Both older and younger subjects walked with significantly greater average MOSML during the phone and SDMT conditions compared to walking only (Wilcoxon signed rank tests, both p=0.001) (Fig. 2). There was no group effect for average MOSML (Mann-Whitney U test, p=0.080). Older subjects showed a trend to walk with slightly greater average MOSML compared to younger subjects. For the average MOSAP, older subjects had significantly smaller average MOSAP compared to the younger subjects (Mann-Whitney U test, p<0.001). There were no group or condition effects for the MOSML variability or MOSAP variability.
Figure 2.
(A) Mean and (B) variability of MOSAP, and (C) mean and (D) variability of MOSML for older (red bars) and younger (grey bars) subjects. Error bars represent 1 STD. ## indicates significant difference between younger and older subjects (Mann-Whitney U test, p<0.05). * indicates significant difference between conditions (Wilcoxon signed rank tests, p<0.017).
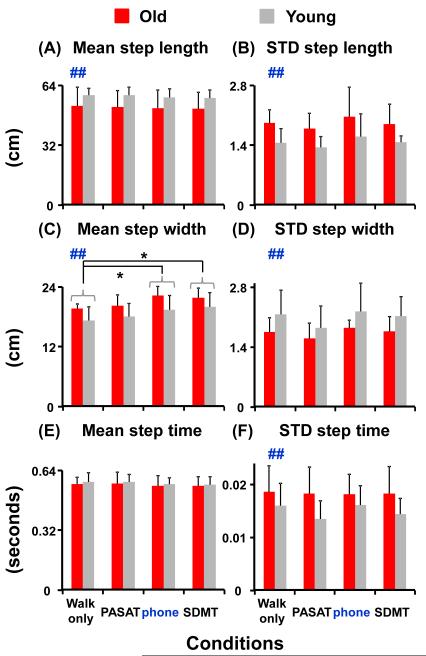
Both older and younger subjects walked with significantly greater average step width during the phone and SDMT conditions compared to walking only (Wilcoxon signed rank tests, both p<0.001) (Fig. 3). For the group effect, older subjects had significantly greater average step width (Mann-Whitney U test, p=0.002) but shorter average step length (p<0.001) compared to the younger subjects. There were no group or condition effects for the average step time. For the variability in step measures, older subjects had significantly greater step length variability (Mann-Whitney U test, p<0.001) and step time variability (p=0.012) but smaller step width variability (p=0.007) compared to the younger subjects. There were no condition effects for the variability on step width, length and time.
Figure 3.
(A) Mean and (B) variability of step length, (C) mean and (D) variability of step width, and (E) mean and (F) variability of step time for older (red bars) and younger (grey bars) subjects. Error bars represent 1 STD. ## indicates significant difference between younger and older subjects. * indicates significant difference between conditions.
Both older and younger subjects walked with less joint angle variability except for the hip joint during dual-task conditions compared to walking only (Fig. 4). For the ankle joint, both groups of subjects had significantly less variability during all dual-task conditions compared to walking only (Wilcoxon signed rank tests, all p<0.017). For the knee joint, both groups of subjects had significantly less variability during PASAT than during walking only (p=0.003). There were no group effects for the ankle or knee joint angle variability. For the hip joint, older subjects had significantly greater hip angle variability compared to younger subjects (Mann-Whitney U test, p=0.002). However, there was no condition effect in hip angle variability in older subjects (Friedman’s test, p=0.435). For younger subjects, hip angle variability was significantly smaller during PASAT compared to walking only (Wilcoxon signed rank test, p=0.017).
Figure 4.
Mean standard deviation (meanSD) of ankle, knee, and hip joint angle for older (red bars) and younger (grey bars) subjects. Error bars represent 1 STD. ## indicates significant difference between younger and older subjects. * indicates significant difference between conditions. The meanSD of joint kinematics was calculated across strides at each normalized time point (0-100%) of the gait cycle and then averaged over the whole gait cycle to produce a single measure of the mean variability for each trial.
Both older and younger subjects had significantly greater mediolateral trunk position variability, indicating more lateral drifts on the treadmill, during phone and SDMT conditions compared to walking only (Wilcoxon signed rank tests, p=0.003 and p=0.017, respectively) (Fig. 5). However, both group of subjects had significantly smaller anteroposterior trunk position variability during PASAT compared to walking only (p=0.001). There were no group effects for the trunk position variability in the mediolateral or anteroposterior directions.
Figure 5.
Mean standard deviation (meanSD) of C7 marker position in the anteroposterior (A-P) and mediolateral (M-L) directions for older (red bars) and younger (grey bars) subjects. Error bars represent 1 STD. * indicates significant difference between conditions. The meanSD of trunk position was calculated across strides at each normalized time point (0-100%) of the gait cycle and then averaged over the whole gait cycle to produce a single measure of the mean variability for each trial.
Discussion
Our findings do not support our hypothesis that healthy adults’ walking stability would be compromised during the cell phone dialing task and the two classic cognitive tests. We found that both healthy older and younger adults walked with similar levels of local stability during dual-tasking compared to walking only. This result is similar to the previous finding of Dingwel et al. (2008) [24], showing that walking stability was not affected by a concurrent cognitive task during treadmill walking in healthy adults. However, in the current study, healthy older and younger adults also walked with greater average mediolateral margins of stability and average step width during phone and SDMT conditions than during walking only. Moreover, healthy adults had less lower-limb joint angle variability during dual-task walking than during walking only. These findings suggest that healthy adults walked with a cautious walking pattern by adopting those energetically costly stabilization strategies (e.g., wider steps and less kinematic variability) to compensate for the increased stability challenges during dual-tasking. Healthy adults may try to control foot placement and joint kinematics during dual-task walking to ensure sufficient dynamic margins of stability and maintain local stability similar to walking only. Moreover, the increased gait variability during dual-tasking shown in the previous studies involving walking over ground may have resulted from reduced walking speed.
We also found that healthy older and younger adults had significantly greater mediolateral drift on the treadmill, average mediolateral margins of stability, and average step width during phone and SDMT conditions compared to walking only. However, these measures during PASAT were not significantly different from those during walking only. The findings suggest that phone and SDMT dual-task walking may pose greater stability challenges to the subjects compared to PASAT as increasing step width and margins of stability are common compensatory strategies to manage balance perturbations [25]. This is somewhat surprising since it is widely known clinically that patients find the PASAT to be a demanding task. Similar to the findings of Marone et al. (2014) [26], our results suggest that the added physical demand such as reduced arm swing and altered head orientation may play an important role in modifying gait during dual-tasking since both the phone and SDMT tasks require subjects to hold and look at something in their hands. Thus, minimizing the physical alteration associated with phone manipulation may be key to reducing the risk of falls. However, it is important to note that both the phone and SDMT tasks have a large visual component not present in the PASAT and others have speculated that this characteristic of the cognitive task is paramount in producing gait changes while dual tasking [12]. In addition, both the phone and SDMT tasks are self-paced while PASAT is externally-paced. The temporal constraints of PASAT might have been linked to the timing of gait and thus, limiting the influence of PASAT on walking.
We did not find significant group effects on mediolateral local stability or margins of stability during walking only or dual-tasking. Our older subjects only showed a trend to have slightly more local instability and walked with slightly greater mediolateral margins of stability compared to younger subjects regardless of conditions. In addition, we did not find greater dual-tasking effects on walking stability in older adults than in younger adults. Older and younger subjects had a similar trend of gait modification during dual-task walking except for the hip angle variability. It is possible that the older subjects in the current study were relatively young [average age: 61 years] compared to those studied previously by e.g., Kang and Dingwell (2009) [27] [average age: 72.1 years], Lockhart and Liu (2008) [28] [average age: 71.3 years], and Buzzi et al (2003) [29] [age range: 71-79 years]. To better understand the aging effect on walking stability during cell phone use, future studies should include subjects with age of greater than 65 years.
It is usually assumed that reduced variability is related to increased stability. However, in the current study, walking with reduced movement variability did not enhance walking stability during dual-tasking in healthy adults. It was hypothesized that there are two components of motor variability in control of human movement [30]. One component of motor variability, manifested as the errors or noise in the neuromuscular control, leads to errors regarding the task performance and/or mechanical instability (i.e., “bad” variability). Another component of motor variability, manifested as the flexibility of the central nervous system for effectively controlling movements during unpredictable situations, does not lead to errors in task performance and/or mechanical instability (i.e., “good” variability). It is possible that healthy adults reduced good motor variability during dual-task walking, which might be also explained by their cautious, “inflexible” gait pattern. Although walking stability was not compromised during cell phone use, the reduction of good variability would lower the flexibility of motor control when responding to unexpected perturbations (e.g., unnoticed obstacles, uneven walking surface), which might also lead to an increased risk of falls.
We performed all the assessments during treadmill walking in the current study. Testing at a constant walking speed during the dual-task conditions was intended to determine if the increased overground gait variability during dual-tasking shown previously [8] resulted from the reduced walking speed or reflected reduced stability. In addition, a plethora of research findings have shown that the overall mechanics of treadmill and overground gaits are very similar in healthy young and older adults regarding the kinematic, kinetic, and temporal gait patterns [31-34]. Furthermore, our subjects were given time to familiarize themselves to treadmill walking.
The current study examined gait stability and variability in healthy adults during concurrent cell phone use or a classic cognitive task. Our results demonstrate that walking stability was not compromised by the dual task in healthy adults. During dual-tasking, healthy adults walked cautiously by having wider steps and less lower-limb joint variability compared to walking only. In addition, a dual task that also introduces physical alteration or taxes visual attention may likely pose greater stability challenges and result in greater gait modification than a dual task that only taxes auditory attention. Therefore, minimizing the physical alteration or visual distraction associated with cell phone manipulation may help reduce the risk of falls.
Highlights.
We examined walking stability during cell phone use and classic cognitive tasks.
Healthy subjects’ walking stability was not compromised by the dual task.
Subjects increased step width and reduced lower-limb joint variability during dual-tasking.
A dual task taxing physical alteration or visual attention causes greater gait modification.
Minimizing physical alteration or visual distraction associated with cell phone use may help reduce falls.
Table 1.
Descriptive statistics for gait stability and variability parameters for the older and younger groups
|
| |||||||||||
| Old | Young | Group | Condition | Post-hoc comparisons |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Walk only |
PASAT | phone | SDMT | Walk only |
PASAT | Phone | SDMT | (p-value) | (p-value) | (vs. walk only) | |
|
| |||||||||||
| M-L local stability |
0.134 ± 0.034 |
0.137 ± 0.033 |
0.139 ± 0.036 |
0.133 ± 0.027 |
0.108 ± 0.023 |
0.105 ± 0.033 |
0.120 ± 0.027 |
0.115 ± 0.044 |
0.079 | 0.878 | n.s. |
|
| |||||||||||
| A-P local stability |
0.151 ± 0.024 |
0.151 ± 0.014 |
0.164 ± 0.025 |
0.153 ± 0.018 |
0.158 ± 0.020 |
0.140 ± 0.020 |
0.153 ± 0.014 |
0.150 ± 0.018 |
0.478 | 0.160 | n.s. |
|
| |||||||||||
| VT local stability |
0.301 ± 0.069 |
0.315 ± 0.132 |
0.344 ± 0.128 |
0.290 ± 0.111 |
0.275 ± 0.069 |
0.253 ± 0.086 |
0.297 ± 0.070 |
0.294 ± 0.078 |
0.415 | 0.233 | n.s. |
|
| |||||||||||
| Mean MOSAP (cm) |
40.6 ± 6.0 |
40.2 ± 5.8 |
40.1 ± 5.9 |
40.2 ± 5.4 |
47.5 ± 2.5 |
47.1 ± 2.5 |
46.8 ± 2.5 |
46.8 ± 2.6 |
<0.001 | 0.225 | n.s. |
|
| |||||||||||
| STD MOSAP (cm) |
1.16 ± 0.24 |
1.04 ± 0.13 |
1.11 ± 0.27 |
1.09 ± 0.26 |
1.16 ± 0.23 |
0.97 ± 0.15 |
1.13 ± 0.22 |
1.04 ± 0.14 |
0.382 | 0.160 | n.s. |
|
| |||||||||||
| Mean MOSML (cm) |
13.8 ± 1.2 |
14.2 ± 1.6 |
15.1 ± 1.6 |
15.0 ± 1.6 |
13.2 ± 2.8 |
13.8 ± 2.7 |
14.4 ± 2.6 |
14.5 ± 2.5 |
0.080 | <0.001 | phone SDMT |
|
| |||||||||||
| STD MOSML (cm) |
0.89 ± 0.06 |
0.81 ± 0.11 |
0.82 ± 0.07 |
0.86 ± 0.12 |
0.99 ± 0.23 |
0.81 ± 0.18 |
0.95 ± 0.25 |
0.95 ± 0.14 |
0.194 | 0.168 | n.s. |
|
| |||||||||||
| Mean step length (cm) |
53.0 ± 9.8 |
52.3 ± 8.9 |
51.7 ± 9.8 |
51.5 ± 8.9 |
58.8 ± 3.5 |
58.6 ± 4.3 |
57.6 ± 4.4 |
57.2 ± 4.3 |
<0.001 | 0.836 | n.s. |
|
| |||||||||||
| STD step length (cm) |
1.92 ± 0.31 |
1.79 ± 0.35 |
2.07 ± 0.68 |
1.89 ± 0.47 |
1.46 ± 0.33 |
1.34 ± 0.26 |
1.60 ± 0.53 |
1.47 ± 0.14 |
<0.001 | 0.618 | n.s. |
|
| |||||||||||
| Mean step width (cm) |
19.6 ± 1.0 |
20.2 ± 2.1 |
22.2 ± 1.8 |
21.7 ± 2.0 |
17.3 ± 2.7 |
18.1 ± 2.6 |
19.4 ± 2.9 |
20.0 ± 2.8 |
0.002 | <0.001 | phone SDMT |
|
| |||||||||||
| STD step width (cm) |
1.76 ± 0.33 |
1.61 ± 0.35 |
1.85 ± 0.18 |
1.76 ± 0.35 |
2.16 ± 0.57 |
1.85 ± 0.50 |
2.23 ± 0.67 |
2.13 ± 0.45 |
0.007 | 0.077 | n.s. |
|
| |||||||||||
| Mean step time (sec) |
0.566 ± 0.037 |
0.569 ± 0.062 |
0.558 ± 0.054 |
0.557 ± 0.049 |
0.579 ± 0.049 |
0.578 ± 0.041 |
0.567 ± 0.032 |
0.564 ± 0.040 |
0.424 | 0.056 | n.s. |
|
| |||||||||||
| STD step time (sec) |
0.019 ± 0.005 |
0.018 ± 0.005 |
0.018 ± 0.004 |
0.018 ± 0.005 |
0.016 ± 0.004 |
0.014 ± 0.003 |
0.016 ± 0.004 |
0.014 ± 0.003 |
0.012 | 0.457 | n.s. |
|
| |||||||||||
| meanSD Ankle (°) |
1.37 ± 0.16 |
1.27 ± 0.12 |
1.27 ± 0.23 |
1.22 ± 0.21 |
1.43 ± 0.24 |
1.08 ± 0.15 |
1.24 ± 0.23 |
1.20 ± 0.08 |
0.319 | 0.001 | PASAT phone SDMT |
|
| |||||||||||
| meanSD Knee (°) |
2.42 ± 0.48 |
2.10 ± 0.41 |
2.28 ± 0.35 |
2.16 ± 0.33 |
2.32 ± 0.51 |
1.80 ± 0.27 |
2.09 ± 0.37 |
2.01 ± 0.31 |
0.053 | 0.002 | PASAT |
|
| |||||||||||
| meanSD Hip (°) |
1.49 ± 0.28 |
1.45 ± 0.42 |
1.47 ± 0.23 |
1.41 ± 0.23 |
1.41 ± 0.21 |
1.09 ± 0.12 |
1.24 ± 0.17 |
1.16 ± 0.21 |
0.002 | 0.024 | PASAT (only in Young) |
|
| |||||||||||
| meanSD A-P position (cm) |
4.16 ± 1.80 |
2.86 ± 1.25 |
3.47 ± 0.67 |
4.54 ± 2.38 |
4.48 ± 0.89 |
2.53 ± 0.29 |
3.11 ± 0.69 |
3.25 ± 1.26 |
0.327 | 0.007 | PASAT |
|
| |||||||||||
| meanSD M-L position (cm) |
1.93 ± 0.20 |
1.75 ± 0.37 |
2.38 ± 0.40 |
2.37 ± 0.58 |
1.83 ± 0.45 |
1.54 ± 0.31 |
2.30 ± 0.46 |
2.23 ± 0.30 |
0.382 | <0.001 | phone SDMT |
|
| |||||||||||
Acknowledgements
The authors thank Amy Bucha for assisting with data collection. This work was partially supported by NIH grant HD 038582.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The study was partially published as an abstract in the Proceedings of the 7th World Congress of Biomechanics (Boston, MA, 2014).
Conflict of Interest Statement
There are no conflicts of interest in this work.
References
- [1].Nasar JL, Troyer D. Pedestrian injuries due to mobile phone use in public places. Accident; analysis and prevention. 2013;57:91–5. doi: 10.1016/j.aap.2013.03.021. [DOI] [PubMed] [Google Scholar]
- [2].Catherine Chase JD. U.s. State and federal laws targeting distracted driving. Annals of advances in automotive medicine / Annual Scientific Conference Association for the Advancement of Automotive Medicine Association for the Advancement of Automotive Medicine Scientific Conference; 2014. pp. 84–98. [PMC free article] [PubMed] [Google Scholar]
- [3].Schabrun SM, van den Hoorn W, Moorcroft A, Greenland C, Hodges PW. Texting and walking: strategies for postural control and implications for safety. PLoS One. 2014;9:e84312. doi: 10.1371/journal.pone.0084312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Stavrinos D, Byington KW, Schwebel DC. Distracted walking: cell phones increase injury risk for college pedestrians. Journal of safety research. 2011;42:101–7. doi: 10.1016/j.jsr.2011.01.004. [DOI] [PubMed] [Google Scholar]
- [5].Lamberg EM, Muratori LM. Cell phones change the way we walk. Gait Posture. 2012;35:688–90. doi: 10.1016/j.gaitpost.2011.12.005. [DOI] [PubMed] [Google Scholar]
- [6].Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture. 2002;16:1–14. doi: 10.1016/s0966-6362(01)00156-4. [DOI] [PubMed] [Google Scholar]
- [7].Yogev-Seligmann G, Hausdorff JM, Giladi N. The role of executive function and attention in gait. Mov Disord. 2008;23:329–42. doi: 10.1002/mds.21720. quiz 472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Yogev-Seligmann G, Rotem-Galili Y, Mirelman A, Dickstein R, Giladi N, Hausdorff JM. How does explicit prioritization alter walking during dual-task performance? Effects of age and sex on gait speed and variability. Phys Ther. 2010;90:177–86. doi: 10.2522/ptj.20090043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hollman JH, Kovash FM, Kubik JJ, Linbo RA. Age-related differences in spatiotemporal markers of gait stability during dual task walking. Gait Posture. 2007;26:113–9. doi: 10.1016/j.gaitpost.2006.08.005. [DOI] [PubMed] [Google Scholar]
- [10].Amboni M, Barone P, Hausdorff JM. Cognitive contributions to gait and falls: evidence and implications. Mov Disord. 2013;28:1520–33. doi: 10.1002/mds.25674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Beurskens R, Bock O. Does the walking task matter? Influence of different walking conditions on dual-task performances in young and older persons. Hum Mov Sci. 2013;32:1456–66. doi: 10.1016/j.humov.2013.07.013. [DOI] [PubMed] [Google Scholar]
- [12].Beurskens R, Bock O. Age-related deficits of dual-task walking: a review. Neural plasticity. 2012;2012:131608. doi: 10.1155/2012/131608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dingwell JB, Marin LC. Kinematic variability and local dynamic stability of upper body motions when walking at different speeds. J Biomech. 2006;39:444–52. doi: 10.1016/j.jbiomech.2004.12.014. [DOI] [PubMed] [Google Scholar]
- [14].Ortega JD, Fehlman LA, Farley CT. Effects of aging and arm swing on the metabolic cost of stability in human walking. J Biomech. 2008;41:3303–8. doi: 10.1016/j.jbiomech.2008.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Collins SH, Adamczyk PG, Kuo AD. Dynamic arm swinging in human walking. Proceedings Biological sciences / The Royal Society. 2009;276:3679–88. doi: 10.1098/rspb.2009.0664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Raphan T, Imai T, Moore ST, Cohen B. Vestibular compensation and orientation during locomotion. Annals of the New York Academy of Sciences. 2001;942:128–38. doi: 10.1111/j.1749-6632.2001.tb03740.x. [DOI] [PubMed] [Google Scholar]
- [17].Hof AL, Gazendam MG, Sinke WE. The condition for dynamic stability. J Biomech. 2005;38:1–8. doi: 10.1016/j.jbiomech.2004.03.025. [DOI] [PubMed] [Google Scholar]
- [18].Tombaugh TN. A comprehensive review of the Paced Auditory Serial Addition Test (PASAT) Archives of clinical neuropsychology : the official journal of the National Academy of Neuropsychologists. 2006;21:53–76. doi: 10.1016/j.acn.2005.07.006. [DOI] [PubMed] [Google Scholar]
- [19].Sheridan LK, Fitzgerald HE, Adams KM, Nigg JT, Martel MM, Puttler LI, Wong MM, Zucker RA. Normative Symbol Digit Modalities Test performance in a community-based sample. Archives of clinical neuropsychology : the official journal of the National Academy of Neuropsychologists. 2006;21:23–8. doi: 10.1016/j.acn.2005.07.003. [DOI] [PubMed] [Google Scholar]
- [20].Beurskens R, Wilken JM, Dingwell JB. Dynamic stability of individuals with transtibial amputation walking in destabilizing environments. J Biomech. 2014;47:1675–81. doi: 10.1016/j.jbiomech.2014.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Dingwell JB, Cusumano JP. Nonlinear time series analysis of normal and pathological human walking. Chaos. 2000;10:848–63. doi: 10.1063/1.1324008. [DOI] [PubMed] [Google Scholar]
- [22].England SA, Granata KP. The influence of gait speed on local dynamic stability of walking. Gait Posture. 2007;25:172–8. doi: 10.1016/j.gaitpost.2006.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].McAndrew Young PM, Dingwell JB. Voluntarily changing step length or step width affects dynamic stability of human walking. Gait Posture. 2012;35:472–7. doi: 10.1016/j.gaitpost.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Dingwell JB, Robb RT, Troy KL, Grabiner MD. Effects of an attention demanding task on dynamic stability during treadmill walking. J Neuroeng Rehabil. 2008;5:12. doi: 10.1186/1743-0003-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hak L, Houdijk H, Steenbrink F, Mert A, van der Wurff P, Beek PJ, van Dieen JH. Speeding up or slowing down?: Gait adaptations to preserve gait stability in response to balance perturbations. Gait Posture. 2012;36:260–4. doi: 10.1016/j.gaitpost.2012.03.005. [DOI] [PubMed] [Google Scholar]
- [26].Marone JR, Patel PB, Hurt CP, Grabiner MD. Frontal plane margin of stability is increased during texting while walking. Gait Posture. 2014;40:243–6. doi: 10.1016/j.gaitpost.2014.04.188. [DOI] [PubMed] [Google Scholar]
- [27].Kang HG, Dingwell JB. Dynamic stability of superior vs. inferior segments during walking in young and older adults. Gait Posture. 2009;30:260–3. doi: 10.1016/j.gaitpost.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lockhart TE, Liu J. Differentiating fall-prone and healthy adults using local dynamic stability. Ergonomics. 2008;51:1860–72. doi: 10.1080/00140130802567079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Buzzi UH, Stergiou N, Kurz MJ, Hageman PA, Heidel J. Nonlinear dynamics indicates aging affects variability during gait. Clin Biomech (Bristol, Avon) 2003;18:435–43. doi: 10.1016/s0268-0033(03)00029-9. [DOI] [PubMed] [Google Scholar]
- [30].Latash ML, Scholz JP, Schoner G. Motor control strategies revealed in the structure of motor variability. Exerc Sport Sci Rev. 2002;30:26–31. doi: 10.1097/00003677-200201000-00006. [DOI] [PubMed] [Google Scholar]
- [31].Riley PO, Paolini G, Della Croce U, Paylo KW, Kerrigan DC. A kinematic and kinetic comparison of overground and treadmill walking in healthy subjects. Gait Posture. 2007;26:17–24. doi: 10.1016/j.gaitpost.2006.07.003. [DOI] [PubMed] [Google Scholar]
- [32].Lee SJ, Hidler J. Biomechanics of overground vs. treadmill walking in healthy individuals. Journal of applied physiology. 2008;104:747–55. doi: 10.1152/japplphysiol.01380.2006. [DOI] [PubMed] [Google Scholar]
- [33].Parvataneni K, Ploeg L, Olney SJ, Brouwer B. Kinematic, kinetic and metabolic parameters of treadmill versus overground walking in healthy older adults. Clin Biomech (Bristol, Avon) 2009;24:95–100. doi: 10.1016/j.clinbiomech.2008.07.002. [DOI] [PubMed] [Google Scholar]
- [34].Rosenblatt NJ, Grabiner MD. Measures of frontal plane stability during treadmill and overground walking. Gait Posture. 2010;31:380–4. doi: 10.1016/j.gaitpost.2010.01.002. [DOI] [PubMed] [Google Scholar]