Abstract
PURPOSE
This study aimed to evaluate the effect of implant thread depth on primary stability in low density bone.
MATERIALS AND METHODS
The insertion torque was measured by inserting Ti implants with different thread depths into solid rigid polyurethane blocks (Sawbones) with three different bone densities (0.16 g/cm3, 0.24 g/cm3, and 0.32 g/cm3). The insertion torque value was evaluated with a surgical engine. The static compressive strength was measured with a universal testing machine (UTM) and the Ti implants were aligned at 30° against the loading direction of the UTM. After the static compressive strength test, the Ti implants were analyzed with a Measurescope.
RESULTS
The Ti implants with deeper thread depth showed statistically higher mean insertion torque values (P<.001). Groups A and group B had similar maximum static compressive strengths, as did groups C and D (P>.05). After the static compressive strength, the thread shape of the Ti implants with deeper thread depth did not show any breakage but did show deformation of the implant body and abutment.
CONCLUSION
The implants with deeper thread depth had higher mean insertion torque values but not lower compressive strength. The deep threads had a mechanical stability. Implants with deeper thread depth may increase the primary stability in areas of poor quality bone without decreasing mechanical strength.
Keywords: Deep thread, Primary stability, Insertion torque, Compressive strength, Dental implant, Mechanical stability
INTRODUCTION
Success rates of dental implants in the edentulous mandible exceed 95% in most long-term clinical studies.1,2 However, implant failure is still considerable in areas of poor quality bone3,4 such as the maxillary region. The long-term success of implant therapy is achieved by the primary stability of the implant for mechanical support from the surrounding bone in the early stage and osseointegration between the surrounding bone and implant through bone regeneration and remodeling in the late stage.5 Primary stability is especially necessary in poor quality bone. The instability of dental implants results in fibrous encapsulation and failure to achieve osseointegration.6 Primary stability is fundamental for successful osseointegration. Clinicians and implant manufacturers have made a major effort to increase the success rates of dental implants by improving primary stability. One of the methods of increasing primary stability is by modifying the surgical technique for implant placement. Studies have reported that the undersized surgical technique, which uses a final drill diameter smaller than the diameter of the implant, results in higher primary stability than dose the press-fit technique.5,7 Other studies have reported higher implant stability with the bone-condensing technique compared with bone-drilling technique8,9 and the conventional technique compared with the osteotome technique.10,11
Surface roughness is also important for achieving good primary stability. In mechanical evaluation, dental implants having higher average roughness showed better primary stability than machined implants did5,12,13 and good osseointegration between the implant and surrounding bone in animal studies.14,15,16
Another method for increasing primary stability is to change the implant design, such as the shape of the implant body and thread, the length, or the diameter. Various thread designs in tapered implants and various designs of dental implants have been reported to have an effect on primary stability. It has been reported that tapered implants showed higher primary stability than cylindrical implants.17,18,19 In addition, dental implants with a long length or wide diameter showed a significant increase in insertion torque.17,19 One study has reported that using dental implants without self-tapping blades increases the primary stability compared with that with self-tapping blades.20
Several studies have described the stress distribution in Ti implants with various thread depths by using finite element analysis (FEA) and reported the most effective thread depth for stress distribution.21,22,23 Thread depth has a greater contribution than thread width to stress distribution to the bone.23 Ti implants with a deeper thread depth provide a larger surface area and have an advantage in areas of poor quality bone by increasing stability.24 Ti implants with deeper thread depths may increase loads on and mechanical interlocking with poor quality bone. Although several studies have measured the mechanical stability through stress distribution in Ti implants with various thread depths by FEA, to our knowledge, no mechanical studies investigating the effects of the thread depth of dental implants on enhancing primary stability have been published.
We used tapered implants with deeper thread depths than commercially available dental implants to increase the primary stability. We investigated the primary stability in tapered implants with various thread depths by mechanical testing. To measure the primary stability of implants, Periotest, resonance frequency analysis (RFA), insertion torque, and removal torque are possible methods. However, the Periotest is not able to identify minor differences25,26 and with RFA an implant stability quotient (ISQ) cutoff value for sufficient primary stability has not been defined, so ISQ values for different implant systems cannot be compared.27 The insertion torque and removal torque is commonly used to measure the primary stability of dental implants. Increasing the insertion torque can increase the primary stability through reduction of the micromotion in soft bone,28 but excessive insertion torque causes a high incidence of failure.29
Therefore, the control of insertion torque for implant placement is important. We evaluated the primary stability of dental implants with various thread depths by using the insertion torque test, and the stability of deeper threads from breakage after mechanical strength testing was also analyzed.
MATERIALS AND METHODS
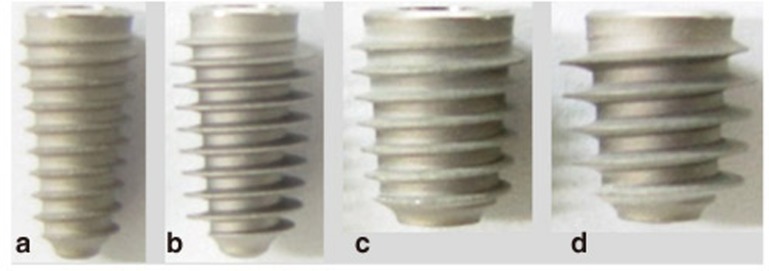
Commercial Ti implants (AnyRidge® Internal implants) roughened by grit-blasting were used in this study (Megagen Co. Ltd., Kyungsan, Korea). The Ti implants had various lengths, diameters, and thread depths (Fig. 1). Detailed information about the length, diameter, and thread depth of the Ti implants is specified in Table 1. We selected Ti implants possessing the same length and inner diameter but with different outer diameters. We compared the test values of group A and group B and those of group C and group D. EZ post abutments were prepared for static compressive strength. The EZ Post had a profile diameter of 5.0 mm, a cuff height of 3.0 mm, and a post height of 5.5 mm for groups A and B and a profile diameter of 6.0 mm, a cuff height of 3.0 mm, and a post height of 7.0 mm for groups C and D.
Fig. 1. Photographs of four different Ti implants: (a) Group A; (b) Group B; (c) Group C; (d) Group D.
Table 1. The characteristics of four different Ti implants.
| Group | Length (mm) | Outer diameter (mm) | Inner diameter (mm) | Thread depth (mm) |
|---|---|---|---|---|
| A | 10 | 4.0 | 3.3 | 0.35 |
| B | 10 | 5.0 | 3.3 | 0.85 |
| C | 8 | 6.0 | 4.8 | 0.60 |
| D | 8 | 7.0 | 4.8 | 1.10 |
Solid rigid polyurethane blocks (Sawbones Pacific Research Laboratories Inc., Vashon Island, WA, USA) with uniformity were used as an alternative to human cancellous bone. There is little variation in the qualities of the material among samples, and thus the blocks can be used as materials for comparative tests. Insertion tests using solid rigid polyurethane blocks provide more objective data than those using animal or human cadaver bones. The bone mineral density of the solid rigid polyurethane blocks was 0.16 g/cm3, 0.24 g/cm3, and 0.32 g/cm3. All of the bone holes for implant placement were prepared according to the recommended surgical protocol supplied by the manufacturer. The Ti implants were installed using a surgical engine (Elcomed SA200C, W&H, Bürmoos, Austria) with a rotation speed of 30 rpm and a torque value of 70 Ncm. The recorded torque value was read by impDAT software (Kea Software GmbH, Poecking, Germany).
The Ti implant and the EZ Post abutment were tightened with the recommended torque (30 Ncm) by using a digital torque meter (Mark-10, New York, NY, USA). The hemispherical loading member was assembled above the EZ Post. The Ti implants tightened with the EZ Post containing the hemispherical loading member were fixed with a specimen holder that was made from brass and clamped in the jig of a universal test machine (Instron, 3366, Instron, Corp., Norwood, MA, USA). The implant/abutment assembly was placed at 30° against the axis of the loading direction and set at a distance of about l = 11 mm from the center of the hemispherical loading member to the clamping plane of a jig, as shown Fig. 2. The loading device was positioned in contact with the top of the hemispherical loading member and loaded at a rate of 1.0 mm/min in a unidirectional vertical direction until the failure load that induced buckling was observed. The value of the load and displacement was recorded by Series IX software (Instron, 3366, Instron, Corp., Norwood, MA, USA).
Fig. 2. Photograph depicting the installation of Ti implants and abutment complex for the static compressive strength test. The axis of the loading direction against the axis of the dental implant system was 30°.
The hemispherical loading member was removed from the implant/abutment assembly after the static compressive strength tests. The implant/abutment was mounted with an acrylic resin (R&B, Daejeon, Korea) using an automatic mounting press (R&B, Daejeon, Korea) and was polished by using a polisher (R&B, Daejeon, Korea) changing the grit of the sand paper (400, 800, 1500). The morphology of the thread was observed with a Measurescope.
Statistical analysis was performed with SPSS 11.0 statistical software (SPSS Inc., Chicago, IL, USA). The paired Student's t-test was performed to compare the significance of the differences. Values of P were statistically significant at <.05.
RESULTS
The results of the mean insertion torque found for a bone density of 0.16 g/cm3 are shown in Table 2. The mean insertion torques of group A and group B were 12.37 ± 0.40 and 20.53 ± 1.07, and those of group C and the group D were 28.93 ± 1.07 and 36.17 ± 0.40, respectively. The results of the mean insertion torque found for a bone density of 0.24 g/cm3 are shown in Table 3. The mean insertion torques of groups A and B were 20.77 ± 1.07 and 32.67 ± 2.02, and those of groups C and D were 26.83 ± 1.46 and 50.87 ± 2.83, respectively. The results of the mean insertion torque found for a bone density of 0.32 g/cm3 are shown in Table 4. The mean insertion torques of groups A and B were 9.10 ± 1.21 and 35.47 ± 0.40 and those of groups C and D were 35.70 ± 4.20 and 68.83 ± 2.65, respectively. The Ti implants with deeper threads had significantly higher insertion torque for all bone densities tested (P<.001).
Table 2. The insertion torque values with a bone density of 0.16 g/cm3 (mean ± SD; n=5).
| Group | Insertion torque value (Ncm) | Comparison | P value |
|---|---|---|---|
| A | 12.37 ± 0.40 | A versus B | <.001 |
| B | 20.53 ± 1.07 | ||
| C | 28.93 ± 1.07 | C versus D | <.001 |
| D | 36.17 ± 0.40 |
Table 3. The insertion torque values with a bone density of 0.24 g/cm3 (mean ± SD; n=5).
| Group | Insertion torque value (Ncm) | Comparison | P value |
|---|---|---|---|
| A | 20.77 ± 1.07 | A versus B | <.001 |
| B | 32.67 ± 2.01 | ||
| C | 26.83 ± 1.46 | C versus D | <.001 |
| D | 50.87 ± 2.83 |
Table 4. The insertion torque values with a bone density of 0.32 g/cm3 (mean ± SD; n=5).
| Group | Insertion torque value (Ncm) | Comparison | P value |
|---|---|---|---|
| A | 9.1 ± 1.21 | A versus B | <.001 |
| B | 35.47 ± 0.40 | ||
| C | 35.7 ± 4.20 | C versus D | <.001 |
| D | 68.83 ± 2.65 |
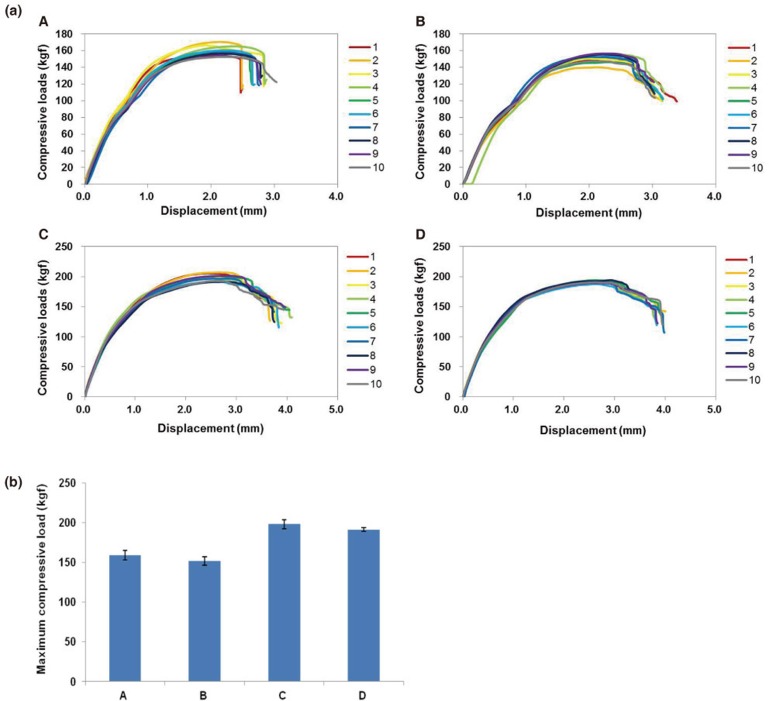
The load-displacement curves from the static compressive test are shown in Fig. 3a. The 10 load-displacement curves in the same group showed a similar pattern and the distance of displacement in the implants with the same inner diameter (group A and B; group C and D) was similar. The maximum compressive values, that is, the maximum compressive load, are shown in Fig. 3b. The Ti implants with the same length and inner diameter showed a similar maximum compressive load regardless of the thread depth (P>.05).
Fig. 3. (a) The load-displacement curve of group A (A), group B (B), group C (C), and group D (D). The 10 specimens of each group showed a similar pattern. (b) The maximum compressive strengths of four different Ti implants. Data is expressed as the mean ± SD (n=10). There were no significant differences between A and B or C and D (P>.05).
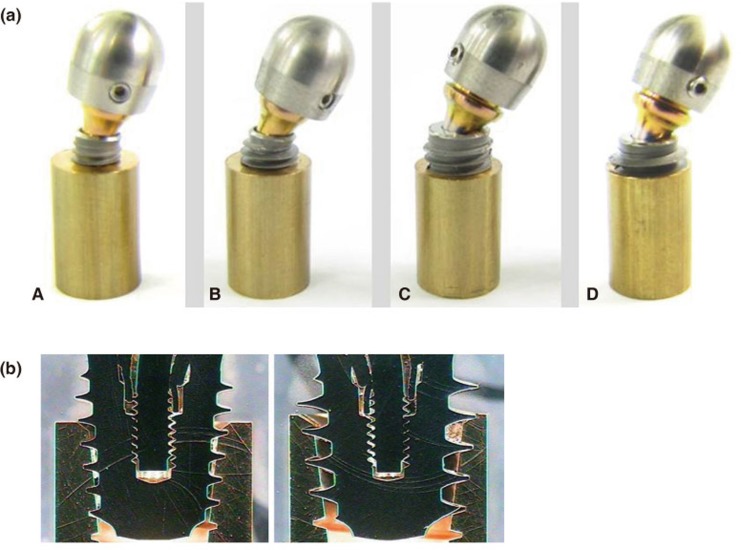
After the static compressive strength tests, the Ti implants were examined macroscopically. The failure mode was observed to be deformation in the abutment and being torn horizontally at the upper side of the Ti implant (Fig. 4A). The threads in the Ti implants with deeper threads did not show breakage (Fig. 4B).
Fig. 4. (a) The failure mode of group A (A), group B (B), group C (C), and group D (D) after the static compressive strength tests. The deformation was observed in the implant body and the abutment but not the threads. (b) The thread morphology of group C (A) and group D (B) after the static compressive strength tests. Breakage was not observed in the threads in the Ti implants with deeper threads.
DISCUSSION
Primary stability is important for osseointegration. We enlarged the surface area by creating a deeper thread depth to improve the primary stability. Our study investigated the primary stability in tapered implants with various thread depths using mechanical tests. Tapered implants with deeper thread depths resulted in higher insertion torque and thus showed better primary stability. The Periotest has a low correlation with torque and does not explain the variation between the parameters.25 It is more effective at gathering information on osseointegration than primary stability.26 RFA is not comparable to the ISQ values obtained from different implant systems and has a low correlation with insertion torque.27 Thus RFA is not suitable as a single method for the measurement of primary stability. The insertion torque and removal torque is commonly used to measure the primary stability of dental implants in mechanical testing. Insertion torque is a more effective indicator of primary stability than the RFA and the Periotest. Our studies investigated the effect of thread depth on the insertion torque values in various bone densities. Dental implants with deeper thread depth showed higher insertion torques than those with shallower thread depth when having the same inner diameter in the same bone density (Table 2, Table 3, Table 4). This means that the increase in the thread depth in dental implants with the same inner diameter provides better primary stability at lower bone densities. Thread depth affects bone stresses and implant/abutment complex stability, and the effect of thread depth differs according to the bone density.21 Therefore, it was thought that confirming the optimal thread depth at specific bone densities is necessary. The insertion torque is increased with increasing bone density.5 In our data, the insertion torque did not show a direct association with bone density. This is related to the drill used for implant placement. We used different drill diameters for different bone densities of the solid rigid polyurethane block. Specifically, we used a drill with a larger diameter in higher bone density and a smaller diameter in lower bone density.
We have demonstrated that Ti implants with the same length and inner diameter have a similar maximum compressive strength. The mechanical strength is more related to the length and diameter than the thread depth. The failure mode was observed in the fixtures and abutments but not the threads. The thread depth did not have a major effect on the mechanical strength. Ti implants with deeper threads did not induce the breakage of threads applying the maximum compressive strength. Dental implants may fracture at load levels below the maximum compressive strength of the implant/abutment complex. Thus, the maximum compressive strength may suggest a standard point of acute overload. Mechanical failures of dental implants appear through a repeated loading process at low loads.30 The fatigue test is a general method used in the laboratory to mimic actual intraoral use. The fatigue limits of the dental implants with a diameter of 4.0 mm and thread depth of 0.6 mm (636 N) and those with a diameter of 4.0 mm and thread depth of 0.35 mm (619 N) in the fatigue test on the basis of the International Organization for Standardization (ISO14801) were both more than 600 N (Data is not shown). The fatigue limit of the Ti implants with deeper threads is similar to that of Ti implants with shallow thread depth. Our study indicated that the Ti implants with the deeper threads have similar mechanical stability.
This is the first study that attempted mechanical test by varying the thread depth in Ti implants with the same implant body (tapered implants). Recently, we published our finding that the bone is formed until it is inside the deep threads (root portion) and that Ti implants with deeper thread depth are osseointegrated in animal studies.31 We also have ongoing research on clinical application of Ti implants with deeper thread depth in areas of poor quality bone in order to confirm their primary stability and survival rate.
This study suggests that Ti implants with deeper threads have greater insertion torque without a concomitant decrease in mechanical strength. Implants with deeper thread depth may increase the primary stability in areas of poor quality bone without decreasing the mechanical strength. Dental implants with primary stability increase the percentage of direct bone-to-implant contact (BIC),6 while dental implants without primary instability result in a lack of osseointegration, and ultimately implant failure.32,33
CONCLUSION
An increase in primary stability may increase biological stability through bone regeneration and remodeling between the surrounding bone and implant. Dental implants with deeper thread depth may lead to successful osseointegration and decrease implant failure in areas of poor quality bone.
Footnotes
This research was supported by a grant from the Industry Original Technology Development Projectfunded by the Ministry of Knowledge Economy, Korea.
References
- 1.Heschl A, Payer M, Platzer S, Wegscheider W, Pertl C, Lorenzoni M. Immediate rehabilitation of the edentulous mandible with screw type implants: results after up to 10 years of clinical function. Clin Oral Implants Res. 2012;23:1217–1223. doi: 10.1111/j.1600-0501.2011.02292.x. [DOI] [PubMed] [Google Scholar]
- 2.Testori T, Wiseman L, Woolfe S, Porter SS. A prospective multicenter clinical study of the Osseotite implant: four-year interim report. Int J Oral Maxillofac Implants. 2001;16:193–200. [PubMed] [Google Scholar]
- 3.Friberg B, Ekestubbe A, Sennerby L. Clinical outcome of Brånemark System implants of various diameters: a retrospective study. Int J Oral Maxillofac Implants. 2002;17:671–677. [PubMed] [Google Scholar]
- 4.Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62:2–4. doi: 10.1902/jop.1991.62.1.2. [DOI] [PubMed] [Google Scholar]
- 5.Tabassum A, Meijer GJ, Wolke JG, Jansen JA. Influence of the surgical technique and surface roughness on the primary stability of an implant in artificial bone with a density equivalent to maxillary bone: a laboratory study. Clin Oral Implants Res. 2009;20:327–332. doi: 10.1111/j.1600-0501.2008.01692.x. [DOI] [PubMed] [Google Scholar]
- 6.Lioubavina-Hack N, Lang NP, Karring T. Significance of primary stability for osseointegration of dental implants. Clin Oral Implants Res. 2006;17:244–250. doi: 10.1111/j.1600-0501.2005.01201.x. [DOI] [PubMed] [Google Scholar]
- 7.Tabassum A, Walboomers XF, Wolke JG, Meijer GJ, Jansen JA. Bone particles and the undersized surgical technique. J Dent Res. 2010;89:581–586. doi: 10.1177/0022034510363263. [DOI] [PubMed] [Google Scholar]
- 8.Fanuscu MI, Chang TL, Akça K. Effect of surgical techniques on primary implant stability and peri-implant bone. J Oral Maxillofac Surg. 2007;65:2487–2491. doi: 10.1016/j.joms.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 9.Marković A, Calasan D, Colić S, Stojčev-Stajčić L, Janjić B, Mišić T. Implant stability in posterior maxilla: bone-condensing versus bone-drilling: a clinical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:557–563. doi: 10.1016/j.tripleo.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Cehreli MC, Kökat AM, Comert A, Akkocaoğlu M, Tekdemir I, Akça K. Implant stability and bone density: assessment of correlation in fresh cadavers using conventional and osteotome implant sockets. Clin Oral Implants Res. 2009;20:1163–1169. doi: 10.1111/j.1600-0501.2009.01758.x. [DOI] [PubMed] [Google Scholar]
- 11.Padmanabhan TV, Gupta RK. Comparison of crestal bone loss and implant stability among the implants placed with conventional procedure and using osteotome technique: a clinical study. J Oral Implantol. 2010;36:475–483. doi: 10.1563/AAID-JOI-D-09-00049. [DOI] [PubMed] [Google Scholar]
- 12.Dos Santos MV, Elias CN, Cavalcanti Lima JH. The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res. 2011;13:215–223. doi: 10.1111/j.1708-8208.2009.00202.x. [DOI] [PubMed] [Google Scholar]
- 13.Tabassum A, Meijer GJ, Wolke JG, Jansen JA. Influence of surgical technique and surface roughness on the primary stability of an implant in artificial bone with different cortical thickness: a laboratory study. Clin Oral Implants Res. 2010;21:213–220. doi: 10.1111/j.1600-0501.2009.01823.x. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz Z, Raz P, Zhao G, Barak Y, Tauber M, Yao H, Boyan BD. Effect of micrometer-scale roughness of the surface of Ti6Al4V pedicle screws in vitro and in vivo. J Bone Joint Surg Am. 2008;90:2485–2498. doi: 10.2106/JBJS.G.00499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wennerberg A, Albrektsson T, Johansson C, Andersson B. Experimental study of turned and grit-blasted screw-shaped implants with special emphasis on effects of blasting material and surface topography. Biomaterials. 1996;17:15–22. doi: 10.1016/0142-9612(96)80750-2. [DOI] [PubMed] [Google Scholar]
- 16.Wennerberg A, Albrektsson T, Lausmaa J. Torque and histomorphometric evaluation of c.p. titanium screws blasted with 25- and 75-microns-sized particles of Al2O3. J Biomed Mater Res. 1996;30:251–260. doi: 10.1002/(SICI)1097-4636(199602)30:2<251::AID-JBM16>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 17.Kim YK, Kim YJ, Yun PY, Kim JW. Effects of the taper shape, dual-thread, and length on the mechanical properties of mini-implants. Angle Orthod. 2009;79:908–914. doi: 10.2319/071808-374.1. [DOI] [PubMed] [Google Scholar]
- 18.Sakoh J, Wahlmann U, Stender E, Nat R, Al-Nawas B, Wagner W. Primary stability of a conical implant and a hybrid, cylindric screw-type implant in vitro. Int J Oral Maxillofac Implants. 2006;21:560–566. [PubMed] [Google Scholar]
- 19.Wilmes B, Ottenstreuer S, Su YY, Drescher D. Impact of implant design on primary stability of orthodontic mini-implants. J Orofac Orthop. 2008;69:42–50. doi: 10.1007/s00056-008-0727-4. [DOI] [PubMed] [Google Scholar]
- 20.Kim YS, Lim YJ. Primary stability and self-tapping blades: biomechanical assessment of dental implants in medium-density bone. Clin Oral Implants Res. 2011;22:1179–1184. doi: 10.1111/j.1600-0501.2010.02089.x. [DOI] [PubMed] [Google Scholar]
- 21.Ao J, Li T, Liu Y, Ding Y, Wu G, Hu K, Kong L. Optimal design of thread height and width on an immediately loaded cylinder implant: a finite element analysis. Comput Biol Med. 2010;40:681–686. doi: 10.1016/j.compbiomed.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Chun HJ, Cheong SY, Han JH, Heo SJ, Chung JP, Rhyu IC, Choi YC, Baik HK, Ku Y, Kim MH. Evaluation of design parameters of osseointegrated dental implants using finite element analysis. J Oral Rehabil. 2002;29:565–574. doi: 10.1046/j.1365-2842.2002.00891.x. [DOI] [PubMed] [Google Scholar]
- 23.Kong L, Hu K, Li D, Song Y, Yang J, Wu Z, Liu B. Evaluation of the cylinder implant thread height and width: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2008;23:65–74. [PubMed] [Google Scholar]
- 24.Abuhussein H, Pagni G, Rebaudi A, Wang HL. The effect of thread pattern upon implant osseointegration. Clin Oral Implants Res. 2010;21:129–136. doi: 10.1111/j.1600-0501.2009.01800.x. [DOI] [PubMed] [Google Scholar]
- 25.Carr AB, Papazoglou E, Larsen PE. The relationship of Periotest values, biomaterial, and torque to failure in adult baboons. Int J Prosthodont. 1995;8:15–20. [PubMed] [Google Scholar]
- 26.Isidor F. Mobility assessment with the Periotest system in relation to histologic findings of oral implants. Int J Oral Maxillofac Implants. 1998;13:377–383. [PubMed] [Google Scholar]
- 27.Rabel A, Köhler SG, Schmidt-Westhausen AM. Clinical study on the primary stability of two dental implant systems with resonance frequency analysis. Clin Oral Investig. 2007;11:257–265. doi: 10.1007/s00784-007-0115-2. [DOI] [PubMed] [Google Scholar]
- 28.Trisi P, De Benedittis S, Perfetti G, Berardi D. Primary stability, insertion torque and bone density of cylindric implant ad modum Branemark: is there a relationship? An in vitro study. Clin Oral Implants Res. 2011;22:567–570. doi: 10.1111/j.1600-0501.2010.02036.x. [DOI] [PubMed] [Google Scholar]
- 29.Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006;17:109–114. doi: 10.1111/j.1600-0501.2005.01211.x. [DOI] [PubMed] [Google Scholar]
- 30.Wiskott HW, Nicholls JI, Belser UC. Stress fatigue: basic principles and prosthodontic implications. Int J Prosthodont. 1995;8:105–116. [PubMed] [Google Scholar]
- 31.Lee SY, Yang DJ, Yeo S, An HW, Kim SJ, Choi WM, Park KB. Effect of XPEED® on Ti implants with deep threads. Key Eng Mater. 2012;493-4:442–446. [Google Scholar]
- 32.Isidor F. Loss of osseointegration caused by occlusal load of oral implants. A clinical and radiographic study in monkeys. Clin Oral Implants Res. 1996;7:143–152. doi: 10.1034/j.1600-0501.1996.070208.x. [DOI] [PubMed] [Google Scholar]
- 33.Isidor F. Histological evaluation of peri-implant bone at implants subjected to occlusal overload or plaque accumulation. Clin Oral Implants Res. 1997;8:1–9. doi: 10.1111/j.1600-0501.1997.tb00001.x. [DOI] [PubMed] [Google Scholar]