Abstract
Objective
The current study examines the temporal relationship between changes in obsessive-compulsive symptoms and changes in depressive symptoms during exposure and response prevention (EX/RP) therapy for obsessive-compulsive disorder (OCD).
Method
Participants were 40 adults (53% female) who received EX/RP in a randomized controlled trial comparing serotonin reuptake inhibitor (SRI) augmentation strategies. Participants completed clinician-administered assessments of OCD (Yale Brown Obsessive Compulsive Scale) and depressive symptoms (Hamilton Depression Rating Scale) every four weeks from baseline to 32-week follow-up.
Results
Lagged multilevel mediational analyses indicated that change in OCD symptoms accounted for 65% of subsequent change in depressive symptoms. In contrast, change in depressive symptoms only partially mediated subsequent change in OCD symptoms, accounting for 20% of the variance in outcome.
Conclusions
These data indicate that reductions in co-morbid depressive symptoms during EX/RP for OCD are largely driven by reductions in obsessive compulsive symptoms.
Keywords: CBT, Exposure and response prevention, obsessive-compulsive disorder, depression, mediation
Obsessive Compulsive Disorder (OCD) is a debilitating condition characterized by intrusive and distressing thoughts, images, or impulses (obsessions) and repetitive mental or behavioral acts (compulsions). With a lifetime prevalence of 2.3% (Ruscio, Stein, Chiu, & Kessler, 2010) and often a chronic course, OCD is associated with poor quality of life (Koran, 2000), severe functional impairment, and high rates of co-morbidity (Ruscio et al., 2010). Major depression is one of the most common co-morbidities among patients with OCD. Epidemiological and clinical research has found lifetime rates of co-morbid depression as high as 40.7% (Ruscio et al., 2010) and 67.2% (Pinto, Mancebo, Eisen, Pagano, & Rasmussen, 2006), respectively, with the onset of OCD typically preceding the onset of depression (Millet et al., 2004). The impact of co-morbid depression on OCD treatment outcome is unclear. Some studies suggest that OCD patients with severe depression experience attenuated response to evidence-based treatments such as exposure and response prevention (EX/RP; Abramowitz, Franklin, Street, Kozak, & Foa, 2000; Abramowitz & Foa, 2000; Steketee, Chambless, & Tran, 2001), while other studies have found no relationship between depression and OCD treatment outcome (Anholt et al., 2011; Foa, Kozak, Steketee, & McCarthy, 1992).
What is clear from the literature is the positive impact of EX/RP on depressive symptoms. Numerous studies have found that EX/RP – which focuses explicitly on reduction of OCD symptoms – leads to a significant improvement in OCD as well as co-morbid depression (See for review: Abramowitz, Franklin, & Foa, 2002) without the addition of adjunctive depressive treatment (e.g., anti-depressant medication; cognitive therapy). This pattern of decreased depressive symptoms following OCD treatment is consistent with treatment outcome data from other fear-based disorders. Namely, when symptoms of the primary disorder decrease, reductions in co-morbid disorders such as depression often occur as well (e.g., Persons, Roberts, & Zalecki, 2003; Tsao, Mystkowski, Zucker & Craske, 2002; Borkovec, Abel, & Newman, 1995). Although we know less about how change in anxiety and depressive symptoms are related to each other during treatment, research suggests that changes in the fear-based disorder being targeted account for a greater proportion of changes in depressive symptoms than the reverse. For example, reduction in social anxiety symptoms was found to mediate 91% of reduction in depression, whereas depression mediated only 6% of reduction in social anxiety symptoms (Moscovitch, Hofmann, Suvak, & In-Albon, 2005). Similarly, reduction in posttraumatic stress disorder (PTSD) symptoms has been found to mediate between 64% (Aderka, Foa, Applebaum, Shafran, & Gilboa-Schechtman, 2011) and 80% (Aderka, Gillihan, McLean, & Foa, 2013) of subsequent reduction in depression, whereas changes in depression mediated only 11% (Aderka et al., 2011) and 45% (Aderka et al., 2013) of subsequent PTSD changes, respectively.
In the context of OCD research, two previous studies have examined this issue. In a trial (N = 121) comparing cognitive therapy and behavioral therapy with and without fluvoxamine (Anholt et al., 2011), changes in OCD symptoms mediated 89% of changes in depressive symptoms in the combined sample of participants. In contrast, changes in depressive symptoms accounted for only 23% of the change in OCD symptoms. The work of Anholt et al. is an important initial effort, yet as the authors note, most participants (64%) received additional pharmacological or psychological treatment in the five years following the treatment phase, which makes it difficult to attribute the mediation findings to the study interventions. In addition, Anholt et al. used a statistical approach that does not account for temporal precedence of symptom change in OCD versus depressive symptoms. In another investigation, Olatunji et al. (2013) examined whether change in obsessive beliefs mediated OCD change across behavioral and cognitive therapy using panel mediation analyses that tested obsessive beliefs, depression, and avoidance in a concurrent model (N = 62). Contrary to expectations, change in depression emerged as the only significant mediator of subsequent change in OCD symptoms. The percent of variance the depression accounted for was not reported. Unlike Anholt et al. (2011), change in OCD did not significantly predict change in depression. However, the authors did not investigate the effects of OCD symptom change on depression without the contributions of obsessive beliefs and avoidance, both features that are related to OCD symptom severity.
Additional study of this topic is warranted using advanced statistical procedures that account for the temporal precedence of OCD versus depressive symptom change across evidence-based OCD treatment. Thus, the present investigation employs time-lagged multi-level mediational analyses to examine the relationship between changes in OCD and depressive symptoms during EX/RP, the treatment of OCD that has been most extensively studied and empirically validated (Rosa-Alcázar, Sánchez-Meca, Gómez-Conesa, & Marín-Martínez, 2008; McKay et al., 2015). Elucidating the association between OCD and depressive symptoms during EX/RP is important, given the prevalence of co-morbid depression among treatment-seeking OCD patients. Moreover, conducting mediational research on processes of symptom change is an essential step toward better understanding how single-diagnostic focus treatments like EX/RP impact both targeted symptoms and co-morbidities. This knowledge will inform important clinical questions regarding whether to adapt single-diagnosis treatments to address co-morbid depression concurrently, versus focusing on the primary fear-based disorder as a means of reducing symptoms of both conditions. Based on previous findings in OCD and other fear-based disorders, we hypothesized that changes in OCD and depressive symptoms would reciprocally influence each other, with reductions in OCD having a greater impact on reductions in depression than the reverse.
Methods
Participants
Participants were 40 adults with OCD randomized to EX/RP in the context of an RCT investigating serotonin reuptake inhibitor (SRI) augmentation strategies (Simpson, Foa et al., 2013). Thus, participants had to be stabilized on an optimal dose of SRI for at least 12 weeks to enter the trial, and were continued on this medication throughout the study. Other study inclusion criteria were: (a) principal diagnosis of OCD based on the criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), and (b) moderately severe symptoms of OCD, as indicated by a score of 16 or greater on the Yale-Brown Obsessive-Compulsive Scale [Y-BOCS]. Exclusion criteria were active bipolar or psychotic disorder, substance abuse or dependence in the prior 3 months, prominent suicidal ideation, severe depression (indicated by a score of 25 or greater on the HAM-D), and unstable medical or neurological condition. Participants were also excluded if they were previously treated with an SRI in combination with either risperidone or EX/RP.
Participant age ranged from 18 to 65 (m = 34.27; SD = 12.67). Fifty-three percent of the sample were female, and 90% were Non-Hispanic white. Mean Y-BOCS score at baseline was 27.18 (SD = 3.94), corresponding to severe OCD. Mean duration of OCD at baseline was 16.18 years (SD = 11.13). Twenty-three percent of the sample (n = 9) met criteria for current depressive disorder (i.e., major depressive disorder, dysthymia, or depressive disorder NOS), and 55% endorsed history of a depressive disorder. Baseline HAM-D scores ranged from 0 (no depression) to 24 (very severe depression). Mean HAM-D score at baseline was 7.80 (SD = 6.09), corresponding to mild depression. Seventy three percent of the sample endorsed depressive symptoms in the mild or normal range; 25% endorsed symptoms in the moderate range; and one participant endorsed very severe depression.
Procedures
For a detailed description of the parent RCT, please refer to Simpson, Foa et al. (2013). Study eligibility was determined by trained clinicians who conducted an assessment of psychiatric diagnoses, treatment history, and medical history with each participant. Eligible participants were randomized to 8 weeks of either: EX/RP, risperdone, or pill placebo while remaining on a stable dose of SRI. The present sample is comprised exclusively of the 40 participants randomized to EX/RP. Responders at week 8 (defined as Y-BOCS decrease ≥ 25%) were eligible to enter the 6-month maintenance phase, while non-responders were referred for open treatment. During the maintenance phase, participants continued their SRI and the adjunctive treatment to which they were originally assigned, to assess whether participants were able to maintain improvements or show additional treatment gains. Severity of depressive and OCD symptoms were assessed by independent evaluators who were blind to condition at 4-week intervals throughout the duration of the study.
Treatment
EX/RP (Foa, Yadin, & Lichner, 2012) is an evidence-based cognitive behavioral treatment for OCD comprised of psycho-education, graded exposure to feared stimuli, and ritual prevention. During the acute phase of the study (weeks 0-8), all participants received 17, twice weekly 90-minute EX/RP sessions provided by a trained study clinician (PhD or PsyD). EX/RP treatment included 2 introductory sessions, 15 exposure sessions, daily homework, and between-session telephone check-ins. In the maintenance phase of the study (weeks 8-32), participants received up to 15 additional 90-minute EX/RP sessions as needed (m = 8; SD = 6) to achieve excellent response, defined as Y-BOCS score ≤121. Subsequently, patients received four weekly 45-minute maintenance sessions followed by biweekly 45-minute sessions until the end of the maintenance phase (m = 8; SD = 5). These sessions were implemented to maximize maintenance of treatment gains and promote relapse prevention.
Three participants dropped out during the acute phase of treatment (week 0-8), two prior to receiving exposure sessions. At week 8, 32 EX/RP patients were deemed responders. Of these, 30 entered the maintenance phase, and 26 completed it. For participants who dropped out or crossed over to open treatment (i.e., non-responders who did not enter the maintenance phase), all data points collected prior to attrition were included in the present analyses.
Measures
Yale Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al., 1989)
The Y-BOCS is a 10-item semi-structured clinician-administered interview used to assess symptom severity of obsessions and compulsions in the past week. Each item is rated on a 5-point Likert scale (0 = no symptoms, 4 = extreme). Total scores range from 0 to 40. The Y-BOCS has good internal consistency, excellent inter-rater reliability, and good test-retest reliability (Goodman et al., 1989). Internal consistency in the present sample was 0.73.
Hamilton Depression Scale (HAM-D; Hamilton, 1960)
The HAM-D is a 17-item clinician-administered interview that is widely-used for assessing severity of depressive symptoms. Eight items are scored on a 5-point scale (0 = not present; 4 = severe) and nine items are scored on a 3-point scale (0 = absent; 2 = frequent). Total scores range from 0 to 50 (0-7 = no depression; 8-16 = mild depression; 17-23 = moderate depression; >23 = severe depression). The HAM-D has excellent inter-rater reliability, good internal consistency, and high test-retest reliability (Trajkovic et al., 2011). Internal consistency in the current sample was 0.78.
Data Analyses
Analyses were conducted using SPSS, version 20. The longitudinal nature of the data formed a multilevel data structure: Level 1 data (i.e., OCD and depressive symptoms) were nested within Level 2 units (i.e., participants). This data structure is appropriate for multi-level modeling techniques (Raudenbush, 2001), which allow the number of observations to vary between participants and handles missing data effectively. Multi-level mediational analyses (MLM; Kenny, Korchmaros, & Bolger, 2003) were conducted to evaluate the relationship between OCD and depressive symptoms from baseline (week 0) to 32-week follow-up. Lagged mediation analyses were used to control for the temporal precedence of mediator versus outcome variables. Thus, we examined whether changes in the mediator variable at Time t accounted for changes in the outcome variable at Time t+1. Participants who provided only one data point (baseline) due to early drop-out were automatically excluded by SPSS (n = 2).
Two models were tested. The first one examined to what extent changes in OCD symptoms accounted for changes in depressive symptoms between baseline and week 32, with Time designated as the predictor, OCD symptoms as the mediator, and depressive symptoms as the outcome. The second test employed a reverse model to examine to what extent changes in depressive symptoms accounted for changes in OCD symptoms. In this model, Time was the predictor, depressive symptoms were the mediator, and OCD symptoms were the outcome. The RMediation package (Tofighi & MacKinnon 2011) was used to calculate the confidence interval (CI) of random indirect effects. Percent mediation was calculated as an indicator of effect size of the mediator (Kenny et al., 2003).
Time was modeled using measurement number (i.e., 1, 2, 3, 4, 5, and 6). Prior to running analyses, we compared a model with a linear time variable, a nonlinear, natural log time variable, and a quadratic time variable using Akaike's information criterion (Akaike, 1987) and the deviance statistic. Results indicated a better fit for the non-linear model across all study variables; thus, consistent with standards for mediation analyses (Kraemer et al., 2002), a log time variable was used in all analyses to bring the data in line with the linearity assumption.
Results
Multilevel Mediational Analyses
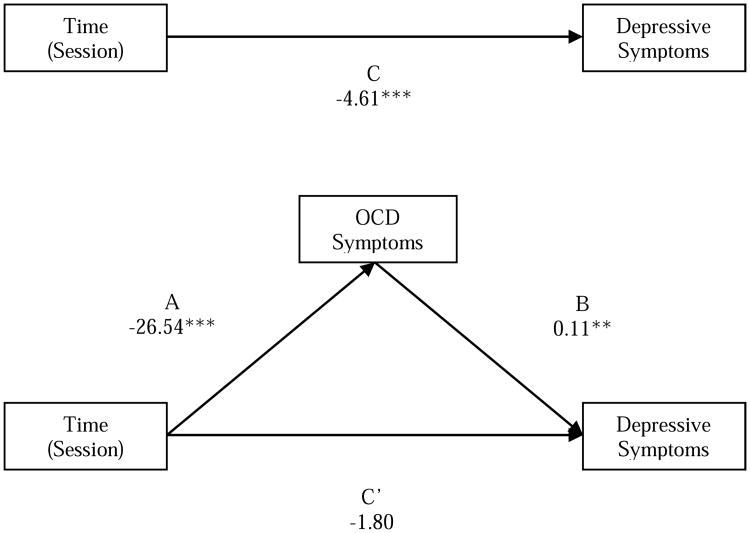
First, we regressed depressive symptoms on Time (Path C in Figure 1 and Table 1). Results indicated that depressive symptoms significantly decreased between baseline and follow-up (t=-4.11, p<.001). We then regressed OCD symptoms on Time (Path A in Figure 1 and Table 1). OCD symptoms also significantly decreased from baseline to follow-up (t=-14.56, p<.001).
Figure 1. Mediational model testing the impact of change in OCD on change in depression.
Note. Coefficients represent unstandardized regression coefficients. Paths indicate Level 1 re gression analysis. **p<.01; ***p<.001.
Table 1. Summary Of Multilevel Regression Analyses for the Mediational Model.
| Step | Path | Predictor variable | Outcome variable | b | SE b | t | p |
|---|---|---|---|---|---|---|---|
| 1 | C | Time | Depression | -4.61 | 1.12 | -4.11 | <.001 |
| 2 | A | Time | OCD symptoms | -26.54 | 1.82 | -14.56 | <.001 |
| 3 | B | OCD symptoms | Depression | 0.11 | 0.04 | 2.63 | <.01 |
| C′ | Time | Depression | -1.80 | 1.54 | -1.17 | 1.24 |
Note. Paths indicate Level 1 regression analysis.
Next, we regressed depressive symptoms on Time and OCD symptoms simultaneously. The effect of OCD symptoms (Path B in Figure 1 and Table 1) was significant, indicating that reductions in OCD symptoms significantly predicted subsequent reductions in depressive symptoms. The effect of Time (Path C in Figure 1 and Table 1) was non-significant, indicating that Time did not have an additional effect on depressive symptoms beyond the effect accounted for by OCD symptoms. Thus, change in OCD symptoms fully mediated the relationship between Time and change in depressive symptoms. As depicted in Figure 1 and Table 1, the original pathway between Time and depressive symptoms (Path C) was reduced from -4.61 to -1.80 when OCD symptoms were entered (Path C′). The confidence intervals for the indirect effect did not include zero, 95% CI [-5.33 to -0.79], providing clear evidence for multilevel mediation. OCD symptoms accounted for 64.8% of the total effect of time on depressive symptoms.2
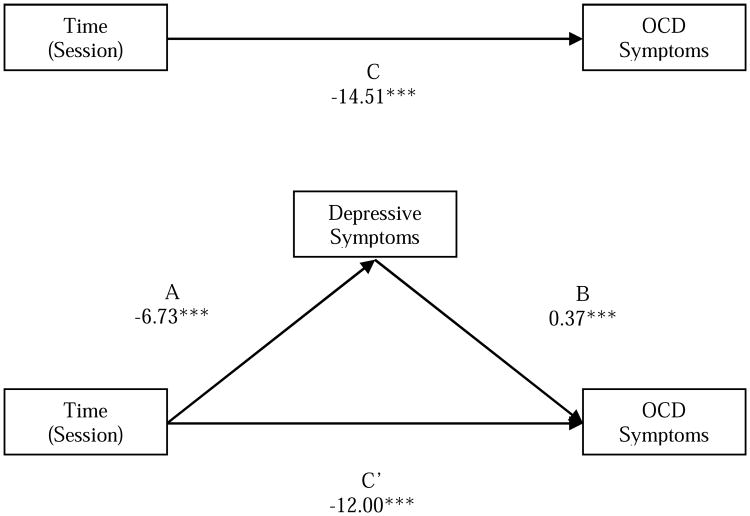
Results for the reverse model are presented in Table 2 and Figure 2. In the second model, the effect of Time on OCD symptoms (Path C′) remained significant after OCD symptoms were regressed on Time and depressive symptoms simultaneously. Thus, change in depressive symptoms partially mediated the relationship between Time and change in OCD symptoms. We found evidence for multilevel mediation, 95% CI [-4.68, -0.90], with depressive symptoms accounting for 19.6% of the total effect of time on OCD symptoms.
Table 2. Summary of Multilevel Regression Analysis for the Reverse Mediation Model.
| Step | Path | Predictor variable | Outcome variable | b | SE b | t | p |
|---|---|---|---|---|---|---|---|
| 1 | C | Time | OCD symptoms | -14.51 | 1.83 | -7.91 | <.001 |
| 2 | A | Time | Depression | -6.73 | 1.24 | -5.44 | <.001 |
| 3 | B | Depression | OCD symptoms | 0.37 | 0.1 | 3.91 | <.001 |
| C′ | Time | OCD symptoms | -12.00 | 1.89 | -6.34 | <.001 |
Note. Paths indicate Level 1 regression analysis.
Figure 2.
Reverse mediational model testing the impact of change in depression on change in OCD.
Note. Coefficients represent unstandardized regression coefficients. Paths indicate Level 1 regression analysis. ***p<.001
Discussion
The present study examined the relationship between reduction in OCD and depressive symptoms among adult OCD patients receiving SRI augmentation with exposure and response prevention (EX/RP). As hypothesized, changes in OCD and depressive symptoms reciprocally influenced one another, with reductions in OCD having a greater impact on reductions in depression than the reverse. Specifically, change in OCD symptoms fully mediated the effect of treatment on depressive symptoms, accounting for approximately 65% of subsequent change in depressive symptoms in this sample. In contrast, change in depressive symptoms partially mediated the effect of treatment on OCD symptoms, accounting for approximately 20% of subsequent change in OCD symptoms. Consistent with prior studies of OCD (Anholt et al., 2011), PTSD (Aderka et al., 2011; 2013), and social anxiety disorder (Moscovitch et al., 2005), the current results suggest that reductions in depressive symptoms are largely driven by reductions in symptoms of the principle disorder being targeted in treatment. This has important clinical implications, suggesting that for individuals who present with a primary fear-based disorder and mild-to-moderate secondary depressive symptoms, treatment that is effective in addressing the primary disorder will also reduce depressive symptoms without the explicit use of additional therapeutic interventions.
The present study replicates and extends the findings of Anholt et al. (2011), who found that change in OCD symptoms during both cognitive and behavioral treatment fully mediated (89%) change in depressive symptoms, while change in depressive symptoms partially mediated (23%) change in OCD symptoms. The current study produced comparable results employing a more rigorous statistical approach that accounts for the temporal precedence of OCD versus depressive symptom change over time. In addition, the present study focuses on the acute and maintenance phase of a controlled OCD treatment study in which all participants were kept on a stable dose of SRI treatment and received maintenance EX/RP sessions throughout the 32-week follow-up. This allows for a clearer understanding of the relationship between the treatment employed and the observed symptom reduction. Our findings indicate that EX/RP reduces OCD symptoms, and that reduction in OCD symptoms is responsible for the majority of subsequent change in depressed mood.
Several explanations can be put forward to account for the interplay between OCD and depressive symptoms demonstrated here and in Anholt et al. (2011). For example, reduction in OCD symptoms during treatment may improve depressed mood by enhancing self-efficacy and mastery (Bandura, 1977). Alternatively, reduction of OCD symptoms and related avoidance may reduce depression by eliminating barriers to pleasurable social and occupational activities (Loas, 1996). Thus, as OCD symptoms remit, improvements in functioning may facilitate changes in depression. Finally, as suggested by Aderka et al. (2013), reductions in anxiety symptoms may impact depressed mood by decreasing feelings of hopelessness or demoralization associated with having an anxiety disorder (helplessness-hopelessness theory; Alloy, Kelly, Mineka, & Clements, 1990). This may be particularly relevant for patients for whom OCD preceded the onset of depression. Indeed, research suggests that OCD patients typically suffer impairment for years before seeking treatment (see for review see Garcia-Soriano, Rufer, Delsignore, & Weidt, 2014) and many have failed alternative therapy modes prior to receiving EX/RP (Levy, Mclean, Yadin, & Foa, 2013). While the role of hopelessness was not assessed here, this would present a fruitful area for future study.
We found that improvement in depressive symptoms partially mediated subsequent improvement in OCD. Both Anholt et al. (2011) and Olatunji et al. (2013) also found partial or full mediation effects, respectively, in this direction. There are several possible explanations for this finding. It may be that as depressive symptoms decrease, mood and energy improvements allow patients to engage treatment in a manner that stimulates further OCD symptom improvement; for example, facilitating increased homework adherence, which is known to predict positive OCD outcomes (Simpson et al., 2011). Thus, treatment engagement or adherence may account for the relationship between change in depression and OCD observed here. Given that OCD symptoms can fluctuate with general distress levels, it may also be that reduction of depressive symptoms, for some patients, may be associated with fewer obsessions and compulsions. Additional research is needed to clarify the processes by which change in one symptom dimension produces change in the other.
Several study limitations should be noted. First, while sufficient for multi-level mediational analyses, the current sample size was relatively small (n = 40). Second, all participants were on a therapeutic dose of an SRI, and severe depression was an exclusion criteria for the study. On average, severity of co-morbid depressive symptoms was in the mild or moderate range. Thus, our findings are meaningful to similar samples, in which OCD is the primary disorder and co-morbid depressive symptoms are not severe. Future research is recommended in larger samples characterized by more severe depression. Third, to ensure non-responders to EX/RP received effective treatment, 8 patients did not enter the maintenance phase and were referred for alternative treatment. As such, these participants only provided data between baseline and week 8. While multi-level modeling is equipped to handle this missing data, it is possible that the pattern of findings would differ if the sample included maintenance data on EX/RP non-responders. Finally, the EX/RP treatment offered in this trial was provided in twice-weekly format for up to 32 sessions and followed the treatment protocol adherently, including 90-minute appointments and between session phone check-ins. As such, the generalizability of the results to less intensive treatment schedules (e.g., once weekly) and non-research settings requires additional study.
Despite these limitations, this study is the first to employ lagged multi-level mediational analyses with the specific aim of examining the interplay between OCD and depressive symptoms during EX/RP. The current findings support a reciprocal relationship between OCD and depressive symptoms for individuals with primary OCD and co-morbid depression, with change in OCD symptoms largely responsible for subsequent change in depressive symptoms.
Highlights.
This study examined change in OCD and co-morbid depression during EX/RP
Lagged multilevel mediational analyses were employed
Change in OCD symptoms accounted for 65% of subsequent change in depression
Change in depression accounted for 20% of subsequent change in OCD symptoms
Findings suggest change in co-morbid depression is largely driven by change in OCD
Acknowledgments
Funding/Support: This study was funded by National Institute of Mental Health grants R01 MH45404 (Dr Foa) and R01 MH045436 (Dr Simpson). Medication was provided at no cost by Janssen Scientific Affairs LLC.
Role of the Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Y-BOCS ≤12 is generally considered mild OCD, not requiring clinical intervention, and is the score range most predictive of symptoms remission, good quality of life, and high levels of adaptive functioning (Farris, McLean, Van Meter, Simpson, & Foa, 2013).
The total effect is the sum of the direct effect (C), the indirect effect (AB), and the covariance between A and B (Kenny et al., 2003). Thus, % mediation was calculated as: 100 × {[C′ + AB + Cov (AB)]-C′ } / [C′ + AB + Cov (AB)], or 100 × (total effect - direct effect)/ (total effect). The covariance between the ordinary-least-squares estimates for Paths A and B was -0.40 for the mediational model and -0.43 for the reverse model.
Conflict of Interest Disclosures: Dr. Simpson has received research funds from Janssen Pharmaceuticals (2006-2012), Transcept Pharmaceuticals (2011-2013), and Neuropharm, Ltd (2009), served on a Scientific Advisory Board for Pfizer (for Lyrica, 2009-2010) and Jazz Pharmaceuticals (for Luvox CR, 2007-2008), consulted for Quintiles, Inc (on therapeutic needs for OCD, September, 2012), and receives royalties from Cambridge University Press and UpToDate, Inc. Dr Foa was a consultant to Jazz Pharmaceuticals (for Acetelion), and she receives royalties from Bantam and Oxford University Press for book sales, including a manual of cognitive-behavioral therapy for OCD. Drs. McLean, Zandberg, and Zang, and Miss Yeh have no conflicts to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramowitz JS, Franklin ME, Foa EB. Empirical status of cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analytic review. Romanian Journal of Cognitive & Behavioral Psychotherapies. 2002;2:89–104. [Google Scholar]
- Abramowitz JS, Foa EB. Does major depressive disorder influence outcome of exposure and response prevention for OCD? Behavior Therapy. 2000;31:795–800. [Google Scholar]
- Abramowitz JS, Franklin ME, Street GP, Kozak MJ, Foa EB. Effects of comorbid depression on response to treatment for obsessive-compulsive disorder. Behavior Therapy. 2000;31:517–528. [Google Scholar]
- Aderka IM, Foa EB, Applebaum E, Shafran N, Gilboa-Schechtman E. Direction of influence between posttraumatic and depressive symptoms during prolonged exposure therapy among children and adolescents. Journal of Consulting and Clinical Psychology. 2011;79:421–425. doi: 10.1037/a0023318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aderka IM, Gillihan SJ, McLean CP, Foa EB. The relationship between posttraumatic and depressive symptoms during prolonged exposure with and without cognitive restructuring for the treatment of posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2013;81:375–382. doi: 10.1037/a0031523. [DOI] [PubMed] [Google Scholar]
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th., text rev. Washington, DC: Author; 2000. [Google Scholar]
- Anholt GE, Aderka IM, van Balkom A, Smit JH, Hermesh H, de Haan E, van Oppen P. The impact of depression on the treatment of obsessive-compulsive disorder: Results from a 5-year follow-up. Journal of Affective Disorders. 2011;135:201–207. doi: 10.1016/j.jad.2011.07.018. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Abel JL, Newman H. Effects of psychotherapy on comorbid conditions in generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1995;63:479–483. doi: 10.1037//0022-006x.63.3.479. [DOI] [PubMed] [Google Scholar]
- Farris SG, McLean CP, Van Meter PE, Simpson HB, Foa EB. Treatment response, symptom remission, and wellness in obsessive-compulsive disorder. Journal of Clinical Psychiatry. 2013;74:685–90. doi: 10.4088/JCP.12m07789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Kozak MJ, Steketee GS, McCarthy PR. Treatment of depressive and obsessive-compulsive symptoms in OCD by imipramine and behavior therapy. British Journal of Clinical Psychology. 1992;31:279–292. doi: 10.1111/j.2044-8260.1992.tb00995.x. [DOI] [PubMed] [Google Scholar]
- Foa EB, Simpson HB, Liebowitz MR, Powers MB, Rosenfield D, Cahill SP, et al. Williams MT. Six-month follow-up of a randomized controlled trial augmenting serotonin reuptake inhibitor treatment with exposure and ritual prevention for obsessive-compulsive disorder. Journal of Clinical Psychiatry. 2013;74(5):464–469. doi: 10.4088/JCP.12m08017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Yadin E, Lichner TK. Exposure and Response (Ritual) Prevention for Obsessive-Compulsive Disorder. 2nd. New York, NY: Oxford University Press; 2012. [Google Scholar]
- Garcia-Soriano G, Rufer M, Delsignore A, Weidt S. Factors associated with non-treatment or delayed treatment seeking in OCD sufferers: A review of the literature. Psychiatry Research. 2014;220:1–10. doi: 10.1016/j.psychres.2014.07.009. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS. The Yale-Brown Obsessive Compulsive scale: II. Validity. Archives of General Psychiatry. 1989;46:1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, Korchmaros JD, Bolger N. Lower level mediation in multilevel models. Psychological Methods. 2003;8:115–128. doi: 10.1037/1082-989x.8.2.115. [DOI] [PubMed] [Google Scholar]
- Koran LM. Quality of life in obsessive-compulsive disorder. Psychiatric Clinics of North America. 2000;23:509–517. doi: 10.1016/s0193-953x(05)70177-5. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT. Mediators and Moderators of Treatment Effects in Randomized Clinical Trials. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Levy H, Mclean C, Yadin E, Foa EB. Characteristics of individuals seeking treatment for obsessive-compulsive disorder. Behavior Therapy. 2013;44:408–416. doi: 10.1016/j.beth.2013.03.007. [DOI] [PubMed] [Google Scholar]
- McKay D, Sookman D, Neziroglu F, Wilhelm S, Stein DJ, Kyrios M, et al. Veale D. Efficacy of cognitive-behavioral therapy for obsessive-compulsive disorder. Psychiatry Research. 2015;225:236–246. doi: 10.1016/j.psychres.2014.11.058. [DOI] [PubMed] [Google Scholar]
- Moscovitch DA, Hofmann SG, Suvak MK, In-Albon T. Mediation of changes in anxiety and depression during treatment of social phobia. Journal of Consulting and Clinical Psychology. 2005;73:945–952. doi: 10.1037/0022-006X.73.5.945. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Rosenfield D, Tart CD, Cottraux J, Powers MB, Smits JA. Behavioral versus cognitive treatment of obsessive-compulsive disorder: An examination of outcome and mediators of change. Journal of Consulting and Clinical Psychology. 2013;81:415–428. doi: 10.1037/a0031865. [DOI] [PubMed] [Google Scholar]
- Persons JB, Roberts NA, Zalecki CA. Anxiety and depression change together during treatment. Behavior Therapy. 2003;34:149–163. [Google Scholar]
- Pinto A, Mancebo MC, Eisen JL, Pagano ME, Rasmussen SA. The Brown Longitudinal Obsessive Compulsive Study: Clinical features and symptoms of the sample at intake. Journal of Clinical Psychiatry. 2006;67:703–711. doi: 10.4088/jcp.v67n0503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa-Alcázar AI, Sánchez-Meca J, Gómez-Conesa A, Marín-Martínez F. Psychological treatment of obsessive–compulsive disorder: a meta-analysis. Clinical Psychology Review. 2008;28:1310–1325. doi: 10.1016/j.cpr.2008.07.001. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15:53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Simpson HB, Maher MJ, Wang Y, Bao Y, Foa EB, Franklin M. Patient adherence predicts outcome from cognitive behavioral therapy in obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2011;79:247–252. doi: 10.1037/a0022659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson HB, Foa EB, Liebowitz MR, Huppert JD, Cahill S, Maher MJ, et al. Campeas R. Cognitive-behavioral therapy vs. risperidone for augmenting serotonin reuptake inhibitors in obsessive-compulsive disorder: A randomized clinical trial. JAMA Psychiatry. 2013;70:1190–1198. doi: 10.1001/jamapsychiatry.2013.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steketee G, Chambless DL, Tran GQ. Effects of axis I and II comorbidity on behavior therapy outcome for obsessive-compulsive disorder and agoraphobia. Comprehensive Psychiatry. 2001;42:76–86. doi: 10.1053/comp.2001.19746. [DOI] [PubMed] [Google Scholar]
- Togighi D, Mackinnon DP. RMediation: An R package for mediation analysis confidence. Behavior Research Methods. 2012;43(3):692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trajkovic G, Starcevic V, Latas M, Lestarevic M, Ille T, Bukumiric Z, Marinkovic J. Reliability of the Hamilton Rating Scale for Depression: A meta-analysis over a period of 49 years. Psychiatry Research. 2011;189:1–9. doi: 10.1016/j.psychres.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Tsao JCI, Mystkowski JL, Zucker BG, Craske MG. Effects of cognitive-behavioral therapy for panic disorder on comorbid conditions: Replication and extension. Behavior Therapy. 2002;33:493–509. [Google Scholar]