Abstract
Rationale, aims and objectives
Obesity is significantly underdiagnosed and undertreated in primary care settings. The purpose of this clinical practice change project was to increase provider adherence to national clinical practice guidelines for the diagnosis and treatment of obesity in adults.
Methods
Based upon the National Institutes of Health guidelines for the diagnosis and treatment of obesity, a clinical change project was implemented. Guided by the theory of planned behaviour, the Provider and Healthcare team Adherence to Treatment Guidelines (PHAT-G) intervention includes education sessions, additional provider resources for patient education, a provider reminder system and provider feedback.
Results
Primary care providers did not significantly increase on documentation of diagnosis and planned management of obesity for patients with body mass index (BMI) greater than or equal to 30. Medical assistants increased recording of height, weight and BMI in the patient record by 13%, which was significant.
Conclusions
Documentation of accurate BMI should lead to diagnosis of appropriate weight category and subsequent care planning. Future studies will examine barriers to adherence to clinical practice guidelines for obesity. Interventions are needed that include inter-professional team members and may be more successful if delivered separately from routine primary care visits.
Keywords: adult obesity, clinical practice guidelines, practice change, provider adherence
Introduction
Obesity is a major contributor to the development of multiple chronic conditions (MCCs) such as coronary heart disease (CHD) [1,2], stroke [2], diabetes [1,2], hypertension [2], hyperlipidaemia [1], musculoskeletal disorders [2], certain cancers [2], depression [3] and disability [4]. In the past three decades, worldwide obesity has almost doubled [5]. The estimated global indirect costs related to obesity are between $448.29 million and $65.67 billion [6]. As of 2012, 35.8% of the US population was overweight, with 27.6% as obese [7]. Not only does obesity contribute to complications of other MCC, obesity itself carries increased risk for mortality [8].
Historically, the health care system has prioritized chronic conditions that result from obesity, but did not focus on obesity to the same extent. Furthermore, in the United States, health insurance payers have not uniformly listed obesity counselling or treatment as a reimbursable condition [9]. However, in June 2013, the American Medical Association declared obesity to be a disease state with its own unique physiological factors. Recognition of obesity as a disease has the potential to change the health care system because it will likely lead to reimbursement for obesity interventions [10] and may help focus health care provider attention on strategies to manage the obesity epidemic. Although clinical recommendations for health care providers to address obesity are widely available [11,12], primary care providers significantly underdiagnose and undertreat excess weight [13–15].
Both patient and provider factors have been identified as barriers to management of obesity [16,17]. Patient barriers have been identified as blame from providers, lack of desire for provider assistance with weight loss [18], lack of awareness of the chronicity of obesity, socio-economic status, time constraints, lack of social support, co-morbidities, medications and substance abuse [19]. Provider barriers include lack of provider confidence in obesity management, concerns about treatment efficacy, frustration with prior attempts, negative attitudes towards obese patients [20], and perceptions that patients lack time for exercise and self-control to avoid unhealthy foods [18]. A lack of utilization of objective screening tools contributes to decreased management of obesity and increased negative health outcomes in overweight and obese individuals [13, 16].
Body mass index (BMI) is the current standard to quantify overweight and obesity status. The National Institutes of Health (NIH) clinical guidelines on the diagnosis and treatment of obesity define overweight as a BMI greater than or equal to 25, and obesity as a BMI greater than or equal to 30 [11]. Appropriate management of patients who are overweight or obese could significantly diminish the downstream consequences of obesity. In addition, documentation of obesity diagnosis positively correlates with documentation of a treatment plan for obesity [13]. An effective treatment plan is essential. The recommended treatment plan for individuals with obesity is a combination of diet modification, increased physical activity and behaviour therapy [11]. Treatment plans that lead to even a loss of 5–10% of current weight have been linked to significant reductions in adverse health outcomes [21].
The purpose of this study was to evaluate the impact of the Provider and Healthcare team Adherence to Treatment Guidelines (PHAT-G) intervention on adherence to current obesity clinical practice guidelines in an academic primary care centre. This longitudinal practice-based evaluation project had three phases: firstly, assessment of baseline provider adherence to clinical practice guideline for obesity [11]; secondly, implementation of the PHAT-G intervention in the clinical setting; and thirdly, evaluation of provider adherence to guideline recommendations for the diagnosis of obesity and treatment of overweight and obesity. This project had three outcome aims:
to increase documentation of BMI;
to increase frequency of diagnosis of obesity if documented BMI was greater than or equal to 30; and
to increase documentation of a weight loss plan consistent with clinical practice guideline recommendations for patients with excess weight.
Theoretical framework
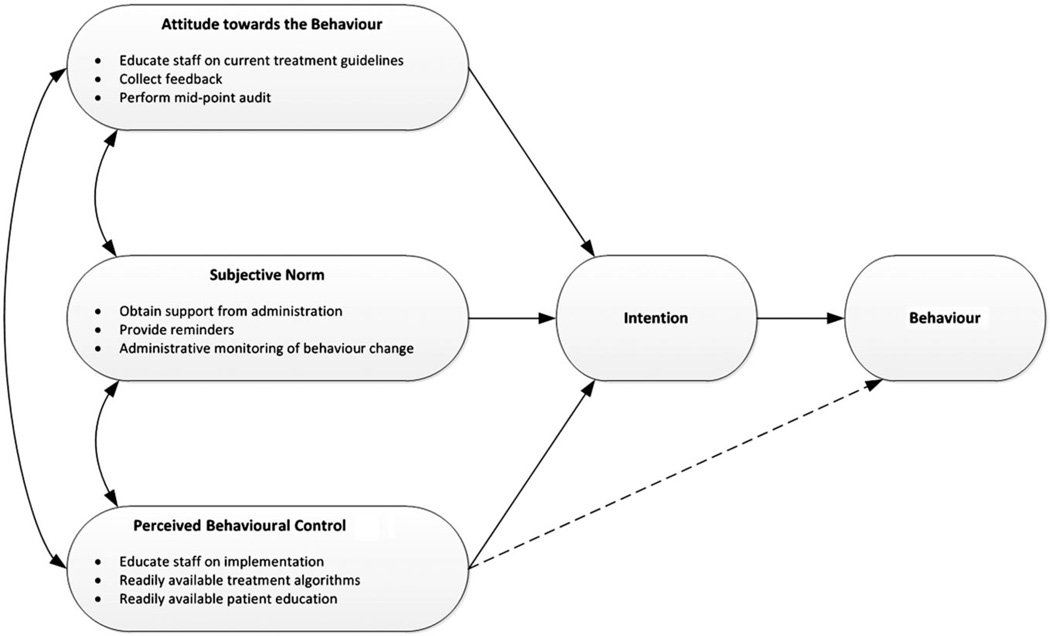
The theory of planned behaviour (TPB) provided the theoretical foundation for the development of the PHAT-G intervention. The TPB is found elsewhere in the literature as a framework in studies investigating behaviour change of nurses, doctors and other health care providers [22–24]. According to the TPB, intention is the most significant determinant of behaviour. Attitude, social norm and perceived behavioural control each influences intention [25]. The design and activities of the project were rooted in the TPB and address each of the influencing factors of intention to perform behaviour (see Fig. 1).
Figure 1.
Theory of planned behaviour: a framework for the PHAT-G intervention.
Methods
A three-phase evaluation project was implemented to meet the aims. The project was evaluated using baseline assessment data and post-implementation data found in the health record. The project received a letter of exemption from the West Virginia University Institutional Review Board.
Setting
PHAT-G was implemented in a primary care centre operated by the School of Medicine at a large state university in West Virginia, located approximately 75 miles from an urban area. At the time of the project, the centre was staffed by doctors, a doctor’s assistant, nurse practitioners, medical residents, registered nurses, licensed practical nurses and medical assistants, all of whom provided patient care as part of the health care team. Currently, 33.8% of the population of West Virginia is obese [7]. At the time of the project, nearly one-third of the West Virginia state population was obese [26]. The clinic has over 24 000 completed patient visits annually and cares for approximately 130 patients on a given day. In the 12-month period prior to this project, less than 1% of the health records included documentation of obesity as one of the first three documented diagnoses for patient encounters. In this clinic, only the first three diagnoses for each encounter were reportable, so it is possible that obesity was a diagnosis for more than 1% of the clinic population. However, the fact that so few encounters included obesity as a top-three diagnosis indicates the lack of priority for this health issue.
Study sampling
The collection of phase 1 assessment data, and phase 3 evaluation data, was accomplished by examining the health records of adult patients aged 18–64 who attended visits at the academic health centre. Sample size was determined by the Joint Commission requirement of a sample size of 70 cases when the population is greater than 500 [27]. At both data collection time points, oversampling occurred for a total sample of 100 medical records. The records were selected randomly using a random number chart and drawn from the total population of arrived patients for the designated data collection day. Phase 1 data collection occurred 6 months prior to the intervention, and phase 3 data collection occurred 6 weeks after the last day of implementation.
Project variables
The variables were selected based upon the Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults [11], the NIH clinical guideline on overweight and obesity.
Documentation of BMI
Documentation of BMI was collected as a categorical variable with potential categories of yes and no. If documented, BMI was calculated using a BMI wheel or online calculator after clinic staff had measured height and weight. Staff recorded height, weight and BMI in the health record.
BMI
BMI was collected as a number recorded in the health record within the past 12 months. If this number was unavailable in the record, it was calculated by study staff using recorded height and weight. BMI is calculated using body weight in kilograms divided by the height in meters squared.
Waist circumference
Waist circumference was collected as a continuous numerical variable as documented in the health record.
Obesity diagnosis
Obesity diagnosis was collected as a categorical variable, with potential categories of yes or no.
Co-morbidities
Diagnoses of hypertension, diabetes, dyslipidaemia, depression, osteoarthritis, CHD, stroke and sleep apnoea were coded categorically as yes or no if they appeared in the diagnosis list.
Blood pressure
Blood pressure was collected as diastolic and systolic and coded as separate continuous numerical variables.
Tobacco use
Tobacco use was collected as a categorical variable with potential categories of yes or no.
Family history of premature CHD
Family history of premature CHD was collected as a categorical variable with potential categories of yes or no.
Fasting glucose, low-density lipoprotein (LDL) and high-density lipoprotein (HDL)
Fasting glucose, LDL and HDL were collected as continuous numerical variables as recorded in the health record.
Documented weight loss plan
Documented weight loss plan was collected as a categorical variable with potential categories of yes or no.
Specified weight loss planning
Readiness to change assessment, weight loss goals, reduced calorie intake, increased physical activity, referral to behaviour therapy, referral to nutritionist, use of pharmacotherapy, referral to bariatric surgery and documented other weight loss strategy were all assessed categorically as yes or no.
Description of study phases
Phase 1: baseline assessment
A retrospective chart review was conducted of 100 records selected from a usual clinic day 6 months prior to the implementation. All baseline data for phase 1 were collected from these records.
Phase 2: PHAT-G implementation
Education
The intervention included education for both clinical support staff and primary care providers. The clinical support staff participated in a training session on the measurement, calculation and documentation of BMI. This training occurred with the support of the nurse manager and aimed to standardize the procedure for height and weight measurement, as well as calculation and documentation of BMI in the patient record. The educational component of phase 2 for providers was designed to target previously identified barriers to obesity management. Barriers and lack of knowledge related to treatment efficacy were addressed during the provider education session. Providers were given the opportunity to discuss their frustration with previous attempts to manage obesity during the question and answer time following the education session. During the education sessions, it was communicated to both staff and providers that documentation of their assessment of BMI, appropriate diagnoses of obesity and any relevant treatment plan based upon the clinical practice guideline recommendations would be assessed as part of the project.
Reminder system
A reminder system was another major element of phase 2 of the project. A BMI chart was hung above each scale as a visual reminder for the nursing staff to measure, calculate and document BMI. Charts to calculate BMI were also available in the waiting room, nurses’ stations and patient care rooms to increase the visual reminder effect on behaviour. One of the tools available in The Practical Guide [28] is A Quick Reference Tool to ACT [29], a treatment algorithm based upon the clinical practice guideline recommendations. This treatment algorithm was displayed in patient care rooms as a reminder and a resource to both clinical staff and providers. Once every week, the project director communicated with the clinical staff and providers regarding the project objectives. This reminder communication occurred through a card in their clinic mailbox. Audit and feedback results were communicated as part of the reminders via email at the mid-point of the 6-week implementation phase.
Additional provided resources
In an effort to minimize concerns regarding lack of time, providers were given access to a packet of patient education materials from The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults [28]. Providers were given the one-page Your Weight and Health Profile [30] form recommended by the NIH for implementation of the clinical practice guideline to enhance their ability to quickly assess readiness to lose weight. The tool was made available in each examination room.
Phase 3: evaluation
Six weeks after the implementation of the PHAT-G intervention, post-intervention data were collected for all variables. Table 1 provides a summary of the three phases.
Table 1.
Key elements of each project phase
| Pre-intervention phase | Intervention phase | Post-intervention phase |
Project planning
|
Education
|
Evaluation
|
Reminder system
| ||
Additional available resources
|
BMI, body mass index.
Data Analysis
Version 21.0 of SPSS (IBM, Armonk, NY, USA) was used for all data analyses and the level of significance was determined as P < 0.05. After exploring the data for missing data, impossible values or outliers, descriptive and comparative data analyses were completed. Comparative analyses included the proportion of charts with a documented BMI and appropriate obesity diagnosis, and appropriate weight loss treatment plan was compared between the pre-implementation and post-implementation data.
Results
There was no difference in the co-morbid diseases, calculated BMI, systolic blood pressure, diastolic blood pressure, fasting glucose or HDL levels between the randomly selected health records at time 1 and time 2 (see Tables 2 and 3). There was no routine documentation of BMI prior to the PHAT-G intervention. From time 1 (phase 1) to time 2 (phase 3), overall BMI documentation increased by 13%, which was significant (P < 0.01). At time 1, no chart in the sample had a documented BMI, but the authors were able to calculate BMI for 21 of the charts. Of those 21, 5 (23.8%) had a BMI 25–29.9 and 8 (38%) had a BMI >30 (obese). Only 2 of the 21 (<1%) charts that met the criteria for obesity diagnosis (BMI >30) also had a documented diagnosis of obesity. However, at time 1, there were a total of 12 charts (12%) with a documented diagnosis of obesity, despite no documented BMIs. At time 2, 13% of the charts had a BMI documented. Of the documented BMIs at time 2, all met the diagnostic criteria for either overweight or obesity. The authors were able to calculate BMI for an additional 26 charts. The additional calculated BMIs fell into the following classifications: 1 was underweight, 3 were normal weight, 7 were overweight and 15 were obese. At time 2, only seven charts had documented obesity diagnosis, three of those without a documented BMI. The number of charts with a BMI of 30 or higher and a documented diagnosis of obesity did increase from 2 to 4, which is an improvement but not significant. Documentation rate of weight loss plan increased from 2 to 6 from time 1 to time 2, and this was not a statistically significant change.
Table 2.
χ2 comparison of co-morbidities between phase 1 and phase 3
| Descriptor | Phase 1 sample (n = 100) (%) |
Phase 3 sample (n = 100) (%) |
χ2 | Significance |
| Hypertension | 42 | 38 | 0.33 | 0.67 |
| Diabetes | 21 | 18 | 0.29 | 0.72 |
| Dyslipidaemia | 27 | 35 | 1.50 | 0.28 |
| Mood disorder | 22 | 14 | 2.17 | 0.20 |
| Osteoarthritis | 12 | 9 | 0.48 | 0.64 |
| CHD | 5 | 12 | 3.15 | 0.13 |
| Stroke | 1 | 1 | 0.00 | 1.00 |
| Sleep apnoea | 2 | 1 | 0.34 | 1.00 |
CHD, coronary heart disease.
Table 3.
Comparison of biomarkers between phase 1 and phase 3
| Biomarkers | Phase 1 mean | Phase 3 mean | t | Significance |
| BMI | 30.23 | 32.50 | −1.07 | 0.53 |
| Systolic BP | 131.55 | 131.20 | 0.14 | 0.70 |
| Diastolic BP | 79.33 | 79.84 | −0.31 | 0.19 |
| Fasting glucose | 102.04 | 113.38 | −1.66 | 0.92 |
| HDL | 40.59 | 45.07 | −1.75 | 0.62 |
Note. Equal variances assumed.
BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein.
Discussion
This project had several limitations. One of the limitations is that this project was conducted at a single site and therefore may not be applicable in other primary care practices. Additionally, the population served at this clinic is predominantly Caucasian, which also may limit the generalizability of the results. The cross-sectional sample of this project does not allow for causal relationship to be established. Another limitation is the lack of a control group. As there is an established standard of care related to obesity, it would have been unethical to attempt to improve the care of only some of the patients with obesity. It is possible that factors outside the intervention influenced the results of this project. Lastly, although the minimum standard for the sample size was 70 and we oversampled to 100 at each time, a larger sample size may have allowed more robust statistical analysis, including effect size.
Although PHAT-G was theoretically derived to change provider behaviour, improvements were minimal and mainly occurred with non-licensed personnel. Nelson et al. [31] suggested focusing resources on changing the social norms or increasing perceived control of behaviour rather than on increasing knowledge to achieve changes in medical assistant and licensed practical nurse behaviours. Provider behaviours may be independent of knowledge or attitudes towards evidence-based practice and may be more likely to change due to institutional policy [32]. Future studies that incorporate policy changes and the effect on provider behaviour related to obesity management are warranted.
Provider barriers have been identified in the literature [18,20]. The known provider barriers to obesity management were addressed during the educational session and through the additional resources available in the clinic during the project. As steps were taken to overcome the known barriers, additional qualitative studies related to the appropriate interventions to overcome known barriers, in addition to identifying other provider barriers to appropriate assessment, diagnosis and management of overweight and obesity, may be needed. Future studies that evaluate the process of care for patients with obesity may identify effective interventions that overcome barriers and improve quality of care.
The clinical change project highlighted the importance of the interdisciplinary team in the care of persons with excess weight. Each role in the interdisciplinary team has responsibilities that other members of the team rely on. The results of this study may indicate that primary care providers will need to fully utilize other members of the health care team to successfully care for patients with obesity. National and international bodies call for the improved functioning of inter-professional teams in health care [28]. The PHAT-G intervention incorporated multiple health care disciplines and further supports the call for utilization of inter-professional teams to implement the national guidelines for the care of patients with obesity [33].
Creating a clinical culture that routinely includes a proactive approach to the diagnosis and treatment of obesity based upon current clinical guidelines will require significant leadership. The PHAT-G project was implemented by a part-time project director and this may have limited the potential success of the project. The part-time schedule limited opportunities for communication, particularly face-to-face reminders. Although there is a paucity of research that looks at time as a factor in leadership, the general understanding is that the relationship between leaders and followers develops over time [34]. Future projects could be designed to include a full-time on-site project director. The daily physical presence of a project director could increase communication about current guidelines for obesity, serve as a reminder to staff and providers that obesity is a clinic priority, and promote the adoption of new behaviours that are consistent with a focus on obesity as a health priority.
Implementation of this clinical change project brought attention to an important health issue that contributes to multiple chronic conditions that are costly to the health care system [35]. Rather than looking to health care providers to manage obesity, it may be more cost-effective to refer patients to commercially available community services [36]. It may not be feasible to manage obesity within the confines of acute clinic visits. Providers need to identify and diagnose patients with obesity and then have effective interventions and treatment services available beyond the primary care visit. Future studies of the comparative effectiveness of obesity management options may help providers better identify which treatments will be most effective for particular patients. If obesity is left undiagnosed and untreated, the health of patients will suffer.
Acknowledgement
I would like to thank Brian Mallow for his help in creating the figure for the paper.
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Marinou K, Tousoulis D, Antonopoulos AS, Stefanadi E, Stefanadis C. Obesity and cardiovascular disease: from pathophysiology to risk stratification. International Journal of Cardiology. 2010;138(1):3–8. doi: 10.1016/j.ijcard.2009.03.135. [DOI] [PubMed] [Google Scholar]
- 2.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brumpton B, Langhammer A, Romundstad P, Chen Y, Mai XM. The associations of anxiety and depression symptoms with weight change and incident obesity: the HUNT Study. International Journal of Obesity (London) 2013;37(9):1268–1274. doi: 10.1038/ijo.2012.204. [DOI] [PubMed] [Google Scholar]
- 4.Alley DE, Chang VW. The changing relationship of obesity and disability, 1988–2004. JAMA: The Journal of the American Medical Association. 2007;298(17):2020–2027. doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. [last accessed 5 November 2014];Obesity and Overweight: Fact Sheet No. 311. 2014 Available at: http://www.who.int/mediacentre/factsheets/fs311/en.
- 6.Trogdon J, Finkelstein E, Hylands T, Dellea P, Kamal-Bahl S. Indirect costs of obesity: a review of the current literature. Obesity Reviews. 2008;9(5):489–500. doi: 10.1111/j.1467-789X.2008.00472.x. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. [last accessed 4 June 2014];Prevalence and Trends Data Overweight and Obesity (BMI) – 2012. 2012 Available at: http://apps.nccd.cdc.gov/brfss/list.asp?cat=OB&yr=2012&qkey=8261&state=All.
- 8.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. The New England Journal of Medicine. 2006;355(8):763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 9.Hampl SE, Davis AM, Sampilo ML, Stephens KL, Dean K. Insurer and employer views on pediatric obesity treatment: a qualitative study. Obesity (Silver Spring) 2013;21(4):795–799. doi: 10.1002/oby.20112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beal E. The pros and cons of designating obesity a disease. The American Journal of Nursing. 2013;113(11):18–19. doi: 10.1097/01.NAJ.0000437102.45737.c7. [DOI] [PubMed] [Google Scholar]
- 11.NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US) Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda, MD: National Heart, Lung, and Blood Institute; 1998. [last accessed 15 December 2014]. Available at: http://www.ncbi.nlm.nih.gov/books/NBK2003/ [Google Scholar]
- 12.National Institute for Health and Care Excellence. [last accessed 5 November 2014];Managing Overweight and Obesity in Adults – Lifestyle Weight Management Services. 2014 Available at: http://www.nice.org.uk/guidance/ph53 updated May 2014. [Google Scholar]
- 13.Bardia A, Holtan SG, Slezak JM, Thompson WG. Diagnosis of obesity by primary care physicians and impact on obesity management. Mayo Clinic Proceedings. 2007;82(8):927–932. doi: 10.4065/82.8.927. [DOI] [PubMed] [Google Scholar]
- 14.Gunther S, Guo F, Sinfield P, Rogers S, Baker R. Barriers and enablers to managing obesity in general practice: a practical approach for use in implementation activities. Quality in Primary Care. 2012;20(2):93–103. [PubMed] [Google Scholar]
- 15.Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Archives of Internal Medicine. 2009;169(3):312–316. doi: 10.1001/archinternmed.2008.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Archives of Internal Medicine. 2009;169(3):313–314. doi: 10.1001/archinternmed.2008.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gunther S, Guo F, Sinfield P, Rogers S, Baker R. Barriers and enablers to managing obesity in general practice: a practical approach for use in implementation activities. Quality in Primary Care. 2012;20(2):93–103. [PubMed] [Google Scholar]
- 18.Ruelaz AR, Diefenbach P, Simon B, Lanto A, Arterburn D, Shekelle PG. Perceived barriers to weight management in primary care – perspectives of patients and providers. Journal of General Internal Medicine. 2007;22(4):518–522. doi: 10.1007/s11606-007-0125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mauro M, Taylor V, Wharton S, Sharma AM. Barriers to obesity treatment. European Journal of Internal Medicine. 2008;19(3):173–180. doi: 10.1016/j.ejim.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Jay M, Kalet A, Ark T, et al. Physicians’ attitudes about obesity and their associations with competency and specialty: a cross-sectional study. BMC Health Services Research. 2009;9(1):106. doi: 10.1186/1472-6963-9-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–1486. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Boyle CA, Henly SJ, Larson E. Understanding adherence to hand hygiene recommendations: the theory of planned behavior. American Journal of Infection Control. 2001;29(6):352–360. doi: 10.1067/mic.2001.18405. [DOI] [PubMed] [Google Scholar]
- 23.Millstein SG. Utility of the theories of reasoned action and planned behavior for predicting physician behavior: a prospective analysis. Health Psychology. 1996;15(5):398. doi: 10.1037//0278-6133.15.5.398. [DOI] [PubMed] [Google Scholar]
- 24.Perkins M, Jensen P, Jaccard J, et al. Applying theory-driven approaches to understanding and modifying clinicians’ behavior: what do we know? Psychiatric Services. 2007;58(3):342–348. doi: 10.1176/ps.2007.58.3.342. [DOI] [PubMed] [Google Scholar]
- 25.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. [Google Scholar]
- 26.Centers for Disease Control and Prevention. [last accessed 4 June 2014];Prevalence and Trends Data Overweight and Obesity (BMI) 2008. 2008 Available at: http://apps.nccd.cdc.gov/brfss/list.asp?cat=OB&yr=2008&qkey=4409&state=All.
- 27.The Joint Commission. Specifications manual for Joint Commission national quality measures (v2013A1) population and sampling specifications. 2012 [Google Scholar]
- 28.National Institutes of Health (NIH), National Heart, Lung and Blood Institute (NHLBI) & North American Association for the Study of Obesity (NAASO) The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. 2000 NIH Publication No. 00–4084. [Google Scholar]
- 29.National Institutes of Health (NIH), National Heart, Lung and Blood Institute (NHLBI) & North American Association for the Study of Obesity (NAASO) The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Bethesda, MD: National Heart, Lung, and Blood Institute; 2000. [last accessed 17 December 2014]. A quick reference tool to ACT; pp. 79–80. Available at: http://www.nhlbi.nih.gov/files/docs/guidelines/prctgd_c.pdf. [Google Scholar]
- 30.National Institutes of Health (NIH) & National Heart, Lung and Blood Institute (NHLBI) Tips to Weight Loss Success. NIH; 2002. [last accessed 11 June 2014]. p. 2314. Available at: http://www.nhlbi.nih.gov/health/prof/heart/obesity/aim_kit/tips.pdf. [Google Scholar]
- 31.Nelson JM, Cook PF, Ingram JC. Utility of the theory of planned behavior to predict nursing staff blood pressure monitoring behaviours. Journal of Clinical Nursing. 2014;23(3–4):461–470. doi: 10.1111/jocn.12183. [DOI] [PubMed] [Google Scholar]
- 32.Lopez MA, Osterberg LD, Jensen-Doss A, Rae WA. Effects of workshop training for providers under mandated use of an evidence-based practice. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38(4):301–312. doi: 10.1007/s10488-010-0326-8. [DOI] [PubMed] [Google Scholar]
- 33.Monsen KA, Attleson IS, Erickson KJ, Neely C, Oftedahl G, Thorson DR. Translation of obesity practice guidelines: interprofessional perspectives regarding the impact of public health nurse system-level intervention. Public Health Nursing. 2014 doi: 10.1111/phn.12139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shamir B. Leadership takes time: some implications of (not) taking time seriously in leadership research. The Leadership Quarterly. 2011;22(2):307–315. [Google Scholar]
- 35.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Affairs. 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 36.Wadden TA, Volger S, Tsai AG, et al. Managing obesity in primary care practice: an overview with perspective from the POWER-UP study. International Journal of Obesity. 2013;37:S3–S11. doi: 10.1038/ijo.2013.90. [DOI] [PMC free article] [PubMed] [Google Scholar]