Abstract
Portal vein thrombosis is an important cause of portal hypertension. PVT occurs in association with cirrhosis or as a result of malignant invasion by hepatocellular carcinoma or even in the absence of associated liver disease. With the current research into its genesis, majority now have an underlying prothrombotic state detectable. Endothelial activation and stagnant portal blood flow also contribute to formation of the thrombus. Acute non-cirrhotic PVT, chronic PVT (EHPVO), and portal vein thrombosis in cirrhosis are the three main variants of portal vein thrombosis with varying etiological factors and variability in presentation and management. Procoagulant state should be actively investigated. Anticoagulation is the mainstay of therapy for acute non-cirrhotic PVT, with supporting evidence for its use in cirrhotic population as well. Chronic PVT (EHPVO) on the other hand requires the management of portal hypertension as such and with role for anticoagulation in the setting of underlying prothrombotic state, however data is awaited in those with no underlying prothrombotic states. TIPS and liver transplant may be feasible even in the setting of PVT however proper selection of candidates and type of surgery is warranted. Thrombolysis and thrombectomy have some role. TARE is a new modality for management of HCC with portal vein invasion.
Keywords: PVT, prothrombotic, acute and chronic, imaging, anticoagulation
Abbreviations: ACLA, anti-cardiolipin antibody; AFP, alpha feto protein; BCS, Budd-Chiari syndrome; CDUS, color doppler ultrasonography; CT, computed tomography; CTP, Child Turcotte Pugh; EHPVO, extra hepatic portal venous obstruction; EST, endoscopic sclerotherapy; HCC, hepatocellular carcinoma; HVPG, hepatic venous pressure gradient; IGF-1, insulin like growth factor-1; IGFBP-3, insulin like growth factor binding protein-3; INR, international normalized ratio; JAK-2, Janus kinase 2; LA, lupus anticoagulant; LMWH, low molecular weight heparin; MELD, model for end stage liver disease; MPD, myeloproliferative disorder; MRI, magnetic resonance imaging; MTHFR, methylenetetrahydrofolate reductase; MVT, mesenteric vein thrombosis; OCPs, oral contraceptive pills; PAI-1 4G-4G, plasminogen activator inhibitor type 1- 4G/4G genotype; PNH, paroxysmal nocturnal hemoglobinuria; PV, portal vein; PVT, portal vein thrombosis; PWUS, Pulsed Wave ultrasonography; SMA, superior mesenteric artery; SMV, superior mesenteric vein; RFA, radio frequency ablation; rtPA, recombinant tissue plasminogen activator; TAFI, thrombin activatable fibrinolysis inhibitor; TARE, Trans arterial radioembolization; TB, tuberculosis; TIPS, transjugular intrahepatic portosystemic shunt; UFH, unfractionated heparin
Portal vein thrombosis (PVT) refers to thrombosis that develops in the trunk of the portal vein including its right and left intrahepatic branches and may even extend to the splenic or superior mesenteric veins or towards the liver involving intrahepatic portal branches. PVT occurs either in association with cirrhosis or malignancy of liver or may occur without an associated liver disease. The terminology of Extra Hepatic Portal Venous Obstruction (EHPVO) refers to the development of portal cavernoma in the absence of associated liver disease. EHPVO should be considered as a separate entity. Portal vein thrombosis is an important cause of non-cirrhotic prehepatic portal hypertension all over the world.
Balfour and Stewart described the first case of PVT in 1868 in a patient with ascites, splenomegaly and variceal dilation.1 Since then portal vein thrombosis has been well studied and described in patients with or without cirrhosis. The prevalence of PVT in compensated liver disease has been reported to be 0.6–16%, 15% (5–26%) in patients awaiting liver transplantation and upto 36% in explanted liver on histopathology.2–4 PVT is seen in upto 35% of cirrhotic patients with hepatocellular carcinoma.5,6 The lifetime risk of PVT in general population is reported to be 1%.7 This review article is mainly focused on portal vein thrombosis in non-cirrhotic population-acute (recent thrombosis), chronic long standing (extrahepatic portal venous obstruction) and in patients with cirrhosis.
Etiology
The pathophysiology of portal vein thrombosis encompasses one or more features of Virchow's triad, viz., reduced portal blood flow, a hypercoagulable state or vascular endothelial injury as in Figure 1. Based on the three pathogenetic mechanisms, the etiological risk factors for non-cirrhotic and cirrhotic PVT will be discussed separately.
Figure 1.
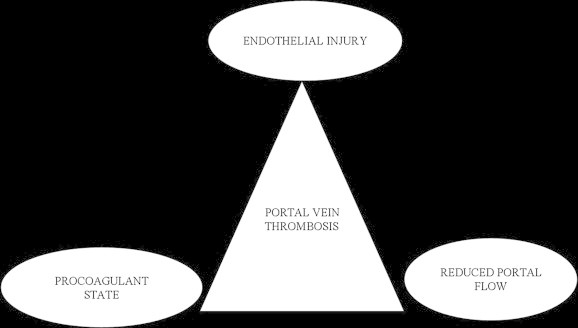
Virchow's triad for portal vein thrombosis.
Acute Non-cirrhotic Portal Vein Thrombosis
Procoagulant State
Various prothrombotic states leading to portal vein thrombosis have been identified (Table 1). Significant advances over the last decade have shown the earlier labeled idiopathic cases now being associated with thrombophilic conditions which are identified in approximately 60% of patients and an additional local predisposing factor in 30–40% of cases. In upto 80% cases the underlying cause is identified when rigorously searched for.8–13 In some cases multiple prothrombotic factors may be associated in the development of PVT.14–16 In one study one or more risk factors namely prothrombotic state or abdominal inflammation was present in 87% of patients.17 Amongst the thrombophilic states, primary myeloproliferative disorders (MPD) are common in 30.5%. Occult MPD as a cause of PVT is seen in 16.7% and classical MPD in 13.8%.18 The diagnosis of myeloproliferative disorders as a cause of PVT has increased by 20% with the identification of Janus kinase 2 (JAK 2) V617F gene mutation. The presence of JAK 2 mutation is seen in around 17–35% patients of PVT. It is now recommended by the WHO as a major diagnostic criterion for the diagnosis of MPD.19–21 PVT is a manifestation of myeloproliferative disease in 22–48% of patients. In the West, latent MPD has been reported in 58% of patients with idiopathic PVT and 51% of these developed overt MPD on follow up.22 A recent study reported PVT as the first manifestation of MPD in 70% (31 of 44 patients).23 Meta analysis of myeloproliferative disorders in PVT showed that the mean prevalence of MPD is 31.5% (95% CI 25.1–38.8%) and JAK2 mutation is 27.7% (95% ci 20.8–35.8). JAK2 and MPD both are more frequent in BCS than PVT. JAK2 mutation in splanchnic venous thrombosis without MPD features was able to identify MPD in 15.4% of PVT patients.24 In Asians, the prevalence of JAK2 mutation is 24–26.6% in non-cirrhotic non-malignant PVT versus 1.4% in cirrhosis with PVT.25,26 An Indian study reported 14% prevalence of JAK2 mutation in portal vein thrombosis out of 58 patients of intra-abdominal venous thrombosis (which included portal vein thrombosis and Budd-Chiari syndrome).27 Other prothrombotic conditions that cause PVT include paroxysmal nocturnal hemoglobinuria (PNH), antiphospholipid syndrome, hyperhomocysteinemia, inherited prothrombotic disorders such as protein C (in 0–9.1%), S (0.9–30%) and antithrombin III deficiencies (0–4.5%) and less frequently factor V Leiden mutation (1.3–7.6%), factor II mutation (G20210A in 0–22%) and methylenetetrahydrofolate reductase (MTHFR) gene mutation.9–11 These inherited disorders may be a secondary phenomenon rather than primary, since they are produced from the liver and may be affected in parenchymal liver disease. They may ultimately be confirmed by investigating first degree relatives.9,12,28 Recently mutation in thrombin activatable fibrinolysis inhibitor (TAFI) gene and high levels of factor VIII have been shown to be associated with a risk of PVT.29,30 A recent data on thrombophilia by D Amico et al showed that myeloproliferative disorders were the most common cause in PVT patients and thrombophilia work up in the PVT patients revealed PAI-1 4G-4G (plasminogen activator inhibitor type 1- 4G/4G genotype) as the most common cause (55.5%) followed by MTHFR mutation (28.6%), factor V Leiden mutation (7.4%) and prothrombin gene mutation (7.4%). Atleast one thrombophilic state was present in 81.5% and more than one hypercoagulable state was present in 18.5%.31 The meta analysis on thrombophilia in portal venous system thrombosis showed the prevalence of antithrombin III deficiency in 3.9%, protein C deficiency in 5.6% and protein S deficiency in 2.6% with Odds ratio of 8.89, 17.63 and 8.00 respectively.32 Indian data on hypercoagulable states in portal vein thrombosis reveal that the inherited thrombophilia is infrequent in the Indian population. Protein C deficiency is seen in 8–9%, protein S deficiency in 3–4%, factor V Leiden mutation in 3–6% and antiphospholipid antibody in 18–23%.11,33–35 Antithrombin III deficiency and prothrombin gene mutation are however uncommon. However another study from India of 26 PVT patients showed the presence of protein C deficiency in 12, protein S deficiency in 9, antithrombin III deficiency in 8 patients, ACLA in 3 and LA in 4 patients. No prothrombin gene mutation and PNH states were seen in this study.36 High factor VIII levels have also been shown to be associated with portal vein thrombosis in Indian patients.37 Heterozygous MTHFR has been reported in 21% of PVT patients and hyperhomocysteinemia in 7.6% while homozygous MTHFR has not been seen.11 A strong link of Bacteroides fragillus infection with PVT has also been demonstrated possibly due to transient development of anti-cardiolipin antibodies.38 Other conditions that are associated with PVT are use of oral contraceptives, cytomegalovirus infection,39 pregnancy, chronic inflammatory diseases and malignancies in the background of the above prothrombotic causes.8
Table 1.
Prothrombotic Causes of Portal Vein Thrombosis.
Inherited prothrombotic disorders
|
Acquired thrombophilic disorders
|
Vascular Endothelial Injury
Local risk factors may also lead to thrombosis via endothelial activation of prothrombotic factors as a result of various intra-abdominal inflammatory diseases. The intra-abdominal inflammatory conditions leading to sepsis that cause PVT include pancreatitis, cholecystitis, cholangitis, appendicitis, liver abscess and local injury to portal venous axis following splenectomy including laparoscopic splenectomy, laparoscopic colectomy, abdominal trauma, portocaval shunts & other intra-abdominal surgical procedures in association with the above acquired or inherited prothrombotic conditions.40–44 A recent study of 102 patients with non-cirrhotic non-malignant acute PVT showed the presence of local factors as a cause for thrombosis in upto 21% and acute pancreatitis as the most common cause followed by cholecystitis or cholangitis and liver abscess.45 PVT may also occur after ablative therapy for HCC and fine needle aspiration of pancreatic mass.46–48 PVT sometimes occurs after liver transplantation at the anastomotic site due to donor/recipient portal vein diameter mismatch.49,50 Transient PVT has been reported in 23% of patients with acute pancreatitis and 57% in those with pancreatic necrosis.51 PVT may also occur with Budd-Chiari syndrome mainly due to stagnant portal venous flow and an underlying prothrombotic state.52 Recently thrombosis of the portal and mesenteric veins has been described presenting as a medical emergency in troops posted at high altitudes in India.53 In the Asian Pacific region PVT in children has been attributed to omphalitis, neonatal umbilical sepsis overt or unrecognized and umbilical vein cannulation.54 However, a study has shown that although umbilical venous catheter associated thrombosis is common spontaneous resolution occurs in most cases.55 Therapeutic contralateral portal vein embolization before major hepatic resection is practiced at a few centers, where the future remnant liver volume is likely to be less than 30% of total liver. With successful therapeutic PVT of the contralateral site, there is hypertrophy of functional residual liver by 47% after 4–8 weeks, which helps in prevention of liver failure.56
Reduced Portal Blood Flow
Direct vascular invasion by hepatocellular carcinoma and cholangiocarcinoma leads to malignant portal vein obstruction. Malignancy as a cause of PVT is seen in 21–24%. Apart from vascular invasion, compression by tumor mass or hypercoagulable state are the mechanisms involved. Portal vein compression by lymph node (TB, lymphoma) also contributes to PVT by reducing portal blood flow.
Chronic Portal Vein Thrombosis (Extra Hepatic Portal Venous Obstruction)
EHPVO in children
Infection
It is hypothesized that EHPVO in children has initial component of phlebosclerosis, with thrombosis as a secondary event,57 due to infection or a primary thrombotic disorder. Omphalitis, neonatal umbilical sepsis, umbilical vein cannulation, repeated abdominal infections, sepsis, abdominal surgery and trauma can also result in EHPVO.54
Congenital Anomaly
Congenital anomalies of left and right vitelline veins from which the portal vein develops can result in obstruction and congenital defects of other systems have also been reported.58
Prothrombotic State
The frequency of prothrombotic disorders has been found to be variable in children.11,59
Idiopathic
The cause of EHPVO may remain obscure in 50% of patients.
EHPVO in adults
Prothrombotic Disorders
Prothrombotic states are more common in adults.11 In the West, latent myeloproliferative disorder has been reported in 58% patients with EHPVO of unknown etiology, and 57% of these go on to develop an overt myeloproliferative disorder during follow-up.22 Other studies have not corroborated these findings. One study found only methyl tetrahydrofolate reductase mutation to be higher in EHPVO patients than deep vein thrombosis patients among the prothrombotic states.12
Infection and Surgery
Intra-abdominal sepsis and abdominal surgery contribute to EHPVO.
Pregnancy and Oral Contraceptives
Both pregnancy and OCPs in the presence of a prothrombotic disorder can result in EHPVO.
Portal Vein Thrombosis in Cirrhosis
Procoagulant State
Cirrhosis is no longer considered a hypocoagulable state. In fact the procoagulant and anticoagulant factors are in a state of balance in cirrhosis with no increased bleeding risk. Instead, increased factor VIII levels, reduced albumin tilt the balance towards hypercoagulability in cirrhosis. In patients with cirrhosis, G20210A mutation of prothrombin has a prevalence of 21.4–29% with Odds ratio of 5.9 for development of PVT. Mutation of prothrombin gene was found to be the only thrombophilic condition associated with PVT in 701 cirrhotics.5 Thrombophilic state is detected in 69.5% patients of cirrhosis with PVT. The frequencies of factor V Leiden mutation, prothrombin gene mutation, and homozygous MTHFR C677T in cirrhotics with PVT were detected in 13%, 34.8% and 43.5% respectively.60 Another study on PVT in cirrhotics concluded that prothrombotic mutations by themselves are not causative of PVT, but sclerotherapy and previous abdominal surgery favors development of PVT in 2/3rd of cases but is elusive in others.61 The frequency of Factor V Leiden mutation (29%) and prothrombin gene mutation (29%) are more frequent in cirrhosis with PVT compared to cirrhosis without PVT, non-cirrhotics with PVT and healthy controls.62
Reduced Portal Blood Flow
In cirrhosis, portal hemodynamics play an important role in the development of portal vein thrombosis. A study by Zocco et al showed portal flow velocity of less than 15 cm/s on Doppler ultrasound as a predictive factor for the development of portal vein thrombosis with a risk of 47.8% when compared to 2% risk with a flow of more than 15 cm/s.63 The parenchymal architectural distortion in cirrhosis and altered vascular reactivity results in increased intrahepatic vascular resistance and reduction in portal blood flow. The development of portosystemic collateral circulation and splanchnic vasodilatation on venous side also adds to stagnation of the portal blood flow leading to PVT. A recent study has also shown that in patients with PVT, the largest collateral vessel blood flow was an independent predictor of PVT. The blood flow velocity in the largest collateral (>10 cm/s) and flow volume (>400 ml/min) were associated with increased incidence of portal vein thrombosis in virus related cirrhosis.64
Vascular Endothelial Injury
Endoscopic therapy of bleeding varices also leads to direct endothelial damage or procedure related bacteremia leading to development of thrombosis. PVT has been described following endoscopic sclerotherapy in patients with cirrhosis in association with these thrombophilic conditions.65 Endotoxemia in cirrhosis may increase the risk of PVT in cirrhosis.
Presentation
Clinically PVT may be acute or chronic. Although no time frame exists, to distinguish acute from chronic PVT, it is usually considered acute if symptoms developed <60 days prior to hospital assessment.66 This may not hold true always as patients with chronic PVT may first present with upper GI bleeding. An easy way to differentiate acute PVT from chronic PVT is the absence or insignificant portoportal collaterals on imaging and no evidence of portal hypertension including splenomegaly and esophageal varices. The proportion of patients who develop chronic PVT from acute is known for those who develop symptomatic PVT recognized early however it is unclear for those who develop asymptomatic PVT.
Acute Non-cirrhotic Portal Vein Thrombosis
In acute PVT there is a sudden formation of thrombosis within the portal vein that leads to a complete or partial obstruction of the portal vein. Acute PVT in non-cirrhotic non-malignant PVT usually presents with abdominal pain (91%), fever (53%), ascites (38%) which is small volume ascites (detectable only on imaging in 33% and clinical ascites in 5%).45 Splenomegaly is seen in 37% patients and 40% of which have an underlying myeloproliferative disorder. In the remaining 63% patients without splenomegaly, myeloproliferative disorder is detected in only 5% patients.45 Involvement of superior mesenteric vein and the mesenteric venous arches may lead to intestinal ischemia, bowel infarction and ileus. Patients may then present with hematochezia, rebound tenderness, fever and ascites. Bowel infarction is an important cause of mortality in patients with thrombosis of portal venous system.40 Partial obstruction of portal vein may be associated with lesser symptoms. Acute development of ascites, although rare, may also be seen which is usually mild and transient due to intestinal venous congestion. The natural history of acute PVT is usually uncertain and modified by medical intervention.
Chronic Portal Vein Thrombosis (Extra Hepatic Portal Venous Obstruction)
Patients with chronic PVT or classically referred to as EHPVO present with portal hypertension related complications like a well tolerated variceal bleed, splenomegaly, anemia and thrombocytopenia or may be asymptomatic with incidental detection following an imaging procedure.
The most common presentation in children is recurrent upper gastrointestinal bleeding.67,68 Bleeding usually occurs in the first or second decade of life. The bleed is well tolerated due to underlying normal functioning liver. Transient ascites is seen in one fifth of children following the episode of bleed.69 About 10% of children present with isolated splenomegaly.70 Splenomegaly is almost universal and may be symptomatic with left upper abdominal discomfort (due to massive splenomegaly) or as pain (due to splenic infarcts) or sometimes as symptomatic hypersplenism. Hypersplenism is seen in upto one third of patients and is usually asymptomatic. Splenomegaly may transiently reduce during episodes of acute variceal bleed. Growth retardation may be seen in upto 50% of children due to possibly impaired synthesis of growth factors, insulin like growth factor (IGF-1) and insulin like growth factor binding protein-3 (IGFBP-3) and increased levels of growth hormone leading to growth hormone resistance, increased frequency of bleed and malabsorption due to portal hypertensive enteropathy.71,72 Mild cognitive and psychomotor dysfunction has also been reported in children. Ectopic varices at sites like duodenum, anorectum, colon or gallbladder are significantly more common in chronic PVT than in patients' with cirrhosis.73,74 Ascites and encephalopathy are not common and usually transient precipitated by gastrointestinal bleed. A spurt in growth after shunt surgery in children has been observed.75 Another study however did not show any growth impairment in children with PVT.76
Chronic PVT in adults presents with recurrent upper gastrointestinal bleed like children. Bleed may occur from esophago-gastric varices or ectopic varices in duodenum or elsewhere. Transient ascites may occur following bleed. Overt hepatic encephalopathy is rare but minimal hepatic encephalopathy may be seen in 50% of patients due to portosystemic shunting. Hypersplenism may rarely be symptomatic and patients can also develop portal biliopathy.77 Other rare clinical manifestations include obstructive jaundice, cholangitis and even choledocholithasis late in the natural course of the disease due to pseudosclerosing cholangitis or portal hypertensive biliopathy.78–83
Portal Vein Thrombosis in Cirrhosis
In a study of 701 cirrhotics, development of portal vein thrombosis occurred in 79 (11.2%) patients. Majority of patients were in child B and C. PVT was asymptomatic in 43% and symptomatic in 57%. Symptoms included gastrointestinal bleed in 31 (39.2%) patients (18 were variceal bleed and 13 were portal hypertensive gastropathy related) and abdominal pain in 14 (17.7%). Ten patients (70%) with abdominal pain had intestinal infarction.5 Mesenteric venous involvement was never asymptomatic and lead to intestinal ischemia or infarction. Another study which included cirrhosis and cancer both (n = 19), abdominalia (abdominal pain, loss of appetite, nausea, vomiting, diarrhea) was seen in 63%, bleeding (hematemesis, melena or rectal) in 58%, splenomegaly in 63%, fever in 37%, ascites in 32%, and weight loss in 16% patients.17
Diagnosis
Liver Function
The liver functions are normal or near normal except if PVT occurs in a patient with cirrhosis. Prothrombin levels and other coagulation factors may be decreased while D-dimer is usually increased.18,84 Patients with portal hypertensive biliopathy may show a rise in alkaline phosphatase. Liver grossly is normal in PVT, but may show atrophy and regenerative nodular hyperplasia, related to apoptosis and compensatory arterial vasodilation in chronic PVT.85–87 Liver function derangement may be seen in EHPVO in the form of ascites, prothrombin time prolongation and low serum albumin in patients with prolonged portal hypertension.69
Ultrasound
Ultrasound is the investigation of choice. It shows solid isoechoic or hypoechoic material within portal vein either filling the lumen partially or complete.88 It is the least expensive method but sensitivity and specificity is affected by interpatient variability and expertise of the given radiologist.89 Overall the sensitivity and specificity of ultrasound for detecting portal vein thrombosis ranges from 80 to 100% with an accuracy of 88–98%. Demonstration of a portal cavernoma (multiple tortuous small vessels replacing the portal vein) is suggestive of chronic PVT, and is usually associated with splenomegaly and collaterals in relation to portal venous system. Color Doppler ultrasonography (CDUS) and Pulsed Wave ultrasonography (PWUS) demonstrated the absence or reduced flow in portal vein. The diagnostic sensitivity and specificity for Color Doppler Ultrasound (CDUS) in detecting portal vein thrombosis varies from 66% to 100%.90,91 Contrast enhanced ultrasound (CDUS) is another modality that has been found to be superior to ultrasound in demonstrating the presence or absence of flow and is more reliable in patients with extremely low portal vein velocity. Endoscopic ultrasound has also been reported to be a sensitive (81%) and specific (93%) test to diagnose portal vein thrombosis.92–94 Gallbladder varices on ultrasound have been seen in 12–30% of adults with chronic PVT.95
Computed Tomography and Magnetic Resonance Imaging
CT and MRI provide additional information such as extension of thrombus, evidence of bowel infarction and status of adjacent organs. On non-contrast enhanced CT, portal vein thrombus is generally seen to be isodense to adjacent soft tissue, but may be hyperdense if it occurred within a month.96 Following intravenous administration of iodinated contrast on CT, a bland thrombus is seen as a low density, non-enhancing defect within portal veins, while a tumor thrombus enhances following contrast administration. Moreover dynamic CT shows a filling defect partially or totally occluding the vessel lumen with rim enhancement of the vessel wall.97 Certain other features of malignant portal vein obstruction include expansive effect (portal vein enlargement due to the mass forming thrombus), disruption of the vessel wall and intra thrombus arterial neovascularization. The sensitivity and specificity of MRI for detecting main PVT are 100% and 98% respectively in patients undergoing liver transplantation, the discordance being due to a decreased caliber of main portal vein that may be interpreted as recanalised chronic thrombus.98 MR portography has been shown to be superior to color Doppler US in detecting partial thrombosis, and occlusion of the main portal venous vessels. It also identifies portosplenic collaterals and portal venous vessels more adequately that cannot be visualized on color Doppler. MR portographic demonstration of portal vein occlusion may be reported as normal on CDUS and vice versa due to slow flow velocity in portal vein.99 True fast imaging with steady state precession (true FISP) with MRI has been shown to be a useful adjunct to contrast enhanced MR angiography in severely debilitated patients, where respiratory motion may degrade the images or when the use of contrast medium is not possible due to poor venous access.100 MR portography is valuable in determining the resectability of neoplasm involving the portal venous system101 and follow-up after therapeutic procedures102 including surgical splenorenal and mesocaval shunts. MR angiography has precluded the use of effective, but more invasive techniques like carbon dioxide portography or intraarterial digital subtraction angiography.103,104 PET CT has been shown to be helpful in discriminating between benign and malignant portal vein obstruction.105
Splenoportovenography
This investigation involves injecting dye in the splenic pulp and visualizing the splenoportal venous axis which helps not only in diagnosing PVT but also identifying the patency of splenoportal axis for future shunt surgery. Of the cases done by us in the preUS/CT/MRI era, it proved to be a safe procedure which also helped detecting the portal pressure and assessing the effect of drugs, since HVPG is fallacious in PVT.106 With the advent of newer non-invasive techniques splenoportovenography is now an obsolete procedure.
Endoscopy
It is important to have endoscopy in patients with PVT as portal hypertensive gastropathy is more often present in the acute PVT with cancer or cirrhosis, while large esophageal varices are present more often in patients with chronic PVT.17 In chronic PVT gastric varices are seen in upto 40% of patients.107 Ectopic varices are more often seen in chronic PVT compared with other causes of portal hypertension. Rectal varices are seen in 80% of patients. Large varices are an independent risk factor for bleeding in patients with PVT however despite large varices, with red signs, the frequency of bleeding in patients with PVT is 0.25% over 2 years which appears to be far less than in cirrhotics with similar variceal characteristics (20–30% bleeding risk over 2 years).108
Procoagulant Work up
Once the diagnosis of PVT is made, extensive investigation of prothrombotic disorders and local factors is recommended8,15,109 especially for patients with a life expectancy of more than 3–6 months and where anticoagulation is considered relevant. A list of procoagulant work up is given in Table 2. Differential diagnosis for various forms of PVT is given in Table 3.
Table 2.
Procoagulant Work Up.
| Thrombophiliac state | Test |
|---|---|
| Myeloproliferative disorder | V617F JAK2 mutation |
| Prothrombin/Factor II gene mutation | G20210A mutation |
| Factor V Leiden mutation | Increased protein C resistance, R605Q factor V mutation |
| Protein C deficiency | Decreased protein C levels plus normal PT/positive family history |
| Protein S deficiency | Decreased protein S levels plus normal PT/positive family history |
| Antithrombin deficiency | Decreased antithrombin levels plus normal PT/positive family history |
| Antiphospholipid syndrome | High anti-cardiolipin antibodies/lupus anticoagulant/antibeta 2 glycoprotein 1 antibodies plus clinical criteria |
| PNH (paroxysmal nocturnal hemoglobinuria) | Flow cytometry for CD 55 ad CD59 deficient clones |
| Hyperhomocysteinemia | Increased homocysteine levels |
Table 3.
Differential Diagnosis for Variants of PVT.
| Variant of PVT | Differentials | Differentiating features |
|---|---|---|
| Acute PVT | Acute abdominal conditions like pancreatitis, cholecystitis, appendicitis, cholangitis, liver abscess, abd. surgery or trauma | US/CT/MRI will detect fresh thrombus or any local intra-abdominal inflammatory focus or both together |
| Chronic PVT (EHPVO) | NCPF (Non-cirrhotic portal fibrosis) | Age of presentation varies, Imaging shows preserved portal vein in NCPF and cavernoma formation in EHPV |
| Cirrhosis | Ascites, jaundice, hepatic encephalopathy are common in cirrhosis and uncommon in EHPVO. Liver functions are preserved in EHPVO. Splenomegaly is mild in cirrhosis unlike EHPVO. Imaging shows irregular liver outline and dilated portal vein in cirrhosis. | |
| PVT in cirrhosis | PVT (bland thrombosis) | CT shows non-enhancing filling defect in the background of cirrhotic liver |
| PV invasion by HCC (in cirrhosis) | CT shows filling defect with rim enhancement of vessel wall (due to malignant invasion), disruption of vessel wall, expansile effect due to tumor mass and tumor itself also (with or without underlying cirrhotic liver) |
Prognosis
Acute Non-cirrhotic Portal Vein Thrombosis
Mortality in the past was 20%–50% with acute portal vein thrombosis and other splanchnic vessels, but with an early diagnosis, increased clinical awareness, improved diagnostic techniques and use of early anticoagulation the 5 yr survival rate has improved to 85%.110,111 Outcome of PVT is generally good and mortality primarily is due to underlying cause and less to consequences of portal hypertension. Acute PVT usually has a good prognosis when treated before the occurrence of intestinal infarction. However in the event of bowel infarction and multi organ failure, the in hospital mortality is approximately 20–50%.112 Mortality is highest at one year in patients with cancer or cirrhosis compared with those without (26% vs 8%).40 Bleeding related mortality in patients with PVT is much lower than in patients with cirrhosis due to preserved liver function.
Chronic Portal Vein Thrombosis
The overall mortality in chronic onset PVT is less than 10%8,113 whereas in cirrhosis and malignancy, it is 26%.17 A multivariate analysis done on determinants of survival in extra hepatic portal vein thrombosis showed that advanced age, malignancy, cirrhosis, mesenteric vein thrombosis, absence of abdominal inflammation, serum levels of aminotransferase and albumin are associated with reduced survival and not to complications of portal hypertension.15 Chronic PVT did not show any extension of the thrombus as shown by repeat imaging after as long as 10 years.114 Bleeding after initial variceal eradication occurs usually within first 4–10 years and the risk of bleeding reduces as age progresses especially after 10 years.115 Liver dysfunction in long term is a concern and other long term consequences in nutrition, mental function and portal biliopathy.
Portal Vein Thrombosis in Cirrhosis
A recent study on natural course of non-malignant partial PVT in cirrhosis showed that untreated partial PVT progressed in 48%, improved in 45% and was stable in 7%. The probability of hepatic decompensation at 1 and 2 years was 41% and 57% respectively. The survival rates at 1 and 2 years were 77% and 57% respectively. The progression or regression of partial PVT did not affect the clinical outcome.116
Treatment
Anticoagulation
The aim of the treatment is to reverse or prevent advancement of thrombosis in the portal venous system and to treat complications of established PVT. Most of the management decisions have to be individualized depending on the local expertise, since there is lack of randomized controlled trials. A systematic review reported that upto 83.3% of cases of acute PVT do not recanalise in the absence of anticoagulation and the remaining 16.7% cases that recanalized occurred in the setting of self limiting illness like acute pancreatitis.117 There is a clear recommendation for the use of anticoagulation in non-cirrhotic acute PVT with good safety and efficacy data. The data in the setting of cirrhosis is limited and the current guidelines do not give clear directions towards the management of PVT in cirrhosis. However certain situations require a strong recommendation for early use of anticoagulation like, in the setting of intestinal ischemia heralding an infarction, decompensated liver disease awaiting liver transplantation, compensated liver disease, PVT presenting with acute variceal bleed and even asymptomatic patients with mesenteric venous occlusion, whereas unsuitability for liver transplant in advanced liver disease and cavernoma formation in the absence of thrombotic risk factors are situations where anticoagulation may not benefit survival and outcomes.
Non-cirrhotic Acute Portal Vein Thrombosis
Anticoagulation in Non-cirrhotic Acute Portal Vein Thrombosis
A recent systematic review of various studies on management of acute non-malignant non-cirrhotic PVT demonstrated the variability in location and extent of the thrombus, methods in initiating anticoagulation whether intravenous, subcutaneous or oral.117 The recanalization rates were complete in 38.3% and partial in 14%, overall 52.3% (complete plus partial). The time for recanalization varied from 1 to 197 days, which may have been overestimated due to time lag between diagnosis to performance of a repeat imaging. Nonetheless the long duration for recanalization to occur as demonstrated in certain studies could suggest that the anticoagulation duration may actually be indicated for upto 6 months duration. Although few authors recommended lifelong anticoagulation in case of prothrombotic disorder, certain studies gave anticoagulation for lifelong irrespective of the etiology. Follow up of upto 12 months in majority and development of portal cavernoma occurred in 19.9% patients. Minor complication is reported in 3 cases, retroperitoneal bleed in 1 and gum bleed/epistaxis in 2 patients. Varices were seen in 47 patients and variceal bleed occurred in 5 patients, all five had failed to recanalize the portal vein.117
A recent multicenter 2 year follow up study evaluated 102 patients of acute PVT unrelated to cirrhosis and anticoagulation was given in 95 patients.45 Following anticoagulation 1 year portal vein recanalization rate was 39% and no recanalization occurred beyond 6 months after initiation of anticoagulation. Splenic vein and superior mesenteric vein patency was achieved in 80% and 73% respectively. Ascites and splenic vein thrombosis are independent factors predicting failure of recanalization.45 Table 4 summarizes the clinical studies on anticoagulation in acute non-cirrhotic non-malignant PVT.
Table 4.
Clinical Studies on Anticoagulation in Acute Non-cirrhotic Non-malignant PVT.
| Reference | No. of patients | Drug and dosage | Duration | Recanalization | Complication |
|---|---|---|---|---|---|
| Plessier et al45 (2010) | 95/102 | 61 LMWH, 23 UFH, 11 OA | – | 39% | Portal cavernoma in 40% GIbleed-9, intestinal infarction-2 |
| Tumes et al13 (2008) | 27 | IV OR LMWH, OA | OA 6 months or lifelong in case of prothrombotic risk | 44% (22% complete and 22% partial) | 1 retroperitoneal hematoma, variceal bleed in 4, ascites in 5 |
| Sogaard et al17 (2007) | 17 | Not specified (16/17) anticoagulated | – | 10 had improved flow | 47% varices, no bleed, 47% ascites |
| Amitrano et al114 (2007) | 21 | LMWH 200 IU/kg/d, OA | OA 6 months (lifelong if bowel resection, incomplete recanalization or thrombophila) | 45.5% complete | Minor gum bleed/epistaxis in 2, Rethrombosis at 22 months |
| Romano et al118 (2006) | 12 | IV heparin, OA | – | 58.3% | – |
| Condat B et al111 (2000) | 33-recent PVT, 108-portal cavernoma | IV heparin, OA | 28 days-4 months | 10/27-complete 15/27-partial 2/27-none |
1 had 2 variceal bleeds, 1 hemorrhage into ovarian cyst |
| Sheen et al119 (2000) | 9 | IV heparin, OA | 3 months OA | 55.5%, at median 197 days from diagnosis | – |
The duration of anticoagulation is not well defined. Recanalization occurs within 4–6 months after anticoagulation, hence these patients should be kept on anticoagulation for at least 6 months. Long term anticoagulation may be recommended in patients with identified prothrombotic disorders, recurrent episodes of thrombosis or family history of venous thrombosis.120 Anticoagulation should be initiated with heparin & maintained for 2–3 week. Later oral Vit K antagonists should be given to maintain an INR of 2–3. There is more controversy of its role in chronic PVT. There is insufficient evidence for starting anticoagulation in patients with portal cavernoma, although recanalization in partial PVT has been reported in patients with cirrhosis.121 Anticoagulation has also been shown to reverse biliary abnormalities due to acute portal vein thrombosis.122 Early initiation of anticoagulation preferably within 30 days of symptoms is recommended since no spontaneous recanalization is reported except in acute pancreatitis. Recanalization decreases from 69% when anticoagulation was instituted within first week to 25% when instituted at 2nd week.13 Thirty five percent of acute PVT show recanalization with early anticoagulation.13,45,111 In another study early anticoagulation could achieve recanalization in 12 of 27 (40%) patients without cirrhosis and malignancy compared with none of the 11 patients who were not given anticoagulation. Varices appeared as early as 1 month after PVT.15 In yet another study anticoagulation was able to achieve recanalization of acute splanchnic venous thrombosis in 45.4% of patients and prevented them from recurrent thrombosis when given lifelong.114 Recanalization is less likely, if the thrombosis is extensive due to more than one prothrombotic disorder and associated with ascites.114 Early anticoagulation in mesenteric and portal vein thrombosis minimizes serious complications like peritonitis due to bowel necrosis and also significantly decreases the development of esophageal varices related complications.13,121
The outcome of portal vein thrombosis in adults has been studied in relation to anticoagulation. Out of 136 patients of non-cirrhotic non-malignant portal vein thrombosis, 84 received anticoagulation. Over a median follow up of 46 months, the incidence rate of gastrointestinal bleeding was 12.5 (95% confidence interval [CI], 10–15) per 100 patient-years. Large varices were an independent predictor for bleeding. Anticoagulant therapy did not increase the risk or the severity of bleeding. The incidence rate of thrombotic events was 5.5 (95% CI, 3.8–7.2) per 100 patient-years. Underlying prothrombotic state and absence of anticoagulant therapy were independent predictors for thrombosis. In patients with underlying prothrombotic state, the incidence rates of splanchnic venous infarction were 0.82 and 5.2 per 100 patient-years in periods with and without anticoagulant therapy, respectively (P = 0.01). Two non-anticoagulated patients died of bleeding and thrombosis, respectively.40 Another recent retrospective data of 120 patients of non-cirrhotic portal vein thrombosis showed that of 66 patients who were anticoagulated, the overall thrombotic risk at 1, 5, 10 years was 4%, 8% and 27% respectively. The presence of a prothrombotic disorder was the only independent predictor of recurrent thrombosis and use of anticoagulation tended to reduce the risk. Eighty three gastrointestinal bleed events occurred in 37 patients and the rebleeding risk at 1, 5, 10 years was 19%, 46% and 49% respectively. Anticoagulation therapy was a predictor of bleed but not associated with severity of the bleeding.123
Thrombolysis in Non-cirrhotic Acute Portal Vein Thrombosis
Thrombolytic therapy in very recent portal vein thrombosis can be done via indirect intraarterial infusion into the superior mesenteric artery or directly via catheter introduced into portal vein either transhepatically or through transjugular approach and may improve regional clot lysis.124–127 Catheterization of SMA operatively and intraarterial infusion of thrombolytic drugs like recombinant tissue plasminogen activator,128 urokinase and streptokinase have all been shown to have gratifying results.129 Indirect infusion of thrombolytics into SMA is technically less demanding but does not allow direct infusion into the thrombus. As a result the thrombolytics have a propensity to be diverted into the collaterals and prolong the total infusion into SMA. Prolonged catheterization may itself pose a risk of embolizing SMA and its arterial branches itself. Direct access to portal vein via transjugular or percutaneous intrahepatic route targets the thrombus directly and improvement in flow and clinical symptoms. It also has the advantage of being less time consuming, more efficient and reduced dose of thrombolytics thereby reducing the thrombolysis related complications. Liu FY et al130 described a case series of 46 patients of acute symptomatic portal-meseteric venous thrombosis treated with thrombolysis. They were treated with interventional therapy, including direct thrombolysis (26 cases through a transjugular intrahepatic portosystemic shunt; 6 through percutaneous transhepatic portal vein cannulation) and indirect thrombolysis (10 through the femoral artery to superior mesenteric artery catheterization; 4 through the radial artery to superior mesenteric artery catheterization). Complete or partial success was achieved in 34 patients. In 11 patients with no reperfusion collateral vessels increased significantly. Symptoms improved dramatically in these 45 patients however 1 patient who did not respond had bowel necrosis requiring surgical intervention.130 A retrospective review of 33 cases of portal vein thrombosis treated with conservative treatment in 5, all of whom died and with thrombolysis using streptokinase or rtPA in 28 patients. Recanalization was noted in 10 patients, all of whom had history of less than 2 weeks. In patients with longer duration of history, partial occlusion persisted in 13 patients. In 5 patients with history of more than 30–40 days, thrombolysis failed. Four patients died (2 from portal rethrombosis, 1 each due to liver failure and cerebral stroke).66 In a series of 20 patients with acute or subacute portal and mesenteric vein thrombosis with severe symptoms treatment with thrombolytic therapy was initiated via transhepatic, common femoral or SMA routes. Fifteen of the 20 patients exhibited some degree of lysis of the thrombosis, 3 having complete resolution, 12 partial and five no resolution. Eighty five percent had resolution of symptoms, but major complications including bleeding developed in 60% patients. The investigators felt thus that thrombolytic therapy should be reserved for patients with severe disease. Most centers now tend to choose a more conservative therapeutic strategy.127 Another series of 12 patients with acute symptomatic superior mesenteric vein thrombosis treated with urokinase infusion via transjugular route resulted in substantial clinical improvement and technical success in all. SMV thrombosis disappeared in all with no recurrence of thrombotic episode. However all these patients had failed anticoagulation therapy and subsequently intervened by thrombolysis.131 Another 12 patient series of thrombolysis showed complete success in three and partial in four patients. Minor bleeding was noted in two (17%) and major bleeding in six (50%) with a fatal outcome in two.132 Thrombolysis via omental vein catheterization and via creation of intrahepatic portosystemic shunts (IPS) have also been reported.133,134
Thrombectomy
Surgical thrombectomy is associated with recurrence of thrombosis, surgical morbidity and mortality and hence not recommended. Mechanical thrombectomy by percutaneous transhepatic route has the advantage of rapidly removing thrombus in a recently developed PVT (<30 days) although its drawbacks include intimal or vascular trauma to the portal vein, that may promote recurrent thrombosis.135 Percutaneous transhepatic thromboaspiration within 72 h has been done successfully in some patients.136 Mechanical aspiration thromobectomy during TIPs placement has also been attempted successfully.137 Pharmacological lysis of the thrombus with local urokinase and local removal of the clot allowed restoration of normal blood flow to the liver in three patients who developed PVT following liver transplantation. Balloon dilation and placement of vascular stent are helpful in decreasing the risk of recurrent thrombosis where a defective surgical technique is the reason for thrombosis.138
Portal Vein Thrombosis in Cirrhosis
Anticoagulation in Cirrhotic Portal Vein Thrombosis
In patients with cirrhosis there are only few studies on the use of anticoagulation for PVT. The numbers have been small in these studies and majority was partial PVT. The treatment regimens mainly used low molecular weight heparin (LMWH), one study also used oral Vitamin K antagonist. Complete recanalization rates achieved with anticoagulation are 42–75% and the risk of extension of thrombosis is 5–7% only. The choice of anticoagulant is not clearly certain. However the studies on cirrhosis have predominantly used low molecular weight heparin than unfractionated heparin (UFH) in the treatment of PVT with an advantage of no monitoring requirement, lower bleeding risk and risk of thrombocytopenia with LMWH. LMWH when compared to oral anticoagulants where INR monitoring is a complicated issue as a whole in the setting of cirrhosis again has an advantage. The control of bleeding related to oral anticoagulant use is also difficult to predict due to prolonged half life and anticoagulant effects of oral drugs. Studies on the use of anticoagulation in cirrhosis with portal vein thrombosis are limited and are shown in Table 5.
Table 5.
Studies on the Use of Anticoagulation in Cirrhosis with PVT.
| Reference | No. of patients | Drug and dosage | Duration | Recanalization | Complication |
|---|---|---|---|---|---|
| Amitrano et al139 (2010) | 28 uncontrolled | Enoxaparin 200 u/kg/d | 6 months | Complete-21 Partial-2 |
None |
| Francoz et al121 (2005) | 19 cohort study | LMWH (Nadroparin) 5700 IU/d, followed by VKA | Complete-8 | Post EVL ulcer bleed-1 | |
| Senzolo et al140 (2009) | 33 uncontrolled | LMWH antiXa 95 U/kg/bw TID | Complete-12 Partial-9 |
HIT-1, Non-variceal bleed-1 | |
| Pellicelli et al141 (2010) | 9 uncontrolled | Enoxaparin 100 U/kg/d | 3–4months | Complete-3 Partial-6 |
None |
| Warmer et al142 (2012) | 28 uncontrolled | Warfarin | 1 year or until recanalization | Complete-11 Partial-12 |
Vaginal bleed-1 |
| Delgado et al143 (2012) | 55 uncontrolled | LMWH (in 27, 21 shifted to VKA), VKA (in 8) | Complete-25 Partial-8 |
Non-variceal bleed-5 Variceal bleed-6 |
|
| Senzolo et al144 (2012) | 56 non-randomized, Treatment group-35 Control-21 |
Nadroparin (95 antiXa U/kg body weight) TID (n = 33), 2 had portal cavernoma | Treatment group: Complete-12 Partial-9 Control: Complete-1 Thrombus progression in treatment group was 5 and control was 15 (P < 0.001), TIPS placed in 6 patients |
Treatment group: Variceal bleed-1 Control: Variceal bleed-5, intestinal ischemia-2 |
Newer oral anticoagulants in portal vein thrombosis have not been studied. However a recent case report of the use of rivaroxaban (orally active direct factor Xa inhibitor) in Child A NASH related cirrhosis with acute PVT and MVT was reported. Unfractionated heparin followed by transition to oral rivaroxaban 20 mg daily was given for 6 months. There was complete dissolution of the clot on repeat imaging at 6 months.145 Due to its predominant hepatic metabolism it is currently contra indicated in Child B and C cirrhosis, coagulopathy and clinically relevant bleeding risk. Another case of successful treatment of portal vein thrombosis has also been reported with rivaroxaban.146
Thrombolysis in Cirrhotic Portal Vein Thrombosis
A pilot study of systemic thrombolysis in 9 patients of cirrhosis with portal vein thrombosis was performed with rtPA a plus low molecular weight heparin. Complete regression of thrombosis was achieved in 4, partial in 4 and none in 1. There were no significant side effects.147
Role as Prophylactic Anticoagulation to Prevent Portal Vein Thrombosis
Low molecular weight heparin has been shown to prevent portal vein thrombosis and liver decompensation in patients with advanced cirrhosis in a recent randomized controlled trial.148 The trial showed that enoxaparin (4000 IU/day, subcutaneously for 48 weeks) was effective in preventing PVT in cirrhosis with Child score 7–10 such that no patient in enoxaparin group developed PVT compared to placebo group (16.6%). Liver decompensation was less in enoxaparin group (11.7%) than controls (59.4%) and actuarial probability of survival was higher.148 Enoxaparin was safe with no significant side effects or hemorrhagic events. It is too early to recommend anticoagulation for a prophylactic role in preventing PVT due to limited data availability.
Chronic Portal Vein Thrombosis (Extra Hepatic Portal Venous Obstruction)
Endotherapy
Acute gastrointestinal bleeding due to varices is treated in a similar way as in cirrhotics with endotherapy. There is no study on the use of vasopressors, although there may be a slightly increased risk of PVT in view of presence of procoagulant factors. No studies have addressed the role of primary prophylaxis in PVT associated portal hypertension. There is concern of extension of thrombosis with beta-blockers as well as vasopressors due to decrease in splanchnic blood flow.108 No report has addressed this complication with terlipressin; but a case report does exist with use of vasopressin.149
Two retrospective studies have suggested that beta adrenergic blockade may play a role in secondary prophylaxis as they reduce the risk of rebleeding and improve survival after variceal bleed.40 Endoscopic variceal ligation is safe and highly effective in children and adults with PVT.150,151 Band ligation plus sclerotherapy is considered to be better in treating children with chronic PVT than EST alone as it required fewer sessions and fewer complications.152 Our study has shown that variceal obliteration following endoscopic sclerotherapy opens up spontaneous shunts due to a possible increase in portal pressure in 40% of patients, which in turn protects these patients from further bleeds and recurrence of varices.153
Patients with chronic portosystemic venous thrombosis have an acceptable long term outcome with 1 and 5 year survival rates of 85.7% and 82.1% respectively. Factors associated with improved survival were use of beta blockers and anticoagulation. Presence of ascites and hyperbilirubinemia at presentation were associated with reduced survival.154
Shunt Surgery
Decompressive shunt surgery should be considered in cases with failed endotherapy although it needs to be borne in mind that 37% of patients with PVT also have thrombosis of splenic and superior mesenteric vein.155 It is also indicated for correcting symptomatic portal hypertensive biliopathy, symptomatic hypersplenism, ectopic variceal bleed, non-compliance to endotherapy, severe growth retardation, poor chances of follow up and “on demand” one time treatment. Shunts may be selective or non-selective. Non-selective shunts are end to side or side to side portocaval, proximal lienorenal, end to side mesocaval and large diameter interposition portocaval or mesocaval shunts. Selective shunts include distal lienorenal shunt, and mesenteric-left portal vein bypass (Rex shunt) which restores mesenteric blood flow to the liver through the Rex venous recessus (interposition of a jugular venous allograft between the superior mesenteric vein and the intrahepatic left portal vein), which may improve the growth potential. Warren Zeppa distal splenorenal shunts have been shown to be effective in control of bleeding and long term survival in patients with PVT.156 Mesocaval shunts may be necessary when Warren shunt is precluded. Our own study of side to side lienorenal shunts demonstrated that it not only prevented rebleed but also corrected the hypersplenism.157
Rex shunt (mesenteric left portal by pass) between the superior mesenteric vein and left portal vein is widely used now and has been considered to be more physiological over other shunts, which do not return blood directly to the liver.158 Although commonly done in children its use in adults needs to be validated.159 The intrahepatic portal vein is assessed by dissecting the terminal branches of the left portal vein in the recessus of Rex between segments III and IV of the left lobe of the liver. The vein should be relatively large for adequate flow of blood. It should be avoided if cirrhosis coexists. This bypass requires an autologous vein graft. The internal jugular vein provides a suitable and easily obtainable venous conduit. An autogenous saphenous vein, and a cryopreserved graft have also been used at some centers.160 A novel shunt approach when other surgical options fail include using the right or left gonadal vein for shunting with mesenteric veins.161
Non-shunt Surgery
Esophageal transection with or without splenectomy is less useful to control bleeding due to a high risk of late rebleeding and reappearance of varices and but can be resorted to as a non-shunt option in patients with portosystemic encephalopathy, hepatopulmonary syndrome or portopulmonary syndrome.162 Moreover splenectomy destroys the opportunity to use the splenic vein later for a shunt. In MPD spleen becomes an organ for extramedullary marrow formation and should be preserved.157
Anticoagulation in Chronic Portal Vein Thrombosis
Anticoagulation in chronic PVT has a controversial role. The recommendations for anticoagulation in this setting remain for those with underlying prothrombotic state. The usage of anticoagulation in chronic PVT has been around 30% in most studies. Condat et al111 had given some information on its use in the setting of chronic PVT with no significant bleeding differences from those without anticoagulation. However there was a significant reduction in new thrombotic episodes. A recent retrospective study by Hoekstra et al showed that the use of anticoagulation in pregnancy with chronic PVT had favorable maternal and fetal outcomes for most pregnancies reaching 20 week gestation, however the rate of miscarriage and preterm delivery appeared to be increased when anticoagulated on individual basis.163 Thrombocytosis was a risk factor for unfavorable pregnancy outcome. Variceal bleed occurred in three, all without appropriate primary prophylaxis. No lower limb or mesenteric vein thrombosis occurred during pregnancy or post partum period.163 The study also concluded that recommendations still remain the same even in pregnancy as for other patients.
TIPS
There is a concern for the use of TIPS in the setting of portal vein thrombosis due to the technical reasons of performing TIPS, inability to use in advanced cirrhosis and may hamper transplant later in case of a misplacement. However the use of TIPS in PVT has been studied with possibility of achieving recanalization by disrupting the thrombus and mechanical thrombectomy. The feasibility rate of performing TIPS in PVT ranges between 75 and 100%. Hepatic encephalopathy may be seen in 4–27% and TIPS dysfunction in 20–38% of patients.164 Long term anticoagulation use varies from 11 to 100% due to study designs.164 Studies have shown long term patency rates even without anticoagulation in TIPS, hence routine anticoagulant use may not be recommended after TIPS placement except in those patients with prothrombotic states. In a few cases with PVT, TIPS has been shown to be successful165,166 in treating patients with portal biliopathy and portal vein thrombosis complicating Budd-Chiari syndrome. In 23 of the 28 patients with complete portal vein thrombosis success was achieved in 73% including 6 of 9 patients with cavernomatous transformation.165 Another study on TIPS performed on 15 patients with cirrhosis and PVT leading to refractory ascites, variceal hemorrhage and refractory pleural effusion showed its success in 75% (3/4) patients with cavernomatous transformation and 10/11 (94%) patients with acute PVT with an overall survival of 87%. It may thus be a treatment option in certain patients.167 In chronic PVT (portal cavernoma) TIPS placement has been successful in 35%–80%.168–171 TIPS is unsuccessful if the lumen of thrombosed portal vein is not catheterizable and cavernomatous vein is not amenable to dilatation.
Liver transplant (LT) in portal vein thrombosis
PVT was considered to be a major obstacle to liver transplantation which led to increased surgical complexity and perioperative morbidity and mortality. Following the successful LT in the presence of PVT in 1985, experience has increased in this condition.172 Portal vein thrombosis is associated with greater operative complexity and rethrombosis but has no influence on overall morbidity and mortality.173 Liver transplantation in PVT however has been associated with an increased operative time, transfusion requirements, reintervention and lower survival rate depending on PVT extension.174 Surgical techniques like thrombectomy, thromboendovenectomy with venous reconstitution, interposition of vein graft, portocaval liver transposition have all been done including radiological endovascular interventions to overcome venous obstruction in the recipient.175
The most frequent technique employed is thrombectomy/thromboendovenectomy with end to end donor-recipient portal anastomosis (75%).176 Other techniques that follow are venous jump graft interposition between donor and recipient PV (8.4%), low dissection of PV (5%), portocaval hemitransposition (end to side or end to end, 3.3%), collateral vessel as influx (2.4%), extra anatomic reconstruction involving autologous vessels (1.4%), and arterialization of PV (0.2%). Various classification systems exist for PVT grading in cirrhosis.176 As per Yerdel's grading, for the purpose of liver transplantation PVT has been classified into four grades i.e. Grade 1 PV minimal or partially thrombosed less than 50% of the vessel lumen, Grade 2 more than 50% occlusion of the PV including total occlusion, Grade 3 complete thrombosis of both PV and proximal SMV, Grade 4 complete thrombosis of PV as well as proximal and distal SMV.177 While patients with Grade 1–2 PVT can be adequately managed by terminal to terminal portal vein anastomosis with or without thrombectomy with an advantage that it maintains the portal physiology. Those with Grade 3 PVT in the absence of available distal SMV segments for PV reconstruction, dilated branches of recipient portal venous system could be selected as inflow vessels or anastomosis to the coronary vein can be performed. In the absence of a suitable vein, interposition graft of donor iliac vein may be anastomosed to the SMV. With Grade 4 PVT classic porto-caval hemitransposition is a widely accepted approach, however renoportal anastomosis or anastomosis to the coronary vein or large collateral vessel is also an option. Residual portal hypertension is seen in approximately 50% with the use of portocaval hemitransposition or renoportal anastomosis.176 Overall variceal bleeding risk is 20%, persistent ascites in 58% and renal dysfunction in 26%. In patients with diffuse portal mesenteric vein thrombosis, combined liver intestine transplantation has been advocated.176
Rethrombosis has been reported in 10.3% in the absence of a preventive strategy and it decreases to 6.1% with the utilization of anticoagulation for prevention of rethrombosis in a systematic review. Male sex, prior PVT therapy, Child C class and alcoholic liver disease are the risk factors for recurrence. Intra portal pump use temporarily has also been shown to have reduced rethrombosis rates (7% vs 30%).176
Forty two of the 465 liver transplants have been done at a center with associated PVT. This study found a higher incidence of rethrombosis (7.1% vs 0.9%) and renal failure (16.7% vs 8.5%) because of complex surgical procedure damaging the portal vein thrombosis and prolonged an hepatic phase.177 Liver transplant is indicated in a rare patient to life threatening complications of PVT not manageable conservatively or by shunt surgery as in those with encephalopathy, hypoxia or pulmonary artery hypertension. Outcome in patients with PVT is dependent on the preoperative liver disease severity as patients with a MELD of <15 and PVT had a decreased 1 y survival as compared with those without PVT (57% vs 89%) while those with a MELD >15 and PVT had an equal and slightly better survival vs non-PVT patients (1 y survival 91% vs 75%) with an only slightly increased morbidity.178 Liver transplant has also been reported in a patient with bile duct complications due to cavernoma.179
Portal Vein Thrombosis in special situations
Portal Cholangiopathy
Portal cholangiopathy has been dealt with in detail in a separate issue in the same journal Vol 4 March 2014Ss1-S98-supplement 2.
Portal Vein Obstruction in HCC
HCC is commonly associated with portal vein obstruction. It is associated with worse survival and indicates advanced disease. Advanced stage, higher CTP class, major vessel involvement, low serum albumin and high AFP levels are predictive of PV obstruction in patients with HCC.180 In a study on thrombophilic genetic factors in 94 patients with HCC with & without PV obstruction, the Odds Ratio was 3.85 for MTHFR C6777TT with HCC versus healthy controls. Prothrombin gene G20210A mutation was also more frequent among HCC patients mainly with PV obstruction thereby concluding that all cirrhotics should be looked for thrombophilic genetic factors to individualize patients at risk for PV obstruction in HCC.181 Survival in PV obstruction and HCC has been shown to be better in those with normal AFP.182
Contrast enhanced US (CEUS) has been found to be superior than color Doppler sonography, conventional US, and CT in PV invasion detection and characterization complicating hepatic malignancies.183 In a study CEUS detected tumor invasion in 100% and correctly characterized it in 98% of patients, while CT detected tumor invasion in 68% and correctly characterized it in 68% of them, CEUS may thus be helpful in staging HCC.184
Patients with small HCC and PV obstruction can be safely treated with RFA.185 Similarly Yttrium −90 glass microspheres (Theraspheres) appear to be safe and well tolerated in patients with portal vein obstruction without cavernous transformation.186 Similarly conformal radiotherapy induced a 45.8% objective response rate for PV obstruction in HCC and may be considered an important treatment option.187 Patients with PV obstruction in the setting of HCC has a poor patient outcome. Patients should be assessed preoperatively whether the thrombus is associated with tumor invasion or with stagnant flow. In a study of 12 consecutive patients who underwent liver transplantation for HCC in the setting of PV obstruction 42% had no evident portal vein invasion and only 17% had tumor invasion. Only one third experienced tumor recurrence in first year post transplant and one third became long term survivors (median 36 months) with no evidence of tumor recurrence.187 Radiation therapy is considered to be treatment of choice for selected patients with HCC and PV invasion especially for those with a favorable performance status.188 A recent phase 2 study of Yttrium 90 radioembolization (TARE—trans arterial radioembolization) in intermediate and advanced HCC showed a median survival of 15 months with no significant difference between PV obstruction present or absent.189 However the responders had a significantly higher median survival than non-responders. The median time to progression was 11 months with TARE.190
Conclusion
Portal vein thrombosis is being increasingly recognized in non-cirrhotic, cirrhosis and in malignant conditions like hepatocellular carcinoma. The identification of an underlying hypercoagulable state is possible in more than 80% of cases with rigorous search. The presentation is variable in acute and chronic PVT and imaging helps in differentiating the two different presentations. Doppler ultrasound detects most of the cases adequately however advanced imaging with CT or MRI may be required for defining the extent of thrombosis and planning a shunt surgery. In non-cirrhotic non-malignant acute PVT, anticoagulation remains the mainstay of therapy whereas decompressive shunt surgery like Rex shunt should be offered for cavernomatous (chronic) PVT. The data on anticoagulation use in cirrhosis with acute PVT is convincing with appreciable results and no added bleeding risk, and should be offered to patients especially awaiting liver transplantation. However, lack of consensus on the type of anticoagulant to be used, duration of anticoagulation, monitoring of anticoagulation keeps the research on portal vein thrombosis open for debate and opportunity to work on. TIPS is another option for PVT. Liver transplantation in the expert hands is not affected by the portal vein thrombosis or its extent. The prophylactic role of anticoagulants in preventing PVT needs to be studied.
Conflicts of interest
All authors have none to declare.
References
- 1.Balfour G.W., Stewart T.G. Cases of enlarged spleen complicated with ascites, both depending upon varicose dilatation and thrombosis of the portal vein. Edinb Med J. 1869;14:589–598. [PMC free article] [PubMed] [Google Scholar]
- 2.Okuda K., Ohnishi K., Kimura K. Incidence of portal vein thrombosis in liver cirrhosis. An angiographic study in 708 patients. Gastroenterology. 1985;89:279–286. doi: 10.1016/0016-5085(85)90327-0. [DOI] [PubMed] [Google Scholar]
- 3.Gaiani S., Bolondi L., Li B.S., Zironi G., Siringo S., Barbara L. Prevalence of spontaneous hepatofugal portal flow in liver cirrhosis. Clinical and endoscopic correlation in 228 patients. Gastroenterology. 1991;100:160–167. doi: 10.1016/0016-5085(91)90596-d. [DOI] [PubMed] [Google Scholar]
- 4.Manzanet G., Sanjuan F., Orbis P. Liver transplantation in patients with portal vein thrombosis. Liver Transpl. 2001;7:125–131. doi: 10.1053/jlts.2001.21295. [DOI] [PubMed] [Google Scholar]
- 5.Amitrano L., Guardascione M.A., Brancaccio V. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol. 2004;40:736–741. doi: 10.1016/j.jhep.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Belli L., Romani F., Sansalone C.V., Aseni P., Rondinara G. Portal thrombosis in cirrhotics. A retrospective analysis. Ann Surg. 1986;203:286–291. doi: 10.1097/00000658-198603000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogren M., Bergqvist D., Björck M., Acosta S., Eriksson H., Sternby N.H. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006;12:2115–2119. doi: 10.3748/wjg.v12.i13.2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Denninger M.H., Chaït Y., Casadevall N. Cause of portal or hepatic venous thrombosis in adults: the role of multiple concurrent factors. Hepatology. 2000;31:587–591. doi: 10.1002/hep.510310307. [DOI] [PubMed] [Google Scholar]
- 9.Janssen H.L., Meinardi J.R., Vleggaar F.P. Factor V Leiden mutation, prothrombin gene mutation, and deficiencies in coagulation inhibitors associated with Budd-Chiari syndrome and portal vein thrombosis: results of a case-control study. Blood. 2000;96:2364–2368. [PubMed] [Google Scholar]
- 10.Bombeli T., Basic A., Fehr J. Prevalence of hereditary thrombophilia in patients with thrombosis in different venous systems. Am J Hematol. 2002;70:126–132. doi: 10.1002/ajh.10103. [DOI] [PubMed] [Google Scholar]
- 11.Bhattacharyya M., Makharia G., Kannan M., Ahmed R.P.H., Gupta P.K., Saxena R. Inherited prothrombotic defects in Budd-Chiari syndrome and portal vein thrombosis – a study from north India. Am J Clin Pathol. 2004;121:844–847. doi: 10.1309/F2U1-XBV4-RXYU-AYG0. [DOI] [PubMed] [Google Scholar]
- 12.Primignani M., Martinelli I., Bucciarelli P. Risk factors for thrombophilia in extrahepatic portal vein obstruction. Hepatology. 2005;41:603–608. doi: 10.1002/hep.20591. [DOI] [PubMed] [Google Scholar]
- 13.Turnes J., García-Pagán J.C., González M. Portal hypertension-related complications after acute portal vein thrombosis: impact of early anticoagulation. Clin Gastroenterol Hepatol. 2008;6:1412–1417. doi: 10.1016/j.cgh.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 14.Rosendaal F.R. Venous thrombosis: a multicausal disease. Lancet. 1999;353:1167–1173. doi: 10.1016/s0140-6736(98)10266-0. [DOI] [PubMed] [Google Scholar]
- 15.Janssen H.L., Wijnhoud A., Haagsma E.B. Extrahepatic portal vein thrombosis: aetiology and determinants of survival. Gut. 2001;49:720–724. doi: 10.1136/gut.49.5.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43:167–176. doi: 10.1016/j.jhep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Sogaard K.K., Astrup L.B., Vilstrup H., Gronbaek H. Portal vein thrombosis; risk factors, clinical presentation and treatment. BMC Gastroenterol. 2007;7:34. doi: 10.1186/1471-230X-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Condat B., Valla D. Nonmalignant portal vein thrombosis in adults. Nat Clin Prac Gastroenterol Hepatol. 2006;3:505–515. doi: 10.1038/ncpgasthep0577. [DOI] [PubMed] [Google Scholar]
- 19.Kiladjian J.J., Cervantes F., Leebeek F.W. The impact of JAK2 and MPL mutations on diagnosis and prognosis of splanchnic vein thrombosis: a report on 241 cases. Blood. 2008;111:4922–4929. doi: 10.1182/blood-2007-11-125328. [DOI] [PubMed] [Google Scholar]
- 20.Patel R.K., Lea N.C., Heneghan M.A. Prevalence of the activating JAK2 tyrosine kinase mutation V617F in the Budd-Chiari syndrome. Gastroenterology. 2006;130:2031–2038. doi: 10.1053/j.gastro.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 21.Tefferi A., Thiele J., Orazi A. Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood. 2007;110:1092–1097. doi: 10.1182/blood-2007-04-083501. [DOI] [PubMed] [Google Scholar]
- 22.Valla D., Casadevall N., Huisse M.G. Myeloproliferative disorders in portal vein thrombosis in adults. Gastroenterology. 1998;94:1063–1069. doi: 10.1016/0016-5085(88)90567-7. [DOI] [PubMed] [Google Scholar]
- 23.Hoekstra J., Bresser E.L., Smalberg J.H., Spaander M.C., Leebeek F.W., Janssen H.L. Long-term follow-up of patients with portal vein thrombosis and myeloproliferative neoplasms. J Thromb Haemost. 2011;9:2208–2214. doi: 10.1111/j.1538-7836.2011.04484.x. [DOI] [PubMed] [Google Scholar]
- 24.Smalberg J.H., Arends L.R., Valla D.C., Kiladjian J.J., Janssen H.L.A., Leebeek F.W.G. Myeloproliferative neoplasms in Budd-Chiari syndrome and portal vein thrombosis: a meta-analysis. Blood. 2012;120:4021–4028. doi: 10.1182/blood-2011-09-376517. [DOI] [PubMed] [Google Scholar]
- 25.Qi X., Zhang C., Han G. Prevalence of the JAK2V617F mutation in Chinese patients with Budd-Chiari syndrome and portal vein thrombosis: a prospective study. J Gastroenterol Hepatol. 2012;27:1036–1043. doi: 10.1111/j.1440-1746.2011.07040.x. [DOI] [PubMed] [Google Scholar]
- 26.Qi X., Yang Z., Bai M., Shi X., Han G., Fan D. Meta-analysis: the significance of screening for JAK2V617F mutation in Budd-Chiari syndrome and portal venous system thrombosis. Aliment Pharmacol Ther. 2011;33:1087–1103. doi: 10.1111/j.1365-2036.2011.04627.x. [DOI] [PubMed] [Google Scholar]
- 27.Deepak A., Punamiya S., Patel N., Parekh S., Mehta S., Shah N. Prevalence of JAK29V617F) mutation in intra-abdominal venous thrombosis. Trop Gastroenterol. 2011;32:279–284. [PubMed] [Google Scholar]
- 28.Fisher N.C., Wilde J.T., Roper J., Elias E. Deficiency of natural anticoagulant proteins C, S, and antithrombin in portal vein thrombosis: a secondary phenomenon? Gut. 2000;46:534–539. doi: 10.1136/gut.46.4.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Bruijne E.L., Murad S.D., de Maat M.P., Liver and Thrombosis Study Group Genetic variation in thrombin-activatable fibrinolysis inhibitor (TAFI) is associated with the risk of splanchnic vein thrombosis. Thromb Haemost. 2007;97:181–185. [PubMed] [Google Scholar]
- 30.Martinelli I., Primignani M., Aghemo A. High levels of factor VIII and risk of extra-hepatic portal vein obstruction. J Hepatol. 2009;50:916–922. doi: 10.1016/j.jhep.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 31.D'Amico M., Sammarco P., Pasta L. Thrombophilic genetic factors PAI-1, MTHFRC677T, V Leiden 506Q, and prothrombin 20210A in noncirrhotic portal vein thrombosis and Budd-Chiari syndrome in a caucasian population. Int J Vas Med. 2013;2013:717480. doi: 10.1155/2013/717480. Epub 2013 Dec 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qi X., De Stefano V., Wang J. Prevalence of inherited antithrombin, protein C, and protein S deficiencies in portal vein system thrombosis and Budd-Chiari syndrome: a systematic review and meta-analysis of observational studies. J Gastroenterol Hepatol. 2013;28:432–442. doi: 10.1111/jgh.12085. [DOI] [PubMed] [Google Scholar]
- 33.Mohanty D., Shetty S., Ghosh K., Pawar A., Abraham P. Hereditary thrombophilia as a cause of Budd-Chiari syndrome: a study from Western India. Hepatology. 2001;34:666–670. doi: 10.1053/jhep.2001.27948. [DOI] [PubMed] [Google Scholar]
- 34.Sharma S., Kumar S.I., Poddar U., Yachha S.K., Aggarwal R., Factor V. Leiden and prothrombin gene G20210A mutations are uncommon in portal vein thrombosis in India. Indian J Gastroenterol. 2006;25:236–239. [PubMed] [Google Scholar]
- 35.Koshy A., Jeyakumari M., Factor V. Leiden is not commonly associated with idiopathic portal vein thrombosis in southern India. Indian J Gastroenterol. 2006;25:140–142. [PubMed] [Google Scholar]
- 36.Shah S.R., Dasgupta A., Sharma A., Joshi A., Desai D., Abraham P. Thrombophilic conditions in non cirrhotic portal vein thrombosis. Indian J Gastroenterol. 2005;24:205–210. [PubMed] [Google Scholar]
- 37.Koshy A., Jeyakumari M. High FVIII level is associated with idiopathic portal vein thrombosis in South India. Am J Med. 2007;120 doi: 10.1016/j.amjmed.2006.02.016. 552.e9-11. [DOI] [PubMed] [Google Scholar]
- 38.Liappis A.P., Roberts A.D., Schwartz A.M., Simon G.L. Thrombosis and infection: a case of transient anti-cardiolipin antibody associated with pylephlebitis. Am J Med Sci. 2003;325:365–368. doi: 10.1097/00000441-200306000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Amitrano L., Guardascione M.A., Scaglione M., Menchise A., Romano L., Balzano A. Acute portal and mesenteric thrombosis: unusual presentation of cytomegalovirus infection. Eur J Gastroenterol Hepatol. 2006;18:443–445. doi: 10.1097/00042737-200604000-00021. [DOI] [PubMed] [Google Scholar]
- 40.Condat B., Pessione F., Hillaire S. Current outcome of portal vein thrombosis in adults: risk and benefit of anticoagulant therapy. Gastroenterology. 2001;120:490–497. doi: 10.1053/gast.2001.21209. [DOI] [PubMed] [Google Scholar]
- 41.Poultsides G.A., Lewis W.C., Feld R., Walters D.L., Cherry D.A., Ruby S.T. Portal vein thrombosis after laparoscopic colectomy: thrombolytic therapy via the superior mesenteric vein. Am Surg. 2005;71:856–860. [PubMed] [Google Scholar]
- 42.Bernades P., Baetz A., Lévy P., Belghiti J., Menu Y., Fékété F. Splenic and portal venous obstruction in chronic pancreatitis. A prospective longitudinal study of a medical-surgical series of 266 patients. Dig Dis Sci. 1992;37:340–346. doi: 10.1007/BF01307725. [DOI] [PubMed] [Google Scholar]
- 43.Fujita F., Lyass S., Otsuka K. Portal vein thrombosis following splenectomy: identification of risk factors. Am Surg. 2003;69:951–956. [PubMed] [Google Scholar]
- 44.Bick R.L. Coagulation abnormalities in malignancy: a review. Semin Thromb Hemost. 1992;18:353–372. doi: 10.1055/s-2007-1002575. [DOI] [PubMed] [Google Scholar]
- 45.Plessier A., Darwish-Murad S., Hernandez-Guerra M. Acute portal vein thrombosis unrelated to cirrhosis: a prospective multicenter follow-up study. Hepatology. 2010;51:210–218. doi: 10.1002/hep.23259. [DOI] [PubMed] [Google Scholar]
- 46.Habu D., Nishiguchi S., Shiomi S. Portal vein thrombosis following percutaneous ethanol injection therapy for hepatocellular carcinoma. Indian J Gastroenterol. 2002;21:162–163. [PubMed] [Google Scholar]
- 47.Zheng R.Q., Kudo M., Inui K. Transient portal vein thrombosis caused by radiofrequency ablation for hepatocellular carcinoma. J Gastroenterol. 2003;38:101–103. doi: 10.1007/s005350300015. [DOI] [PubMed] [Google Scholar]
- 48.Matsumoto K., Yamao K., Ohashi K. Acute portal vein thrombosis after EUS-guided FNA of pancreatic cancer: case report. Gastrointest Endosc. 2003;57:269–271. doi: 10.1067/mge.2003.79. [DOI] [PubMed] [Google Scholar]
- 49.Langnas A.N., Marujo W., Stratta R.J., Wood R.P., Shaw B.W., Jr. Vascular complications after orthotopic liver transplantation. Am J Surg. 1991;161:76–82. doi: 10.1016/0002-9610(91)90364-j. [DOI] [PubMed] [Google Scholar]
- 50.Doria C., Marino I.R. Acute portal vein thrombosis secondary to donor/recipient portal vein diameter mismatch after orthotopic liver transplantation: a case report. Int Surg. 2003;88:184–187. [PubMed] [Google Scholar]
- 51.Dörffel T., Wruck T., Rückert R.I., Romaniuk P., Dörffel Q., Wermke W. Vascular complications in acute pancreatitis assessed by color duplex ultrasonography. Pancreas. 2000;21:126–133. doi: 10.1097/00006676-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 52.Murad S.D., Valla D.C., de Groen P.C. Pathogenesis and treatment of Budd-Chiari syndrome combined with portal vein thrombosis. Am J Gastroenterol. 2006;101:83–90. doi: 10.1111/j.1572-0241.2006.00353.x. [DOI] [PubMed] [Google Scholar]
- 53.Anand A.C., Sashindran V.K., Mohan L. Gastrointestinal problems at high altitude. Trop Gastroenterol. 2006;27:147–153. [PubMed] [Google Scholar]
- 54.Yadav S., Dutta A.K., Sarin S.K. Do umbilical vein catheterization and sepsis lead to portal vein thrombosis? A prospective, clinical, and sonographic evaluation. J Pediatr Gastroenterol Nutr. 1993;17:392–396. doi: 10.1097/00005176-199311000-00010. [DOI] [PubMed] [Google Scholar]
- 55.Sakha S.H., Rafeey M., Tarzamani M.K. Portal venous thrombosis after umbilical vein catheterization. Indian J Gastroenterol. 2007;26:283–284. [PubMed] [Google Scholar]
- 56.Giraudo G., Greget M., Oussoultzoglou E., Rosso E., Bachellier P., Jaeck D. Preoperative contralateral portal vein embolisation before major hepatic resection is a safe and efficient procedure: a large single institution experience. Surgery. 2008;143:476–482. doi: 10.1016/j.surg.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 57.Stringer M.D., Heaton N.D., Karani J. Patterns of portal vein occlusion and their etiological significance. Br J Surg. 1994;81:1328–1331. doi: 10.1002/bjs.1800810923. [DOI] [PubMed] [Google Scholar]
- 58.Odievre M., Pige G., Alagille D. Congenital abnormalities associated with extraheptic portal hypertension. Arch Dis Child. 1977;52:383–385. doi: 10.1136/adc.52.5.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pinto R.B., Silveira T.R., Bandenilli E., Rohsig L. Portal vein thrombosis in children and adolescents: the low prevalence of hereditary thrombophilic disorders. J Pediatr Surg. 2004;39:1356–1361. doi: 10.1016/j.jpedsurg.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 60.Amitrano L., Brancaccio V., Guardascione M.A., Margaglione M., Iannaccone L., D'Andrea G. Inherited coagulation disorders in cirrhotic patients with portal vein thrombosis. Hepatology. 2000;31:345–348. doi: 10.1002/hep.510310213. [DOI] [PubMed] [Google Scholar]
- 61.Mangia A., Villani M.R., Cappucci G. Causes of portal venous thrombosis in cirrhotic patients: the role of genetic and acquired factors. Eur J Gastroenterol Hepatol. 2005;17:745–751. doi: 10.1097/00042737-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 62.Erkan O., Bozdayi A.M., Disibeyaz S., Oguz D., Ozcan M., Bahar K. Thrombophilic gene mutations in cirrhotic patients with portal vein thrombosis. Eur J Gastroenterol Hepatol. 2005;17:339–343. doi: 10.1097/00042737-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 63.Zocco M.A., Di Stasio E., De Cristofaro R. Thrombotic risk factors in patients with liver cirrhosis: correlation with MELD scoring system and portal vein thrombosis development. J Hepatol. 2009;51:682–689. doi: 10.1016/j.jhep.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 64.Maruyama H., Okugawa H., Takahashi M., Yokosuka O. De novo portal vein thrombosis in virus-related cirrhosis: predictive factors and long-term outcomes. Am J Gastroenterol. 2013;108:568–574. doi: 10.1038/ajg.2012.452. [DOI] [PubMed] [Google Scholar]
- 65.Amitrano L., Brancaccio V., Guardascione M.A. Portal vein thrombosis after variceal endoscopic sclerotherapy in cirrhotic patients: role of genetic thrombophilia. Endoscopy. 2002;34:535–538. doi: 10.1055/s-2002-33210. [DOI] [PubMed] [Google Scholar]
- 66.Malkowski P., Pawlak J., Michalowicz B., Szczerban J., Wroblewski T., Leowska E. Thrombolytic treatment of portal thrombosis. Hepatogastroenterology. 2003;50:2098–2100. [PubMed] [Google Scholar]
- 67.Poddar U., Thapa B.R., Rao K.L., Singh K. Etiological spectrum of esophageal varices due to portal hypertension in Indian children: is it different from the West? J Gastroenterol Hepatol. 2008;23:1354–1357. doi: 10.1111/j.1440-1746.2007.05102.x. [DOI] [PubMed] [Google Scholar]
- 68.Valla D.C., Condat B., Lebrec D. Spectrum of portal vein thrombosis in the West. J Gastroenterol Hepatol. 2002;17:S224–S227. doi: 10.1046/j.1440-1746.17.s3.4.x. [DOI] [PubMed] [Google Scholar]
- 69.Rangari M., Gupta R., Jain M., Malhotra V., Sarin S.K. Hepatic dysfunction in patients with extrahepatic portal venous obstruction. Liver Int. 2003;23:434–439. doi: 10.1111/j.1478-3231.2003.00879.x. [DOI] [PubMed] [Google Scholar]
- 70.Arora N.K., Lodha R., Gulati S. Portal hypertension in north Indian children. Indian J Pediatr. 1998;65:585–591. doi: 10.1007/BF02730901. [DOI] [PubMed] [Google Scholar]
- 71.Mehrotra R.N., Batia V., Dabadghao P., Yachha S.K. Extrahepatic portal vein obstruction in children: anthropometry, growth hormone, and insulin-like growth factor I. J Pediatr Gastroenterol Nutr. 1997;25:520–523. doi: 10.1097/00005176-199711000-00006. [DOI] [PubMed] [Google Scholar]
- 72.Nihal N., Bapat M.R., Rathi P. Relation of insulin like growth factor-1 and insulin-like growth factor binding protein-3 levels to growth retardation in extrahepatic portal vein obstruction. Hepatol Int. 2009;3:305–309. doi: 10.1007/s12072-008-9102-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ganguly S., Sarin S.K., Bhatia V., Lahoti D. The prevalence and spectrum of colonic lesions in patients with cirrhotic and noncirrhotic portal hypertension. Hepatology. 1995;21:1226–1231. [PubMed] [Google Scholar]
- 74.Chawla Y., Dilawari J.B. Gall Bladder varices in portal vein thrombosis. AJR. 1994;162:643–645. doi: 10.2214/ajr.162.3.8109513. [DOI] [PubMed] [Google Scholar]
- 75.de Ville de Goyet J., Alberti D., Falchetti D. Treatment of extrahepatic portal hypertension in children by mesenteric-to-left portal vein bypass: a new physiological procedure. Eur J Surg. 1999;165:777–781. doi: 10.1080/11024159950189573. [DOI] [PubMed] [Google Scholar]
- 76.Bellomo-Brandao M.A., Morcillo A.M., Hessel G., Cardoso S.R., Servidoni Mde F., da Corta Pinto E.A. Growth assessment in children with extrahepatic portal vein obstruction and portal hypertension. Ar Gastro. 2003;40:247–250. doi: 10.1590/s0004-28032003000400009. [DOI] [PubMed] [Google Scholar]
- 77.Minguez B., Garcia-Pagan J.C., Bosch J. Noncirrhotic portal vein thrombosis exhibits neuropsychological and MR changes consistent with minimal hepatic encephalopathy. Hepatology. 2006;43:707–714. doi: 10.1002/hep.21126. [DOI] [PubMed] [Google Scholar]
- 78.Dilawari J.B., Chawla Y. Pseudoscleoring cholangitis in extrahepatic portal venous obstruction. Gut. 1992;33:272–276. doi: 10.1136/gut.33.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khuroo M.S., Yattoo G.N., Zasyar S.A. Biliary abnormalities associated with extrahepatic portal venous obstruction. Hepatology. 1993;17:807–813. [PubMed] [Google Scholar]
- 80.Dhiman R.K., Puri D., Chawla Y. Biliary changes in extrahepatic portal venous obstruction compression by collaterals or ischemia? Gastrointest Endosc. 1999;50:646–652. doi: 10.1016/s0016-5107(99)80013-3. [DOI] [PubMed] [Google Scholar]
- 81.Condat B., Vilgram V., Asselak T. Portal cavernoma associated cholangiopathy a clinical and MR cholangiography coupled with MR portography imaging study. Hepatology. 2003;37:1302–1308. doi: 10.1053/jhep.2003.50232. [DOI] [PubMed] [Google Scholar]
- 82.Malkhan G.H., Bhatia S.T., Bastin K. Cholangiography associated with portal hypertension diagnostic evaluation and clinical implications. Gastroint Endos. 1999;49:344–348. doi: 10.1016/s0016-5107(99)70011-8. [DOI] [PubMed] [Google Scholar]
- 83.Sezgin O., Oguz D., Attritas E., Saritas U., Sahin B. Endoscopic management of biliary obstruction carried by cavernous transformation of portal vein. Gastroint Endos. 2003;58:602–608. doi: 10.1067/s0016-5107(03)01975-8. [DOI] [PubMed] [Google Scholar]
- 84.Kocher G., Himmelmann A. Portal vein thrombosis (PVT): a study of 20 non-cirrhotic cases. Swiss Med Wkly. 2005;135:372–376. doi: 10.4414/smw.2005.11035. [DOI] [PubMed] [Google Scholar]
- 85.Kobayashi S., Ng C.S., Kazama T. Hemodynamic and morphological changes after portal vein embolisation: different efforts central and peripheral zones in the liver on multiphasic computed tomography. J Comput Assist Tomog. 2004;28:804–810. doi: 10.1097/00004728-200411000-00013. [DOI] [PubMed] [Google Scholar]
- 86.Vilgrain V., Condat B., Bureau C. Atrophy-hypertrophy complex in patients with cavernous transformation of the portal vein: CT evaluation. Radiology. 2006;241:149–155. doi: 10.1148/radiol.2411051102. [DOI] [PubMed] [Google Scholar]
- 87.Bilodeau M., Aubry M.C., Houle R., Burnes P.N., Ethier C. Evaluation of hepatocytes injury following partial ligation of the left portal vein. J Hepatol. 1999;30:29–37. doi: 10.1016/s0168-8278(99)80005-1. [DOI] [PubMed] [Google Scholar]
- 88.Van Gansbeke D., Avni E.F., Delcour C., Engelholm L., Struyven J. Sonographic features of portal vein thrombosis. AJR Am J Roentgenol. 1985;144:749–752. doi: 10.2214/ajr.144.4.749. [DOI] [PubMed] [Google Scholar]
- 89.Wang J.T., Zhao H.Y., Liu Y.L. Portal vein thrombosis. Hepatobiliary Pancreat Dis Int. 2005;4:515–518. [PubMed] [Google Scholar]
- 90.Tessler F.N., Gehring B.J., Gomes A.S. Diagnosis of portal vein thrombosis: value of color Doppler imaging. AJR Am J Roentgenol. 1991;157:293–296. doi: 10.2214/ajr.157.2.1853809. [DOI] [PubMed] [Google Scholar]
- 91.Parvey H.R., Eisenberg R.L., Giyanani V., Krebs C.A. Duplex sonography of the portal venous system: pitfalls and limitations. Am J Roentgenol. 1989;152:765–770. doi: 10.2214/ajr.152.4.765. [DOI] [PubMed] [Google Scholar]
- 92.Lai L., Brugge W.R. Endoscopic ultrasound is a sensitive and specific test to diagnose portal venous system thrombosis (PVST) Am J Gastroenterol. 2004;99:40–44. doi: 10.1046/j.1572-0241.2003.04020.x. [DOI] [PubMed] [Google Scholar]
- 93.Palazzo l, Hochain P., Helmer C. Biliary varices on endoscopic ultrasonography: clinical presentation ad outcome. Endoscopy. 2000;32:520–524. doi: 10.1055/s-2000-9009. [DOI] [PubMed] [Google Scholar]
- 94.Umpheren J.L., Pecha R.E., Urayama S. Biliary stricture caused by portal biliopathy. Diagnosis by EUS with Doppler US. Gastrointest Endosc. 2004;60:1021–1024. doi: 10.1016/s0016-5107(04)02216-3. [DOI] [PubMed] [Google Scholar]
- 95.Chawla A., Dewan R., Sarin S.K. The frequency and influence of gall bladder varices on gall bladder function in patients with portal hypertension. Am J Gastroenterol. 1995;90:2011–2014. [PubMed] [Google Scholar]
- 96.Parvey H.R., Raval B., Sandler C.M. Portal vein thrombosis: imaging findings. Am J Roentgenol. 1994;162:77–81. doi: 10.2214/ajr.162.1.8273695. [DOI] [PubMed] [Google Scholar]
- 97.Lee H.K., Park S.J., Yi B.H., Yeon E.K., Kim J.H., Hong H.S. Portal vein thrombosis: CT features. Abdom Imaging. 2008;33:72–79. doi: 10.1007/s00261-007-9200-x. [DOI] [PubMed] [Google Scholar]
- 98.Shah T.U., Semelka R.C., Voultsinos V. Accuracy of magnetic resonance imaging for preoperative detection of portal vein thrombosis in liver transplant candidates. Liver Transpl. 2006;12:1682–1688. doi: 10.1002/lt.20873. [DOI] [PubMed] [Google Scholar]
- 99.Cakmak O., Elmas N., Tamsel S. Role of contrast-enhanced 3D magnetic resonance portography in evaluating portal venous system compared with color Doppler ultrasonography. Abdom Imaging. 2008;33:65–71. doi: 10.1007/s00261-007-9229-x. [DOI] [PubMed] [Google Scholar]
- 100.Smith C.S., Sheehy N., McEniff N., Keogan M.T. Magnetic resonance portal venography: use of fast-acquisition true FISP imaging in the detection of portal vein thrombosis. Clin Radiol. 2007;62:1180–1188. doi: 10.1016/j.crad.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 101.Lin J., Zhou K.R., Chen Z.W., Wang J.H., Wu Z.Q., Fan J. Three-dimensional contrast-enhanced MR angiography in diagnosis of portal vein involvement by hepatic tumors. World J Gastroenterol. 2003;9:1114–1118. doi: 10.3748/wjg.v9.i5.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Glockner J.F., Forauer A.R., Solomon H., Varma C.R., Perman W.H. Three-dimensional gadolinium enhanced MR angiography of vascular complications after liver transplantation. Am J Roentgenol. 2000;174:1447–1453. doi: 10.2214/ajr.174.5.1741447. [DOI] [PubMed] [Google Scholar]
- 103.Vlachogiannakos J., Patch D., Watkinson A., Tibballs J., Burroughs A.K. Carbon-dioxide portography: an expanding role? Lancet. 2000;355:987–988. doi: 10.1016/s0140-6736(00)99020-2. [DOI] [PubMed] [Google Scholar]
- 104.Kreft B., Strunk H., Flacke S. Detection of thrombosis in the portal venous system: comparison of contrast-enhanced MR angiography with intraarterial digital subtraction angiography. Radiology. 2000;216:86–92. doi: 10.1148/radiology.216.1.r00jl2386. [DOI] [PubMed] [Google Scholar]
- 105.Sun L., Guan Y.S., Pan W.M. Highly metabolic thrombus of the portal vein: 18F fluorodeoxyglucose positron emission tomography/computer tomography demonstration and clinical significance in hepatocellular carcinoma. World J Gastroenterol. 2008;14:1212–1217. doi: 10.3748/wjg.14.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dilawari J.B., Chawla Y.K., Raju G.S., Kaur U., Bambery P. Splenoportovenography in portal hypertension: a safe outpatient procedure. Can Assoc Radiol J. 1990;41:146–148. [PubMed] [Google Scholar]
- 107.Sarin S.K., Lahoti D., Saxena S.P., Murthy N.S., Makwana U.K. Prevalence, classification and natural history of gastric varices: a long-term follow up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–1349. doi: 10.1002/hep.1840160607. [DOI] [PubMed] [Google Scholar]
- 108.Webster G.J., Burroughs A.K., Riordan S.M. Review article: portal vein thrombosis – new insights into aetiology and management. Aliment Pharmacol Ther. 2005;21:1–9. doi: 10.1111/j.1365-2036.2004.02301.x. [DOI] [PubMed] [Google Scholar]
- 109.DeLeve L.D., Valla D.C., Garcia-Tsao G. Vascular disorders of the liver. Hepatology. 2009;49:1729–1764. doi: 10.1002/hep.22772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Baril N., Wren S., Radin R., Ralla P., Stain S. The role of anticoagulation in pylephlebitis. Am J Surg. 1996;172:449–452. doi: 10.1016/S0002-9610(96)00220-6. [DOI] [PubMed] [Google Scholar]
- 111.Condat B., Pessine T., Helene D.M., Hillaire S., Valla D. Recent portal or mesenteric venous thrombosis, increased recognition and frequent recanalisation on anticoagulant therapy. Hepatology. 2000;32:466–470. doi: 10.1053/jhep.2000.16597. [DOI] [PubMed] [Google Scholar]
- 112.Kumar S., Sarr M.G., Kamath P.S. Mesenteric venous thrombosis. N Engl J Med. 2001;345:1683–1688. doi: 10.1056/NEJMra010076. [DOI] [PubMed] [Google Scholar]
- 113.Voorhees A.B., Jr., Price J.B., Jr. Extrahepatic portal hypertension. A retrospective analysis of 127 cases and associated clinical implications. Arch Surg. 1974;108:338–341. doi: 10.1001/archsurg.1974.01350270068012. [DOI] [PubMed] [Google Scholar]
- 114.Amitrano L., Guardascione M.A., Scaglione M. A. Prognostic factors in noncirrhotic patients with splanchnic vein thromboses. Am J Gastroenterol. 2007;102:2464–2470. doi: 10.1111/j.1572-0241.2007.01477.x. [DOI] [PubMed] [Google Scholar]
- 115.Thomas V., Jose T., Kumar S. Natural history of bleeding after esophageal variceal eradication in patients with extrahepatic portal venous obstruction; a 20-year follow-up. Indian J Gastroenterol. 2009;28:206–211. doi: 10.1007/s12664-009-0086-0. [DOI] [PubMed] [Google Scholar]
- 116.Luca A., Caruso S., Milazzo M. Natural course of extrahepatic nonmalignant partial portal vein thrombosis in patients with cirrhosis. Radiology. 2012;265:124–132. doi: 10.1148/radiol.12112236. [DOI] [PubMed] [Google Scholar]
- 117.Hall T.C., Garcea G., Metcalfe M., Bilku D., Dennison A.R. Management of acute non cirrhotic non malignant portal vein thrombosis: a systematic review. World J Surg. 2011;35:2510–2520. doi: 10.1007/s00268-011-1198-0. [DOI] [PubMed] [Google Scholar]
- 118.Romano F., Caprotti R., Conti M. Thrombosis of the splenoportal axis after splenectomy. Langenbecks Arch Surg. 2006;391:483–488. doi: 10.1007/s00423-006-0075-z. [DOI] [PubMed] [Google Scholar]
- 119.Sheen C.L., Lamparelli H., Milne A., Green I., Ramage J.K. Clinical features, diagnosis and outcome of acute portal vein thrombosis. Q J Med. 2000;93:531–534. doi: 10.1093/qjmed/93.8.531. [DOI] [PubMed] [Google Scholar]
- 120.Dolorich L.R., Ginsberg J.S., Douketis J.D., Holbrook A.M., Cheah G. A meta analysis comparing low molecular wt heparin with unfractionated heparin in treatment of venous thrombolism examining some unanswered questions regarding location of treatment product use and dosing frequency. Arch Int Med. 2000;160:181–188. doi: 10.1001/archinte.160.2.181. [DOI] [PubMed] [Google Scholar]
- 121.Francoz C., Belghiti J., Vilgrain V. Splanchnic vein thrombosis in candidates for liver transplantation: usefulness of screening and anticoagulation. Gut. 2005;54:691–697. doi: 10.1136/gut.2004.042796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Louvet A., Texier F., Dharancy S. Anticoagulation therapy may sense biliary abnormalities due to acute portal thrombosis. Dig Dis Sci. 2006;51:11–17. doi: 10.1007/s10620-006-3075-5. [DOI] [PubMed] [Google Scholar]
- 123.Spaander M.C., Hoekstra J., Hansen B.E., Van Buuren H.R., Leebeek F.W., Jansenn H.L. Anticoagulant therapy in patients with non-cirrhotic portal vein thrombosis: effect on new thrombotic events and gastrointestinal bleeding. J Thromb Haemost. 2013;11:452–459. doi: 10.1111/jth.12121. [DOI] [PubMed] [Google Scholar]
- 124.Lopeia J.E., Correa G., Brazzini A. Percutaneous transhepatic treatment of symptomatic mesenteric venous thrombosis. J Vasc Surg. 2002;36:1058–1067. doi: 10.1067/mva.2002.127526. [DOI] [PubMed] [Google Scholar]
- 125.Aytekin C., Boyvat F., Kurt A., Yologlu Z., Coskun M. Catheter directed thrombolysis with transjugular access in portal vein thrombosis secondary to pancreatitis. Eur J Radiol. 2001;39:80–82. doi: 10.1016/s0720-048x(01)00289-3. [DOI] [PubMed] [Google Scholar]
- 126.Hollingshead M., Burke C.T., Mauro M.A., Weeks S.M., Dixon R.G., Jaques P.F. Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Inter Radiol. 2005;16:651–661. doi: 10.1097/01.RVI.0000156265.79960.86. [DOI] [PubMed] [Google Scholar]
- 127.Kercher K.W., Sing R.F., Watson K.W., Matthews B.D., LeQuire M.H., Heniford B.T. Transhepatic thrombolysis in acute portal vein thrombosis after laproscopic splenectomy. Sung Laproso Endo Percutan Tech. 2002;12:131–136. doi: 10.1097/00129689-200204000-00013. [DOI] [PubMed] [Google Scholar]
- 128.Henao E.A., Bohamon W.T., Silva M.B., Jr. Treatment of portal vein thrombosis with relative superior mesenteric artery infusion of recombinant tissue plasminogen activator. J Vase Surg. 2003;38:1411–1415. doi: 10.1016/s0741-5214(03)01052-8. [DOI] [PubMed] [Google Scholar]
- 129.Tateishi A., Mitsui M., Oki T. Extensive mesenteric vein and portal vein thrombosis significantly treated by thrombosis and anticoagulation. J Gastroenterol Hepatol. 2001;16:1429–1433. doi: 10.1046/j.1440-1746.2001.02557.x. [DOI] [PubMed] [Google Scholar]
- 130.Liu F.Y., Wang M.Q., Fan Q.S., Duan F., Wang Z.J., Song P. Interventional treatment for symptomatic acute-subacute portal and superior mesenteric venous thrombosis. World J Gastro. 2009;15:5028–5034. doi: 10.3748/wjg.15.5028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wang M.Q., Liu F.Y., Duan F., Wang Z.J., Song P., Fan Q.S. Acute symptomatic mesenteric venous thrombosis: treatment by catheter directed thrombolysis with transjugular intrahepatic route. Abdom Imaging. 2011;36:390–398. doi: 10.1007/s00261-010-9637-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Smalberg J.H., Spaander M.V., Jie K.S., Pattynama P.M., van Buuren H.R. Risks and benefits of transcatheter thrombolytic therapy in patients with splanchnic venous thrombosis. Thromb Haemost. 2008;100:1084–1088. [PubMed] [Google Scholar]
- 133.Fonseca A.L., Cleary M.A., Cholewczynski W., Sumpio B.E., Atweh N.A. Omental vein catheter thrombolysis for acute porto-mesenteric vein thrombosis. Ann Vasc Surg. 2013;27 doi: 10.1016/j.avsg.2012.09.009. 497.e1–4. [DOI] [PubMed] [Google Scholar]
- 134.Luo J., Yan Z., Wang J., Liu Q., Qu X. Endovascular treatment for nonacute symptomatic portal venous thrombosis through intrahepatic portosystemic shunt approach. J Vasc Interv Radiol. 2011;22:61–69. doi: 10.1016/j.jvir.2010.07.028. [DOI] [PubMed] [Google Scholar]
- 135.Uflacher R. Applications of percutaneous mechanical thromboectomy in transjugular intrahepatic portosystemic shunt and portal vein thrombosis. Tech Vas Inter Radiol. 2003;6:59–69. doi: 10.1053/tvir.2003.36433. [DOI] [PubMed] [Google Scholar]
- 136.Oğuzkurt P., Tercan F., Ince E., Ezer S.S., Hiçsönmez A. Percutaneous treatment of portal vein thrombosis in a child who has undergone splenectomy. J Pediatr Surg. 2008;43:e29–32. doi: 10.1016/j.jpedsurg.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 137.Ferro C., Rossi C.G., Bovio G., Dahamane M., Centenaro M. Transjugular intrahepatic portosystemic shunt, mechanical aspiration thrombectomy, and direct thrombolysis in the treatment of acute portal and superior mesenteric vein thrombosis. Cardiovas Interv Radiol. 2007;30:1070–1074. doi: 10.1007/s00270-007-9137-z. [DOI] [PubMed] [Google Scholar]
- 138.Adani G.L., Baccarani U., Risaliti A. Percutaneous transhepatic portography for the treatment of early portal vein thrombosis after surgery. Cardiovasc Interv Radiol. 2007;30:1222–1226. doi: 10.1007/s00270-007-9056-z. [DOI] [PubMed] [Google Scholar]
- 139.Amitrano L., Guardascione M.A., Menchise A. Safety and efficacy of anticoagulation therapy with low molecular weight heparin for portal vein thrombosis in patients with liver cirrhosis. J Clin Gastroenterol. 2010;44:448–451. doi: 10.1097/MCG.0b013e3181b3ab44. [DOI] [PubMed] [Google Scholar]
- 140.Senzolo M., Ferronato C., Burra P., Sartori M.T. Anticoagulation for portal vein thrombosis in cirrhotic patients should be always considered. Intern Emerg Med. 2009;4:161–162. doi: 10.1007/s11739-008-0219-y. [DOI] [PubMed] [Google Scholar]
- 141.Pellicelli A.M., Guarascio P., D'Ambrosio C. Portal vein thrombosis in cirrhotic patients: safety and efficacy of low dosage of enoxaparin. J Hepatol. 2010;52:S80. [Google Scholar]
- 142.Werner K.T., Sando S., Carey E.J. Portal vein thrombosis in patients with end stage liver disease awaiting liver transplantation: outcome of anticoagulation. Dig Dis Sci. 2013;58:1776–1780. doi: 10.1007/s10620-012-2548-y. [DOI] [PubMed] [Google Scholar]
- 143.Delgado M.G., Seijo S., Yepes I. Efficacy and safety of anticoagulation on patients with cirrhosis and portal vein thrombosis. Clin Gastroenterol Hepatol. 2012;10:776–783. doi: 10.1016/j.cgh.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 144.Senzolo M., M Sartori T., Rossetto V. Prospective evaluation of anticoagulation and transjugular intrahepatic portosystemic shunt for the management of portal vein thrombosis in cirrhosis. Liver Int. 2012;32:919–927. doi: 10.1111/j.1478-3231.2012.02785.x. [DOI] [PubMed] [Google Scholar]
- 145.Martinez M., Tandra A., Vuppalanchi R. Treatment of acute portal vein thrombosis by non-traditional anticoagulation. Hepatology. 2014 Jan 7 doi: 10.1002/hep.26998. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 146.Pannach S., Babatz J., Beyer-Westendorf J. Successful treatment of acute portal vein thrombosis with rivaroxaban. Thromb Haemost. 2013;110:626–627. doi: 10.1160/TH13-05-0407. [DOI] [PubMed] [Google Scholar]
- 147.De Santis A., Moscatelli R., Catalano C., Iannetti A., Gigliotti F., Cristofari F. Systemic thrombolysis of portal vein thrombosis in cirrhotic patients: a pilot study. Dig Liver Dis. 2010;42:451–455. doi: 10.1016/j.dld.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 148.Villa E., Cammà C., Marietta M., Luongo M., Critelli R., Colopi S. Enoxaparin prevents portal vein thrombosis and liver decompensation in patients with advanced cirrhosis. Gastroenterology. 2012;143:1253–1260. doi: 10.1053/j.gastro.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 149.Brearley S., Hawker P.C., Dykes P.W., Keighley M.R. A lethal complication of peripheral vein vasopressin infusion. Hepatogastroenterology. 1985;32:224–225. [PubMed] [Google Scholar]
- 150.Celińska-Cedro D., Teisseyre M., Woynarowski M., Socha P., Socha J., Ryzko J. Endoscopic ligation of esophageal varices for prophylaxis of first bleeding in children and adolescents with portal hypertension: preliminary results of a prospective study. J Pediatr Surg. 2003;38:1008–1011. doi: 10.1016/s0022-3468(03)00181-7. [DOI] [PubMed] [Google Scholar]
- 151.Spaander M.C., Murad S.D., van Buuren H.R., Hansen B.E., Kuipers E.J., Janssen H.L. Endoscopic treatment of esophagogastric variceal bleeding in patients with noncirrhotic extrahepatic portal vein thrombosis: a long-term follow-up study. Gastrointest Endosc. 2008;67:821–827. doi: 10.1016/j.gie.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 152.Poddar U., Thapa B.R., Singh K. Band ligation plus sclerotherapy versus sclerotherapy alone in children with extrahepatic portal venous obstruction. J Clin Gastroenterol. 2005;39:626–629. doi: 10.1097/01.mcg.0000170765.36825.66. [DOI] [PubMed] [Google Scholar]
- 153.Dilawari J.B., Raju G.S., Chawla Y.K. Development of large spleno-adrenorenal shunt after endoscopic sclerotherapy. Gastroenterology. 1989;97:421–426. doi: 10.1016/0016-5085(89)90078-4. [DOI] [PubMed] [Google Scholar]
- 154.Orr D.W., Harrison P.M., Devlin J. Chronic mesenteric venous thrombosis: evaluation and determinants of survival during long-term follow-up. Clin Gastroenterol Hepatol. 2007;5:80–86. doi: 10.1016/j.cgh.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 155.Wolff M., Hirner A. Current state of portosystemic shunt surgery. Langenbecks Arch Surg. 2003;388:141–149. doi: 10.1007/s00423-003-0367-5. [DOI] [PubMed] [Google Scholar]
- 156.Livingstone A.S., Koniaris L.G., Perez E.A., Alvarez N., Levi J.U., Hutson D.G. 507 Warren-Zeppa distal splenorenal shunts: a 34-year experience. Ann Surg. 2006;243:884–892. doi: 10.1097/01.sla.0000219681.08312.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sharma B.C., Singh R.P., Chawla Y.K. Effect of shunt surgery on spleen size, portal pressure and oesophageal varices in patients with non-cirrhotic portal hypertension. J Gastroenterol Hepatol. 1997;12:582–584. doi: 10.1111/j.1440-1746.1997.tb00489.x. [DOI] [PubMed] [Google Scholar]
- 158.Dasgupta R., Roberts E., Superina R.A., Kim P.C. Effectiveness of Rex shunt in the treatment of portal hypertension. J Pediatr Surg. 2006;41:108–112. doi: 10.1016/j.jpedsurg.2005.10.059. [DOI] [PubMed] [Google Scholar]
- 159.Krebs-Schmitt D., Briem-Richter A., Grabhorn E. Effectiveness of Rex shunt in children with portal hypertension following liver transplantation or with primary portal hypertension. Pediatr Transpl. 2009;13:540–544. doi: 10.1111/j.1399-3046.2008.01109.x. [DOI] [PubMed] [Google Scholar]
- 160.Query J.A., Sandler A.D., Sharp W.J. Use of autogenous saphenous vein as a conduit for mesenterico-left portal vein bypass. J Pediatr Surg. 2007;42:1137–1140. doi: 10.1016/j.jpedsurg.2007.01.066. [DOI] [PubMed] [Google Scholar]
- 161.Kim H.B., Pomposelli J.J., Lillehei C.W. Mesogonadal shunts for extrahepatic portal vein thrombosis and variceal hemorrhage. Liver Transpl. 2005;11:1389–1394. doi: 10.1002/lt.20487. [DOI] [PubMed] [Google Scholar]
- 162.Shaw B.W., Jr., Iwatsuki S., Bron K., Starzl T.E. Portal vein grafts in hepatic transplantation. Surg Gynecol Obstet. 1985;161:66–68. [PMC free article] [PubMed] [Google Scholar]
- 163.Hoekstra J., Seijo S., Rautou P.E. Pregnancy in women with portal vein thrombosis: results of a multicentric European study on maternal and fetal management and outcome. J Hepatol. 2012;57:1214–1219. doi: 10.1016/j.jhep.2012.07.034. [DOI] [PubMed] [Google Scholar]
- 164.Francoz C., Valla D., Durand F. Portal vein thrombosis, cirrhosis, and liver transplantation. J Hepatol. 2012;57:203–212. doi: 10.1016/j.jhep.2011.12.034. [DOI] [PubMed] [Google Scholar]
- 165.Bilbao J.I., Elorz M., Vivas I., Martínez-Cuesta A., Bastarrika G., Benito A. Transjugular intrahepatic portosystemic shunt (TIPS) in the treatment of venous symptomatic chronic portal thrombosis in non-cirrhotic patients. Cardiovasc Interv Radiol. 2004;27:474–480. doi: 10.1007/s00270-004-0241-z. [DOI] [PubMed] [Google Scholar]
- 166.Van Ha T.G., Hodge J., Funaki B. Transjugular intrahepatic portosystemic shunt placement in patients with cirrhosis and concomitant portal vein thrombosis. Cardiovasc Interv Radiol. 2006;29:785–790. doi: 10.1007/s00270-005-0090-4. [DOI] [PubMed] [Google Scholar]
- 167.Superina R., Shneider B., Emre S., Sarin S., de Ville de Goyet J. Surgical guidelines for the management of extra-hepatic portal vein obstruction. Pediatr Transpl. 2006;10:908–913. doi: 10.1111/j.1399-3046.2006.00598.x. [DOI] [PubMed] [Google Scholar]
- 168.Luo X., Nie L., Zhou B. Transjugular intrahepatic portosystemic shunt for the treatment of portal hypertension in noncirrhotic patients with portal cavernoma. Gastroenterol Res Pract. 2014;2014:659726. doi: 10.1155/2014/659726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Qi X., Han G., Yin Z. Transjugular intrahepatic portosystemic shunt for portal cavernoma with symptomatic portal hypertension in non-cirrhotic patients. Dig Dis Sci. 2012;57:1072–1082. doi: 10.1007/s10620-011-1975-5. [DOI] [PubMed] [Google Scholar]
- 170.Han G., Qi X., He C. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J Hepatol. 2011;54:78–88. doi: 10.1016/j.jhep.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 171.Fanelli F., Angeloni S., Salvatori F.M. Transjugular intrahepatic portosystemic shunt with expanded-polytetrafuoroethylene-covered stents in non-cirrhotic patients with portal cavernoma. Dig Liver Dis. 2011;43:78–84. doi: 10.1016/j.dld.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 172.Lladó L., Fabregat J., Castellote J. Management of portal vein thrombosis in liver transplantation: influence on morbidity and mortality. Clin Transpl. 2007;2:716–721. doi: 10.1111/j.1399-0012.2007.00728.x. [DOI] [PubMed] [Google Scholar]
- 173.Lendoire J., Raffin G., Cejas N. Liver transplantation in adult patients with portal vein thrombosis: risk factors, management and outcome. HPB (Oxford) 2007;9:352–356. doi: 10.1080/13651820701599033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Harmanci O., Bayraktar Y. Portal hypertension due to portal venous thrombosis: etiology, clinical outcomes. World J Gastroenterol. 2007;13:2535–2540. doi: 10.3748/wjg.v13.i18.2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yerdel M.A., Gunson B., Mirza D. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management and outcome. Transplantation. 2000;69:1873–1881. doi: 10.1097/00007890-200005150-00023. [DOI] [PubMed] [Google Scholar]
- 176.Rodriguez-Castro K.I., Porte R.J., Nadal E., Germani G., Burra P., Senzolo M. Management of non neoplastic portal vein thrombosis in the setting of liver transplantation: a systematic review. Transplantation. 2012;94:1145–1153. doi: 10.1097/TP.0b013e31826e8e53. [DOI] [PubMed] [Google Scholar]
- 177.Tao Y.F., Teng F., Wang Z.X. Liver transplant recipients with portal vein thrombosis: a single center retrospective study. Hepatobiliary Pancreat Dis Int. 2009;8:34–39. [PubMed] [Google Scholar]
- 178.Doenecke A., Tsui T.Y., Zuelke C. Pre-existent portal vein thrombosis in liver transplantation: influence of pre-operative disease severity. Clin Transpl. 2010;24:48–55. doi: 10.1111/j.1399-0012.2009.00977.x. [DOI] [PubMed] [Google Scholar]
- 179.Hajdu C.H., Murakami T., Diflo T. Intrahepatic portal cavernoma as an indication for liver transplantation. Liver Transpl. 2007;13:1312–1316. doi: 10.1002/lt.21243. [DOI] [PubMed] [Google Scholar]
- 180.Connolly G.C., Chen R., Hyrien O. Incidence, risk factors and consequences of portal vein and systemic thromboses in hepatocellular carcinoma. Thromb Res. 2008;122:299–306. doi: 10.1016/j.thromres.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.D'Amico M., Pasta L., Sammarco P. MTHFR C677TT, PAI1 4G-4G, V Leiden Q506, and prothrombin G20210A in hepatocellular carcinoma with and without portal vein thrombosis. J Thromb Thrombolysis. 2009;28:70–73. doi: 10.1007/s11239-008-0246-6. [DOI] [PubMed] [Google Scholar]
- 182.Carr B.I., Buch S.C., Kondragunta V., Pancoska P., Branch R.A. Tumor and liver determinants of prognosis in unresectable hepatocellular carcinoma: a case cohort study. J Gastroenterol Hepatol. 2008;23:1259–1266. doi: 10.1111/j.1440-1746.2008.05487.x. [DOI] [PubMed] [Google Scholar]
- 183.Rossi S., Rosa L., Ravetta V. Contrast-enhanced versus conventional and color Doppler sonography for the detection of thrombosis of the portal and hepatic venous systems. Am J Roentgenol. 2006;186:763–773. doi: 10.2214/AJR.04.1218. [DOI] [PubMed] [Google Scholar]
- 184.Rossi S., Ghittoni G., Ravetta V. Contrast-enhanced ultrasonography and spiral computed tomography in the detection and characterization of portal vein thrombosis complicating hepatocellular carcinoma. Eur Radiol. 2008;18:1749–1756. doi: 10.1007/s00330-008-0931-z. [DOI] [PubMed] [Google Scholar]
- 185.Neeman Z., Libutti S.K., Patti J.W., Wood B.J. Percutaneous radiofrequency ablation of hepatocellular carcinoma in the presence of portal vein thrombosis. Clin Imaging. 2003;27:417–420. doi: 10.1016/S0899-7071(03)00015-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Salem R., Lewandowski R., Roberts C. Use of yttrium-90 glass microspheres (TheraSphere) for the treatment of unresectable hepatocellular carcinoma in patients with portal vein thrombosis. J Vasc Interv Radiol. 2004;15:335–345. doi: 10.1097/01.rvi.0000123319.20705.92. [DOI] [PubMed] [Google Scholar]
- 187.Kulik L.M., Carr B.I., Mulcahy M.F. Safety and efficacy of 90Y radiotherapy for hepatocellular carcinoma with and without portal vein thrombosis. Hepatology. 2008;47:71–81. doi: 10.1002/hep.21980. [DOI] [PubMed] [Google Scholar]
- 188.Sotiropoulos G.C., Radtke A., Schmitz K.J. Liver transplantation in the setting of hepatocellular carcinoma and portal vein thrombosis: a challenging dilemma? Dig Dis Sci. 2008;53:1994–1999. doi: 10.1007/s10620-007-0099-4. [DOI] [PubMed] [Google Scholar]
- 189.Huang Y.J., Hsu H.C., Wang C.Y. The treatment responses in cases of radiation therapy to portal vein thrombosis in advanced hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2009;73:1155–1163. doi: 10.1016/j.ijrobp.2008.06.1486. [DOI] [PubMed] [Google Scholar]
- 190.Mazzaferro V., Sposito C., Bhoori S. Ytterium-90 radioembolization for intermediate-advanced hepatocellular carcinoma: a phase 2 study. Hepatology. 2013;57:1826–1837. doi: 10.1002/hep.26014. [DOI] [PubMed] [Google Scholar]


