Abstract
Aim:
The aim of this study is to highlight the development of pyogenic granuloma and hemangioma after the placement of dental implants.
Materials and Methods:
A literature search was performed using MEDLINE, accessed via the National Library of Medicine PubMed Interface, for articles published between 2000 and 2014 in English, relating to the occurrence of pyogenic granuloma or hemangioma in relation to dental implants.
Results:
Our search identified only four case reports of pyogenic granuloma and hemangioma related to dental implants as reported in the English literature.
Conclusion:
Placement of dental implants can cause development of pyogenic granuloma and hemangioma, indicating that placement of dental implants requires well-trained specialists with perfect skills in dental implantology. Furthermore, the critical selection of the appropriate case is of paramount importance to avoid the occurrence of such complications.
Keywords: Dental implant, hemangioma, pyogenic granuloma
INTRODUCTION
Dental implantation is considered as one of the most widely employed procedures in dental practice, as most of dental implants are manufactured with the osseointegrated biocompatible titanium material. However, some complications correlated with dental implants may occur, resulting in peri-implantitis and failure of the implant. These complications may include dental plaque, inadequate oral hygiene, anatomical drawbacks, and traumatic occlusion.[1] Moreover, some factors such as chronic inflammation and corrosion of the implant fixture surface may cause chronic irritation process and act as contributing factors to these pathogenic conditions.[2]
Pyogenic granuloma is an example of the inflammatory hyperplasias that may occur in the oral cavity. Although its name implies infection, this condition has no relation to the infection either clinically or histopathologically. It usually arises in response to a variety of stimuli, like hormonal factors, local irritation of low grade, or traumatic injury. From a clinical view, pyogenic granuloma appears as a smooth or lobulated exophytic mass with red erythematous papules on a pedunculated or sessile base, with the tendency for bleeding.[3] It can be treated with different modalities, such as surgical excision, which is the best method, as well as using Nd: YAG laser, flash lamp pulsed dye laser, intra-lesional injection of ethanol or corticosteroids, cryosurgery, and sodium tetradecyl sulfate sclerotherapy.[4]
Hemangioma commonly occurs in neonates and children. Based on the size of vascular spaces and histology, it can be of cavernous or capillary type.[5] Postoperative hematoma formation or bleeding can be induced by administration of antithrombotic therapy.[2] There is only one report about the relationship between this condition and dental implant.[2]
MATERIALS AND METHODS
A literature search was carried out from August to September 2014 using MEDLINE, accessed via the National Library of Medicine PubMed Interface (http://www.ncbi.nlm.nih.gov/pubmed), for articles published in English relating to the occurrence of pyogenic granuloma or hemangioma with dental implants. We used the following search strings: Pyogenic granuloma and dental implants, hemangioma and dental implants, relationship between pyogenic granuloma and dental implants, relationship between hemangioma and dental implants, pyogenic granuloma and hemangioma and their relation to dental implants. The search was limited to articles published between 2000 and 2014. We also used the “related article feature” of PubMed to identify further references of interest within the primary search. These references were obtained, and their bibliographies and pertinent secondary references were also identified and acquired. This process was repeated until no further new articles could be identified. The abstracted literature was reviewed. Several publications were excluded as they did not meet the inclusion criteria.
Inclusion criterion
All evaluated studies should involve the occurrence of pyogenic granuloma or hemangioma or both of them in relation to the dental implant placement.
Exclusion criterion
All studies that do not support the occurrence of pyogenic granuloma or hemangioma or both in relation to dental implant placement were excluded.
RESULTS
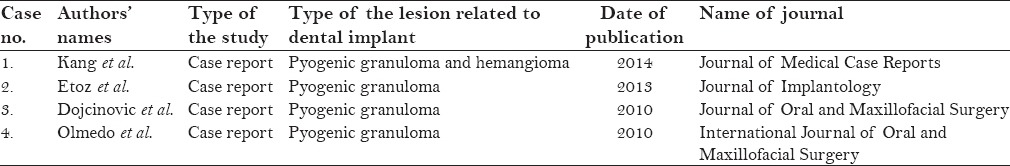
Only four articles related to the occurrence of pyogenic granuloma and hemangioma after the placement of dental implants were identified in the English literature. All these articles were case reports. One of these cases reported the coexistence of pyogenic granuloma and hemangioma in the same case, while the other three cases only reported pyogenic granuloma. Results are summarized in Table 1.
Table 1.
Publications from 2000 to 2014 on occurrence of pyogenic granuloma or hemangioma in relation to dental implants
DISCUSSION
One of the important key factors in the success of dental implants is the condition of the oral soft tissue. Some complications may occur around the implant, such as fistula formation, mucositis, dehiscence, gingival inflammation and hyperplasia, as well peri-implantitis.[6] These complications have many causative factors like poor oral hygiene, long-term irritation, and loose fitting of abutment screw or framework leading to gap formation. Furthermore, it may be caused by a corrosion of the fixture surface and metal particles of the implant.[1]
Gingivitis and gingival hyperplasia represent the most common soft tissue complications of dental implants, and have been reported in about 1–30% of cases.[6,7,8,9,10] They may result from incorrect choice of implant parts, like healing caps, abutments that are too close to each other or too short, thus favoring the formation of dead spaces under superstructures. Furthermore, the loss of attached mucosa and correct alignment of implants are contributing factors. All of these factors usually hinder the right oral hygienic procedures in dental implant patients.[11]
A rare form of these complications is the occurrence of pyogenic granuloma or hemangioma in relation to dental implant, but case reports about these conditions are still limited.
The site of occurrence of pyogenic granuloma is either extraoral or intraoral. The favorable site of pyogenic granuloma in the oral cavity is the gingiva (60–70%), followed by the lip (14%), tongue (9%), buccal mucosa (7%), and palate (2%).[12,13] The exact cause is not clearly identified; however, it might be attributed to trauma, bad oral hygiene, low-grade irritation, and dental plaque. As pyogenic granuloma is a reactive lesion, it will regress after the removal of the stimulating factor.[11]
We identified only four published articles (case reports) reporting the occurrence of pyogenic granuloma or hemangioma in association with dental implant. Olmedo et al.[1] reported two cases of reactive lesions related to dental implant; one case was diagnosed histopathologically as pyogenic granuloma, while the other one was peripheral giant cell granuloma. The authors stated that the presence of metal-like particles within the tissues has a role in the corrosion process of the metal component of the implant, which may give an account on the etiology of the lesion. They proposed that macrophages will engulf these metal particles, stimulating the cytokines’ release, which play a role in bone reabsorption by osteoclast activation and suppression of osteoblast function, thus reducing the bone formation, leading to osteolysis.[14,15] These metal particles can be created during the steps of implant placement procedures, such as implant insertion and abutment connection, or in case of removal of failed implants.[14,16]
Dojcinovic et al.[11] identified a case with pyogenic granuloma related to dental implant. They stated that about 30–50% of patients with pyogenic granuloma have been subjected to local trauma. The main causative factor in most of these cases was related to poor oral hygiene. In their reported case, they clarified that the implant was stable, but the incorrect choice of healing cap allowed the accumulation of dental plaque, which led to chronic gingivitis and peri-implantitis, facilitating the development of pyogenic granuloma. So, the authors concluded that it was important to choose a healing cap that corresponds to the size of the implant used.
Etöz et al.[17] identified a case of pyogenic granuloma associated with placement of dental implant. They clarified that the development of pyogenic granuloma may result from gap formation due to splitting procedure, which was used in the implant surgery, between the alveolar bone and the implant. Also, they added that the trauma from antagonist dentition with lack of adequate keratinized mucosa may allow the entrapment of soft tissue between the implant and the alveolar bone, which may be responsible for the development of pyogenic granuloma.
Kang et al.[2] reported a case under warfarin antithrombotic therapy. Patient history showed intermittent bleeding and a dome-shaped overgrowing mass in the upper alveolar ridge. Histopathologic report showed the co-existence of pyogenic granuloma and capillary hemangioma in relation to dental implant. So, they stated that the use of antithrombotic therapy with the presence of chronic inflammation around the implant had led to formation of pyogenic granuloma and neovascularization.[18,19] However, antithrombotic agents like heparin or warfarin are used as an augmentation treatment in cancer therapy due to their anti-angiogenic property in tumors, as they bind to angiogenic growth factors such as fibroblast growth factors and vascular endothelial growth factors, which inhibit angiogenesis.[20] This contradictory point needs further investigations. This is the first case in the literature with co-existence of pyogenic granuloma and hemangioma in relation to dental implant in the same case. They recommended that patients with dental implants who have chronic peri-implantitis under anti-thrombotic therapy should be followed for a long period of time to ensure early detection of the oral mucosal abnormalities.
Pyogenic granuloma can be treated with variety of treatment options such as surgical removal, cryotherapy, electro-cauterization, laser applications,[21] and steroid injections.[22]
We have noticed in the updated literature that the development of pyogenic granuloma and hemangioma after placement of dental implants has different causes or etiological factors such as poor oral hygiene, chronic irritation, presence of dead space around dental implant, metal corrosion of implant surface, inappropriate choice of implant abutments or healing caps, local trauma, inadequate available soft tissues, and the use of antithrombotic therapy that allows frequent bleeding.
CONCLUSION
Placement of dental implants can cause development of pyogenic granuloma and hemangioma, indicating that placement of dental implants requires well-trained specialists with perfect skills in dental implantology. Furthermore, the critical selection of the appropriate case is of paramount importance to avoid the occurrence of such complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Olmedo DG, Paparella ML, Brandizzi D, Cabrini RL. Reactive lesions of peri-implant mucosa associated with titanium dental implants: A report of 2 cases. Int J Oral Maxillofac Surg. 2010;39:503–7. doi: 10.1016/j.ijom.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Kang YH, Byun JH, Choi MJ, Lee JS, Jang JH, Kim YI, et al. Co-development of pyogenic granuloma and capillary hemangioma on the alveolar ridge associated with a dental implant: A case report. J Med Case Rep. 2014;8:192. doi: 10.1186/1752-1947-8-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: A review. J Oral Sci. 2006;48:167–75. doi: 10.2334/josnusd.48.167. [DOI] [PubMed] [Google Scholar]
- 4.Ichimiya M, Yoshikawa Y, Hamamoto Y, Muto M. Successful treatment of pyogenic granuloma with injection of absolute ethanol. J Dermatol. 2004;31:342–4. doi: 10.1111/j.1346-8138.2004.tb00682.x. [DOI] [PubMed] [Google Scholar]
- 5.Dilsiz A, Aydin T, Gursan N. Capillary hemangioma as a rare benign tumor of the oral cavity: A case report. Cases J. 2009;2:8622. doi: 10.4076/1757-1626-2-8622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent. 1999;81:537–52. doi: 10.1016/s0022-3913(99)70208-8. [DOI] [PubMed] [Google Scholar]
- 7.Tolman DE, Laney WR. Tissue-integrated prosthesis complications. Int J Oral Maxillofac Implants. 1992;7:477–84. [PubMed] [Google Scholar]
- 8.Wyatt CC, Zarb GA. Treatment outcomes of patients with implant-supported fixed partial prostheses. Int J Oral Maxillofac Implants. 1998;13:204–11. [PubMed] [Google Scholar]
- 9.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 10.Wennerberg A, Jemt T. Complications in partially edentulous implant patients: A 5-year retrospective follow-up study of 133 patients supplied with unilateral maxillary prostheses. Clin Implant Dent Relat Res. 1999;1:49–56. doi: 10.1111/j.1708-8208.1999.tb00091.x. [DOI] [PubMed] [Google Scholar]
- 11.Dojcinovic I, Richter M, Lombardi T. Occurrence of a pyogenic granuloma in relation to a dental implant. J Oral Maxillofac Surg. 2010;68:1874–6. doi: 10.1016/j.joms.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 12.Bhaskar SN, Jacoway JR. Pyogenic granuloma-clinical features, incidence, histology, and result of treatment: Report of 242 cases. J Oral Surg. 1966;24:391–8. [PubMed] [Google Scholar]
- 13.Angelopoulos AP. Pyogenic granuloma of the oral cavity: Statistical analysis of its clinical features. J Oral Surg. 1971;29:840–7. [PubMed] [Google Scholar]
- 14.Cohen J. Current concepts review. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am. 1998;80:1554. [PubMed] [Google Scholar]
- 15.Urban RM, Jacobs JJ, Tomlinson MJ, Gavrilovic J, Black J, Peoc’h M. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82:457–76. doi: 10.2106/00004623-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Flatebø RS, Johannessen AC, Grønningsaeter AG, Bøe OE, Gjerdet NR, Grung B, et al. Host response to titanium dental implant placement evaluated in a human oral model. J Periodontol. 2006;77:1201–10. doi: 10.1902/jop.2006.050406. [DOI] [PubMed] [Google Scholar]
- 17.Etoz OA, Soylu E, Kiliç K, Günhan Ö, Akcay H, Alkan A. A reactive lesion (pyogenic granuloma) associated with dental implant: A case report. J Oral Implantol. 2013;39:733–6. doi: 10.1563/AAID-JOI-D-11-00166. [DOI] [PubMed] [Google Scholar]
- 18.Tözüm TF, Sençimen M, Ortakoğlu K, Ozdemir A, Aydin OC, Keleş M. Diagnosis and treatment of a large periapical implant lesion associated with adjacent natural tooth: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e132–8. doi: 10.1016/j.tripleo.2005.11.029. [DOI] [PubMed] [Google Scholar]
- 19.McGuff HS, Heim-Hall J, Holsinger FC, Jones AA, O’Dell DS, Hafemeister AC. Maxillary osteosarcoma associated with a dental implant: Report of a case and review of the literature regarding implant-related sarcomas. J Am Dent Assoc. 2008;139:1052–9. doi: 10.14219/jada.archive.2008.0307. [DOI] [PubMed] [Google Scholar]
- 20.Folkman J, Langer R, Linhardt RJ, Haudenschild C, Taylor S. Angiogenesis inhibition and tumor regression caused by heparin or a heparin fragment in the presence of cortisone. Science. 1983;221:719–25. doi: 10.1126/science.6192498. [DOI] [PubMed] [Google Scholar]
- 21.White JM, Chaudhry SI, Kudler JJ, Sekandari N, Schoelch ML, Silverman S., Jr Nd: YAG and CO2 laser therapy of oral mucosal lesions. J Clin Laser Med Surg. 1998;16:299–304. doi: 10.1089/clm.1998.16.299. [DOI] [PubMed] [Google Scholar]
- 22.Parisi E, Glick PH, Glick M. Recurrent intraoral pyogenic granuloma with satellitosis treated with corticosteroids. Oral Dis. 2006;12:70–2. doi: 10.1111/j.1601-0825.2005.01158.x. [DOI] [PubMed] [Google Scholar]


