Abstract
Aim:
To investigate the possible effects of preoperative oral Midazolam on parental separation anxiety, emergence delirium, and post-anesthesia care unit time on children undergoing dental rehabilitation under general anesthesia.
Methods:
Randomized, prospective, double-blind study. Seventy-eight American Society of Anesthesiology (ASA) I children were divided into two groups of 39 each. Children of the first group were premedicated with oral Midazolam 0.5 mg/kg, while children of the control group were premedicated with a placebo. Scores for parental separation, mask acceptance, postoperative emergence delirium, and time spent in the post-anesthesia care unit were compared statistically.
Results:
The test group showed significantly lower parental separation scores and high acceptance rate for anesthetic mask. There was no significant difference between the two groups regarding emergence delirium and time spent in post-anesthesia care unit.
Conclusions:
Preoperative oral Midazolam could be a useful adjunct in anxiety management for children suffering dental anxiety. The drug may not reduce the incidence of postoperative emergence delirium. The suggested dose does not seem to affect the post-anesthesia care unit time.
Keywords: Child dentistry, dental rehabilitation, general anesthesia
INTRODUCTION
Addressing child anxiety during medical procedures is a growing trend and dental treatment is not an exception.[1] In today's dentistry, parents and caregivers may not be contented with some non-pharmacological behavior management techniques such as voice control, hand over mouth, and intimidation.[2] When treating a child with limited cooperation margin due to fear or anxiety, the use of physical restraining might not result in a satisfactory outcome, especially if the child is in need of comprehensive dental treatment which may necessitate the use of general anesthesia. Physical restraining in the dental office affects the image of the pediatric dentist and may harm the self-respect of the child at a very young stage of psychological development not to mention the legal implications of harming a vulnerable human being.[3] Dental General Anesthesia (DGA) might save the child from the psychic trauma he/she might get in the dental office and may help deliver better quality of dental treatment; however, when a pediatric dentist decides to expose his/her patient to the calculated risk of general anesthesia, the decision should not substitute psychic trauma in the dental office with another psychic trauma in the operating theater in the form of parental separation anxiety with the added psychic trauma of physical restraining during induction of anesthesia. A survey conducted by Homer and Bass in 2010[4] showed that up to 60% of anesthetists frequently use physical restraints on resistant and fearful children.
In 2009, Sheta and AlSarheed[5] studied the anxiolytic effect of different doses of Midazolam on 60 children aged 2–6 years undergoing DGA. They reported that satisfactory anxiolytic effect can be achieved with higher doses which raised the potential risk of some adverse effects.
In 2011, Mountain et al.[6] conducted a study to compare the effects of Midazolam versus Dexmedetomidine premedication on preoperative anxiety and postoperative emergence delirium (ED) on 41 children aged 1–6 years and concluded that the latter has an advantage of reducing the incidence of postoperative ED.
The uniqueness of dental situation where children are already suffering dental fear with substantial need for dental treatment added to the fear of operating room atmosphere merits more investigation on the topic on a larger scale.
The aim of this work was, therefore, to investigate the possible effect of preoperative oral Midazolam given to children undergoing full dental rehabilitation under general anesthesia (DGA), on parental separation anxiety, ease of anesthesia induction, ED, and post-anesthesia care unit time (PACUT).
MATERIALS AND METHODS
Study design
The flow chart of the study design is given in Figure 1. This study used a randomized, prospective, double-blinded design and was conducted on children undergoing full dental rehabilitation under general anesthesia in a Joint Commission for International Accreditation (JCIA) accredited private hospital in Jeddah, Saudi Arabia during 2012.
Figure 1.
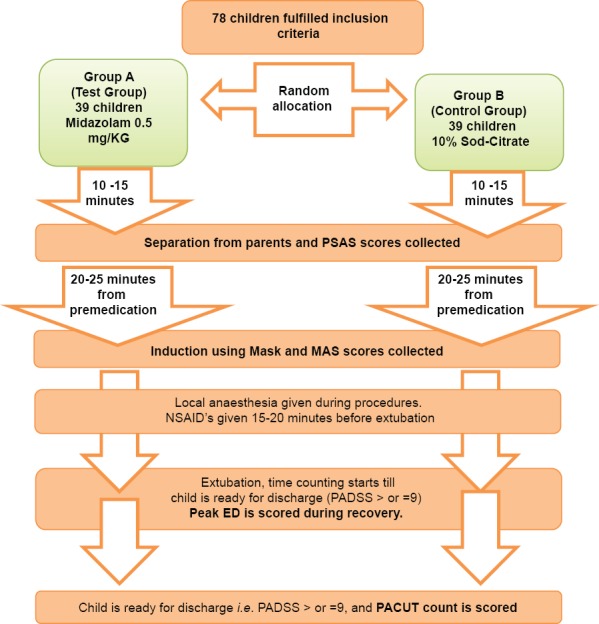
Flow chart of the study design
Ethical consents
Institutional ethical approval of the concerned committees based on the hospital's Corporate Social Responsibility (CSR) standards was obtained. Informed consents were obtained from parents or guardians following JCIA standards and complying with the World Medical Association's Declaration of Helsinki on ethical principles for medical research involving human subjects, October 2001.[7]
Inclusion criteria
Healthy, American Society of Anesthesiology (ASA) I children who underwent DGA due to lack of cooperative behavior to a degree that might impact the quality of dental treatment and/or due to the extensive amount of needed dental procedures were selected.
Exclusion criteria
Children excluded from the study were those with history of allergy to Midazolam (none were detected), history of post-anesthesia ED, children with ASA scores greater than I, and children with special needs whenever their condition was thought to affect their pre- or postoperative behavior.
Procedures
Seventy-eight children fulfilled the criteria for inclusion and their guardians agreed to participate in the study. Children were randomly allocated to two groups. Group A, the intervention group, consisted of 39 children who were premedicated with 0.5 mg/kg (maximum total dose was 20 mg) of oral Midazolam (Dormicum®; Roche, Brussels, Belgium) in 20 ml of 10% sodium citrate solution, 30 min prior to induction.[8] Children of the control group, group B (39 children), were premedicated with 20 ml of plain 10% sodium citrate solution. Premedication was done 10–15 min prior to separation from parents and 20–25 min prior to intubation, by a blinded anesthesia assistant.
Sampling and standardization
A child undergoing DGA was to be interviewed 1 or 2 days prior to the operation day for preoperative anesthesia assessment by an anesthetist. During these interviews, the anesthetist randomly allocated the children to one of the two groups using the stratified random selection method. With the aid of a biostatistician, some alterations were made to ensure that the two groups had no statistically significant demographic differences.
Anesthesia protocol
Same anesthesia protocol was applied on both groups. Children were not allowed to eat or drink for at least 6 h before the procedure. Induction was carried out via a facemask with 8% Sevoflurane (Abbott Co. North Chicago, Illinois, USA) in 100% oxygen. After loss of consciousness, an intravenous line was established through which Propofol (Diprivan®; AstraZeneca Co. London, UK.) was administered to allow nasotracheal intubation. Anesthesia was maintained with 2–3% Sevoflurane® in a mixture of oxygen and nitrous oxide. All children were nasally intubated to allow the pediatric dentist to check occlusion. An oropharyngeal pack was inserted to prevent aspiration of water and dental material fragments into the patient's airway. Intraligamental local anesthesia was administered prior to extractions and steel crown insertions, while intrapulpal route was used for pulpotomies in order to help control physiologic pain reaction during the procedure.[9] With the exception of three asthmatic children, all children were given approximately 1–2 mg/kg diclofenac sodium (Voltaren®; Novartis Pharmaceuticals Basel, Switzerland) in the form of 12.5 or 25 mg suppositories 15 min before extubation to help reduce postoperative pain.[10]
Study tools
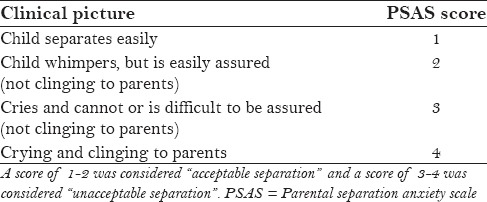
Parental Separation Anxiety Scale (PSAS) [Table 1], developed by Dashiff and Weaver[11] and validated by Mountain et al.[6] and Kaviani et al.,[12] was used. It is a 4-point scale; a PSAS score of 1–2 was considered “acceptable separation” and a score of 3–4 was considered an “unacceptable separation.”
Table 1.
Parental separation anxiety scale
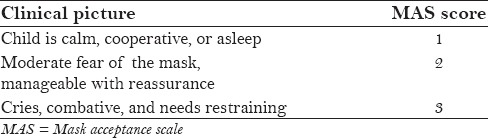
Ease of induction was assessed using a 3-point Mask Acceptance Scale (MAS) adopted by Akin et al.[13] [Table 2].
Table 2.
Mask acceptance scale
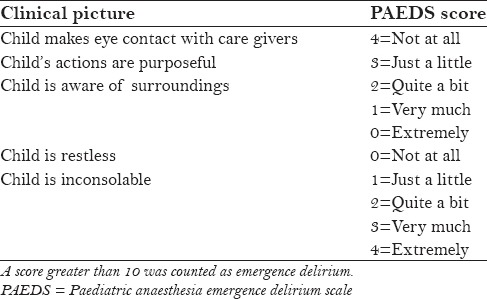
Paediatric Anaesthesia Emergence Delirium Scale (PAEDS) [Table 3], developed by Sikich and Lerman in 2004[14] and validated by Pieters et al.,[15] Mountain et al.,[6] and Shung,[16] was used to assess ED. Out of 20 points, a score greater than 10 was counted as ED. Scoring for PAEDS was done at the peak of the ED episode.
Table 3.
Paediatric anaesthesia emergence delirium scale
Research team members were trained on data collection and scoring for each tool. Scoring was done by two independent and blinded members of the team. No differences were recorded between the two.
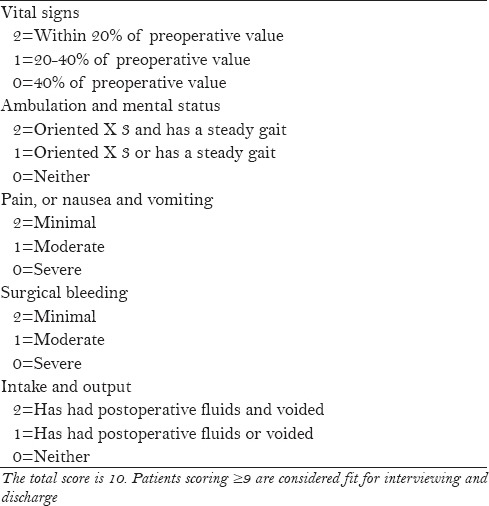
PACUT was defined in this study as the time elapsed from the moment of extubation till the blinded anesthesia assistant considered the child ready for discharge. A patient was considered ready for discharge when his/her Post Anaesthesia Discharge Scoring System (PADSS) equalled 9 or higher[17] [Table 4].
Table 4.
Post anaesthesia discharge scoring system
Statistical methods
Collected data were transferred to a Microsoft Excel file. The two groups were statistically compared using Excel's data analysis tool pack. Demographic data, mask acceptance (MAS), and PACUT for the two groups were compared using Student's t-test for comparison of sample means. A preliminary F test for comparison of sample variances was performed to determine the appropriate t-test variant to use, according to whether the sample variances were found to be equal. A “P” value less than 0.05 was considered significant.
The statistical test used for comparison of PSAS and PAEDS was Pearson Chi-squared test. The level of significance was set at P = 0.05 for that test.
RESULTS
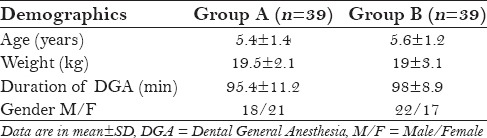
A total of 78 children were included in the study; their ages ranged from 34 to 102 months. There was no statistical difference found between the study and control groups regarding age, weight, gender, and duration of anesthesia, indicating that both study group and control group were comparable [Table 5].
Table 5.
Demographic and operative data compared
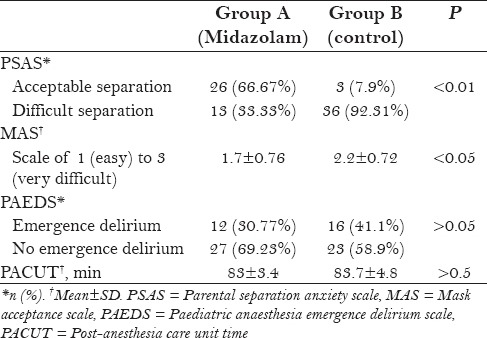
Parental separation scores (PSAS) were significantly lower in group A. Twenty-six children (66.67%) in group A showed acceptable separation from parents, compared to 3 children (7.9%) in group B (P < 0.01). Acceptance of anesthesia mask was significantly observed in group A as well (P < 0.05). However, there was a lower score for postoperative ED in group A, but the difference was not of statistical significance (P > 0.05). Mean PACUT for each group was found to be around 83 min, with no statistical difference found between the two groups (P > 0.05) [Table 6].
Table 6.
Study variables compared
DISCUSSION
The current study demonstrates that Midazolam in a dose of 0.5 mg/kg is an effective adjunct in managing preoperative dental anxiety and in facilitating induction of general anesthesia, but it failed to reduce the incidence of ED. The results are in agreement with those of Sheta and AlSarheed,[5] Mountain et al.,[6] and Kaviani et al.[12]
The time spent in the operating room holding area prior to surgery is often traumatic to children's psychology,[18] especially for children who already suffer dental fear. This may contribute to extreme anxiety during the induction of anesthesia. In 1999, Kain et al.[19] demonstrated that extreme preoperative anxiety is associated with the occurrence of negative postoperative behavioral changes. The lack of effect on postoperative ED may appear contradictory to Kain et al.'s report;[19] however, they demonstrated that reducing preoperative anxiety does reduce the incidence of postoperative behavioral changes, but not postoperative ED. Our study does support this conclusion and may resolve the controversy on the effect of Midazolam on postoperative ED.
Points of strength in the current study worth noting are related to the randomization process, double blinding, and the implementation of updated study tools (scales) that were relatedly validated by several authors and standardized for ease of reproduction in further studies.
An optimal dosage of Midazolam based on a balance between safety and efficacy in pediatric dentistry has not been well established. The current study is in agreement with Mountain et al.'s[6] report that a dose of 0.5 mg/kg significantly reduces preoperative anxiety and helps in anesthetic mask acceptance by children. They compared Midazolam to Dexmedetomidine as preoperative anxiolytic medications and reported that the latter has an advantage of reducing postoperative ED. However, the current study was limited to Midazolam because till now, the US Food and Drug Administration has not approved the use of Dexmedetomidine for children. Other studies[5,20] demonstrated a better anxiolytic outcome with higher doses of Midazolam up to 1.0 mg/kg. However, in the current study being done in a private hospital, a decision was made to adhere to Midazolam manufacturer's recommended dose of 0.5 mg/kg. It is worth noting that while using this dose, no adverse effects that might be attributed to the drug were observed among children of the study group. In 1992, McMillan et al.[21] reported no beneficial effect using higher doses of 0.75 mg/kg and 1.0 mg/kg compared to 0.5 mg/kg. They also reported more side effects with higher doses, such as prolonged postoperative recovery time and undue over sedation. The potential for adverse effects is a major concern regarding routine preoperative medication. Consequently, before suggesting routine use of Midazolam premedication, more studies on a larger scale are recommended to identify patients who might not benefit from Midazolam preoperative medication. In that context, Finley et al.[22] demonstrated that Midazolam has no anxiolytic effect on children with impulsive temperament.
In the current study, the time selected to separate the child from his/her parents was 10–15 min after Midazolam administration. This was guided by Levine et al.[23] who reported that 10 min after premedication was the minimum time needed for smooth separation from parents. The same authors reported that the peak sedative effect of Midazolam was achieved 20–30 min after administration; consequently, the peak-effect time was reserved for induction time which was 20–25 min in our study.
On using the PAEDS to assess postoperative emergence delirium, no favorable effect of oral Midazolam on postoperative ED was found in our study. Although the PAEDS used in the study is reported to be the most comprehensive and validated scale currently available to measure ED, it lacks an appropriate cut-off value to actually diagnose ED,[15] which might be considered a limitation of the study. However, it might be worth noting that dental surgeries constituted 52% of the number of surgeries included during the development of the scale by Sikich and Lerman.[14] Other limitations may be related to the study being conducted in a private hospital where due to medico-legal concerns, we had to stick to Midazolam manufacturer's dose recommendation and avoid including higher doses in the study. Another limitation is that the study did not include assessment of the possible effect of Midazolam on postoperative behavior due to certain factors confined to the Saudi and Gulf communities where parents are not necessarily the primary child care givers. To conduct such a study, the researcher would rely on the primary care giver as a source of information. In Saudi Arabia and Gulf countries, the primary care giver might be a recruited domestic helper or a step mother in addition to the biological mother, which may render obtaining such information unreliable, especially in an environment that restricts inter-gender communication. Further studies are needed to investigate the possible effect of the drug on long-term postoperative child's behavior and toward testing new agents that might have an effect on postoperative ED and PACUT. Such investigations may lead to adopting routine practices that may render dental anesthesia costs more affordable by parents and insurance companies as well.
Many agents have been tested to flavor oral Midazolam, including orange juice, cola drinks, and pomegranate juice. The current study is in agreement with Isik et al.'s[8] report that adding 10% sodium citrate solution to Midazolam enjoys high acceptance by children, as in our study only one child in the test group (A) was reported to resist the intake of the drug due to its taste.
CONCLUSION
Effective management of preoperative dental anxiety is an essential part of pediatric dental treatment under general anesthesia
Oral preoperative Midazolam in a dose of 0.5 mg/kg might be a useful treatment adjunct in reducing parental separation anxiety, for anesthetic mask acceptance, and for ease of anesthesia induction
Preoperative Midazolam sedation has no reducing effect on postoperative ED in children undergoing dental treatment under general anesthesia
The time spent in the post-anesthesia care unit does not seem to be affected by the use of preoperative Midazolam in a dose of 0.5 mg/kg.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Al-Jundi SH, Mahmood AJ. Factors affecting preoperative anxiety in children undergoing general anaesthesia for dental rehabilitation. Eur Arch Paediatr Dent. 2010;11:32–7. doi: 10.1007/BF03262707. [DOI] [PubMed] [Google Scholar]
- 2.Damle SG, Gandhi M, Laheri V. Comparison of oral ketamine and oral midazolam as sedative agents in pediatric dentistry. J Indian Soc Pedod Prev Dent. 2008;26:97–101. [PubMed] [Google Scholar]
- 3.Kupietzky A. Strap him down or knock him out: Is conscious sedation with restraint an alternative to general anaesthesia? Br Dent J. 2004;196:133–8. doi: 10.1038/sj.bdj.4810932. [DOI] [PubMed] [Google Scholar]
- 4.Homer JR, Bass S. Physically restraining children for induction of general anesthesia: Survey of consultant pediatric anesthetists. Paediatr Anesth. 2010;20:638–46. doi: 10.1111/j.1460-9592.2010.03324.x. [DOI] [PubMed] [Google Scholar]
- 5.Sheta SA, Alsarheed M. Oral midazolam premedication for children undergoing general anaesthesia for dental care. Int J Pediatr 2009. 2009 doi: 10.1155/2009/274380. 274380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mountain BW, Smithson L, Cramolini M, Wyatt TH, Newman M. Dexmedetomidine as a pediatric anesthetic premedication to reduce anxiety and to deter emergence delirium. AANA J. 2011;79:219–24. [PubMed] [Google Scholar]
- 7.World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79:373–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Isik B, Baygin O, Bodur H. Effect of drinks that are added as flavoring in oral midazolam premedication on sedation success. Pediatr Anesth. 2008;18:494–500. doi: 10.1111/j.1460-9592.2008.02462.x. [DOI] [PubMed] [Google Scholar]
- 9.El Batawi HY. Lidocaine use for pain management during paediatric dental rehabilitation under general anaesthesia. Eur Arch Paediatr Dent. 2013;14:381–7. doi: 10.1007/s40368-013-0027-6. [DOI] [PubMed] [Google Scholar]
- 10.El Batawi HY. Effect of intraoperative analgesia on children's pain perception during recovery after painful dental procedures performed under general anaesthesia. Eur Arch Paediatr Dent. 2015;16:35–41. doi: 10.1007/s40368-014-0143-y. [DOI] [PubMed] [Google Scholar]
- 11.Dashiff CJ, Weaver M. Development and testing of a scale to measure separation anxiety of parents of adolescents. J Nurs Meas. 2008;16:61–80. doi: 10.1891/1061-3749.16.1.61. [DOI] [PubMed] [Google Scholar]
- 12.Kaviani N, Shahtusi M, Haj Norousali Tehrani M, Nazari S. Effect of oral midazolam premedication on children's co-operation before general anesthesia in pediatric dentistry. J Dent (Shiraz) 2014;15:123–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Akin A, Bayram A, Esmaoglu A, Tosun Z, Aksu R, Altuntas R, et al. Dexmedetomidine vs midazolam for premedication of pediatric patients undergoing anesthesia. Paediatr Anaesth. 2012;22:871–6. doi: 10.1111/j.1460-9592.2012.03802.x. [DOI] [PubMed] [Google Scholar]
- 14.Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004;100:1138–45. doi: 10.1097/00000542-200405000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Pieters BJ, Penn E, Nicklaus P, Bruegger D, Mehta B, Weatherly R. Emergence delirium and postoperative pain in children undergoing adenotonsillectomy: A comparison of propofol vs sevoflurane anesthesia. Paediatr Anaesth. 2010;20:944–50. doi: 10.1111/j.1460-9592.2010.03394.x. [DOI] [PubMed] [Google Scholar]
- 16.Shung J. Refresher course: The agitated child in recovery. South Afr J Anaesth Analg. 2011;17:96–9. [Google Scholar]
- 17.Ead H. From Aldrete to PADSS: Reviewing discharge criteria after ambulatory surgery. J Perianesth Nurs. 2006;21:259–67. doi: 10.1016/j.jopan.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Kain ZN, Caldwell-Andrews AA, Maranets I, McClain B, Gaal D, Mayes LC, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg. 2004;99:1648–54. doi: 10.1213/01.ANE.0000136471.36680.97. table of contents. [DOI] [PubMed] [Google Scholar]
- 19.Kain ZN, Wang SM, Mayes LC, Caramico LA, Hofstadter MB. Distress during the induction of anesthesia and postoperative behavioral outcomes. Anesth Analg. 1999;88:1042–7. doi: 10.1097/00000539-199905000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Feld LH, Negus JB, White PF. Oral midazolam preanesthetic medication in pediatric outpatients. Anesthesiology. 1990;73:831–4. doi: 10.1097/00000542-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 21.McMillan CO, Spahr-Schopfer IA, Sikich N, Hartley E, Lerman J. Premedication of children with oral midazolam. Can J Anaesth. 1992;39:545–50. doi: 10.1007/BF03008315. [DOI] [PubMed] [Google Scholar]
- 22.Finley GA, Stewart SH, Buffett-Jerrott S, Wright KD, Millington D. High levels of impulsivity may contraindicate midazolam premedication in children. Can J Anaesth. 2006;53:73–8. doi: 10.1007/BF03021530. [DOI] [PubMed] [Google Scholar]
- 23.Levine MF, Spahr-Schopfer IA, Hartley E, Lerman J, MacPherson B. Oral midazolam premedication in children: The minimum time interval for separation from parents. Can J Anaesth. 1993;40:726–9. doi: 10.1007/BF03009769. [DOI] [PubMed] [Google Scholar]


