Abstract
Purpose of review
Polyphosphate (polyP) is an inorganic polymer that has recently been shown to be secreted by activated platelets. It is a potent modulator of the blood clotting and complement systems in hemostasis, thrombosis, and inflammation.
Recent findings
This review focuses on what is currently known about which blood cells secrete polyP, and the roles that polyP plays in modulating the blood clotting and complement systems in health and disease.
Summary
PolyP is a novel player in normal hemostasis and likely plays roles in thrombotic diseases and also in host responses to pathogens. It is also potentially a drug target, as its contributions to hemostasis appear to be to accelerate blood clotting but are not required for blood clotting to happen.
Keywords: polyphosphate, platelets, coagulation, inflammation
INTRODUCTION
Inorganic polyphosphate (polyP) is an intensely anionic, linear polymer of orthophosphate units linked by high-energy phosphoanhydride bonds that are widespread in biology (Fig. 1). Polymer sizes vary from about ten phosphates to thousands of phosphates long, depending on organism and cell type [1, 2]. In microorganisms, polyP is synthesized from ATP via a fully reversible enzymatic reaction [3], and is degraded by endopolyphosphatases (cleavage within chain) and exopolyphosphatases (progressive removal of terminal phosphates)[4]. Roles for polyP in mammalian systems are rapidly emerging, but polyP has been most intensively studied in prokaryotes and unicellular eukaryotes. Microorganisms store polyP in granules (with varying names, including “acidocalcisomes”[5]), which typically contain very long-chain polyP, ranging in length from hundreds to thousands of phosphate units [3]. Mammalian cellular compartments identified to contain polyP include lysosomes [6], platelet dense granules [7], mitochondria, and nuclei [8]. Tissue extracts from mammalian heart, liver, lung and kidneys are reported to contain heterogeneous polyP of 50 to 800 phosphate units long, while brain polyP is longer and more narrowly distributed at about 800 phosphates long [8]. Functions ascribed to polyP in mammalian systems include angiogenesis [9], apoptosis [10], cell proliferation [11], energy metabolism [12], osteoblast function [13], bone mineralization [14, 15], and tumor metastasis [16, 17]. Here we review the emerging understanding of the roles of polyP in hematology. Recent studies from our lab and others have revealed that polyP is potently prohemostatic, prothrombotic and proinflammatory [18-26], primarily via its influences on the blood coagulation and complement cascades (Fig. 2).
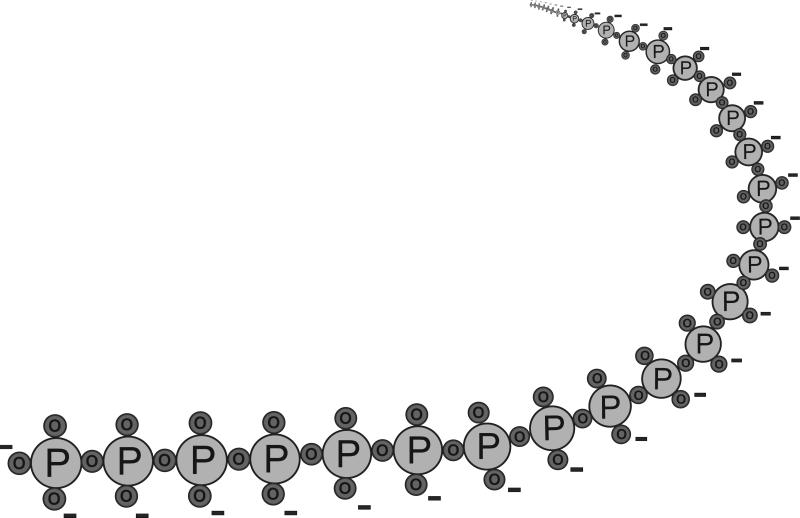
FIGURE 1.
Structure of inorganic polyphosphate (polyP). PolyP is a linear, highly anionic polymer of phosphates held together by high-energy phosphoanhydride bonds. Platelet polyP is approximately 60 to 100 phosphate units long [7, 21, 23], while microbial polyP can be hundreds to thousands of phosphate units long [3, 73].
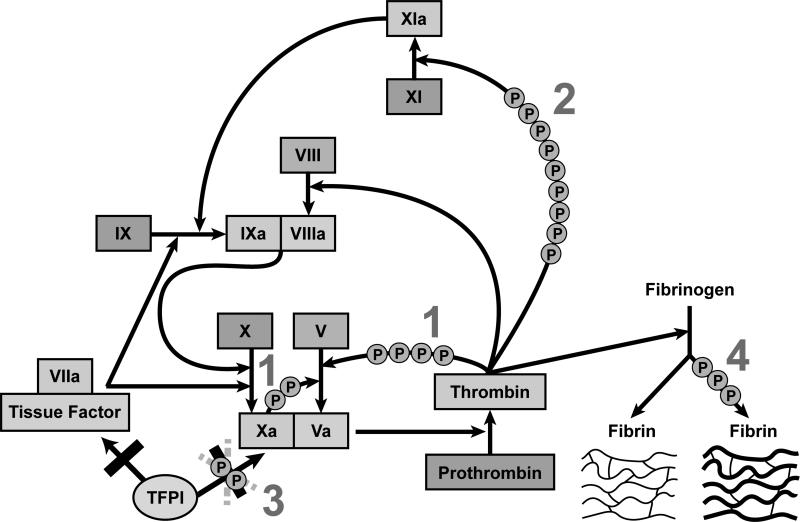
FIGURE 2.
The roles of platelet polyP in blood coagulation. PolyP of platelet size (60-100 units) enhances thrombin generation through multiple points in the coagulation cascade. PolyP 1: accelerates factor V activation by factors Xa and thrombin [18]; 2: accelerates factor XI back-activation by thrombin [25]; and 3: abrogates the ability of tissue factor pathway inhibitor (TFPI) to inhibit factor Xa [18, 41]. PolyP also 4: enhances fibrin polymerization [20, 23, 26], but this effect optimally requires longer polyP of >400 phosphate units in length.
POLYP IN PLATELETS
Acidocalcisomes in microorganisms, in addition to polyP, contain divalent metal ions such as Ca2+, Mg2+ and Zn2+ [27], and are spherical, acidic [28], and electron-dense [29]. Platelet dense granules share these properties, and have long been known to contain inorganic phosphate and pyrophosphate [27]. Ruiz et al. [7] reported that platelet dense granules are essentially acidocalcisomes, containing abundant polyP inside the granules. Platelet alpha granules also contain polyP, but at markedly lower concentrations [30]. Platelet polyP is smaller and much less heterodisperse than microbial polyP, with lengths of approximately 60 to 100 phosphate units [7, 21]. Dense granule polyP is secreted along with other granule contents when platelets are activated [7, 21]. Furthermore, patients diagnosed with platelet dense granule defects have abnormally low levels of polyP (approximately 10% of normal) and experience a bleeding tendency [31]. Knocking out the gene for inositol hexakisphosphate kinase 1 in mice resulted in a tenfold decrease in polyP accumulation in platelet dense granules, which was associated with deficiencies in hemostasis and thrombosis [32].
POLYP IN MAST CELLS AND BASOPHILS
Like platelet dense granules, a subset of mast cell and basophil granules share many features with bacterial acidocalcisomes; they are spherical, electron-dense (14), and contain phosphorus and cations [33]. These granules contain polyP of about 60 units (similar to the size found in platelets). PolyP co-localizes in mast cell granules with serotonin, but not with histamine, and is released when the cells are stimulated to secrete their granule contents [33].
POLYP AND OTHER HEMATOLOGIC CELLS
PolyP stimulates apoptosis in plasma cells and myeloma cells, but not in normal B or T lymphocytes, or non-lymphoid cell lines [10]. Myeloma cells contain much higher levels of nuclear polyP than normal plasma cells [34]. In human erythrocytes, polyP is reported to be a component of the Ca2+-ATPase pump [35, 36].
ROLES OF POLYP IN COAGULATION
The discovery that polyP was released from platelets [7] suggested a potential role in coagulation.
Amplification of thrombin generation
The production of a fibrin clot is highly dependent on the ability to generate a burst of thrombin that exceeds a necessary threshold. The rate of thrombin generation is a function of 1) rates of activation of procoagulant factors and cofactors, and 2) the inhibitory ability of anticoagulants. PolyP acts at several steps that influence thrombin generation: it enhances the generation of factor Va; it enhances the generation of factor XIa; and it opposes the anticoagulant activity tissue factor pathway inhibitor (TFPI) (Fig. 2). The combined result of these polyP effects is that the time to achieve a thrombin burst is shortened [18]. The relevance of polyP amplification of thrombin generation is demonstrated by the fact that platelets lacking dense granules (from Hermansky-Pudlak syndrome patients) are less able to generate thrombin and form a plasma clot in vitro, but activity can be restored by adding exogenous polyP [21].
Factor Va is of critical importance in the generation of thrombin, as it serves as the cofactor for factor Xa in the prothrombinase complex. The presence of factor Va enhances activation of prothrombin by several orders of magnitude. Relatively short polyP chains (of the size in platelets) [23] accelerate the activation of factor V to Va by both factor Xa and thrombin [18].
While the classic waterfall cascade of coagulation describes factor XIIa as activating factor XI to factor XIa, recent work has indicated that this reaction, while relevant to clotting in vitro, is of no consequence to hemostasis in vivo [37]. Rather, factor XI is now thought to be activated via a feedback mechanism by thrombin, and this reaction is markedly enhanced by polyP [25]. PolyP also potently accelerates factor XI activation by factor XIa (i.e., factor XI autoactivation) [25]. PolyP of the size secreted by platelets is able to enhance activation of factor XI by either enzyme, and polyP in platelet releasates strongly promotes factor XI activation by thrombin [25]. It is likely that polyP provides a template for assembly of the enzyme/substrate complex in these reactions [18, 22, 25, 38].
TFPI, a protease inhibitor found on endothelial cells, in plasma, and in platelets, targets factor Xa, and then the tissue factor-factor VIIa complex [39]. In vitro experiments indicate that polyP profoundly abrogates the inhibitory function of TFPI [18], and polyP in platelet releasates strongly inhibits TFPI function [18, 21]. Factor Xa that is already bound to factor Va (i.e., assembled into the prothrombinase complex) is resistant to TFPI, especially in the presence of the substrate, prothrombin [40]. Recent work, however, has revealed that TFPI can still inhibit prothrombinase assembled with partially cleaved versions of FVa (i.e., that still retain portions of the B domain, as may be released from activated platelets), and polyP can block the ability of TFPI to inhibit factor Xa in this version of the prothrombinase [41].
Impacts on fibrin clot structure and stability
PolyP influences fibrin clot structure. As compared to clots without polyP, fibrin clots formed in the presence of polyP are more turbid, contain thicker fibrin fibrils, are more resistant to elastic stretching, and more resistant to fibrinolysis [20]. PolyP appears to become incorporated directly into fibrin clots, although the mechanism is not known. PolyP of the size secreted by activated platelets is just large enough to have an impact on fibrin clot structure, but optimal fibrin enhancement requires longer polyP polymers (>400mer) [23]. Interestingly, pyrophosphate abrogates the ability of polyP to enhance fibrin clot structure, while having no effect on fibrin clots formed in the absence of polyP [23]. Platelet dense granules also contain pyrophosphate (in quantities greater than polyP) [7], but little has been discovered about the function of this pyrophosphate.
The mechanism by which fibrin with incorporated polyP is resistant to fibrinolysis is not entirely clear. Anionic polymers other than polyP (e.g. heparin) similarly increase fibrin clot turbidity, but cause a clot that is more susceptible to fibrinolysis [42]. One possibility is that the shift toward earlier thrombin generation allows for more activation of thrombin activatable fibrinolysis inhibitor (TAFI) [18]. Since TAFI modifies binding sites for plasmin on the fibrin molecule, earlier TAFI generation results in less plasmin binding sites and consequently resistance to lysis [18]. The presence of polyP also inhibits the binding of tissue-type plasminogen activator and plasminogen to fibrin [26].
Contact Activation
The contact pathway is triggered when factor XII, prekallikrein and high molecular weight kininogen assemble on anionic polymers or surfaces. Factor XIIa can then activate factor XI to XIa, which in turn activates factor IX, leading to propagation of the clotting cascade and ultimately thrombin generation. While this pathway is important for the clotting of blood or plasma ex vivo, it is dispensable for clotting in vivo since complete factor XII deficiency is not associated with a bleeding tendency [43].
Although the contact pathway is not required for normal hemostasis, recent evidence indicates that contact activation contributes to thrombosis. Clinical studies have determined that elevated plasma factor XII, factor XI, or kallikrein is associated with atherosclerosis [44] or myocardial infarction [45-47], while patients with severe factor XI deficiency have reduced risk of stroke [48]. In animal models, factor XII deficiency is protective against both arterial and venous thrombus formation [49, 50].
The identity of the true (patho)physiologic activator(s) of the contact pathway in vivo has not been definitively determined. Most in vitro studies have employed artificial anionic surfaces such as glass, kaolin (powdered clay), diatomaceous earth, ellagic acid, or sulfatides. RNA [51] and misfolded proteins [52] have been proposed as possible natural activators, but polyP is a very potent activator of the contact pathway in both plasma and purified protein systems [18, 21]. PolyP binds with high affinity to the proteins responsible for initiating the contact pathway [18, 23, 38]. PolyP-mediated contact activation, like polyP-mediated FXI activation, likely occurs via a template mechanism [18, 23].
Contact activation by polyP is profoundly dependent on polymer length, with optimal activity requiring very long polyP polymers [23]. It has long been known that activated human platelets express a weak but measurable ability to trigger the contact pathway in a factor XII-dependent manner [53]. Platelet-derived polyP is able to weakly activate contact factors, but is thousands of times less potent than long-chain polyP [23]. The weak contact activation ability of platelet polyP is consistent with the idea that platelets are much more effective at accelerating coagulation reactions than they are at initiating them.
Recent studies in animal models of thrombosis have suggested a role for polyP in vivo [21]. PolyP administered intravenously leads to lethal pulmonary embolism in normal mice, while mice deficient in factor XII, or those given an inhibitor to factor XIIa, survive [21]. In vivo activation of platelets via intravenous injection of a platelet agonist similarly causes fatal pulmonary embolism in normal mice, but not when factor XII activity is absent [21]. If an enzyme that degrades polyP is injected at high doses, the mice are more likely to survive. These experiments indicate that polyP is thrombogenic in vivo, and that the thrombogenicity is dependent on factor XII [21]. Proof-of-principal polyP inhibitors have recently been identified, and were shown to be antithrombotic in mouse arterial thrombosis models, while having fewer bleeding side effects than conventional anticoagulant drugs [54, 55].
POLYP IS PROINFLAMMATORY
While the contact pathway is dispensable for hemostasis, it plays important roles in inflammatory responses (Fig. 3). Activation of the contact pathway (often called the kallikreinkinin pathway) results in kallikrein-mediated release of bradykinin from high molecular weight kininogen. Bradykinin is a potent vasoactive peptide. When bradykinin binds to its receptors on the endothelial cell, it causes release of prostacyclin, nitric oxide, and endothelium-derived hyperpolarizing factor, resulting in vasodilation [56]. In addition to bradykinin generation, kallikrein has been shown to directly activate complement components C3 and C5 [57, 58], while factor XIIa also initiates the classical complement cascade [59].
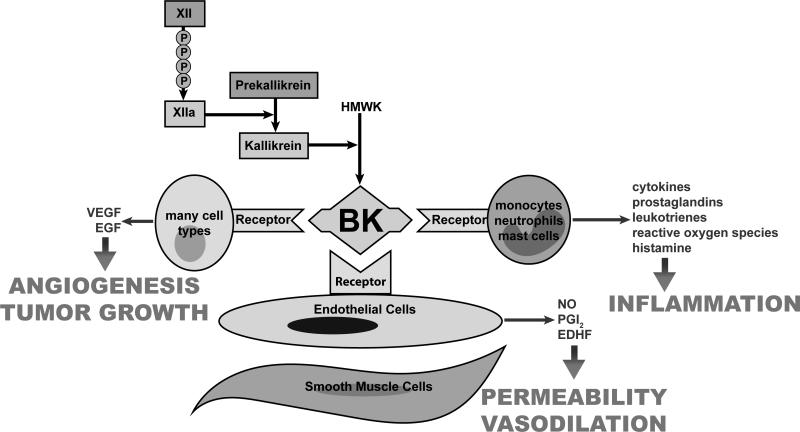
FIGURE 3.
The roles of polyP in bradykinin-mediated inflammation. PolyP strongly supports activation of FXII to FXIIa [18]. Factor XIIa cleaves prekallikrein resulting in the production of kallikrein, which cleaves high molecular weight kininogen (HMWK) releasing bradykinin. PolyP of the size released from platelets and mast cells has been demonstrated to increase the formation of bradykinin both in vitro and in vivo [21, 33]. However, long-chain polyP (hundreds to thousands of units) like that within microorganisms is several orders of magnitude more potent as an activator of Factor XII [23].
Bradykinin binds to bradykinin receptors on many cell types, causing a multitude of effects. Many cells are stimulated to release vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF) which promote angiogenesis and tumor growth. Leucocytes are attracted, activated, and release proinflammatory mediators. Endothelial cells synthesize and release nitric oxide (NO), prostacyclin (PGI2) and endothelial derived hyperpolarizing factor (EDHF). These mediators increase vascular permeability (causing edema) and cause smooth muscle relaxation with the associated vasodilation.
The importance of the contact pathway in vivo is demonstrated by the severe clinical manifestations of hereditary angioedema. In this disease, patients are deficient in an important inhibitor of the contact pathway. Unregulated activation of contact factors leads to vasodilation and vascular leakage, resulting in potentially lethal edema and hypotension [60]. Another circumstance demonstrating the importance of contact activation in vivo was the severe and fatal adverse reactions reported for pharmaceutical heparin that was contaminated with a potent contact activator [61, 62]. Factor XII gene knockout in mice causes defective immune responses to infection [63], indicating that the contact pathway also contributes to host responses to pathogens. The identification of multiple microbial contact activators (e.g. bacterial surface proteins [64, 65], lipopolysaccharide [66], teichoic/lipoteichoic acid [66], and long-chain polyP[18, 23]) is consistent with this concept.
As noted above, long-chain polyP is an extremely potent trigger of the contact pathway [18, 21, 23], suggesting that polyP is a proinflammatory mediator. Mast-cell derived polyP [33] and platelet-derived polyP [23] are also able to initiate the contact pathway, but more weakly. As with other activators of the contact system, polyP promotes release of bradykinin [21]. In mouse models, subcutaneous injection of polyP causes localized capillary leak [21, 54], and intraperitoneal injection leads to a rapid drop in systemic arterial blood pressure and death [21]. Based on gene knockout studies, these polyP-mediated effects are dependent on both factor XII and bradykinin.
PolyP additionally contributes to inflammatory processes through mechanisms that are independent of the contact pathway. PolyP substantially enhances the activity of histones, resulting in increased platelet activation and thrombin generation that is independent of factor XII [24]. Extracellular histones have been shown to exhibit potent proinflammatory and procoagulant activities [67]. PolyP also activates NF-κB [68]. PolyP has been shown to induce proliferation and differentiation of mesenchymal stem cells via activation of fibroblast growth factors [69]. Interestingly, long-chain polyP suppresses complement via the terminal pathway by destabilizing C5b,6, thereby reducing the lytic capacity of the membrane attack complex [70].
OTHER ROLES FOR POLYP
The extent of the contributions of polyP to physiologic processes is just beginning to be explored. PolyP is present in von Willebrand factor (vWF) isolated from platelet alpha granules or plasma. It binds vWF in vitro with high affinity and modulates its interaction with glycoprotein Ib [30]. PolyP accelerates the autoactivation of factor seven-activating protease, a broad spectrum enzyme with possible roles in coagulation, fibrinolysis, vascular biology, atherosclerosis, and autoimmune disease [71]. In a mouse model, polyP blocked metastasis of melanoma cells due to anti-angiogenic activity [9]. PolyP stimulates the protein kinase mTOR (mammalian target of rapamycin) in mammary cancer cells, making the cells markedly deficient in their response to mitogens. This suggests that polyP is a regulatory factor in the activation of mTOR in proliferative signaling pathways [11]. PolyP serves as a molecular chaperone, stabilizing proteins in vivo and protecting them against stress-induced unfolding and aggregation. It binds to unfolding proteins with high affinity and supports refolding once stress conditions are resolved [72].
CONCLUSION
The work reviewed here shows that polyP accelerates thrombin generation, reverses the anticoagulant activity of a variety of anticoagulants in vitro (including heparins, direct factor Xa inhibitors, and thrombin inhibitors), and shortens the clotting times of plasma from patients with hemophilia A or B, or patients taking vitamin K antagonists [19]. PolyP or suitable derivatives– might consequently have use in the future as parenteral or topical hemostatic agents. Recent work suggests that polyP is a key player in the web of host-pathogen interactions. Long-chain microbial polyP is a potent activator of the blood clotting system via the contact pathway and can trigger thrombosis and inflammation. The activities of polyP in vivo may therefore also represent a novel target for future anti-thrombotic and/or anti-inflammatory agents. The detailed molecular mechanisms by which polyP acts as modulator of coagulation and inflammation have yet to be definitively described. Further, it is likely that future research will reveal many more physiologic roles for this ancient molecule.
KEY POINTS.
PolyP is procoagulant due to its ability to enhance thrombin generation and fibrin clot structure.
PolyP is prothrombotic, primarily via its activation of the contact (kallikrein-kinin) pathway.
PolyP is proinflammatory via both its activation of the contact pathway and its interaction with other host-pathogen responses.
Acknowledgements
We thank Catherine Baker for assistance with figures. The authors’ studies were supported by grants R01 HL047014 from the National Heart, Lung and Blood Institute of the National Institutes of Health.
Footnotes
Conflict-of-interest disclosure
The authors are a co-inventors on patents and pending patent applications on medical uses of polyP.
REFERENCES AND RECOMMENDED READING
- 1.Ault-Riché D, Fraley CD, Tzeng CM, Kornberg A. Novel assay reveals multiple pathways regulating stress-induced accumulations of inorganic polyphosphate in Escherichia coli. J Bacteriol. 1998;180:1841–1847. doi: 10.1128/jb.180.7.1841-1847.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown MR, Kornberg A. Inorganic polyphosphate in the origin and survival of species. Proc Natl Acad Sci U S A. 2004;101:16085–16087. doi: 10.1073/pnas.0406909101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kornberg A, Rao NN, Ault-Riche D. Inorganic polyphosphate: a molecule of many functions. Annu Rev of Biochem. 1999;68:89–125. doi: 10.1146/annurev.biochem.68.1.89. [DOI] [PubMed] [Google Scholar]
- 4**.Moreno SN, Docampo R. Polyphosphate and its diverse functions in host cells and pathogens. PLoS Pathog. 2013;9:e1003230. doi: 10.1371/journal.ppat.1003230. [Informative review of the many new roles that have been discovered for polyP, with an emphasis to pathogens and the host response to them.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Docampo R, Moreno SN. Acidocalcisomes. Cell Calcium. 2011;50:113–119. doi: 10.1016/j.ceca.2011.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pisoni RL, Lindley ER. Incorporation of [32P]orthophosphate into long chains of inorganic polyphosphate within lysosomes of human fibroblasts. J Biol Chem. 1992;267:3626–3631. [PubMed] [Google Scholar]
- 7.Ruiz FA, Lea CR, Oldfield E, Docampo R. Human platelet dense granules contain polyphosphate and are similar to acidocalcisomes of bacteria and unicellular eukaryotes. J Biol Chem. 2004;279:44250–44257. doi: 10.1074/jbc.M406261200. [DOI] [PubMed] [Google Scholar]
- 8.Kumble KD, Kornberg A. Inorganic polyphosphate in mammalian cells and tissues. J Biol Chem. 1995;270:5818–5822. doi: 10.1074/jbc.270.11.5818. [DOI] [PubMed] [Google Scholar]
- 9.Han KY, Hong BS, Yoon YJ, et al. Polyphosphate blocks tumour metastasis via anti-angiogenic activity. Biochem J. 2007;406:49–55. doi: 10.1042/BJ20061542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hernandez-Ruiz L, Gonzalez-Garcia I, Castro C, et al. Inorganic polyphosphate and specific induction of apoptosis in human plasma cells. Haematologica. 2006;91:1180–1186. [PubMed] [Google Scholar]
- 11.Wang L, Fraley CD, Faridi J, et al. Inorganic polyphosphate stimulates mammalian TOR, a kinase involved in the proliferation of mammary cancer cells. Proc Natl Acad Sci U S A. 2003;100:11249–11254. doi: 10.1073/pnas.1534805100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pavlov E, Aschar-Sobbi R, Campanella M, et al. Inorganic polyphosphate and energy metabolism in mammalian cells. J Biol Chem. 2010;285:9420–9428. doi: 10.1074/jbc.M109.013011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kawazoe Y, Shiba T, Nakamura R, et al. Induction of calcification in MC3T3-E1 cells by inorganic polyphosphate. J Dent Res. 2004;83:613–618. doi: 10.1177/154405910408300806. [DOI] [PubMed] [Google Scholar]
- 14.Schröder HC, Kurz L, Müller WE, Lorenz B. Polyphosphate in bone. Biochemistry (Mosc) 2000;65:296–303. [PubMed] [Google Scholar]
- 15.Leyhausen G, Lorenz B, Zhu H, et al. Inorganic polyphosphate in human osteoblast-like cells. J Bone Miner Res. 1998;13:803–812. doi: 10.1359/jbmr.1998.13.5.803. [DOI] [PubMed] [Google Scholar]
- 16.Galasso A, Zollo M. The Nm23-H1-h-Prune complex in cellular physiology: a 'tip of the iceberg' protein network perspective. Mol Cell Biochem. 2009;329:149–159. doi: 10.1007/s11010-009-0115-4. [DOI] [PubMed] [Google Scholar]
- 17.Tammenkoski M, Koivula K, Cusanelli E, et al. Human metastasis regulator protein H-prune is a short-chain exopolyphosphatase. Biochemistry. 2008;47:9707–9713. doi: 10.1021/bi8010847. [DOI] [PubMed] [Google Scholar]
- 18.Smith SA, Mutch NJ, Baskar D, et al. Polyphosphate modulates blood coagulation and fibrinolysis. Proc Natl Acad Sci U S A. 2006;103:903–908. doi: 10.1073/pnas.0507195103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith SA, Morrissey JH. Polyphosphate as a general procoagulant agent. J Thromb Haemost. 2008;6:1750–1756. doi: 10.1111/j.1538-7836.2008.03104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith SA, Morrissey JH. Polyphosphate enhances fibrin clot structure. Blood. 2008;112:2810–2816. doi: 10.1182/blood-2008-03-145755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muller F, Mutch NJ, Schenk WA, et al. Platelet polyphosphates are proinflammatory and procoagulant mediators in vivo. Cell. 2009;139:1143–1156. doi: 10.1016/j.cell.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mutch NJ, Myles T, Leung LLK, Morrissey JH. Polyphosphate binds with high affinity to exosite II of thrombin. J Thromb Haemost. 2010;8:548–555. doi: 10.1111/j.1538-7836.2009.03723.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith SA, Choi SH, Davis-Harrison R, et al. Polyphosphate exerts differential effects on blood clotting, depending on polymer size. Blood. 2010;116:4353–4359. doi: 10.1182/blood-2010-01-266791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Semeraro F, Ammollo CT, Morrissey JH, et al. Extracellular histones promote thrombin generation through platelet-dependent mechanisms: involvement of platelet TLR2 and TLR4. Blood. 2011;118:1952–1961. doi: 10.1182/blood-2011-03-343061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi SH, Smith SA, Morrissey JH. Polyphosphate is a cofactor for the activation of factor XI by thrombin. Blood. 2011;118:6963–6970. doi: 10.1182/blood-2011-07-368811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mutch NJ, Engel R, Uitte de Willige S, et al. Polyphosphate modifies the fibrin network and down-regulates fibrinolysis by attenuating binding of tPA and plasminogen to fibrin. Blood. 2010;115:3980–3988. doi: 10.1182/blood-2009-11-254029. [DOI] [PubMed] [Google Scholar]
- 27.Fukami MH, Dangelmaier CA, Bauer JS, Holmsen H. Secretion, subcellular localization and metabolic status of inorganic pyrophosphate in human platelets. A major constituent of the amine-storing granules. Biochem J. 1980;192:99–105. doi: 10.1042/bj1920099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dean GE, Fishkes H, Nelson PJ, Rudnick G. The hydrogen ion-pumping adenosine triphosphatase of platelet dense granule membrane. Differences from F1F0- and phosphoenzyme-type ATPases. J Biol Chem. 1984;259:9569–9574. [PubMed] [Google Scholar]
- 29.White JG. The dense bodies of human platelets: inherent electron opacity of the serotonin storage particles. Blood. 1969;33:598–606. [PubMed] [Google Scholar]
- 30.Montilla M, Hernández-Ruiz L, García-Cozar FJ, et al. Polyphosphate binds to human von Willebrand factor in vivo and modulates its interaction with glycoprotein Ib. J Thromb Haemost. 2012;10:2315–2323. doi: 10.1111/jth.12004. [DOI] [PubMed] [Google Scholar]
- 31.Hernández-Ruiz L, Sáez-Benito A, Pujol-Moix N, et al. Platelet inorganic polyphosphate decreases in patients with delta storage pool disease. J Thromb Haemost. 2009;7:361–363. doi: 10.1111/j.1538-7836.2008.03238.x. [DOI] [PubMed] [Google Scholar]
- 32**.Ghosh S, Shukla D, Suman K, et al. Inositol hexakisphosphate kinase 1 maintains hemostasis in mice by regulating platelet polyphosphate levels. Blood. 2013;122:1478–1486. doi: 10.1182/blood-2013-01-481549. [For the first time, this study provides a way to knock down polyP accumulation in platelets, giving insights into its function in vivo. The study also underscores the connection between the synthesis between highly phosphorylated derivatives of inositol and polyphosphate, although how these synthetic pathways are linked in vivo remains a puzzle.] [DOI] [PubMed] [Google Scholar]
- 33.Moreno-Sanchez D, Hernandez-Ruiz L, Ruiz FA, Docampo R. Polyphosphate is a novel pro-inflammatory regulator of mast cells and is located in acidocalcisomes. J Biol Chem. 2012;287:28435–28444. doi: 10.1074/jbc.M112.385823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jimenez-Nunez MD, Moreno-Sanchez D, Hernandez-Ruiz L, et al. Myeloma cells contain high levels of inorganic polyphosphate which is associated with nucleolar transcription. Haematologica. 2012;97:1264–1271. doi: 10.3324/haematol.2011.051409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reusch RN, Huang R, Kosk-Kosicka D. Novel components and enzymatic activities of the human erythrocyte plasma membrane calcium pump. FEBS Lett. 1997;412:592–596. doi: 10.1016/s0014-5793(97)00863-6. [DOI] [PubMed] [Google Scholar]
- 36.Reusch RN. Transmembrane ion transport by polyphosphate/poly-(R)-3-hydroxybutyrate complexes. Biochemistry (Mosc) 2000;65:280–295. [PubMed] [Google Scholar]
- 37.Renne T. The procoagulant and proinflammatory plasma contact system. Semin Immunopathol. 2012;34:31–41. doi: 10.1007/s00281-011-0288-2. [DOI] [PubMed] [Google Scholar]
- 38.Choi SH, Collins JN, Smith SA, et al. Phosphoramidate end labeling of inorganic polyphosphates: facile manipulation of polyphosphate for investigating and modulating its biological activities. Biochemistry. 2010;49:9935–9941. doi: 10.1021/bi1014437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Broze GJ., Jr. Tissue factor pathway inhibitor and the current concept of blood coagulation. Blood Coagul Fibrinolysis. 1995;6(Suppl 1):S7–13. doi: 10.1097/00001721-199506001-00002. [DOI] [PubMed] [Google Scholar]
- 40.Mast AE, Broze GJ., Jr Physiological concentrations of tissue factor pathway inhibitor do not inhibit prothrombinase. Blood. 1996;87:1845–1850. [PubMed] [Google Scholar]
- 41*.Wood JP, Bunce MW, Maroney SA, et al. Tissue factor pathway inhibitor-alpha inhibits prothrombinase during the initiation of blood coagulation. Proc Natl Acad Sci U S A. 2013;110:17838–17843. doi: 10.1073/pnas.1310444110. [This study provides new mechanistic insights into both the nature of platelet factor V and also the role of polyP in blood clotting.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Collen A, Smorenburg SM, Peters E, et al. Unfractionated and low molecular weight heparin affect fibrin structure and angiogenesis in vitro. Cancer Res. 2000;60:6196–6200. [PubMed] [Google Scholar]
- 43.Colman RW, Schmaier AH. Contact system: a vascular biology modulator with anticoagulant, profibrinolytic, antiadhesive, and proinflammatory attributes. Blood. 1997;90:3819–3843. [PubMed] [Google Scholar]
- 44.Colhoun HM, Zito F, Norman Chan N, et al. Activated factor XII levels and factor XII 46C>T genotype in relation to coronary artery calcification in patients with type 1 diabetes and healthy subjects. Atherosclerosis. 2002;163:363–369. doi: 10.1016/s0021-9150(02)00022-9. [DOI] [PubMed] [Google Scholar]
- 45.Grundt H, Nilsen DW, Hetland O, et al. Activated factor 12 (FXIIa) predicts recurrent coronary events after an acute myocardial infarction. Am Heart J. 2004;147:260–266. doi: 10.1016/j.ahj.2003.07.012. [DOI] [PubMed] [Google Scholar]
- 46.Doggen CJ, Rosendaal FR, Meijers JC. Levels of intrinsic coagulation factors and the risk of myocardial infarction among men: Opposite and synergistic effects of factors XI and XII. Blood. 2006;108:4045–4051. doi: 10.1182/blood-2005-12-023697. [DOI] [PubMed] [Google Scholar]
- 47.Merlo C, Wuillemin WA, Redondo M, et al. Elevated levels of plasma prekallikrein, high molecular weight kininogen and factor XI in coronary heart disease. Atherosclerosis. 2002;161:261–267. doi: 10.1016/s0021-9150(01)00666-9. [DOI] [PubMed] [Google Scholar]
- 48.Salomon O, Steinberg DM, Koren-Morag N, et al. Reduced incidence of ischemic stroke in patients with severe factor XI deficiency. Blood. 2008;111:4113–4117. doi: 10.1182/blood-2007-10-120139. [DOI] [PubMed] [Google Scholar]
- 49.Gailani D, Renné T. Intrinsic pathway of coagulation and arterial thrombosis. Arterioscler Thromb Vasc Biol. 2007;27:2507–2513. doi: 10.1161/ATVBAHA.107.155952. [DOI] [PubMed] [Google Scholar]
- 50.Müller F, Renné T. Novel roles for factor XII-driven plasma contact activation system. Curr Opin Hematol. 2008;15:516–521. doi: 10.1097/MOH.0b013e328309ec85. [DOI] [PubMed] [Google Scholar]
- 51.Kannemeier C, Shibamiya A, Nakazawa F, et al. Extracellular RNA constitutes a natural procoagulant cofactor in blood coagulation. Proc Natl Acad Sci USA. 2007;104:6388–6393. doi: 10.1073/pnas.0608647104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maas C, Govers-Riemslag JW, Bouma B, et al. Misfolded proteins activate factor XII in humans, leading to kallikrein formation without initiating coagulation. J Clin Invest. 2008;118:3208–3218. doi: 10.1172/JCI35424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Caen J, Wu Q. Hageman factor, platelets and polyphosphates: early history and recent connection. J Thromb Haemost. 2010;8:1670–1674. doi: 10.1111/j.1538-7836.2010.03893.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith SA, Choi SH, Collins JN, et al. Inhibition of polyphosphate as a novel strategy for preventing thrombosis and inflammation. Blood. 2012;120:5103–5110. doi: 10.1182/blood-2012-07-444935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jain S, Pitoc GA, Holl EK, et al. Nucleic acid scavengers inhibit thrombosis without increasing bleeding. Proc Natl Acad Sci U S A. 2012;109:12938–12943. doi: 10.1073/pnas.1204928109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bjorkqvist J, Jamsa A, Renne T. Plasma kallikrein: the bradykinin-producing enzyme. Thromb Haemost. 2013;110:399–407. doi: 10.1160/TH13-03-0258. [DOI] [PubMed] [Google Scholar]
- 57.DiScipio RG. The activation of the alternative pathway C3 convertase by human plasma kallikrein. Immunology. 1982;45:587–595. [PMC free article] [PubMed] [Google Scholar]
- 58.Wiggins RC, Giclas PC, Henson PM. Chemotactic activity generated from the fifth component of complement by plasma kallikrein of the rabbit. J Exp Med. 1981;153:1391–1404. doi: 10.1084/jem.153.6.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ghebrehiwet B, Randazzo BP, Dunn JT, et al. Mechanisms of activation of the classical pathway of complement by Hageman factor fragment. J Clin Invest. 1983;71:1450–1456. doi: 10.1172/JCI110898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60*.Walford HH, Zuraw BL. Current update on cellular and molecular mechanisms of hereditary angioedema. Ann Allergy Asthma Immunol. 2014;112:413–418. doi: 10.1016/j.anai.2013.12.023. [The contact pathway plays a key role in the pathobiology of hereditary angioedema and it is possible that polyP contributes to this process.] [DOI] [PubMed] [Google Scholar]
- 61.Kishimoto TK, Viswanathan K, Ganguly T, et al. Contaminated heparin associated with adverse clinical events and activation of the contact system. New Engl J Med. 2008;358:2457–2467. doi: 10.1056/NEJMoa0803200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guerrini M, Beccati D, Shriver Z, et al. Oversulfated chondroitin sulfate is a contaminant in heparin associated with adverse clinical events. Nat Biotechnol. 2008;26:669–675. doi: 10.1038/nbt1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Frick IM, Akesson P, Herwald H, et al. The contact system--a novel branch of innate immunity generating antibacterial peptides. EMBO J. 2006;25:5569–5578. doi: 10.1038/sj.emboj.7601422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ben Nasr A, Wistedt A, Ringdahl U, Sjöbring U. Streptokinase activates plasminogen bound to human group C and G streptococci through M-like proteins. Eur J Biochem. 1994;222:267–276. doi: 10.1111/j.1432-1033.1994.tb18865.x. [DOI] [PubMed] [Google Scholar]
- 65.Ben Nasr A, Olsen A, Sjöbring U, et al. Assembly of human contact phase proteins and release of bradykinin at the surface of curli-expressing Escherichia coli. Mol Microbiol. 1996;20:927–935. doi: 10.1111/j.1365-2958.1996.tb02534.x. [DOI] [PubMed] [Google Scholar]
- 66.Kalter ES, van Dijk WC, Timmerman A, et al. Activation of purified human plasma prekallikrein triggered by cell wall fractions of Escherichia coli and Staphylococcus aureus. J Infect Dis. 1983;148:682–691. doi: 10.1093/infdis/148.4.682. [DOI] [PubMed] [Google Scholar]
- 67.Semeraro N, Ammollo CT, Semeraro F, Colucci M. Sepsis, thrombosis and organ dysfunction. Thromb Res. 2012;129:290–295. doi: 10.1016/j.thromres.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 68.Bae JS, Lee W, Rezaie AR. Polyphosphate elicits pro-inflammatory responses that are counteracted by activated protein C in both cellular and animal models. J Thromb Haemost. 2012;10:1145–1151. doi: 10.1111/j.1538-7836.2012.04671.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kawazoe Y, Katoh S, Onodera Y, et al. Activation of the FGF signaling pathway and subsequent induction of mesenchymal stem cell differentiation by inorganic polyphosphate. Int J Biol Sci. 2008;4:37–47. doi: 10.7150/ijbs.4.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wat JM, Foley JH, Krisinger MJ, et al. Polyphosphate suppresses complement via the terminal pathway. Blood. 2014;123:768–776. doi: 10.1182/blood-2013-07-515726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Muhl L, Galuska SP, Oorni K, et al. High negative charge-to-size ratio in polyphosphates and heparin regulates factor VII-activating protease. The FEBS journal. 2009;276:4828–4839. doi: 10.1111/j.1742-4658.2009.07183.x. [DOI] [PubMed] [Google Scholar]
- 72.Gray MJ, Wholey WY, Wagner NO, et al. Polyphosphate is a primordial chaperone. Mol Cell. 2014;53:689–699. doi: 10.1016/j.molcel.2014.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brown MR, Kornberg A. The long and short of it - polyphosphate, PPK and bacterial survival. Trends Biochem Sci. 2008;33:284–290. doi: 10.1016/j.tibs.2008.04.005. [DOI] [PubMed] [Google Scholar]