Abstract
Background
Various national campaigns launched in recent years focused on young women with acute myocardial infarction (AMI). Contemporary longitudinal data about sex differences in clinical characteristics, hospitalization rates, length of stay (LOS), and mortality have not been examined.
Objective
To determine sex differences in clinical characteristics, hospitalization rates, LOS, and in-hospital mortality by age groups and race among young patients with AMI using a large national dataset of U.S. hospital discharges.
Methods
Using the National Inpatient Sample (NIS), we compared clinical characteristics, AMI hospitalization rates, LOS, and in-hospital mortality for patients with AMI across ages 30–54 years, dividing them into 5-year subgroups from 2001–2010, using survey data analysis techniques.
Results
We identified 230,684 hospitalizations with a principal discharge diagnosis of AMI in 30–54-year-old patients from NIS data, representing an estimated 1,129,949 hospitalizations in the U.S. from 2001–2010. No statistically significant declines in AMI hospitalization rates were observed in the age groups <55 years, or stratified by sex. Prevalence of comorbidities was higher in women and increased among both sexes through the study period. Women had longer LOS and higher in-hospital mortality than men across all age groups. However, observed inhospital mortality declined significantly for women from 2001 to 2010 (3.3% to 2.3%, relative change 30.5%, p-for-trend<0.0001); but not for men (2.0% to 1.8%, relative change 8.6%, p-for-trend=0.6).
Conclusions
AMI hospitalization rates for young people have not declined over the past decade. Young women with AMI have more comorbidity, longer LOS, and higher in-hospital mortality than young men.
Keywords: Acute myocardial hospitalization, trends, young women, sex differences
Introduction
Each year, more than 30,000 women younger than 55 years old are hospitalized with acute myocardial infarction (AMI) in the United States alone (1). Growing public recognition of the importance of heart disease in young women in the late 1990s and early 2000s led to several national campaigns (2) and evidence-based guidelines with focus on young women. However, contemporary data about trends in clinical characteristics, hospitalization and mortality rates of young patients with AMI are lacking. Moreover, patients younger than 55 years with AMI have been historically examined collectively in prior studies, yielding little insight into the relationship of age and race with sex differences in the epidemiology of this disease within that group.
Accordingly, we studied sex differences in the patient characteristics, hospitalization rates, and short-term outcomes among a national sample of 30–54—year-old patients with AMI from 2001 through 2010. Specifically, we examined temporal trends with attention to subgroups of age and race. We used data from the Nationwide Inpatient Sample (NIS), a national all-payer administrative database, and U.S. Census data to obtain a national perspective on recent trends. Then, we stratified secondary analyses by age-race-sex subgroups in the 21 states that collected data on race during this time period.
Methods
Data Sources and Coding
We obtained data from the Agency for Healthcare Research and Quality’s (AHRQ) Healthcare Cost and Utilization Project (HCUP)-NIS files between 2001 and 2010. It is the largest all-payer inpatient database publicly available in the U.S., comprising discharge data from more than 1,000 hospitals across 44 states. The database was designed to approximate a 20% stratified sample of U.S. community hospitals, representing more than 95% of the U.S. population (including urban/rural hospitals across all geographic locations) (3). Statistical sampling weights provided by the NIS allow extrapolation to calculate expected hospitalization rates within the United States (4). The NIS includes all claims from each selected hospital regardless of payer or insurance status, because it is derived from state-mandated hospital discharge reports. We classified a hospital admission as AMI if the principal discharge diagnosis code was ICD-9-CM 410.xx, excluding cases for which the last digit was 2 (410.×2), which does not indicate an acute event.
Study Cohort and Patient Characteristics
From an initial sample of all discharges in the HCUP-NIS from 2001 through 2010 (n=79,171,880), we excluded the following hospitalizations: those with missing data on patient age, sex, LOS, or in-hospital death (n=278,653); discharges in which patients were <30 years or >54 years (n=58,687,675); discharges in which patients were admitted and discharged alive the same day (n=474,676) as they may not reflect a diagnosis of AMI; and discharges in which patients were admitted from another hospital (n=419,817) to avoid duplication of records, leaving a cohort of 19,311,059 discharges. Secondary analyses stratified by age-race-sex subgroups were conducted in a subset of patients hospitalized in 21 states that reported complete data on patient race during this time period, leaving a cohort of 12,059,714 discharges. These states represent approximately 60% of the U.S. population and include approximately 60% of Caucasians and 60% of Africans Americans of the national population, which may not be representative of the entire country. However, an AHRQ study comparing the HCUP-NIS database with the National Hospital Discharge Survey (NHDS) database showed that there were no significant differences in the discharge estimates for the white and black subgroups (5). Additionally, different states do not compare uniformly for inclusion criteria for the ‘Other race’ subgroup. We did not include the ‘other races’ in our analyses as they include a lot of missing values and are very heterogeneous for comparison.
We examined subgroups of age by 5-year categories (30–34, 35–39, 40–44, 45–49, and 50–54 years), sex (women and men) and race (whites and blacks). We identified clinical comorbidities using ICD-9-CM secondary diagnosis codes and classified them according to hierarchical condition categories, similar to those used by the U.S. Centers for Medicare & Medicaid Services for calculating their 30-day AMI mortality measure (6).
Statistical Analyses
We employed survey analysis methods that used hospital-level discharge weights provided by the NIS to estimate the number of AMI hospitalizations on a national level (7). We examined AMI hospitalization rates among subgroups of age, gender, and ethnicity for each year between 2001 and 2010 and reported them as the rates per 100,000 persons. We assessed the annual trend over time in AMI hospitalization rates using Poisson regression that included a variable representing the time of the year.
We evaluated in-hospital mortality and LOS among AMI admissions for patients in subgroups of age (30–34, 35–39, 40–44, 45–49, and 50–54 years), sex (women and men), and race (whites and blacks). We also examined trends in these outcomes stratified by age, sex, and race. We assessed annual changes in in-hospital mortality rate and mean LOS using linear regression. All p-values were two-sided with a significance threshold of p<0.05. Statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, North Carolina). Yale University’s Institutional Review Board approved the study protocol.
Results
Our final study sample consisted of 230,684 hospitalizations with a principal discharge diagnosis of AMI among 30–54 year old patients in the U.S. from 2001–2010 corresponding to an estimated 1,129,949 AMI hospitalizations nationally during the same time period after applying sampling weights.
For secondary analyses involving race comparisons, our study sample consisted of 134,150 hospitalizations with a principal discharge diagnosis of AMI from the 21 states that report complete race data corresponding to an estimated 656,436 AMI hospitalizations from these states from 2001 to 2010 after applying sampling weights.
Patient Characteristics
Women represented approximately one-quarter of young patients hospitalized with AMI (women: 25.9%; men: 74.1%). Secondary analyses involving race revealed that more women were black (19.7%) than men (10.5%). Several comorbidities were more prevalent in women as compared with men across all age subgroups, including congestive heart failure, hypertension, renal failure, chronic obstructive pulmonary disease, and diabetes mellitus (Table 1). Dyslipidemia, however, was more prevalent in men than women (14.1% vs 11.5%). In trend analyses for selected comorbidities, the prevalence of hypertension and diabetes increased significantly for all the groups from 2001 to 2010 (Figure 1).
Table 1.
Characteristics of Patients Hospitalized for AMI, 2001–2010*
| Description | Overall | 30–34 years | 35–39 years | 40–44 years | 45–49 years | 50–54 years | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| Race | ||||||||||||
| White | 54.0 | 49.2 | 45.3 | 43.5 | 50.4 | 45.7 | 52.3 | 47.7 | 54.5 | 49.2 | 55.4 | 50.7 |
| Black | 8.4 | 15.4 | 13.3 | 21.2 | 10.3 | 17.4 | 8.7 | 15.6 | 8.0 | 15.3 | 8.0 | 14.6 |
| Hispanic | 6.8 | 6.5 | 10.9 | 7.4 | 7.5 | 6.7 | 7.1 | 6.4 | 6.4 | 6.4 | 6.6 | 6.5 |
| Other | 30.8 | 28.9 | 30.5 | 28.0 | 31.8 | 30.3 | 31.9 | 30.3 | 31.1 | 29.1 | 30.0 | 28.1 |
| Cardiovascular | ||||||||||||
| PTCA | 9.7 | 7.5 | 5.5 | 5.0 | 7.9 | 6.3 | 9.0 | 7.2 | 10.0 | 8.1 | 10.4 | 7.7 |
| CABG | 3.2 | 3.0 | 0.9 | 1.7 | 1.5 | 1.6 | 2.2 | 2.3 | 2.9 | 2.3 | 4.2 | 3.6 |
| Congestive Heart Failure | 13.7 | 18.8 | 12.8 | 16.3 | 11.0 | 15.8 | 11.4 | 14.9 | 12.8 | 17.8 | 15.8 | 21.8 |
| AMI | 1.0 | 0.9 | 1.0 | 0.7 | 0.9 | 1.0 | 1.0 | 0.9 | 1.0 | 0.9 | 1.0 | 1.0 |
| Unstable Angina | 1.8 | 1.7 | 1.7 | 1.9 | 1.7 | 1.8 | 2.0 | 1.9 | 1.8 | 1.7 | 1.8 | 1.7 |
| Anterior Myocardial Infarction | 18.3 | 14.3 | 18.6 | 18.1 | 19.8 | 16.6 | 19.3 | 16.1 | 18.6 | 13.8 | 17.4 | 13.4 |
| Other Location of Myocardial Infarction | 29.4 | 21.8 | 26.4 | 19.7 | 29.1 | 20.2 | 30.1 | 21.9 | 29.9 | 22.4 | 29.0 | 21.8 |
| Chronic atherosclerosis | 78.7 | 70.9 | 65.1 | 62.6 | 74.0 | 67.1 | 77.5 | 69.7 | 79.6 | 71.8 | 80.3 | 71.9 |
| Cardio-respiratory failure and shock | 9.4 | 10.5 | 6.8 | 9.6 | 7.6 | 9.4 | 8.3 | 9.0 | 9.2 | 10.3 | 10.5 | 11.4 |
| Valvular or Rheumatic Heart Disease | 4.2 | 6.4 | 3.8 | 5.9 | 3.3 | 5.8 | 3.4 | 5.8 | 3.9 | 6.1 | 4.8 | 7.0 |
| Comorbidity | ||||||||||||
| Hypertension | 48.5 | 51.1 | 36.8 | 34.3 | 42.5 | 40.2 | 45.2 | 46.7 | 48.5 | 52.1 | 51.6 | 54.9 |
| Stroke | 0.6 | 0.9 | 0.5 | 0.6 | 0.5 | 0.9 | 0.5 | 0.7 | 0.5 | 0.7 | 0.7 | 1.1 |
| Cerebrovascular Disease | 0.7 | 1.2 | 0.2 | 0.4 | 0.3 | 0.7 | 0.4 | 0.9 | 0.7 | 1.1 | 1.0 | 1.6 |
| Renal Failure | 6.7 | 9.5 | 6.9 | 10.0 | 5.9 | 9.6 | 5.7 | 7.6 | 6.0 | 8.8 | 7.7 | 10.6 |
| Chronic Obstructive Pulmonary Disease | 7.7 | 11.4 | 2.7 | 3.4 | 2.9 | 5.2 | 5.0 | 8.3 | 7.3 | 11.0 | 10.2 | 14.3 |
| Pneumonia | 3.7 | 4.5 | 3.2 | 4.0 | 3.0 | 3.3 | 3.1 | 3.9 | 3.4 | 4.2 | 4.2 | 5.2 |
| Diabetes and DM Complications | 22.7 | 32.6 | 15.3 | 25.7 | 18.1 | 29.5 | 19.9 | 29.2 | 22.1 | 32.2 | 25.5 | 35.3 |
| Dyslipidemia | 14.1 | 11.5 | 11.3 | 8.7 | 13.8 | 8.7 | 13.9 | 10.1 | 14.3 | 11.9 | 14.2 | 12.3 |
| Protein-Calorie Malnutrition | 0.5 | 0.8 | 0.4 | 0.6 | 0.3 | 0.6 | 0.4 | 0.6 | 0.4 | 0.8 | 0.6 | 1.0 |
| Dementia and Senility | 0.2 | 0.3 | 0.1 | 0.2 | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.3 | 0.2 | 0.3 |
| Hemiplegia, Paralysis, Functional Disability | 1.3 | 1.8 | 1.0 | 1.3 | 1.0 | 1.7 | 0.9 | 1.5 | 1.3 | 1.7 | 1.6 | 2.2 |
| Vascular or Circulatory Disease | 4.2 | 6.2 | 2.0 | 4.3 | 2.3 | 4.4 | 2.8 | 4.9 | 3.9 | 6.0 | 5.3 | 7.4 |
| Metastatic Cancer and Acute Leukemia | 0.3 | 0.6 | 0.2 | 0.4 | 0.1 | 0.2 | 0.1 | 0.3 | 0.3 | 0.5 | 0.4 | 0.8 |
| Trauma | 1.0 | 0.8 | 1.1 | 0.6 | 1.1 | 0.8 | 0.9 | 0.7 | 1.0 | 0.9 | 1.1 | 0.9 |
| Major Psych Disorders | 1.8 | 3.1 | 2.1 | 3.5 | 1.8 | 3.4 | 1.9 | 3.2 | 1.7 | 3.3 | 1.7 | 2.9 |
| Liver and Biliary Disease | 1.1 | 1.0 | 0.6 | 0.8 | 0.6 | 0.6 | 0.7 | 0.8 | 1.1 | 1.0 | 1.4 | 1.2 |
All numbers are %ages
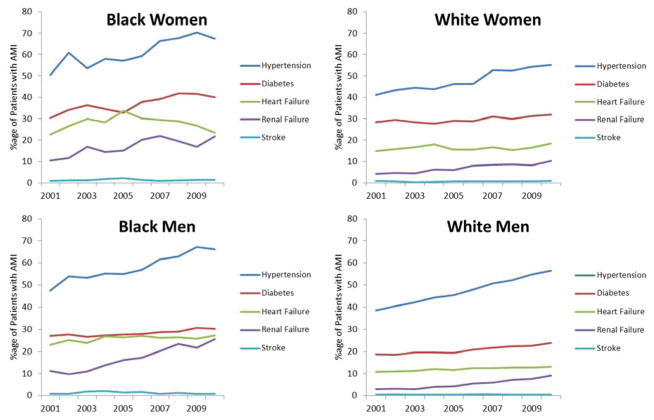
Figure 1. Trends in Selected Comorbidities among Young Patients with AMI, 2001–2010.
Trends in selected comorbidities including hypertension, diabetes, heart failure, renal failure, and stroke are shown for black women, white women, black men and white men respectively with AMI from 2001–2010. Black women had the highest prevalence of hypertension, diabetes, and heart failure across all groups. The prevalence of hypertension and diabetes increased significantly for all subgroups from 2001–2010.
In secondary analyses, black women had the highest prevalence of selected comorbidities including hypertension, heart failure, and diabetes, as compared with white women, black men and white men. Although the prevalence of heart failure was highest among black women, they did not show a significant change as opposed to other groups that showed an increase through the study period (white women: 24.5%, black men: 18.0%, white men: 21.1%).
AMI Hospitalization Rates
Hospitalization rates for AMI were higher in men as compared with women across all age subgroups (Table 2). The absolute number of discharges for AMI among women increased from 28,681 (56 per 100,000) in 2001 to 31,777 (61 per 100,000) in 2010. In contrast, the absolute number of discharges for AMI among men decreased from 87,084 (174 per 100,000) to 86,734 (171 per 100,000). While absolute declines were noted for most subgroups of men, women demonstrated either no change (30–34 years and 35–39 years) or slight absolute increase (40–44 years and 45–49 years) in hospitalization rates.
Table 2.
Hospitalization Rates (per 100,000 persons) for Young Patients with AMI Stratified by Age and Gender, 2001–2010
| Age (years) | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P-for-trend |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | |||||||||||
| Male | 174 | 168 | 173 | 150 | 153 | 160 | 153 | 173 | 181 | 171 | 0.7 |
| Female | 56 | 57 | 57 | 52 | 53 | 55 | 55 | 61 | 65 | 61 | 0.4 |
| 30 to 34 | |||||||||||
| Male | 25 | 25 | 28 | 23 | 26 | 25 | 26 | 26 | 27 | 26 | 0.8 |
| Female | 8 | 8 | 8 | 8 | 8 | 9 | 9 | 9 | 8 | 9 | 0.7 |
| 35 to 39 | |||||||||||
| Male | 62 | 59 | 61 | 51 | 54 | 55 | 57 | 66 | 65 | 63 | 0.5 |
| Female | 20 | 21 | 20 | 20 | 20 | 19 | 19 | 21 | 25 | 22 | 0.6 |
| 40 to 44 | |||||||||||
| Male | 142 | 136 | 137 | 114 | 125 | 128 | 118 | 138 | 139 | 132 | 0.8 |
| Female | 44 | 46 | 44 | 43 | 41 | 45 | 43 | 49 | 51 | 50 | 0.4 |
| 45 to 49 | |||||||||||
| Male | 258 | 251 | 259 | 224 | 220 | 229 | 217 | 246 | 259 | 237 | 0.5 |
| Female | 80 | 80 | 81 | 74 | 76 | 79 | 78 | 88 | 92 | 88 | 0.2 |
| 50 to 54 | |||||||||||
| Male | 427 | 406 | 412 | 357 | 348 | 361 | 343 | 379 | 399 | 370 | 0.06 |
| Female | 140 | 137 | 138 | 116 | 115 | 118 | 118 | 127 | 139 | 126 | 0.5 |
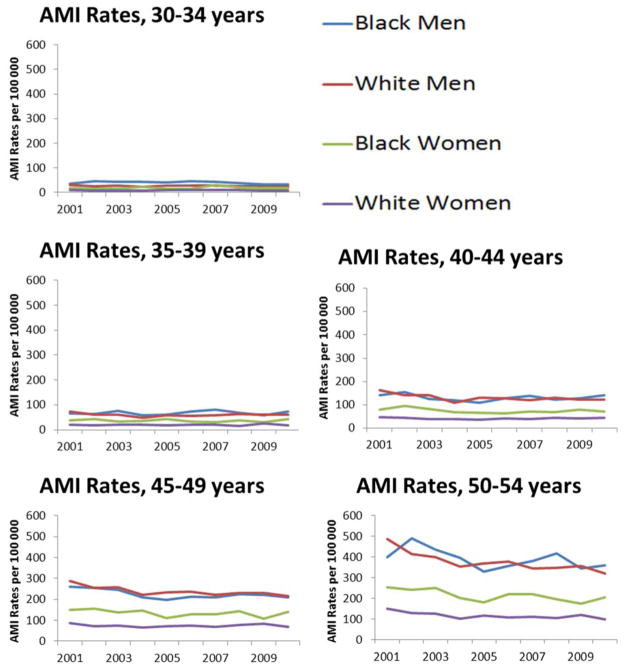
In secondary analyses including age-sex-race comparisons, black women had much higher hospitalization rates than white women consistently from 2001 to 2010, while hospitalization rates were comparable for black and white men (Figure 2). Trend analyses from 2001 to 2010 demonstrated a significant decline among black men in all age-subgroups more than 35 years old (p<0.05 for all), without significant decline all age-subgroups of white men. We observed no significant change among black women, however, with statistically significant declines in AMI hospitalization rates demonstrated by a few subgroups of white women (30–34 years, 40–44 years and 45–49 years; p<0.05 for all).
Figure 2. AMI Hospitalization Rates by Race and Sex among Young Patients with AMI, 2001–2010.
Trends in hospitalizations rates for persons aged 30–54 years with AMI are shown by race and sex across 5-year subgroups of age. Of note, black women had much higher hospitalization rates than white women consistently from 2001–2010, while hospitalization rates were comparable for black and white men.
In-hospital mortality
Women had higher in-hospital mortality than men across all subgroups (Table 3a and 3b). From 2001 to 2010, overall observed in-hospital mortality for women with AMI declined significantly (3.3% to 2.3%, 30.6% decrease, p-for-trend<0.0001); however, the decrease for men was not significant (2.0% to 1.8%, 8.5% decrease, p-for-trend=0.6). In age-sex analyses, statistically significant declines were noted among women in all age subgroups 35–54 years of age. Women had longer LOS than men across all age-subgroups (Table 4a and 4b).
Table 3a.
In-hospital Mortality (in %) among Men and Women with AMI aged 30–54 years in the US, 2001–2010
| Age (years) | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P-for-trend |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | |||||||||||
| Male | 2.0 | 2.0 | 1.7 | 2.1 | 1.9 | 1.9 | 1.9 | 2.0 | 1.9 | 1.8 | 0.6 |
| Female | 3.3 | 3.0 | 3.3 | 3.0 | 2.5 | 2.5 | 2.4 | 2.2 | 2.1 | 2.3 | <0.01 |
| 30 to 34 | |||||||||||
| Male | 2.1 | 2.0 | 1.7 | 2.3 | 2.0 | 1.4 | 1.3 | 1.4 | 1.6 | 1.6 | 0.3 |
| Female | 2.3 | 1.7 | 3.7 | 1.3 | 3.9 | 1.2 | 2.4 | 1.7 | 2.6 | 2.6 | 1.0 |
| 35 to 39 | |||||||||||
| Male | 0.8 | 1.6 | 1.2 | 1.9 | 0.9 | 2.0 | 1.4 | 1.4 | 1.5 | 1.3 | 0.3 |
| Female | 3.5 | 1.7 | 2.9 | 2.3 | 3.1 | 1.5 | 2.1 | 0.7 | 2.5 | 1.1 | 0.03 |
| 40 to 44 | |||||||||||
| Male | 1.6 | 1.4 | 1.1 | 1.7 | 1.3 | 1.1 | 1.6 | 1.6 | 1.8 | 1.8 | 0.1 |
| Female | 3.2 | 2.1 | 3.1 | 2.5 | 2.2 | 2.3 | 1.7 | 1.6 | 2.1 | 1.9 | 0.01 |
| 45 to 49 | |||||||||||
| Male | 1.8 | 1.8 | 1.4 | 1.7 | 1.7 | 2.2 | 1.8 | 1.8 | 1.6 | 1.5 | 0.9 |
| Female | 2.5 | 3.2 | 2.8 | 2.9 | 2.0 | 2.7 | 2.2 | 2.3 | 1.9 | 2.1 | 0.01 |
| 50 to 54 | |||||||||||
| Male | 2.6 | 2.5 | 2.1 | 2.6 | 2.5 | 2.1 | 2.3 | 2.4 | 2.3 | 2.1 | 0.1 |
| Female | 3.9 | 3.6 | 3.9 | 3.6 | 2.8 | 2.6 | 2.9 | 2.6 | 2.2 | 2.8 | <0.01 |
Table 3b.
In-hospital Mortality (in %) by Race and Gender among Patients with AMI aged 30–54 years in the US, 2001–2010
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Black men | 2.7 | 3.2 | 2.8 | 3.4 | 3.0 | 2.7 | 2.6 | 2.2 | 2.1 | 1.6 |
| White men | 2.1 | 1.8 | 1.4 | 2.2 | 1.7 | 1.9 | 1.8 | 1.9 | 1.8 | 1.8 |
| Black women | 4.8 | 5.2 | 5.2 | 4.1 | 2.4 | 2.7 | 2.9 | 1.8 | 3.5 | 2.1 |
| White women | 3.0 | 2.6 | 2.8 | 2.9 | 2.5 | 2.7 | 2.2 | 2.4 | 1.8 | 2.2 |
Table 4a.
Length-of-Stay (in days) among Men and Women with AMI aged 30–54 years in the US, 2001–2010*
| Age (years) | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P-for-trend |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | |||||||||||
| Male | 4.1 | 4.0 | 4.0 | 4.0 | 3.8 | 3.9 | 3.8 | 3.8 | 3.9 | 3.8 | 0.1 |
| Female | 4.4 | 4.5 | 4.5 | 4.4 | 4.2 | 4.4 | 4.1 | 4.1 | 4.2 | 4.0 | <0.01 |
| 30 to 34 | |||||||||||
| Male | 3.8 | 3.3 | 3.8 | 3.7 | 3.6 | 3.6 | 3.4 | 3.5 | 3.7 | 3.5 | 0.3 |
| Female | 4.1 | 4.8 | 4.1 | 4.2 | 3.5 | 4.2 | 4.3 | 3.8 | 3.9 | 4.0 | 0.5 |
| 35 to 39 | |||||||||||
| Male | 3.5 | 3.5 | 3.6 | 3.5 | 3.6 | 3.6 | 3.4 | 3.4 | 3.3 | 3.6 | 0.4 |
| Female | 3.8 | 4.1 | 4.1 | 4.1 | 4.0 | 4.1 | 3.8 | 3.9 | 3.7 | 3.6 | 0.6 |
| 40 to 44 | |||||||||||
| Male | 3.8 | 3.7 | 3.7 | 3.5 | 3.5 | 3.6 | 3.4 | 3.5 | 3.6 | 3.5 | 0.04 |
| Female | 4.2 | 4.1 | 4.0 | 3.8 | 3.8 | 3.9 | 3.9 | 3.9 | 3.9 | 3.7 | 0.5 |
| 45 to 49 | |||||||||||
| Male | 4.0 | 3.9 | 4.0 | 3.9 | 3.7 | 3.8 | 3.7 | 3.8 | 3.8 | 3.7 | 0.1 |
| Female | 4.3 | 4.5 | 4.5 | 4.3 | 3.9 | 4.3 | 3.9 | 4.0 | 4.2 | 4.0 | <0.01 |
| 50 to 54 | |||||||||||
| Male | 4.3 | 4.2 | 4.2 | 4.3 | 4.1 | 4.1 | 4.2 | 4.1 | 4.1 | 4.0 | 0.3 |
| Female | 4.6 | 4.8 | 4.8 | 4.8 | 4.7 | 4.7 | 4.4 | 4.3 | 4.5 | 4.2 | <0.01 |
All values are in days
Table 4b.
Length-of-Stay by Race and Gender among Patients with AMI aged 30–54 years in the US, 2001–2010*
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Black men | 4.8 | 4.7 | 4.8 | 4.6 | 4.2 | 4.7 | 4.3 | 4.4 | 4.0 | 4.5 |
| White men | 4.1 | 3.8 | 3.9 | 3.9 | 3.7 | 3.8 | 3.6 | 3.7 | 3.7 | 3.6 |
| Black women | 4.7 | 5.3 | 5.4 | 5.0 | 5.0 | 5.3 | 4.8 | 4.6 | 4.7 | 4.4 |
| White women | 4.2 | 4.3 | 4.4 | 4.3 | 4.0 | 4.1 | 4.0 | 3.9 | 4.0 | 3.9 |
All values are in days
Discussion
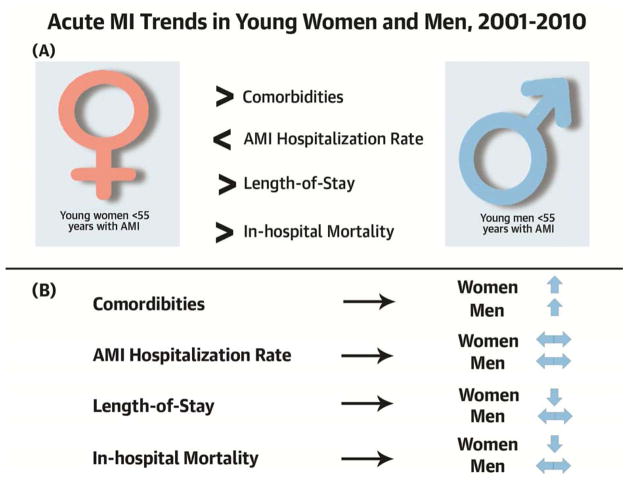
Utilizing a national all-payer database, we found several important sex and race differences among younger patients with AMI. First, in contrast to what is occurring in older patients (8), younger people are not experiencing reductions in AMI hospitalizations. In addition, differences between hospitalization rates of blacks and whites are much more pronounced among young women as compared with men (Central Illustration). We demonstrate that young women with AMI have a higher prevalence of several comorbidities than men and that prevalence of comorbidities has increased in both groups over the past decade. Additionally, young women had higher in-hospital mortality and longer LOS as compared with men.
Our most notable finding is that we did not find significant declines in hospitalization rates among young women and men across all age subgroups from 2001 to 2010. This observation is in contrast to the Medicare population studies in which we described a greater than 20% decline in hospitalization rates for AMI during this time period (8). One potential explanation for this difference could be lack of awareness and poorer control of risk factors among the young population. The National Health and Nutrition Examination Survey (NHANES) reports that while significant reductions were observed in the proportion of the U.S. population having at least 1 of the 3 cardiovascular risk factors (uncontrolled blood pressure, elevated low-density lipoprotein, and current smoking) in the elderly, no significant declines were observed for women younger than 60 years of age and men younger than 40 years from 1999 to 2010 (9). In general, coronary heart disease at younger ages is strongly influenced by genetic factors that are harder to modify resulting in a less impressive decline in hospitalization rates as compared with the elderly (10). Moreover, it is possible that young persons, who are more likely to survive a hospitalization for AMI, have more admissions for a subsequent AMI. If the rate of these subsequent events is not declining then it could be responsible for less prominent hospitalization rate declines in this age group.
We did observe that subgroups of men aged 40–54 years showed a trend toward decreasing AMI rates, but women showed either no change or an increasing trend for most age subgroups. This finding is consistent with studies that reported an increasing trend for hospitalization rates among young women less than 55 years, including a recent study from British Columbia (1,11). In the general U.S. population, the 10-year risk for incident cardiovascular disease has not decreased at the same rate in women as compared with men and the Framingham coronary risk score has actually increased in women 35 to 54 years of age (12,13). Also, women belonging to the peri-menopausal age group may have abnormal lipid levels that might contribute to the increased risk for AMI in young women (14). In fact, prevalence of dyslipidemia among women in our study was highest in those aged 50–54 years, which is consistent with population-based estimates from NHANES (15). It is also possible that these findings suggest inadequacy of screening and risk factor control (like hypertension and elevated cholesterol) efforts among women (16,17). Black women had much higher rates than white women, while black and white men had comparable AMI hospitalization rates. Black women also had the highest prevalence of several comorbidities including hypertension, diabetes, and heart failure in our study. Our findings are consistent with a separate study that demonstrated a markedly higher prevalence of multiple cardiovascular risk factors in black women as compared with white women with AMI (18). In another study, black women were less likely to have optimal blood pressure and cholesterol control compared with white women (19).
We found that young women had higher in-hospital mortality as compared with men across all age subgroups. This is consistent with studies reporting a higher likelihood of mortality in young women with AMI as compared with men (11). Women have longer presentation and treatment times after symptom onset as compared with men that may account for worse in-hospital mortality among them (20). It is interesting to note that in-hospital mortality declined significantly in almost all age subgroups of young women, but similar declines were not observed among men. Meanwhile, while presentation time continues to be higher in women, there has been significant reduction in the recent decade, which may account for improving inhospital outcomes as well (21).
Limitations
Our study has some limitations. First, we did not have detailed clinical data to assess severity of AMI hospitalization or quality of care and treatments delivered. Second, ‘hospitalization rates’ do not include all AMIs as we were unable to account for pre-hospital mortality. Moreover, patients in this dataset are not linked and as a result we are not able to differentiate first AMI from subsequent AMI. In addition, we were not able to assess whether pre-hospital or post-discharge mortality increased to offset declines in inpatient mortality observed among young women. Further, estimates of prevalence of dyslipidemia are based on claims data and definitions are not standardized. Also, not all HCUP states report ethnicity data and thus trends in race-analyses may not apply to all states. Finally, we relied on administrative data to obtain information on comorbidities.
Conclusions
In conclusion, AMI hospitalization rates have not declined for young women and men from 2001 to 2010. Moreover, trends in the frequencies of comorbidities have increased for both women and men hospitalized with AMI in the past decade, suggesting a greater need for intensive primary prevention efforts in the high-risk young population. Racial differences for AMI hospitalizations in young patients were more pronounced for women as compared with men, which require further study about underlying causes and remedies. Although in-hospital mortality rates are declining for young women, they remain higher than men. The reasons contributing to these trends warrant further investigation to identify the biological, clinical, and social factors that contribute to these differences.
Figure 3. Central Illustration: Acute MI Trends in Young Women and Men, 2001–2010.
(A) Overall comparisons of comorbidities, hospitalization rates, and short term outcomes in young women with AMI as compared to young men (B) Trends in young women and men with AMI, 2001–2010
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE1
Hospitalization rates for younger patients with acute myocardial infarction (AMI) have not declined as they have for older people.
COMPETENCY IN MEDICAL KNOWLEDGE 2
Among younger patients hospitalized with AMI, women have more comorbidities, longer stays and higher mortality rates than men.
COMPETENCY IN INTERPERSONAL AND COMMUNICATION SKILLS
Physicians and other health care professionals should seek opportunities to inform patients, the public and policy-makers about cardiovascular disease risk factors and direct resources toward younger segments of the population for primary prevention.
COMPETENCY IN PATIENT CARE
Because of their generally greater burden of comorbidities, young women may gain more benefit from aggressive control of cardiovascular risk factors, including early identification and treatment of hypertension, hyperlipidemia, obesity, smoking, diabetes, and other modifiable risk factors.
TRANSLATIONAL OUTLOOK 1
Mechanisms underlying the higher risks associated with AMI in young women than men warrant further investigation to identify the gender-specific biological, clinical and social factors responsible.
TRANSLATIONAL OUTLOOK 2
Racial differences in hospitalizations for AMI in young patients were more pronounced among women compared to men, warranting merit further investigation of potential causes.
Acknowledgments
Funding: This work was supported by grant U01 HL105270-04 (Center for Cardiovascular Outcomes Research at Yale University) and grant R01 LH081153-06 [Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO)], both from the National Heart, Lung, and Blood Institute.
ABBREVIATIONS AND ACRONYMS
- AMI
Acute myocardial infarction
- HCUP
Healthcare Cost and Utilization Project
- NIS
Nationwide Inpatient Sample
- LOS
Length-of-stay
Footnotes
Relationships with Industry: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Towfighi A, Markovic D, Ovbiagele B. National gender-specific trends in myocardial infarction hospitalization rates among patients aged 35 to 64 years. Am J Cardiol. 2011;108:1102–7. doi: 10.1016/j.amjcard.2011.05.046. [DOI] [PubMed] [Google Scholar]
- 2. [Accessed:12/24/2013];The Go Red For Women Campaign. Available at: http://www.goredforwomen.org/
- 3.HCUP-NIS Database information. [Accessed: 12/13/2013]; Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2011.pdf.
- 4.Healthcare Cost and Utilization Project. [Accessed: 12/26/2013];HCUP Methods Series. Available at http://www.hcup-us.ahrq.gov/reports/methods/methods_topic.jsp.
- 5. [Accessed: 02/12/2014];Comparative Analysis of HCUP and NHDS Inpatient Discharge Data. Available at: http://www.ahrq.gov/research/data/hcup/nhds/niscomp.html.
- 6.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113:1683–92. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 7.Healthcare Cost and Utilization Project. [Accessed: 12/24/2013];Nationwide Inpatient Sample Trends Supplemental Files. Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/nistrends.jsp.
- 8.Chen J, Normand SL, Wang Y, et al. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–8. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 9.Fryar CD, Chen TC, Li X. Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010. NCHS Data Brief. 2012:1–8. [PubMed] [Google Scholar]
- 10.Marenberg ME, Risch N, Berkman LF, et al. Genetic susceptibility to death from coronary heart disease in a study of twins. N Engl J Med. 1994;330:1041–6. doi: 10.1056/NEJM199404143301503. [DOI] [PubMed] [Google Scholar]
- 11.Izadnegahdar M, Singer J, Lee MK, et al. Do Younger Women Fare Worse? Sex Differences in Acute Myocardial Infarction Hospitalization and Early Mortality Rates Over Ten Years. J Womens Health (Larchmt) 2013 doi: 10.1089/jwh.2013.4507. [DOI] [PubMed] [Google Scholar]
- 12.Towfighi A, Zheng L, Ovbiagele B. Sex-specific trends in midlife coronary heart disease risk and prevalence. Arch Intern Med. 2009;169:1762–6. doi: 10.1001/archinternmed.2009.318. [DOI] [PubMed] [Google Scholar]
- 13.Lopez-Jimenez F, Batsis JA, Roger VL, et al. Trends in 10-year predicted risk of cardiovascular disease in the United States, 1976 to 2004. Circ Cardiovasc Qual Outcomes. 2009;2:443–50. doi: 10.1161/CIRCOUTCOMES.108.847202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matthews KA, Crawford SL, Chae CU, et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol. 2009;54:2366–73. doi: 10.1016/j.jacc.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toth PP, Potter D, Ming EE. Prevalence of lipid abnormalities in the United States: the National Health and Nutrition Examination Survey 2003–2006. J Clin Lipidol. 2012;6:325–30. doi: 10.1016/j.jacl.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 17.Persell SD, Baker DW. Aspirin use among adults with diabetes: recent trends and emerging sex disparities. Arch Intern Med. 2004;164:2492–9. doi: 10.1001/archinte.164.22.2492. [DOI] [PubMed] [Google Scholar]
- 18.Leifheit-Limson EC, Spertus JA, Reid KJ, et al. Prevalence of Traditional Cardiac Risk Factors and Secondary Prevention Among Patients Hospitalized for Acute Myocardial Infarction (AMI): Variation by Age, Sex, and Race. J Womens Health (Larchmt) 2013;22:659–66. doi: 10.1089/jwh.2012.3962. [DOI] [PubMed] [Google Scholar]
- 19.Jha AK, Varosy PD, Kanaya AM, et al. Differences in medical care and disease outcomes among black and white women with heart disease. Circulation. 2003;108:1089–94. doi: 10.1161/01.CIR.0000085994.38132.E5. [DOI] [PubMed] [Google Scholar]
- 20.Ting HH, Bradley EH, Wang Y, et al. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med. 2008;168:959–68. doi: 10.1001/archinte.168.9.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaul P, Armstrong PW, Sookram S, et al. Temporal trends in patient and treatment delay among men and women presenting with ST-elevation myocardial infarction. Am Heart J. 2011;161:91–7. doi: 10.1016/j.ahj.2010.09.016. [DOI] [PubMed] [Google Scholar]