Abstract
Allergic diseases, such as asthma and allergic rhinitis, are common. Therefore, the discovery of therapeutic drugs for these conditions is essential. Methyleugenol (ME) is a natural compound with antiallergic, antianaphylactic, antinociceptive, and anti-inflammatory effects. This study examined the antiallergic effect of ME on IgE-mediated inflammatory responses and its antiallergy mechanism in the mast cell line, RBL-2H3. We found that ME significantly inhibited the release of β-hexosaminidase, tumor necrosis factor- (TNF-) α, and interleukin- (IL-) 4, and was not cytotoxic at the tested concentrations (0–100 μM). Additionally, ME markedly reduced the production of the proinflammatory lipid mediators prostaglandin E2 (PGE2), prostaglandin D2 (PGD2), leukotriene B4 (LTB4), and leukotriene C4 (LTC4). We further evaluated the effect of ME on the early stages of the FcεRI cascade. ME significantly inhibited Syk phosphorylation and expression but had no effect on Lyn. Furthermore, it suppressed ERK1/2, p38, and JNK phosphorylation, which is implicated in proinflammatory cytokine expression. ME also decreased cytosolic phospholipase A2 (cPLA2) and 5-lipoxygenase (5-LO) phosphorylation and cyclooxygenase-2 (COX-2) expression. These results suggest that ME inhibits allergic response by suppressing the activation of Syk, ERK1/2, p38, JNK, cPLA2, and 5-LO. Furthermore, the strong inhibition of COX-2 expression may also contribute to the antiallergic action of ME. Our study provides further information about the biological functions of ME.
1. Introduction
Allergic airway diseases, such as asthma and allergic rhinitis, are common diseases caused by hypersensitivity of the immune system. Approximately 10–20% of the world population is affected by allergies, with the number of allergy patients increasing annually [1, 2]. Most allergy patients are genetically predisposed to produce IgE. Mast cells are a key player in early allergic response, which typically occurs within minutes of exposure to an appropriate antigen, and other biological responses, including inflammatory disorders [3]. These cells are critical effector cells in IgE-dependent immediate hypersensitivity reactions [4]. Mast cell degranulation can initiate an acute inflammatory response and contribute to the progression of chronic diseases [5]. When an IgE-antigen binds with FcεRI, the receptor is activated, and a variety of biologically active mediators are released, causing allergic reactions, including the release of β-hexosaminidase, a common degranulation marker, histamine, arachidonic acid metabolites, and inflammatory cytokines [6]. Importantly, arachidonic acid metabolites, including prostaglandins and leukotrienes, mediate acute and chronic allergic reactions [7, 8]. RBL-2H3 cells are a mast cell line that originated from rat basophilic leukemia and have been widely used to study IgE-FcεRI interactions and degranulation. Furthermore, RBL-2H3 cells are a useful model for in vitro screening of antiallergy drug candidates.
The MAP kinase cascade is an important signaling pathway that regulates the differentiation, activation, proliferation, degranulation, and migration of immune cells, including mast cells [9]. MAPK signaling molecules are divided into three groups: extracellular signal-regulated kinase (ERK) 1/2, p38 MAPK, and c-JunNH2-terminal kinase (JNK) 1/2. Erk1/2 is an essential signal in the production of interleukin- (IL-) 5, tumor necrosis factor- (TNF-) α, IL-3, and IL-13 in mast cells [10]. p38 MAP kinase stimulates IL-4 production in bone marrow mast cells (BMMCs) [11]. Additionally, the activation of JNK is also responsible, at least partially, for the expression and production of several cytokines, including TNF-α, IL-2, and IL-6 in mast cells [12, 13].
Methyleugenol (ME,1-allyl-3,4-dimethoxybenzene) is an analog of the phenolic compound eugenol, and it is found in essential oils, including basil, anise, clove, lemon grass, and laurel leaf oils. In East Asia, ME is found in the essential oil fraction of Asiasari radix (Xixin in Chinese). It is used as a flavoring substance in dietary products, including cookies, ice cream, and nonalcoholic beverages, and is found in cosmetics, shampoos, soaps, fragrances, and herbal products in Europe, the USA, and other countries [14]. Previous work indicates that ME exerts antiallergic [15], antispasmodic [16], antinociceptive [14], and anti-inflammatory [17] effects. It was reported that ME inhibited passive cutaneous anaphylaxis (PCA) in rats, release of 5-lipoxygenase (5-LO) from RBL-1 cells and leukotriene D4 (LTD4) induced constriction of guinea pig ileum. ME also inhibited compound 48/80-induced systemic anaphylaxis and antidinitrophenyl IgE-induced local anaphylaxis in mice [18]. However, the effects of ME on allergic response in IgE-activated RBL-2H3 cells and its antiallergic mechanism remain unknown.
In this study, we investigated the antiallergic effects of ME in IgE-activated RBL-2H3 cells. Furthermore, we evaluated the mechanisms responsible for the antiallergic effects of ME.
2. Materials and Methods
2.1. Reagents
ME was purchased from the National Institute for Food and Drug Control (Beijing, China; purity, ≥99.5%). Dulbecco's minimum essential medium (DMEM), penicillin, streptomycin, and fetal bovine serum (FBS) were purchased from GIBCO (Grand Island, NY, USA). 4-[3-(4-Iodophenyl)-2-4(4-nitrophenyl)-2H-5-tetrazolio]-1,3-benzene disulfonate (WST-1) was obtained from Dojindo (Kumamoto, Japan). Specific antibodies against phospho-Lyn, Lyn, phospho-Syk, Syk, phospho-ERK1/2, ERK1/2, phospho-p38, p38, phospho-JNK, JNK, cytosolic phospholipase A2 (cPLA2), phospho-cPLA2, cyclooxygenase-2 (COX-2), and β-actin were purchased from Cell Signaling Technology (Beverly, MA, USA). Specific antibodies against phospho-5-lipoxygenase (5-LO) and 5-LO, and enzyme immunoassay (EIA) kits for prostaglandin E2 (PGE2), prostaglandin D2 (PGD2), leukotriene B4 (LTB4), and leukotriene C4 (LTC4) were purchased from Cayman Chemical (Ann Arbor, MI, USA). The enzyme-linked immunosorbent assay (ELISA) kits for TNF-α and IL-4 were obtained from Bangyi Technologies Inc. (Shanghai, China). Dinitrophenyl- (DNP-) IgE was obtained from Sigma-Aldrich (St Louis, MO, USA), and DNP-bovine serum albumin (BSA) was obtained from Biosearch Technologies Inc. (Novato, CA, USA). All other chemicals were of analytical grade and were purchased from Sigma-Aldrich.
2.2. Cell Culture
RBL-2H3 cells were purchased from the Type Culture Collection of the Chinese Academy of Sciences (Shanghai, China). Cells were cultured in DMEM medium supplemented with 10% FBS and antibiotics (100 U/mL penicillin and 100 μg/mL streptomycin) at 37°C in a humidified 5% CO2 atmosphere.
2.3. Cytotoxicity Assay
Cell respiration served as an indicator of cell viability and was determined by measuring the mitochondrial-dependent reduction of WST-1 to water-soluble tetrazolium salt [19]. Briefly, RBL-2H3 cells were seeded onto a 96-well plate (1 × 104 cells/well) in DMEM with 10% FBS at 37°C overnight. The cells were washed and incubated with DNP-IgE (10 μg/mL) for 24 h. The IgE-sensitized cells were incubated with ME (0–100 μM) for 1 h and stimulated with DNP-BSA (100 ng/mL) for 4 h. WST-1 reagent (10 μL) was added, and the mixture was further incubated for 1 h. Cell viability was determined by measuring the difference in absorbance at a wavelength of 450 nm.
2.4. β-Hexosaminidase Release Activity
RBL-2H3 cells were incubated in a 24-well plate (2 × 105 cells/well) at 37°C overnight. The cells were washed with 1× PBS and incubated with DNP-IgE (10 μg/mL) for 24 h. The IgE-sensitized cells were incubated with ME (0–100 μM) for 1 h, followed by 4 h incubation with DNP-BSA (100 ng/mL). To measure β-hexosaminidase activity, the culture medium was centrifuged (17,000 ×g, 10 min) at 4°C. The supernatant (25 μL) was mixed with 10 mM poly-N-acetyl glucosamine (p-NAG; 50 μL) in 0.1 M sodium citrate buffer (pH 4.5) in a 96-well plate and incubated for 1 h at 37°C. The reaction was terminated by stop buffer (0.1 M Na2CO3 buffer, pH 10.0). The β-hexosaminidase activity was determined by measuring the difference in absorbance at 405 nm. Data were displayed as the mean ± standard deviation (SD) of triplicate experiments.
2.5. ELISA
To measure the TNF-α and IL-4 concentrations in the culture media, all samples were centrifuged (17,000 ×g, 10 min) at 4°C and stored at −80°C until analysis. The TNF-α and IL-4 concentrations were measured using ELISA kits according to the manufacturer's instructions. Data were displayed as the mean ± SD of triplicate experiments.
2.6. EIA
To determine the PGE2, PGD2, LTB4, and LTC4 concentrations in the culture media, all samples were centrifuged (17,000 ×g for 10 min) at 4°C, and the supernatant was stored at −80°C until analysis. The PGE2, PGD2, LTB4, and LTC4 concentrations were measured with EIA kits according to the manufacturer's instructions. Data were displayed as the mean ± SD of triplicate experiments.
2.7. Western Blot Analysis
RBL-2H3 cells were seeded onto a 6-well plate (5 × 105 cells/well) in DMEM with 10% FBS at 37°C overnight. The cells were washed and incubated with DNP-IgE (10 μg/mL) for 24 h. The cells were then incubated in ME (0−100 μM) for 1 h and stimulated with DNP-BSA (100 ng/mL) for 4 h. The harvested cells were lysed, and the target protein was resuspended in protein lysis buffer. The cell lysates were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to polyvinylidene fluoride (PVDF) membranes. The membranes were then incubated with a 1 : 1,000 dilution of specific antibodies against phospho-Lyn, Lyn, phospho-Syk, Syk, phospho-ERK1/2, ERK1/2, phospho-p38, p38, phospho-JNK, JNK, phospho-cPLA2, cPLA2, COX-2, and β-actin and antibodies against phospho-5-LO and 5-LO. The blots were washed with TBS-T and incubated in a 1 : 5,000 dilution of horseradish peroxidase-conjugated IgG secondary antibodies. The proteins on the membranes were detected using a chemiluminescent reaction, and the membranes were exposed to Hyperfilm ECL. The target protein concentrations were compared to the control concentrations, and the results for each protein were expressed as a density ratio based on a protein standard size marker. The density of each band was determined using ImageJ software.
2.8. Statistical Analysis
The results were expressed as mean ± standard deviation (SD) and differences between mean values of normally distributed data were assessed by the one-way analysis of variance (ANOVA) followed by Duncan's test for multiple comparisons. P values of 0.05 or 0.01 were considered statistically significant.
3. Results
3.1. Inhibitory Effect of ME on IgE-Mediated Allergic Response in RBL-2H3 Cells
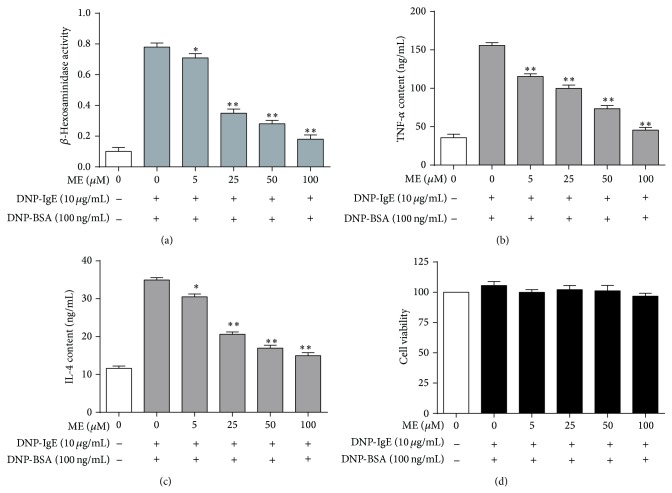
To determine the optimal concentrations of ME for our study, we assessed the cytotoxicity of ME and antigen (DNP-BSA) cotreatment. We treated the RBL-2H3 mast cells with ME concentrations ranging from 1 to 100 μM in subsequent experiments. The IgE-sensitized RBL-2H3 cells were exposed to ME at various concentrations (0−100 μM) for 1 h and stimulated with 100 ng/mL DNP-BSA for 4 h for the β-hexosaminidase assay. ME markedly inhibited the release of β-hexosaminidase (Figure 1(a)), which is a general biomarker of degranulation and a hallmark characteristic of allergic reactions caused by allergen exposure. Additionally, the release of TNF-α and IL-4, two proinflammatory cytokines, from RBL-2H3 cells was markedly suppressed by ME in a dose-dependent manner (Figures 1(b) and 1(c)). ME treatment (0−100 μM) for 24 h produced no significant cytotoxic effect (Figure 1(d)).
Figure 1.
Effect of ME on activity of β-hexosaminidase and level of TNF-α, IL-4 released in IgE-activated RBL-2H3 cells. RBL-2H3 cells were seeded on a 24-well plate in DMEM with 10% FBS at 37°C overnight, and then the cells were washed and further incubated with DNP-IgE for 24 h. The cells were incubated with ME (0–100 μM) for 1 h and then stimulated by DNP-BSA (100 ng/mL) for 4 h. β-Hexosaminidase activity (a) and TNF-α level (b) and IL-4 level (c) were determined as described in Section 2. RBL-2H3 cells were seeded on a 96-well plate (2.5 × 104 cells/well) in DMEM with 10% FBS at 37°C overnight, and then the cells were washed and further incubated with DNP-IgE for 24 h. The cells were incubated with ME (0–100 μM) for 1 h, simultaneously treated with DNP-BSA (100 ng/mL) and WST-1 reagent (10 μL), and then incubated for 4 h. Cell viability (d) was determined as described in Section 2. Data represent the mean ± SD of three independent experiments and differences between mean values were assessed by one-way ANOVA. * P < 0.05, ** P < 0.01 indicate significant differences compared with the DNP-BSA-treated group.
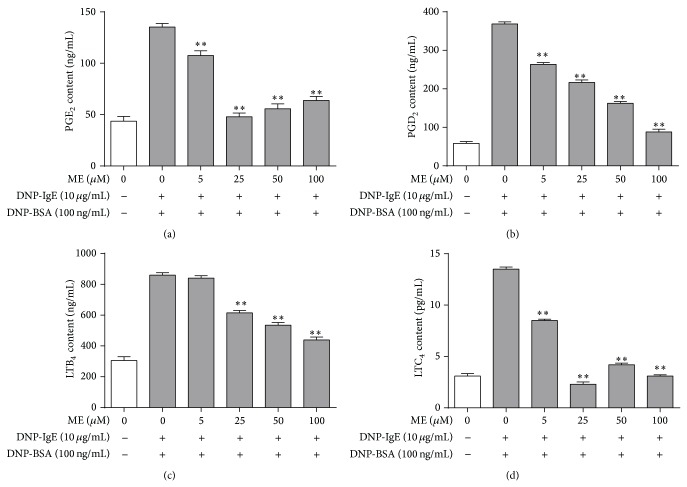
3.2. Inhibitory Effects of ME on the Formation of Proinflammatory Lipid Mediators
We next examined the effect of ME on the formation of PGE2, PGD2, LTB4, and LTC4, which are proinflammatory lipid mediators that regulate allergic response [20–23] produced via arachidonate signaling downstream of IgE-mediated FcεRI activation [24]. RBL-2H3 cells were preincubated with ME (0–100 μM) prior to antigen challenge, and the formation of PGE2, PGD2, LTB4, and LTC4 was measured by EIA assay. As shown in Figure 2, ME markedly inhibited the formation of PGE2, PGD2, and LTC4 and suppressed LTB4 formation to a lesser extent. Collectively, these results suggest that ME suppresses allergic inflammation induced by PGE2, PGD2, LTB4, and LTC4. This indicates that ME directly inhibits an enzyme involved in prostaglandin and leukotriene biosynthesis.
Figure 2.
Effect of ME on formation of PGE2, PGD2, LTB4, and LTC4 in IgE-activated RBL-2H3 cells. RBL-2H3 cells were seeded on a 24-well plate in DMEM with 10% FBS at 37°C overnight, and then the cells were washed and further incubated with DNP-IgE for 24 h. The cells were incubated with ME (0–100 μM) for 1 h and then stimulated by DNP-BSA for 4 h. The amounts of PGE2 (a), PGD2 (b), LTB4 (c), and LTC4 (d) were determined as described in Section 2. Data represent the mean ± SD of three independent experiments and differences between mean values were assessed by one-way ANOVA. * P < 0.05, ** P < 0.01 indicate significant differences compared with the DNP-BSA-treated group.
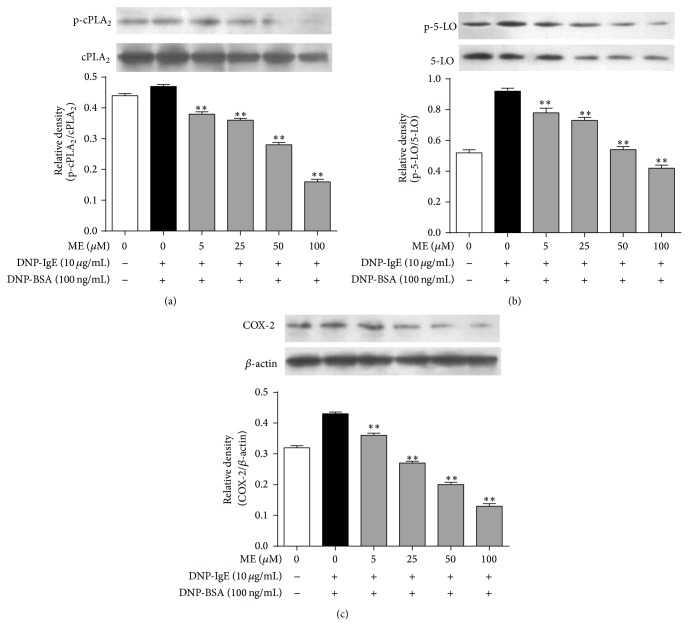
3.3. Regulatory Effects of ME on Enzymes Associated with the Arachidonate Cascade
We additionally investigated the antiallergic effects of ME on the activation of enzymes in the arachidonate cascade. Arachidonate cascade activation has been implicated in FcεRI receptor activation in IgE-activated mast cells [22]. Therefore, we hypothesized that ME, which showed antiallergic effects, would affect cPLA2, 5-LO, or COX-2 activation (Figure 3). When the IgE-sensitized RBL-2H3 cells were exposed to ME at various concentrations for 1 h prior to antigen stimulation, phosphorylation of cPLA2, the rate-limiting step of the arachidonate cascade, was diminished. Similarly, ME suppressed 5-LO phosphorylation, the rate-limiting step of leukotriene biosynthesis, and inhibited COX-2 expression, which catalyzes the rate-limiting step of prostaglandin biosynthesis. These findings indicate that ME decreases the activation of several targets, including cPLA2, 5-LO, and COX-2, suggesting that the antiallergic action of ME may be mediated by arachidonate cascade suppression.
Figure 3.
Effect of ME on a late stage of the FcεRI signal cascade in IgE-activated RBL-2H3 cells. RBL-2H3 cells were seeded on a 6-well plate in DMEM with 10% FBS at 37°C overnight, and then the cells were washed and further incubated with DNP-IgE for 24 h. The cells were incubated with ME (0–100 μM) for 1 h and then stimulated by DNP-BSA for 4 h. The cells were rinsed and lysed with a cell lysis buffer. The expression of p-cPLA2, cPLA2, p-5-LO, 5-LO, COX-2, and β-actin was determined as described in Section 2. Data represent the mean ± SD of three independent experiments and differences between mean values were assessed by one-way ANOVA. * P < 0.05, ** P < 0.01 indicate significant differences compared with the DNP-BSA-treated group.
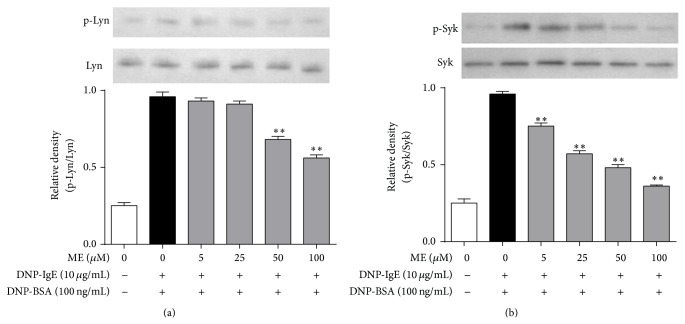
3.4. Suppressive Effect of ME on FcεRI Signaling Pathway
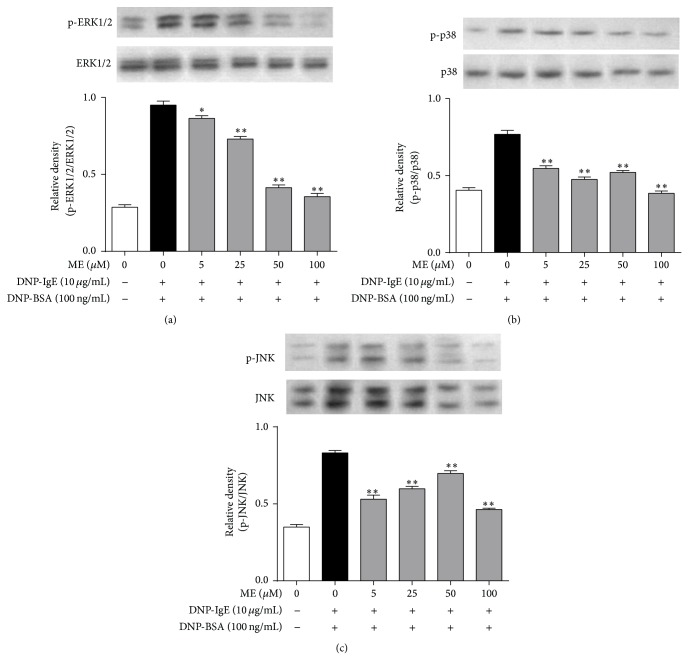
Next, we investigated the mechanism of the antiallergic action of ME. Activation of the FcεRI receptor induces Lyn and Syk phosphorylation, mediating the degranulation of mast cells [22]. In this respect, ME may affect Lyn or Syk phosphorylation in the early phase of the FcεRI receptor cascade. When RBL-2H3 cells were preincubated with ME for 1 h before antigen challenge, and the incubation was extended an additional 10 min, the phosphorylation of Syk, but not Lyn, was inhibited in a dose-dependent manner (Figure 4). Notably, ME markedly reduced the expression and phosphorylation of ERK1/2 (Figure 5(a)). Thus, ME could reduce ERK1/2 function by directly suppressing ERK1/2 expression. Additionally, phosphorylation of MAP kinases, such as p38 or JNK, was also suppressed by ME, although p38 phosphorylation was more sensitive to ME (Figures 5(b) and 5(c)).
Figure 4.
Effect of ME on early stage of FcεRI cascade in IgE-activated RBL-2H3 cells. IgE-sensitized RBL-2H3 cells were exposed to ME (0–100 μM) for 1 h and then stimulated by DNP-BSA (100 ng/mL) for 10 min. The cells were rinsed with 1× PBS and lysed with cell lysis buffer. The expression of p-Lyn, Lyn, p-Syk, and Syk was determined as described in Section 2. Data represent the mean ± SD of three independent experiments and differences between mean values were assessed by one-way ANOVA. * P < 0.05, ** P < 0.01 indicate significant differences compared with the DNP-BSA-treated group.
Figure 5.
Effect of ME on MAP kinase pathway in IgE-activated RBL-2H3 cells. IgE-sensitized RBL-2H3 cells were exposed to ME (0–100μM) for 1 h and then stimulated by DNP-HSA (100 ng/mL) for 10 min. The cells were rinsed with 1× PBS and lysed with cell lysis buffer. The expression of p-ERK1/2, ERK1/2, p-p38, p38, p-JNK1/2, or JNK1/2 was determined as described in Section 2. Data represent the mean ± SD of three independent experiments and differences between mean values were assessed by one-way ANOVA. * P < 0.05, ** P < 0.01 indicate significant differences compared with the DNP-BSA-treated group.
4. Discussion
The essential oil of Asiasari radix has many beneficial health effects, exhibiting anti-inflammatory, antibacterial, and antiallergy properties, as well as affecting the respiratory and circulatory systems [25]. Asiasari radix essential oils contain a considerable number of chemical ingredients, including ME, asarylketone, cineol, safrole, limonene, and eucarvone [26]. Previously, ME was reported to have beneficial effects on inflammation, ischemia, anaphylaxis, and nociception. Our present data demonstrate that ME exerts antiallergic effects in IgE-activated RBL-2H3 cells. ME significantly suppresses degranulation and proinflammatory cytokine release in antigen-sensitized mast cells. Several cytokines play critical roles in allergic inflammation. For example, TNF-α, which is secreted from IgE-activated mast cells, plays an important role in allergic responses [27]. Therefore, the inhibitory effect of ME on TNF-α formation may indicate its added advantage as an antiallergy agent. During the pathogenesis of allergic disease, IL-4 is crucial for the induction of IgE synthesis and mast cell development [28]. IL-4 also modulates the inflammatory response, owing to its ability to affect adhesion molecule expression and cytokine production in endothelial cells, and promotes growth and activation of neutrophils, mast cells, T cells, and eosinophils [29]. These results suggest that ME significantly inhibits mast cell degranulation and proinflammatory cytokine release.
One possible mechanism of ME-induced antiallergic activity may be its effect on the FcεRI signal cascade. IgE-induced degranulation in mast cells is associated with activation of the FcεRI receptor, and this activation induces the release of various inflammatory mediators, including TNF-α, leukotrienes, and prostaglandins via phosphorylation of the Lyn/Syk pathway [23]. In turn, the activation of Syk increases intracellular Ca2+ and the activation of the MAP kinase family [23]. Thus, Lyn and Syk are important intracellular mediators in early signaling following FcεRI receptor activation. In the present study, Syk was markedly inhibited by ME, supporting the notion that it is a primary target of ME. In support of this observation, ME significantly reduced the phosphorylation of ERK1/2, p38, and JNK, which are downstream effectors of FcεRI [23].
In the present study, 100 μM ME obviously inhibited cPLA2 and 5-LO phosphorylation and decreased the formation of the 5-LO products, LTB4 and LTC4. This effect may improve the antiallergy action of ME, because LTB4 is a potent chemoattractant and activator of neutrophils and other immune cells in severe asthma [30, 31]. LTC4 is a potent spasmogenic agent and an agonist of cysteinyl-LT receptors, which are known to induce chronic inflammatory reactions in allergic diseases [21]. Furthermore, ME also inhibited COX-2 expression and dramatically reduced the levels of the COX-2 products PGE2 and PGD2, which are enhanced in activated immune cells, including mast cells [20, 32]. The suppressive effects of ME on PGE2 formation may contribute to its increased antiallergic activity, as PGE2 may mediate asthma development and inflammation associated with IL-4 and IL-5, which are produced by helper T cells [32]. Moreover, the inhibitory effect of ME on PGD2 formation may add to the antiallergic action, as PGD2 is known to cause bronchoconstriction and vasodilation and increases capillary permeability and mucous production in asthma [20]. Collectively, these findings suggest that ME can reduce allergic reactions through suppression of cPLA2 and 5-LO activation and through inhibition of COX-2 activity. Taken together, ME can inhibit allergic reaction by suppressing the activation of Syk, ERK1/2, p38, and JNK and reducing the activity of the enzymes responsible for the biosynthesis of PGD2 and LTB4. Further, these effects may be extended to anti-inflammatory effects on other cells or tissues. Additionally, the expression of TNF-α is associated with p38, JNK, and ERK1/2 activation in the FcεRI receptor cascade in IgE-activated mast cells [23]. Therefore, the reduction of TNF-α formation by ME may provide an additional advantage to ME as an antiallergic agent.
In conclusion, the present study demonstrates that ME has antiallergic effects in IgE-activated RBL-2H3 cells. The mechanisms responsible for its antiallergic effects may involve multiple targets including Sky, ERK1/2, p38, JNK, cPLA2, 5-LO, and COX-2. Such effects may provide further information for the application of ME as an antiallergic agent. Therefore, our future studies will focus on providing additional pharmacological evidence to demonstrate this possibility.
Acknowledgments
This research was supported by the Science and Technology Development Funding Foundation of Guangdong Province (Grant no. 2012A032400002), the Medical Scientific Research Foundation of Guangdong Province (B2013074), the National Natural Science Foundation of China (Grant no. 81202431), and the Natural Science Foundation of Guangdong Province (Grant no. S2012010009576).
Conflict of Interests
The authors declare that they have no conflict of interests.
References
- 1.Flohr C., Quinnell R. J., Britton J. Do helminth parasites protect against atopy and allergic disease? Clinical and Experimental Allergy. 2009;39(1):20–32. doi: 10.1111/j.1365-2222.2008.03134.x. [DOI] [PubMed] [Google Scholar]
- 2.Erb K. J. Can helminths or helminth-derived products be used in humans to prevent or treat allergic diseases? Trends in Immunology. 2009;30(2):75–82. doi: 10.1016/j.it.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Bochner B. S., Schleimer R. P. Mast cells, basophils, and eosinophils: distinct but overlapping pathways for recruitment. Immunological Reviews. 2001;179:5–15. doi: 10.1034/j.1600-065x.2001.790101.x. [DOI] [PubMed] [Google Scholar]
- 4.Galli S. J. New concepts about the mast cell. The New England Journal of Medicine. 1993;328(4):257–265. doi: 10.1056/NEJM199301283280408. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen M., Pace A. J., Koller B. H. Age-induced reprogramming of mast cell degranulation. Journal of Immunology. 2005;175(9):5701–5707. doi: 10.4049/jimmunol.175.9.5701. [DOI] [PubMed] [Google Scholar]
- 6.Gilfillan A. M., Tkaczyk C. Integrated signalling pathways for mast-cell activation. Nature Reviews Immunology. 2006;6(3):218–230. doi: 10.1038/nri1782. [DOI] [PubMed] [Google Scholar]
- 7.Church M. K., Levi-Schaffer F. The human mast cell. Journal of Allergy and Clinical Immunology. 1997;99(2):155–160. doi: 10.1016/S0091-6749(97)70089-7. [DOI] [PubMed] [Google Scholar]
- 8.Metcalfe D. D., Kaliner M., Donlon M. A. The mast cell. Critical Reviews in Immunology. 1981;3(1):23–74. [PubMed] [Google Scholar]
- 9.Duan W., Wong W. S. F. Targeting mitogen-activated protein kinases for asthma. Current Drug Targets. 2006;7(6):691–698. doi: 10.2174/138945006777435353. [DOI] [PubMed] [Google Scholar]
- 10.Lorentz A., Klopp I., Gebhardt T., Manns M. P., Bischoff S. C. Role of activator protein 1, nuclear factor-kappaB, and nuclear factor of activated T cells in IgE receptor-mediated cytokine expression in mature human mast cells. Journal of Allergy and Clinical Immunology. 2003;111(5):1062–1068. doi: 10.1067/mai.2003.1342. [DOI] [PubMed] [Google Scholar]
- 11.Frossi B., Rivera J., Hirsch E., Pucillo C. Selective activation of Fyn/PI3K and p38 MAPK regulates IL-4 production in BMMC under nontoxic stress condition. The Journal of Immunology. 2007;178(4):2549–2555. doi: 10.4049/jimmunol.178.4.2549. [DOI] [PubMed] [Google Scholar]
- 12.Kawakami Y., Hartman S. E., Holland P. M., Cooper J. A., Kawakami T. Multiple signaling pathways for the activation of JNK in mast cells: involvement of Bruton's tyrosine kinase, protein kinase C, and JNK kinases, SEK1 and MKK7. Journal of Immunology. 1998;161(4):1795–1802. [PubMed] [Google Scholar]
- 13.Hata D., Kawakami Y., Inagaki N., et al. Involvement of Bruton's tyrosine kinase in FcepsilonRI-dependent mast cell degranulation and cytokine production. Journal of Experimental Medicine. 1998;187(8):1235–1247. doi: 10.1084/jem.187.8.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yano S., Suzuki Y., Yuzurihara M., et al. Antinociceptive effect of methyleugenol on formalin-induced hyperalgesia in mice. European Journal of Pharmacology. 2006;553(1–3):99–103. doi: 10.1016/j.ejphar.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 15.Hashimoto K., Yanagisawa T., Okui Y., Ikeya Y., Maruno M., Fujita T. Studies on anti-allergic components in the roots of Asiasarum sieboldi. Planta Medica. 1994;60(2):124–127. doi: 10.1055/s-2006-959432. [DOI] [PubMed] [Google Scholar]
- 16.Lima C. C., Criddle D. N., Coelho-De-Souza A. N., Monte F. J. Q., Jaffar M., Leal-Cardoso J. H. Relaxant and antispasmodic actions of methyleugenol on guinea-pig isolated ileum. Planta Medica. 2000;66(5):408–411. doi: 10.1055/s-2000-8594. [DOI] [PubMed] [Google Scholar]
- 17.Choi Y. K., Cho G.-S., Hwang S., et al. Methyleugenol reduces cerebral ischemic injury by suppression of oxidative injury and inflammation. Free Radical Research. 2010;44(8):925–935. doi: 10.3109/10715762.2010.490837. [DOI] [PubMed] [Google Scholar]
- 18.Shin B. K., Lee E. H., Kim H. M. Suppression of L-histidine decarboxylase mRNA expression by methyleugenol. Biochemical and Biophysical Research Communications. 1997;232(1):188–191. doi: 10.1006/bbrc.1997.6260. [DOI] [PubMed] [Google Scholar]
- 19.Ishiyama M., Tominaga H., Shiga M., Sasamoto K., Ohkura Y., Ueno K. A combined assay of cell viability and in vitro cytotoxicity with a highly water-soluble tetrazolium salt, neutral red and crystal violet. Biological and Pharmaceutical Bulletin. 1996;19(11):1518–1520. doi: 10.1248/bpb.19.1518. [DOI] [PubMed] [Google Scholar]
- 20.Arima M., Fukuda T. Prostaglandin D2 and TH2 inflammation in the pathogenesis of bronchial asthma. The Korean Journal of Internal Medicine. 2011;26(1):8–18. doi: 10.3904/kjim.2011.26.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nettis E., D'Erasmo M., di Leo E., et al. The employment of leukotriene antagonists in cutaneous diseases belonging to allergological field. Mediators of Inflammation. 2010;2010:6. doi: 10.1155/2010/628171.628171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kawakami Y., Kitaura J., Satterthwaite A. B., et al. Redundant and opposing functions of two tyrosine kinases, Btk and Lyn, in mast cell activation. Journal of Immunology. 2000;165(3):1210–1219. doi: 10.4049/jimmunol.165.3.1210. [DOI] [PubMed] [Google Scholar]
- 23.Roth K., Chen W. M., Lin T. J. Positive and negative regulatory mechanisms in high-affinity IgE receptor-mediated mast cell activation. Archivum Immunologiae et Therapiae Experimentalis. 2008;56(6):385–399. doi: 10.1007/s00005-008-0041-2. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y., Lee Y.-S., Hahn J.-H., et al. Hyaluronic acid targets CD44 and inhibits FcεRI signaling involving PKCδ, Rac1, ROS, and MAPK to exert anti-allergic effect. Molecular Immunology. 2008;45(9):2537–2547. doi: 10.1016/j.molimm.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y. S. Pharmacology and Application of Chinese Materia Medica. Beijing, China: People’s Health Publisher; 1983. [Google Scholar]
- 26.Zhou R. H. Resource Science of Chinese Medicinal Materials. Beijing, China: China Medical & Pharmaceutical Sciences Press; 1993. [Google Scholar]
- 27.Theoharides T. C., Kalogeromitros D. The critical role of mast cells in allergy and inflammation. Annals of the New York Academy of Sciences. 2006;1088:78–99. doi: 10.1196/annals.1366.025. [DOI] [PubMed] [Google Scholar]
- 28.Nabeshima Y., Hiragun T., Morita E., Mihara S., Kameyoshi Y., Hide M. IL-4 modulates the histamine content of mast cells in a mast cell/fibroblast co-culture through a Stat6 signaling pathway in fibroblasts. FEBS Letters. 2005;579(29):6653–6658. doi: 10.1016/j.febslet.2005.09.104. [DOI] [PubMed] [Google Scholar]
- 29.Boulay J.-L., Paul W. E. The interleukin-4 family of lymphokines. Current Opinion in Immunology. 1992;4(3):294–298. doi: 10.1016/0952-7915(92)90079-T. [DOI] [PubMed] [Google Scholar]
- 30.Ford-Hutchinson A. W., Bray M. A., Doig M. V., Shipley M. E., Smith M. J. H. Leukotriene B, a potent chemokinetic and aggregating substance released from polymorphonuclear leukocytes. Nature. 1980;286(5770):264–265. doi: 10.1038/286264a0. [DOI] [PubMed] [Google Scholar]
- 31.Tager A. M., Luster A. D. BLT1 and BLT2: the leukotriene B(4) receptors. Prostaglandins Leukotrienes and Essential Fatty Acids. 2003;69(2-3):123–134. doi: 10.1016/s0952-3278(03)00073-5. [DOI] [PubMed] [Google Scholar]
- 32.van der Pouw Kraan T. C. T. M., Boeije L. C. M., Smeenk R. J. T., Wijdenes J., Aarden L. A. Prostaglandin-E2 is a potent inhibitor of human interleukin 12 production. Journal of Experimental Medicine. 1995;181(2):775–779. doi: 10.1084/jem.181.2.775. [DOI] [PMC free article] [PubMed] [Google Scholar]