Abstract
To estimate the proportion of healthcare workers (HCWs) willing to work during an influenza pandemic and identify associated risk factors, we undertook a systematic review and meta-analysis compliant with PRISMA guidance. Databases and grey literature were searched to April 2013, and records were screened against protocol eligibility criteria. Data extraction and risk of bias assessments were undertaken using a piloted form. Random-effects meta-analyses estimated (i) pooled proportion of HCWs willing to work and (ii) pooled odds ratios of risk factors associated with willingness to work. Heterogeneity was quantified using the I2 statistic, and publication bias was assessed using funnel plots and Egger's test. Data were synthesized narratively where meta-analyses were not possible. Forty-three studies met our inclusion criteria. Meta-analysis of the proportion of HCWs willing to work was abandoned due to excessive heterogeneity (I2 = 99·2%). Narrative synthesis showed study estimates ranged from 23·1% to 95·8% willingness to work, depending on context. Meta-analyses of specific factors showed that male HCWs, physicians and nurses, full-time employment, perceived personal safety, awareness of pandemic risk and clinical knowledge of influenza pandemics, role-specific knowledge, pandemic response training, and confidence in personal skills were statistically significantly associated with increased willingness. Childcare obligations were significantly associated with decreased willingness. HCWs' willingness to work during an influenza pandemic was moderately high, albeit highly variable. Numerous risk factors showed a statistically significant association with willingness to work despite significant heterogeneity between studies. None of the included studies were based on appropriate theoretical constructs of population behaviour.
Keywords: Healthcare worker, pandemic, willingness to work
Introduction
Although variable in severity,1,2 one consistent feature of pandemic influenza is a surge in demand for health care.3,4 Hospitalization due to influenza A(H1N1)pdm09 in the USA was estimated at approximately 274 000 cases between April 2009 and April 20105 contrasting with 95 000 annual influenza-associated primary hospitalizations from 1979 to 2001.6 In 2009–10, the availability of intensive care unit beds came under pressure in most national health systems.1,7 Healthcare workers (HCWs) play key roles during an influenza pandemic, but a serious shortage of personnel may occur at peak times or in severe pandemics because of absenteeism due to illness, caring for family members who are ill, or refusal to work.8 Effective preparation for the next pandemic requires estimates of HCWs' willingness to work and an understanding of influencing factors.
The available data are highly variable. One Nigerian study found only one quarter of HCWs stating they would be willing to work in a unit treating patients with influenza A(H1N1)pdm09,9 whilst an Australian qualitative study of family physicians found 100% of participants willing to work.10 Chaffee11 first reviewed willingness to work during disasters and reported that the following factors would be influential: type of disaster, concern for close family, friends and pets, responsibility for dependants, the perceived value of one's response, belief in a duty of care, access to personal protective equipment (PPE), provision of basic needs (water, food, rest, shelter and communication tools) and prolonged working hours. Three published reviews reported that similar factors would be associated with willingness to work during an influenza pandemic,12–14 but the data were not summarized quantitatively.
We addressed this evidence gap by conducting a systematic review and meta-analysis in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement. The review questions sought to elucidate the proportion of HCWs willing to work during an influenza pandemic, and to identify risk factors associated with willingness to work. Our findings are interpreted with reference to sociological understandings of population behaviour, which have to date largely been absent from the peer-reviewed literature, but are highly relevant to the development of appropriate interventions to minimize refusal to work.
Methods
Search strategy
The study protocol was registered with the National Institute for Health Research international prospective register of scientific reviews (PROSPERO; #CRD42013004865) prior to executing the literature search strategy.15 The PRISMA checklist is available as supporting information.
We sought to analyse data collected exclusively from HCWs including doctors, nurses, hospital workers, emergency healthcare service workers, public health workers, medical and nursing students, non-clinical support staff and retirees. The outcome measures of interest were the proportion of HCWs reporting willingness to work during an influenza pandemic, and odds ratios or case counts allowing the derivation of odds ratios pertaining to factors associated with willingness to work. We included study manuscripts written in English reporting original quantitative research derived from a cross-sectional design, studies pertaining to a prior or hypothetical influenza pandemic, and studies reporting data pertaining to the aforementioned outcome measures, with no limitations on the time and place of publication.
The following databases were searched from their inception to April 2013: MEDLINE, EMBASE, Web of Knowledge, SCOPUS, AMED, ASSIA, BioEthicsWeb, CINAHL, Cochrane Library and PsycINFO. Google Scholar and OpenGrey were also searched. Search terms were ‘pandemic + influenza + willingness to work/report to work’ to avoid including studies on willingness to accept vaccination. These terms were used in both keyword and MeSH searches as appropriate for each database as follows: #1. pandemics (MeSH); #02. influenza, human (MeSH); #03. ‘attitude of health personnel’ (MeSH) or willingness (keyword); #04. hospital administration (MeSH) or report to work (keyword); #05. willing* adj5 work (keyword); #06. respon* adj5 work (keyword); #07. would come (keyword); #08. #03 OR #04 OR #05 OR #06 OR #07; #09. #01 AND #02 AND #08 (see also Table S1). Reference lists in eligible articles were also searched.
All identified records were imported to endnote software X4 (Thomson Reuters, Toronto, CA, USA) and duplicate entries removed. The remaining records were screened by a single researcher (YA) against the protocol eligibility criteria following a sequential assessment of the study title, abstract and full-text article. Where this was unclear, agreement on eligibility of each study was achieved through discussion with a second researcher (RD or JSN-V-T). Data extraction was performed by a single researcher (YA) using a piloted form collecting details of study characteristics {title, author, publication year, place, study period, study design, participants, subject [pandemic of avian influenza origin/influenza A(H1N1)pdm09/non-specified, hypothetical influenza pandemic]}; definition of outcome measures; questionnaire type; validation; statistical analysis and any stated limitations; percentage of willingness to work; and risk factors association with willingness. Odds ratios (ORs) of factors both unadjusted and adjusted were extracted to estimate the association with willingness to work. Crude case counts and the percentage of people in each risk factor stratum were extracted where available. Risk of bias was assessed for each study using a Newcastle–Ottawa assessment scale modified for cross-sectional studies by Herzog et al.16
Summary measures and analysis
Descriptive statistics were calculated using Microsoft® Office Excel® 2010 (Microsoft Corporation, Richmond, VA, USA). Random-effects meta-analysis estimated the proportion of HCWs (including 95% confidence intervals [CIs]) who reported willingness to work during an influenza pandemic. Random-effect meta-analysis of pooled odds ratios (including 95% CIs) estimated the association of factors with willingness to work.17 Heterogeneity between studies was assessed using the I2 statistic.18 We considered it statistically inappropriate to perform meta-analysis where I2 exceeded 85%.19 To explore sources of heterogeneity, we planned to conduct subgroup analyses according to the type of influenza pandemic; geographical region; survey time period; type of questionnaire; type of participants; sex of participants; and Newcastle–Ottawa assessment scale score. We used Galbraith plots to detect those studies that contributed substantial heterogeneity and conducted sensitivity analyses excluding them from our pooled estimates.20 For each meta-analysis, publication bias was assessed graphically using a funnel plot of effect size versus standard error and statistically using Egger's regression test.21 Meta-analysis of pooled proportions was conducted using statsdirect version 2.7.9 (StatsDirect Ltd., Cheshire, UK), and meta-analysis of pooled odds ratios was conducted using stata® version 11.2 (StataCorp LP, College Station, TX, USA).
Results
Study selection
We identified a total of 1133 unique records of which 43 studies met protocol eligibility criteria (see Figure1). Two studies did not describe the percentage of participants reporting willingness to work; therefore, 41 were included in the meta-analysis of the pooled proportion of HCWs willing to work during an influenza pandemic.
Figure 1.
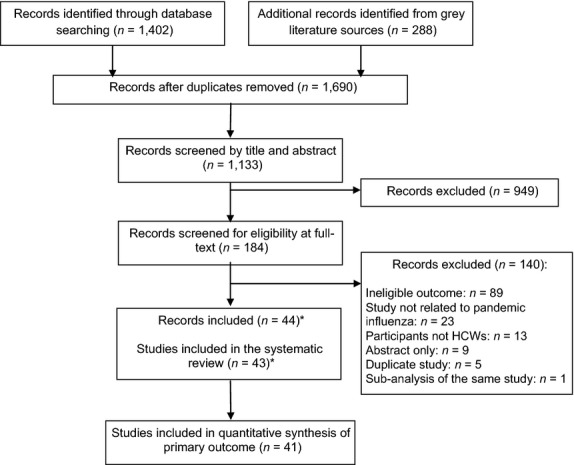
Overview of the selection process. *The findings from one study were reported in two separate papers.51,52
Study characteristics
The included studies comprised entirely of cross-sectional surveys including two pre-/post-intervention studies and are summarized in Table1. The participant population sizes ranged from 60 to 4306 with a median of 725 (interquartile range [IQR] 308–1711). The earliest publication was in 2006, and the majority of articles were published in 2009 (11; 25·6%) and 2010 (13; 30·2%). 28 of 43 (67·4%) studies used a hypothetical influenza pandemic as the subject, 21 (48·8%) were conducted in the USA, and 21 (48·9%) investigated both clinical and non-clinical staff within hospital settings.
Table 1.
Characteristics and results of individual included studies
| Study | Country | Study period | Participants | Sample size (response rate) | Sampling method | Proportion of HCWs willing to work (95% CI) |
|---|---|---|---|---|---|---|
| Hypothetical scenarios of an influenza pandemic | ||||||
| Kaiser (2009)23 | USA | November 2007–March 2008 | Medical students | 523 (61%) | All medical students in the USA | 95·8% (93·7–97·3) |
| Syrett (2007)24 | USA | Before 2003 | Emergency healthcare department workers | 186 (100%) | Convenience (in a medical centre) | 77% (70·2–82·7) |
| Martinese (2009)25 | Australia | 2006 (May–August) | Hospital workers | 560 (98%) | Convenience (attendants of meetings) | 64·2% (60·2–68·3) |
| Barnett (2010)34 | USA | 2009 (May–June) | Emergency medical service's workers | 586 (49%) | Convenience (responders of other survey) | 93·1% (90·8–95·1) |
| Barnett (2009)35 | USA | 2006–2007 | Health department workers | 1835 (83%) | Convenience (all employees in four clusters of local health departments) | 92% (90·7–93·2) |
| Errett (2013)36 | USA | 2009 (June–August) | Medical Reserve Corps | 3181 (not stated) | Convenience (volunteer group units of which leaders had an interest of the survey) | 91·9% (90·9–92·8) |
| Barnett (2012)37 | USA | April 2009–June 2010 | Local public health department workers | 2993 (66%) | Convenience (from 8 local public healthcare departments) | 91% (89·9–92·0) |
| Martin (2011)38 | USA | 2009 (October–December) | Nurses | 735 (61%) | Stratified random (from the licence registry list in the region) | 90·1% (87·7–92·1) |
| Stergachis (2011)39 | USA | 2008 (May–November) | Healthcare workers | 4306 (50%) | Stratified random (from licence database and hospitals in the region) | 89% (88·0–89·9) |
| Seale (2012)40 | China | January 2009 | Hospital workers | 1909 (99%) | Convenience (participants of other RCT in selected wards in 24 hospitals) | 86% (84·4–87·5) |
| Adams (2012)41 | USA | –* | Healthcare workers | 1342 (50%) | Convenience (all staff in selected wards in 6 hospitals) | 85·1% (83·1–87·0) |
| Seale (2009)42 | Australia | 2007 (June–October) | Hospital workers | 1079 (90%) | Convenience (all workers in randomly selected wards in two hospitals) | 83·3% (81·0–85·5) |
| Balicer (2010)43 | USA | 2009 (January–March) | Hospital workers | 3426 (18%) | Convenience (all employees in a hospital) | 82·5% (81·2–83·7) |
| Barr (2008)44 | UK | –* | Hospital workers | 406 (40%) | Convenience (all doctors, medical students attending a lecture and 500 nurses in a hospital) | 79% (74·8–82·9) |
| Daugherty (2009)45 | USA | Early 2007 | ICU and CCU staff | 256 (88%) | Convenience (attendants of meetings in two hospitals) | 79% (73·4–83·7) |
| Cone (2006)46 | USA | 2001–2002 | Hospital workers | 1711 (85%) | Convenience (from 9 hospitals) | 72% (69·8–74·1) |
| Dickinson (2009)47 | Canada | 2009 (September–November) | Family physicians | 192 (22%) | Stratified random (from the list of all family physicians in the region) | 71% (63·9–77·2) |
| Yonge (2010)48 | Canada | 2006 (September) | Nursing students | 484 (31%) | Convenience (all nursing students in a university) | 67·9% (63·6–72·1) |
| Stuart (2008)49 | Australia | 2007 (February–April) | Hospital workers | 1440 (14%) | Convenience (all staff in a hospital) | 67% (64·5–69·4) |
| Hope (2010)50 | Australia | 2007–2008 | Hospital workers | 868 (54%) | Convenience (randomly selected from a health service facility) | 67% (63·8–70·2) |
| Gershon (2010)51 | USA | November 2008–June 2009 | Department of health, police, fire, emergency medical services and hospital workers | 1103 (42%) | Convenience (six essential organizations including hospital workers and emergency medical service personnel) | 66% (63·1–68·8) |
| Damery (2009)52 and Damery (2010)53 | UK | 2008 (July–September) | Hospital workers | 1032 (34%) | Convenience (from 3 healthcare trusts) | 63% (60·0–65·9) |
| Gershon (2009)54 | USA | Not stated | Emergency medical services personnel | 129 (not stated) | Convenience (attendants of training programme) | 63% at pre-intervention (53·8–71·1%) 66% at post-intervention |
| Cowden (2010)55 | USA | 2007 (February–June) | Hospital workers | 778 (31%) | Convenience (all staff in a hospital) | 59·6% (56·1–63·1) |
| Tippett (2010)56 | Australia | May 2006 | Emergency pre-hospital medical care providers | 725 (25%) | Stratified random (from national network of 9 ambulance services) | 56·3% (52·6–59·9) |
| Basta (2009)57 | USA | 2006 (November–December) | Health department workers | 2414 (51%) | Stratified random (from 67 county health departments) | 56·2% (54·2–58·2) |
| Balicer (2006)58 | USA | 2005 (March–July) | Health department workers | 308 (58%) | Judgement sampling (3 health departments) | 53·8% (48·2–59·6) |
| Hope (2011)59 | Australia | Late 2008 | Senior nurse | 60 (93%) | Convenience (attendants of an field exercise from 36 emergency department in the region) | 47% at pre-intervention (33·7–60·0%) 82% at post-intervention |
| Gershon (2010)60 | USA | 2008 (fall) | Home healthcare workers | 384 (92%) | Convenience (attendants of training sessions) | 43% for current patients (38·0–48·1%) 27% for new patients |
| Garrett (2009)61 | USA | 2007 | Hospital workers | 2864 (17%) | Convenience (attendants of focus groups) | Not available; mean willingness score (0–100): 75·6% |
| Studies of avian influenza | ||||||
| Butsashvili (2007)62 | Georgia | During 2003–2007 | Hospital workers | 288 (not stated) | Convenience (random from selected two hospital) | 76% (70·7–80·9) |
| Bell (2014)63 | USA | 2011 (July–September) | Emergency nurses | 332 (46%) | Random (from national database) | 84% (79·6–87·8) |
| Mortelmans (2009)64 | Belgium | 2006 (October–December) | Medical students | 243 (30%) | Convenience (all senior medical students in 6 universities) | 82·3% (76·9–86·9) |
| Mitani (2011)65 | Japan | 2008 (September–December) | Hospital workers | 1975 (63%) | Convenience (all workers in 6 hospitals) | 63·3%; 18·8% unconditionally + 44·5% conditionally (61·1–65·4%) |
| Tzeng (2006)66 | Taiwan | December 2005 | Nurses | 225 (95%) | Convenience (attendants of classes) | 56·9% (50·1–63·5) |
| Irvin (2008)67 | USA | 2006 (July–August) | Hospital workers | 169 (90%) | Convenience (attendants of lecture) | 50% (42·5–58·1) |
| Studies of influenza A(H1N1)pdm09 | ||||||
| Wong (2010)22 | Hong Kong | 2009 (June) | Community nurses | 401 (67%) | All community nurses in the region | 23·1% (19·1–27·6) |
| Ma (2011)68 | China | December 2009 | ICU staff | 695 (95%) | Convenience (21 ICUs) | 82·3% (79·3–85·1) |
| Tebruegge (2010)69 | Australia | May 2009 | Healthcare workers | 822 (not stated) | Convenience (selected healthcare interest groups, such as Australian Infection Control Association) | 82%; 17·6% unconditionally + 64·4% if treatment or prophylaxis are available (79·2–84·6%) |
| Kaboli (2010)70 | Canada | 2009 (August–September) | Healthcare workers | 4046 (not stated) | All healthcare workers (in all 6 health authorities) in the region | 69% (67·6–70·4) |
| Saleh (2010)71 | Egypt | After the 2009 pandemic | Nurse and nursing students | 256 (not stated) | Convenience (2 hospitals and 2 schools) | 58%; 20·6% without any concern and 37·9% with some requests (51·7–63·9%) |
| Etokidem (2012)72 | Nigeria | 2010 | Hospital workers | 350 (not stated) | Not stated | 25·4% (20·9–30·3) |
| Imai (2010)73 | Japan | 2009 (June–July) | Hospital workers | 1693 (47%) | Convenience (all employees in 3 hospitals) | Not available; 28·4% strong motivation; 14·7% strong hesitation to work |
HCW, healthcare worker; ICU, intensive care unit; CCU, critical care unit.
Study period not specified.
Assessment of risk of bias
Assessments using the modified Newcastle–Ottawa scale showed that 23 of 43 studies were at moderate risk of bias (2–3 of five stars) for the selection domain, whilst 10 studies were at low risk (4–5 stars) and ten studies were at high risk (0–1 stars); many studies used convenience sampling and few justified the study sample size, appropriately considered non-responders and used a validated measurement tool. For the comparability domain, 24 were at high risk (0 of two stars), eight at moderate risk (one star) and 11 at low risk of bias (two stars). Many studies did not clarify how statistical adjustment for confounding variables was carried out, or reported unadjusted estimates only. For the outcome domain, 39 studies were at moderate risk of bias (two of three stars) and four were at high risk (one star). Willingness to work was self-reported in all 43 studies although the statistical test used was clearly described in only 39 studies (see Figure S1).
Willingness to work
The percentage of participants who expressed a willingness to work ranged from 23·1% (community nurses during the influenza A(H1N1)pdm09 pandemic in Hong Kong in 2009)22 to 95·8% (a study of US medical students targeting a hypothetical influenza pandemic).23 We abandoned meta-analysis to estimate a pooled mean proportion of HCWs willing to work due to very high statistical heterogeneity between studies (I2 = 99·2%). Our planned subgroup analyses were unable to adequately explain the sources of heterogeneity between studies as this remained above our threshold of 85% in each analysis. The percentage of willingness to work seemed to depend on the particular context of the study. Studies of hypothetical influenza pandemics, which did not include detailed conditions such as virulence of the strain and availability of protective equipment, tended to show a high level of willingness to work. However, studies of precise scenarios or those which investigated willingness during the relatively mild influenza A(H1N1)pdm09 pandemic tended to present relatively low levels of willingness. This finding may correspond with earlier work by Syrett et al.24 which showed that willingness to work declined from over 75% to <55% as two simulated mass casualty events progressed and more detailed data became available.
Factors associated with willingness to work
Data were extracted from 33 studies. Pooled estimates from meta-analyses of individual factors associated with willingness to work are summarized in Table2. Overall, females were one-third less likely to be willing to work compared with males. By occupational group, physicians were most likely to be willing to work, followed by nurses, then other health workers. Urban or metropolitan area workers were less likely to be willing to work than rural area workers. Full-time workers were more likely to be willing to work than part-time employees. Respondents living with children or having childcare obligations were one-third less likely to be willing to work compared with those without these obligations. One study identified that pregnancy in a family member reduced willingness to work.25 Marital status (not meta-analysed) did not influence willingness to work.
Table 2.
Summary of meta-analysis for individual factors associated with willingness to work in included studies
| Risk factor | Reference group | Comparator group | Statistical adjustment | Number of studies | Pooled OR (95% CI) | P value of OR | I2 (%) | P value of Egger's test |
|---|---|---|---|---|---|---|---|---|
| Sex (Female/Male) | 3037 | 8362 | Adjusted | 8 | 0·64 (0·50–0·81) | <0·01 | 63·4 | NS |
| 4440 | 13 130 | Unadjusted | 14 | 0·60 (0·49–0·74) | <0·01 | 73·1 | NS | |
| Doctor/Nurse | 134 | 122 | Adjusted | 1 | – | – | – | – |
| 5402 | 2742 | Unadjusted | 13 | 1·43 (1·05–1·94) | 0·02 | 78·6 | 0·04 | |
| Nurse/Others | 1919 | 927 | Adjusted | 2 | 2·14 (1·43–3·20) | <0·01 | 20·1 | – |
| 8256 | 4023 | Unadjusted | 8 | 1·56 (1·17–2·08) | <0·01 | 82·0 | NS | |
| Doctor/Others | 204 | 357 | Adjusted | 2 | 2·73 (1·37–5·43) | <0·01 | 29·2 | – |
| 6403 | 1574 | Unadjusted | 7 | 2·43 (1·78–3·31) | <0·01 | 58·9 | NS | |
| Clinical/Non-clinical | 964 | 1622 | Adjusted | 3 | Not valid | – | 88·8* | NS* |
| 2472 | 4825 | Unadjusted | 7 | Not valid | – | 96·1* | NS* | |
| Location (Urban/Rural) | 302** | 284** | Adjusted | 2 | 0·64 (0·48–0·85) | <0·01 | 0·0 | – |
| 1078 | 2776 | Unadjusted | 2 | 0·76 (0·61–0·94) | 0·01 | 0·0 | – | |
| Employment (Full/Part) | 520 | 4385 | Adjusted | 3 | 2·14 (1·58–2·90) | <0·01 | 6·5 | NS |
| 769 | 4445 | Unadjusted | 3 | 1·76 (1·20–2·57) | <0·01 | 60·1 | NS | |
| Childcare | 3650** | 2230** | Adjusted | 4 | 0·62 (0·51–0·75) | <0·01 | 0·0 | NS |
| 7790** | 5621** | Unadjusted | 11 | 0·66 (0·56–0·77) | <0·01 | 43·3 | NS | |
| Personal safety | 2333** | 2855** | Adjusted | 5 | 4·42 (2·89–6·77) | <0·01 | 68·2 | NS |
| 766 | 410 | Unadjusted | 2 | 3·71 (2·85–4·82) | <0·01 | 0·0 | – | |
| Protective measures | 458 | 410 | Adjusted | 1 | – | – | – | |
| 458** | 410** | Unadjusted | 3 | Not valid | – | 97·8* | NS* | |
| Risk perception | 2307** | 1987** | Adjusted | 6 | Not valid | – | 88·5* | NS* |
| 206** | 873** | Unadjusted | 3 | 2·27 (1·52–3·41) | <0·01 | 45·9 | NS | |
| Training | 1206** | 1694** | Adjusted | 6 | 1·38 (1·13–1·68) | <0·01 | 45·3 | 0·01 |
| 1966** | 1822** | Unadjusted | 6 | Not valid | – | 86·2* | NS* | |
| General Knowledge | 2713 | 4375 | Adjusted | 5 | 2·02 (1·31–3·11) | <0·01 | 83·7 | NS |
| 2801** | 2467** | Unadjusted | 6 | 1·78 (1·40–2·26) | <0·01 | 51·6 | NS | |
| Role importance | 1750** | 1984** | Adjusted | 4 | 4·93 (4·01–6·07) | <0·01 | 19·0 | NS |
| 737** | 439** | Unadjusted | 3 | Not valid | – | 86·2* | NS* | |
| Role knowledge | 2498 | 2517 | Adjusted | 4 | 2·66 (1·59–4·45) | <0·01 | 71·9 | NS |
| 1180** | 1277** | Unadjusted | 5 | 2·64 (1·62–4·33) | <0·01 | 73·5 | NS | |
| Confidence in skills | 1313** | 2699** | Adjusted | 4 | 8·06 (3·35–19·4) | <0·01 | 74·8 | NS |
| 436** | 1018** | Unadjusted | 4 | 4·99 (2·51–9·92) | <0·01 | 78·9 | NS | |
| Pre-experience | 284** | 117** | Adjusted | 2 | 1·23 (0·93–1·63) | 0·14 | 0·0 | – |
| 603** | 493** | Unadjusted | 3 | 1·36 (1·13–1·67) | <0·01 | 0·0 | NS | |
| Confidence in employer | 3154** | 3721** | Adjusted | 8 | Not valid | – | 86·6* | NS* |
| 2110** | 753** | Unadjusted | 5 | Not valid | – | 85·7* | NS* | |
| Communication skills | 2480 | 2122 | Adjusted | 3 | Not valid | – | 96·5* | NS* |
| 890 | 286 | Unadjusted | 2 | 3·87 (1·26–11·9) | 0·02 | 0·0 | NS | |
| Family preparedness | 2099 | 3089 | Adjusted | 4 | Not valid | – | 92·6* | NS* |
| 628 | 548 | Unadjusted | 2 | Not valid | – | 88·3* | –* |
OR, odds ratio; CI, confidence interval; NS, not statistically significant.
Meta-analysis abandoned due to excessive statistical heterogeneity, therefore pooled OR and P-value considered invalid, not shown.
Not all studies provided the numbers of participants in each group.
Perceived personal safety at work and perception of pandemic risk (aware that a pandemic was likely) were both associated with increased willingness to work. Likewise, the provision of protective measures (mainly personal protective equipment) increased willingness to work, although meta-analysis was abandoned due to high heterogeneity (I2 = 97·8%).
Training in pandemic preparedness, general and specific role knowledge, confidence in personal skills, good communication skills and perception of role importance all had positive effects on willingness to work. Confidence in employers as judged by ‘belief that the employer can provide timely information’ also positively influenced willingness to work, although meta-analysis was abandoned due to high heterogeneity.
Risk of bias across studies
The funnel plot of the percentage of HCWs willing to work did not present a clear funnel shape, appeared to scatter widely without any detectable association with the standard error and overflowed the false 95% CI range. Egger's regression test reached statistical significance and showed that studies reporting a lower percentage were more likely to be published (P = 0·004). Funnel plots and Egger's regressions tests pertaining to meta-analyses of factors associated with willingness to work revealed no evidence of publication bias except for previous training and comparison of physicians and nurses (see Table2), which suggested possible underreporting of studies with an adverse result.
Discussion
This study advances knowledge from previous reviews on willingness to work during influenza pandemics by adding further new studies and subjecting the findings to statistical evaluation where possible. The search was conducted comprehensively and yielded 43 studies from 11 countries. However, quality of the included studies was not uniformly high and excessive statistical heterogeneity prevented meta-analysis of the primary outcome measure. Whilst it was not possible to identify a single clear source of the heterogeneity encountered, almost certainly the wide variation in settings, scenarios and respondents contributed significantly. Meta-analysis suggested that sex and job category would affect willingness to work although studies varied greatly in the composition of their samples. Hypothetical scenarios varied in virulence, stage and the amount of information provided to respondents. Studies of influenza A(H1N1)pdm09 were conducted at different junctures during the evolution of the 2009–10 pandemic. There was no consistency in terms of how respondents were asked about their willingness to work, and the design of questionnaires used to collect outcome data from respondents varied between studies. Remarkably, despite such high heterogeneity, some factors emerged showing a consistent association with willingness to work. Whilst previous reviews suggested these from a narrative approach, this study has confirmed them statistically.
Being male, a physician or nurse (especially the former), and a full-time worker were all positively associated with willingness to work. These factors are essentially non-modifiable; without access to the raw data, we could not disentangle any potential confounding between being male and the likelihood of being a physician or full-time worker in studies providing only unadjusted ORs. Nevertheless these were consistent findings across most studies and firm knowledge that these are reliable and statistically proven influencers of willingness to work is important information for both policy makers and healthcare service managers, even though they are difficult factors to influence.
Childcare obligation was a consistent barrier to HCWs' willingness to work. The importance of this factor may be an artefact of the high participation of women in the HCW workforce in most countries, combined with traditional cultural expectations that they will take primary responsibility for childcare. It is, nevertheless, an important finding for managers. It is not clear whether this is driven mainly by practicality, that is the need to provide childcare at home, or by concerns about whether the safety of children might be compromised by infection brought in from the parental workplace. Paradoxically, the evidence that HCWs are at increased risk of influenza infection is rather mixed and somewhat inconsistent,26 whereas the evidence that children (rather than adults) are usually the introducers of influenza infection into households is firmly established.27 This question should be further investigated because it has implications for appropriate organizational responses. If it is simply a practical matter, then managers need to consider what help could be given in emergencies through the expansion of onsite or community childcare provision. If it is a concern about cross-infection, then appropriate education and information programmes may resolve the problem. In either case, it is unlikely that simple disciplinary sanctions will be effective, because of the social force of parental obligations. Indeed, these may well be counterproductive, if other workers perceive them to have been unreasonably applied by managers unsympathetic to real personal dilemmas.
Confidence in safety, risk perception, prior training, general and role knowledge and confidence in skills were statistically proven facilitators for willingness to work. These are all addressable by detailed pandemic preparedness educational activities at healthcare unit level. Importantly, one message arising from assessments of pandemic planning activities prior to the 2009–10 pandemic was that whilst national level pandemic planning was generally successful, the level of planning at local level was insufficient, including training on pandemic influenza for HCWs.28 A particular feature of pandemics is the level of anxiety provoked by the disruption of ‘business as usual’ and the destabilization of usually stable organizational environments.29 Whilst it is not necessary to retrain HCWs frequently, this is a topic that should be addressed in their basic education and managers should ensure that updating materials are readily available, and regularly revised, so that programmes can rapidly be rolled out when a pandemic is identified. Evidence of organizational preparedness will contribute to the confidence of HCWs that they will not be placed at undue risk by being asked to work in different ways or in different environments from those that they are accustomed to.
A number of limitations with the present study warrant discussion. Our literature search was limited to records published in English. Therefore, we cannot exclude the possibility of having omitted outcome data published in other languages. Many of the included studies were at moderate or high risk of bias. Moreover, only a small number were available for analysis in relation to some risk factors; these results should be interpreted cautiously. The possibility of publication bias might also be a limitation. However, considering that the percentage of willingness was relatively high in most studies, this suggests that unpublished data may not have found statistically significantly higher percentages of willingness to work. Whilst some studies used questionnaires based on recognized psychological theories, these were commonly ‘fear-appeal’ theories. Unfortunately, this may not be appropriate as the preferable behaviour (working during an influenza pandemic) would not result in release from personal fear.30 We did not identify any studies that investigated the interaction between individual and organizational responses, which biased the findings towards individual fears rather than the social conditions that might provoke or alleviate these.
As important as our specific results themselves, is the fact that we identified a multiplicity of approaches to studying the issue of HCW willingness to work during a pandemic; mainly small, ad hoc enquiries, not based on any consistent scenarios or theoretical approaches. To solve this, a consistent methodological framework is needed before any further studies are undertaken. The outbreaks of Ebola virus disease in West Africa and MERS-CoV in the Middle East offer two very different settings in which to improve study designs and understanding of HCWs' willingness to work where infectious disease creates appreciable personal risk.
In the meantime, policy makers should recognize that HCW willingness to work during an influenza pandemic is likely to be improved by practical measures to support childcare responsibilities and by the timely provision of relevant and high-quality training and information as a pandemic develops. Whilst the above would hold true for influenza, the actual risks and perceptions are not consistent across all novel respiratory viruses. For example, 5% of nurses in Ontario refused to work during the SARS crisis when the risk to HCWs was almost exclusively nosocomial (compared with pandemic influenza where the risk is community-wide).31 Similarly, in the ongoing MERS-CoV epidemic, the risk of nosocomial infection is presently greater than in wider community settings.32,33
Conclusions
HCWs' willingness to work during an influenza pandemic is moderately high although highly variable, and substantial statistical heterogeneity precluded formal meta-analysis. Numerous risk factors are associated with willingness of HCWs to work during an influenza pandemic, revealing potential points of intervention to increase willingness to work. We identified a wide variety of approaches to the study of willingness to work. For improved future understanding, we advocate a coordinated global approach with standardized protocols and based on appropriate theoretical constructs; and the evaluation of packages of intervention through controlled studies.
Acknowledgments
We thank the authors of the articles cited in this paper. We also thank Nicola Darlington (University of Nottingham) for assistance with developing the search terms and John Mair Jenkins (Health Education East Midlands) and Roshni Joshi (University of Nottingham) for help with manuscript preparation.
Funding
This research was supported by the University of Nottingham as a Master of Public Health dissertation project.
Competing interests
JSN-V-T and CRB are respectively Editor-in-Chief and Associate Editor for Influenza and Other Respiratory Viruses; however they played no role whatsoever in the editorial process for this paper, including decisions to send the manuscript for independent peer-review or about final acceptance of a revised version. All of the above functions were handled alone by Dr John Wood, Senior Editor (Reviews).
Supporting Information
Additional Supporting Information may be found in the online version of this article:
Table S1. Full electronic search strategy (MEDLINE).
Figure S1. Summary of risk of bias of included studies using the modified Newcastle-Ottawa Scale (n = 43).
Data S1. PRISMA 2009 checklist.
References
- Van-Tam J, Sellwood C. Pandemic Influenza. 2nd edn. Wallingford: CABI; 2013. [Google Scholar]
- Viboud C, Miller M, Olson DR, Osterholm M, Simonsen L. Preliminary estimates of mortality and years of life lost associated with the 2009 A/H1N1 pandemic in the US and comparison with past influenza seasons. PLoS Curr. 2010;2:RRN1153. doi: 10.1371/currents.RRN1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Pandemic Influenza Preparedness and Response: A WHO Guidance Document. Geneva: World Health Organization; 2009. [PubMed] [Google Scholar]
- Crosby AW. America's Forgotten Pandemic. Cambridge: Cambridge University Press; 2003. [Google Scholar]
- Shrestha SS, Swerdlow DL, Borse RH, et al. Estimating the burden of 2009 pandemic influenza A (H1N1) in the United States (April 2009–April 2010) Clin Infect Dis. 2011;52(Suppl 1):S75–S82. doi: 10.1093/cid/ciq012. [DOI] [PubMed] [Google Scholar]
- Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333–1340. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- Reed C, Chaves SS, Perez A, et al. Complications among adults hospitalized with influenza: a comparison of seasonal influenza and the 2009 H1N1 pandemic. Clin Infect Dis. 2014;59:166–174. doi: 10.1093/cid/ciu285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nap RE, Andriessen M, Meessen N, van der Werf TS. Pandemic influenza and hospital resources. Emerg Infect Dis. 2007;13:1714. doi: 10.3201/eid1311.070103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebenso B, Influenza A. H1NI (Pandemic 2009): how prepared are healthcare providers in Calabar, Nigeria? J Infect Dis Immun. 2012;4:23–28. [Google Scholar]
- Shaw KA, Chilcott A, Hansen E, Winzenberg T. The GP's response to pandemic influenza: a qualitative study. Fam Pract. 2006;23:267–272. doi: 10.1093/fampra/cml014. [DOI] [PubMed] [Google Scholar]
- Chaffee M. Willingness of health care personnel to work in a disaster: an integrative review of the literature. Disaster Med Public Health Prep. 2009;3:42–56. doi: 10.1097/DMP.0b013e31818e8934. [DOI] [PubMed] [Google Scholar]
- Pandemic Influenza Preparedness Team. 2011. Healthcare workers willingness to work during a pandemic. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/215675/dh_125428.pdf (Accessed 08 March 2015)
- Devnani M. Factors associated with the willingness of health care personnel to work during an influenza public health emergency: an integrative review. Prehosp Disaster Med. 2012;1:1–16. doi: 10.1017/S1049023X12001331. [DOI] [PubMed] [Google Scholar]
- Rossow CC. Healthcare Workers' Willingness to Report to Work During an Influenza Pandemic: A Systematic Literature Review. Michigan: Central Michigan University; 2012. [Google Scholar]
- Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L. An international registry of systematic-review protocols. Lancet. 2011;377:108–109. doi: 10.1016/S0140-6736(10)60903-8. [DOI] [PubMed] [Google Scholar]
- Herzog R, Alvarez-Pasquin MJ, Diaz C, Del Barrio JL, Estrada JM, Gil A. Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck CR, McKenzie BC, Hashim AB, et al. Influenza vaccination for immunocompromised patients: systematic review and meta-analysis from a public health policy perspective. PLoS ONE. 2011;6:e29249. doi: 10.1371/journal.pone.0029249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galbraith RF. Graphical display of estimates having differing standard errors. Technometrics. 1988;30:271–281. [Google Scholar]
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong ELY, Wong SYS, Kung K, Cheung AWL, Gao TT, Griffiths S. Will the community nurse continue to function during H1N1 influenza pandemic: a cross-sectional study of Hong Kong community nurses? BMC Health Serv Res. 2010;10:107. doi: 10.1186/1472-6963-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser HE, Barnett DJ, Hsu EB, Kirsch TD, James JJ, Subbarao I. Perspectives of future physicians on disaster medicine and public health preparedness: challenges of building a capable and sustainable auxiliary medical workforce. Disaster Med Public Health Prep. 2009;3:210. doi: 10.1097/DMP.0b013e3181aa242a. [DOI] [PubMed] [Google Scholar]
- Syrett JI, Benitez JG, Livingston WH, III, Davis EA. Will emergency health care providers respond to mass casualty incidents? Prehosp Emerg Care. 2007;11:49–54. doi: 10.1080/10903120601023388. [DOI] [PubMed] [Google Scholar]
- Martinese F, Keijzers G, Grant S, Lind J. How would Australian hospital staff react to an avian influenza admission, or an influenza pandemic? Emerg Med Australas. 2009;21:12–24. doi: 10.1111/j.1742-6723.2008.01143.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuster SP, Shah PS, Coleman BL, et al. Incidence of influenza in healthy adults and healthcare workers: a systematic review and meta-analysis. PLoS ONE. 2011;6:e26239. doi: 10.1371/journal.pone.0026239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longini IM, Koopman JS, Monto AS, Fox JP. Estimating household and community transmission parameters for influenza. Am J Epidemiol. 1982;115:736–751. doi: 10.1093/oxfordjournals.aje.a113356. [DOI] [PubMed] [Google Scholar]
- WHO Regional Office for Europe. Recommendations for Good Practice in Pandemic Preparedness: Identified Through Evaluation of the Response to Pandemic (H1N1) 2009. Copenhagen: WHO Regional Office for Europe; 2010. [Google Scholar]
- Dingwall R, Hoffman LM, Staniland K. Introduction: why a sociology of pandemics? Sociol Health Illn. 2013;35:167–173. doi: 10.1111/1467-9566.12019. [DOI] [PubMed] [Google Scholar]
- Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr. 1992;59:329–349. [Google Scholar]
- Campbell A. SARS Commission (Ontario), Volume 3: Spring of Fear, Chapter 6: The Nurses' Survey. 2007. Available at http://www.archives.gov.on.ca/en/e_records/sars/report/v3-pdf/Vol3Chp6.pdf (Accessed 08 March 2015)
- Al-Abdallat MM, Payne DC, Alqasrawi S, et al. Hospital-associated outbreak of Middle East respiratory syndrome Coronavirus: a serologic, epidemiologic, and clinical description. Clin Infect Dis. 2014;59:1225–1233. doi: 10.1093/cid/ciu359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assiri A, McGeer A, Perl TM, et al. Hospital outbreak of Middle East respiratory syndrome Coronavirus. N Engl J Med. 2013;369:407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett DJ, Levine R, Thompson CB, et al. Gauging US emergency medical services workers' willingness to respond to pandemic influenza using a threat-and efficacy-based assessment framework. PLoS ONE. 2010;5:e9856. doi: 10.1371/journal.pone.0009856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett DJ, Balicer RD, Thompson CB, et al. Assessment of local public health workers' willingness to respond to pandemic influenza through application of the extended parallel process model. PLoS ONE. 2009;4:e6365. doi: 10.1371/journal.pone.0006365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Errett NA, Barnett DJ, Thompson CB, et al. Assessment of medical reserve corps volunteers' emergency response willingness using a threat-and efficacy-based model. Biosecur Bioterror. 2013;11:29–40. doi: 10.1089/bsp.2012.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett DJ, Thompson CB, Errett NA, et al. Determinants of emergency response willingness in the local public health workforce by jurisdictional and scenario patterns: a cross-sectional survey. BMC Public Health. 2012;12:164. doi: 10.1186/1471-2458-12-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin SD. Nurses' ability and willingness to work during pandemic flu. J Nurs Manag. 2011;19:98–108. doi: 10.1111/j.1365-2834.2010.01190.x. [DOI] [PubMed] [Google Scholar]
- Stergachis A, Garberson L, Lien O, D'Ambrosio L, Sangare L, Dold C. Health care workers' ability and willingness to report to work during public health emergencies. Disaster Med Public Health Prep. 2011;5:300. doi: 10.1001/dmp.2011.77. [DOI] [PubMed] [Google Scholar]
- Seale H, Wang Q, Yang P, et al. Hospital health care workers' understanding of and attitudes toward pandemic influenza in Beijing. Asia Pac J Public Health. 2012;24:39–47. doi: 10.1177/1010539510365097. [DOI] [PubMed] [Google Scholar]
- Adams L, Berry D. Who will show up? Estimating ability and willingness of essential hospital personnel to report to work in response to a disaster. Online J Issues Nurs. 2012;17:8. [PubMed] [Google Scholar]
- Seale H, Leask J, Po K, MacIntyre CR. “Will they just pack up and leave?”–attitudes and intended behaviour of hospital health care workers during an influenza pandemic. BMC Health Serv Res. 2009;9:1–8. doi: 10.1186/1472-6963-9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balicer RD, Barnett DJ, Thompson CB, et al. Characterizing hospital workers' willingness to report to duty in an influenza pandemic through threat-and efficacy-based assessment. BMC Public Health. 2010;10:436. doi: 10.1186/1471-2458-10-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr H, Macfarlane J, Macgregor O, Foxwell R, Buswell V, Lim W. Ethical planning for an influenza pandemic. Clin Med. 2008;8:49–52. doi: 10.7861/clinmedicine.8-1-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daugherty EL, Perl TM, Rubinson L, Bilderback A, Rand CS. Survey study of the knowledge, attitudes, and expected behaviors of critical care clinicians regarding an influenza pandemic. Infect Control Hosp Epidemiol. 2009;30:1143–1149. doi: 10.1086/648085. [DOI] [PubMed] [Google Scholar]
- Cone DC, Cummings B. Hospital disaster staffing: if you call, will they come? Am J Disaster Med. 2006;1:28. [PubMed] [Google Scholar]
- Dickinson J, Bani-Adam G, Berzins S, et al. 2009. Survey of Alberta family physicians' reactions to the spring and summer phase of pH1N1 (pandemic swine flu) outbreak, 2009.
- Yonge O, Rosychuk RJ, Bailey TM, Lake R, Marrie TJ. Willingness of university nursing students to volunteer during a pandemic. Public Health Nurs. 2010;27:174–180. doi: 10.1111/j.1525-1446.2010.00839.x. [DOI] [PubMed] [Google Scholar]
- Stuart RL, Gillespie EE. Preparing for an influenza pandemic: healthcare workers' opinions on working during a pandemic. Healthc Infect. 2008;13:95–99. doi: 10.1071/HI08024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope K, Durrheim D, Barnett D, et al. Willingness of frontline health care workers to work during a public health emergency. Austr J Emerg Manag. 2010;25:39–47. [Google Scholar]
- Gershon RRM, Magda LA, Qureshi KA, et al. Factors associated with the ability and willingness of essential workers to report to duty during a pandemic. J Occup Environ Med. 2010;52:995. doi: 10.1097/JOM.0b013e3181f43872. [DOI] [PubMed] [Google Scholar]
- Damery S, Wilson S, Draper H, et al. Will the NHS continue to function in an influenza pandemic? A survey of healthcare workers in the West Midlands, UK. BMC Public Health. 2009;9:142. doi: 10.1186/1471-2458-9-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damery S, Draper H, Wilson S, et al. Healthcare workers' perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010;36:12–18. doi: 10.1136/jme.2009.032821. [DOI] [PubMed] [Google Scholar]
- Gershon RRM, Vandelinde N, Magda LA, Pearson JM, Werner A, Prezant D. Evaluation of a pandemic preparedness training intervention of emergency medical services personnel. Prehosp Disaster Med. 2009;24:508. doi: 10.1017/s1049023x00007421. [DOI] [PubMed] [Google Scholar]
- Cowden J, Crane L, Lezotte D, Glover J, Nyquist AC. Pre-pandemic planning survey of healthcare workers at a tertiary care children's hospital: ethical and workforce issues. Influenza Other Respir Viruses. 2010;4:213–222. doi: 10.1111/j.1750-2659.2010.00145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tippett VC, Watt K, Raven SG, et al. Anticipated behaviors of emergency prehospital medical care providers during an influenza pandemic. Prehosp Disaster Med. 2010;25:20. doi: 10.1017/s1049023x00007603. [DOI] [PubMed] [Google Scholar]
- Basta NE, Edwards SE, Schulte J. Assessing public health department employees' willingness to report to work during an influenza pandemic. J Public Health Manag Pract. 2009;15:375. doi: 10.1097/PHH.0b013e3181a391e2. [DOI] [PubMed] [Google Scholar]
- Balicer R, Omer S, Barnett D, Everly G. Local public health workers' perceptions toward responding to an influenza pandemic. BMC Public Health. 2006;6:99. doi: 10.1186/1471-2458-6-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope K, Epi C, Massey PD, et al. Senior clinical nurses effectively contribute to the pandemic influenza public health response. Aust J Adv Nurs. 2011;28:47–53. [Google Scholar]
- Gershon RR, Magda LA, Canton AN, et al. Pandemic-related ability and willingness in home healthcare workers. Am J Disaster Med. 2010;5:15. doi: 10.5055/ajdm.2010.0002. [DOI] [PubMed] [Google Scholar]
- Garrett AL, Park YS, Redlener I. Mitigating absenteeism in hospital workers during a pandemic. Disaster Med Public Health Prep. 2009;3(Suppl 2):S141. doi: 10.1097/DMP.0b013e3181c12959. [DOI] [PubMed] [Google Scholar]
- Butsashvili M, Triner W, Kamkamidze G, Kajaia M, McNutt LA. Knowledge and anticipated behavior of health care workers in response to an outbreak of pandemic influenza in Georgia. J Infect Dev Ctries. 2007;1:329–332. [PubMed] [Google Scholar]
- Bell MA, Dake JA, Price JH, Jordan TR, Rega P. A national survey of emergency nurses and avian influenza threat. J Emerg Nurs. 2014;40:212–217. doi: 10.1016/j.jen.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Mortelmans LJM, Cauwer HGD, Dyck EV, Monballyu P, Giel RV, Turnhout EV. Are Belgian senior medical students ready to deliver basic medical care in case of a H5N1 pandemic? Prehosp Disaster Med. 2009;24:438–442. doi: 10.1017/s1049023x00007287. [DOI] [PubMed] [Google Scholar]
- Mitani S, Ozaki E, Fujita N, et al. Ensuring adequate human medical resources during an avian influenza A/H5N1 pandemic. Prehosp Disaster Med. 2011;26:15–20. doi: 10.1017/s1049023x10000075. [DOI] [PubMed] [Google Scholar]
- Tzeng HM, Yin CY. Nurses' fears and professional obligations concerning possible human-to-human avian flu. Nurs Ethics. 2006;13:455–470. doi: 10.1191/0969733006nej893oa. [DOI] [PubMed] [Google Scholar]
- Irvin CB, Cindrich L, Patterson W, Southall A. Survey of hospital healthcare personnel response during a potential avian influenza pandemic: will they come to work. Prehosp Disaster Med. 2008;23:328–335. doi: 10.1017/s1049023x00005963. [DOI] [PubMed] [Google Scholar]
- Ma X, Zhenyang H, Yushan W, et al. Knowledge and attitudes of healthcare workers in Chinese intensive care units regarding 2009 H1N1 influenza pandemic. BMC Infect Dis. 2011;11:24. doi: 10.1186/1471-2334-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebruegge M, Pantazidou A, Ritz N, et al. Perception, attitudes and knowledge regarding the 2009 swine-origin influenza A (H1N1) virus pandemic among health-care workers in Australia. J Paediatr Child Health. 2010;46:673–679. doi: 10.1111/j.1440-1754.2010.01820.x. [DOI] [PubMed] [Google Scholar]
- Kaboli F, Astrakianakis G, Li G, Guzman J, Naus M, Donovan T. Influenza vaccination and intention to receive the pandemic H1N1 influenza vaccine among healthcare workers of British Columbia, Canada: a cross-sectional study. Infect Control Hosp Epidemiol. 2010;31:1017–1024. doi: 10.1086/655465. [DOI] [PubMed] [Google Scholar]
- Saleh D, Elshaer I. Nurses' perspectives and concerns towards an infectious disease epidemic in Egypt. Egypt J Community Med. 2010;28:1–17. [Google Scholar]
- Etokidem A, Ogaji D, Nsan E, Ikpeme B, Oyo-Ita A, Ndifon W, et al. Influenza A H1NI (pandemic 2009): how prepared are healthcare providers in Calabar, Nigeria? J Infect Dis Immun. 2012;4:23–28. [Google Scholar]
- Imai H, Matsuishi K, Ito A, et al. Factors associated with motivation and hesitation to work among health professionals during a public crisis: a cross sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC Public Health. 2010;10:672. doi: 10.1186/1471-2458-10-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Full electronic search strategy (MEDLINE).
Figure S1. Summary of risk of bias of included studies using the modified Newcastle-Ottawa Scale (n = 43).
Data S1. PRISMA 2009 checklist.


