Abstract
Statin treatment in association with physical exercise practice can substantially reduce cardiovascular mortality risk of dyslipidemic individuals, but this practice is associated with myopathic event exacerbation. This study aimed to present the most recent results of specific literature about the effects of statins and its association with physical exercise on skeletal musculature. Thus, a literature review was performed using PubMed and SciELO databases, through the combination of the keywords “statin” AND “exercise” AND “muscle”, restricting the selection to original studies published between January 1990 and November 2013. Sixteen studies evaluating the effects of statins in association with acute or chronic exercises on skeletal muscle were analyzed. Study results indicate that athletes using statins can experience deleterious effects on skeletal muscle, as the exacerbation of skeletal muscle injuries are more frequent with intense training or acute eccentric and strenuous exercises. Moderate physical training, in turn, when associated to statins does not increase creatine kinase levels or pain reports, but improves muscle and metabolic functions as a consequence of training. Therefore, it is suggested that dyslipidemic patients undergoing statin treatment should be exposed to moderate aerobic training in combination to resistance exercises three times a week, and the provision of physical training prior to drug administration is desirable, whenever possible.
Keywords: Hydroxymethylglutaryl-CoA reductase inhibitors; Exercise; Muscle, skeletal; Dyslipidemia
Introduction
High serum lipoprotein levels are recognized as one of the most significant risk factors for cardiovascular diseases. Alone, lipid abnormalities are accountable for 56% of heart disease and 18% of cases of infarction, being also associated to one third of deaths worldwide 1. Due to the magnitude of its effects, great efforts have been made by the medical community to prevent and control this metabolic condition, with the therapeutic strategies recommended by the Brazilian Society of Cardiology (SBC) and adopted by area specialists being such as encouraging the adoption of healthy eating, increased physical exercise and drug prescription2,3.
Specifically on the drug therapy, inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A reductase, (HMG-CoA reductase), also known as statins, are most effective class of drugs for the treatment of lipid disorders2-4. Recent evidence indicates that the combination of medical treatment and physical exercise can substantially reduce the risk of cardiovascular mortality in dyslipidemic patients when compared to both treatments separately, suggesting that treatment with statins associated with moderate to high physical fitness level provides additional protection against premature cardiovascular death5.
However, the use of statins is associated with the occurrence of undesirable muscle effects such as muscular pain, cramps, and/or stiffness6-8, as well as reduced muscle strength in elderly individuals9. The practice of physical exercises, in turn, is related to the exacerbation of these discomforts, being directly associated with the intensity of the physical effort performed7,8. Evidently, this situation presents as a paradox, as it is not desirable that lack of physical activity be a prerequisite for treatment with statins without complications. It is thus necessary to further assess the evidence of this association, as well as clarify the mechanisms by which these effects are mediated. Considering these facts, the aim of this study was to review recent data from specific technical literature on the effects of statins and physical exercise combination on skeletal muscle.
Methods
The survey was carried out in the databases PubMed and Scientific Electronic Library Online (SciELO), using the combination of the terms "statin / statins" AND "exercise" AND "muscle" (as well as the equivalent terms in Portuguese), Only original articles in English or Portuguese, published between January 1990 and November 2013 that aimed to evaluate the effect of the association of statins with acute or chronic exercise on skeletal muscle were selected for this update. Review studies, editorials, letters and consensuses were not included. A total of 109 articles were found in the PubMed search, of which 15 were original articles that comprised the established criteria; the search in SciELO, in turn, resulted in a single original article, totaling 16 articles analyzed.
Data on the sample (sample size, gender, age and study groups), on the specific characteristics of the drug therapy (statin type and dose), the physical exercise protocol (type and intensity of exercise, and time of intervention) were extracted from the articles, as well as the results and the conclusions of the studies.
Results and Discussion
The results of the present study are described in the text and systematized in Chart 1. As the understanding of the effect of statins on skeletal muscle is critical to understand the effects of its association with exercise, it was considered important to contextualize the reader about such aspects and, therefore, the results are shown as two topics.
Chart 1.
Description of the studies investigating the effect of statins and physical exercise on skeletal muscle
| Reference | Sample | Drug therapy | Physical exercise protocol | Results |
|---|---|---|---|---|
| Use of statins in athletes | ||||
| Parker et al.37 | n = 80 individuals (59♂ and 21♀) | Different statin types and doses (n = 37) | Running a marathon | Increase in CK after 24 horas in the statin group |
| Statins and acute physical exercises | ||||
| Thompson et al.38 | n = 59 men (18-65 years) Double-blind randomized trial | Lovastatin (40 mg/day; n = 22) or placebo (n = 27) for 5 weeks | Treadmill (45'; 15% incline; 65% HRmax) | Increase in CK 24 and 48 hours after the walk in the lovastatin group |
| Elbow flexion (4x10 repetitions; 50% MF) | ||||
| Reust et al.39 | n = 10 men (27-28 years) Double-blind crossover randomized trial | Lovastatin (40 mg/day; n = 5) or placebo (n = 5) for 30 days | Treadmill (60'; 14% incline; 3 km/h) | Maintenance of CK after lovastatin compared with placebo |
| Kearns et al.40 | n = 79 men Randomized trial | Atorvastatin (10 mg/day, n = 42; or 80 mg/day, n = 37) for 5 weeks | Treadmill (3x15'; 15% incline; 65% HRmax) | ↑ total CK, CK-MB and muscular pain after exercise |
| Panayiotou et al.41 | n = 28 sedentary men (> 65 years) | Atorvastatin (10-80 mg/day; n = 14) for ≥ 1 year | Knee extension (5x8 maximum EC; 2 sessions) | Similar muscular function between groups |
| Urso et al.42 | n = 8 sedentary men (18-30 years) Randomized double-blind trial | Atorvastatin (80 mg/day; n = 4) or placebo (n = 4) for 4 weeks | Knee extension (300 EC) before and after treatment | Different expression of genes from the PSU pathway of catabolism and of apoptosis |
| Statins and chronic physical exercises | ||||
| Accioly et al.43 | n = 80 male rats (hyperlipidic diet, n = 60; standard diet, n = 20) in 8 groups | Simvastatin (20 mg, n = 20), Fluvastatin (10 mg, n = 20) or placebo (n = 20) | Treadmill (60'; 9.75 m/min) 5x/week for 8 weeks | Higher frequency of morphological alterations after statin, with or without exercise |
| Seachrist et al.44 | n = 48 female rats divided into 8 groups | Cerivastatin (0.1; 0.5; 1.0 mg/kg/day) or placebo for 14 days | Treadmill (25'; 20 m/minute; 15° of incline angle) 5x/week for 2 weeks | Exacerbation of muscular degeneration; mitochondrial involvement |
| Meex et al.45 | n = 38 sedentary elderly men | Different types and doses of statins (n = 14) | Cycloergometer (30'; 55% ML) 2x/week and 8 resistance exercises (3x8 repetitions; 55 and 75%) 1x/week, 12 weeks | Increase in ML, muscular strength, muscular density and mitochondrial function in both groups |
| Mikus et al.46 | n = 37 sedentary individuals with risk factor for MS (13♂ and 24♀: 25-59 years) | Simvastatin (40 mg/day) (n = 19) | Treadmill (45'; 60-75% rHR) 5x/ week for 12 weeks | Increase in LM and decrease in muscular citrate synthase activity |
| Coen et al.47 | n = 31 sedentary individuals (15♂ and 16♀; 40-65 years) Randomized trial | Rosuvastatin (10 mg/day) for 20 weeks | Treadmill (20'; 60-70% rHR) and 8 resistance exercises (70-80% 1MR), 3x/weeks for 10 weeks | Increase in CK 48 hours after the 1st session; absence of reports of pain/fatigue |
| Mechanisms of muscular responses to statins and to physical exercises | ||||
| Bouitbir et al.26 | n = 34 male rats divided into 4 groups | Atorvastatin (10 mg/kg/day; n = 18) or placebo for 2 weeks | Treadmill (40'; 40 cm/s with increase of 5 cm/s up to exhaustion; 1 session) | Increase in ROS and decrease in mitochondrial respiration |
| Wu et al.48 | n = 10 subjects (5♂ and 5♀; 35-69 years) | Different types and doses of statins for 4 weeks | Plantar flexion (40% ML) for 7' or up to exhaustion | Increase in time of metabolic recovery and CK maintenance |
| Hubal et al.49 | n = 14 users of statins (n = 9 symptomatic; n = 6 asymptomatic) | Simvastatin or Atorvastatin (10-80 mg) up to myalgia onset (2 weeks to 4 months) | Sitting down and getting up from a chair 300 times or up to exhaustion | Decrease in the expression of oxidative phosphorylation genes and of mitochondrial proteins in symptomatic individuals |
| Meador and Huey50 | n = 59 mice divided in 6 groups | Cerivastatin (1 mg/kg/day) or saline solution (days 15-28) | Running wheels (adapted: days 1-28; non-adapted: days 15-28) | Adaptation to exercise prevented loss of strength and increased fatigue associated with statin |
| Bouitbir et al.25 | n = 20 male rats (trained, n = 10; sedentary, n = 10) | Atorvastatin application (4, 10, 40, 100, 200 and 400 µM) to the plantaris muscle | Treadmill (30'; 40 cm/s; 15% incline) for 10 days | Increased mitochondrial tolerance to the drug and decrease in production of free radicals |
CK: creatine kinase; HRmax: Maximum heart rate; MF: maximum force; CK-MB: cardiac creatine kinase; EC: eccentric contractions; UPS ubiquitin proteasome; ML: maximum load; MS: metabolic syndrome; rHR: resting heart rate; LM: lean mass; MR: maximal repetition; ROS: Reactive Oxygen Species.
Statins and skeletal muscle
Statins work by inhibiting the activity of HMG-CoA reductase enzyme, preventing the formation of mevalonate (Figure 1), which leads to a reduction in the liver synthesis of cholesterol and, consequently, increased synthesis of low-density lipoprotein (LDL) receptors in hepatocytes, thereby increasing its uptake from circulation to restore intracellular cholesterol10. Although well tolerated by most patients, statins are associated with the occurrence of muscle toxicity11,12, which may be mild or severe, ranging from myalgia to rhabdomyolysis, and affecting 5 to 10% of patients6-8,12.
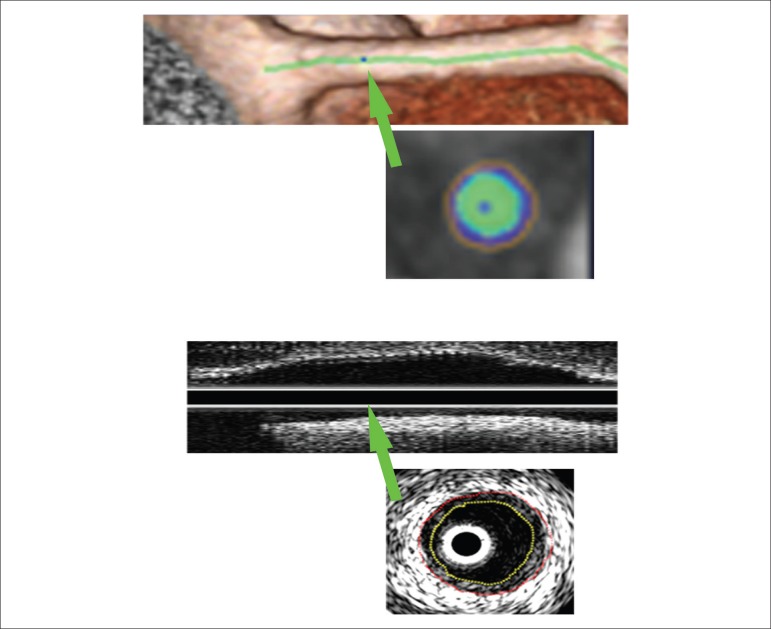
Figure 1.
Cholesterol biosynthesis stages and statin action. The enzyme 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase catalyzes the conversion of HMG-CoA into mevalonate; the action of inhibiting this enzyme by statins results in the reduction of cholesterol synthesis, as well as other intermediates (prenylated proteins, dolichols and ubiquinone), which can contribute to muscle injury resulting from statin use. CoA: Coenzyme A; PP: pyrophosphate.
According to Parker and Thompson13, identifying the actual incidence of muscle alterations caused by the use of statins may be considered practically impossible, as these problems are usually not evaluated in clinical trials funded by pharmaceutical industries. They point out, however, that clinical reports have confirmed the suspicion that muscle injuries produced by statins are much more frequent. In fact, retrospective studies in medical records have indicated that musculoskeletal injuries and pain are more common among statin users when compared to non-users14, with a high number of reports associated with statins as primary suspects15.
A randomized clinical trial on the use of atorvastatin (80 mg/day) or placebo for 6 months using a double-blind16 design found a higher incidence of myalgia among treated individuals and only the symptomatic ones had decreased muscle strength/resistance values17, with no association being observed between creatine kinase (CK) increases and muscle function, indicating that the levels of this injury marker are not predictive of muscle symptoms associated with statins18. This evidence indicates that statins can cause muscle damage to its users; however, the discrepancy on how to identify such alterations limits the identification of their incidence7,12.
The most prevalent theories about the mechanisms of muscle damage by statins are related to the inhibition of mevalonate formation by the drug, which, in turn, limits the formation of several intermediates in cholesterol biosynthesis (Figure 1), such as ubiquinone (coenzyme Q10), one of the intermediates in the mitochondrial electron transport chain19-21. Although there is evidence regarding mitochondrial dysfunction due to coenzyme Q10 deficiency (CoQ10)22, this mechanism of muscle injury by statins is quite controversial in the literature, as ubiquinone supplementation has not shown to improve muscle function23, suggesting possible direct effects of the drug on muscle.
A study of the extensor digitorum longus (EDL) muscle of rats (n = 32) indicated that drug treatment with lipid‑lowering drugs alters the expression of proteins involved in cellular defense against oxidative stress, also being observed a significant reduction in the expression of oxidative and glycolytic enzymes, and showing a therapy trend of modifying proteins associated with energy supply systems24.
Similarly, Bouitbir et al.25,26 found that low doses of atorvastatin may increase the production and concentration of Reactive Oxygen Species (ROS) and reduce the maximum mitochondrial respiration, muscle glycogen content and mitochondrial DNA content in skeletal muscle of mice, indicating that the statins may induce oxidative stress in skeletal muscle and, consequently, cause mitochondrial dysfunction due to reduction of its biogenesis.
Similar results have been found in research with humans. In the study by Stringer et al.27, it was found that the skeletal muscles of symptomatic patients had lower content of mitochondrial DNA than that of asymptomatic ones, suggesting that statins can induce mitochondrial DNA depletion. Moreover, Larsen et al.28 found that individuals treated with simvastatin had reduced CoQ10 content, antioxidant proteins, compounds of complex IV of the mitochondrial electron transport chain and type 1 fibers, when compared to their peers without medication, suggesting that exposure to statins may limit the maximum capacity of mitochondrial phosphorylation of skeletal muscle. However, the mitochondrial alterations seem to represent the early stage of the cascade of deleterious mechanisms induced by statins. According to Sirvent et al.19,29,30, alterations in the mitochondrial respiratory chain result in depolarization of the mitochondrial inner membrane, causing calcium extrusion, which in turn would increase its sarcoplasmic concentrations and overload the sarcoplasmic reticulum, resulting in the so‑called "calcium waves" and the consequent statin‑induced myotoxicity. Although isolated effects of statins on calcium homeostasis have been reported in rat muscles31 and in both symptomatic32 and asymptomatic33 individuals, apparently its dysregulation is, in fact, a consequence of mitochondrial lesions.
In fact, in a recent study, Sirvent et al.34 observed that the skeletal musculature of patients treated with statins, symptomatic or not, showed alterations in complex I of the electron transport chain, which modified mitochondrial function and deregulated calcium homeostasis, confirming their previous results observed in in vitro experiments. Similar results were found in a double-blind randomized clinical trial developed by Galtier et al.35, who found that atorvastatin-induced muscle toxicity was associated with a physiopathological mechanism, of which changes in mitochondrial respiration caused by the drug resulted in irregular calcium homeostasis.
Analyzed together, this evidence explains, in large part, statin-induced myotoxicity: mitochondrial and calcium homeostasis alterations are related to modifications in the production of proteins activated by calcium, such as calpains and caspases, which in turn, are directly related to the apoptotic processes, protein degradation and muscle remodeling; in addition, this condition can modify the excitation-contraction coupling of muscular fibers, causing episodes of muscle weakness, pain and cramps19,33.
Effect of statins and exercise on skeletal muscle
The negative effects of statins on skeletal muscle, as well as the reported reduction in exercise capacity caused by the drug, culminate in the increasing dissemination of the theory of lesion exacerbation caused by the association of statins and exercise, which can be characterized as a limiting factor for the recommendation of physical activity in dyslipidemic patients. In an attempt to clarify these associations, the literature search information is shown as subtopics, which include the effects of statins in athletes and response to acute and chronic exercises, as well as the mechanisms responsible for muscle responses to this interaction.
Use of statins in athletes
Regarding physical exercises, it is important to understand what the effects of statins are on athletes’ musculature. In this regard, Sinzinger and O'Grade36 evaluated 22 professional athletes of different modalities, all diagnosed with familial hypercholesterolemia, which were followed for 8 years and who received different classes of statins. Of the assessed athletes, 78% did not tolerate any of the administered compounds; the experienced symptoms were similar between athletes and types of statins administered to them and consisted of muscle pain, cramps and weakness. After drug use cessation, symptoms disappeared in all athletes after approximately 3 weeks.
In a more recent study, Parker et al.37 evaluated 37 athletes that used statins for over 6 months and 43 control subjects, before and after a marathon race. The results showed that marathon runners that used statins had more significant increases in CK levels 24 hours after the marathon completion when compared to non-users. It is concluded that athletes may experience deleterious effects on skeletal muscle when using statins, as these may exacerbate muscle injury associated with intense and strenuous exercise, both performed acutely or as part of training (Chart 1).
Statins and acute physical exercises
The pioneering studies that aimed to identify the exacerbation of muscle injury by exercise were double-blind clinical trials randomized for the use of lovastatin (40 mg/day) or placebo, carried out in adult men (n = 59, 18-65 years)38 or young individuals (n = 10, 27-28 years)39, which found that acute provision of eccentric and strenuous effort by walking downhill after a 4-week treatment with lovastatin (40 mg/day), could increase38 or not39 serum CK levels. A more recent study reproduced the abovementioned research protocol, in which adult males (n = 79, age > 40 years) were randomly exposed to doses of 10 or 80 mg of atorvastatin for 4 weeks, and then submitted to an acute eccentric and strenuous exercise session by walking downhill. It was observed that exposure to physical effort after the drug use increased CK levels and reports of pain in both groups, with no significant differences being identified between treatments with low or high dose40. Together, the results a possible exacerbating effect of muscle injury in response to these associations.
In contrast, a cross-sectional study that investigated the effects of acute sessions of isokinetic eccentric exercises of the knee extensors (five series of eight maximal voluntary repetitions) on muscle function of elderly men (n = 28, age > 65 years) treated with atorvastatin (10-80 mg / day) for more than one year, found no differences in muscle function, in both moments, pre and post-exercise, when compared to control patients. These results indicated that the proposed eccentric exercise did not have a negative impact on torque, range of motion and pain sensation during squatting exercises and walking in statin users41.
Similarly, the double-blind trial randomized for the use of atorvastatin (80 mg/day) or placebo for 4 weeks in healthy men (n = 8, age 18 to 30), in which Bear et al.42 provided acute strenuous exercise, characterized by 300 eccentric contractions of the lower limbs before and after drug treatment, showed no significant increases in CK levels with the combination of the drug and the physical effort. However, it was observed that this interaction increased the expression of genes involved in protein catabolism and the ubiquitin proteasome (UPS) pathway, changing the balance between protein breakdown and muscle repair, indicating that the absence of changes in CK may not reflect muscle tissue responses.
In general, the studies seem to indicate that men using different statin classes, at low or high doses, show changes in muscle function and injury markers when exposed to acute sessions of eccentric and strenuous exercises walking downhill, but not with lower-limb eccentric exercises alone. However, they warn that this reality does not rule out the occurrence of possible structural and metabolic changes in muscle tissue. It is also noteworthy that the heterogeneity of methodological protocols, as well as the absence of women in the studies significantly limits these conclusions, indicating the need for further studies to satisfactorily establish this association.
Statins and chronic physical exercises
Considering the body’s adaptation to training, it can be assumed that muscle responses to chronic exercises are different from those observed in acute exercises. An experimental study with an animal model, which evaluated the effects of 60 minutes of moderate aerobic physical activity (9.75 m/min) on a treadmill, performed five times a week for two months, concomitant with simvastatin (20 mg/kg) and fluvastatin (20 mg/kg) treatment in rats showed that the drug use caused mild to severe muscle changes in the soleus muscle, which were more frequent when the drug was associated with exercise43.
Similarly, in the study carried out with guinea pigs performed by Seachrist et al.44, high doses of cerivastatin were concomitantly administered to the practice of intense physical exercise on a treadmill for 14 days. Results showed that this association increased CK levels and exacerbated degeneration of mitochondria and other organelles of skeletal muscles. Evidence from animal studies indicated that physical training, of both high and moderate intensity, when associated with statin treatment at low or potentially harmful doses, results in muscle damage. However, studies performed in humans have shown different results.
In the study performed by Meex et al.45, elderly men, users or not of statins, were exposed to a 12-week training protocol, characterized by the practice of moderate aerobic exercise on a cycle ergometer and resistance exercises three times a week, with the following parameters being evaluated: substrate oxidation, phosphocreatine (PCr) recovery and expression of proteins from the skeletal muscle mitochondrial electron transport chain complex. The results of this study showed that treatment with statins (atorvastatin, rosuvastatin, pravastatin and simvastatin) at different doses did not limit the practice of physical exercise or training-induced gains in muscle mass and mitochondrial quality of those practicing exercises, indicating that the proposed associations were safe.
When comparing previously sedentary adults with risk factors for metabolic syndrome (n = 37, aged 25-59 years), exposed to 12 weeks of moderate exercise on a treadmill, performed five days a week, alone (n = 19 ) or associated with the use of simvastatin (40 mg / day, n = 18), Mikus et al.46 found that, although the association caused more significant reductions in total cholesterol (TC) and LDL-cholesterol levels, the increases in cardiorespiratory fitness and citrate synthase enzyme activity of the vastus lateralis muscle, in response to exercise, were attenuated in subjects treated with statins, indicating that the drug may inhibit some of the body’s adaptive responses to exercise. Despite their significance, these results were obtained in the absence of a group treated with statins only, which considerably limits the advance of knowledge about the exacerbation of the deleterious effects of statins by physical exercise.
In this regard, the present literature review found only one study that assessed the effect of adding moderate chronic exercise to regular treatment with rosuvastatin (10 mg/day) in dyslipidemic adults of both sexes (n = 31, aged 40-65 years). In this randomized clinical trial, it was observed that both drug treatment and its association with 12 weeks of aerobic training on a treadmill and resistance exercises, performed three times a week, led to significant decreases in the participants’ lipid profile, with the reduction in oxidized LDL more effective in individuals submitted to exercises47. Statin users that practiced physical exercises had an increase in maximum oxygen consumption compared to their sedentary peers, with a similar effect observed for the muscle strength variables, with no increase in CK levels or the reports of pain, which demonstrates that this combination results in health variable improvements with no additional damage to the musculature of practitioners47.
In summary, it can be observed that treatment with statins, both in elderly men and the general adult population, when combined with 12 weeks of aerobic training with aerobic and resistance exercises, does not increase reports of pain or CK levels, in addition to leading to gains in muscle and metabolic functions resulting from the training. Despite the little evidence and the need for longer studies, with different exercise modalities and training intensities, and the assessment of alterations in muscle tissue, these results show that performing moderate exercise during statin use is safe and more beneficial than remaining sedentary.
Mechanisms of muscle responses to statins and physical exercises
To date, evidence from research indicates that the intense training performed by athletes, as well as the practice of eccentric and strenuous exercise may exacerbate muscle injury caused by statin administration. In this regard, Meador and Huey21 proposed, in their review study, some of the mechanisms by which exercise exacerbates muscle injury caused by statins. According to the authors, the mitochondrial damage caused by statins, associated with increased energy flow and glycogen depletion due to the exercise, could be an exacerbation factor; however, they add other possibilities, such as the activation of the protein kinase pathway signaled by isoprenoids and stimulated by muscle contraction, as well as increases in the UPS pathway activity mediated by both statins and exercise.
In spite of this theoretical explanatory model of possible muscle injury exacerbation mechanisms, the scientific evidence to support these hypotheses is still scarce. The increased expression of genes involved in protein catabolism and UPS pathway was identified only in the research Urso et al.42, while mitochondrial damages and energy supply disorders have been further explored, having been verified in both the studies by Seachrist et al.44, as in more recent studies.
In this regard, Bouitbir et al.26 reported that rats treated with atorvastatin (10 mg / kg / day) showed mitochondrial function loss in the plantar muscle. The exposure of these animals to an exhaustive exercise test on a treadmill produced 226% more ROS than in the placebo group, with a reduction in maximum mitochondrial respiration (-39%) also being observed, which was significantly associated with the shortest distance walked in the test (r = 0.62; p <0.01). ROS are generated in the mitochondria as a result of energy metabolism and their increased production can cause damage to lipids, proteins and cellular DNA, altering mitochondrial function and triggering deleterious effects to muscle. These results indicate that exhaustive exercise, associated with mitochondrial damage resulting from treatment with statins, actually exacerbate metabolic disorders in skeletal muscle, resulting in a more oxidant status in this structure and, consequently, reducing the effort capacity of the animals.
This disorder in the muscle energy supply system caused by the use of statins has also been found in humans, as shown in the work by Wu et al.48, which characterized the kinetics of PCr recovery after calf effort in individuals of both sexes (n = 10, 35 to 69 years) treated with statins for 4 weeks.
The muscle PCr metabolic recovery rate is a parameter used as an index of muscle oxidative capacity in vivo, with a longer recovery time reflecting impaired oxidative phosphorylation and/or mitochondrial ATP synthesis. The results showed that exposure to statins did not alter CK levels, but resulted in a significant increase in metabolic recovery time after effort (from 28.1 to 55.4 seconds; p = 0.02), suggesting that this drug may impair mitochondrial oxidative function, which could explain the possible muscle involvement caused by its association with physical exercise.
Despite evidence indicating non-selective mitochondrial damage in the muscles of statin users, symptomatic individuals are apparently more predisposed to lesions and show more marked injury. In this regard, Hubal et al.49 assessed the global pattern of gene expression on skeletal muscle of patients of both sexes that used myalgia-inducing statins (n = 9) or not (n = 5) in response to eccentric exercise. After 4 months of drug treatment, it was found that patients who had classic signs and symptoms of myalgia had decreased NADH expression of complex I of the electron transport chain, as well as decreased succinate dehydrogenase in complex II, cytochrome c oxidase in complex IV and ATP4B in complex V, indicating that pre-existing deficiencies in energy production could contribute to the development of symptoms caused by physical effort during statin therapy49.
However, information about the association of statins to moderate chronic exercise suggests that other responses may occur, in addition to muscle injury exacerbation. According to Meador and Huey21, muscle adaptations caused by training, such as increased heat shock protein protection (related to the reduction in oxidative stress, apoptosis inhibition and muscle injury attenuation), direct suppression of apoptotic factors and increased mitochondrial biogenesis may result in muscle injury attenuation. To test this hypothesis, the same authors submitted mice to 14 days of combined treatment consisting of physical exercise and statins, after a previous adaptation of 14 days to exercise or physical inactivity and found that the drug reduced muscle strength and fatigue resistance in sedentary and non-adapted animals, when compared to adapted ones, indicating that adaptation to exercise protects the skeletal muscles against the deleterious effects of statins50.
Similarly, Bouitbir et al.25 found that training for 10 days on a treadmill improved the oxidative and antioxidant capacity of the plantar muscle in Wistar rats compared to sedentary animals, and that in vitro exposure of the muscles of sedentary animals to atorvastatin reduced the oxidative capacity in a dose-dependent manner. However, they demonstrated that the impaired mitochondrial function caused by drug exposure was lower in the muscles of trained animals, indicating a protective effect of physical exercise related to the improvement of mitochondrial respiration and antioxidant capacity, aimed at attenuating statin-induced oxidative stress.
The extrapolation of these results to humans seems to suggest that physically active individuals prior to treatment with statins may be protected from the deleterious drug effects, indicating that the prescription of exercise training prior to drug therapy with statins might be a preventive measure to muscle effects. Despite the evidence, Bonfim et al.51 recently found that many patients with dyslipidemia undergoing treatment with statins are sedentary and, therefore, would not be previously protected if they chose to carry out changes in their lifestyle.
Practical contributions
In a recent review study, Opie52 briefly explored the controversies between beneficial heart effects and myopathic side effects of the statin and exercise association, outlining some practical guidelines for this situation. Based on the findings of Kokkinos et al.5, who found that statin therapy associated with a moderate-to-high physical fitness level offers additional protection against premature cardiovascular death, and a meta-analysis of prospective studies that assessed the association of dose-response between exercise intensity and cardiovascular protection, the author recommends the practice of brisk walking for at least 3 hours a week to maintain cardiovascular protection, but does not provide more specifications regarding the intensity.
Considering the side effects on musculature, the author proposes that dyslipidemic individuals using statins that have their running capacity limited due to isolated muscle pain, choose carrying out shorter or slower runs; however, he emphasizes that the lack of evidence in the literature to deal with cases where the pain is accompanied by an increase in CK levels allows both the cessation or reduction in medication dose, as well as reducing the intensity of exercise as possible therapeutic measures, stressing the urgent need to perform further research to find the balance between muscle symptoms and cardiovascular protection levels52.
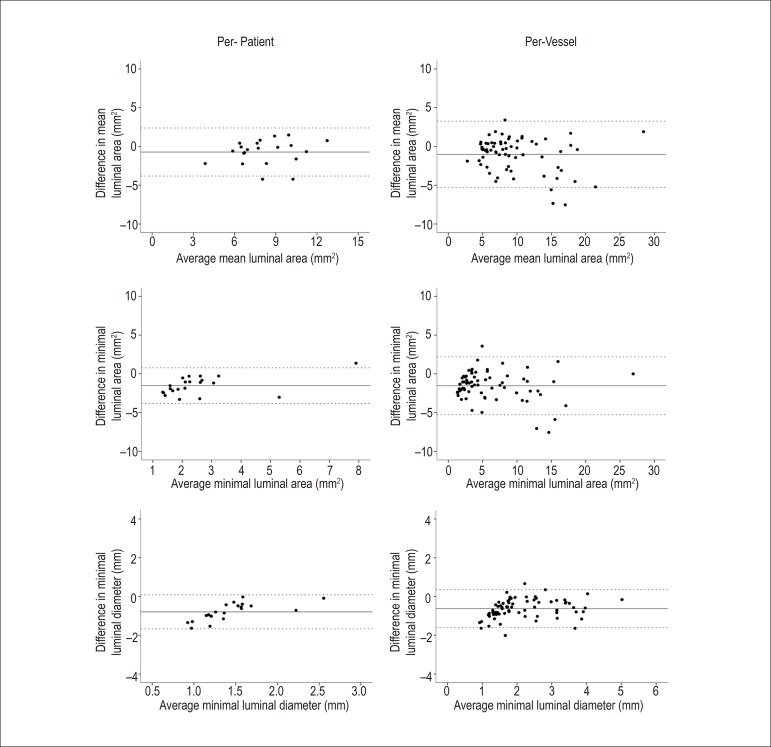
In summary, considering the current state-of-the-art, it is observed that the situations of muscle injury caused by statins may be exacerbated by high-intensity physical training and acute eccentric and strenuous exercises, while the chronic practice of exercises at moderate intensity, both before and concomitantly to treatment with statins, can attenuate the injuries and even improve muscle function of the practitioners (Figure 2). In this sense, it is suggested that dyslipidemic patients on statins be exposed to aerobic exercises combined with resistance exercises of moderate intensity, three days a week. The provision of physical training prior to the administration of drug treatment is desirable; however, in cases when this is not feasible, we suggest caution in prescribing physical activity during the first weeks, when strenuous and eccentric exercises should be avoided.
Figure 2.
Muscle responses of the association of statins with physical exercise. Strenuous exercises are characterized by acute eccentric exercises, maximum capacity tests and/or competitive activities; moderate exercises are characterized by aerobic training, with or without resistance training, usually performed three times a week for 12 weeks. UP: ubiquitin proteasome.
Conclusion
The research evidence shows that intense training performed by athletes, as well as the practice of eccentric and strenuous exercises may exacerbate muscle injury resulting from the administration of statins. On the other hand, chronic exercises of moderate intensity, performed both before and concurrently to treatment with statins, can attenuate the harmful effects and improve muscle function in its practitioners.
Footnotes
Author contributions
Conception and design of the research:Bonfim MR. Acquisition of data: Bonfim MR. Analysis and interpretation of the data: Bonfim MR. Writing of the manuscript: Bonfim MR, Oliveira ASB, Amaral SL, Monteiro HL. Critical revision of the manuscript for intellectual content: Oliveira ASB, Amaral SL, Monteiro HL.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This article is part of the thesis of Doctoral submitted by Mariana Rotta Bonfim, from Programa de Pós-Graduação em Ciências da Motricidade of Universidade Estadual Paulista - UNESP, Campus de Rio Claro.
References
- 1.World Health Organization . The World Health Report 2002. Reducing risks, promoting healthy life. Geneva: 2002. [DOI] [PubMed] [Google Scholar]
- 2.Xavier HT, Izar MC, Neto Faria, JR, Assad MH, Rocha VZ, Sposito AC, Sociedade Brasileira de Cardiologia V Diretriz brasileira de dislipidemias e prevenção da aterosclerose. Arq Bras Cardiol. 2013;101(4) supl. 1:1–22. doi: 10.5935/abc.2013S010. [DOI] [PubMed] [Google Scholar]
- 3.Sposito AC, Caramelli B, Fonseca FA, Bertolami MC, Afiune A, Neto, Souza AD, et al. Sociedade Brasileira de Cardiologia IV Diretriz brasileira sobre dislipidemias e prevenção da aterosclerose. Arq Bras Cardiol. 2007;88(supl 1):1–18. [Google Scholar]
- 4.National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 5.Kokkinos PF, Faselis C, Myers J, Panagiotakos D, Doumas M. Interactive effects of fitness and statin treatment on mortality risk in veterans with dyslipidaemia: a cohort study. Lancet. 2013;381(9864):394–399. doi: 10.1016/S0140-6736(12)61426-3. [DOI] [PubMed] [Google Scholar]
- 6.Joy TR, Hegele RA. Narrative review: statin-related myopathy. Ann Intern Med. 2009;150(12):858–868. doi: 10.7326/0003-4819-150-12-200906160-00009. [DOI] [PubMed] [Google Scholar]
- 7.Thompson PD, Clarkson PM, Rosenson RS, National Lipid Association Statin Safety Task Force Muscle Safety Expert Panel An assessment of statin safety by muscle experts. Am J Cardiol. 2006;97(8A):69C–76C. doi: 10.1016/j.amjcard.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Bruckert E, Hayem G, Dejager S, Yau C, B´Egaud B Mild to moderate muscular symptoms with high-dosage statin therapy in hyperlipidemic patients: the PRIMO study. Cardiovasc Drugs Ther. 2005;19(6):403–414. doi: 10.1007/s10557-005-5686-z. [DOI] [PubMed] [Google Scholar]
- 9.Krishnan GM, Thompson PD. The effects of statins on skeletal muscle strength and exercise performance. Curr Opin Lipidol. 2010;21(4):324–328. doi: 10.1097/MOL.0b013e32833c1edf. [DOI] [PubMed] [Google Scholar]
- 10.Veillard NR, Mach F. Statins: the new aspirin? Cell Mol Life Sci. 2002;59(11):1771–1786. doi: 10.1007/PL00012505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown WV. Safety of statins. Curr Opin Lipidol. 2008;19(6):558–562. doi: 10.1097/MOL.0b013e328319baba. [DOI] [PubMed] [Google Scholar]
- 12.Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA. 2003;289(13):1681–1690. doi: 10.1001/jama.289.13.1681. [DOI] [PubMed] [Google Scholar]
- 13.Parker BA, Thompson PD. Effect of statin on skeletal muscle: exercise, myopathy and muscle outcomes. Exerc Sport Sci Rev. 2012;40(4):188–194. doi: 10.1097/JES.0b013e31826c169e. Erratum in: Exerc Sport Sci Rev. 2013;41(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mansi I, Freil CR, Pugh MJ, Makris U, Mortensen EM. Statins and musculoskeletal conditions, arthropathies, and injuries. JAMA Intern Med. 2013;173(15):1477. doi: 10.1001/jamainternmed.2013.6184. [DOI] [PubMed] [Google Scholar]
- 15.Hoffman KB, Kraus C, Dimbil M, Golomb BA. A survey of the FDA's AERS database regarding muscle and tendon adverse events linked to the statin drug class. Plos One. 2012;7(8): doi: 10.1371/journal.pone.0042866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thompson PD, Parker BA, Clarkson PM, Pescatello LS, White CM, Grimaldi AS, et al. A randomized clinical trial to assess the effects of statins on skeletal muscle function and performance: rationale and study design. Prev Cardiol. 2010;13(3):104–111. doi: 10.1111/j.1751-7141.2009.00063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parker BA, Capizzi JA, Grimaldi AS, Clarkson PM, Cole SM, Keadle J, et al. Effect of statin on skeletal muscle function. Circulation. 2013;127(1):96–103. doi: 10.1161/CIRCULATIONAHA.112.136101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ballard KD, Parker BA, Capizzi JA, Grimaldi AS, Clarkson PM, Cole SM, et al. Increases in creatine kinase with atorvastatin treatment are not associated with decreases in muscular performance. Atherosclerosis. 2013;230(1):121–124. doi: 10.1016/j.atherosclerosis.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sirvent P, Mercier J, Lacampagne A. New insights into mechanisms of statin-associated myotoxicity. Curr Opin Pharmacol. 2008;8(3):333–338. doi: 10.1016/j.coph.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 20.Di Stasi SL, Macleod TD, Winters JD, Binder-Macleod SA. Effects of statins on skeletal muscle: a perspective for physical therapists. Phys Ther. 2010;90(10):1530–1542. doi: 10.2522/ptj.20090251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meador B, Huey KA. Statin-associated myopathy and its exacerbation with exercise. Muscle Nerve. 2010;42(4):469–479. doi: 10.1002/mus.21817. [DOI] [PubMed] [Google Scholar]
- 22.Muraki A, Miyashita K, Mitsuishi M, Tamaki M, Tanaka K, Itoh H. Coenzyme Q10 reverses mitochondrial dysfunction in atorvastatin-treated mice and increases exercise endurance. J Appl Physiol (1985) 2012;113(3):479–486. doi: 10.1152/japplphysiol.01362.2011. [DOI] [PubMed] [Google Scholar]
- 23.Deichmann R, Lavie C, Andrews S. Coenzyme q10 and statin-induced mitochondrial dysfunction. Ochsner J. 2010;10(1):16–21. [PMC free article] [PubMed] [Google Scholar]
- 24.Camerino GM, Pellegrino MA, Brocca L, Digennaro C, Camerino DC, Pierno S, et al. Statin or fibrate chronic treatment modifies the proteomic profile of rat skeletal muscle. Biochem Pharmacol. 2011;81(8):1054–1064. doi: 10.1016/j.bcp.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 25.Bouitbir J, Daussin F, Charles AL, Rasseneur L, Dufour S, Richard R, et al. Mitochondria of trained skeletal muscle are protected from deleterious effects of statins. Muscle Nerve. 2012;46(3):367–373. doi: 10.1002/mus.23309. [DOI] [PubMed] [Google Scholar]
- 26.Bouitbir J, Charles AL, Rasseneur L, Dufour S, Piquard F, Geny B, et al. Atorvastatin treatment reduces exercise capacities in rats: involvement of mitochondrial impairments and oxidative stress. J Appl Physiol (1985) 2011;111(5):1477–1483. doi: 10.1152/japplphysiol.00107.2011. [DOI] [PubMed] [Google Scholar]
- 27.Stringer HA, Soshi GK, Maguire JA, Côté HC. Decreased skeletal muscle mitochondrial DNA in patients with statin-induced myopathy. J Neurol Sci. 2013;325(1-2):142–147. doi: 10.1016/j.jns.2012.12.023. [DOI] [PubMed] [Google Scholar]
- 28.Larsen S, Stride N, Hey-Mogensen M, Hansen CN, Bang LE, Bundgaard H, et al. Simvastatin effects on skeletal muscle: relation to decreased mitochondrial function and glucose intolerance. J Am Coll Cardiol. 2013;61(1):44–53. doi: 10.1016/j.jacc.2012.09.036. [DOI] [PubMed] [Google Scholar]
- 29.Sirvent P, Mercier J, Vassort G, Lacampagne A. Simvastatin triggers mitochondria-induced Ca2+ signaling alteration in skeletal muscle. Biochem Biophys Res Commun. 2005;329(3):1067–1075. doi: 10.1016/j.bbrc.2005.02.070. [DOI] [PubMed] [Google Scholar]
- 30.Sirvent P, Bordenave S, Vermaelen M, Roels B, Vassort G, Mercier J, et al. Simvastatin induces impairment in skeletal muscle while heart is protected. Biochem Biophys Res Commun. 2005;338(3):1426–1434. doi: 10.1016/j.bbrc.2005.10.108. [DOI] [PubMed] [Google Scholar]
- 31.Liantonio A, Giannuzzi V, Cippone V, Camerino GM, Pierno S, Camerino DC. Fluvastatin and atorvastatin affect calcium homeostasis of rat skeletal muscle fibers in vivo ans in vitro by impairing the sarcoplasmic reticulum/mitochondria Ca2+-release system. J Pharmacol Exp Ther. 2007;321(2):626–634. doi: 10.1124/jpet.106.118331. [DOI] [PubMed] [Google Scholar]
- 32.Mohaupt MG, Karas RH, Babiychuk EB, Sanchez-Freire V, Monastyrskaya K, Iyer L, et al. Association between statin-associated myopathy and skeletal muscle damage. CMAJ. 2009;181(1-2):E11–E18. doi: 10.1503/cmaj.081785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Draeger A, Sanchez-Freire V, Monastyrskaya K, Hoppeler H, Mueller M, Breil F, et al. Statin therapy and the expression of genes that regulate calcium homeostasis and membrane repair in skeletal muscle. Am J Pathol. 2010;177(1):291–299. doi: 10.2353/ajpath.2010.091140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sirvent P, Fabre O, Bordenave S, Hillaire-Buys D, Raynaud De Mauverger E, Lacampagne A, et al. Muscle mitochondrial metabolism and calcium signaling impairment in patients treated with statins. Toxicol Appl Pharmacol. 2012;259(2):263–268. doi: 10.1016/j.taap.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 35.Galtier F, Mura T, Mauverger ER, Chevassus H, Farret A, Gagnol JP, et al. Effect of a high dose of simvastatin on muscle mitochondrial metabolism and calcium signaling in healthy volunteers. Toxicol Appl Pharmacol. 2012;263(3):281–286. doi: 10.1016/j.taap.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 36.Sinzinger H, O'Grade J. Professional athletes suffering from familial hypercholesterolemia rarely tolerate statin treatment because of muscular problems. Br J Clin Pharmacol. 2004;57(4):525–528. doi: 10.1111/j.1365-2125.2004.02044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Parker BA, Augeri AL, Capizzi JA, Ballard KD, Troyanos C, Gaggish AL, et al. Effects of statin on creatine kinase levels before and after a marathon run. Am J Cardiol. 2012;109(2):282–287. doi: 10.1016/j.amjcard.2011.08.045. [DOI] [PubMed] [Google Scholar]
- 38.Thompson PD, Zmuda JM, Domalik LJ, Zimet RJ, Staggers J, Guyton JR. Lovastatin increases exercised-induced skeletal muscle injury. Metabolism. 1997;46(10):1206–1210. doi: 10.1016/s0026-0495(97)90218-3. [DOI] [PubMed] [Google Scholar]
- 39.Reust CS, Curry SC, Guidry JR. Lovastatin use and muscle damage in healthy volunteers undergoing eccentric muscle exercise. West J Med. 1991;154(2):198–200. [PMC free article] [PubMed] [Google Scholar]
- 40.Kearns AK, Bilbie CL, Clarkson PM, White CM, Sewright KA, et al. O´Fallon KS The creatine kinase response to eccentric exercise with atorvastatin 10 mg or 80 mg. Atherosclerosis. 2008;200(1):121–125. doi: 10.1016/j.atherosclerosis.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 41.Panayiotou G, Paschalis V, Nikolaidis MG, Theodorou AA, Deli CK, Fotopoulou N, et al. No adverse effects of statin on muscle function ans health-related parameters in the elderly: an exercise study. Scand J Med Sci Sports. 2013;23(5):556–567. doi: 10.1111/j.1600-0838.2011.01437.x. [DOI] [PubMed] [Google Scholar]
- 42.Urso ML, Clarkson PM, Hittel D, Hoffman E, Thompson PD. Changes in ubiquitin proteasome pathway gene expression in skeletal muscle with exercise and statins. Asterioscler Thromb Vasc Biol. 2005;25(12):2560–2566. doi: 10.1161/01.ATV.0000190608.28704.71. [DOI] [PubMed] [Google Scholar]
- 43.Aciolly MF, Camargo JC, Filho, Padulla SAT, Lima ALZ, Bonfim MR, Carmo EM, et al. Efeito do exercício físico e estatinas na função muscular em animas com dislipidemia. Rev Bras Med Esp. 2012;18(3):198–202. [Google Scholar]
- 44.Seachrist JL, Loi C, Evans MG, Criswell KA, Rothwell CE. Roles of exercise and pharmacokinetics in cerivastatin-induced skeletal muscle toxicity. Toxicol Sci. 2005;88(2):551–561. doi: 10.1093/toxsci/kfi305. [DOI] [PubMed] [Google Scholar]
- 45.Meex RC, Phielix E, Schrauwen-Hinderling VB, Moonen-Kornips E, Schaart G, Schrauwen P, et al. The use of statins potentiates the insulin-sensitizing effect of exercise training in obese males with and without type 2 diabetes. Clin Sci. 2010;119(7):293–301. doi: 10.1042/CS20100153. [DOI] [PubMed] [Google Scholar]
- 46.Mikus CR, Boyle LJ, Borengasser SJ, Oberlin DJ, Naples SP, Fletcher J, et al. Simvastatin impairs exercise training adaptations. J Am Coll Cardiol. 2013;62(8):709–714. doi: 10.1016/j.jacc.2013.02.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Coen PM, Flynn MG, Markifski MM, Pence BD, Hannemann RE. Adding exercise training to rosuvastatin treatment: influence on serum lipids and biomarkers of muscle and liver damage. Metabolism. 2009;58(7):1030–1038. doi: 10.1016/j.metabol.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 48.Wu JS, Buettner C, Smithline H, Ngo LH, Greenman RL. Evaluation of skeletal muscle during calf exercise by 31-phosphorus magnetic resonance spectroscopy in patients on statin medications. Muscle Nerve. 2011;43(1):76–81. doi: 10.1002/mus.21847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hubal MJ, Reich KA, Biase A, Bilbie C, Clarkson PM, Hoffman EP, et al. Transcriptional deficits in oxidative phosphorylation with statin myopathy. Muscle Nerve. 2011;44(3):393–401. doi: 10.1002/mus.22081. [DOI] [PubMed] [Google Scholar]
- 50.Meador B, Huey KA. Statin-associated changes in skeletal muscle function and stress response after novel or accustomed exercise. Muscle Nerve. 2011;44(6):882–889. doi: 10.1002/mus.22236. [DOI] [PubMed] [Google Scholar]
- 51.Bonfim MR, Hansen A, Turi BC, Zanini GS, Oliveira AS, Amaral SL, et al. Aderência ao tratamento por estatinas e fatores associados em usuárias do SUS. Rev Esc Enferm USP. 2014;48(3):477–483. doi: 10.1590/s0080-623420140000300013. [DOI] [PubMed] [Google Scholar]
- 52.Opie LH. Exercise-induced myalgia may limit the cardiovascular benefits of statins. Cardiovasc Drugs Ther. 2013;27(6):569–572. doi: 10.1007/s10557-013-6483-8. [DOI] [PubMed] [Google Scholar]