Abstract
Introduction
Luseogliflozin, a potent, selective sodium glucose cotransporter 2 inhibitor, promotes urinary glucose excretion (UGE) and reduces plasma glucose concentrations. Luseogliflozin was approved for use in Japan after favorable pharmacokinetic, pharmacodynamic, and safety profiles were reported in healthy Japanese subjects and patients with type 2 diabetes mellitus (T2DM) in clinical development studies. We aimed to investigate the pharmacokinetics, pharmacodynamics, and safety of multiple doses of luseogliflozin administered once daily for 7 days in Japanese patients with T2DM.
Methods
We conducted a randomized, placebo-controlled, single-blind, parallel-group, clinical pharmacology study at the P-One Clinic, Keikokai Medical Corporation (Tokyo, Japan) between August 2009 and November 2009. Forty Japanese patients with T2DM were randomly assigned to receive once-daily 0.5, 1, 2.5 or 5 mg luseogliflozin or placebo for 7 days. We assessed the pharmacokinetics, pharmacodynamics (including changes in UGE and plasma glucose concentrations), and safety of luseogliflozin.
Results
The plasma concentrations of luseogliflozin and its active metabolite, M2, were dose proportional, without accumulation. 24-h UGE was greater in all luseogliflozin groups versus placebo. Least-squares mean differences in 24-h UGE on Day 7 increased dose dependently in the luseogliflozin groups, with values of 49.2, 66.5, 89.4, and 101 g/day at 0.5, 1, 2.5, and 5 mg, respectively. On Day 7, the areas under the concentration–time curves for post-meal plasma glucose and the mean plasma glucose for 0–16 h were significantly lower in all luseogliflozin groups versus placebo. Seven patients had mild adverse events (AEs); all were resolved. No AEs led to study discontinuation.
Conclusion
Once-daily administration of luseogliflozin for 7 days increased 24-h UGE in a dose-dependent manner, reduced plasma glucose concentrations, and was well tolerated in Japanese patients with T2DM. The pharmacokinetic and pharmacodynamic profile of luseogliflozin observed in this study supports its once-daily dosing regimen.
Funding
Taisho Pharmaceutical Co., Ltd.
Electronic supplementary material
The online version of this article (doi:10.1007/s12325-015-0200-x) contains supplementary material, which is available to authorized users.
Keywords: Luseogliflozin, Pharmacodynamics, Sodium glucose cotransporter 2 (SGLT2), Type 2 diabetes mellitus, Urinary glucose excretion
Introduction
Glucose filtered through the glomerulus is reabsorbed by sodium glucose cotransporters (SGLTs) 1 and 2, which are expressed in the renal proximal tubules. SGLT2, in particular, plays a major role in glucose reabsorption, accounting for approximately 90% of glucose reabsorbed in the kidney [1]. In healthy subjects, all glucose is reabsorbed in the kidney and none is excreted into urine. However, if plasma glucose concentrations exceed 160–180 mg/dL, saturation of glucose reabsorption occurs and some glucose is excreted into urine [2]. Inhibition of SGLT2 decreases the threshold of glucose reabsorption in the kidney, promotes urinary glucose excretion (UGE), and reduces plasma glucose concentrations. Because of this effect, several SGLT2 inhibitors have been developed and some have already been approved [3–5].
Luseogliflozin is a potent and selective SGLT2 inhibitor with a 50% inhibitory concentration (IC50) of 2.26 nM, which is 1765-fold lower than its IC50 for SGLT1 [6, 7]. In previous Phase I clinical studies, single doses of 1–25 mg luseogliflozin and multiple doses of 5 or 10 mg luseogliflozin for 7 days were well tolerated, and showed favorable pharmacokinetic and pharmacodynamic profiles in healthy Japanese males [8]. Subsequent Phase II [9, 10] and Phase III [11] studies have demonstrated that luseogliflozin monotherapy significantly improves hemoglobin A1c (HbA1c), fasting plasma glucose (FPG), postprandial plasma glucose, body weight, and abdominal circumference over 12–24 weeks of administration in Japanese patients with type 2 diabetes mellitus (T2DM). Administration of luseogliflozin was also well tolerated in these studies, with most adverse events (AEs) being rated as mild in severity. Based on the results of these studies, luseogliflozin was recently approved in Japan for the treatment of T2DM [12].
As part of the clinical development of luseogliflozin, we conducted this study to assess the pharmacokinetics, pharmacodynamics (including the changes in UGE and plasma glucose concentrations), and safety of multiple doses of luseogliflozin administered once daily (OD) for 7 days in patients with T2DM. The objective of the study was to compare the pharmacokinetics and pharmacodynamics of varying doses of luseogliflozin and provide the rationale for the doses used in the recently published Phase II [9, 10] and Phase III [11] studies.
Methods
This study was conducted at P-One Clinic, Keikokai Medical Corporation (Tokyo, Japan) between August 2009 and November 2009. All procedures were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national), the Helsinki Declaration of 1964, as revised in 2000 and 2008, the Japanese Pharmaceutical Affairs Law and Good Clinical Practice. The study protocol was approved by the Institutional Review Board of P-One Clinic, Keikokai Medical Corporation. Informed consent was obtained from all patients for being included in the study. This study was registered with the Japan Pharmaceutical Information Center (identifier: JapicCTI-090909).
Study Design
This randomized, single-blind, placebo-controlled, parallel-group, 7-day multiple-dose study was performed in 40 patients with T2DM. The randomization scheme was prepared by the drug allocation manager using the PLAN procedure (SAS version 9.1.3; SAS Institute Inc., Cary, NC, USA); the drug allocation manager placed the individual randomization codes into envelopes, which were sent to the study drug allocation controller. After the investigator confirmed the patient’s eligibility (see “Eligibility criteria” section below), the study drug allocation controller opened the envelope and notified the investigator of the allocated group. All study drugs were indistinguishable in appearance and the patients were blinded to the treatment received. Each patient was admitted to the study institution from Days −2 to 2 and from Days 6 to 11. Subjects were randomized to receive 0.5, 1, 2.5 or 5 mg luseogliflozin, or placebo, OD for 7 days from Day 1 to Day 7. On Days 1 and 7, the study drugs were administered with 150 mL of water before breakfast. On Days −1 (1 day before starting drug administration), 1 (first dose), and 7 (last dose), the patients consumed a standardized meal of approximately 600 kcal (approximately 16% protein, 21% fat, and 63% carbohydrate). On these days, the patients ate lunch and dinner at 4 and 12 h, respectively, after breakfast (Day −1) or study drug administration (Days 1 and 7).
Pharmacokinetic parameters were assessed using venous blood samples obtained at the following times: before study drug administration (0 h), and 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, and 24 h after administration on Days 1 and 7; and before breakfast on Days 9, 10, and 11. Plasma glucose was measured using blood samples obtained at the following times: before breakfast, and 0.5, 1, 2, 4, 4.5, 5, 6, 8, 12, 12.5, 13, 14, 16, and 24 h after breakfast on Day −1; before study drug administration (0 h), and 0.5, 1, 2, 4, 4.5, 5, 6, 8, 12, 12.5, 13, 14, 16, and 24 h after study drug administration on Days 1 and 7; and before breakfast on Days 11 and 14. Serum insulin was measured using venous blood samples obtained at the following times: before breakfast, and 0.5, 1, 2, and 4 h after breakfast on Day −1; and before study drug administration (0 h), and 0.5, 1, 2, and 4 h after study drug administration on Days 1 and 7. Glucose concentrations were measured using an enzymatic method based on glucose dehydrogenase with ultraviolet measurement. Insulin concentrations were measured using a chemiluminescent assay kit. For pharmacokinetic and pharmacodynamic assessments, urine samples were pooled for 0–2, 2–4, 4–6, 6–8, 8–10, 10–12, 12–14, 14–16, and 16–24 h on Days −1, 1, and 7, and for 0–24 h on Days 8, 9, 10, and 13. The volume of water intake was recorded for similar periods to urine collection.
Eligibility Criteria
Japanese outpatients with T2DM diagnosed according to the guidelines proposed by the Japan Diabetes Society [13] were eligible if they met the following criteria: HbA1c 6.9–10.5%; FPG ≥126 mg/dL; prescribed stable diet therapy for 4 weeks before study drug administration; and aged 20–74 years. The exclusion criteria included the following: insulin-dependent state; diagnosis of diabetes other than T2DM; the presence of an endocrine disease likely to affect blood glucose; current renal disease; history of chronic renal disorder (based on the investigator’s diagnosis and considering the standard values for renal variables, such as serum creatinine level) or nephrectomy/renal transplantation; current or history of repeated urinary tract infection (as diagnosed by the investigator); clinically evident hepatic disorder (e.g., alanine aminotransferase or aspartate aminotransferase activities ≥2.5 times the upper limit of the reference range); current serious gastrointestinal disorder, serious cardiac disorder or severe diabetic microangiopathy; current or history of malignant tumor; serious allergic disposition; use of oral antidiabetic drugs/insulin ≤ 4 weeks or thiazolidinedione ≤12 weeks before study drug administration; use of an investigational drug ≤12 weeks before the start of the observation period; prior administration of luseogliflozin; heavy alcohol consumption (average consumption of >100 mL of 100% ethanol per day); pregnancy or breastfeeding; positive results in any infection-related blood test; or were deemed by the investigator to be unsuitable for any other reason. All patients provided written informed consent before enrollment.
Clinical Evaluations
Pharmacokinetic endpoints included the plasma and urinary concentrations of luseogliflozin and its active metabolite, M2 (O-deethyl form). Blood and urine samples were collected at the times specified above. The blood samples were immediately processed to extract plasma by centrifugation and stored at −70 °C until analysis. The urine samples were pooled at 4 °C, and then 4 mL samples were stored at −70 °C until pharmacokinetic analysis.
The plasma and urinary concentrations of luseogliflozin and M2 were determined by four validated and separate methods using high-performance liquid chromatography tandem mass spectrometry (LC–MS/MS). For the quantification, stable isotope (deuterium)-labeled internal standards (luseogliflozin-d5 and M2-d5, Taisho Pharmaceutical Co. Ltd., Tokyo, Japan) were used. After solid-phase extraction from plasma or urine, these samples were analyzed by LC–MS/MS. For luseogliflozin, the lower limits of quantification (LLOQ) were 0.05 and 0.5 ng/mL in plasma and urine, respectively. The LLOQ for M2 were 0.1 and 1 ng/mL in plasma and urine, respectively. These analyses were performed by JCL Bioassay Corp. (Nishiwaki, Japan).
Pharmacodynamic endpoints included UGE, and plasma glucose and insulin concentrations. Safety endpoints included the nature and frequency of AEs and adverse drug reactions, the changes in laboratory values (e.g., serum electrolytes, renal function markers, and hematology), body weight, vital signs, and 12-lead electrocardiography. Hypoglycemia was defined as symptoms consistent with hypoglycemia or plasma glucose concentration <70 mg/dL.
Assessments and Statistical Methods
For this study, we planned to enroll eight patients into each of the luseogliflozin groups to evaluate the safety, pharmacokinetics, and pharmacodynamics of each dose. We also planned to enroll eight patients into the control group as a reference.
All statistical analyses were performed using SAS statistical software (version 9.1.3; SAS Institute Inc.). All of the patients who received luseogliflozin or placebo at least once were included in the safety analysis set. Patients who completed the study without critical protocol deviations and whose data for pharmacokinetic and pharmacodynamic assessment were available were included in the pharmacokinetic and pharmacodynamic analysis sets, respectively.
Pharmacokinetic variables were determined using the plasma concentrations of luseogliflozin or M2, and included the maximum concentration (C max), the time to the maximum concentration (t max), the area under the concentration–time curve (AUC), and the elimination half-life (t 1/2), which were calculated using the non-compartmental method. The pharmacokinetic dose proportionality was evaluated using a power model with C max and the AUC for the dosing period (AUCτ) for luseogliflozin on Day 7.
Pharmacodynamic variables included 24-h cumulative UGE, total UGE, and UGE rate in each collection period. In addition, the AUC, C max, and t max for plasma glucose and serum insulin concentrations on Days −1, 1, and 7 were calculated using the non-compartment model. The mean plasma glucose (MPG) was calculated as the mean of the plasma glucose values at 0, 2, 4, 6, 12, 14, and 16 h. The dose effect and dose proportionality were assessed using pharmacodynamic parameters determined using the power model (Eq. 1) and were compared among the study groups using β coefficients (converted to log10 values) and 95% confidence intervals. The least-squares (LS) mean differences between placebo and each luseogliflozin dose with 95% confidence intervals were estimated for each parameter. Correlations between the change in UGE and the change in plasma glucose were also assessed graphically.
| 1 |
where eij is an error term based on an independent normal distribution, κi the dose (I = 1 [0.5 mg], 2 [1 mg], 3 [2.5 mg] or 4 [5 mg]), μ the overall mean value, N the total number of patients in each treatment group, and yij the value for the pharmacodynamic parameter of interest.
Regression analysis was performed using the sigmoid E max model (Eq. 2) with the AUC0–24h for plasma glucose and the change in UGE for each subject.
| 2 |
where AUC is the area under the curve, EC50 the AUC at 50% of the UGE, E max the maximum change in UGE, γ the Hill coefficient, and UGE the urinary glucose excretion.
Adverse events were coded using the Medical Dictionary for Regulatory Activities (MedDRA) version 12.1. AEs were classified in terms of severity (mild, moderate, or severe) and possible association with the study drug (definitely related, probably related, possibly related, not related, or unknown) by an investigator.
Results
Patients and Baseline Characteristics
Forty patients with T2DM (34 male and 6 female) were randomly assigned to receive luseogliflozin (0.5, 1, 2.5, or 5 mg) or placebo OD, of whom 39 completed the study. One patient who was allocated to 0.5 mg luseogliflozin discontinued with the study immediately after the first dose owing to withdrawal of consent. The ranges for mean values for age, body mass index, HbA1c, and estimated glomerular filtration rate among the five groups were 55.9–59.8 years, 23.43–26.78 kg/m2, 7.99–8.70%, and 84.7–103.9 mL/min/1.73 m2, respectively (Table 1).
Table 1.
Patient characteristics at baseline
| Placebo (N = 8) | Luseogliflozin | ||||
|---|---|---|---|---|---|
| 0.5 mg (N = 8) | 1 mg (N = 8) | 2.5 mg (N = 8) | 5 mg (N = 8) | ||
| Sex | |||||
| Male | 7 | 7 | 6 | 8 | 6 |
| Female | 1 | 1 | 2 | 0 | 2 |
| Age (years) | 57.3 ± 7.4 | 58.8 ± 10.1 | 59.8 ± 10.8 | 55.9 ± 8.8 | 57.6 ± 8.2 |
| Body weight (kg) | 75.96 ± 9.70 | 66.75 ± 13.61 | 72.12 ± 18.57 | 68.00 ± 7.90 | 71.80 ± 9.59 |
| BMI (kg/m2) | 26.78 ± 3.13 | 23.43 ± 3.37 | 25.94 ± 4.98 | 24.38 ± 3.35 | 26.13 ± 2.83 |
| Diabetes duration (years) | 3.4 ± 2.5 | 3.5 ± 3.9 | 5.3 ± 4.9 | 2.4 ± 1.6 | 4.4 ± 1.8 |
| HbA1c (%) | 8.51 ± 0.91 | 8.55 ± 1.02 | 8.01 ± 1.01 | 8.70 ± 1.08 | 7.99 ± 1.01 |
| FPG (mg/dL) | 166.5 ± 21.4 | 162.0 ± 29.2 | 151.3 ± 32.0 | 166.5 ± 37.9 | 150.1 ± 22.0 |
| UGE0–24h (g) | 26.3 ± 19.7 | 30.5 ± 24.7 | 17.0 ± 15.3 | 44.1 ± 29.4 | 16.2 ± 14.0 |
| eGFR (mL/min/1.73 m2) | 103.9 ± 21.4 | 84.7 ± 17.4 | 87.8 ± 13.2 | 89.3 ± 16.2 | 88.9 ± 22.4 |
Values are presented as the mean ± standard deviation
BMI body mass index, HbA1c hemoglobin A1c, FPG fasting plasma glucose, UGE 0–24h urinary glucose excretion from 0 to 24 h, eGFR estimated glomerular filtration rate
Pharmacokinetics
Figure 1 shows the plasma luseogliflozin concentration–time profiles on Days 1 and 7. The pharmacokinetic parameters of luseogliflozin and its active deethyl metabolite (M2) are summarized in Table 2. Luseogliflozin was rapidly absorbed after administration, reaching the C max between 0.625 and 1.00 h, measured as t max. The mean t 1/2 was approximately 10 h for all four doses. The plasma luseogliflozin concentration–time profile was similar on Days 1 and 7, although its concentrations were slightly higher on Day 7 than on Day 1. The AUC was extrapolated to infinity on Day 1 and AUCτ on Day 7 was comparable, which indicates that luseogliflozin does not accumulate after multiple doses in patients with T2DM. The plasma luseogliflozin concentration increased in a dose-dependent manner, and the power model revealed the dose proportionality for C max and AUCτ on Day 7 for the doses tested in this study (data not shown). Regarding M2, the mean t max was 2.00–5.86 h, t 1/2 was approximately 20 h, and the plasma concentration increased in a dose-dependent manner. On a molar basis, the ratio of M2 to luseogliflozin for the AUCs on Day 7 ranged from 0.138 to 0.148.
Fig. 1.
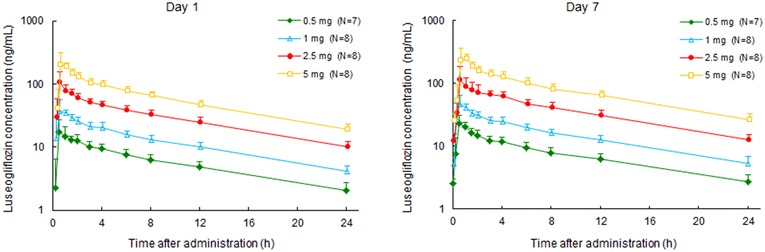
Plasma concentration–time profiles after single (Day 1) and multiple (Day 7) doses of luseogliflozin. Luseogliflozin was rapidly absorbed, reaching C max between 0.625 and 1.000 h. The concentration–time profiles were similar on Days 1 and 7, although the luseogliflozin concentrations were slightly higher on Day 7 than on Day 1. Values are presented as the mean ± standard deviation. C max maximum plasma concentration
Table 2.
Pharmacokinetic parameters of luseogliflozin and its major metabolite (M2) after single (Day 1) and multiple (Day 7) doses of luseogliflozin
| Dose | Day | C max (ng/mL) | t max (h) | AUC (ng h/mL)a | AUC ratiob | t 1/2 (h) | Ae0–24 (% of dose) |
|---|---|---|---|---|---|---|---|
| Luseogliflozin | |||||||
| 0.5 mg (N = 7) | Day 1 | 21.9 ± 2.88 | 0.857 ± 0.556 | 171 ± 38.4 | – | 9.86 ± 1.57 | 3.76 ± 0.832 |
| Day 7 | 25.6 ± 4.25 | 0.643 ± 0.244 | 179 ± 32.6 | – | 10.5 ± 1.03 | 4.56 ± 1.04 | |
| 1 mg (N = 8) | Day 1 | 43.7 ± 10.8 | 0.688 ± 0.259 | 357 ± 53.9 | – | 9.61 ± 1.34 | 4.06 ± 0.497 |
| Day 7 | 52.3 ± 10.9 | 0.688 ± 0.259 | 370 ± 55.5 | – | 10.0 ± 1.37 | 4.30 ± 0.875 | |
| 2.5 mg (N = 8) | Day 1 | 119 ± 27.0 | 0.625 ± 0.354 | 864 ± 132 | – | 9.24 ± 0.928 | 4.51 ± 1.13 |
| Day 7 | 136 ± 42.0 | 1.00 ± 0.886 | 899 ± 148 | – | 9.20 ± 0.710 | 4.79 ± 1.09 | |
| 5 mg (N = 8) | Day 1 | 243 ± 45.7 | 0.625 ± 0.231 | 1690 ± 271 | – | 8.96 ± 1.11 | 4.11 ± 0.763 |
| Day 7 | 299 ± 50.3 | 0.688 ± 0.259 | 1880 ± 318 | – | 9.54 ± 1.26 | 4.56 ± 0.617 | |
| M2 | |||||||
| 0.5 mg (N = 7) | Day 1 | 0.726 ± 0.136 | 4.71 ± 3.04 | 28.6 ± 6.17 | – | 24.7 ± 8.12 | 5.22 ± 0.848 |
| Day 7 | 1.30 ± 0.196 | 2.07 ± 0.932 | 22.8 ± 3.03 | 0.138 ± 0.0172 | 18.6 ± 2.45 | 10.4 ± 1.65 | |
| 1 mg (N = 8) | Day 1 | 1.61 ± 0.383 | 4.75 ± 1.83 | 62.7 ± 10.5 | – | 24.0 ± 8.91 | 5.86 ± 0.674 |
| Day 7 | 2.95 ± 0.522 | 2.44 ± 1.32 | 50.4 ± 7.62 | 0.147 ± 0.0229 | 17.6 ± 4.28 | 11.1 ± 1.27 | |
| 2.5 mg (N = 8) | Day 1 | 4.13 ± 0.554 | 3.31 ± 2.53 | 140 ± 31.3 | – | 20.2 ± 4.39 | 6.72 ± 0.749 |
| Day 7 | 6.64 ± 0.776 | 2.75 ± 1.13 | 116 ± 15.3 | 0.140 ± 0.0244 | 16.6 ± 2.42 | 11.2 ± 2.13 | |
| 5 mg (N = 7) | Day 1 | 8.90 ± 1.22 | 5.86 ± 3.08 | 306 ± 63.8 | – | 19.5 ± 4.41 | 6.70 ± 1.18 |
| Day 7 | 15.3 ± 2.37 | 2.00 ± 1.12 | 259 ± 50.8 | 0.148 ± 0.0136 | 19.3 ± 3.63 | 11.6 ± 2.49 | |
Values are presented as the mean ± standard deviation
Ae 0–24 amount of unchanged drug excreted in urine from 0 to 24 h, AUC inf area under the plasma concentration–time curve extrapolated to infinity, AUC τ area under the plasma concentration–time curve during the dosing interval, C max maximum plasma concentration, M2 active metabolite of luseogliflozin (O-deethyl form), t max time to the maximum plasma concentration, t 1/2 elimination half-life
aDay 1: AUCinf, Day7: AUCτ
bCalculated as AUCτ (M2)/AUCτ (luseogliflozin)
Pharmacodynamics
The pharmacodynamic variables after a single dose or multiple doses of luseogliflozin administered OD for 7 days are summarized in Table 3, and the changes in mean daily UGE from baseline (Day −1) are shown in Fig. 2. All four doses of luseogliflozin significantly increased UGE compared with placebo on Days 1 and 7 (all P < 0.05). The increases in 24-h UGE were dose dependent, and the LS mean differences versus placebo were 49.2, 66.5, 89.4, and 101 g for 0.5, 1, 2.5, and 5 mg luseogliflozin, respectively. Although UGE decreased in all four luseogliflozin groups after the last dose on Day 7, the UGE remained significantly greater in the 1 and 2.5 mg luseogliflozin groups (P < 0.05 versus placebo) up to Day 8, and in the 5 mg luseogliflozin group up to Day 9.
Table 3.
Pharmacodynamic parameters of luseogliflozin after single (Day 1) and multiple (Day 7) doses of luseogliflozin compared with placebo
| Placebo (N = 8) | Luseogliflozin | ||||
|---|---|---|---|---|---|
| 0.5 mg (N = 7) | 1 mg (N = 8) | 2.5 mg (N = 8) | 5 mg (N = 8) | ||
| UGE0–24h (g) | |||||
| Baseline | 26.3 ± 19.7 | 33.5 ± 25.0 | 17.0 ± 15.3 | 44.1 ± 29.4 | 16.2 ± 14.0 |
| Day 1 | 26.9 ± 20.0 | 81.5 ± 33.2 | 75.1 ± 23.3 | 139 ± 31.1 | 116 ± 29.0 |
| Day 7 | 26.6 ± 17.8 | 81.7 ± 30.1 | 85.3 ± 18.8 | 131 ± 29.9 | 120 ± 33.1 |
| LS mean difference at Day 1a | – | 46.4 (32.9, 60.0)* | 58.9 (45.7, 72.1)* | 91.7 (78.1, 105)* | 101 (87.6, 114)* |
| LS mean difference at Day 7a | – | 49.2 (27.9, 70.5)* | 66.5 (45.8, 87.1)* | 89.4 (68.2, 111)* | 101 (80.7, 122)* |
| Plasma glucose | |||||
| C max0–4h (after breakfast) (mg/dL) | |||||
| Baseline | 290 ± 34.9 | 278 ± 42.7 | 266 ± 45.2 | 304 ± 54.3 | 262 ± 29.7 |
| Day 1 | 281 ± 42.1 | 278 ± 53.0 | 255 ± 44.1 | 254 ± 48.7 | 231 ± 16.6 |
| Day 7 | 269 ± 37.9 | 243 ± 42.1 | 240 ± 31.3 | 219 ± 26.3 | 222 ± 19.4 |
| LS mean difference at Day 1a | – | 7.49 (−16.9, 31.9) | −5.69 (−29.6, 18.2) | −38.4 (−62.0, −14.8)* | −26.2 (−50.3, −2.12)* |
| LS mean difference at Day 7a | – | −19.0 (−41.1, 3.04) | −15.5 (−37.1, 6.15) | −58.1 (−79.4, −36.7)* | −31.3 (−53.1, −9.47)* |
| C max4–8h (after lunch) (mg/dL) | |||||
| Baseline | 269 ± 30.5 | 302 ± 53.9 | 252 ± 35.6 | 293 ± 48.2 | 237 ± 30.6 |
| Day 1 | 270 ± 48.8 | 259 ± 52.3 | 223 ± 33.7 | 250 ± 54.5 | 207 ± 33.1 |
| Day 7 | 277 ± 40.8 | 256 ± 61.7 | 229 ± 33.7 | 230 ± 30.0 | 211 ± 35.1 |
| LS mean difference at Day 1a | – | −43.5 (−68.5, −18.5)* | −30.5 (−54.1, −7.02)* | −43.5 (−67.2, −19.7)* | −32.4 (−56.5, −8.28)* |
| LS mean difference at Day 7a | – | −46.2 (−76.1, −16.3)* | −34.7 (−62.8, −6.53)* | −65.6 (−94.0, −37.1)* | −41.0 (−69.8, −12.1)* |
| C max12–16h (after dinner) (mg/dL) | |||||
| Baseline | 273 ± 37.0 | 297 ± 42.4 | 277 ± 42.0 | 300 ± 47.9 | 252 ± 33.6 |
| Day 1 | 283 ± 39.1 | 286 ± 32.5 | 255 ± 37.3 | 279 ± 40.2 | 225 ± 33.2 |
| Day 7 | 269 ± 30.5 | 274 ± 34.6 | 242 ± 41.3 | 250 ± 23.3 | 223 ± 38.8 |
| LS mean difference at Day 1a | – | −16.0 (−35.0, 3.05) | −31.3 (−49.4, −13.3)* | −26.1 (−44.6, −7.60)* | −41.8 (−60.2, −23.5)* |
| LS mean difference at Day 7a | – | −9.79 (−35.5, 15.9) | −29.4 (−53.8, −5.06)* | −36.2 (−61.2, −11.3)* | −33.7 (−58.4, −9.02)* |
| AUC0–4h (after breakfast) (mg h/dL) | |||||
| Baseline | 972 ± 163 | 950 ± 178 | 886 ± 163 | 1020 ± 204 | 875 ± 109 |
| Day 1 | 935 ± 160 | 946 ± 175 | 812 ± 158 | 868 ± 166 | 752 ± 87.6 |
| Day 7 | 931 ± 162 | 810 ± 156 | 780 ± 116 | 738 ± 102 | 708 ± 87.5 |
| LS mean difference at Day 1a | – | 29.4 (−25.0, 83.8) | −48.9 (−102, 4.37) | −106 (−159, −53.6)* | −100 (−154, −46.5)* |
| LS mean difference at Day 7a | – | −108 (−186, −29.3)* | −96.7 (−173, −20.0)* | −221 (−297, −145)* | −162 (−239, −84.9)* |
| AUC4–8h (after lunch) (mg h/dL) | |||||
| Baseline | 965 ± 108 | 1060 ± 202 | 875 ± 158 | 1060 ± 199 | 829 ± 115 |
| Day 1 | 937 ± 168 | 915 ± 207 | 766 ± 131 | 879 ± 176 | 710 ± 120 |
| Day 7 | 986 ± 133 | 887 ± 209 | 787 ± 126 | 802 ± 127 | 710 ± 105 |
| LS mean difference at Day 1a | – | −111 (−191, −31.1)* | −89.1 (−166, −11.9)* | −147 (−224, −69.0)* | −104 (−183, −25.1)* |
| LS mean difference at Day 7a | – | −165 (−267, −64.2)* | −138 (−236, −40.8)* | −250 (−348, −152)* | −184 (−284, −84.3)* |
| AUC12–16h (after dinner) (mg h/dL) | |||||
| Baseline | 945 ± 117 | 1030 ± 165 | 944 ± 147 | 1050 ± 190 | 882 ± 127 |
| Day 1 | 943 ± 111 | 989 ± 114 | 851 ± 117 | 944 ± 123 | 766 ± 118 |
| Day 7 | 921 ± 91.7 | 924 ± 108 | 824 ± 125 | 828 ± 63.2 | 755 ± 137 |
| LS mean difference at Day 1a | – | −16.3 (−69.6, 37.0) | −91.4 (−142, −40.8)* | −71.1 (−123, −19.2)* | −133 (−184, −81.7)* |
| LS mean difference at Day 7a | – | −44.7 (−122, 32.2) | −96.2 (−169, −23.2)* | −149 (−224, −73.6)* | −131 (−205, −57.5)* |
| MPG0–16h (mg/dL) | |||||
| Baseline | 222 ± 31.6 | 233 ± 45.2 | 206 ± 34.7 | 238 ± 45.4 | 199 ± 26.8 |
| Day 1 | 220 ± 34.3 | 224 ± 38.8 | 188 ± 30.0 | 210 ± 35.7 | 173 ± 26.7 |
| Day 7 | 221 ± 32.9 | 204 ± 35.3 | 184 ± 24.0 | 181 ± 21.2 | 168 ± 27.8 |
| LS mean difference at Day 1a | – | −6.39 (−16.6, 3.79) | −18.4 (−28.3, −8.55)* | −23.8 (−33.7, −13.9)* | −27.4 (−37.4, −17.4)* |
| LS mean difference at Day 7a | – | −25.0 (−42.2, −7.90)* | −27.5 (−44.1, −10.8)* | −50.1 (−66.7, −33.4)* | −38.9 (−55.7, −22.1)* |
| FPG (24 h after dose) (mg/dL) | |||||
| Baseline | 167 ± 21 | 166 ± 29 | 151 ± 32 | 167 ± 38 | 150 ± 22 |
| Day 1 | 164 ± 21 | 156 ± 23 | 146 ± 25 | 141 ± 23 | 132 ± 12 |
| Day 7 | 163 ± 25 | 145 ± 18 | 139 ± 14 | 122 ± 14 | 126 ± 13 |
| LS mean difference at Day 1a | – | −7.15 (−16.0, 1.71) | −7.90 (−16.6, 0.795) | −23.0 (−31.6, −14.4)* | −20.8 (−29.5, −12.1)* |
| LS mean difference at Day 7a | – | −18.4 (−31.1, −5.75)* | −18.1 (−30.5, −5.62)* | −41.3 (−53.5, −29.0)* | −30.6 (−43.1, −18.1)* |
| Serum insulin | |||||
| AUC0–4h (after breakfast) (μIU h/mL) | |||||
| Baseline | 157 ± 74.2 | 92.2 ± 34.7 | 161 ± 54.7 | 119 ± 45.7 | 198 ± 132 |
| Day 1 | 168 ± 74.4 | 95.0 ± 33.9 | 161 ± 67.9 | 101 ± 56.1 | 190 ± 118 |
| Day 7 | 158 ± 78.6 | 81.4 ± 39.4 | 125 ± 43.4 | 75.1 ± 29.4 | 157 ± 82.5 |
| LS mean difference at Day 1a | – | −13.8 (−43.1, 15.6) | −12.1 (−39.4, 15.3) | −32.7 (−60.4, −4.93)* | −17.0 (−44.8, 10.8) |
| LS mean difference at Day 7a | – | −32.3 (−62.8, −1.82)* | −36.1 (−64.5, −7.72)* | −56.7 (−85.4, −27.9)* | −28.6 (−57.5, 0.198) |
| Urine volume (mL/day) | |||||
| Baseline | 2895.8 ± 1011.5 | 2881.3 ± 1004.2 | 2701.9 ± 592.4 | 3121.1 ± 1138.6 | 3372.1 ± 1413.1 |
| Day 1 | 2702.6 ± 1341.8 | 3148.1 ± 718.5 | 3284.5 ± 653.4 | 3511.4 ± 522.9 | 3939.8 ± 1386.0 |
| Day 7 | 2762.3 ± 1171.4 | 3053.3 ± 1067.7 | 2421.0 ± 795.6 | 3048.5 ± 868.2 | 3471.4 ± 1204.5 |
| LS mean difference at Day 1a | – | 456.1 (−212.4, 1124.7) | 723.8 (76.7, 1370.9)* | 643.8 (−3.8, 1291.3) | 888.4 (235, 1541.8)* |
| LS mean difference at Day 7a | – | 303.5 (−208.4, 815.3) | −174.9 (−670.3, 320.5) | 92.9 (−402.9, 588.6) | 300.4 (−199.9, 800.6) |
| Water intake (mL/day) | |||||
| Baseline | 2754.9 ± 1039.9 | 2630.9 ± 1044.0 | 2578.1 ± 602.5 | 3196.5 ± 1175.2 | 3311.3 ± 1429.3 |
| Day 1 | 2686.0 ± 1513.1 | 2694.4 ± 936.4 | 3023.8 ± 883.4 | 2964.0 ± 940.1 | 3256.8 ± 1581.7 |
| Day 7 | 2618.5 ± 1447.3 | 2686.4 ± 929.1 | 2400.4 ± 583.5 | 3049.1 ± 856.6 | 3141.0 ± 1387.3 |
| LS mean difference at Day 1a | – | 131.8 (−455.8, 719.3) | 513.6 (−54.5, 1081.7) | −161.3 (−733.9, 411.4) | 17.3 (−558.5, 593.1) |
| LS mean difference at Day 7a | – | 175.8 (−407.1, 758.7) | −64.4 (−628, 499.2) | 46.5 (−521.6, 614.6) | 38.5 (−532.7, 609.8) |
| Body weight (24 h after dose) (kg) | |||||
| Baseline | 75.96 ± 9.70 | 67.71 ± 14.40 | 72.13 ± 18.57 | 68.00 ± 7.90 | 71.80 ± 9.59 |
| Day 1 | 75.80 ± 9.63 | 67.49 ± 14.32 | 71.71 ± 18.26 | 67.43 ± 7.73 | 70.96 ± 9.34 |
| Day 7 | 75.28 ± 9.61 | 66.76 ± 14.29 | 71.01 ± 18.10 | 66.70 ± 7.84 | 70.24 ± 9.09 |
| LS mean difference at Day 1a | – | −0.19 (−0.58, 0.20) | −0.31 (−0.68, 0.07) | −0.53 (−0.91, −0.15)* | −0.74 (−1.11, −0.36)* |
| LS mean difference at Day 7a | – | −0.45 (−1.14, 0.24) | −0.51 (−1.17, 0.14) | −0.79 (−1.46, −0.12)* | −0.97 (−1.62, −0.31)* |
Values are presented as the mean ± standard deviation or LS mean (95% confidence interval)
AUC area under the plasma concentration–time curve, C max maximum plasma concentration, FPG fasting plasma glucose, LS least-squares, MPG 0–16h, mean plasma glucose from 0 to 16 h, UGE urinary glucose excretion
* P < 0.05
aData represent the LS mean difference (95% confidence interval) between each luseogliflozin group and placebo. The time-matched baseline on Day −1 was used as a covariate
Fig. 2.
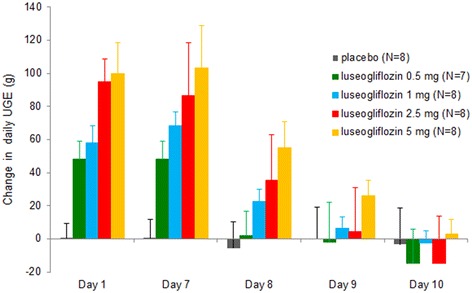
Changes in daily urinary glucose excretion from baseline (Day −1) to Day 10. All four doses of luseogliflozin significantly increased UGE compared with placebo. Although UGE decreased in all four luseogliflozin groups after the last dose on Day 7, the UGE remained significantly greater in the 1 and 2.5 mg luseogliflozin groups (P < 0.05 vs placebo) up to Day 8, and in the 5 mg luseogliflozin group up to Day 9. Values are presented as the mean ± standard deviation. UGE urinary glucose excretion
The UGE rate was significantly greater in all four luseogliflozin groups than in the placebo group at all times on Days 1 and 7 (Fig. 3), reaching a peak at 2–4 h after each meal.
Fig. 3.
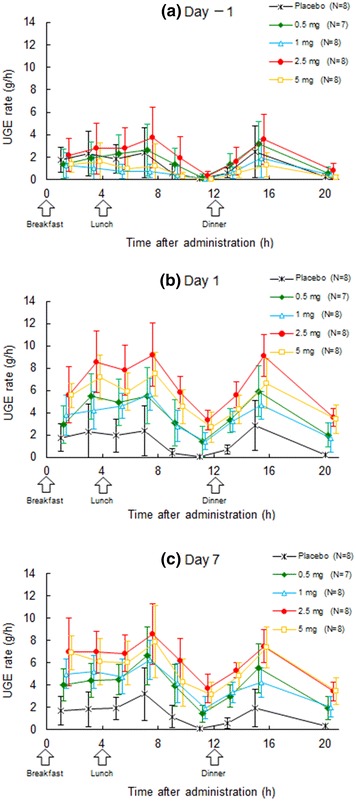
Urinary glucose excretion rate–time profiles on Day −1 (a), Day 1 (b), and Day 7 (c). The UGE rate was significantly greater in all four luseogliflozin groups than in the placebo group at all times on Days 1 and 7, reaching a peak at 2–4 h after each meal. Values are presented as the mean ± standard deviation. UGE urinary glucose excretion
The plasma glucose concentration–time profiles on Days −1, 1, and 7 are shown in Fig. 4. Plasma glucose concentrations decreased from Day −1 to Days 1 and 7 in all four luseogliflozin groups. Reductions in FPG (i.e., PG at 24 h after administration) were observed for 2.5 mg and 5 mg luseogliflozin on Day 1, and for all doses on Day 7 compared with placebo. The C max and AUC for postprandial plasma glucose at 4 h after each meal decreased in all four luseogliflozin groups, and the decreases were significant in the 2.5 mg and 5 mg luseogliflozin groups compared with placebo. MPG decreased significantly in all four luseogliflozin groups compared with placebo.
Fig. 4.
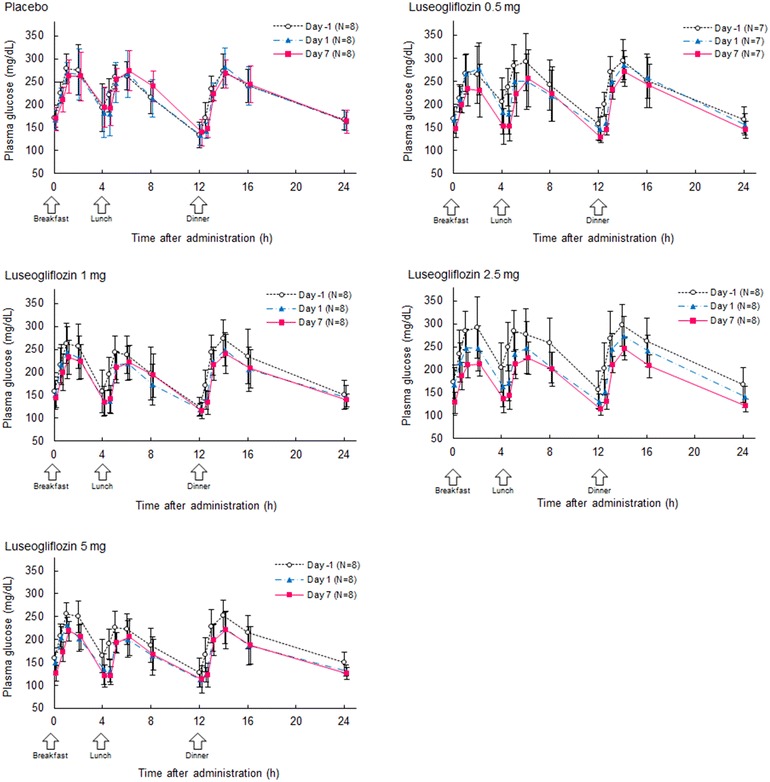
Plasma glucose concentration–time profiles at each dose of luseogliflozin on Days −1, 1, and 7. The plasma glucose concentrations decreased from baseline (Day −1) to Days 1 and 7 in all four luseogliflozin groups. Values are presented as the mean ± standard deviation
The serum insulin concentrations tended to decrease in all four luseogliflozin groups. The AUC0–4h for insulin on Day 7 was significantly lower in the 0.5, 1, and 2.5 mg luseogliflozin groups than in the placebo group.
Figure 5 shows the relationship between the change in UGE from Day −1 and the change in plasma glucose AUC on Day 1. As shown in this figure, the decrement in plasma glucose AUC increased with increasing UGE.
Fig. 5.
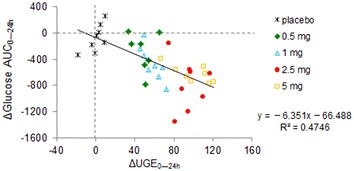
Relationship between the changes in the area under the concentration–time curve for plasma glucose and the changes in urinary glucose excretion from baseline (Day −1) to Day 7. The decrement in plasma glucose AUC increased with increasing UGE. ΔAUC 0–24h change from baseline to Day 7 in the area under the concentration–time curve from 0 to 24 h, ΔUGE 0–24h change from baseline to Day 7 in urinary glucose excretion from 0 to 24 h
Regression analysis with the E max model was used to examine the relationship between the plasma luseogliflozin concentration and the change in UGE in each subject. The estimated values of E max, EC50, and γ were 119 g/day, 254 ng h/mL, and 0.931, respectively (Fig. 6).
Fig. 6.
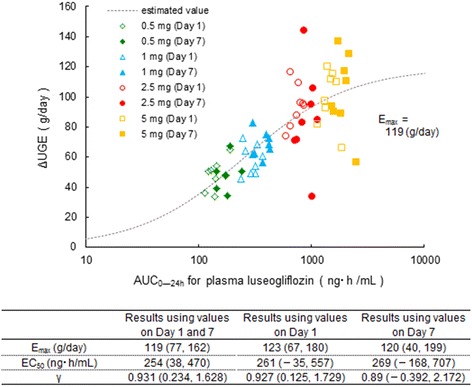
Regression analysis with the E max model was used to examine the relationship between the plasma luseogliflozin concentration and the change in UGE in each subject. The values are presented as the estimates (95% confidence interval). E max maximum change in urinary glucose excretion, EC 50 area under the concentration–time curve at 50% of the urinary glucose excretion, γ Hill coefficient, UGE urinary glucose excretion
Safety
Forty patients were included in the safety assessments. Nine AEs occurred in seven patients (Table 4). One adverse drug reaction (constipation) occurred in one patient in the 0.5 mg luseogliflozin group. All of the events were mild in severity. There were no serious AEs or AEs leading to discontinuation. There were no episodes of hypoglycemia or urinary tract/genital infection reported. The changes in clinical laboratory tests and vital signs on Days 1 and 7 are shown in Table 5. Regarding serum and urine electrolytes on Day 1, serum phosphorus increased and urinary phosphorus decreased, although these changes were not much greater on Day 7 compared with placebo. Similar patterns were observed in urinary sodium, urinary potassium, and urinary chloride (data not shown). No apparent changes were observed in other electrolytes (data not shown). There were no clinically significant changes in renal function-related markers (creatinine, blood urea nitrogen, plasma/urinary uric acid, cystatin C, urinary N-acetyl-β-(d)-glucosaminidase, urinary type IV collagen, urinary β2-microglobulin, urinary albumin) or a hypovolemia-related marker (hematocrit) (Table 5). There were no clinically significant changes in vital signs or electrocardiography. Although urine volume increased slightly on Day 1, it was not markedly different between Days −1 and 7. Fluid intake did not change markedly, except for an increase in the 1 mg luseogliflozin group on Day 1. Body weight decreased slightly from Day −1 onwards.
Table 4.
Summary of adverse events
| Placebo (N = 8) | Luseogliflozin | ||||
|---|---|---|---|---|---|
| 0.5 mg (N = 8) | 1 mg (N = 8) | 2.5 mg (N = 8) | 5 mg (N = 8) | ||
| Any adverse event, n | 0 | 3 | 1 | 1 | 2 |
| Any related event, n | 0 | 1 | 0 | 0 | 0 |
| Constipation | 0 | 1 | 0 | 0 | 0 |
| Diarrhea | 0 | 1 | 0 | 0 | 0 |
| Dermatitis contact | 0 | 0 | 1 | 0 | 0 |
| Pruritus | 0 | 1 | 0 | 0 | 0 |
| Headache | 0 | 1 | 0 | 0 | 1 |
| Blood urine present | 0 | 0 | 0 | 0 | 1 |
| ALT increased | 0 | 0 | 0 | 1 | 0 |
| γ-GTP increased | 0 | 0 | 0 | 1 | 0 |
Values are presented as the number of subjects
ALT alanine aminotransferase, γ-GTP gamma-glutamyltransferase
Table 5.
Changes in clinical/laboratory variables after single (Day 1) and multiple (Day 7) doses of luseogliflozin compared with placebo
| Placebo (N = 8) | Luseogliflozin | ||||
|---|---|---|---|---|---|
| 0.5 mg (N = 7) | 1 mg (N = 8) | 2.5 mg (N = 8) | 5 mg (N = 8) | ||
| Urinary uric acid (g/day) | |||||
| Baseline | 0.75 ± 0.12 | 0.65 ± 0.08 | 0.64 ± 0.11 | 0.78 ± 0.09 | 0.70 ± 0.13 |
| Change from baseline to Day 1 | −0.04 ± 0.05 | 0.04 ± 0.05 | 0.08 ± 0.07 | −0.01 ± 0.04 | 0.08 ± 0.12 |
| Change from baseline to Day 7 | −0.03 ± 0.07 | −0.01 ± 0.07 | −0.03 ± 0.20 | −0.06 ± 0.07 | 0.01 ± 0.10 |
| Cystatin C (mg/L) | |||||
| Baseline | 0.804 ± 0.111 | 0.944 ± 0.174 | 0.906 ± 0.109 | 0.880 ± 0.138 | 0.925 ± 0.139 |
| Change from baseline to Day 1 | −0.035 ± 0.042 | −0.040 ± 0.018 | 0.005 ± 0.077 | 0.016 ± 0.060 | 0.028 ± 0.042 |
| Change from baseline to Day 7 | −0.060 ± 0.050 | −0.067 ± 0.029 | −0.061 ± 0.043 | −0.064 ± 0.054 | −0.027 ± 0.065 |
| Urinary NAG (U/L) | |||||
| Baseline | 2.80 ± 1.27 | 2.19 ± 1.05 | 2.38 ± 1.88 | 2.58 ± 1.99 | 2.70 ± 1.78 |
| Change from baseline to Day 1 | 0.43 ± 0.68 | −0.31 ± 0.67 | −0.33 ± 0.99 | −0.68 ± 1.33 | −0.81 ± 1.01 |
| Change from baseline to Day 7 | 0.26 ± 0.81 | −0.06 ± 0.80 | 0.73 ± 0.80 | −0.08 ± 1.26 | −0.11 ± 1.18 |
| Urinary β2-microglobulin (μg/L) | |||||
| Baseline | 65.5 ± 32.2 | 76.0 ± 117.3 | 44.3 ± 38.6 | 77.3 ± 45.2 | 30.5 ± 15.4 |
| Change from baseline to Day 1 | 11.9 ± 25.7 | −12.4 ± 25.2 | −8.5 ± 31.3 | −11.0 ± 44.9 | −1.3 ± 13.5 |
| Change from baseline to Day 7 | 4.1 ± 36.6 | −7.4 ± 27.1 | 17.3 ± 54.9 | 5.5 ± 44.0 | 1.4 ± 20.3 |
| Serum calcium (mg/dL) | |||||
| Baseline | 9.16 ± 0.30 | 9.45 ± 0.37 | 9.09 ± 0.35 | 9.19 ± 0.34 | 9.29 ± 0.16 |
| Change from baseline to Day 1 | −0.19 ± 0.27 | −0.19 ± 0.12 | −0.19 ± 0.16 | −0.15 ± 0.23 | −0.10 ± 0.20 |
| Change from baseline to Day 7 | −0.15 ± 0.33 | −0.24 ± 0.05 | −0.41 ± 0.14 | −0.40 ± 0.27 | −0.16 ± 0.45 |
| Urinary calcium (g/day) | |||||
| Baseline | 0.13 ± 0.05 | 0.10 ± 0.05 | 0.13 ± 0.05 | 0.11 ± 0.08 | 0.13 ± 0.05 |
| Change from baseline to Day 1 | 0.01 ± 0.04 | 0.01 ± 0.04 | 0.00 ± 0.00 | −0.01 ± 0.04 | −0.01 ± 0.04 |
| Change from baseline to Day 7 | 0.03 ± 0.07 | 0.01 ± 0.04 | 0.00 ± 0.00 | 0.00 ± 0.05 | −0.03 ± 0.05 |
| Serum phosphorus (mg/dL) | |||||
| Baseline | 3.16 ± 0.38 | 3.38 ± 0.44 | 3.06 ± 0.32 | 3.13 ± 0.24 | 3.59 ± 0.36 |
| Change from baseline to Day 1 | 0.00 ± 0.05 | 0.30 ± 0.40 | 0.57 ± 0.32 | 0.68 ± 0.23 | 1.08 ± 0.37 |
| Change from baseline to Day 7 | 0.11 ± 0.15 | 0.16 ± 0.40 | 0.20 ± 0.21 | 0.38 ± 0.29 | 0.42 ± 0.39 |
| Urinary phosphorus (g/day) | |||||
| Baseline | 0.78 ± 0.13 | 0.78 ± 0.20 | 0.69 ± 0.16 | 0.81 ± 0.11 | 0.78 ± 0.18 |
| Change from baseline to Day 1 | −0.08 ± 0.07 | −0.13 ± 0.10 | −0.13 ± 0.10 | −0.24 ± 0.07 | −0.24 ± 0.11 |
| Change from baseline to Day 7 | −0.05 ± 0.13 | −0.04 ± 0.13 | 0.00 ± 0.13 | −0.03 ± 0.17 | −0.01 ± 0.14 |
| Urinary type IV collagen (μg/g creatinine) | |||||
| Baseline | 3.74 ± 1.46 | 3.39 ± 2.95 | 3.31 ± 1.55 | 4.03 ± 1.95 | 3.18 ± 0.95 |
| Change from baseline to Day 1 | 0.36 ± 0.53 | −0.40 ± 1.08 | −0.44 ± 0.61 | −0.05 ± 1.13 | 0.11 ± 0.97 |
| Change from baseline to Day 7 | −0.26 ± 0.99 | −0.21 ± 1.25 | 0.66 ± 1.22 | 0.21 ± 1.85 | 0.31 ± 1.26 |
| Hematocrit (%) | |||||
| Baseline | 40.26 ± 3.10 | 42.11 ± 3.99 | 42.60 ± 3.63 | 41.15 ± 3.32 | 41.95 ± 3.93 |
| Change from baseline to Day 1 | −1.57 ± 1.19 | −1.14 ± 0.73 | −1.26 ± 0.86 | −0.58 ± 1.48 | −0.54 ± 0.85 |
| Change from baseline to Day 7 | −3.06 ± 0.44 | −2.20 ± 0.95 | −2.68 ± 0.89 | −2.89 ± 1.81 | −1.66 ± 1.99 |
| SBP (mmHg) | |||||
| Baseline | 133.8 ± 20.9 | 124.3 ± 12.4 | 123.3 ± 15.9 | 123.0 ± 17.4 | 120.0 ± 18.6 |
| Change from baseline to Day 1 | 4.5 ± 5.1 | −1.7 ± 6.0 | 3.5 ± 9.6 | −5.6 ± 9.5 | −1.3 ± 12.5 |
| Change from baseline to Day 7 | −1.4 ± 7.2 | −5.9 ± 3.8 | −2.4 ± 12.8 | −8.8 ± 10.9 | −11.3 ± 11.8 |
| DBP (mmHg) | |||||
| Baseline | 84.6 ± 11.4 | 76.6 ± 8.7 | 80.1 ± 8.7 | 82.0 ± 11.3 | 79.6 ± 9.0 |
| Change from baseline to Day 1 | 3.1 ± 6.1 | 3.0 ± 5.2 | 0.4 ± 4.9 | −4.3 ± 5.6 | 0.6 ± 6.0 |
| Change from baseline to Day 7 | 0.4 ± 3.9 | 3.1 ± 3.8 | −0.8 ± 6.6 | −6.1 ± 5.6 | −3.1 ± 6.0 |
Values are presented as the mean ± standard deviation
NAG N-acetyl-β-(d)-glucosaminidase, SBP systolic blood pressure, DBP diastolic blood pressure
Discussion
Once-daily administration of 0.5, 1, 2.5, or 5 mg luseogliflozin for 7 days increased UGE in a dose-dependent manner and reduced both FPG and postprandial plasma glucose in Japanese patients with T2DM. These effects of luseogliflozin were sustained throughout the day with once-daily administration before breakfast.
Once-daily luseogliflozin rapidly and significantly increased UGE compared with placebo. These effects were apparent after the first dose and were sustained throughout the day. UGE increased dose dependently, and the mean daily UGE after 7 days of multiple doses of 5 mg was 101 g, which is approximately 85% of the maximal UGE value (119 g) estimated using the E max model. Therefore, the effects of luseogliflozin on UGE were nearly maximal at 5 mg luseogliflozin and no further increases in UGE are expected at doses exceeding 5 mg, providing rationale for the doses used in the Phase II [9, 10] and Phase III [11] clinical trials. In addition, the UGE for 2.5 and 5 mg luseogliflozin was similar to the maximal UGE (85–100 g) reported for other SGLT2 inhibitors, including dapagliflozin, canagliflozin, empagliflozin, and ipragliflozin, in patients with T2DM [14–17].
In this study, we observed that the UGE rate tended to increase after each meal. Because of the postprandial increase in plasma glucose level, greater concentrations of glucose are filtered through the renal glomerulus, which may cause an increase in UGE during the inhibition of SGLT2. Furthermore, after administering luseogliflozin OD for 7 days, the mean UGE in the 5 mg luseogliflozin group was 101 g/day, which is greater than that reported in healthy subjects on luseogliflozin (58.0 g/day) [8]. The increased UGE rate might also be caused by the higher plasma glucose concentrations in patients with T2DM than in healthy subjects. As would be expected, UGE returned toward the baseline value in each group within 1–3 days after treatment discontinuation, consistent with the elimination of the last dose of luseogliflozin. These data highlight the need for continued once-daily dosing to maintain the pharmacokinetic and pharmacodynamic profile of luseogliflozin.
In association with the increase in UGE, plasma glucose decreased immediately after the first dose. On Day 7 of luseogliflozin treatment, plasma glucose AUC and C max decreased after dinner as did MPG and FPG. These results indicate that once-daily administration of luseogliflozin before breakfast improved FPG and postprandial glucose in patients with T2DM. Further, these glucose-lowering effects were sustained throughout the day.
A correlation between the increment of UGE and the decrement of plasma glucose was observed in this study. Therefore, the glycemic-lowering effect of luseogliflozin in patients with T2DM was considered to depend on the amount of UGE. In addition, because UGE seemed to depend on the baseline glucose concentrations, the glucose-lowering effect of this agent appeared to be dependent on the baseline plasma glucose levels.
The present study also revealed that luseogliflozin increased UGE and decreased plasma glucose concentrations without increasing insulin concentrations, as expected from its mechanism of action. The results suggest the potential of luseogliflozin in improving glycemic control, without increasing the burden on pancreatic β cell function. Phase II and Phase III studies of 12- to 24-week duration confirmed that the reductions in plasma glucose concentrations after 7 days of dosing are maintained for up to 24 weeks in patients with T2DM [9–11].
The pharmacokinetic results for luseogliflozin and M2 in this study of patients with T2DM are similar to those observed in healthy males [8]. On Day 7, the C max and AUC of luseogliflozin and M2 showed dose dependency of the agents, and exposure to M2 at a molar ratio to luseogliflozin was low. Luseogliflozin was rapidly absorbed with a t max of about 1 h, and the t 1/2 was about 10 h at all doses. The pharmacokinetic profile of luseogliflozin observed in this study supports its once-daily dosing regimen, as used in the Phase II and Phase III clinical trials [9–11].
Luseogliflozin was well tolerated in this 7-day multiple-dose study in patients with T2DM with a low incidence of AEs. In longer clinical trials, luseogliflozin was also associated with a low incidence of AEs, with most AEs being rated as mild in severity [9–11]. Furthermore, the safety profile of luseogliflozin does not appear to be related to its dose.
Like other SGLT2 inhibitors [1], luseogliflozin acts in an insulin-independent manner and is expected to carry a low risk of hypoglycemia. Although luseogliflozin decreased FPG, none of the patients had extremely low glucose concentrations of <70 mg/dL or experienced hypoglycemic events. The incidence of hypoglycemia was also very low in the Phase II and III studies, occurring in 1.9% (1/54) of patients treated with 5 mg luseogliflozin [10], in 1.7% (1/60) of patients treated with 0.5 mg luseogliflozin [9], and in 1.3% (1/79) of patients treated with 2.5 mg luseogliflozin [11], but not in the other dose groups.
It is possible that enhanced UGE affects the electrolyte balance in relation to change in water loss. Although changes in urinary electrolytes (sodium, potassium, chloride, phosphorus) and serum phosphorus were observed on Day 1 in the present study, these changes were not considered clinically meaningful. The mechanism of action of SGLT2 inhibitors has also raised concern over the risk of urinary tract/genital infections and changes in renal function [18, 19]. In the present study, there were no findings indicative of urinary tract/genital infections, nor were there any signs of worsening of renal function during the 7 days of treatment. In the Phase III study, the incidences of AEs related to genital infection and renal function were similar between the 2.5 mg luseogliflozin group and the placebo group [1.3% (1/79) versus 1.3% (1/79), respectively, for genital infection, and 7.6% (6/79) versus 7.6% (6/79), respectively, for renal function]. Likewise, there were no significant deteriorations in markers for renal function, such as serum creatinine, in the 2.5 mg luseogliflozin group compared with placebo [11]. Nevertheless, additional long-term, large-scale studies may be needed to verify the safety of luseogliflozin, especially in terms of long-term changes in renal function.
The increase in UGE in the 5 mg luseogliflozin group corresponded to about 100 g glucose/day, which is equivalent to an energy loss of approximately 400 kcal. There was a slight increase in urine volume on Day 1, which may be related to osmotic diuresis caused by UGE. These calorie loss and increased urine volume observations may be associated with a reduction in body weight during longer term administration. In fact, a small reduction in body weight was observed on Day 7, which is probably related to a decrease in fluid volume. Over 24 weeks of treatment, 2.5 mg luseogliflozin was associated with a body weight change of −2.70 versus −0.93 kg for placebo (P < 0.05), which probably reflects an increase in energy loss and a change in fluid volume. The increase in urine output may also increase the risk of hypovolemia or pollakiuria. Although neither was observed in the present study, pollakiuria occurred in 2.5% (2/79) and 1.3% (1/79) of patients treated with 2.5 mg luseogliflozin and placebo, respectively, in the Phase III study, but no episodes of volume depletion were observed [11].
Conclusion
In this study, administration of 0.5–5 mg luseogliflozin increased UGE in a dose-dependent manner, decreased plasma glucose, and was well tolerated in Japanese patients with T2DM. The pharmacokinetic and pharmacodynamic profile of luseogliflozin observed in this study supports its once-daily dosing regimen, as used in recently published clinical trials [9–11].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
Sponsorship for the clinical trial described in this study and article processing charges were funded by Taisho Pharmaceutical Co., Ltd. Editorial assistance was provided by Nicholas D. Smith, PhD and Keyra Martinez Dunn, PhD of Edanz Group Ltd. and funded by Taisho Pharmaceutical Co., Ltd. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. The authors wish to thank the participants as well as the investigators and the clinic staff for helping to perform the study.
Conflict of interest
Takashi Sasaki has received joint research funds from Canon Inc. and Taisho Toyama Pharmaceutical Co., Ltd., and consulting fees or lecture fees from Taisho Pharmaceutical Co., Ltd., Taisho Toyama, Sanofi, Kowa, Mitsubishi-Tanabe, Novo Nordisk Pharma, MSD, and the LIGHT Study group (LIGHT Study; UMIN ID 000015112). Yutaka Seino has received consulting fees or lecture fees from Sanofi, Novo Nordisk, Eli Lilly, GlaxoSmithKline, Astellas, Takeda, Boehringer Ingelheim, Johnson & Johnson, Becton–Dickinson, AstraZeneca, Taisho Toyama and Taisho. Atsushi Fukatsu has received consulting fees or lecture fees from Taisho Toyama and Taisho. Michito Ubukata, Soichi Sakai, and Yoshishige Samukawa are employees of Taisho Pharmaceutical Co., Ltd.
Compliance with ethics guidelines
All procedures were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national), the Helsinki Declaration of 1964, as revised in 2000 and 2008, the Japanese Pharmaceutical Affairs Law and Good Clinical Practice. The study protocol was approved by the Institutional Review Board of P-One Clinic, Keikokai Medical Corporation. Informed consent was obtained from all patients for being included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Footnotes
Trial registration: Japan Pharmaceutical Information Center; Identifier: JapicCTI-090909.
References
- 1.Ghosh RK, Ghosh SM, Chawla S, Jasdanwala SA. SGLT2 inhibitors: a new emerging therapeutic class in the treatment of type 2 diabetes mellitus. J Clin Pharmacol. 2012;52(4):457–463. doi: 10.1177/0091270011400604. [DOI] [PubMed] [Google Scholar]
- 2.Harada N, Inagaki N. Role of sodium-glucose transporters in glucose uptake of the intestine and kidney. J Diabetes Investig. 2012;3(4):352–353. doi: 10.1111/j.2040-1124.2012.00227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bays H. Sodium glucose co-transporter type 2 (SGLT2) inhibitors: targeting the kidney to improve glycemic control in diabetes mellitus. Diabetes Ther. 2013;4(2):195–220. doi: 10.1007/s13300-013-0042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurosaki E, Ogasawara H. Ipragliflozin and other sodium-glucose cotransporter-2 (SGLT2) inhibitors in the treatment of type 2 diabetes: preclinical and clinical data. Pharmacol Ther. 2013;139(1):51–59. doi: 10.1016/j.pharmthera.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Tahrani AA, Barnett AH, Bailey CJ. SGLT inhibitors in management of diabetes. Lancet Diabetes Endocrinol. 2013;1(2):140–151. doi: 10.1016/S2213-8587(13)70050-0. [DOI] [PubMed] [Google Scholar]
- 6.Kakinuma H, Oi T, Hashimoto-Tsuchiya Y, et al. (1S)-1,5-anhydro-1-[5-(4-ethoxybenzyl)-2-methoxy-4-methylphenyl]-1-thio-d-glucitol (TS-071) is a potent, selective sodium-dependent glucose cotransporter 2 (SGLT2) inhibitor for type 2 diabetes treatment. J Med Chem. 2010;53(8):3247–3261. doi: 10.1021/jm901893x. [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto K, Uchida S, Kitano K, et al. TS-071 is a novel, potent and selective renal sodium-glucose cotransporter 2 (SGLT2) inhibitor with anti-hyperglycaemic activity. Br J Pharmacol. 2011;164(1):181–191. doi: 10.1111/j.1476-5381.2011.01340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sasaki T, Seino Y, Fukatsu A, Sakai S, Samukawa Y. Safety, pharmacokinetics, and pharmacodynamics of single and multiple luseogliflozin dosing in healthy Japanese males: a randomized, single-blind, placebo-controlled trial. Adv Ther. 2014;31(3):345–361. doi: 10.1007/s12325-014-0102-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seino Y, Sasaki T, Fukatsu A, Sakai S, Samukawa Y. Efficacy and safety of luseogliflozin monotherapy in Japanese patients with type 2 diabetes mellitus: a 12-week, randomized, placebo-controlled, phase II study. Curr Med Res Opin. 2014;30(7):1219–1230. doi: 10.1185/03007995.2014.901943. [DOI] [PubMed] [Google Scholar]
- 10.Seino Y, Sasaki T, Fukatsu A, Ubukata M, Sakai S, Samukawa Y. Dose-finding study of luseogliflozin in Japanese patients with type 2 diabetes mellitus: a 12-week, randomized, double-blind, placebo-controlled, phase II study. Curr Med Res Opin. 2014;30(7):1231–1244. doi: 10.1185/03007995.2014.909390. [DOI] [PubMed] [Google Scholar]
- 11.Seino Y, Sasaki T, Fukatsu A, Ubukata M, Sakai S, Samukawa Y. Efficacy and safety of luseogliflozin as monotherapy in Japanese patients with type 2 diabetes mellitus: a randomized, double-blind, placebo-controlled, phase 3 study. Curr Med Res Opin. 2014;30(7):1245–1255. doi: 10.1185/03007995.2014.912983. [DOI] [PubMed] [Google Scholar]
- 12.Markham A, Elkinson S. Luseogliflozin: first global approval. Drugs. 2014;74(8):945–950. doi: 10.1007/s40265-014-0230-8. [DOI] [PubMed] [Google Scholar]
- 13.Kuzuya T, Nakagawa S, Satoh J, et al. Committee of the Japan Diabetes Society on the diagnostic criteria of diabetes mellitus. Report of the Committee on the classification and diagnostic criteria of diabetes mellitus. Diabetes Res Clin Pract. 2002;55(1):65–85. doi: 10.1016/S0168-8227(01)00365-5. [DOI] [PubMed] [Google Scholar]
- 14.Devineni D, Curtin CR, Polidori D, et al. Pharmacokinetics and pharmacodynamics of canagliflozin, a sodium glucose co-transporter 2 inhibitor, in subjects with type 2 diabetes mellitus. J Clin Pharmacol. 2013;53(6):601–610. doi: 10.1002/jcph.88. [DOI] [PubMed] [Google Scholar]
- 15.Heise T, Seman L, Macha S, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of multiple rising doses of empagliflozin in patients with type 2 diabetes mellitus. Diabetes Ther. 2013;4(2):331–345. doi: 10.1007/s13300-013-0030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.List JF, Woo V, Morales E, Tang W, Fiedorek FT. Sodium-glucose cotransport inhibition with dapagliflozin in type 2 diabetes. Diabetes Care. 2009;32(4):650–657. doi: 10.2337/dc08-1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwartz SL, Akinlade B, Klasen S, Kowalski D, Zhang W, Wilpshaar W. Safety, pharmacokinetic, and pharmacodynamic profiles of ipragliflozin (ASP1941), a novel and selective inhibitor of sodium-dependent glucose co-transporter 2, in patients with type 2 diabetes mellitus. Diabetes Technol Ther. 2011;13(12):1219–1227. doi: 10.1089/dia.2011.0012. [DOI] [PubMed] [Google Scholar]
- 18.Abdul-Ghani MA, Norton L, DeFronzo RA. Efficacy and safety of SGLT2 inhibitors in the treatment of type 2 diabetes mellitus. Curr Diabetes Rep. 2012;12(3):230–238. doi: 10.1007/s11892-012-0275-6. [DOI] [PubMed] [Google Scholar]
- 19.Komala MG, Panchapakesan U, Pollock C, Mather A. Sodium glucose cotransporter 2 and the diabetic kidney. Curr Opin Nephrol Hypertens. 2013;22(1):113–119. doi: 10.1097/MNH.0b013e32835a17ae. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


