Abstract
Introduction
Non-communicable diseases (NCDs) such as metabolic, cardiovascular, cancers, injuries and mental health disorders are increasingly contributing to the disease burden in South Asia, in light of demographic and epidemiologic transitions in the region. Home to one-quarter of the world's population, the region is also an important priority area for meeting global health targets. In this review, we describe the current burden of and trends in four common NCDs (cardiovascular disease, diabetes, cancer and chronic obstructive pulmonary disease) in South Asia.
Sources of data
The 2010 Global Burden of Disease Study supplemented with the peer-reviewed literature and reports by international agencies and national governments.
Areas of agreement
The burden of NCDs in South Asia is rising at a rate that exceeds global increases in these conditions. Shifts in leading risk factors—particularly dietary habits, tobacco use and high blood pressure—are thought to underlie the mounting burden of death and disability due to NCDs. Improvements in life expectancy, increasing socioeconomic development and urbanization in South Asia are expected to lead to further escalation of NCDs.
Areas of controversy
Although NCD burdens are currently largest among affluent groups in South Asia, many adverse risk factors are concentrated among the poor, portending a future increase in disease burden among lower income individuals.
Growing points
There continues to be a notable lack of national surveillance data to document the distribution and trends in NCDs in the region. Similarly, economic studies and policy initiatives addressing NCD burdens are still in their infancy.
Areas timely for developing research
Opportunities for innovative structural and behavioral interventions that promote maintenance of healthy lifestyles—such as moderate caloric intake, adequate physical activity and avoidance of tobacco—in the context of socioeconomic development are abundant. Testing of health care infrastructure and systems that best provide low-cost and effective detection and treatment of NCDs is a priority for policy researchers.
Keywords: non-communicable disease, South Asia, cardiovascular diseases, cancers, diabetes, chronic obstructive pulmonary disease
Introduction
Globally, the burden of non-communicable diseases (NCDs)—chronic metabolic, heart, cancerous and psychological illnesses, and injuries that are not transmittable by contact—is rising. Between 1990 and 2010, deaths from NCDs rose by nearly 8 million, and these conditions now account for two of every three deaths (34.5 million) per year worldwide.1 In 2010, 8 million people died from cancer—38% more than in 1990. Coronary heart disease (CHD) and stroke together accounted for one in four deaths in 2010, compared with one in five deaths in 1990, and resulted in 12.9 million deaths globally in 2010. In 2010, 1.3 million deaths were due to diabetes, twice as many as in 1990.
South Asia (Fig. 1) is the most densely populated region. As home to one-quarter of the world's population, South Asia is a high-priority region for many public health concerns.2 The region is also in the midst of an epidemiological transition. Since the 1970s, South Asia has experienced significant reductions in premature death and disability from communicable and nutritional diseases such as pneumonia, diarrheal diseases and malnutrition.2 Still, infectious disease, maternal health and nutritional deficiencies remain prevalent and contribute to disease burdens. Meanwhile, NCDs have been emerging as leading causes of death as individuals are living longer and as globalization and urbanization are exposing individuals to concentrated risk factors.2 NCDs account for sizeable proportions (from one third to two thirds) of all death and disability in the region,2 casting increasing attention upon NCDs among public health researchers and practitioners. In considering the context of these NCD challenges and responses, it should be noted that the region consists of a wide variety of countries at varying stages of economic development, about half of each country's population lives below the poverty line (earning <US$2 per day), and access to health care is generally limited.3
Fig. 1.

Countries in South Asia. Source: The World Bank.
Objectives and methods
In this review, we describe burdens and recent trends in NCDs in South Asia. Although NCDs are a broad and diverse group of conditions, we focus on four major diseases: cardiovascular diseases (CVDs), diabetes, selected cancers and chronic obstructive pulmonary disease (COPD). These four disease groups are linked by common risk factors: dietary patterns, physical inactivity, tobacco use and harmful use of alcohol.4 Mounting evidence suggests that environmental pollution is another common risk factor for COPD5 and CVD,6 and possibly diabetes.7,8
For each of the diseases described, we report (1) prevalence/incidence, (2) morbidity and mortality and (3) economic costs. ‘Prevalence’ is defined as the proportion of a population found to have a condition or risk factor, expressed as a percentage. Related to prevalence is ‘cumulative incidence’, the number of new cases within a specified time period divided by the size of the population initially at risk. We also report ‘morbidity’ as disability-adjusted life years (DALYs; the sum of years lost due to premature death and years lived with disability due to a disease or risk factor),2 and ‘mortality’, the number or proportion of deaths (usually premature) due to a disease or risk factor. ‘Direct costs’ (due to medical care costs, treatments or specified interventions) and ‘indirect costs’ (the value of lost productivity from time off work or suboptimal work performance due to illness, pain or suffering), key measures of the social and economic tolls of NCDs, are also discussed where data were available.
Aligned with our focus on the descriptive epidemiology of NCDs in the region, we drew heavily on the Global Burden of Disease (GBD) Study, which aggregated all available population surveys and published literature on multiple diseases and risk factors worldwide.2 In addition, we used disease-specific databases with international coverage, including the International Diabetes Federation Diabetes Atlas9 and GLOBOCAN,10 and supplemented with studies published in the peer-reviewed literature and reports by the World Bank, World Health Organization and country governments. It is important to note that although this article covers South Asia, most of the data available come from small studies conducted in a few clinics, cities or regions in India or on Indian populations, rather than from nationally representative surveillance studies of each of South Asia's countries. These subnational studies represent heterogeneous populations with differing access to health care, cultural practices, ethnic background and distributions of underlying risk factors. As such, findings should be interpreted with appropriate caution.
Cardiovascular diseases
CVD burdens are large and growing in South Asia. CHD and stroke are on the rise, while long-established diseases like rheumatic or hypertensive heart disease are declining.3 In South Asian countries, the age of onset of first myocardial infarction is, on average, 10 years earlier compared with other countries, and this is largely attributed to higher prevalence of CVD risk factors at younger ages.11 Two major case–control studies on first acute myocardial infarction and stroke in countries throughout Africa, Asia, Australia, Europe, the Middle East and North and South America—Interheart and Interstroke—found that more than 86% of CVD was attributable to nine key risk factors [smoking, lipids, hypertension, diabetes, obesity (including abdominal adiposity), diet, physical activity, alcohol consumption and psychosocial factors].12,13 In this section, we focus on CHD and stroke.
Prevalence/incidence
Most of the data on CVD in South Asia came from regional studies within India that use varying data collection methods; there is a particular lack of data from Pakistan, Nepal and Sri Lanka.14 In 2003, the prevalence of CHD in India was estimated to be 3–4% in rural areas and 8–10% in urban areas among adults older than 20 years (∼29.8 million individuals), representing a 2-fold rise in rural areas and a 6-fold rise in urban areas over four decades.15 The estimated annual incidence of stroke in 2001 was 203 per 100 000 among individuals ages 20 years and older.16
Morbidity/mortality
Data from 2005 showed that CVD was associated with an estimated 11% of morbidity and 29% of mortality in India.17 Between 1990 and 2010, healthy years of life lost (YLL) from CHD increased dramatically by 73%.2 CHD and stroke are currently leading causes of death in India, and nearly half of these deaths occur among adults aged 30–60 years old.18
Costs
A 2010 World Bank study showed that CVD leads to catastrophic expenditure for 25% of Indian families and drives 10% of families into poverty.19 An estimated 9.2 million productive years of life were lost to CVD in India in 2000, with an expected increase to 17.9 million years in 2030; similar figures are likely for the rest of South Asia.20
Diabetes
Diabetes is a complex metabolic disorder and growing worldwide.9 Diabetes requires lifelong self-motivated care and particular attention to controlling blood sugar, blood pressure and cholesterol levels. Care can become increasingly costly over time, requiring progressively more medications to control risk factors. Longstanding or poorly controlled diabetes leads to the emergence of CVD (e.g. CHD, strokes and heart failure),21 eye diseases (e.g. cataracts, retinopathy),22 chronic kidney disease and failure,23 neurovascular limb diseases (e.g. foot ulcers and peripheral vascular disease, PVD)24 and mental health or cognitive disorders (e.g. depression, dementia).25,26 These conditions are all disabling and sometimes fatal; this was reflected in the GBD report showing that diabetes is a leading contributor to years lived with disability.1
Prevalence/incidence
Estimating diabetes prevalence is challenging. Diabetes is asymptomatic until complications set in, so blood testing is required to know one's status. Relying on self-report is limited by recall bias and/or low awareness of one's status. Another challenge is that there are several biochemical indicators for diabetes used in epidemiologic studies (e.g. fasting and non-fasted glucose levels, glycated hemoglobin and oral glucose tolerance tests), which are not perfectly congruent, so estimates from studies using different indicators and different thresholds are not comparable. Furthermore, epidemiologic studies are rarely able to obtain blood glucose measurements at two occasions, the clinical gold standard for diagnostic purposes.
Despite data limitations, South Asia is considered an epicenter of the global diabetes epidemic. According to the International Diabetes Federation's 2013 estimates, almost 80 million people or 21% of all diabetes cases worldwide live in South Asia. India, the region's most populous country, is home to more than 65 million people affected by diabetes, the second highest worldwide (after China).9 Nationally, representative country-specific data are limited in the region and prevalence estimates were previously based on small studies that used non-comparable sampling and data collection approaches. Uniformly collected data in 2011 from four states of India estimated that 6.2% of adults in India are affected by diabetes.27 Meanwhile, 2007 data from Pakistan (9.3% in males and 11.1% in females)28 and Sri Lanka (10.9%)29 also show high prevalence. Diabetes prevalence is notably two to three times higher in urban (e.g. 12–20%) compared with rural populations (5–6%) of South Asia.27,30
Because diabetes is a progressive but silent disease, undiagnosed diabetes may be common and self-reported prevalence may substantially underestimate the true burden. More importantly, lack of awareness precludes these individuals from engaging in positive lifestyle behaviors and seeking medical care.
To date, there are few prospective data from the region estimating the incidence of diabetes. One such study from Chennai in 2008 reported a cumulative diabetes incidence of 13.4% among people with normal glucose over 8 years of follow-up (rate = 20.2 per 1000 person years).31 This is noteworthy as annual diabetes incidence in the general US population is about 7.6 per 1000 persons.32 More longitudinal data are expected in the coming decade as large study platforms (e.g. PURE, CARRS) become more established.33,34
Morbidity/mortality
Most available data regarding diabetes complications in South Asia are from clinical settings. This is largely because measuring diabetes complications accurately at a population level requires complex and costly tests (e.g. retinal photographs), which are difficult to integrate into routine chronic disease surveillance. Baseline data from a large trial across 885 clinical centers showed that 22.7 and 41.8% of diabetes patients had some form of macro- (CHD, PVD) or microvascular complication (neuropathy, retinopathy), respectively.35 Data from clinics in Karachi in 2004 showed that 26.4, 6.8 and 3.9% of diabetes patients had stable CHD, previous strokes and diabetic foot, respectively.36 Similar estimates for CHD (27.2%), strokes (9.2%) and PVD or gangrene (4.2%) have also been noted at hospital follow-up in Bombay, although data come from 15 years earlier.37 Data from randomly sampled primary, secondary and tertiary care facilities in Sri Lanka in 2006 report high prevalence of neuropathy (25.2%), CHD (12.4%), retinopathy (20.0%) and nephropathy (22.8%).38 Finally, population-based data from Chennai in 2009 show high prevalence of retinopathy (17.5%), neuropathy (25.7%), nephropathy (5.1%) and microalbuminuria (26.5%).39
Costs
Several cost-of-illness studies have been conducted in clinical settings in South Asia. Reports from 2000 to 2006 show that direct medical costs accounted for the majority of diabetes-related costs and generally amounted to US$ 200 per year.40,41 This is substantial given that over half of South Asia's population lives on <US$ 2 per day (<US$ 730 per year). Furthermore, costs are rising. Total direct costs of diabetes doubled in India between 1998 and 2005,42 and estimates from 2010 show direct costs now amount to US$ 400–500 per year.43 As expected, larger proportions of household income among lower socioeconomic strata get spent on diabetes care, which precludes spending on other opportunities (e.g. education for children).
Cancers
Cancers are a major cause of morbidity and mortality globally and are increasingly prevalent in low-income countries. Based on GLOBOCAN's estimates using available regional population-based registry data, 63% of 7.6 million global cancer deaths occurred in developing countries in 2008.10 The diversity of types of cancer, carcinogenic agents and possible interventions make cancer among the most heterogeneous of the NCDs. There is some socioeconomic patterning across types of cancer in South Asia. To date, cancers related to infectious agents (e.g. cervical, stomach and liver) and tobacco use (e.g. oral and lung) tend to be more frequent than cancers associated with ‘Western’ lifestyles and longevity (e.g. prostate, colorectal and breast). However, due to changes in demography, lifestyles and income, South Asia is expected to experience a cancer transition in which cancers of infectious origin will decline and those related to ‘Western’ lifestyle will rise.44
Prevalence/incidence
Prevalence and incidence vary widely across the different types of cancers and between genders. Consistent with worldwide trends, lung cancer is the most common cancer among men in South Asia (age-standardized incidence per 100 000 in 2008 ranging from 10.9 in India to 30.4 in Bangladesh) according to GLOBOCAN data.10 Cervical cancer is the most frequent cancer among women (age-standardized annual incidence per 100 000 ranging from 11.8 in Sri Lanka to 29.8 in Bangladesh) and also ranks among the leading cancer types among women in the world.10 South Asia, however, stands apart from global trends in its large burden of oral and esophageal cancers (see Table 1). Similarly, ovarian cancer is relatively more frequent in the region than it is globally. Another unique feature of the cancer burden in these selected countries is the relatively larger cancer incidence among women compared with men. The comparatively high colorectal cancer incidence in Sri Lanka is distinctive in the region.
Table 1.
Cancer sites by incidence in selected South Asian countries
| India |
Bangladesh |
Pakistan |
Sri Lanka |
World |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | |
| Number of all cancer cases | 430 096 | 518 762 | 60 028 | 81 058 | 64 912 | 74 251 | 11 041 | 13 406 | 6 617 844 | 6 044 710 |
| Ranking of cancer by incidence | Cancer site (Estimated age-standardized annual incidence rate per 100 000) by ranking in incidence | |||||||||
| 1 | Lung (10.9) | Cervix (27.0) | Lung (30.4) | Cervix (29.8) | Lung (12.3) | Breast (31.5) | Lip, oral cavity (16.5) | Breast (29.1) | Lung (33.8) | Breast (38.9) |
| 2 | Lip, oral cavity (9.8) | Breast (22.9) | Lip, oral cavity (9.6) | Breast (27.2) | Lip, oral cavity (11.0) | Cervix (19.5) | Lung (12.0) | Cervix (11.8) | Prostate (27.9) | Colorectum (14.6) |
| 3 | Other pharynx (8.3) | Ovary (5.7) | Oesophagus (8.0) | Lip, oral cavity (9.9) | Stomach (8.0) | Lip, oral cavity (8.6) | Oesophagus (9.1) | Ovary (9.4) | Colorectum (20.3) | Cervix (15.2) |
| 4 | Oesophagus (6.5) | Lip, oral cavity (5.2) | Other pharynx (6.5) | Lung (8.7) | Other Pharynx (6.4) | Ovary (5.8) | Colorectum (7.5) | Thyroid (9.3) | Stomach (19.7) | Lung (13.5) |
| 5 | Stomach (4.7) | Oesophagus (4.2) | Stomach (5.9) | Oesophagus (7.6) | Oesophagus (6.2) | Oesophagus (5.7) | Leukemia (6.9) | Oesophagus (8.6) | Liver (16.0) | Stomach (9.1) |
Cancer sites affected by infectious agents are shaded in grey; the remaining unshaded sites are largely affected by lifestyle factors.
Source: GLOBOCAN, 2008. Number of cases excludes skin cancers. National cancer incidence in India, Bangladesh, and Pakistan are estimated from smaller regional studies due to the lack of national data; cross-national comparisons within the region should be interpreted with the understanding that data for these estimates are obtained from neighboring countries as needed. In Sri Lanka, the National Cancer Registry provides data.
Morbidity/mortality
Overall, the GBD Study estimated mortality and morbidity from cancers to be lower in South Asia (1645 YLLs and 1700 DALYs per 100 000) compared with the world (2670 YLLs and 2736 DALYs per 100 000) in 2010.45 Yet, within the region, there is indication of an upward secular trend in cancer mortality and morbidity. The proportion of total YLLs due to all cancers is estimated to have increased from 2.9% in 1990 to 5.3% in 2010 in South Asia.45 Disability due to all cancers, measured as share of DALYs, was highest in Bangladesh (7.3% of all DALYs) and lowest in India (3.7% of all DALYs). Lung and stomach cancers are the leading contributors to cancer-related DALYs among men, while breast and cervical cancers are among the leading contributors to DALYs among women. Total DALYs due to cancers are roughly on par between men (1696 per 100 000) and women (1643 per 100 000) in the region.
Costs
Costs related to cancer can be financially devastating to families. The costs associated with diagnostic procedures to detect and confirm cancer, as well as treatment costs, vary substantially by type of cancer, stage of diagnosis, whether private or public care is sought and region of residence.46 In a study of cancer patients at tertiary hospitals in five cities across India, roughly 40% of those surveyed reported that treatment was unaffordable and only half were aware of health insurance schemes.46 The mean costs borne by patients—including diagnostic procedures, treatment, indirect costs (such as travel and lodging) and lost wages—across study sites was ∼US$ 1670 (conversion rate: US$ 1 = 60 INR).46 Catastrophic expenditures, such as those expenditures that can lead an individual or family to impoverishment or bankruptcy, were 1.6-fold higher for hospitalizations due to cancer compared with hospitalizations due to communicable conditions.19
Screening may be a cost-effective strategy to lower disease and cost burdens for some cancers through earlier detection when the cancer is more treatable.47 For cervical cancer, for example, a strategy of screening by two visual inspections throughout the lifetime at a primary health facility amounted to US$ 91 per year of life saved and was deemed ‘very cost effective’ by standards suggested by the WHO's Commission on Macroeconomics and Health.48
Chronic obstructive pulmonary disease
COPD is a progressive condition that causes difficulty in breathing. It has been described as a classic example of ‘gene–environment’ interaction, in which both genetic predisposition and environmental exposures play a role.49 Tobacco smoke, tuberculosis, air pollution and dust—leading risk factors for COPD—are highly prevalent in South Asia and are hypothesized to drive the burden of disease in the region.50–52 Moreover, these risk factors tend to be concentrated among the poor, so higher COPD prevalence is observed among lower socioeconomic groups.49 Regional studies in India suggest that COPD has overtaken communicable diseases as a cause of adult mortality in rural areas.53 COPD is both preventable and treatable, further motivating public health interest in this NCD, both in South Asia and globally.
Prevalence/incidence and morbidity/mortality
Because the symptoms of COPD are often confused with asthma and there is inadequate health care infrastructure in South Asia, COPD is considered underdiagnosed. Thus, figures likely underestimate COPD burdens in South Asia.50,54 The estimated prevalence of COPD in India in 2006 was roughly 4%,51 and ∼4% of the total DALYs in South Asia can be attributed to COPD.45 COPD was also a leading cause of death within the region and accounted for ∼4% of YLLs and over 1 million deaths in 2010 in South Asian countries for which data existed.45 This was a significant proportion of the 2.90 million deaths worldwide due to COPD in 2010. Furthermore, South Asian countries reported among the highest age-adjusted death rates for COPD in the world, ranging from 66.4 per 100 000 in Bangladesh to 73.2 in India, compared with 23.1 in the UK.49 Although the COPD-mortality has declined from 80.3 deaths per 100 000 in 1990 to 64.3 in 2010 in South Asia, years lived with disability due to COPD have increased from 589.9 to 644.4 per 100 000 in the past two decades according to the GBD study. This pattern may be due to increasing diagnosis and better treatment of COPD, combined with increasing survival into older ages when individuals are at higher risk for COPD.2,55
Costs
Studies of costs related to COPD in South Asia are sparse. Based on a report of the National Commission on Macroeconomics and Health in India, the total number of COPD patients in India alone is projected to be 22 million in 2016, with a higher burden in rural compared with urban areas.56 The associated direct medical expenditures by patients is extremely high at US$ 80 million.56 Per patient, up to 30% of one's income may be needed for medical care.50
Trends in major NCDs and their risk factors
Between 1990 and 2010, nearly all NCDs increased at a higher rate in South Asia compared with globally, with diabetes and CHD increasing 104 and 73%, respectively.2 Although diabetes was not always ranked in the top five causes of disability in South Asia, most countries have documented diabetes as their fastest-growing health burden in the last 20 years. In Bangladesh and Pakistan, CHD increased more than 100% in the same time period. Interestingly, unlike DALY trends globally and in the South Asia region, NCDs have been dominant causes of death in Sri Lanka over the last 20 years, suggesting that Sri Lanka is in a more advanced phase of epidemiologic transition.2
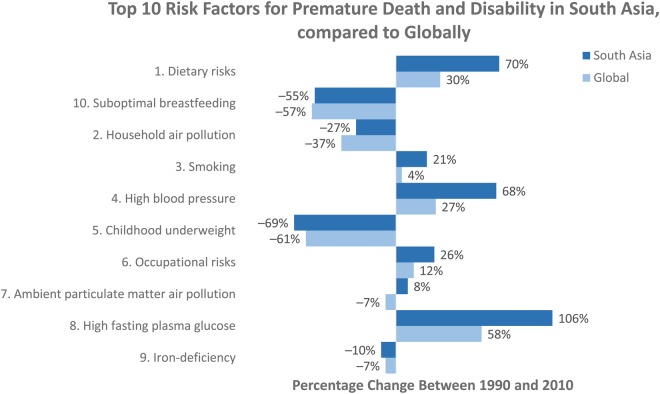
These trends in disease burden are largely due to shifts in leading NCD risk factors in the region. Globally, the leading risk factors (in terms of number of DALYs contributed) in 2010 were dietary risks, high blood pressure, smoking, household air pollution, alcohol use, high body mass index (BMI), high fasting plasma glucose, childhood underweight, ambient particulate matter pollution and physical inactivity. All except household air pollution, childhood underweight and ambient pollution increased in terms of the percentage of DALYs they contributed from 1990 to 2010.
The leading risk factors in South Asia were similar to the global distribution, with some key differences. Similar to globally, dietary risks (low consumption of fruit, nuts and seeds, and high sodium intake) ranked as the leading risk factor for premature death and disability in four countries (Bhutan, India, the Maldives and Sri Lanka) and were the third-largest risk factor in the remaining countries (Afghanistan, Bangladesh, Nepal and Pakistan).2 Smoking was the third-largest risk factor contributing to DALYs regionally and was among the top three risk factors for all countries except the Maldives, which is the only country in the South Asia region with high BMI as a top-five risk factor. Hypertension is a leading risk factor in South Asia, and the prevalence of hypertension has risen exponentially in India over the past three decades, from <5% of adults to over 20–40% of urban and 12–17% of rural adults today.17,57 Lower income countries in South Asia, like Nepal and Pakistan, reported more ill health from household air pollution and childhood underweight.2 In contrast to globally, alcohol use and high BMI are not leading risk factors in South Asia, while occupational risks, iron-deficiency and suboptimal breastfeeding continue to rank in the top 10 risk factors for disability in South Asia (Fig. 2).
Fig. 2.
Relative change in DALYs for top 10 risk factors in South Asia, compared with global. Source: IHME.2
Biological, social and economic determinants
The epidemiological transitions in the leading causes of death and disability in South Asia have multiple biological, social and economic drivers. First, South Asians have, on average, a lower BMI than those of European descent, and NCD risk starts to increase at very low levels of BMI for South Asians.58 Additionally, South Asians’ body compositions have a higher proportion of fat mass, and this is often concentrated in the abdominal area. A greater susceptibility to chronic disease may also be programmed during pregnancy; fetuses of underweight expectant mothers in South Asia are exposed to a low-nutrition environment in utero, which may program high nutrient storage.59 This is one potential explanation for the higher body fat percentage among South Asians when compared with similar individuals of other races/ethnicities. Socioculturally, traditional South Asian diets include many sweets, saturated fats and refined carbohydrates (white rice). The globalization of trade and marketing, as well as urbanization, are associated with a nutrition transition, increased exposure to processed and packaged western foods that are also high in calories, salt, fat and sugar.60
NCDs and their risk factors may manifest differently in rich and poor subgroups in South Asia, and this might also be associated with ongoing rapid urbanization that widens income and social inequities. For example, while the rich are less likely to be physically active, the poor may be less likely to consume adequate fruits and vegetables. Another example is how indoor air pollution continues to be a major contributor to COPD, but largely among poorer individuals that burn wood fuel in their homes.61 Additionally, the rich are likely to recognize their risk earlier and seek medical attention, while the poor, less likely to be aware of their risk and less able to access medical care, tend to develop rapidly progressive disease with early and sudden fatal outcomes.3 Although it is argued that NCDs are less common and therefore of little concern among lower socioeconomic groups in India and the region,28 because lower socioeconomic groups vastly outnumber their higher socioeconomic counterparts, the absolute number of people affected by NCDs in lower socioeconomic groups is substantial. In addition, using representative cross-sectional survey data from India, a recent study54 showed that self-reported NCD prevalence was higher among higher socioeconomic groups, but when using standardized measures of disease, there was no socioeconomic gradient in NCDs between lower and higher socioeconomic groups. Nonetheless, for NCDs, there are a multitude of challenges in trying to address disparities, be they socioeconomic or rural–urban. For example, there are wide differences in awareness of disease, access to care, limited human and infrastructural resources and limited understanding of what works in context.62 More data will be invaluable in designing and responding to growing NCD burdens among rural63 and lower socioeconomic groups.
Care and prevention policies and programs
The dual burden of communicable conditions and NCDs across the life course poses a special challenge for public health and medical resource allocation and programming. Table 2 lists selected key aspects of WHO's proposed Global Strategy for the Prevention and Control of NCDs and the progress in achieving these within South Asia. At the individual level, opportunities include enhancing awareness, preventive behaviors and better self-care for chronic disease prevention and management. The fact that NCDs share common risk factors suggests that structural and behavioral interventions that shift the population distribution of these risk factors should be a priority for primary prevention. Moreover, because individual-level risk factors are influenced by broader environmental, economic, infrastructural and social conditions, addressing these risk factors requires societal-level multisectoral action by agencies beyond ministries of health. In particular, creating environments that facilitate greater physical activity and allow for affordable and healthy dietary choices are complementary goals may be beneficial.
Table 2.
WHO global strategy for prevention and control of NCDs
| WHO objective for NCD control and prevention | Status | Key challenges and opportunities |
|---|---|---|
| To establish and strengthen national policies and plans for the prevention and control of NCDs |
|
Challenges:
|
| To promote interventions to reduce the main shared modifiable risk factors for NCDs: tobacco use, unhealthy diets, physical inactivity and harmful use of alcohol |
|
Challenges:
|
| To monitor NCDs and their determinants and evaluate progress at the national, regional and global levels |
|
Challenge:
|
SEAR, South East Asia Region; STEPS, STEPwise approach to surveillance; WHO, World Health Organization.
Source: WHO.64
Currently, there are limited data from South Asia to demonstrate effective individual or societal-level interventions and also very limited qualitative data about what specific target population preferences can be leveraged to achieve higher impact through interventions. An improved understanding of what works in context will be critical to minimizing disparities in NCD burdens and outcomes between advantaged and disadvantaged groups, for example, urban compared with rural populations, due to existing differences in awareness of disease-specific risks, access to care and limited human and infrastructural resources.
Improving secondary and tertiary prevention of NCDs is also needed and involves strengthening the health care system specifically. Much of the health infrastructure to date has, with justification, catered to infectious diseases and maternal and child health—all of which are components of preventing NCDs. However, instead of acknowledging the importance of reducing life-course NCD risks by managing chronic disease risks in pregnancy or attending to overnutrition disorders (e.g. obesity), current infrastructure is limited in that it is organized to support acute management alone. As such, strengthening health systems for NCDs may need re-designing or re-purposing to reach populations that are at risk for NCDs (e.g. the elderly, pregnant women who develop gestational diabetes, etc.). Possibilities for training frontline workers (such as community health workers) in NCD treatment and management may be an important step in providing care in rural areas where NCDs are only beginning to take a foothold.65
Conclusion
Since 1970, South Asian countries have made much progress in prolonging life and reducing premature mortality and disability from most communicable, newborn, nutritional and maternal causes, while disease burdens from overnutrition and NCDs have increased. Although NCD burdens are currently largest among affluent groups in South Asia, many adverse risk factors are concentrated among the poor, portending a future increase in disease burden among lower income individuals.66 Amidst the changing landscape of diseases and risk factors in South Asia, efforts to address NCDs require multisectoral and multilevel actions. Although NCDs are becoming more prominent and NCD prevention and control are now on the agenda of public health agencies in the region, lack of sustainable financing, strong leadership and governance remain as barriers to progress.
Footnotes
The publisher regrets that table one was originally published containing an error.
References
- 1.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute for Health Metrics and Evaluation. The Global Burden of Disease: Generating Evidence, Guiding Policy—South Asia Regional Edition. Seattle, WA: Institute for Health Metrics and Evaluation, University of Washington and Human Development Network, The World Bank; 2013. [Google Scholar]
- 3.Ghaffar A, Reddy KS, Singhi M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328:807–10. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations. 66/2. Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases, General Assembly, 2012, New York City.
- 5.Ko FWS, Hui DSC. Air pollution and chronic obstructive pulmonary disease. Respirology. 2012;17:395–401. doi: 10.1111/j.1440-1843.2011.02112.x. [DOI] [PubMed] [Google Scholar]
- 6.Brook RD, Franklin B, Cascio W, et al. Air pollution and cardiovascular disease: a statement for healthcare professionals from the expert panel on population and prevention science of the American Heart Association. Circulation. 2004;109:2655–71. doi: 10.1161/01.CIR.0000128587.30041.C8. [DOI] [PubMed] [Google Scholar]
- 7.Thayer KA, Heindel JJ, Bucher JR, et al. Role of environmental chemicals in diabetes and obesity: a National Toxicology Program workshop review. Environ Health Perspect. 2012;120:779–89. doi: 10.1289/ehp.1104597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slotkin TA. Does early-life exposure to organophosphate insecticides lead to prediabetes and obesity? Reprod Toxicol. 2011;31:297–301. doi: 10.1016/j.reprotox.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Diabetes Federation. Diabetes Atlas. 5th edn. Brussels: International Diabetes Federation; 2013. [Google Scholar]
- 10.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. International Journal of Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 11.Joshi P, Islam S, Pais P, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–94. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 12.O'Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case–control study. Lancet. 2010;376:112–23. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 13.Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case–control study. Lancet. 2004;364:953–62. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 14.Nishtar S. Prevention of coronary heart disease in south Asia. Lancet. 2002;360:1015–8. doi: 10.1016/S0140-6736(02)11088-9. [DOI] [PubMed] [Google Scholar]
- 15.Goyal A, Yusuf S. The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res. 2006;124:235–44. [PubMed] [Google Scholar]
- 16.Anand K, Chowdhury D, Singh KB, et al. Estimation of mortality and morbidity due to strokes in India. Neuroepidemiology. 2001;20:208–11. doi: 10.1159/000054789. [DOI] [PubMed] [Google Scholar]
- 17.Srinath Reddy K, Shah B, Varghese C, et al. Responding to the threat of chronic diseases in India. Lancet. 2005;366:1744–9. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva: World Health Organization; 2009. [Google Scholar]
- 19.Mahal A, Karan A, Engelgau M. The Economic Implications of Non-Communicable Disease for India. Washington: The World Bank; 2010. [Google Scholar]
- 20.Leeder S, Raymond S, Greenberg H, et al. A Race Against Time: The Challenge of Cardiovascular Disease in Developing Economies. New York City: The Center for Global Health and Economic Development and The Earth Institute, Columbia University; 2004. [Google Scholar]
- 21.Grundy SM, Benjamin IJ, Burke GL, et al. Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation. 1999;100:1134–46. doi: 10.1161/01.cir.100.10.1134. [DOI] [PubMed] [Google Scholar]
- 22.Fong DS, Aiello L, Gardner TW, et al. Retinopathy in diabetes. Diabetes Care. 2004;27(Suppl 1):S84–7. doi: 10.2337/diacare.27.2007.s84. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. National Chronic Kidney Disease Fact Sheet: General Information and National Estimates on Chronic Kidney Disease in the United States, 2014; available from http://www.cdc.gov/diabetes/pubs/factsheets/kidney.htm. (cited 7 July 2014).
- 24.Adler AI, Boyko EJ, Ahroni JH, et al. Lower-extremity amputation in diabetes. The independent effects of peripheral vascular disease, sensory neuropathy, and foot ulcers. Diabetes Care. 1999;22:1029–35. doi: 10.2337/diacare.22.7.1029. [DOI] [PubMed] [Google Scholar]
- 25.Pan A, Lucas M, Sun Q, et al. Bidirectional association between depression and type 2 diabetes mellitus in women. Arch Intern Med. 2010;170:1884–91. doi: 10.1001/archinternmed.2010.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gudala K, Bansal D, Schifano F, et al. Diabetes mellitus and risk of dementia: a meta-analysis of prospective observational studies. Journal of Diabetes Investigation. 2013;4:640–50. doi: 10.1111/jdi.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anjana RM, Pradeepa R, Deepa M, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 28.Shera AS, Jawad F, Maqsood A. Prevalence of diabetes in Pakistan. Diabetes Res Clin Pract. 2007;76:219–22. doi: 10.1016/j.diabres.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 29.Katulanda P, Constantine GR, Mahesh JG, et al. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka—Sri Lanka Diabetes, Cardiovascular Study (SLDCS) Diabet Med. 2008;25:1062–9. doi: 10.1111/j.1464-5491.2008.02523.x. [DOI] [PubMed] [Google Scholar]
- 30.Kinra S, Bowen LJ, Lyngdoh T, et al. Sociodemographic patterning of non-communicable disease risk factors in rural India: a cross sectional study. BMJ. 2010;341:c4974. doi: 10.1136/bmj.c4974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mohan V, Deepa M, Anjana RM, et al. Incidence of diabetes and pre-diabetes in a selected urban south Indian population (CUPS-19) J Assoc Physicians India. 2008;56:152–7. [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. CDC's Diabetes Program: Data & Trends—Crude and Age-Adjusted Incidence of Diagnosed Diabetes per 1000 Population Aged 18–79 Years, United States, 1980–2011; available from http://www.cdc.gov/diabetes/statistics/incidence/fig2.htm. (cited 31 December 2013).
- 33.Nair M, Ali MK, Ajay VS, et al. CARRS surveillance study: design and methods to assess burdens from multiple perspectives. BMC Public Health. 2012;12:701. doi: 10.1186/1471-2458-12-701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teo K, Chow CK, Vaz M, et al. The Prospective Urban Rural Epidemiology (PURE) study: examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J. 2009;158:1–7e1. doi: 10.1016/j.ahj.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 35.Das AK, Seshiah V, Sahay BK, et al. Improving management practices and clinical outcomes in type 2 diabetes study: prevalence of complications in people with type 2 diabetes in India. Indian J Endocrinol Metab. 2012;16(Suppl 2):S430–1. doi: 10.4103/2230-8210.104119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khuwaja AK, Rafique G, White F, et al. Macrovascular complications and their associated factors among persons with type 2 diabetes in Karachi, Pakistan—a multi-center study. J Pak Med Assoc. 2004;54:60–6. [PubMed] [Google Scholar]
- 37.Patel JC. Complications in 8793 cases of diabetes mellitus 14 years study in Bombay Hospital, Bombay, India. Indian J Med Sci. 1989;43:177–83. [PubMed] [Google Scholar]
- 38.Amarasinghe DA, Dalpatadu KC, Fonseka P, et al. Risk factors for long-term complications in patients with type 2 diabetes attending government institutions in the Western Province of Sri Lanka: a case control study. Diabetes Res Clin Pract. 2007;75:377–8. doi: 10.1016/j.diabres.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 39.Pradeepa R, Anjana RM, Unnikrishnana R, et al. Risk factors for microvascular complications of diabetes among South Indian subjects with type 2 diabetes—the Chennai Urban Rural Epidemiology Study (CURES) Eye Study-5. Diabetes Technol Ther. 2010;12:755–61. doi: 10.1089/dia.2010.0069. [DOI] [PubMed] [Google Scholar]
- 40.Grover S, Avasthi A, Bhansali A, et al. Cost of ambulatory care of diabetes mellitus: a study from north India. Postgrad Med J. 2005;81:391–5. doi: 10.1136/pgmj.2004.024299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khowaja LA, Khuwaja AK, Cosgrove P. Cost of diabetes care in out-patient clinics of Karachi, Pakistan. BMC Health Serv Res. 2007;21:189–96. doi: 10.1186/1472-6963-7-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramachandran A, Ramachandran S, Snehalatha C, et al. Increasing expenditure on health care incurred by diabetic subjects in a developing country: a study from India. Diabetes Care. 2007;30:252–6. doi: 10.2337/dc06-0144. [DOI] [PubMed] [Google Scholar]
- 43.Tharkar S, Devarajan A, Kumpatla S, et al. The socioeconomics of diabetes from a developing country: a population based cost of illness study. Diabetes Res Clin Pract. 2010;89:334–40. doi: 10.1016/j.diabres.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 44.Bray F, Jemal A, Grey N, et al. Global cancer transitions according to the Human Development Index (2008–2030): a population-based study. Lancet Oncol. 2012;13:790–801. doi: 10.1016/S1470-2045(12)70211-5. [DOI] [PubMed] [Google Scholar]
- 45.Institute for Health Metrics and Evaluation. Global Burden of Disease 2010. Institute for Health Metrics and Evaluation and University of Washington; 2013. [Google Scholar]
- 46.Nair KS, Raj S, Tiwari VK, et al. Cost of treatment for cancer: experiences of patients in public hospitals in India. Asian Pac J Cancer Prev. 2013;14:5049–54. doi: 10.7314/apjcp.2013.14.9.5049. [DOI] [PubMed] [Google Scholar]
- 47.Smith RA, Cokkinides V, Brawley OW. Cancer screening in the United States, 2009: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2009;59:27–41. doi: 10.3322/caac.20008. [DOI] [PubMed] [Google Scholar]
- 48.Goldie SJ, Gaffikin L, Goldhaber-Fiebert JD, et al. Cost-effectiveness of cervical-cancer screening in five developing countries. N Engl J Med. 2005;353:2158–68. doi: 10.1056/NEJMsa044278. [DOI] [PubMed] [Google Scholar]
- 49.Mannino DM. COPD and lung cancer have come a long way … baby. Am J Respir Crit Care Med. 2007;176:108–9. doi: 10.1164/rccm.200704-590ED. [DOI] [PubMed] [Google Scholar]
- 50.Jindal SK. Emergence of chronic obstructive pulmonary disease as an epidemic in India. Indian J Med Res. 2006;124:619–30. [PubMed] [Google Scholar]
- 51.Jindal SK, Aggarwal AN, Chaudhry K, et al. A multicentric study on epidemiology of chronic obstructive pulmonary disease and its relationship with tobacco smoking and environmental tobacco smoke exposure. Indian J Chest Dis Allied Sci. 2006;48:23–9. [PubMed] [Google Scholar]
- 52.Anwar SK, Mehmood N, Nasim N, et al. Sweeper's lung disease: a cross-sectional study of an overlooked illness among sweepers of Pakistan. Int J Chron Obstruct Pulmon Dis. 2013;8:193–7. doi: 10.2147/COPD.S40468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bhome AB. COPD in India: iceberg or volcano? J Thorac Dis. 2012;4:298–309. doi: 10.3978/j.issn.2072-1439.2012.03.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vellakkal S, Subramanian SV, Millett C, et al. Socioeconomic inequalities in non-communicable diseases prevalence in India: disparities between self-reported diagnoses and standardized measures. PLoS One. 2013;8:e68219. doi: 10.1371/journal.pone.0068219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370:765–73. doi: 10.1016/S0140-6736(07)61380-4. [DOI] [PubMed] [Google Scholar]
- 56.National Commission on Macroeconomics and Health. NCMH Background 850 Papers—Burden of Disease in India. New Delhi, India: Ministry of Health & Family Welfare; 2005. Economic burden of chronic obstructive pulmonary disease. [Google Scholar]
- 57.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–8. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 58.Ramachandran A. Epidemiology of diabetes in India—three decades of research. J Assoc Physicians India. 2005;53:34–8. [PubMed] [Google Scholar]
- 59.Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129–40. doi: 10.1001/jama.2009.726. [DOI] [PubMed] [Google Scholar]
- 60.Siegel K, Narayan KM, Kinra S. Finding a policy solution to India's diabetes epidemic. Health Aff (Millwood) 2008;27:1077–90. doi: 10.1377/hlthaff.27.4.1077. [DOI] [PubMed] [Google Scholar]
- 61.Torres-Duque C, Maldonado D, Perez-Padilla R, et al. Biomass fuels and respiratory diseases: a review of the evidence. Proc Am Thorac Soc. 2008;5:577–90. doi: 10.1513/pats.200707-100RP. [DOI] [PubMed] [Google Scholar]
- 62.Ali MK, Narayan KM, Mohan V. Innovative research for equitable diabetes care in India. Diabetes Res Clin Pract. 2009;86:155–67. doi: 10.1016/j.diabres.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 63.Zabetian A, Sanchez IM, Narayan KM, et al. Global rural diabetes prevalence: a systematic review and meta-analysis covering 1990–2012. Diabetes Res Clin Pract. 2014;104:206–13. doi: 10.1016/j.diabres.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 64.World Health Organization. The WHO 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 65.Chow CK, Pell JP. Importance of screening to prevent heart attacks. Future Cardiol. 2008;4:103–6. doi: 10.2217/14796678.4.2.103. [DOI] [PubMed] [Google Scholar]
- 66.Narayan KM, Ali MK. Commentary: shielding against a future inferno: the not-so-problematic discourse on socioeconomic status and cardiovascular health in India. Int J Epidemiol. 2013;42:1426–9. doi: 10.1093/ije/dyt082. [DOI] [PubMed] [Google Scholar]