Abstract
Background
Depression is often undiagnosed and untreated. It is not clear if differences exist in the diagnosis and treatment of depression among pregnant and nonpregnant women. We sought to estimate the prevalence of undiagnosed depression, treatment by modality, and treatment barriers by pregnancy status among U.S. reproductive-aged women.
Methods
We identified 375 pregnant and 8,657 nonpregnant women 18–44 years of age who met criteria for past-year major depressive episode (MDE) from 2005–2009 nationally representative data. Chi-square statistics and adjusted prevalence ratios (aPR) were calculated.
Results
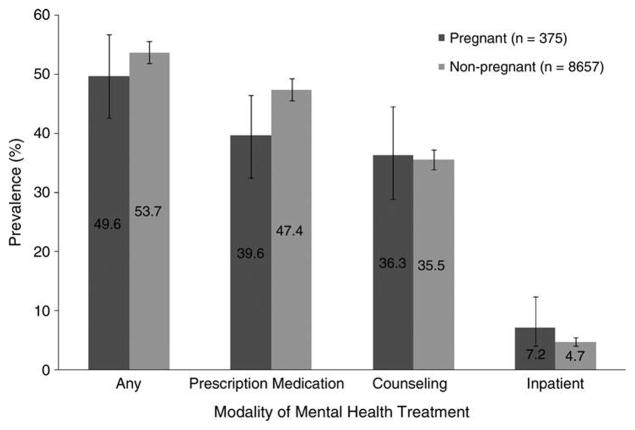
MDE in pregnant women (65.9%) went undiagnosed more often than in nonpregnant women (58.6%) (aPR 1.1, 95% confidence interval [CI] 1.0–1.3). Half of depressed pregnant (49.6%) and nonpregnant (53.7%) women received treatment (aPR 1.0, 95% CI 0.90–1.1), with prescription medication the most common form for both pregnant (39.6%) and nonpregnant (47.4%) women. Treatment barriers did not differ by pregnancy status and were cost (54.8%), opposition to treatment (41.7%), and stigma (26.3%).
Conclusions
Pregnant women with MDE were no more likely than nonpregnant women to be diagnosed with or treated for their depression.
Introduction
Depression is a leading cause of global disability and the second leading cause of global disease burden among people 15–44 years of age.1 Women are disproportionately affected, as they are almost twice as likely as men to report lifetime history of major depressive episode (MDE).2,3 Depression affects 8%–16% of U.S. reproductive-aged women2,4–6 and is associated with concurrent psychiatric and substance use disorders7 and adverse reproductive outcomes, including decreased fertility8; poor pregnancy outcomes, such as preterm delivery or low birthweight (LBW) infant9,10; and impaired maternal functioning and bonding.11
Effective depression treatment for women includes counseling, behavioral therapy, exercise, and antidepressants.12 However, half or fewer of depressed women receive a diagnosis5 or treatment,4,7 and barriers to treatment are not well understood. Among depressed and treated women, prevalence by type of treatment is unknown and may differ by pregnancy status. Understanding the prevalence of pharmacotherapy among women is especially important because 49% of pregnancies are unintended13 and the effects of pre-natal antidepressant use on the fetus are not fully understood.10,14–18 Furthermore, whether depressed pregnant women are more likely to receive a diagnosis and treatment because of their frequent interactions with the healthcare system is unknown. Therefore, we estimate the prevalence and predictors of undiagnosed depression, treatment prevalence overall and by modality, and treatment barriers among a nationally representative population-based sample of U.S. reproductive-aged women.
Materials and Methods
Data source and participants
We used combined public use data from the 2005–2009 National Surveys on Drug Use and Health (NSDUH). The NSDUH, sponsored by the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA), is a cross-sectional survey designed to estimate prevalence and correlates of substance use in U.S. household populations aged ≥12 years. The NSDUH samples the civilian, noninstitutionalized population using multistage area probability sampling to randomly sample households in 50 states and the District of Columbia.
Beginning in 2005, an adult depression module was administered in person via computer-assisted instruments to all respondents aged ≥18 years. The overall weighted response rate for 2005–2009 was 67.6%.19–23 Detailed information about the sampling and survey methodology can be found elsewhere.19–23 As this study uses de-identified, publicly available data, approval by the Centers for Disease Control and Prevention (CDC), institutional review board was not required. Combined 2005–2009 data yielded 77,415 female respondents aged 18–44 years. Of these, 76,772 women (99.2%) reported data on pregnancy status and MDE. A total of 9,032 reproductive-aged women reported having MDE in the year preceding the survey, referred to hereafter as past-year MDE.
Measures
Major depressive episode
MDE was assessed using nine questions about MDE symptoms, as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV).24 A respondent met DSM-IV criteria for past-year MDE if she reported experiencing ≥5 symptoms nearly every day in the same 2-week period in the past 12 months, with at least 1 of the 5 symptoms being depressed mood or loss of interest or pleasure in daily activities. Additionally, any self-reported functional impairment in home management, work, social life, or personal relationships due to depressive symptoms was examined. Women also self-reported whether a doctor or other medical professional had told them that they had depression in the past year, which was asked separately from MDE symptoms and is referred to hereafter as having a clinical diagnosis of depression.
Mental health treatment
Three NSDUH questions assessed past-year treatment. Respondents were asked: “During the past 12 months, did you take any prescription medication that was prescribed for you to treat a mental or emotional condition? During the past 12 months, did you receive any outpatient treatment or counseling for any problem you were having with your emotions, nerves, or mental health? During the past 12 months, have you stayed overnight or longer in a hospital or other facility to receive treatment or counseling for any problem you were having with your emotions, nerves, or mental health? Mental health treatment was defined as receiving prescription medication, counseling, or inpatient care in the past year.
Respondents who answered yes to the question: During the past 12 months, was there any time when you needed mental health treatment or counseling for yourself but didn’t get it? were classified as having unmet treatment needs. We classified barriers to mental health treatment as cost (could not afford cost, insurance did not cover at all, insurance did not pay enough), stigma (fear of neighbors’ negative opinion, fear of negative effects on job, confidentiality concerns, did not want others to find out), opposition to treatment (didn’t think treatment was needed at the time, could handle problems without treatment, didn’t think treatment would help, fear of being committed/medicated), time or transportation limitations (didn’t have time, no transportation, or inconvenient), and did not know where to go.
Pregnancy and sociodemographic characteristics
Women self-reported their pregnancy status. Demographic variables included self-reported age in years (18–25, 26–34, 35–44), race/ethnicity (non-Hispanic white, African American, Hispanic, and other), education (less than high school, high school graduate, some college, college or more), employment (full-time, part-time, unemployed, and other, i.e., disabled, keeping house full-time, in school/training, or retired), annual family income (< $20,000, $20,000–49,999, $50,000–74,999, ≥$75,000), marital status (married; widowed, divorced, or separated; never been married), and health insurance (public: Medicaid, Medicare, health care programs for uniformed service members, retirees, and families including TRICARE/CHAMPUS [Civilian Health and Medical Program of the Uniformed Services], CHAMPVA [Civilian Health and Medical Program of the Department of Veterans Affairs], Veterans Affairs, or other military health insurance, without private insurance; private: health insurance through employment; or uninsured). Whereas MDE and mental health treatment were assessed over the past year, women were asked to report current pregnancy and sociodemographic characteristics at the time of the interview.
Statistical analyses
Chi-square tests were conducted to assess differential distribution of sociodemographic characteristics by pregnancy status. Separate multivariable general linear models with Poisson distribution were used to estimate the adjusted prevalence ratio (aPR) of not receiving a clinical diagnosis among women who met MDE criteria. Correlates of interest included pregnancy status, age, race, education, employment, income, marital status, and health insurance. In addition, we estimated the aPR of receiving any treatment in the past year and the aPR of receiving prescription medication in the past year, adjusted for diagnosis and the correlates listed previously. A sensitivity analysis was conducted on all three adjusted prevalence ratio models, restricting the sample to only women who experienced functional impairment with past-year MDE. The prevalence of self-reported treatment barriers was also examined by pregnancy status. All analyses were conducted using Stata 10.0 and included a weighting variable to account for the complex survey design and probability of sampling.
Results
Characteristics of women
Among all reproductive-aged women, the prevalence of past-year MDE was 10.9%, representing 1.2 million women per year in 2005–2009. Among women with past-year MDE, 99.6% self-reported some functional impairment in home management, work, social life, or personal relationships. The prevalence of past-year MDE among pregnant women was 7.7% compared with 11.1% among nonpregnant women (p < 0.001). Distributions of sociodemographic characteristics by pregnancy status among women with MDE are shown in Table 1. Pregnant women were more likely than nonpregnant women to be younger, have other employment, be married, and have public insurance (p < 0.01). Fewer pregnant women (14.6%) with past-year MDE were uninsured compared to nonpregnant women with past-year MDE (21.6%).
Table 1.
Characteristics of Women with Past-Year Major Depressive Episode, by Pregnancy Status (n = 9,032), National Survey on Drug Use and Health, 2005–2009
| Characteristic | Pregnanta % (95% CI) n = 375 | Nonpregnanta % (95% CI) (n = 8,657) | p value |
|---|---|---|---|
| Age, years | |||
| 18–25 | 48.6 (41.1–56.2) | 31.0 (29.6–32.5) | < 0.001 |
| 26–34 | 39.0 (30.9–47.7) | 30.3 (28.7–32.0) | |
| 35–44 | 12.4 (7.1–20.7) | 38.7 (36.7–40.6) | |
| Race/ethnicity | |||
| Non-Hispanic white | 74.0 (65.8–80.8) | 71.2 (70.0–72.5) | 0.35 |
| African American | 10.0 (6.5–15.0) | 11.6 (10.5–12.7) | |
| Hispanic | 13.1 (8.9–18.9) | 11.9 (10.7–13.1) | |
| Other | 2.9 (1.6–5.4) | 5.4 (4.7–6.2) | |
| Education | |||
| Less than high school | 18.7 (14.5–23.8) | 14.7 (13.6–15.9) | 0.35 |
| High school | 30.7 (24.5–37.8) | 29.1 (27.6–30.6) | |
| Some college | 29.5 (23.4–36.3) | 33.6 (32.2–35.0) | |
| College | 21.1 (14.7–29.3) | 22.7 (21.2–24.2) | |
| Employment | |||
| Full-time | 37.0 (29.6–45.1) | 47.6 (46.0–49.2) | < 0.001 |
| Part-time | 16.8 (12.6–22.0) | 20.0 (18.9–21.1) | |
| Other | 40.0 (32.4–48.1) | 25.0 (23.6–26.5) | |
| Unemployed | 6.3 (3.8–10.1) | 7.4 (6.7–8.3) | |
| Income | |||
| ≥$75,000 | 23.0 (16.5–31.0) | 20.3 (18.5–22.1) | 0.62 |
| $50,000–$74,999 | 15.0 (9.9–22.2) | 15.9 (14.7–17.2) | |
| $20,000–$49,999 | 32.6 (26.2–39.7) | 37.0 (35.1–38.9) | |
| < $20,000 | 29.5 (23.2–36.6) | 26.9 (25.4–28.5) | |
| Marital status | |||
| Married | 49.0 (40.9–57.1) | 36.7 (34.9–38.6) | 0.003 |
| Divorced, separated, or widowed | 10.9 (7.2–16.1) | 19.1 (17.7–20.7) | |
| Never married | 40.2 (33.1–47.6) | 44.2 (42.4–45.9) | |
| Health insurance | |||
| Uninsured | 14.6 (9.4–22.0) | 21.6 (20.4–22.8) | < 0.001 |
| Public | 40.8 (33.3–48.8) | 21.9 (20.4–23.5) | |
| Private | 44.6 (36.3–53.1) | 56.5 (54.8–58.1) | |
Total percentages may not sum to 100.0% because of rounding. CI, confidence interval.
Clinical diagnosis of depression
Among women who met DSM-IV criteria for MDE, 58.8% did not receive a clinical diagnosis in the past year (Table 2). Pregnant women (65.9%) had a higher prevalence of undiagnosed depression compared to nonpregnant women, although this did not reach statistical significance (58.6%) (p = 0.06, aPR 1.1, 95% confidence interval, [CI] 1.0–1.3). Women with a high prevalence of undiagnosed depression were younger (65.8%), African American (73.1%), Hispanic (68.0%), of other racial and ethnic groups (67.6%), and uninsured (65.8%). In adjusted analyses, these same groups of women had statistically significantly higher PRs for having undiagnosed depression, although associations were attenuated, and aPRs ranged from 1.1. to 1.4. Restriction of the sample to women with past-year MDE symptoms and functional impairment did not change the results (data not shown).
Table 2.
Correlates of Not Receiving Clinical Diagnosis of Depression in Past Year Among Women Who Met DSM-IV Criteria for Past-Year Major Depressive Episode, National Survey on Drug Use and Health, 2005–2009
| Diagnosed % (95% CI) | No diagnosis % (95% CI) | Chi-square p-value | No diagnosis aPR (95% CI) | |
|---|---|---|---|---|
| Total | 41.2 (39.3–43.0) | 58.8 (57.0–60.7) | ||
| Pregnancy status | ||||
| Pregnant | 34.1 (27.1–41.9) | 65.9 (58.1–72.9) | 0.06 | 1.1 (1.0–1.3) |
| Nonpregnant | 41.4 (39.5–43.3) | 58.6 (56.7–60.5) | 1.0 | |
| Age, years | ||||
| 18–25 | 34.2 (32.7–35.7) | 65.8 (64.3–67.3) | < 0.001 | 1.2 (1.1–1.2) |
| 26–34 | 42.1 (38.4–46.0) | 57.9 (54.0–61.6) | 1.0 (0.9–1.1) | |
| 35–44 | 46.2 (43.0–49.4) | 53.8 (50.6–57.0) | 1.0 | |
| Race/ethnicity | ||||
| Non-Hispanic white | 45.6 (43.5–47.8) | 54.4 (52.2–56.5) | < 0.001 | 1.0 |
| African American | 26.9 (22.9–31.5) | 73.1 (68.5–77.2) | 1.4 (1.3–1.5) | |
| Hispanic | 32.0 (27.7–36.6) | 68.0 (63.4–72.3) | 1.2 (1.2–1.3) | |
| Other | 32.4 (26.0–39.6) | 67.6 (60.4–74.0) | 1.2 (1.1–1.4) | |
| Education | ||||
| Less than high school | 38.8 (34.5–43.2) | 61.2 (56.8–65.5) | 0.48 | 1.0 (0.9–1.2) |
| High school | 42.3 (39.5–45.3) | 57.7 (54.8–60.6) | 1.0 (0.9–1.0) | |
| Some college | 41.8 (39.4–44.3) | 58.2 (55.7–60.7) | 1.0 (0.9–1.0) | |
| College | 40.2 (36.3–44.3) | 59.8 (55.7–63.8) | 1.0 | |
| Employment | ||||
| Full-time | 38.8 (36.1–41.7) | 61.2 (58.3–64.0) | 0.002 | 1.0 (0.9–1.1) |
| Part-time | 40.1 (36.8–43.5) | 59.9 (56.5–63.2) | 1.0 (0.9–1.1) | |
| Other | 47.1 (43.2–51.1) | 52.9 (48.9–56.8) | 1.0 (0.8–1.0) | |
| Unemployed | 38.3 (32.6–44.5) | 61.7 (55.5–67.4) | 1.0 | |
| Income | ||||
| ≥$75,000 | 38.8 (34.9–42.9) | 61.2 (57.2–65.1) | 0.47 | 1.1 (1.0–1.2) |
| $50,000–$74,999 | 42.9 (38.6–47.4) | 57.1 (52.6–61.4) | 1.0 (0.9–1.1) | |
| $20,000–$49,999 | 41.7 (38.8–44.7) | 58.3 (55.3–61.2) | 1.0 (0.9–1.1) | |
| < $20,000 | 41.1 (38.2–44.1) | 58.9 (56.0–61.8) | 1.0 | |
| Marital status | ||||
| Married | 44.7 (41.3–48.1) | 55.3 (51.9–58.7) | < 0.001 | 1.0 (0.9–1.1) |
| Divorced, separated, or widowed | 45.4 (40.9–50.0) | 54.6 (50.0–59.1) | 1.0 (0.9–1.1) | |
| Never married | 36.4 (34.2–38.6) | 63.6 (61.4–65.8) | 1.0 | |
| Health insurance | ||||
| Uninsured | 34.2 (31.3–37.3) | 65.8 (62.7–68.7) | < 0.001 | 1.1 (1.0–1.2) |
| Public | 48.4 (45.2–51.6) | 51.6 (48.4–54.8) | 0.9 (0.8–0.9) | |
| Private | 40.9 (38.4–43.4) | 59.1 (56.6–61.6) | 1.0 | |
aPR, adjusted prevalence ratio compared to diagnosis and adjusted for sociodemographic characteristics listed.
Mental health treatment
An estimated 49.6% of pregnant women and 53.7% of nonpregnant women with past-year MDE received mental health treatment in the past year (prescription medication, counseling, or inpatient care) but the difference between groups was not statistically significant (p = 0.21) (Fig. 1). Among women with past-year MDE, prescription medication was most commonly reported by pregnant (39.6%) and non-pregnant women (47.4%), followed by counseling (36.3% of pregnant and 35.5% of nonpregnant women), and the least common treatment modality was inpatient care (7.2% of pregnant and 4.7% of nonpregnant women). Of the three treatment modalities, only the prevalence of prescription medication differed between pregnant and nonpregnant women (p = 0.04). Among all women with MDE receiving treatment, 55.4% received both counseling and prescription medication (95% CI 53.1–57.7), with no differences by pregnancy status (data not shown).
FIG. 1.
Prevalence of treatment among pregnant vs. nonpregnant women with past-year major depressive episode. National Survey on Drug Use and Health, 2005–2009.
Women with past-year MDE were more than twice as likely to receive treatment if they had a clinical diagnosis (68.0%) compared with undiagnosed women (32.0%, p < 0.001) (data not shown). Among women with past-year MDE, pregnant women were just as likely to receive any treatment (aPR 1.0, 95% CI 0.9–1.1) and, specifically, prescription medication (aPR 0.93, 95% CI 0.8–1.1) as nonpregnant women, after adjusting for clinical diagnosis and sociodemographic characteristics (data not shown). Restriction of the sample to women with past-year MDE symptoms and functional impairment did not change the results (data not shown).
Unmet treatment need and barriers to receiving treatment
Overall, 38.9% (95% CI 37.1–40.6) of women with past-year MDE reported unmet treatment needs in the past year (data not shown). Among these women, common treatment barriers were cost (54.8%, 95% CI 51.7–57.9), opposition to treatment (41.7%, 95% CI 39.3–44.1), stigma concerns (26.3%, 95% CI 24.1–28.6), time or transportation limitations (18.1%, 95% CI 16.0–20.4), and not knowing where to go for treatment (16.7%, 95% CI 14.9–18.6) (data not shown). Unmet treatment needs and treatment barriers did not differ by pregnancy status. Unmet treatment need was higher among women with a clinical diagnosis (48.6%) than among undiagnosed women (32.2%) (p < 0.001). Treatment barriers were similar between those with and without a diagnosis, although more women with a clinical diagnosis (18.6%) knew where to go for treatment compared with undiagnosed women (14.9%) (p = 0.02).
Discussion
We found that > 1 in 10 reproductive-aged women met criteria for MDE in the past year, representing approximately 1.2 million U.S. women. Additionally, about 60% who met criteria for past-year MDE did not receive a diagnosis of depression, and almost half did not receive any mental health treatment. Pregnant women were no more likely to receive a diagnosis or treatment than were nonpregnant women. Prescription medication was the most common treatment for past-year MDE among both pregnant and nonpregnant women. The top three barriers to mental health treatment for pregnant and nonpregnant women were cost, opposition to treatment, and stigma.
Prevalence estimates of past-year MDE in this study are consistent with other national studies for reproductive-aged women.4,5 We found that the prevalence of MDE among pregnant women was lower than among nonpregnant women, consistent with another nationally representative study that found that the prevalence of major depressive disorder was 5.6% among pregnant women compared to 8.1% among non-pregnant reproductive-aged women.4 A diagnosis of depression is often the first step toward receiving treatment. In this study, women with a diagnosis were more than twice as likely to receive treatment. However, about 60% of reproductive-aged women with past-year MDE in our study did not receive a clinical diagnosis of depression in the past year. This is a concern, as approximately 73% of reproductive-aged women see a clinician for reproductive health concerns at least annually25 and, thus, have an opportunity to discuss their mental health or be screened for depression by a medical professional.
We also found that past-year depression in pregnant women more often went undiagnosed compared with non-pregnant women, even though pregnant women tend to interact with the healthcare system more than nonpregnant women, averaging once every month during a pregnancy.26 We had data only on past-year depressive episodes, and some women were not pregnant when they experienced the reported depressive symptoms. However, the lower prevalence of diagnosis among pregnant women suggests that prenatal care providers may miss opportunities to identify and connect pregnant women with MDE to mental health services or that pregnant women are receiving screening and referrals but not seeking specialized care for diagnosis and treatment. Other studies have found that psychiatric disorders often go unrecognized and undiagnosed by obstetricians27 and gynecologists27–29 and that depression screening rates among their patients are low, with one study finding that only 9%–12% of obstetricians and gynecologists routinely ask or screen for depressive symptoms.29 The rates of depression diagnosis may be low in part because the U.S. Preventive Services Task Force (USPSTF) recommends screening adults for depression only when staff-assisted depression care supports are in place to ensure accurate diagnosis, effective treatment, and follow-up.30 Clinicians who are unprepared to treat depression and have no place to refer uninsured women appropriately may not screen. Although the American College of Obstetricians and Gynecologists (ACOG) states that “at this time, there is insufficient evidence to support a firm recommendation for universal antepartum or postpartum screening,” it also states that “screening for depression has the potential to benefit a woman and her family and should be strongly considered.”31 Continued support for depression screening by ACOG and continued efforts to promote greater awareness of the issue among their members may lead to increased screening rates among providers. Additionally, increasing the availability of and access to affordable treatment may improve depression diagnosis and treatment.
Approximately half of pregnant and nonpregnant women with past-year MDE did not receive treatment. This is consistent with national estimates of depression treatment among the general adult population32,33 and reproductive-aged women with serious psychologic distress.5 However, our estimates are lower than rates reported among reproductive-aged women with any mood disorder.4 A national study using 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) data, conducted by the National Institute on Alcohol Abuse and Alcoholism, found that the prevalence of not receiving treatment for mood disorder was significantly higher among past-year pregnant (86%) and postpartum (85%) women than among nonpregnant women (74%).4 These discrepancies may be due to differences in definitions. The NESARC study estimated treatment for any mood disorder, which included major depressive disorder, dysthymia, and bipolar disorder,4 whereas our study estimated any treatment for emotions, nerves, or mental health among women with MDE. Together, these national studies indicate that mental health treatment is highly underused among depressed, reproductive-aged women.
The low rate of depression diagnosis may explain treatment underuse, as our study also found that almost 90% of women who received a diagnosis of depression also received some form of treatment. Among diagnosed women, however, treatment barriers still exist, with > 48% reporting an unmet treatment need. Younger women, women of racial/ethnic minority groups, and uninsured women were the least likely to receive diagnoses. Disparities among these groups are also reflected in the top three barriers to mental health treatment: cost, opposition to treatment, and stigma. Certain racial/ethnic minority groups and uninsured people consistently demonstrate unmet mental health treatment need in national studies of reproductive-aged women5 and the general adult population.32–35 Several studies have demonstrated that African Americans and Hispanics perceive greater stigma36,37 and have more negative beliefs about the usefulness and effectiveness of anti-depressant medication and counseling compared with non-Hispanic whites.38
We found that reproductive-aged women with past-year MDE most often used prescription medication, followed by counseling and inpatient care, and that type of treatment did not vary by pregnancy status after adjustment for covariates. Our prevalence estimates of treatment modality are similar to those reported for the general U.S. adult population.39 Although prevalence of inpatient care was low, it equates to receipt of inpatient care by over 52,000 reproductive-aged women with severe mental health conditions each year. Our study found that 2 of 5 reproductive-aged women with MDE use prescription medication for mental health treatment; this is important because half of pregnancies are unintended,25 and the effects of antidepressants on the fetus and breastfed infant are not fully understood. Past research suggests possible associations between prenatal antidepressant use and miscarriage, LBW infants, and infant persistent pulmonary hypertension10,14–16; associations between depression and preterm birth and LBW infants have also been observed.9,10
Study limitations
There were several study limitations. First, data were available only on pregnancy status at the time of the interview and not in the past year. Thus, past-year MDE and past-year diagnosis may not have occurred during the pregnancy; on average, pregnant women were in their second trimester. Second, we could not identify postpartum women using publicly available data; however, only 6.9% (95% CI 6.7–7.1) of nonpregnant women aged 18–44 years reported having a child < 1 year of age in the household (personal communication with NSDUH staff regarding data in 2002–2009 non-public use files). Therefore, including postpartum women in the nonpregnant group likely had little effect on prevalence estimates. Third, depressive symptoms were not clinically validated, and mental health diagnosis and treatment were self-reported. Women may be reluctant to disclose depressive symptoms, diagnosis, or treatment, although use of computer-assisted interviews may lessen this bias. Fourth, mental health treatment was not specific to MDE but was rather for emotions, nerves, or mental health; thus, we may have overestimated treatment for depression, as treatment could have been for other psychiatric disorders, such as anxiety.
This study is the first, to our knowledge, to report treatment prevalence by modality and treatment barriers among a nationally representative sample of pregnant and non-pregnant reproductive-aged women. The large dataset and multiple years of data enabled us to stratify estimates by pregnancy status and increase our power to detect associations. Computer-assisted data collection also lessened social desirability bias.
Findings from this study lead to a few public health implications. First, as reproductive-aged women periodically see medical providers for contraception and more often for pregnancy or other reproductive health concerns, reproductive health visits may be opportunities to assess depressive symptoms and refer women to care if needed. Second, expanded insurance coverage for mental health treatment is needed because depression often goes untreated, especially among the uninsured, and because cost was the most common treatment barrier. Finally, given the high prescription medication use among women with past-year MDE, a greater understanding is needed about the antidepressant effects on fetuses and breastfed infants so that women, with the help of their providers, can make informed decisions about mental health treatment during pregnancy and while breastfeeding.
Acknowledgments
Funding was provided by U.S. Centers for Disease Control and Prevention. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.World Health Orgnaization. Depression fact sheet. Geneva: WHO; 2010. [Google Scholar]
- 2.Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: Lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- 3.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 4.Vesga-Lopez O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65:805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farr SL, Bitsko RH, Hayes DK, Dietz PM. Mental health and access to services among US women of reproductive age. Am J Obstet Gynecol. 2010;203:542 e1–9. doi: 10.1016/j.ajog.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Melville JL, Gavin A, Guo Y, Fan MY, Katon WJ. Depressive disorders during pregnancy: Prevalence and risk factors in a large urban sample. Obstet Gynecol. 2010;116:1064–1070. doi: 10.1097/AOG.0b013e3181f60b0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Le Strat Y, Dubertret C, Le Foll B. Prevalence and correlates of major depressive episode in pregnant and postpartum women in the United States. J Affect Disord. 2011;135:128–138. doi: 10.1016/j.jad.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Williams KE, Marsh WK, Rasgon NL. Mood disorders and fertility in women: A critical review of the literature and implications for future research. Hum Reprod Update. 2007;13:607–616. doi: 10.1093/humupd/dmm019. [DOI] [PubMed] [Google Scholar]
- 9.Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intra-uterine growth restriction. Arch Gen Psychiatry. 2010;67:1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yonkers KA, Wisner KL, Stewart DE, et al. The management of depression during pregnancy: A report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Gen Hosp Psychiatry. 2009;31:403–413. doi: 10.1016/j.genhosppsych.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Field T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behav Dev. 2010;33:1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farr SLDP, Williams JR, Gibbs FA, Tregear S. Depression screening and treatment among nonpregnant women of reproductive age in the United States. Prev Chronic Dis. 2011;8:A122. [PMC free article] [PubMed] [Google Scholar]
- 13.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 14.Pearlstein T. Perinatal depression: Treatment options and dilemmas. J Psychiatry Neurosci. 2008;33:302–318. [PMC free article] [PubMed] [Google Scholar]
- 15.Payne JL, Meltzer-Brody S. Antidepressant use during pregnancy: current controversies and treatment strategies. Clin Obstet Gynecol. 2009;52:469–482. doi: 10.1097/GRF.0b013e3181b52e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hemels MEH, Einarson A, Koren G, Lanctt K, Einarson T. Antidepressant use during pregnancy and the rates of spontaneous abortions: A meta-analysis. Ann Pharmacother. 2005;39:803–809. doi: 10.1345/aph.1E547. [DOI] [PubMed] [Google Scholar]
- 17.Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: Impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009;166:557–566. doi: 10.1176/appi.ajp.2008.08081170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chambers CD, Johnson KA, Dick LM, Felix RJ, Jones KL. Birth outcomes in pregnant women taking fluoxetine. N Engl J Med. 1996;335:1010–1015. doi: 10.1056/NEJM199610033351402. [DOI] [PubMed] [Google Scholar]
- 19.National Household Survey on Drug Abuse. 2005 public use file and codebook. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2006. [Google Scholar]
- 20.National Household Survey on Drug Abuse. 2006 public use file and codebook. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2007. [Google Scholar]
- 21.National Household Survey on Drug Abuse. 2007 public use file and codebook. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2008. [Google Scholar]
- 22.National Household Survey on Drug Abuse. 2008 public use file and codebook. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2009. [Google Scholar]
- 23.National Household Survey on Drug Abuse. 2009 public use file and codebook. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2010. [Google Scholar]
- 24.American Psychological Association. Diagnostic and statistical manual of mental disorder. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 25.Chandra AMG, Mosher WD, Abma JC, Jones J. National Center for Health Statistics. 2005. Fertility, family planning, and reproductive health of U.S. women: Data from the 2002 National Survey of Family Growth. [PubMed] [Google Scholar]
- 26.Lockwood C, Lemons JA, Riley L, Blackman L, editors. Guidelines for perinatal care. 6. Chicago, IL: American Academy of Pediatrics; 2007. American Academy of Pediatrics and American College of Obstetricians and Gynecologists. [Google Scholar]
- 27.Kelly R, Zatzick D, Anders T. The detection and treatment of psychiatric disorders and substance use among pregnant women cared for in obstetrics. Am J Psychiatry. 2001;158:213–219. doi: 10.1176/appi.ajp.158.2.213. [DOI] [PubMed] [Google Scholar]
- 28.Miranda J, Azocar F, Komaromy M, Golding JM. Unmet mental health needs of women in public-sector gynecologic clinics. Am J Obstet Gynecol. 1998;178:212–217. doi: 10.1016/s0002-9378(98)80002-1. [DOI] [PubMed] [Google Scholar]
- 29.Dietrich AJ, Williams JW, Jr, Ciotti MC, et al. Depression care attitudes and practices of newer obstetrician-gynecologists: A national survey. Am J Obstet Gynecol. 2003;189:267–273. doi: 10.1067/mob.2003.410. [DOI] [PubMed] [Google Scholar]
- 30.Screening for depression in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:784–792. doi: 10.7326/0003-4819-151-11-200912010-00006. [DOI] [PubMed] [Google Scholar]
- 31.Screening for depression during and after pregnancy. Committee Opinion No. 453. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2010;115:394–395. doi: 10.1097/AOG.0b013e3181d035aa. [DOI] [PubMed] [Google Scholar]
- 32.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 33.Roy-Byrne PP, Joesch JM, Wang PS, Kessler RC. Low socioeconomic status and mental health care use among respondents with anxiety and depression in the NCS-R. Psychiatr Serv. 2009;60:1190–1197. doi: 10.1176/ps.2009.60.9.1190. [DOI] [PubMed] [Google Scholar]
- 34.Dhingra SS, Zack MM, Strine TW, Druss BG, Berry JT, Balluz LS. Psychological distress severity of adults reporting receipt of treatment for mental health problems in the BRFSS. Psychiatr Serv. 2011;62:396–403. doi: 10.1176/ps.62.4.pss6204_0396. [DOI] [PubMed] [Google Scholar]
- 35.Neighbors HW, Caldwell C, Williams DR, et al. Race, ethnicity, and the use of services for mental disorders: Results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:485–494. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- 36.Menke R, Flynn H. Relationships between stigma, depression, and treatment in white and African American primary care patients. J Nerv Ment Dis. 2009;197:407–411. doi: 10.1097/NMD.0b013e3181a6162e. [DOI] [PubMed] [Google Scholar]
- 37.Gary FA. Stigma: Barrier to mental health care among ethnic minorities. Issues Ment Health Nurs. 2005;26:979–999. doi: 10.1080/01612840500280638. [DOI] [PubMed] [Google Scholar]
- 38.Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 39.Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67:1265–1273. doi: 10.1001/archgenpsychiatry.2010.151. [DOI] [PubMed] [Google Scholar]
This article has been cited by
- 1.Yamamoto A, McCormick MC, Burris HH. Disparities in antidepressant use in pregnancy. Journal of Perinatology. 2015;35:246–251. doi: 10.1038/jp.2014.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giurgescu Carmen, Misra Dawn P, Sealy-Jefferson Shawnita, Caldwell Cleopatra H, Templin Thomas N, Slaughter-Acey Jaime C, Osypuk Theresa L. The impact of neighborhood quality, perceived stress, and social support on depressive symptoms during pregnancy in African American women. Social Science & Medicine. 2015;130:172–180. doi: 10.1016/j.socscimed.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lederberg Stone Sarah, Hafsatou Diop, Eugene Declercq, Cabral Howard J, Fox Matthew P, Wise Lauren A. Stressful Events During Pregnancy and Postpartum Depressive Symptoms. Journal of Women’s Health. doi: 10.1089/jwh.2014.4857. ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hogue Carol JR, Parker Corette B, Willinger Marian, Temple Jeff R, Bann Carla M, Silver Robert M, Dudley Donald J, Moore Janet L, Coustan Donald R, Stoll Barbara J, Reddy Uma M, Varner Michael W, Saade George R, Conway Deborah, Goldenberg Robert L. The Association of Stillbirth with Depressive Symptoms 6–36 Months Post-Delivery. Paediatric and Perinatal Epidemiology. 2015;29(2):131–143. doi: 10.1111/ppe.2015.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barth Claudia, Villringer Arno, Sacher Julia. Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Frontiers in Neuroscience. 2015;9 doi: 10.3389/fnins.2015.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Letourneau Nicole, Secco Loretta, Colpitts Jennifer, Aldous Sarah, Stewart Miriam, Dennis Cindy-Lee. Quasi-experimental evaluation of a telephone-based peer support intervention for maternal depression. Journal of Advanced Nursing. 2015 doi: 10.1111/jan.12622. n/a-n/a. [DOI] [PubMed] [Google Scholar]
- 7.Geier Michelle L, Hills Nancy, Gonzales Marco, Tum Karoline, Finley Patrick R. Detection and treatment rates for perinatal depression in a state Medicaid population. CNS Spectrums. 2015;20:11–19. doi: 10.1017/S1092852914000510. [DOI] [PubMed] [Google Scholar]
- 8.Farr Sherry L, Ko Jean Y, Burley Kim, Gupta Seema. Provider communication on perinatal depression: a population-based study. Archives of Women’s Mental Health. 2015 doi: 10.1007/s00737-014-0493-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howard Louise M, Molyneaux Emma, Dennis Cindy-Lee, Rochat Tamsen, Stein Alan, Milgrom Jeannette. Non-psychotic mental disorders in the perinatal period. The Lancet. 2014;384:1775–1788. doi: 10.1016/S0140-6736(14)61276-9. [DOI] [PubMed] [Google Scholar]
- 10.Farr Sherry L, Denk Charles E, Dahms Elizabeth W, Dietz Patricia M. Evaluating Universal Education and Screening for Postpartum Depression Using Population-Based Data. Journal of Women’s Health. 2014;23(8):657–663. doi: 10.1089/jwh.2013.4586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Broussard Cheryl S, Frey Meghan T, Hernandez-Diaz Sonia, Greene Michael F, Chambers Christina D, Sahin Leyla, Collins Sharp Beth A, Honein Margaret A. Developing a systematic approach to safer medication use during pregnancy: summary of a Centers for Disease Control and Prevention convened meeting. American Journal of Obstetrics and Gynecology. 2014 doi: 10.1016/j.ajog.2014.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guy Sarah, Sterling Bobbie Sue, Walker Lorraine O, Harrison Tracie C. Mental Health Literacy and Postpartum Depression: A Qualitative Description of Views of Lower Income Women. Archives of Psychiatric Nursing. 2014 doi: 10.1016/j.apnu.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Claridge Amy M. Efficacy of systemically oriented psychotherapies in the treatment of perinatal depression: a meta-analysis. Archives of Women’s Mental Health. 2014;17:3–15. doi: 10.1007/s00737-013-0391-6. [DOI] [PubMed] [Google Scholar]
- 14.Creanga Andreea A, Berg Cynthia J, Ko Jean Y, Farr Sherry L, Tong Van T, Carol Bruce F, Callaghan William M. Maternal Mortality and Morbidity in the United States: Where Are We Now? Journal of Women’s Health. 2014;23:1, 3–9. doi: 10.1089/jwh.2013.4617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall Kelli Stidham, Kusunoki Yasamin, Gatny Heather, Barber Jennifer. The risk of unintended pregnancy among young women with mental health symptoms. Social Science & Medicine. 2014;100:62–71. doi: 10.1016/j.socscimed.2013.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dimidjian Sona, Goodman Sherryl H. Preferences and Attitudes Toward Approaches to Depression Relapse/Recurrence Prevention among Pregnant Women. Behaviour Research and Therapy. 2013 doi: 10.1016/j.brat.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 17.Connelly Cynthia D, Hazen Andrea L, Baker-Ericzén Mary J, Landsverk John, Horwitz Sarah McCue. Is Screening for Depression in the Perinatal Period Enough? The Co-Occurrence of Depression, Substance Abuse, and Intimate Partner Violence in Culturally Diverse Pregnant Women. Journal of Women’s Health. 2013;22(10):844–852. doi: 10.1089/jwh.2012.4121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Honein Margaret A, Gilboa Suzanne M, Broussard Cheryl S. The need for safer medication use in pregnancy. Expert Review of Clinical Pharmacology. 2013;6:453–455. doi: 10.1586/17512433.2013.827401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ko Jean Y, Farr Sherry L, Dietz Patricia M. Barriers in the diagnosis and treatment of depression in women in the USA: where are we now? Neuropsychiatry. 2013;3:1–3. doi: 10.2217/npy.12.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lutwak Nancy, Dill Curt. The Importance of Screening and Treating Depression in All Women. Journal of Women’s Health. 2012;21:12, 1302–1302. doi: 10.1089/jwh.2012.4042. [DOI] [PubMed] [Google Scholar]
- 21.Payne Jennifer L. Depression: Is Pregnancy Protective? Journal of Women’s Health. 2012;21(8):809–810. doi: 10.1089/jwh.2012.3831. [DOI] [PubMed] [Google Scholar]