Introduction
The exact pathophysiology of acute appendicitis is well known, but the existence of chronic appendicitis (CA) appears to be controversial among many physicians. Several case reports and case series from the last two decades have provided supporting evidence that CA, although uncommon, does occur [Mattei et al. 1994; Rao et al. 1998; Mussack et al. 2002]. CA is a rare clinical entity that poses a diagnostic and therapeutic dilemma for clinicians since a majority of patients present with atypical symptoms. The incidence of CA is 1.5% of all cases with a history of acute appendicitis [Shah et al. 2013], and is thought to be secondary to partial and transient obstruction of the appendix [Vanwinter and Beyer, 2004; Shah et al. 2013]. Although not considered a surgical emergency, it is often a missed diagnosis with complications such as perforation or abscess formation [Shah et al. 2013]. computed tomography (CT) scan is considered to be the best test for diagnosis of CA [Shah et al. 2013]. We describe a 39-year-old man with a history of chronic right lower quadrant pain greater than 6 months duration who was found to have CA while undergoing a colonoscopy.
Case report
A 39-year-old male patient with a history of quiescent proctitis presented with 6 months of intermittent sharp stabbing right lower quadrant pain. The patient reported the pain to be intermittent, “7/10” in severity, sharp in nature, nonradiating, and located mainly in the right lower quadrant with no aggravating or relieving factors. The pain lasted for 6–12 h, sometimes associated with nausea and chills. He was seen in multiple emergency rooms, typically 24–48 h after each episode. He underwent three CT scans without an identifiable source; his blood work and urine studies were normal. Each episode resolved spontaneously after 3–4 days with conservative measures.
The patient then underwent a colonoscopy for his abdominal pain. At the time the patient was in mild distress secondary to pain. The abdomen was soft with moderate tenderness in the right lower quadrant without guarding. The bowel sounds were normal, and no masses were palpable. During colonoscopy, pus was seen to emanate from the appendiceal orifice (Figure 1) with a mild left-sided colitis. The patient was referred to the nearest emergency department for CT of the abdomen and pelvis that demonstrated minimal inflammatory stranding of the periappendiceal fat and thickening of the mid-portion of the appendix (up to 11 mm) compatible with CA (Figures 2 and 3). After a 2-week course of antibiotics, he underwent an uneventful laparoscopic appendectomy. Pathologic evaluation showed the appendix with florid reactive follicular hyperplasia, transmural chronic inflammation with lymphoid aggregates, foci of xanthomatous inflammation, and fibrous obliteration of the lumen, all suggestive of CA without any evidence of Crohn’s disease or malignancy. The patient was seen as an outpatient for 3 months follow up and reported no further attacks of right lower quadrant pain.
Figure 1.
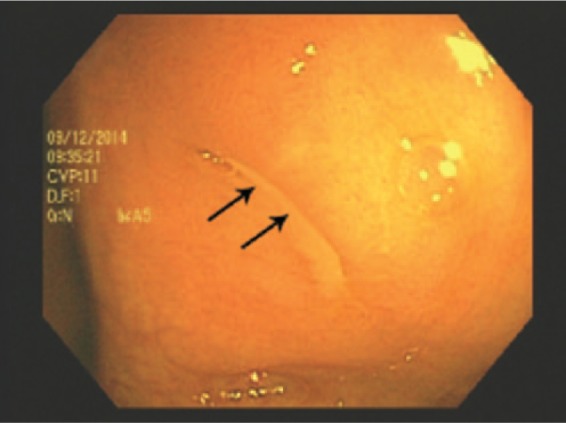
Endoscopic picture of the appendiceal orifice showing oozing pus (arrow).
Figure 2.
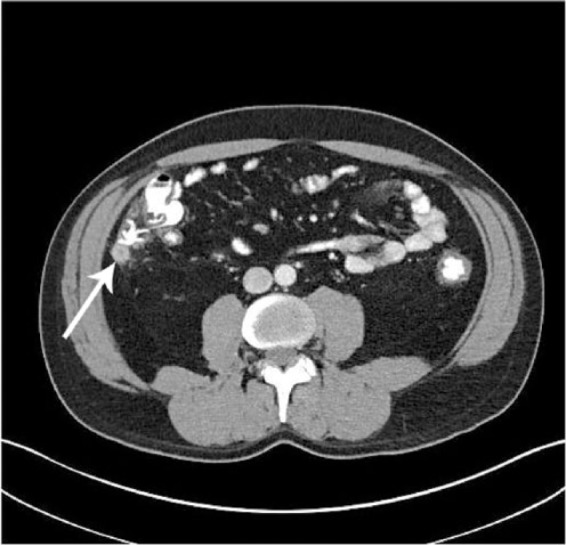
Axial computed tomography scan with contrast of the abdomen demonstrating a thickened and ill-defined appendix (arrow).
Figure 3.

Coronal computed tomography scan with contrast of the abdomen demonstrating a thickened, dilated appendix (arrow) without any abscess, perforation, or fecalith.
Discussion
Although the pathophysiology of acute appendicitis is well understood, the diagnosis and management of CA and recurrent appendicitis remains controversial. The typical presentation of acute appendicitis is characterized by 48 h of periumblical pain localized to the right iliac fossa. It is often associated with nausea, vomiting, anorexia, abdominal guarding, rebound tenderness, and leukocytosis with neutrophil predominance [See et al. 2008; Shah et al. 2013]. Recurrent appendicitis is defined as one or more episodes of acute appendicitis, usually, lasting 24–48 h, and it subsides on its own [See et al. 2008], whereas CA mainly presents as a less severe, nearly continuous abdominal pain lasting longer than the typical 1–2-day period, and often extending to weeks, months, or even years [See et al. 2008].
The precise etiology is unknown. Recurrent appendicitis is thought to occur from transient obstruction of the appendix or secondary to excessive mucus production, while CA is secondary to partial but persistent obstruction of the appendiceal lumen [Mattei et al. 1994; Vanwinter et al. 2004; Shah et al. 2013]. In both cases luminal secretions accumulate until they are subsequently released [Rao et al. 1998]. The causes of intermittent or partial appendiceal obstruction include fecalith, tumors, lymphoid hyperplasia, foreign bodies, and appendiceal folding [Rao et al. 1998; Drezner and Harmon, 2002].
Pathologic findings in acute appendicitis are mucosal hyperemia and ulceration with polymorphonuclear leukocyte infiltration into the luminal wall [Rao et al. 1998]. Partial or complete necrosis or infection of the appendix with or without perforation and/or abscess formation occurs in approximately 10–30% of cases [Rao et al. 1998]. In patients with appendectomy, up to 5% of the specimens show chronic inflammatory changes with infiltration of both lymphocytes and plasma cells into the muscular wall and serosa [Rao et al. 1998]. A case series by Rao and colleagues described chronic inflammation of the appendix noted to have lymphocytic and eosinophilic infiltration, fibrosis and granulomatous reaction, and foreign body giant-cell reaction [Rao et al. 1998]. A very small percentage of patients with CA or recurrent appendicitis show pathologic changes consistent with CA. Thus, there is a possibility of a prolonged subclinical course of appendicitis before patients become symptomatic [Rao et al. 1998]. The significance of fibrous obliteration of the lumen in patients with CA has been controversial. This finding is considered a normal involution of the appendix with age [Mattei et al. 1994]. Mattei and colleagues considered that the fibrous obliteration of the lumen may be secondary to acute inflammation of the appendix that remained subclinical or resolved spontaneously [Mattei et al. 1994].
Imaging that can aid in the diagnosis of CA or recurrent appendicitis includes barium enema, ultrasonography, and CT scan of the abdomen. In the case of acute appendicitis barium enema shows partial filling or nonfilling of the appendicular lumen and indentation of the cecal apex [Rao et al. 1998]. Contrast filling of the appendicular lumen is the most significant criteria for excluding appendicitis. Ultrasonography is used for evaluating patients with suspected appendicitis. It shows a dilated and noncompressible appendix more than 6 mm in diameter with or without associated fecolith and abscess formation [Rao et al. 1998]. There is no consensus regarding sonographic appearance of CA or recurrent appendicitis [Rao et al. 1998]. A CT scan of the abdomen is considered the most accurate imaging modality of choice for diagnosing and excluding appendicitis with an overall accuracy ranging from 93% to 98% [Rao et al. 1998; Babb and Trollope, 1999; Drezner and Harmon, 2002]. Rao and colleagues considered the CT scan finding of CA similar to acute appendicitis [Rao et al. 1998]. The classic CT scan findings in patients with CA include a dilated appendix, periappendiceal fat stranding, appendiceal wall thickening with surrounding edema, calcified appendolith(s), abscess, phlegmon, and inguinal lymphadenopathy [Rao et al. 1998; Mazeh et al. 2009].
Our patient had 6 months history of right lower quadrant pain that remained undiagnosed despite multiple emergency department visits and imaging studies. He was found to have an unusual presentation of pus draining from the appendicular lumen while undergoing a colonoscopy (Figure 1). His surgical pathology findings were consistent with CA.
Unlike acute appendicitis, CA and recurrent appendicitis are not considered a surgical emergency [Shah et al. 2013]. Diagnosis can be missed or delayed secondary to atypical presentation or prior treatment with antibiotics, which may lead to resolution of the infection. A missed diagnosis can have serious complications such as perforation, abscess formation, and peritonitis [Shah et al. 2013].
Conclusion
Although acute appendicitis is the most common disorder affecting the appendix, patients can present with CA or recurrent appendicitis. This rare clinical entity poses a diagnostic and therapeutic dilemma for clinicians with delay in diagnosis. CA or recurrent appendicitis should be considered in the differential diagnosis of the patient with recurrent or chronic right lower quadrant pain. It is of prime importance to review all prior CT scans to evaluate the cause of abdominal pain to reach the correct diagnosis. Appendiceal CT is the best test for diagnosing CA or recurrent appendicitis and appendectomy can be curative.
Footnotes
Conflict of interest statement: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Contributor Information
Jiten P. Kothadia, Department of Internal Medicine, The Brooklyn Hospital Center, Brooklyn, NY, USA
Seymour Katz, Department of Gastroenterology, NYU Langone Medical Center, 1000 Northern Blvd, Suite 140, Great Neck, NY 11021, USA.
Lev Ginzburg, Department of Gastroenterology, NYU Langone Medical Center, Great Neck, NY, USA.
References
- Babb R., Trollope M. (1999) Recurrent appendicitis. Uncommon, but it does occur. Postgrad Med 106: 135–138. [DOI] [PubMed] [Google Scholar]
- Drezner J., Harmon K. (2002) Chronic appendicitis presenting as low back pain in a recreational athlete. Clin J Sport Med 12: 184–186. [DOI] [PubMed] [Google Scholar]
- Mattei P., Sola J., Yeo C. (1994) Chronic and recurrent appendicitis are uncommon entities often misdiagnosed. J Am Coll Surg 178: 385–389. [PubMed] [Google Scholar]
- Mazeh H., Epelboym I., Reinherz J., Greenstein A., Divino C. (2009) Tip appendicitis: clinical implications and management. Am J Surg 197: 211–215. [DOI] [PubMed] [Google Scholar]
- Mussack T., Schmidbauer S., Nerlich A., Schmidt W., Hallfeldt K. (2002) [Chronic appendicitis as an independent clinical entity.] Chirurg 73: 710–715. [DOI] [PubMed] [Google Scholar]
- Rao P., Rhea J., Novelline R., Mccabe C. (1998) The computed tomography appearance of recurrent and chronic appendicitis. Am J Emerg Med 16: 26–33. [DOI] [PubMed] [Google Scholar]
- See T., Watson C., Arends M., Ng C. (2008) Atypical appendicitis: the impact of CT and its management. J Med Imaging Radiat Oncol 52: 140–147. [DOI] [PubMed] [Google Scholar]
- Shah S., Gaffney R., Dykes T., Goldstein J. (2013) Chronic appendicitis: an often forgotten cause of recurrent abdominal pain. Am J Med 126: e7–e8. [DOI] [PubMed] [Google Scholar]
- Vanwinter J., Beyer D. (2004) Chronic appendicitis diagnosed preoperatively as an ovarian dermoid. J Pediatr Adolesc Gynecol 17: 403–406. [DOI] [PubMed] [Google Scholar]


