Abstract
Patients living with diabetes in underserved communities face significant challenges to eating healthy. To support them, we need interventions that integrate community resources into the health care setting. A “prescription” for healthy food may be a promising platform for such a community-linked intervention: it can promote behavior change, provide nutrition education, include financial incentives and connect patients to local resources. We describe Food Rx, a food prescription collaboratively developed by a university research team, Walgreens, a local farmers market, and six health centers on the South Side of Chicago. We share preliminary lessons learned from implementation, highlighting how each stakeholder (university, community partners, and clinics) contributed to this multi-faceted effort while meeting research standards, organizational priorities, and clinic workflow demands. Although implementation is in early stages, Food Rx shows promise as a model for integrating community and health care resources to support the health of underserved patients.
Keywords: diabetes, disparities, nutrition, community, behavioral prescription
Diabetes affects 8.3% of the United States population and disproportionately affects communities of color. In 2010, 18.7% of all non-Hispanic blacks had diabetes, compared to 10.2% of non-Hispanic whites (U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011). Healthy nutritional habits are a key part of diabetes self-management that can help patients control their diabetes and potentially prevent complications. Patients must have strong motivation and clear information to improve their diets, but they must also live in communities where healthy food is affordable and accessible. Thus, effectively addressing diabetes disparities requires a multi-factorial approach to improving dietary practices in racial/ethnic minority communities, with attention to behavioral, educational, environmental and financial barriers to eating healthy. Integrating health care interventions with community resources may be essential to support the health and nutrition of underserved populations (Chin et al., 2012).
One promising community-linked intervention is a “prescription” for diabetes goals and services. The physician’s prescription can serve as a powerful tool for motivating behavior change (Philips, Longoria, Calhoun, & Bates, 1989), in that it can prompt physicians and patients to discuss behavioral change (Fuscaldo, 2002),set realistic goals and/or make behavioral contracts (Hinchman, Beno, Dennison, & Trowbridge, 2005). A prescription can refer patients to particular community services that support the recommended behavior (Leijon, Bendtsen, Nilsen, Ekberg, & Stahle, 2008). While studies document prescriptions for exercise (Kelleher, 1991), we are unaware of any published studies describing a prescription for healthy eating.
Our team designed a “food prescription” to connect health care and community food resources for diabetes patients as a part of a larger project to reduce disparities in diabetes on the South Side of Chicago (Peek et al., 2012). The South Side of Chicago is a predominantly working-class African-American community that bears a disproportionately high rate of diabetes compared to the rest of the city. For example, the rate of diabetes-related deaths from 2004-2008 was 101.6 per 100,000 in Englewood, a neighborhood on the South Side, and 35.8 in Lakeview, a predominantly non-Hispanic white neighborhood on the North Side of Chicago (City of Chicago, 2012). As a region that includes food deserts, there are few local grocery stores, and the limited produce available may not be affordable for residents (Mari Gallagher Research and Consulting Group, 2011). Together with six health centers, Walgreens, and a local farmers market, we designed Food Rx, a prescription program for healthy eating.
With Food Rx, we aimed to leverage the physician’s prescription to encourage behavior change, provide nutrition education, link patients to community resources, and reduce financial barriers to healthy eating. Other studies have combined community resources, nutrition education and financial incentives; these methods show promise (Freedman, Bell, & Collins, 2011). However, to our knowledge this is the first study describing the use of a prescription to promote community food resources as part of a diabetes treatment plan.
In this paper, we describe the development of the Food Rx program as well as preliminary lessons learned from its implementation. The goal of this paper is to provide guidance for others building innovative linkages between universities, community partners, and health care clinics, while highlighting how food prescriptions may be a promising intervention for such partners to pursue together.
Aligning Partners and Their Priorities
Walgreens
Walgreens has many locations on the South Side of Chicago, and in 2010 we contacted them to learn about discounts and services they might offer to diabetes patients. The company agreed to help pilot a food prescription on the South Side as part of their effort to expand their role in health care beyond the traditional retail pharmacy model. Twenty-one of their stores on the South Side had expanded to include “take-care clinics” providing wellness services, treatment of minor illnesses, and basic disease management. Walgreens pharmacists’ had been given time to volunteer in hospitals and health centers, and many stores had hired customer service representatives to help visitors find health products and to encourage them to speak with pharmacists. Several of the pharmacists had also been trained as certified diabetes educators. Finally, Walgreens was adding fresh fruit and vegetable sales and other healthy food offerings (e.g. olive oil and whole grain bread), prioritizing food desert areas. As of December 2012, 19 stores on the South Side had expanded grocery. Walgreens representatives noted that because the Food Rx program aligned with their business interests of increasing customers, the potential for program sustainability was greatly enhanced.
Walgreens was willing to support a food prescription in several ways. Walgreens could cover the cost of coupons associated with Food Rx, and the research team could choose participating stores close to the clinics. Walgreens could train staff to help patients find the foods promoted by Food Rx, offer them diabetes resources, and collect the Rx for evaluation. Finally, Walgreens was able to provide data on what was purchased when the coupon was redeemed.
The Farmers Market
Several members of the research team who live on the South Side of Chicago were familiar with a local farmers market run by a nonprofit organization called Experimental Station. In 2011, this market contacted the research team to discuss partnering on a nutrition program, and we began conversations about piloting Food Rx simultaneously with the Walgreens program. By piloting at both sites, we could streamline design and implementation at the clinics, while exploring patient preferences regarding these two, very different food options in the community.
The Farmers Market is hosted weekly eight months of the year, for a total of 32 market days, and regularly draws 600-650 customers per market day (D. Burke, personal communication, November 16, 2012). The Market has strong commitment to their underserved customers. In 2009, they were the first farmers market in Illinois to pilot doubling the value of LINK (local food stamps). Community members could buy $50 of fresh produce for $25 of LINK (Experimental Station, 2009). From 2008 to 2012, LINK sales grew by 1182%. In 2011 the Market distributed $7,000 to match LINK purchases (D. Burke, personal communication, November 16, 2012). The Market also offers cooking demonstrations and nutrition presentations.
Experimental Station was interested in attracting new customers from the South Side and raising awareness about their LINK program. While the Market was unable to cover the cost of a coupon, they were enthusiastic about Food Rx. The Market committed to training their farmers to use the Food Rx voucher. In addition, the farmers and organizers of the Market could help our team host tours of the Market to orient new customers to the market and any unfamiliar produce. Our team agreed to cover the cost of a pilot voucher for the Market using research funds.
Participating health centers
The six health centers in our diabetes collaborative were enthusiastic about Food Rx. The clinics all serve a large proportion of African American patients and collectively care for approximately 10,000 diabetes patients (Table 1). At all sites, many patients struggle to control their diabetes. Between 43% and 67% of them are not well controlled (hemoglobin A1c>7%).
TABLE 1.
Characteristics of the Participating Clinics
| CLINIC | A | B | C | D | E | F |
|---|---|---|---|---|---|---|
| Total patients | 27,126 | 9,605 | 2,468 | 3,440 | 12,029 | 7,692 |
| % o African American | 65.2% | 42.5% | 91.0% | 89.0% | 38.1% | 89.2% |
| % Medicaid | 7.2% | 5.9% | 59.0% | 60.0% | 43.7% | 57.1% |
| Diabetes patients (%) | 4,831 (17.8%) | 3,281 (34.2%) | 218 (8.8%) | 364 (10.6%) | 883 (7.3%) | 479 (6.2%) |
Throughout our conversations with Walgreens and the Farmers Market, we solicited input from the health center teams. They expressed concerns about collaborating with a corporation, so we consulted institutional policies and avoided corporate branded materials. In addition, there were extensive conversations between the University of Chicago and Walgreens legal teams to create a data sharing agreement that would protect patient information while supporting our research. Finally, clinic teams questioned whether Food Rx had to be limited to diabetes patients; it seemed unnecessarily restricted, and potentially burdensome for providers to remember such a specific target population. As a result, we offered the program to all patients in need of healthy food, while emphasizing patients with diabetes as the primary focus. Overall, the health centers expressed excitement about this partnership.
The Food Rx: Design and Significance
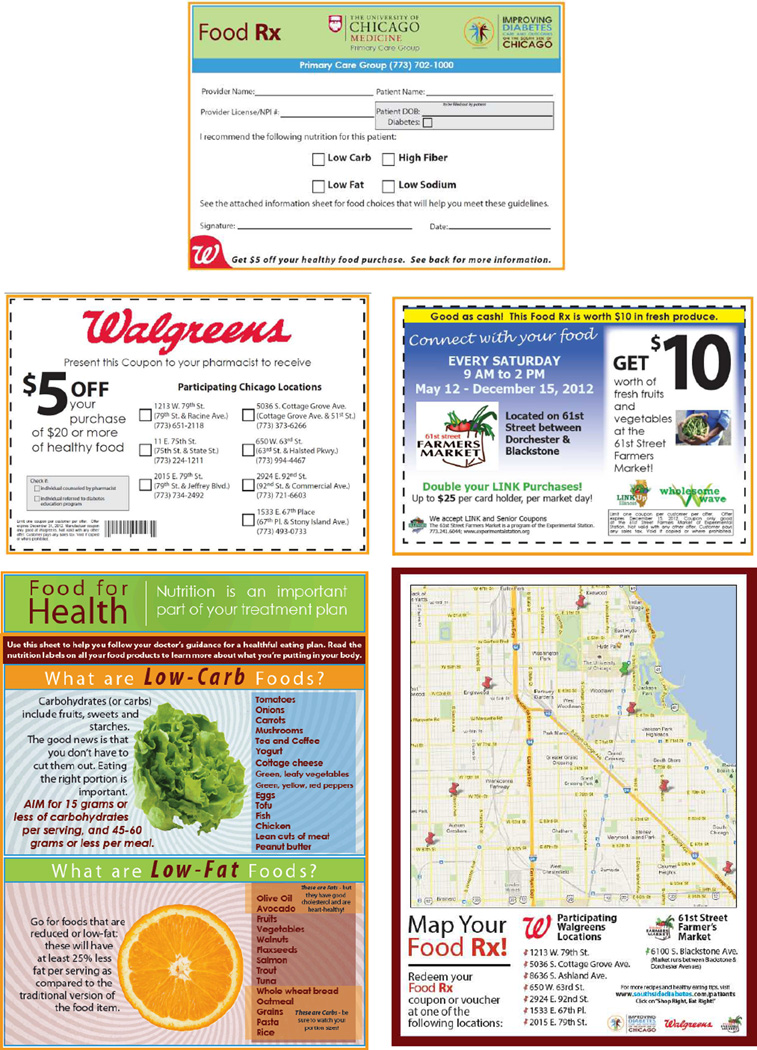
With the input of Walgreens, the Farmers Market, and our health centers, we designed Food Rx to combine a prescription, a coupon, nutrition information and a map (Figure 1). The result is a visually-appealing, low-literacy resource, available at our six health centers, given to patients by their providers during clinic visits, and redeemable at participating Walgreens stores and the Experimental Station Farmers Market. The front of the colorful Food Rx contains a doctor’s prescription for healthful eating, while the back serves as a coupon for either Walgreens or the Farmers Market. Included are guidelines and examples to fulfill the recommendation (e.g. good choices for a low-fat diet), and a map of the South Side of Chicago, which labels where the coupon can be redeemed. This design represents a four-prong approach to the Food Rx program:
FIGURE 1.
From left to right, starting at top: front of Food Rx; back of Walgreens Food Rx; back of Farmers Market Food Rx; front side of the educational handout with guidelines and healthy food examples; map of the South Side of Chicago labeled with participating Walgreens stores and Farmers Market.
Prong 1: Highlighting “The Doctor’s Orders”
A major goal of Food Rx is to leverage the symbolic nature of the prescription, to communicate that healthy eating is “doctor’s orders,” part of a treatment plan. To that end, we designed Food Rx to resemble a common prescription pad. The Rx reads “I recommend the following nutrition for my patient,” followed by checkboxes for low-carbohydrate, low-fat, high fiber, and low sodium. These choices can easily be accomplished at Walgreens and the Farmers Market. We require providers to sign the Rx and note their license number and patient information (Figure 1). We formalized the prescription to stress the importance of the recommendation, prompt nutrition-related conversations, and thus encourage behavior change.
Prong 2: Providing a Coupon for Healthy Purchases
For many of our patients, there are financial and geographic barriers to purchasing healthy food. We highlight local affordable options and incentivize patients to try them. The back of the Rx is a coupon to Walgreens (worth $5 off a $20 purchase) or a voucher for the Farmers Market (worth $10, no matter what the purchase value).
The Food Rx highlights financial programs that can help residents afford healthy food. The Farmers Market voucher advertises that they double LINK (food stamps). The Walgreens coupon highlights that Supplemental Nutrition Assistance Program (SNAP) and Supplemental Nutrition Assistance Program for Women, Infants and Children (WIC) are accepted. While the coupon and voucher do not per se resolve long-term financial barriers, they incentivize patients to visit the organizations and learn about the ongoing financial support they can provide.
Prong 3: Raising Awareness of Local Resources
The third component of our approach is raising awareness of resources on the South Side. Many patients—and providers—are not aware that local Walgreens stores were expanded to include fresh produce, or that a farmers market operates in the neighborhood. Additionally, both Walgreens and the Farmers Market offer educational resources. For example, Walgreens hosts diabetes classes, and some pharmacists are certified diabetes educators. Patients visiting the Farmers Market can watch a cooking demonstration or visit a health education table. By raising awareness of local healthy food options, we support reconceptualizing the South Side as a community that can offer health and wellness resources for its residents.
Prong 4: Providing Education to Patients
Food Rx also includes a handout illustrating how to follow the recipient’s doctor’s recommendation. The handout explains what foods and goals are important and provides guidelines (e.g.“Aim for 45-60 grams of carbohydrates per meal” and “Careful! No salt added means no salt added during processing; it does not necessarily mean sodium-free”) and examples (tuna and vegetables as low-fat, avocado and beans as high-fiber) for each recommendation on the Rx. The handout is also a tool for shopping. It is one-page and printed on cardstock. It employs simple language and includes common grocery items. Including this handout with the Rx ensures that patients who do not redeem the coupon receive information about healthy eating.
Implementation Plan
At the clinics, we train providers to use Food Rx--we present the program at meetings and distribute examples of the Rx materials. In four of our six clinics, provider workrooms are stocked with clear shelves holding the Food Rx, which serve as visual reminders to prescribe the Rx. The other two health centers, given their clinic flow, placed the Rx in or just outside of the exam rooms. Every few weeks our team stops by to restock the shelves, remind providers to use the Rx and collect feedback. At one clinic, medical assistants also have access to Food Rx and give it to providers when they see diabetes patients who may be good candidates for the program. Walgreens and the Farmers Market trained their teams to recognize Food Rx and direct patients to other resources at their sites. To understand the impact of Food Rx, Walgreens and the Market collect de-identified information on each coupon and return these data to research staff.
Early Results and Lessons Learned
Comparing Healthy Options: Walgreens vs. Local Grocers
We formally compared the healthy food at Walgreens with the healthy food at grocers on the South Side. We used the Nutrition Environment Measures Survey in Stores (NEMS-S), a valid and reliable measure of nutrition environments (Glanz, Sallis, Saelens, & Frank, 2007). NEMS-S compares availability, price, and quality of healthy food options. The survey includes ten measures, but we only used the five measures that evaluate food included in the Food Rx educational handout: milk, fruit, vegetables, lean meat, and bread. The measures are objective (e.g. comparing inches of shelf space for skim vs. whole milk), except for rating the “acceptability” versus “unacceptability” of fruit/vegetable quality, for which explicit criteria are given (e.g. presence of a bruise or mold).
Two researchers completed the NEMS-S survey at our nine participating Walgreens stores as well as South Side store locations of three local grocers. These included two different low-cost grocers common to the South Side and a standard commercial grocer with branches throughout Chicago. We did not include the Farmers Market because it does not carry several items in NEMS-S (e.g. milk).
On average, the Walgreens stores had less variety of healthy options available than local grocers (Table 2). However, the Walgreens stores had at least one healthy option in all but one category of food (lean meat). Despite having fewer options, the prices of these healthy options items relative to standard options were comparable and sometimes better than at local grocers. The quality of the healthy food available was essentially the same at Walgreens and the grocers.
TABLE 2.
Rating the Availability, Price, and Quality of Healthy Food Options at Walgreens vs. Low-Cost and Commercial Grocers on the South Side of Chicago1
| Availability of Healthy Options2 | Price of Healthy Options3 | Quality of Healthy Options4 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Walgreens5 | Low-cost Grocers6 |
Commercial Grocer |
Score range (worst-best) |
Walgreens | Low-cost Grocers |
Commercial Grocer |
Score range (worst-best) |
Walgreens | Low-cost Grocers |
Commercial Grocer |
Score range (worst-best) |
|
| Milk | 2.9 | 1.5 | 3.0 | 0–3 | 1.0 | 1.0 | 2.0 | 0–2 | * | * | * | * |
| Fruit | 1.9 | 2.5 | 3.0 | 0–3 | * | * | * | * | 2.9 | 3.0 | 3.0 | 0–3 |
| Veg | 1.8 | 2.5 | 3.0 | 0–3 | * | * | * | * | 3.0 | 3.0 | 3.0 | 0–3 |
| Beef | 0.0 | 3.0 | 3.0 | 0–4 | 0.0 | −1.0 | −1.0 | −1–2 | * | * | * | * |
| Bread | 2.1 | 2.0 | 3.0 | 0–3 | −0.1 | −0.5 | −1.0 | −1–2 | * | * | * | * |
| Total | 8.7 | 11.5 | 15.0 | 0–16 | 0.9 | −0.5 | 0.0 | −2–6 | 5.9 | 6.0 | 6.0 | 0–6 |
NEMS-S survey does not include this measure for this item.
Scores are generated by a series of validated survey measures (Glanz, Sallis, Saelens, & Frank, 2007) to describe healthy food options as compared to standard food options.
Availability refers to whether healthy options are available and if so, how many varieties there are. For example, 2 points are awarded if any whole grain bread is available, and an additional 1 point is awarded if there are more than two varieties.
Price refers to the cost of healthy options as compared to standard options. For example, a higher score in price of milk means skim milk had a better price, i.e. priced the same or lower, as compared to whole milk. A negative score in price of beef denotes that lean meat had a worse price, i.e. was more expensive, than standard options.
Quality refers to whether produce was rated as “acceptable” (good color, firm) or “not acceptable” (e.g. overripe, bruised, or molding).
Average of nine participating stores.
Average of two low-cost grocers visited.
To further formally evaluate the Food Rx program, our next step will be to identify purchasing trends among our patients via redemption data and qualitatively explore food preferences via in-depth interviews. In the interim, we have regular calls and/or in-person check-ins with the clinics, Walgreens, and Farmers Market. We save all anecdotal feedback (e.g. emails, re-stock requests) and regularly speak with team representatives for real-time, on-the-ground issues or suggestions.
Lessons Learned
Integrating Food Rx into the healthcare setting is challenging but may be powerful
When we introduced Food Rx to clinic staff, providers were almost uniformly enthusiastic about the program. Nevertheless, many providers forget to offer Food Rx to their patients. We tried to address this problem via the placement and design of the Food Rx shelves as well as regular check-ins and email updates. Involving clinic members other than physicians may be helpful. For example, medical assistants and/or nurses may help with Food Rx dissemination by reminding patients to ask about them or providing Food Rx to physicians when diabetes patients arrive, thereby incorporating Food Rx into workflow patterns. However, not all diabetes patients may be appropriate recipients of Food Rx and they may be unlikely to use them. Other staff, such as dieticians, are enthusiastic about the program but currently unable to prescribe Food Rx without a physician’s signature (because we track use of the Rx by provider license number). In a future program iteration, in which evaluating exact usage patterns is not a priority, making Food Rx available to all clinic staff may increase distribution rates.
Secondly, some providers do not remember that the program is targeted for patients with diabetes who live on the South Side of Chicago and face food security challenges. They have sometimes encouraged patients who are inappropriate for the program to redeem a Food Rx. After initial implementation, we began to encourage providers to ask a screening question to determine if a patient would benefit from Food Rx: “Do you ever have trouble making your co-pay, or have difficulty accessing/affording healthy foods?” (Hager et al., 2010). The map of the South Side of Chicago serves as an additional reminder of the program’s catchment area.
Providers who have used Food Rx report very positive experiences: they are grateful for a resource to effectively address barriers to healthy eating. One physician wrote in an email: “Gave Food Rx to a patient today […] it’s so empowering to actually be able to help people when they self-identify financial barriers to healthier eating.” Another wrote: “Awesome program. Thanks for putting it together and promoting.”After the value of the Market voucher increased, one nurse practitioner emailed to say, “I use these all the time. We will need a lot!”
The value of the Rx and proximity of redemption sites are likely strong determinants of its use
We have collected anecdotal evidence that patients are happy to receive Food Rx. One nurse practitioner reported, “The farmers market coupons are being very well received by our patients. They really appreciate this help.” A physician emailed to say: “Quite a few of my patients have commented on how useful the information is.”
Ultimately, however, the value and convenience of Food Rx seem to strongly influence whether patients are motivated to redeem it. Many patients were dismayed that the Walgreens coupon required a $20 purchase; as a result, we are exploring with Walgreens a two-option coupon for $3 off a $10 purchase or $5 off a $20 purchase. At the Farmers Market, the voucher was originally worth $3 and did not seem to adequately incentivize new patients to visit the market; the voucher may also have been confused with other $1 vouchers distributed by the market. We increased the voucher to $10 and have started to see an increase in redemption rates..
In addition, the convenience of the store and market locations seems to be important. We prioritized including Walgreens stores that are close to the participating clinics and where their patients often fill pharmacy prescriptions. We also chose stores spread throughout the South Side region. Nevertheless, many patients shop at Walgreens locations that are closer to their homes but not yet expanded to serve fresh produce and thus not included in Food Rx. For these patients, the coupon value may not be enough to motivate shopping at a less convenient store.
Participating in Food Rx may have brought positive culture changes to community partners
Regardless of how many Food Rx are redeemed, developing this program in collaboration with Walgreens and the Farmers Market may have brought positive cultural changes and resources to their organizations. For example, staff trained at Walgreens to find options listed on the Food Rx are now more aware of the healthy food that their store stocks. At the Market, farmers are now familiar with nutrition-oriented tours that our team regularly leads for patients redeeming an Rx. Both of these examples suggest that Food Rx offers an opportunity to change the manner in which food retailers interact with customers who struggle with diet-related diseases.
A small and diverse coordinating team is key
Because the coordinating team included academic researchers, practicing physicians, and community experts from the South Side, we were able to anticipate and troubleshoot competing needs and priorities. For example, what would physicians find burdensome during the clinical encounter? What data were necessary to evaluate the program with methodological rigor? How could we best highlight the strengths of our community partners? Additionally, the diverse team helped balance standardizing the intervention with adapting components to each clinic’s needs. Finally, because our team represented six clinics (several of which are in networks), we could leverage a large patient population in negotiations about coupon value.
University-community food partnerships can accommodate research methodology
We co-developed a project balancing the priorities and needs of our community partners with the research goals and requirements of our university team. Because Walgreens and the Farmers Market were willing to collect data on the redeemed Food Rx, we worked with de-identified data and avoided burdening patients with a consent form to redeem the coupon, which would also further complicate clinic workflow. The university Institutional Review Board helped to design a process whereby patient information is protected but available for use in the study and feasible to collect with community partners.
Future plans for the Food Rx program
We will formally evaluate the Food Rx program via: 1) in-depth interviews with patients and providers to discuss their experience of the program; and 2) quantitative data on the demographics and purchasing patterns of patients who redeemed the Food Rx. These data will inform program development, and there are already several promising ideas. First is to expand Food Rx to new sites at both farmers markets and Walgreens. As noted above, finding sites that are convenient for patients (e.g. close to home, or where they already fill pharmacy prescriptions) will be apriority. Additionally, four of our six participating clinics are members of larger clinic networks and all have expressed interest in bringing Food Rx to their other locations in Chicago. Finally, all six clinics utilize electronic medical record (EMR) systems and integrating Food Rx into the EMR may help overcome barriers to provider usage.
Conclusion
Food Rx is a community-university food partnership to promote healthy eating and combat disparities on the South Side of Chicago, a predominantly African American neighborhood with high rates of diabetes. Food Rx leverages a novel platform—the doctor’s prescription—to link the health care setting with local community resources and deliver a targeted multifactorial intervention. Early anecdotal evidence suggests that Food Rx promotes culture change in the health centers and community partners, and that it may meet some needs of our patient population related to accessing, affording, and understanding the importance of healthy food.
This paper is the first to describe a food prescription program. The major limitation to the Food Rx program is that it does not offer long-term financial support for underserved patients. However, Food Rx was designed to highlight existing resources that support healthy eating, both financial and educational. A major strength of our approach is that we were able to meet the demands of research methodological standards, clinic workflows, and organizational priorities of our partners, a major national corporation and a small, local non-profit organization.
The whole was greater than the sum of its parts in our Food Rx program. The work of each partner—the community organizations, the health centers, and the university research team—was bolstered and amplified by the collaboration. And each component of the Food Rx—the prescription, the coupon, the education and the awareness of local resources—was magnified in effect because it was coupled with the others. Health care clinics, universities, and community organizations, both non- and for-profit, all have important roles to play in addressing disparities in diabetes. Collaborative, multifactorial approaches may be essential to promoting the health of underserved communities and reducing disparities in diabetes outcomes (Chin et al., 2012).
Acknowledgments
The authors would like to thank Denise Scarpelli, Danny Burke, and Julie Whyte for their help acquiring data. This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (Grant No. R18 DK083946), the Chicago Center for Diabetes Translation Research (Grant No. P30 DK092949), and the Alliance to Reduce Disparities in Diabetes of the Merck Company Foundation. Marshall Chin is supported by an NIDDK Midcareer Investigator Award in Patient-Oriented Research (Grant No. K24 DK071933). This work has not been published elsewhere and has not been submitted simultaneously for publication elsewhere.
REFERENCES
- City of Chicago. Public Health Statistics--Selected public health indicators by Chicago community area. 2012 [Data file]. Retrieved from https://data.cityofchicago.org/Health-Human-Services/Public-Health-Statistics-Selected-public-health-in/iqnk-2tcu.
- Chin MH, Clarke AR, Nocon RS, Casey AA, Goddu AP, Keesecker NM, Cook SC. A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. Journal of General Internal Medicine. 2012;27:992–1000. doi: 10.1007/s11606-012-2082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Experimental Station. 61st Street Farmers Market doubles LINK purchase value, thanks to Wholesome Wave Foundation. 2009 Sep 16; Retrieved from http://www.experimentalstation.org/node/175.
- Freedman DA, Bell BA, Collins LV. The Veggie Project: a case study of a multi-component farmers' market intervention. Journal of Primary Prevention. 2011;32(3–4):213–224. doi: 10.1007/s10935-011-0245-9. [DOI] [PubMed] [Google Scholar]
- Fuscaldo JM. Prescribing physical activity in primary care. The West Virginia Medical Journal. 2002;98(6):250–253. [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in stores (NEMS-S): development and evaluation. American Journal of Preventive Medicine. 2007;32(4):282–289. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, Frank DA. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–e32. doi: 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- Hinchman J, Beno L, Dennison D, Trowbridge F. Evaluation of a training to improve management of pediatric overweight. The Journal of Continuing Education in the Health Professions. 2005;25(4):259–267. doi: 10.1002/chp.39. [DOI] [PubMed] [Google Scholar]
- Kelleher K. Prescribing exercise for the adult with diabetes. Nurse Practitioner Forum. 1991;2(3):163–165. [PubMed] [Google Scholar]
- Leijon ME, Bendtsen P, Nilsen P, Ekberg K, Stahle A. Physical activity referrals in Swedish primary health care - prescriber and patient characteristics, reasons for prescriptions, and prescribed activities. BMC Health Services Research. 2008;8:201. doi: 10.1186/1472-6963-8-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mari Gallagher Research and Consulting Group. The Chicago Food Desert Progress Report. Chicago, IL: Mari Gallagher; 2011. [Google Scholar]
- Peek ME, Wilkes AE, Roberson TS, Goddu AP, Nocon RS, Tang H, Chin MH. Early lessons from an initiative on Chicago's South Side to reduce disparities in diabetes care and outcomes. Health Affairs. 2012;31(1):177–186. doi: 10.1377/hlthaff.2011.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philips BU, Longoria JM, Calhoun KH, Bates DF. Behavioral prescription writing in smoking cessation counseling: a new use for a familiar tool. Southern Medical Journal. 1989;82(8):946–953. doi: 10.1097/00007611-198908000-00004. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. 2011 Retrieved on April 17, 2013 from http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf.