Abstract
Objective
Motivational Interviewing (MI) consistent talk by a counselor is thought to produce “change talk” in clients. However, it is possible that client resistance to behavior change can produce MI inconsistent counselor behavior.
Methods
We applied a coding scheme which identifies all of the behavioral counseling about a given issue during a visit (“episodes”), assesses patient concordance with the behavioral goal, and labels providers’ counseling style as facilitative or directive, to a corpus of routine outpatient visits by people with HIV. Using a different data set of comparable encounters, we applied the concepts of episode and concordance, and coded using the Motivational Interviewing Treatment Integrity system.
Results
Patient concordance/discordance was not observed to change during any episode. Provider directiveness was strongly associated with patient discordance in the first study, and MI inconsistency was strongly associated with discordance in the second.
Conclusion
Observations that MI-consistent behavior by medical providers is associated with patient change talk or outcomes should be evaluated cautiously, as patient resistance may provoke MI-inconsistency.
Practice Implications
Counseling episodes in routine medical visits are typically too brief for client talk to evolve toward change. Providers with limited training may have particular difficulty maintaining MI consistency with resistant clients.
Keywords: Motivational Interviewing, HIV Care, Behavioral Counseling
Introduction
Motivational Interviewing (MI) is an evidence based method of behavior change counseling, developed in the 1980’s to increase the effectiveness of alcoholism and drug abuse treatment.[1] It has since been applied to many other health-related behaviors including issues commonly addressed in medical practice such as medication adherence, smoking, and diet and weight management.[2] Originally, MI was delivered by highly trained specialist counselors, but recently there has been interest in training general medical practitioners – physicians and nurses -- to use MI techniques in routine practice. [3]
MI is comprised of a relational and a technical component. [4] The relational component consists of empathy, evocation, and empowerment. Empathy refers to the keen interest of the practitioner in the patient’s point of view, normalizes the experience of ambivalence about change, and is operationalized by complex reflective listening skills. Evocation refers to eliciting the patient’s reasons for change, and preferred processes of change. Empowerment serves to support autonomy.
Based on the hypothesis that what patients say during consultations is the best predictor of subsequent behavior change, the technical component of MI refers to the identification, elicitation, and reinforcement of “change talk”, patient utterances that indicate preparation for, and commitment to behavior change. Practitioner verbal behavior can elicit and reinforce patient change talk, countermand, or extinguish it. Patient change talk is often extinguished when the practitioner misses opportunities to reinforce it, or overuses direct persuasion, which tends to elicit commitment to the status quo. It can also be countermanded when practitioners undermine rapport by over-directing the consultation and limiting patient-perceived choice. There is considerable empirical support both for the connection between client change talk and subsequent behavior change, [5], and between MI consistent practitioner behavior and client change talk.[6]
Counselor fidelity to the technical component of MI is evaluated directly through widely used coding instruments, such as the Motivational Interviewing Treatment Integrity code (MITI) [7, 8] and the Motivational Interviewing Skills Code (MISC). [9] These label practitioner verbal behaviors, at the level of the speaker turn. Some are classified as MI consistent, such as asking permission before giving advice, affirming the client, emphasizing the client’s control, and supporting the client with sympathetic statements. MI inconsistent behaviors are advising without permission, confronting, and directing the client – giving orders or instructions. MI practice also encourages the use of “reflections,” in which the practitioner repeats back an interpretation of what the client has said, often with some elaboration or reframing in order to test hypotheses about the client’s feelings or beliefs, reinforce desirable motivations or beliefs, or reframe undesirable motivations to encourage the client to reconsider. These practices are also coded.
There is an extensive evidence base for the effectiveness of MI in behavioral counseling by trained practitioners. However, evaluation of MI techniques in regular medical practice has been more limited. Some studies have found that training providers to use MI in routine medical practice can result in greater practitioner competence in the technique, [10, 11] and other purportedly positive provider behaviors.[12], or that providers feel more competent and comfortable counseling patients after training. [13] A few have linked MI consistent behavior by medical providers to outcomes such as reduced saturated fat intake [14], patients’ self-reported confidence to improve their nutrition [15] and weight loss. [16]
Leading experts argue that MI consistent behavior by the therapist induces change talk, which in turn predicts positive outcomes. [1, 4, 17]. Indeed, it has been observed that MI consistent verbal behaviors by therapists are more likely to be immediately succeeded by client change talk than are MI inconsistent or other behaviors [6, 18]. On the other hand, client resistance to change has been found to produce more confrontational, MI inconsistent behaviors by practitioners with varying degrees of prior MI training (specifically, 56.3% reported having an unspecified amount of previous MI training) [19].
Here we present empirical data addressing the relationship between patient concordance with provider behavioral change goals and measured MI consistency from two studies of the primary care of people with HIV. In the first study, the Physicians as Counselors coding system (PaCCS) was developed and tested, and provided preliminary support for the hypothesis that patient-provider concordance on behavior change was associated with greater MI consistency. In the second study, ECHO3 (Enhancing Communication for HIV Outcomes, the third in a series of related studies) we tested this hypothesis in a larger, independent sample, using coding more specific to MI consistency. We conducted these analyses because it is important to understand the extent to which MI consistency is a cause, or an effect, of patient change talk.
Methods
PaCCS Study
We coded a corpus of transcribed routine outpatient encounters in HIV care, taken from two previous studies [20, 21]. The material had already been coded using the Generalized Medical Interaction Analysis System,[22] which divides the dialogue into units based on Speech Act Theory [23, 24], and labels each utterance according to the social act it embodies such as various forms of questioning, giving information, expressing desires or opinions, giving instructions, and others.
The Physicians as Counselors coding system (PaCCS) [25] was designed to be relatively easy to implement with clinical encounters. Because the providers in these data were not generally trained in MI or any other specific method of behavioral counseling, we did not try to assess fidelity to specific technical components of MI. In fact the providers rarely used techniques such as reflection, or asking permission to advise. Since the HIV specialists also genereally served as the patients’ primary care providers, many health related behaviors were discussed, including adherence to antiretrovirals and other medications, smoking, alcohol use, other drug use, safe sex, and diet and weight management.
A segment of text is not coded if the patient is reliably performing a positive health behavior, in other words we did not code prophylactic advice-giving or positive reinforcement. Counseling starts when it becomes clear that there is an issue with the patient’s behavior that conflicts with standard medical advice, whether the patient brings it up spontaneously or the physician inquires about it.
We define an “episode” as all discussion of a given targeted behavior change within a single medical encounter, regardless of whether all of the discussion is contiguous. The system labels each episode with the targeted behavior, e.g. smoking. Then it assigns three additional levels of coding, called concordance, counseling style, and counseling technique.
In concordant interactions, the patient shows positive engagement with the behavior change goal. This sentiment is clear through expressive statements of the desire to change. Interactions are coded as discordant if the patient appears to be neutral, avoidant, or resistant to the targeted behavior change. If the patient’s position is unclear, the interaction is coded as discordant. A patient may be concordant with regard to behavior change in one subject and discordant with regard to another. In principle a patient may switch from concordant to discordant or vice versa during the interaction.
The second level of coding indicates the overall approach taken by the provider in behavioral counseling. Interactions are classified as either directive or facilitative. In directive interactions, the provider does not seek patient input, but independently generates advice or instructions about how the patient should modify a behavior. In a facilitative approach, in contrast, the provider is responsive to patient input, such as expressed goals or problem solving strategies. (The provider may or may not actively elicit patient input.) There is shared decision making or problem solving in response to a patient’s expressive need. Additional coding which describes specific strategies employed by the provider is not used in this analysis.
Intercoder reliability
To assess reliability, 5 cases were coded independently by 2 different coders. Twelve behavior change counseling episodes were identified within the 5 cases by both coders. Three behavior change counseling episodes were identified by one coder but not the other. Of these, 1 consisted of only 2 utterances (advice to stop smoking), and another of 8; only one (identified as a discussion of weight management by the single coder) was substantial, consisting of 24 utterances. The disagreement is whether this constituted behavioral counseling, or was purely informational. Of the twelve episodes identified by both coders, agreement on the included utterances was above 95% in 11, and 80% in one. Agreement on whether episodes were concordant or discordant, and facilitative or directive, was perfect for the 12 episodes. We considered this sufficient for a preliminary test of the concepts.
Analyses
We cross-tabulated episodes by concordance/discordance and facilitativeness/directiveness, and used the chi square test of significance. Differences in speech act patterns by concordance/discordance and facilitativeness/directiveness were assessed using the Wilcoxon signed rank test. Speech act patterns hypothesized to be associated with facilitativeness included provider use of open questions, and a lower ratio of provider to patient utterances.
ECHO 3 Study
ECHO3 is a separate pilot study to assess the feasibility of training HIV outpatient care providers in motivational interviewing techniques, compare different levels of intensity of training, and observe effects on provider verbal behaviors. The study was not intended to measure actual behavioral outcomes for patients.
The study took place at a hospital-based HIV outpatient clinic in an east coast city. It was approved by the Institutional Review Board at the study site, and at the institution of the collaborating investigators. All participating providers, patients, and individuals accompanying patients gave written informed consent to participate.
Twelve providers were enrolled in the study and scheduled to participate in a one-day training in MI techniques provided by one of the authors (GR). Prior to the workshop, each participant was intended to have 8 routine outpatient visits audiorecorded using inconspicuous portable equipment, although one ultimately had 9 recorded and one only had 5. Eleven of the twelve providers were able to attend the workshop (one had a personal emergency and was dropped from the study). Following the workshop, the remaining providers were randomly assigned to two arms. One group received no further training (the ”brief intervention” arm). The other group (”intensive intervention”) had subsequent routine visits recorded for training (not research) purposes. These visits were quickly transcribed and the trainer received copies of the recordings and transcripts. He then provided coaching to the providers, via telephone and e-mail. Feedback focused on the consistency of the practitioner’s interview style with the spirit and techniques of MI. Coaching sessions were tailored to the individual provider and continued until the trainer judged that the provider had made good progress or was no longer improving. The number of visits on which providers received feedback ranged from 3–5.
Providers in the brief intervention group had 8 additional visits recorded for research purposes during the 4-month period after the workshop. Finally, all providers had 8 visits audiorecorded 5–6 months after the workshop, although one provider in each study arm left the institution and therefore did not complete follow-up, yielding a total of 206 visits. Two visits were excluded from analysis because people accompanying the patient largely participated on the patient’s behalf, resulting in 204 total visits.
The recordings were transcribed, and the transcripts coded using an adaptation of the Motivational Interviewing Treatment Integrity (MITI) system [8, 26]. The MITI assigns global scales to the encounter capturing the relational component of MI, and also codes for specific provider behaviors, including some which are not specifically encouraged or discouraged in MI, such as giving information and asking questions; and behaviors which are classified as MI adherent or non-adherent. Examples of MI adherent behaviors are ”asking permission before advising,” ”emphasizing the client’s control,” ”supporting the client” with statements of compassion or sympathy.” MI non-adherent behaviors are ”advising without permission,” ”confronting” the client by correcting, shaming, or other derogatory behaviors, and ”directing” the client by giving mandates. The MITI also codes for reflections, which are a specific technique which is encouraged in MI; and distinguishes open and closed questions.
Most of the dialogue in typical medical visits does not consist of behavioral change counseling and cannot meaningfully be MITI coded. For example, physicians give instructions about proper use of medications or other self-care behaviors. This is an expected part of the physician’s role and it would be inappropriate to code it as MI non-adherent. On the other hand, if a patient knows the proper way to follow a medication regimen, but is not doing so because of conflicting motivations, then behavioral counseling could occur and MITI coding would be appropriate.
Consequently, it was first necessary, as in the PaCCS, to identify episodes of behavioral counseling within the visits. As the HIV care providers also generally serve as the patients’ primary care providers in this sample, a variety of targeted behaviors are subjects of counseling episodes and we classified these in a similar way as the PaCCS.
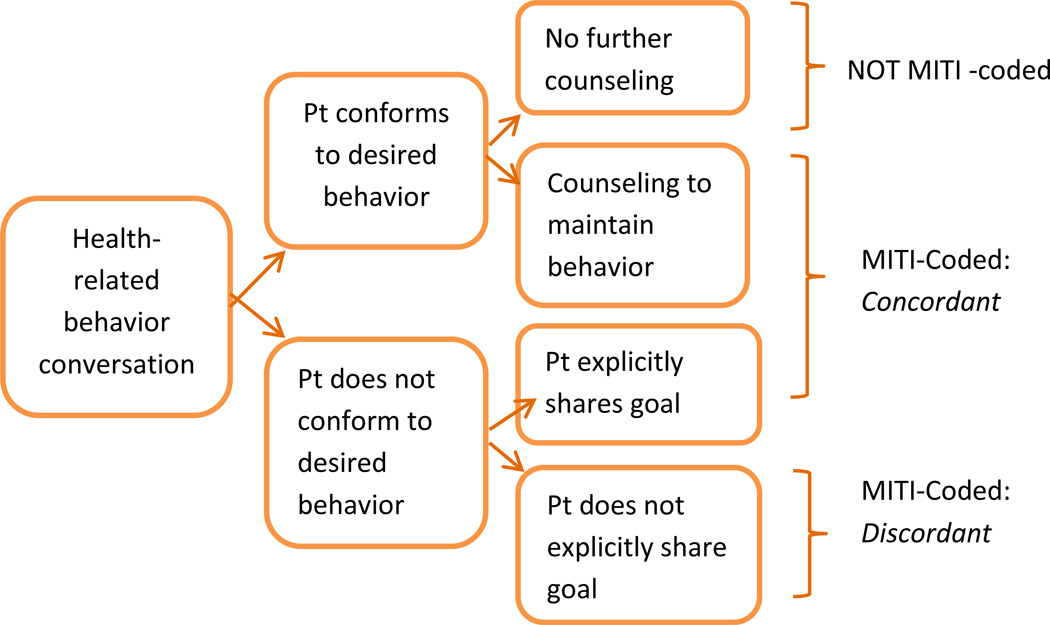
The Figure illustrates the classification of behavior change counseling. When a health-related behavior was discussed, but there was no need for counseling because the client already conformed to the desired behavior and had no problem doing so, it was not considered in this analysis. Cases where the client was not engaging in the desired behavior, or was doing so but received counseling to maintain the behavior (beyond mere affirmation or approval), were included in this analysis and classified as concordant or discordant, consistent with the PaCCS method. Where there was affirmative evidence from the dialogue that the patient shared the behavioral goal, the episode was coded as concordant. Where there was no clear evidence of the patient’s goal or intention, the patient was notably ambivalent, or did not share the behavior change goal, the episode was coded as discordant. Episodes were also MITI coded.
Figure.
Classification and coding of behavior change dialogue
Intercoder reliability
Two coders were trained using tutorials provided by the developers of the MITI, with consultation from experienced MISC/MITI coders. They also consulted with co-author GR to resolve difficulties. After additional work with material drawn from other studies, and preliminarily establishing that they were converging on acceptable reliability, both coded two encounters. The MITI-codable unit of analysis is the speaker turn. The kappa coefficient for agreement that a provider speaker turn constituted behavioral counseling, i.e. that it was MITI codable, was .93 for one visit and agreement was perfect (kappa=1) for the other. In sum, there were only 5 discrepant speaker turns out of a total of 217 in the two visits. In one visit, agreement on MI consistent (MICON) and MI inconsistent (MIIN) codes was 81.2%; in the other, agreement was 72.2%, counting only those episodes in which at least one MICON or MIIN episode occurred, by either coder.
Analyses
Because these count data are highly skewed, we used negative binomial regression to account for the trial arm (brief vs. intensive intervention), and phase (baseline and follow-up), and clustering within providers. We also developed models that did and did not include total provider utterances per episode, to test for any effect of episode length. Because the brief intervention arm included assesment immediately after the workshop, while the intensive intervention arm did not, we developed separate models that did and did not include the intermediate follow-up data. We combined intermediate follow-up with long-term follow-up data to create symmetrical models for all participating providers. Dependent variables are the total number of MI adherent counts per episode, number of MI non-adherent counts per episode (negatively associated with MI fidelity), reflection to question ratio, and the ratio of MI adherent to non-adherent counts per episode. These are all measures of MI fidelity given in the MITI manual. As an additional check of validity, we developed models with total provider questions, and total provider information giving, per episode. These are neutral with respect to MI fidelity and we did not expect them to be associated with concordance.
Results
PaCCS study
We coded 87 encounters, selected at random from the two studies. Of the 38 participating providers, 27 were physicians, 3 were physician assistants, 7 were nurse practitioners, and 1 was a nurse. Their ages ranged from 32–57, with mean age of 45 ± 9 years. 55.3% were female. 65.8% (N=25) of providers in the analysis identified as white/Caucasian, 26.3% (N=10) identified as Asian, 5.3% (N=2) identified as black/African American, and 2.6% (N=1) identified as other.
Of the 87 encounters, 50 (57%) contained at least one episode of behavior change counseling, with a total of 68 episodes. Thirty others contained brief inquiries or other discussion of health risk behavior, but no counseling. The most common behavior change topic was smoking (25 episodes) followed by diet and weight management (18 episodes) and antiretroviral adherence (9 episodes). Less common topics were attendance at appointments, alcohol use, misuse of other drugs, and safe sex practices (2 episodes).
Although the coding system permitted concordance/discordance of a behavior change topic to change within a visit, none did. Compared to typical counseling interventions, most episodes were quite brief; the median consisted of a total of 39.5 utterances, by both provider and patient. Concordance was strongly associated with provider facilitative counseling style. Sixty-two percent (28/45) of concordant episodes were classified as facilitative, compared with 26% (6/23) of discordant episodes (P=0.0048 by Chi Square test, See Table 1).
Table 1.
Results of PACC system coding
| Concordance | Provider Counseling Style | Total | |
|---|---|---|---|
| Directive (N=34) |
Facilitative (N=34) |
||
| Concordant (N=45) |
17 38% |
28 62% |
45 66% |
| Discordant (N=23) |
17 74% |
6 26% |
23 34% |
| Total | 34 50% |
34 50% |
68 100% |
P=.0048
As further tests of validity, we found differences in speech act patterns between concordant and discordant episodes. Note that speech act coding had been done previously, by different coders. These associations were tested post facto. There was a significant association between provider “verbal dominance” (the ratio of provider to patient utterances) and concordance (p=0.0057). In discordant episodes, the median ratio was 1.52 (95% Confidence Interval (CI), 1.16, 2.83), while in concordant episodes, the median ratio was 1.15 (95% CI, 0.82, 1.43). Provider open questions were rare; only 32 episodes (47%) had even one. There was a trend toward more likelihood of the presence of an open questions in facilitative compared with directive episodes (56% vs. 38%, p=.056).
ECHO3 Study
Providers were mostly female (75%), white (75%) and trained as physicians rather than nurse practitioners or physician assistants (75%). Only 2 providers (17%) reported previous exposure to MI training. Fifty-one percent of patients were male and most were African American (88%). Fifty-seven percent had graduated high school.
Four visits had no MITI-coded episodes, leaving a total of 200 encounters in the data. These included a total of 505 episodes for which there was a need for behavioral counseling and concordance could be assessed. However, there were no provider utterances included in 13 of these, in other words the patient asserted a need for behavior change but the provider did not respond with any counseling. In one other episode, there was no MITI coding. This left 491 episodes for analysis, of which 340 (69%) were concordant. Excluding the intermediate follow-up data (present only for the brief intervention group), there were 402 episodes.
Concordance was significantly associated with all four measures MI consistency in all of the models that included only baseline and long-term follow-up data. (See Table 2.) When intermediate follow-up data for the providers in the brief intervention arm was included, the effects were attenuated, resulting in >p=.05 for two of the four measures. (See Table 3.) The MI-neutral behaviors were not associated with concordance in any model.
Table 2.
Models including intermediate follow-up (N=491)
| Total provider questions per episode |
Estimate | SE | Type 3 p- value |
|---|---|---|---|
| Intercept | 0.683 | 0.119 | |
| Arm1 | 0.022 | 0.114 | 0.85 |
| Phase2 | −0.173 | 0.098 | 0.85 |
| Concordance3 | −0.031 | 0.095 | 0.78 |
| Total Dr. utterances/episode | 0.028 | 0.001 | <.0001 |
| Total provider information giving per episode |
Estimate | SE | Type 3 p- value |
| Intercept | −0.168 | 0.088 | |
| Arm1 | −0.237 | 0.111 | 0.033 |
| Phase2 | −0.019 | 0.091 | 0.06 |
| Concordance3 | −0.27 | 0.104 | 0.77 |
| Total Dr. utterances/episode | 0.019 | 0.028 | <.0001 |
| Total MI adherent counts per episode |
Estimate | SE | Type 3 p- value |
| Intercept | −1.604 | 0.207 | |
| Arm1 | −0.309 | 0.198 | 0.017 |
| Phase2 | −0.064 | 0.064 | 0.001 |
| Concordance3 | 1.048 | 0.170 | <.0001 |
| Total Dr. utterances/episode | 0.022 | 0.001 | <.0001 |
| Total MI non-adherent counts per episode |
Estimate | SE | Type 3 p- value |
| Intercept | −0.213 | 0.196 | |
| Arm1 | −0.450 | 0.258 | 0.056 |
| Phase2 | −0.204 | 0.176 | 0.246 |
| Concordance3 | −0.203 | 0.102 | 0.090 |
| Total Dr. utterances/episode | 0.030 | 0.001 | <.0001 |
| Reflection to question ratio | Estimate | SE | Type 3 p- value |
| Intercept | −2.161 | 0.251 | |
| Arm1 | 0.541 | 0.260 | 0.038 |
| Phase2 | 0.377 | 0.234 | 0.107 |
| Concordance3 | 0.340 | 0.012 | 0.012 |
| Total Dr. utterances/episode | 0.008 | 0.002 | 0.000 |
| MI adherent /(MI non- adherent + MI adherent) |
Estimate | SE | Type 3 p- value |
| Intercept | 0.265 | 0.176 | |
| Arm1 | 0.400 | 0.192 | 0.039 |
| Phase2 | 0.262 | 0.119 | 0.028 |
| Concordance3 | 1.038 | 0.162 | <0.001 |
| Total Dr. utterances/episode | −0.003 | 0.002 | 0.083 |
Table 3.
Models excluding intermediate follow-up (N=402)
| Total provider questions per episode |
Estimate | SE | Type 3 p- value |
|---|---|---|---|
| Intercept | 0.630 | 0.132 | |
| Arm1 | 0.051 | 0.112 | 0.667 |
| Phase2 | −0.050 | 0.102 | 0.622 |
| Concordance3 | −0.012 | 0.106 | 0.851 |
| Total Dr. utterances/episode | 0.019 | 0.001 | <.0001 |
| Total provider information giving per episode |
Estimate | SE | Type 3 p- value |
| Intercept | −0.123 | 0.104 | |
| Arm1 | −0.199 | 0.107 | 0.063 |
| Phase2 | −0.196 | 0.100 | 0.049 |
| Concordance3 | −0.099 | 0.126 | 0.430 |
| Total Dr. utterances/episode | 0.028 | 0.002 | <.0001 |
| Total MI adherent counts per episode |
Estimate | SE | Type 3 p- value |
| Intercept | −1.744 | 0.202 | |
| Arm1 | −0.303 | 0.195 | 0.121 |
| Phase2 | −0.211 | 0.081 | 0.009 |
| Concordance3 | 1.253 | 0.195 | <.0001 |
| Total Dr. utterances/episode | 0.021 | 0.001 | <.0001 |
| Total MI non-adherent counts per episode |
Estimate | SE | Type 3 p- value |
| Intercept | −0.193 | 0.183 | |
| Arm1 | −0.513 | 0.221 | 0.020 |
| Phase2 | −0.181 | 0.199 | 0.364 |
| Concordance3 | −0.261 | 0.130 | 0.045 |
| Total Dr. utterances/episode | 0.032 | 0.002 | <.0001 |
| Reflection to question ratio | Estimate | SE | Type 3 p- value |
| Intercept | −2.349 | 0.256 | |
| Arm1 | 0.538 | 0.266 | 0.043 |
| Phase2 | 0.380 | 0.258 | 0.141 |
| Concordance3 | 0.520 | 0.178 | 0.004 |
| Total Dr. utterances/episode | 0.010 | 0.003 | <0.001 |
| MI adherent /(MI non- adherent + MI adherent) |
Estimate | SE | Type 3 p- value |
| Intercept | 0.252 | 0.218 | |
| Arm1 | 0.481 | 0.182 | 0.008 |
| Phase2 | 0.173 | 0.115 | 0.134 |
| Concordance3 | 1.211 | 0.230 | <0.001 |
| Total Dr. utterances/episode | −0.005 | 0.002 | 0.012 |
Discussion
In our first study, we found that coders could reliably isolate episodes of behavioral counseling within medical visits, and reliably label them as concordant or discordant, and as facilitative or directive. We further found that facilitativeness and directiveness were significantly distinguished by certain patterns of speech acts. It may be, of course, that these very features influenced the coders’ judgment about directiveness, but it does support the validity of the distinction. Finally, we found that concordance is strongly associated with facilitativeness.
As facilitativeness but not directiveness is consistent with MI spirit, these findings led us to hypothesize that concordance might also be associated with the technical component of MI in comparable situations. We tested this using a completely separate data set, from a similar clinical setting, i.e. routine outpatient care of people living with HIV. Here, we applied the same concepts of behavioral counseling episodes and concordance/discordance, but applied a widely used method for assessing MI fidelity in place of coders’ global judgment of faciltativeness/ directiveness. We found a strong association between concordance and MI consistency, and that this association persisted even when the providers had some MI training.
These observations support the hypothesis that MI adherence by medical providers is strongly influenced by patients’ expressed concordance with providers’ behavioral goals. This conclusion is intuitively appealing because, obviously, it is much less likely that a provider would confront a patient, or advise without permission, if the patient is cooperative. There would simpy be no opportunity to do so. Conversely, relatively lightly trained providers would seem more likely to use reflections when they are presented with change talk or other positive utterances. Sophisticated MI practitioners will ”dance with discordance,” perhaps reflecting and reframing counterchange talk, for a considerable time, and work gradually to elicit change talk that they can reinforce. Work in progress using GMIAS coding of behavior change counseling visits with trained MI practitioners typically finds 1,500 utterances in a visit (Christopher Kahler, PI). This is sufficient time for client talk to evolve toward change, in accordance with MI theory. This process does not occur in these much briefer counseling episodes within the medical visit. One interpretation is that the practitioners are not skillful enough to avoid being provoked into MI inconsistent behaviors by patients’ normal resistance to change.
It may be that the effect was weaker when we included the short-term follow-up data (collected only from the brief intervention group) because the recent experience of the workshop somewhat innoculated the providers from this effect. (The workshop included role-plays with recalcitrant patients.) If so, the effect apparently faded over the course of a few months.
These findings suggest that observations linking patient change talk in medical visits, and/or subsequent behavioral outcomes, with MI adherence by providers, should be interpreted cautiously. While Pollack et al (2010) [16] in their study of weight loss, did control for patients’ stage of change based on questionnaire data, it is possible that patients’ presentation of concordance during the medical encounter is a more reliable predictor of weight loss than are survey responses. It may also be that patients who presented as concordant during the visit elicited more MI consistent counseling from their providers and that this in turn contributed to subsequent weight loss. Studies of behavioral change counseling by trained MI practitioners have supported the effect of clinician talk in evoking client change talk.[27, 28] However, this may not be as feasible in the context of medical encounters with lightly trained providers. As we noted in the introduction, client resistance has been associated with MI inconsistency previously.[19] A previous observation of the association of change talk with MI consistency in HIV care should be interpreted in light of the possibility of causation in either direction.[29]
This study is limited to HIV care. While it does have a longitudinal component, the experiment which provided the occasion for the data was not related to this hypothesis. An experiment in which concordance is manipulated, either by purposive assignment of patients based on a pre-test, or use of simulated patients, might be more compelling. This is the first time the PACCS, and our adaptation of the MITI, have been used. (Different coders worked on the two studies, which helps establish the reliability of the concordance/discordance distinction.) It is as far as we know unique in defining patient concordance from internal evidence in the dialogue, which is how providers would experience it. Therefore we believe it provides an important caveat to interpretation of evidence concerning the outcomes of MI consistency in brief counseling interactions.
Practice Implications
These finding suggest that medical providers should be mindful that it is more difficult to maintain MI consistency with resistant patients; while this is precisely the situation in which MI technique is posited to be most useful. Training in MI for medical providers should emphasize this point. However, it may be that MI as such is not really applicable to very brief conversations with resistant patients, and that medical encounters require a modified approach.
Highlights.
We coded behavioral counseling in routine outpatient HIV care.
Patient discordance with behavioral goals is associated with physician directiveness.
Patient discordance is associated with Motivational Interviewing (MI) inconsistency.
Counseling episodes are typically brief; evolution of patient talk toward change is not observed.
Association of MI consistency with patient change talk should be interpreted cautiously.
Acknowledgments
This work was supported by the National Institute of Mental Health, grant number 1R34MH089279-01A1. Tatiana Taubin, M.S., supervised MISC coding for the ECHO 3 Study and made important contributions to our adaptation of the system. Sanchita Singhal and Meagan Morse participated in development of the PACCS.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Literature Cited
- 1.Miller W, Rollnick S. Motivational Interviewing: Helping People Change. 3 ed. New York, New York: The Guilford Press; 2012. [Google Scholar]
- 2.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- 3.Soderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns. 2010 doi: 10.1016/j.pec.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 4.Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psychol. 2003;71(5):862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- 6.Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions. J SubstAbuse Treat. 2006;30(3):245–251. doi: 10.1016/j.jsat.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J SubstAbuse Treat. 2005;28(1):19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Pierson HM, Hayes SC, Gifford EV, Roget N, Padilla M, Bissett R, et al. An examination of the Motivational Interviewing Treatment Integrity code. J Subst Abuse Treat. 2007;32(1):11–17. doi: 10.1016/j.jsat.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Moyers TB, Martin T, Catley D, Harris KJ, Ahluwalia JS. Assessing the integrity of motivational interventions: Reliability of the Motivational Interviewing Skills Code. Behav Cogn Psychother. 2003;31:177–184. [Google Scholar]
- 10.Handmaker NS, Hester RK, Delaney HD. Videotaped training in alcohol counseling for obstetric care practitioners: a randomized controlled trial. Obstetrics and gynecology. 1999;93(2):213–218. doi: 10.1016/s0029-7844(98)00377-9. [DOI] [PubMed] [Google Scholar]
- 11.Rubak S, Sandbaek A, Lauritzen T, Borch-Johnsen K, Christensen B. An education and training course in motivational interviewing influence: GPs' professional behaviour--ADDITION Denmark. Br J Gen Pract. 2006;56(527):429–436. [PMC free article] [PubMed] [Google Scholar]
- 12.Saitz R, Sullivan LM, Samet JH. Training Community-Based Clinicians in Screening and Brief Intervention for Substance Abuse Problems: Translating Evidence into Practice. Subst Abus. 2000;21(1):21–31. doi: 10.1080/08897070009511415. [DOI] [PubMed] [Google Scholar]
- 13.Sargeant J, Valli M, Ferrier S, MacLeod H. Lifestyle counseling in primary care: opportunities and challenges for changing practice. Medical teacher. 2008;30(2):185–191. doi: 10.1080/01421590701802281. [DOI] [PubMed] [Google Scholar]
- 14.Brug J, Spikmans F, Aartsen C, Breedveld B, Bes R, Fereira I. Training dietitians in basic motivational interviewing skills results in changes in their counseling style and in lower saturated fat intakes in their patients. J Nutr Educ Behav. 2007;39(1):8–12. doi: 10.1016/j.jneb.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Cox ME, Yancy WS, Jr, Coffman CJ, Ostbye T, Tulsky JA, Alexander SC, et al. Effects of counseling techniques on patients' weight-related attitudes and behaviors in a primary care clinic. Patient Educ Couns. 2011;85(3):363–368. doi: 10.1016/j.pec.2011.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pollak KI, Alexander SC, Coffman CJ, Tulsky JA, Lyna P, Dolor RJ, et al. Physician communication techniques and weight loss in adults: Project CHAT. American journal of preventive medicine. 2010;39(4):321–328. doi: 10.1016/j.amepre.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan JS, Amrhein PC. Client language as a mediator of motivational interviewing efficacy: where is the evidence? Alcohol Clin ExpRes. 2007;31(10 Suppl):40s–47s. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- 18.Gaume J, Gmel G, Faouzi M, Daeppen JB. Counsellor behaviours and patient language during brief motivational interventions: a sequential analysis of speech. Addiction. 2008;103(11):1793–1800. doi: 10.1111/j.1360-0443.2008.02337.x. [DOI] [PubMed] [Google Scholar]
- 19.Francis N, Rollnick S, McCambridge J, Butler C, Lane C, Hood K. When smokers are resistant to change: experimental analysis of the effect of patient resistance on practitioner behaviour. Addiction. 2005;100(8):1175–1182. doi: 10.1111/j.1360-0443.2005.01124.x. [DOI] [PubMed] [Google Scholar]
- 20.Wilson IB, Laws MB, Safren SA, Lee Y, Lu M, Coady W, et al. Provider-focused intervention increases adherence-related dialogue but does not improve antiretroviral therapy adherence in persons with HIV. J Acquir Immune Defic Syndr. 2010;53(3):338–347. doi: 10.1097/QAI.0b013e3181c7a245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beach MC, Saha S, Korthuis PT, Sharp V, Cohn J, Wilson IB, et al. Patient-provider communication differs for black compared to white HIV-infected patients. AIDS Behav. 2011;15(4):805–811. doi: 10.1007/s10461-009-9664-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laws MB, Beach MC, Lee Y, Rogers WH, Saha S, Korthuis PT, et al. Provider-patient Adherence Dialogue in HIV Care: Results of a Multisite Study. AIDS Behav. 2012 doi: 10.1007/s10461-012-0143-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Searle JR. An Essay in the Philosophy of Language. Cambridge University Press; 1969. Speech Acts. [Google Scholar]
- 24.Austin JL. How to Do Things with Words. Oxford University Press; 1962. [Google Scholar]
- 25.Velasco E. Strategies for Effective Behavior Change Discussions in HIV Care. Providence, RI: Brown University; 2012. [Google Scholar]
- 26.Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.0 (MITI 3.0). [Coding manual] 2007 In press. [Google Scholar]
- 27.Glynn LH, Moyers TB. Chasing change talk: the clinician's role in evoking client language about change. J Subst Abuse Treat. 2010;39(1):65–70. doi: 10.1016/j.jsat.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 28.Moyers TB, Martin T, Houck JM, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: a causal chain for motivational interviewing. J Consult Clin Psychol. 2009;77(6):1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flickinger TE, Rose G, Wilson IB, Wolfe H, Saha S, Korthuis PT, et al. Motivational interviewing by HIV care providers is associated with patient intentions to reduce unsafe sexual behavior. Patient education and counseling. 2013;93(1):122–129. doi: 10.1016/j.pec.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]