Abstract
Background
Self-care is an important aspect of managing a chronic disease. In sickle cell disease (SCD), home self-care contributes to individual pain management and thus pain crisis prevention. A better understanding of self-care can help health care providers equip patients with the resources and skills necessary to participate in their disease management.
Aims
To examine factors which influence self-care among young adults with SCD.
Design
A descriptive, cross-sectional study was conducted using secondary data analysis.
Settings
Participants were recruited from two SCD clinics in the southeastern United States.
Participants
The sample consisted of 103 young adults, ages 18–30 years, with SCD.
Methods
Bivariate correlations and regression analyses were used to evaluate the relationships among SCD self-efficacy, social support, socio-demographics, self-care, and hospital visits for pain crises.
Results
Study participants were primarily female (61.2%), unemployed or disabled (68%), lived with family (73.8%), and had an average of three hospital visits for pain crises annually. Participants, on average, had 12 years of education, an annual household income of $35,724, and were 24 years old. Social support (p=.001), SCD self-efficacy (p=.002), and years of education (p=.043) were significantly related to self-care. Of the hypothesized variables, only income was significantly associated with hospital visits for pain crises (r=−.219, p=.05).
Conclusions
Individuals with SCD may benefit from self-care interventions that enhance social support, SCD self-efficacy, and access to education. To inform intervention development, further investigation is needed regarding daily self-care behaviors used by young adults with SCD.
Keywords: pain, sickle cell, self-care, self-efficacy, social support
Background
Sickle cell disease (SCD) is a group of genetic disorders characterized by abnormal hemoglobin molecules, impaired blood flow, decreased oxygen capacity of red blood cells, organ damage, and resultant complications (Olowoyeye & Okwundu, 2010). In the United States, approximately 90,000 to 100,000 individuals have SCD (Centers for Disease Control and Prevention, 2011a). African Americans are primarily affected, with a disease incidence of one in 500 births and the trait or carrier state occurring in one in 12 births. The most common complication of SCD is pain. Pain episodes or crises may occur unpredictably (Fosdal & Wojner-Alexandrov, 2007) and are the most common reason for hospital visits (Yusuf, Atrash, Grosse, Parker, & Grant, 2010). Adults with SCD average over 197,000 emergency department visits annually; 67% of patients report pain as the reason for the emergency department visit and 29% result in hospital admissions (Yusuf et al.), with 90% of the admissions being for the treatment of acute pain (Dunlop & Bennett, 2009). Management of this chronic disease occurs primarily at home and includes a strong emphasis on self-care across the lifespan. The frequency of pain crises and resulting hospitalizations may increase without appropriate self-care in the home setting. Therefore, it is important to understand which factors affect self-care.
Self-care in the home contributes to individual pain management and thus pain crisis prevention, making self-care actions important for enhancing health and well-being. For the purpose of research presented in this article, self-care refers to one’s perceived ability to participate in general therapeutic activities aimed at improving health status and quality of life as well as actual performance of those activities (Jenerette & Murdaugh, 2008). Sickle cell disease management includes focusing on pain, as well as on hydration, and preventing infections and other complications (Lee, Askew, Walker, Stephen, & Robertson-Artwork, 2012). General strategies include receiving regular checkups, staying hydrated, eating a healthy diet, getting adequate rest, and avoiding temperature extremes (Centers for Disease Control and Prevention, 2011b). These general strategies could be considered self-care actions, an important part of pain crisis prevention.
Self-care is a priority, particularly for young adults with SCD. Pain episodes are most frequent between ages 19 and 39 (Yusuf et al., 2010), and health care utilization and re-hospitalization rates are highest between ages 18 and 30 (Brousseau, Owens, Mosso, Panepinto, & Steiner, 2010). Coincidentally, individuals with SCD transition from pediatric to adult care between ages 18 and 25 (Sobota, Neufeld, Sprinz, & Heeney, 2011). They are at a high risk of early death particularly soon after transition, with a mean time of 1.8 years between transfer to adult care and death (Quinn, Rogers, McCavit, & Buchanan, 2010). Young adults lack knowledge about the adult SCD care system, lack financial independence and decision-making experience, and have had a change in or loss of insurance (Jordan, Swerdlow, & Coates, 2013). There is also a shortage of providers with SCD expertise and an interest in serving this population, especially in low income areas (Sobota, Neufeld, Sprinz, & Heeney). Additional constraints include a lack of education and employment or appropriate employment given a lack of educational preparation. Individuals with SCD are likely to be less educated, have lower income, and are more likely to be unemployed or disabled than African Americans without SCD (Laurence, George & Woods, 2006). They may not be able to work or maintain a steady job given poor health and frequent pain crises. All these factors affect the ability of the young adult with SCD to obtain consistent, preventive care, making self-care even more important.
The purpose of this secondary study was to examine the relationships among SCD self-efficacy, social support, socio-demographics, self-care, and hospital visits for pain crises in young, Black adults with SCD. Although the majority of the participants were known to be African American, as 90% of all the SCD patients in the United States are of African descent (American National Red Cross, 2014), their ethnicity was not recorded in the parent study. As a result, participants are categorized in this secondary study by race, Black. The specific aims and hypotheses were as follows:
Aim 1: To evaluate the proposed relationships among SCD self-efficacy, social support, and socio-demographics (age, gender, education, employment status, income, and living situation) in understanding individual differences in self-care (perceived self-care ability and self-care actions).
Hypothesis 1: Greater self-care is associated with higher SCD self-efficacy, greater social support, being employed, living with family or friends, increased age, more years of education, higher income, and male gender.
Aim 2: To evaluate the proposed relationships among SCD self-efficacy, social support, sociodemographics, and self-care in understanding hospital visits for pain crises.
Hypothesis 2: Greater self-care is associated with fewer hospital visits for pain crises.
Aim 3: To evaluate the proposed mediational role of self-care in the relationships among SCD self-efficacy, social support, socio-demographics, and the number of hospital visits for pain crises.
Hypothesis 3: Sickle cell disease self-efficacy, social support, and socio-demographics have both a direct and an indirect relationship with hospital visits for pain crises.
Literature Review
Self-efficacy, social support, socio-demographics, and self-care have been noted as critical concepts associated with the management of SCD and other chronic diseases. According to the Theory of Self-care Management for SCD, self-care resources positively mediate the relationship between vulnerability factors and health outcomes (Jenerette, Brewer, Edwards, Mishel & Gil, 2014). Vulnerability factors (lack of sickle cell crisis cue recognition/response, number of complications, number of acute pain episodes per year, and overprotection) negatively affect self-care resources (self-efficacy, social support, self-care ability, self-care actions, coping behaviors, and assertive communications skills) and thus negatively affect health outcomes (pain management experience, depressive symptoms, self-esteem, and perceived health-related stigma). These self-care resources may assist with the management of daily activities necessary for living with SCD (Jenerette & Murdaugh, 2008).
Self-efficacy links self-perceptions with individual actions, is a mediator of health behaviors, and is considered crucial to chronic disease management (Frei, Svarin, Steurer-Stey & Puhan, 2009). In studies that evaluated chronic conditions, higher levels of self-efficacy were linked to decreased pain severity and fewer self-reported symptoms (Clay & Telfair, 2007) as well as increased used of adaptive coping mechanisms and increased adherence to medical regimens (Edwards, Telfair, Cecil & Lenoci, 2001). Lower levels of self-efficacy were correlated with more symptoms, higher pain severity, and frequent physician visits. In SCD, self-efficacy was negatively correlated with the number of crises per year (Jenerette & Valrie, 2010). In addition, self-efficacy beliefs were inversely related to symptomatology and health care utilization, and these beliefs may predict future changes in SCD symptomatology (Clay & Telfair; Edwards, Telfair, Cecil & Lenoci).
The quality and availability of social support may influence the health outcomes of individuals with chronic disease and may positively affect self-care (Chlebowy & Garvin, 2006). Types of social support include emotional, instrumental, informational, and appraisal support. Support may be obtained from family, friends, work, and the community (Ngamvitroj & Kang, 2007). Patients’ perceptions of satisfaction with this support are important as they have been linked with adherence to medication self-monitoring in individuals with chronic disease. Children with family social support were found to have better disease management behaviors (Sin, Kang & Weaver, 2005). In addition, social support was noted to be helpful in following treatment plans (Cox, 2002; Haynes, McDonald & Garg, 2002; Loeb, Penrod, Falkenstern, Gueldner & Poon, 2003).
Socio-demographics are strong predictors of health related quality of life in individuals with SCD. These predictors include age, sex, income, education, employment, and marital status (Jenerette & Murdaugh, 2008). Panepinto and Bonner (2012) note that health related quality of life (HRQL) in adults with SCD is significantly impaired and may be worse than in other chronic diseases. Variables affecting HRQL in SCD include age, gender, family demographics (education and income), disease-related symptoms, rural versus urban residence, and employment. Age and socio-economic status, for example, negatively affect HRQL. African Americans with SCD were more likely to be less educated, have lower income, and were more likely to be unemployed or disabled when compared to African Americans without SCD (Laurence, George & Woods, 2006). Although males and females are affected equally by SCD (Pack-Mabien & Haynes, 2009), women report higher pain intensity scores, longer crisis episodes, and have a lower median survival than men (Taylor, Stotts, Humphreys, Treadwell & Miaskowski, 2010). These findings may be due in part to routine biological stresses, such as menstruation, on the female body (Samuels-Reid & Scott, 1985). African American women are also more likely to be single heads of households (U.S. Department of Health and Human Services, 2013). Therefore, competing demands of family, work, and/or school may interfere with getting health care needs met (Welch, 2003). There is also some uncertainty as to which socio-demographic variables are most influential in SCD; thus, further investigation is necessary.
Self-care is the ability of an individual with a chronic disease, to participate in a daily, self-motivated, collaborative (conducted with family, social, and healthcare provider support) process to manage symptoms (Schulman-Green et al., 2012). It is important in improving health outcomes, enhancing quality of life, and decreasing healthcare costs (Riegel, Jaarsma & Stromberg, 2012; Ryan & Sawin, 2009). In chronic disease, an individual’s ability to perform behaviors that will alleviate the pain experience is instrumental in adapting to pain long term (Kratz, Molton, Jensen, Ehde & Nielson, 2011). It is important to understand self-care in the context of SCD. General SCD self-care strategies have been identified. In a study assessing strategies used by adults with SCD to manage their disease, themes included self-awareness, emotional support, career selection and success factors, nutrition, advocacy, knowledge, physical activity, and complementary and alternative medicine (Tanabe et al., 2010). In middle-aged and older adults, identified self-care recommendations were physiologic (warmth, hydration, rest, good food, and avoiding drinking, smoking, and using drugs), psychological (knowledge and understanding of the disease, listening to and learning about the body, prayer, and social support), and provider-related (knowledgeable health care providers and following providers’ orders) (Jenerette, Brewer & Leak, 2011). Self-care has many benefits and is correlated with a number of variables, but it is unclear which variable is most influential, particularly in the young adult population. In addition, the relationship between self-care and hospital visits for pain crises needs evaluation.
Methods
Design
This was a descriptive cross-sectional study using secondary analysis. Although the parent study included data from Black adults with SCD ages 18 to73 years, only a subset of the study population, those ages 18 to 30 years, was used for this analysis. A brief summary of the parent study is provided here; see the original study for more details (Jenerette & Murdaugh, 2008).
Parent study
A cross-sectional study of 232 Black patients with SCD was conducted to describe factors predicting quality of life and to test the Theory of Self-Care Management for SCD. Study approvals were obtained from the Institutional Review Boards at the Medical University of South Carolina and the University of North Carolina at Chapel Hill. The study sample included patients, 18 or older, who were recruited from two SCD clinics in the southeastern United States between September 2003 and April 2004. Potential subjects were screened by clinic staff and were excluded if they were not able to read, write, and understand English (Jenerette & Murdaugh, 2008). Those patients who provided informed consent completed study questionnaires with paper and pencil in a designated private area of the clinic. All data were self-report as clinic records were not reviewed.
The following instruments were used to gather data. Evidence of instrument validity and reliability was included in the study report (Jenerette & Murdaugh, 2008). A demographic questionnaire was used to gather information regarding: age, gender, level of education, employment status, zip code (used to estimate annual household income), living situation (alone, with family, or with friends), and number of hospital visits for pain crises annually (Jenerette & Murdaugh). Sickle cell disease self-efficacy, an individual’s perceived ability to function daily and to manage SCD symptoms, was measured using the nine-item Sickle Cell Self-Efficacy Scale. Items are scored on a scale of 1 to 5 (“not at all sure” to “very sure”) and higher total scores indicate higher self-efficacy (Edwards, Telfair, Cecil, & Lenoci, 2001). The perceived availability of social support was measured with the 19-item Medical Outcomes Study Social Support Survey. Items are scored on a scale of 1 to 5 (“none of the time” to “all of the time”) and higher total scores indicate higher perceptions of available support (Sherbourne & Stewart, 1991). Self-care was operationalized as perceived self-care ability and self-care actions. The 24-item Appraisal of Self-Care Agency Scale was used to measure perceived self-care ability; the perceived ability to participate in general therapeutic behaviors aimed at enhancing and/or maintaining health status and quality of life. Items are scored on a scale of 1 to 5 (“totally disagree” to “totally agree”) and higher total scores correspond with higher levels of self-care ability. The eight-item Jenerette Self-care Assessment Tool was used to measure self-care actions; one’s participation in SCD specific therapeutic activities and using resources to enhance health status and quality of life. These actions include knowing about health, understanding medications, taking medications as prescribed, keeping medical appointments, following a recommended diet, staying hydrated, dressing warm, and avoiding stress. Items are scored on a scale of 1 to 4 (“never” to “almost always”) and higher total scores indicate higher self-care actions (Jenerette & Murdaugh). Although one would expect an intrinsic positive correlation among self-efficacy, self-care ability, and self-care actions, each is a distinct concept. For example, belief does not ensure ability or actions. Moreover, having the ability to do something does not ensure the action will be done.
Secondary study
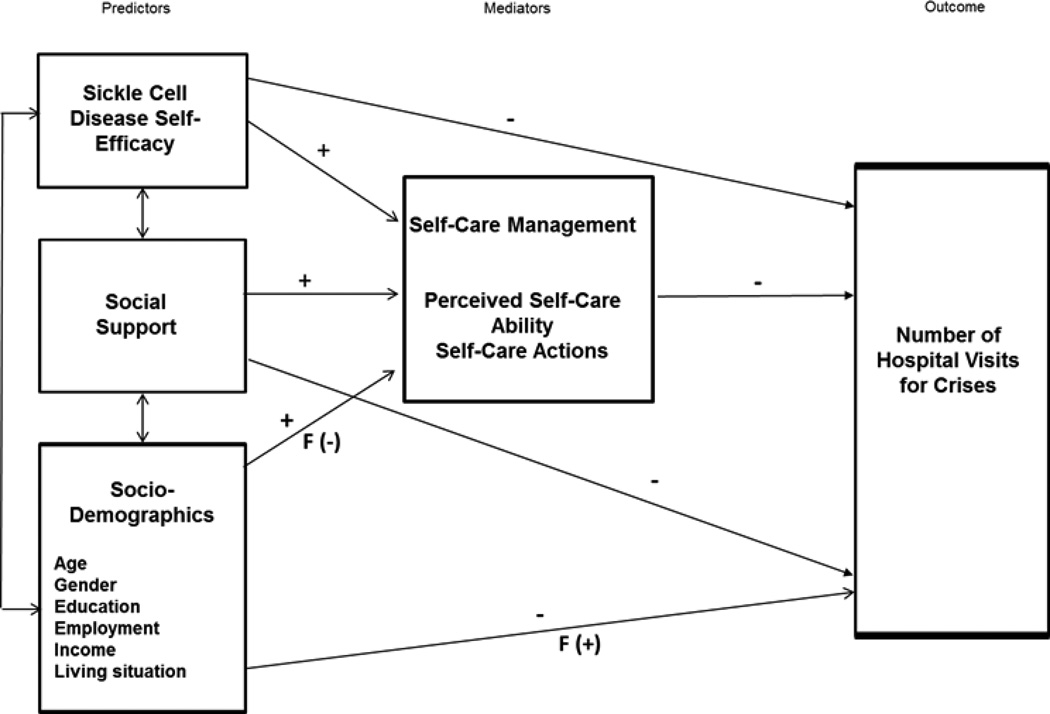
The conceptual model (Figure 1), derived from the literature, outlines the hypothesized relationships and provides the framework that was used to guide analyses.
Figure 1.
Conceptual Model
Procedures
A de-identified data file, with records for only the 103 young, Black adults who were ages 18 to 30 with SCD, was provided by the principal investigator of the parent study for use in this study. Statistical Package for the Social Sciences (SPSS Version 21) was used for analyses. Prior to conducting analyses, the data were evaluated for invalid values and data entry errors using descriptive statistics and frequencies. Missing data were addressed by conducting item-mean substitution. Mean substitution has been described as a conservative method which does not alter the mean of the sample or falsely strengthen correlations (Tabachnick & Fidell, 2007). Total scores for SCD self-efficacy, social support, perceived self-care ability, and self-care actions were used for final analyses. Bivariate correlations were used to describe the relationships among study variables while regression analyses were used to make predictions on the study variables from those relationships.
Results
Study participants were primarily female (61.2%), unemployed or disabled (68%), lived with family (73.8%), and had an average of three hospital visits for pain crises annually (Table 1). On average, participants were 24 years old, had 12 years of education, and an annual household income of $35,724 (Table 2).
Table 1.
Frequency and Percent of Patients by Socio-demographic Variables
| Variable | Category | N | Frequency | Percent |
|---|---|---|---|---|
| Age | 18–20 | 103 | 19 | 18.4 |
| 21–25 | 50 | 48.6 | ||
| 26–30 | 34 | 33.0 | ||
| Gender | Female | 103 | 63 | 61.2 |
| Male | 40 | 38.8 | ||
| Years of Education | 8–12 | 103 | 78 | 75.7 |
| 13–16 | 25 | 24.3 | ||
| Employment Status | Unemployed | 103 | 36 | 35.0 |
| Disabled | 34 | 33.0 | ||
| Full-time | 19 | 18.4 | ||
| Part-time | 14 | 13.6 | ||
| Annual Household | $17,843 – $27,714 | 100 | 28 | 27.4 |
| Income | $28,616 – $37,975 | 37 | 36.2 | |
| $38,470 – $48,251 | 22 | 21.6 | ||
| $50,701 – $65,375 | 13 | 12.6 | ||
| Missing | 3 | 2.2 | ||
| Living Situation | Share house with family | 103 | 76 | 73.8 |
| Live alone | 18 | 17.5 | ||
| Share house with friends | 9 | 8.7 | ||
| Number of Hospital | 0 | 99 | 9 | 8.7 |
| Visits for Pain Crises (per | 1–3 | 67 | 65.0 | |
| year) | 4–6 | 18 | 17.5 | |
| 7–10 | 3 | 3.0 | ||
| 12–20 | 2 | 2.0 | ||
| Missing | 4 | 3.8 |
Sample size (N) varies due to missing data
Table 2.
Means and Standard Deviations
| Variable | N | Range | Mean | Standard Deviation |
|---|---|---|---|---|
| Age | 103 | 18–30 | 23.87 | 3.403 |
| Years of Education | 103 | 8–16 | 12.08 | 1.473 |
| Annual Household Income | 100 | $17,843 – $65,375 | $35,724 | $10,487 |
| Sickle Cell Disease Self-Efficacy | 97 | 17–45 | 31.84 | 6.370 |
| Social Support | 90 | 31–95 | 75.34 | 15.752 |
| Perceived Self-Care Ability | 81 | 64–111 | 86.98 | 8.822 |
| Self-Care Actions | 101 | 17–32 | 27.84 | 3.171 |
| Number of Hospital Visits for Pain Crises | 99 | 0–20 | 2.75 | 2.822 |
Sample size (N) varies due to missing data
Descriptive analyses of SCD self-efficacy, social support, perceived self-care ability, and self-care actions were conducted; overall scores were high for each (Table 2). In terms of SCD self-efficacy, participants were 51.5% “sure” that they can keep doing most of the things they do day-to-day but 53.4% “not sure at all” to “neither sure nor not sure” that they can manage their life from day to day. Regarding social support, 55.3% of participants reported that someone is available “all of the time” to take them to the doctor if they needed it but 68% reported that someone is available “most of the time” to “none of the time” to give them good advice about a crisis. For perceived self-care ability, 57.3% of the participants “agree” that they routinely take measures to ensure the safety of themselves and their family and 56.3% “agree” that in the past, they have changed some of their old habits in order to improve their health. The majority of self-care actions were “almost always” conducted. Of the participants, 48.5% knew about their health, 74.8% understood their medications, 67% took medications as prescribed, 68.9% kept medical appointments, 42.7 % followed a recommended diet, 61.2% remained hydrated, 66% dressed warm, and 43.7% avoided stress. The reliability estimates for the instruments were above α=.70; Sickle Cell Self-Efficacy Scale (α=.86), the Medical Outcomes Study Social Support Survey (α=.95), the Appraisal of Self-Care Agency Scale (α=.73), and the Jenerette Self-Care Assessment Tool (α=.71).
Testing Hypotheses
Hypothesis one stated that greater self-care is associated with higher SCD self-efficacy, greater social support, being employed, living with family or friends, increased age, more years of education, higher income, and male gender. Results showed that higher SCD self-efficacy was associated with higher perceived self-care ability (r=.39, p<.001) and self-care actions (r=.31, p=.002) (Table 3). Greater social support was associated with higher perceived self-care ability (r=.43, p<.001) and self-care actions (r=.33, p=.001). Education was also associated with higher perceived self-care ability (r=.23, p=.018) and self-care actions (r=.20, p=.043). However, there were no significant associations noted among age, annual household income, living situation, employment status, gender, and self-care. Thus, the hypothesis was partially supported.
Table 3.
Pearson Correlations for the Continuous Variables
| SCDSE | SS | PSCA | SCA | Age | Education | Income | HSCD | |
|---|---|---|---|---|---|---|---|---|
| SCDSE | 1 | .502* | .391* | .309* | −.226* | .253* | −.070 | .015 |
| SS | 1 | .433* | .326* | −.197* | .224* | .039 | .050 | |
| PSCA | 1 | .466* | −.153 | .233* | −.047 | −.098 | ||
| SCA | 1 | .062 | .200* | .087 | .054 | |||
| Age | 1 | .168 | .098 | .006 | ||||
| Education | 1 | .133 | −.157 | |||||
| Income | 1 | −.219* | ||||||
| HSCD | 1 |
Correlations with item-mean substitution; listwise N=103. SCDSE, sickle cell disease self-efficacy; SS, social support; PSCA; perceived self-care ability; SCA, self-care actions; HSCD, number of hospital visits for pain crises.
Correlation is significant at the .05 level.
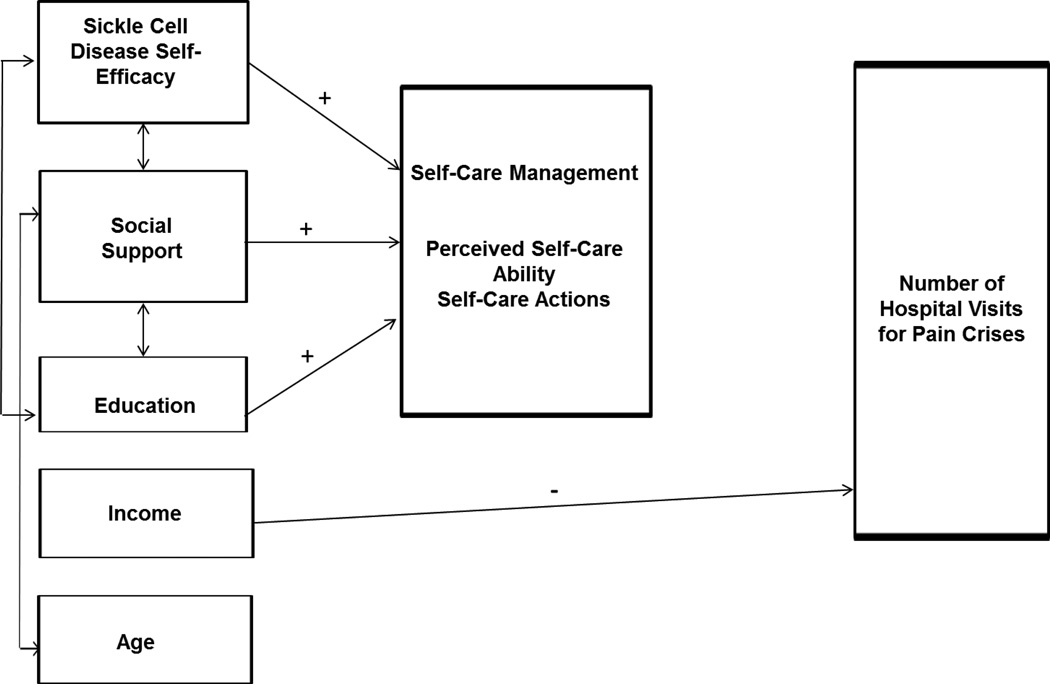
Hypothesis two stated that greater self-care is associated with fewer hospital visits for pain crises. This hypothesis was not supported. Self-care (perceived self-care ability and self-care actions) was not significantly correlated with the number of hospital visits for pain crises. Hypothesis three stated that SCD self-efficacy, social support, and socio-demographics have both a direct and an indirect relationship with hospital visits for pain crises. There was no adequate evidence to support a direct relationship among these variables. The indirect relationships among the variables, with self-care as the mediator, was also non-significant. Of the hypothesized variables, only income was significantly associated with hospital visits for pain crises (r=−.22, p=.05). Thus, this hypothesis was not supported. Observed relationships are outlined in Figure 2.
Figure 2.
Observed Relationships
A regression model with SCD self-efficacy, social support, years of education, and income significantly predicted perceived self-care ability; R2=.243, Adjusted R2=.212, F (4,98)=7.860, and p<.001. Of the four predictors tested, only social support was significant (β =.306 and p=.004). A separate model with SCD self-efficacy, social support, years of education, and income significantly predicted self-care actions; R2=.151, R2 adjusted=.117, F (4,98)=4.370, and p=.003. The individual variables were not significant in predicting self-care actions; social support was barely so (β =.208 and p=.058).
Discussion
Sickle cell disease self-efficacy, social support, and years of education were noted as important in understanding the role of self-care in young adults with SCD. These findings coincide with previous studies in which higher perceived self-care ability and self-care actions have been associated with higher SCD self-efficacy, social support, and education in the general SCD population (Edwards et al., 2001; Frei et al., 2009; Jenerette & Murdaugh, 2008). Social support appears to have the most significant effect on self-care. This finding reinforces the value of social support that has been noted in other studies. Use of self-care in long-term disease management is positively influenced by support from family, friends, and health care professionals (Schulman-Green et al., 2012). Individuals who receive higher levels of social support are more likely to feel as though they have the ability to perform self-care and actually do so to maintain health (Jenerette, Brewer, & Leak, 2011). In this study, higher SCD self-efficacy was associated with better self-care, supporting earlier research that found that self-efficacy has been associated with better self-care in chronic disease (Frei et al., 2009). Persons who believe they can accomplish SCD specific activities daily are likely to have a high perception of their self-care ability (a related concept) and thus may perform more self-care actions.
Of all the variables, income was most significantly and negatively associated with hospital visits for pain crises. This finding suggests that as income increases, the number of hospital visits for pain crises is likely to decrease. Individuals with health insurance can obtain primary care, and thus may experience fewer pain crises and hospital visits. The lack of employment and low income in the SCD population suggests that resources are needed to make health care more accessible and affordable to SCD patients. Although not statistically significant, perceived self-care ability showed a negative trend, self-care actions showed a positive trend, and years of education showed a negative trend toward a relationship with hospital visits for pain crises. These findings may be clinically significant. Further evaluation regarding hospital visits for pain crises is necessary.
While average scores for SCD self-efficacy, social support, perceived self-care ability and self-care actions were high, a high percentage of participants in this study had doubts about being able to manage their life from day to day and lacked someone to provide good advice about pain crises. In addition, a few participants lacked information about their health, did not always follow diet recommendations, and needed to avoid stress. These findings suggest that self-care interventions may be helpful in this population. These self-care interventions may be implemented as supplements to pharmacological pain treatment in the clinical setting and may be used to improve self-care in the home.
Study findings and can be used to guide the development of self-care interventions. Findings suggest that social support may be an important aspect of interventions to improve self-care and thus health outcomes in young adults with SCD. Social support interventions may provide opportunities for individuals with SCD to share self-care strategies. Interventions should also target individuals with lower levels of education. Individuals with lower education are less likely to have knowledge of self-care principles, have a weaker sense of self-care ability as a result, and are less likely to be successful in performing self-care actions than those with higher education. Lower levels of education may also negatively affect health literacy and this may influence an individual’s ability to engage in appropriate self-care activities. Due to the potential interaction between education and health literacy, they should both be considered in developing a collaborative plan of care.
Interventionists should conduct a baseline assessment of SCD self-efficacy then use the results to aid in tailoring self-care activities. The belief that one can achieve a desired goal, or self-efficacy, may be the most important step in improving health outcomes with self-care activities. Because we know that chronic genetic diseases such as sickle cell occur within the context of family and friends, it may also be useful to include a member of the patient’s support system in interventions. Individuals providing social support may serve to encourage patients and assist them in performing self-care actions and this may increase sickle cell self-efficacy.
Implications for Nursing Education, Practice and Research
There continues to be a lack of knowledge about SCD in the clinical setting. To help address this deficiency, nurse educators should incorporate information regarding SCD and self-care into the curriculum at schools of nursing. Continuing education settings should then provide routine updates regarding this information to better enable nurses to meet patients’ needs. Patient education programs aimed at improving self-care as well as nursing interventions to improve SCD self-efficacy should be included as a part of the disease management process. The use and effectiveness of support groups in SCD should also be explored. Moreover, health care resources are needed to enable patients to access the health care system more consistently in order to obtain assistance with self-care.
Study Limitations
This study was not without limitations. Secondary data analysis can be affected by methods used in the parent study; limitations were noted by the study authors (Jenerette & Murdaugh, 2008). Information regarding ethnicity was not obtained during the parent study. Although SCD is most prevalent in individuals of African ancestry, the ethnicity of the participants (for example, African American versus African or Caribbean) may have revealed cultural differences in self-care. Differences in the perception of pain and the response to pain vary by cultural background (International Association for the Study of Pain, 2002), and thus may affect self-care which is heavily focused on pain crisis prevention. Further study is needed.
In the parent study, neither SCD type nor pain severity were ascertained. Pain experience varies by SCD type. Three main types of SCD exist, with sickle cell anemia being the most common and severe (Centers for Disease Control and Prevention, 2011c), thus leading to the need for more pain management. Differences in the pain experience, frequency, and severity, may affect the need for and use of self-care. Further study is needed regarding the effects of self-care on pain severity by SCD type.
In this study, selection criteria for participants included an age restriction (ages 18–30) given the crisis frequency and high healthcare usage associated with that age range. This restriction may have affected the relationships among the socio-demographic variables and the self-care variables. Correlations may have been decreased because age was included as a study variable. Also, despite the use of mean substitution, missing values in the data set may have affected relationships among the variables and decreased power estimates to find significant results.
Conclusions
Study findings complement previous research and contribute to an improved understanding of the role of self-care in young, Black adults with SCD. Sickle cell disease self-efficacy, social support, and years of education may predict important pain outcomes and thus can be useful in designing patient education programs aimed at improving self-care actions. To inform intervention development, further investigation is needed regarding specific self-care strategies SCD patients use daily to prevent and manage pain prior to seeking care.
Acknowledgements
The first author gratefully acknowledges Jason Beckstead, PhD, Constance Visovsky, PhD, RN, ACNP-BC, and William Haley, PhD for their advice and support during the completion of this work.
Funding source:
This work was supported in part by the National Institute of Nursing Research: T32 NR007091.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Nadine Matthie, Email: nmatthie@email.unc.edu.
Coretta Jenerette, Email: coretta.jenerette@unc.edu.
Susan McMillan, Email: smcmilla@health.usf.edu.
References
- American National Red Cross. Sickle cell donor program. 2014 Retrieved from http://www.redcrossblood.org/gcp-bluetag.
- Brousseau D, Owens P, Mosso A, Panepinto J, Steiner C. Acute care utilization and rehospitalizations for sickle cell disease. The Journal of the American Medical Association. 2010;303:1288–1294. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Data and statistics. 2011a Retrieved from http://www.cdc.gov/ncbddd/sicklecell/data.html.
- Centers for Disease Control and Prevention. Living well with sickle cell disease. 2011b Retrieved from http://www.cdc.gov/ncbddd/sicklecell/healthyliving-living-well.html.
- Centers for Disease Control and Prevention. Facts about sickle cell disease. 2011c Retrieved from http://www.cdc.gov/ncbddd/sicklecell/facts.html.
- Chlebowy D, Garvin B. Social support, self-efficacy, and outcome expectations: Impact on self-care behaviors and glycemic control in Caucasian and African American adults with type 2 diabetes. The Diabetes Educator. 2006;32:777–786. doi: 10.1177/0145721706291760. [DOI] [PubMed] [Google Scholar]
- Clay O, Telfair J. Evaluation of a disease-specific self-efficacy instrument in adolescents with sickle cell disease and its relationship to adjustment. Child Neuropsychology. 2007;13:188–203. doi: 10.1080/09297040600770746. [DOI] [PubMed] [Google Scholar]
- Cox L. Social support, medication compliance and HIV/AIDS. Social Work in Health Care. 2002;35:425–460. doi: 10.1300/J010v35n01_06. [DOI] [PubMed] [Google Scholar]
- Dunlop R, Bennett K. Pain management for sickle cell disease in children and adults (review) Cochrane Database of Systematic Reviews. 2009;(2) doi: 10.1002/14651858.CD003350.pub2. Art. no.: CD003350. [DOI] [PubMed] [Google Scholar]
- Edwards R, Telfair J, Cecil H, Lenoci J. Self-efficacy as a predictor of adult adjustment to sickle cell disease: One-year outcomes. Psychosomatic Medicine. 2001;63:850–858. doi: 10.1097/00006842-200109000-00020. Retrieved from http://vb3lk7eb4t.search.serialssolutions.com/?sid=Entrez:PubMed&id=pmid:11573035. [DOI] [PubMed] [Google Scholar]
- Fosdal M, Wojner-Alexandrov A. Events of hospitalization among children with sickle cell disease. Journal of Pediatric Nursing. 2007;22:342–346. doi: 10.1016/j.pedn.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Frei A, Svarin A, Steurer-Stey C, Puhan M. Self-efficacy instruments for patients with chronic diseases suffer from methodological limitations – a systematic review. Health and Quality of Life Outcomes. 2009;7:1–10. doi: 10.1186/1477-7525-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes R, McDonald H, Garg A. Helping patients follow prescribed treatment: Clinical applications. The Journal of the American Medical Association. 2002;288:2880–2883. doi: 10.1001/jama.288.22.2880. [DOI] [PubMed] [Google Scholar]
- International Association for the Study of Pain. Culture and pain. Pain: Clinical Updates, X. 2002:1–9. Retrieved from http://www.iasp-pain.org/AM/AMTemplate.cfm?Section=HOME&SECTION=HOME&CONTENTID=7578&TEMPLATE=/CM/ContentDisplay.cfm.
- Jenerette C, Brewer C, Edwards L, Mishel M, Gil K. An intervention to decrease stigma in young adults with sickle cell disease. Western Journal of Nursing Research. 2014;36:599–619. doi: 10.1177/0193945913512724. [DOI] [PubMed] [Google Scholar]
- Jenerette C, Brewer C, Leak A. Self-care recommendations of middle-aged and older adults with sickle cell disease. Nursing Research and Practice. 2011;22:58–63. doi: 10.1155/2011/270594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenerette C, Valrie C. The influence of maternal behaviors during childhood on self-efficacy in individuals with sickle cell disease. Journal of Family Nursing. 2010;16:422–434. doi: 10.1177/1074840710385000. [DOI] [PubMed] [Google Scholar]
- Jenerette C, Murdaugh C. Testing the theory of self-care management for sickle cell disease. Research in Nursing and Health. 2008;31:355–369. doi: 10.1002/nur.20261. [DOI] [PubMed] [Google Scholar]
- Jordan L, Swerdlow P, Coates T. Systematic review of transition from adolescent to adult care in patients with sickle cell disease. Journal of Pediatric Hematology/Oncology. 2013;35:165–169. doi: 10.1097/MPH.0b013e3182847483. [DOI] [PubMed] [Google Scholar]
- Kratz A, Molton I, Jensen M, Ehde D, Nielson W. Further evaluation of the motivational model of pain self-management: Coping with chronic pain in multiple sclerosis. Annals of Behavioral Medicine. 2011;41:391–400. doi: 10.1007/s12160-010-9249-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurence B, George D, Woods D. Association between elevated depressive symptoms and clinical disease severity in African-American adults with sickle cell disease. The Journal of the National Medical Association. 2006;98:365–369. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1421516/pdf/jnma00190-0057.pdf. [PMC free article] [PubMed] [Google Scholar]
- Lee L, Askew R, Walker J, Stephen J, Robertson-Artwork A. Adults with sickle cell disease: An interdisciplinary approach to home care and self-care management with a case study. Home Healthcare Nurse. 2012;30:172–183. doi: 10.1097/NHH.0b013e318246d83d. [DOI] [PubMed] [Google Scholar]
- Loeb S, Penrod J, Falkenstern S, Gueldner S, Poon L. Supporting older adults living with multiple chronic conditions. Western Journal of Nursing Research. 2003;25:8–23. doi: 10.1177/0193945902238830. [DOI] [PubMed] [Google Scholar]
- Ngamvitroj A, Kang D. Effects of self-efficacy, social support and knowledge on adherence to PEFR self-monitoring among adults with asthma: A prospective repeated measures study. International Journal of Nursing Studies. 2007;44:882–892. doi: 10.1016/j.ijnurstu.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Olowoyeye A, Okwundu CI. Gene therapy for sickle cell disease (review) Cochrane Database of Systematic Reviews. 2010;(8):1–8. doi: 10.1002/14651858.CD007652.pub2. Art. no: CD007652. [DOI] [PubMed] [Google Scholar]
- Pack-Mabien A, Haynes J. A primary care provider’s guide to preventive and acute care management of adults and children with sickle cell disease. American Academy of Nurse Practitioners. 2009;21:250–257. doi: 10.1111/j.1745-7599.2009.00401.x. [DOI] [PubMed] [Google Scholar]
- Panepinto J, Bonner M. Health-related quality of life in sickle cell disease: Past, present, and future. Pediatric Blood & Cancer. 2012;59:377–385. doi: 10.1002/pbc.24176. [DOI] [PubMed] [Google Scholar]
- Quinn C, Rogers Z, McCavit T, Buchanan G. Improved survival of children and adolescents with sickle cell disease. Blood. 2010;115:3447–3452. doi: 10.1182/blood-2009-07-233700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegel B, Jaarsma T, Stromberg A. A middle-range theory of self-care of chronic illness. Advances in Nursing Science. 2012;35:194–204. doi: 10.1097/ANS.0b013e318261b1ba. [DOI] [PubMed] [Google Scholar]
- Ryan P, Sawin K. The individual and family self-management theory: Background and perspectives on context, process, and outcomes. Nursing Outlook. 2009;57:217–225. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuels-Reid J, Scott R. Painful crises and menstruation in sickle cell disease. Southern Medical Journal. 1985;78:384–385. doi: 10.1097/00007611-198504000-00007. Retrieved from http://vb3lk7eb4t.search.serialssolutions.com/?sid=Entrez:PubMed&id=pmid:3983658. [DOI] [PubMed] [Google Scholar]
- Schulman-Green D, Jaser S, Martin F, Alonzo A, Grey M, McCorkle R, Whittemore R. Processes of self-management in chronic illness. Journal of Nursing Scholarship. 2012;44:136–144. doi: 10.1111/j.1547-5069.2012.01444.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CS, Stewart AL. The MOS social support survey. Social Science and Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. Retrieved from http://ac.els-cdn.com/027795369190150B/1-s2.0-027795369190150B-main.pdf?_tid=a2d96434-c18f-11e3-95d9-00000aab0f26&acdnat=1397231020_0ee038c33db52c5f9b116ac2cc6a809c. [DOI] [PubMed] [Google Scholar]
- Sin M, Kang D, Weaver M. Relationships of asthma knowledge, self-management, and social support in African American adolescents with asthma. International Journal of Nursing Studies. 2005;42:307–313. doi: 10.1016/j.ijnurstu.2004.06.013. [DOI] [PubMed] [Google Scholar]
- Sobota A, Neufeld E, Sprinz P, Heeney M. Transition from pediatric to adult care for sickle cell disease: Results of a survey of pediatric providers. American Journal of Hematology. 2011;86:512–515. doi: 10.1002/ajh.22016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B, Fidell L. Using multivariate statistics. 5th ed. Boston, MA: Allyn & Bacon Inc.; 2007. [Google Scholar]
- Tanabe P, Porter J, Creary M, Kirkwood E, Miller S, Ahmed-Williams E, Hassell K. A qualitative analysis of best self-management practices: Sickle cell disease. Journal of the National Medical Association. 2010;102:1033–1041. doi: 10.1016/s0027-9684(15)30730-6. [DOI] [PubMed] [Google Scholar]
- Taylor L, Stotts N, Humphreys J, Treadwell M, Miaskowski C. A review of the literature on the multiple dimensions of chronic pain in adults with sickle cell disease. Journal of Pain and Symptom Management. 2010;40:416–435. doi: 10.1016/j.jpainsymman.2009.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. Women's health USA 2012. Rockville, MD: 2013. Retrieved from http://www.mchb.hrsa.gov/whusa12/pc/pages/hc.html. [Google Scholar]
- Welch M. Care of Blacks and African Americans. In: Bigby J, editor. Cross-cultural medicine. American College of Physicians; 2003. pp. 29–60. [Google Scholar]
- Yusuf H, Atrash H, Grosse S, Parker C, Grant A. Emergency department visits made by patients with sickle cell disease: A descriptive study, 1999–2007. American Journal of Preventive Medicine. 2010;38:S536–S541. doi: 10.1016/j.amepre.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]