Abstract
Colorectal cancer (CRC) is one of the most common causes of cancer-associated mortality worldwide, but it is truly a preventable disease. Both curcumin and boswellic acids are well-established dietary botanicals with potent anti-tumorigenic properties which have been shown to modulate multiple oncogenic pathways. Recent data suggest that the chemopreventive effects of these botanicals may in part be mediated through regulation of key cancer-related microRNAs (miRNAs) and their downstream gene targets. Here, we investigated the anti-tumorigenic effects of curcumin and 3 acetyl-11-keto-β-boswellic acid (AKBA) on modulation of specific cancer-related miRNAs in CRC cells and validated their protective effects in vivo using a xenograft mouse model. Both curcumin and AKBA inhibited cellular proliferation, induced apoptosis and cell cycle arrest in CRC cell lines, and these effects were significantly enhanced with combined treatment. Gene-expression arrays revealed that curcumin and AKBA regulated distinct cancer signaling pathways including key cell-cycle regulatory genes. Combined bioinformatics and in-silico analysis identified apoptosis, proliferation and cell-cycle regulatory signaling pathways as key modulators of curcumin and AKBA-induced anti-cancer effects. We discovered that curcumin and AKBA induced upregulation of tumor-suppressive miR-34a and downregulation of miR-27a in CRC cells. Furthermore, we demonstrated in a mouse xenograft model that both curcumin and AKBA treatments suppressed tumor growth, which corresponded with alterations in the expression of miR-34a and miR-27a, consistent with our in vitro findings. Herein we provide novel mechanistic evidence for the chemopreventive effects of curcumin and AKBA through regulation of specific miRNAs in colorectal cancer.
Keywords: curcumin, boswellic acid, colon cancer, microRNA, chemoprevention
Introduction
Colorectal cancer (CRC) is one of the leading causes of cancer-related mortality in the United States (1). There is growing evidence suggesting that dietary and lifestyle modifications can influence risk prevention for CRC (2). Increasing focus on chemopreventive properties of natural compounds from traditional medicine has led to discovery of potential therapeutic agents targeting CRC and other cancers. Curcumin, the principle curcuminoid and a derivative of the spice turmeric curcuma longa, is used as a naturally occurring medicine to treat variety of inflammatory disorders, and human cancers (3). In terms of its well-established anti-tumorigenic properties, curcumin has been shown to interfere with various stages of colorectal tumorigenesis including tumor initiation, promotion, and progression (4–7). While curcumin is known to regulate multiple signaling pathways involved in carcinogenesis, the mechanism by which curcumin simultaneously interferes with these pathways remains unclear. One probable explanation is that some botanicals, including curcumin, have the capacity to regulate microRNAs (miRNAs) associated with cancer (8). MiRNAs are small non-coding RNAs that regulate gene expression via interaction with the 3’untranslated regions of target mRNAs thereby regulating up to several hundred genes post-transcriptionally (9). Although miRNAs are known for their involvement in many physiological processes, dysregulation of miRNA expression in cancer is well established (10). Curcumin has been shown to downregulate putative oncogenic miRNAs such as miR-21 (11, 12), while it upregulates key tumor suppressor miRNAs including miR-200 family, let-7 family, miR-185b and miR-22 (13–15). Therefore, regulation of miRNAs appears to be a crucial anti-tumorigenic mechanism of curcumin and warrants further systematic and comprehensive investigation.
Boswellic acid, an organic acid derived from the plant boswellia serrata, is another botanical used traditionally for the treatment of various inflammatory diseases including colitis and arthritis. Although boswellia serrata is comprised of various derivatives including, acetyl-β-boswellic acid, 11-keto-β-boswellic acid and 3 acetyl-11-keto-β-boswellic acid (AKBA), AKBA is identified as the most potent anti-inflammatory constituent of boswellic acid (16, 17). Similar to curcumin, AKBA exerts its anti-tumorigenic effects through regulation of multiple cancer signaling pathways (16, 18–22). Interestingly, we recently demonstrated that AKBA upregulates key putative tumor suppressive miRNAs in CRC and the expression of these miRNAs inversely corresponded with tumor size and volume in a xenograft animal model (23).
Despite lack of preclinical studies on combined treatment with curcumin and AKBA together, curcumin has been used in combination approaches with other dietary components. Treatment with curcumin and green tea catechins attenuated aberrant crypt formation in a carcinogen-induced CRC mouse model (24), while a combination of curcumin and resveratrol synergistically suppressed tumor proliferation in a mouse xenograft model (25). Although further investigations are required to fully understand the anti-tumorigenic properties of these compounds individually and in combination, these studies highlight the enormous therapeutic potential of using these safe and cost-effective botanicals together to help prevent and possibly treat CRC. Here, we identified key molecular mechanisms by which curcumin and AKBA both individually and in combination affect specific miRNAs and their downstream target genes involved in the cell cycle regulation of CRC cell lines. Furthermore, we confirmed these anti-tumorigenic properties of curcumin and AKBA, both alone and together, in a mouse xenograft model.
Materials and Methods
Materials and cell lines
Human colorectal cancer cell lines, HCT116, RKO, SW480, SW620, HT29 and Caco2 CRC cell lines were purchased from American Type Culture Collection (Manassas, VA). All cell lines were routinely authenticated by analyzing a panel of specific genetic and epigenetic biomarkers. The HCT116p53−/− cell line was a generous gift from Bert Vogelstein, Johns Hopkins Medical Institute, Baltimore, MD. All cells were grown in Iscove’s Modified Dulbecco’s medium (IMDM) (Invitrogen, Carlsbad, CA) with 10% fetal bovine serum and 1% penicillin and streptomycin and maintained at 37°C in a humidified incubator (5% CO2). Both curcumin (BCM-95) and AKBA (Bospure) were provided by Dolcas Biotech (Chester, NJ). These botanicals were dissolved in DMSO and diluted to appropriate experimental concentrations with tissue culture medium.
Cellular cytotoxicity, cell cycle, apoptosis and clonogenic assays
Cellular cytotoxicity was determined by the 3-(4, 5-dimethylthiazole-2-yl_2,5-diphenyl tetrazolium bromide (MTT)) assay as described previously (23). In brief, approximately 4,000 cells were seeded in each well and treated with various concentrations of curcumin and/or AKBA for 72 hours. Optical density was determined using Tecan Infinite 200 Pro multi-reader and i-control 1.10 software (Tecan Group Ltd, Mannedorf, Switzerland). The Chou-Talalay equation (26) was used to calculate the combination index (CI) to determine the interaction between curcumin and AKBA treatments. Cell cycle analysis was conducted using Cell cycle assay kit (MCH100106; Millipore, Billerica, MA) and apoptotic cell fraction was measured using Annexin V and Dead Cell Assay Kit (Millipore) according to the manufacturer’s instructions using the Muse Cell Analyzer (Millipore). For clonogenic assays approximately 500 cells were seeded in each well of a six-well plate, and were treated with various concentrations of curcumin and/or AKBA. After 8 days, colonies were stained with crystal violet (Sigma-Aldrich, St. Louis, MO) and dried overnight at room temperature. The number of colonies with >50 cells were counted using GeneTools (Syngene, Cambridge, UK). All experiments were conducted in replicates and at least three independent experiments.
Gene-expression microarray analysis
Microarray gene-expression analysis was performed in HCT116 and SW480 cell lines treated with curcumin and/or AKBA and DMSO treated controls according to the manufacturer’s instructions and a method described previously (27). Detailed methodologies are supplied in Supplementary materials and methods
Quantitative real-time PCR analysis
Total RNA was extracted from curcumin and AKBA-treated CRC cell lines (10 mu;M curcumin, 30 μM AKBA or the combination of both botanicals for 24 hours) and from the xenograft tumor tissue samples using the miRNeasy Mini Kit (Qiagen) following the manufacturer’s instructions. For analysis of the mRNA expression, 1μg of total RNA was reverse transcribed to complementary DNA using Advantage RT PCR-kit (Clontech Laboratories Inc., Mountain View, CA). Power SYBR Green (Applied Biosystems, Foster City, CA) real-time PCR was performed using StepOnePlus system (Applied Biosystems). For specific primer sequences refer to Supplementary Figures (Suppl. Table 1). All qRT-PCR target genes expression was normalized to the expression of glyceraldehydes-3-phosphate dehydrogenase (GAPDH) and analyzed using the ΔΔCt method. The expression of miRNAs was analyzed using TaqMan® real-time PCR assay kit (Applied Biosystems). All miRNA primers used in this study were purchased from Ambion (Austin, TX). Ten nano grams of RNA from each sample was reverse transcribed using TaqMan® microRNA Reverse Transcription kit (Applied Biosystems) and 6 ng of complementary DNA was used for real-time qRT-PCR. All data were analyzed using ΔΔCt method and normalized to RNU6B.
Transfection of miRNA
A total of 1 × 105 cells were seeded and transfected with pre-miR-34a, anti-miR-27a, pre-miR-negative-control 1 or anti-miR-negative-control 1 (Ambion) at a final concentration of 50 nmol/L using siPort NeoFX (Applied Biosystems) and Opti-MEM (Gibco, Carlsbad, CA) according to manufacturer’s instructions. The relative levels of miRNAs were measured to confirm the efficiency of miRNA transfection and functional analyses were conducted as described above.
Western blotting
Western immunoblotting experiments were performed as described previously (28). In brief, cells were treated with curcumin and/or AKBA for 24 hours, thereafter lysed using 100 μl of 1X SDS sample buffer containing β-mercaptoethanol. All antibodies are listed in Supplementary Table 2. 1. All samples were compared against β-actin as a reference (Sigma-Aldrich). The bands were visualized using GeneTools (Syngene, Cambridge, UK) and images were captured using Syngene GBox (Cambridge, UK).
DAPI staining of apoptotic cells
Apoptotic cells were evaluated using 4′,6-diamidino-2-phenylindole (DAPI) staining as described previously (29). In brief, cells were treated with different concentrations of curcumin and/or AKBA for 24 hours. The cells were then fixed with methanol for 30 min at 4°C and incubated in DAPI solution for 1 h in the dark. The number of apoptotic cells were evaluated under fluorescence microscope (Leica, Germany).
3D cultures
3D cultures were generated as described previously (30). In brief, approximately 1 × 106 cells were seeded on a cellulose filter on top of a steel mesh bridge. Cells were then treated with curcumin (10 μM), AKBA (30 μM) or the combination of both for 1, 3, 7, or 10 days. The growth of 3D cultures was assessed by determining the diameter of the 3D cultures using light microscopy.
Mouse xenograft model
The 5 week-old male athymic nude mice were purchased from Harlan Laboratories (Houston, TX) and kept under controlled conditions of light (12 h cycles), fed ad libitum diet and had free access to water. Xenograft tumors were generated by subcutaneous injection of 5×106 HCT116 cells. Tumor growth was determined by measuring the length (L) and width (W) of the tumor every other day using calipers and the tumor volume was calculated according to the following formula: 1/2LW2. Once average tumor size reached 50 mm3, animals were randomly divided into 4 groups with 10 animals in each group: 1. control vehicle (DMSO), 2. Curcumin (25 mg kg−1), 3. AKBA (75 mg kg−1), or 4. Curcumin and AKBA. Treatments or vehicle were injected intraperitoneally daily for three weeks. The tumor samples were fixed in RNAlater (Sigma-Aldrich) then stored in a −80 °C freezer for subsequent analyses. For the xenograft tumor growth experiment, the interaction between curcumin and AKBA was evaluated as described previously (31). The fraction of tumor volume (FTV) affected by curcumin and/or AKBA was calculated individually and together as a ratio to control. The ratio of expected FTV (Exp FTV) and observed FTV (Obs FTV) was calculated for the combined treatment (A ratio >1 indicates synergistic effect, <1 indicates an additive effect). The animal protocol was approved by Institutional Animal Care and Use Committee at the Baylor Research Institute, Dallas, Texas.
Statistical analysis
All analyses were performed using GraphPad Prism Ver. 6.0 (GraphPad Software Inc. San Diego, CA). All data were expressed as mean ± SEM with statistical significance indicated when P < 0.05. Statistical comparisons between control and treatment groups were determined using unpaired t test or one-way ANOVA with Tukey’s post-hoc tests.
Results
Combination of curcumin and AKBA enhances cytotoxicity and inhibits proliferation of CRC
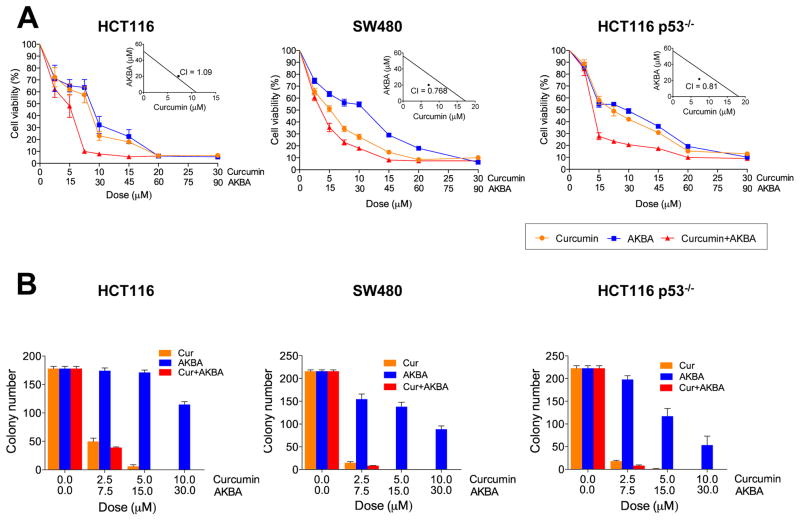
The average IC50 of four cell lines (HCT116, RKO, SW480, and SW620; Suppl. Fig. 1A) was used to determine the potency of both botanicals and the ratio between these botanicals was calculated (Curcumin:AKBA, 1:2.76; Suppl. Fig. 1B). Based on these data, we selected the concentration of AKBA as three times the dose of curcumin for this study. We then examined the cytotoxicity of curcumin and/or AKBA on two primary CRC cell lines (HCT116 and SW480). Both curcumin and AKBA treatment increased the cytotoxicity in a dose-dependent manner (Fig. 1A). The combined treatment further enhanced cytotoxicity in both cell lines. Next we determined whether this enhanced cytotoxicity by the combined treatment was synergistic using the Chou-Talalay Combination index (CI) (26). Interestingly, while the cytotoxicity of the both treatments together was additive in HCT116 cell line (CI = 1.09), combined treatment of curcumin and AKBA in the SW480 cell line resulted in synergism (CI = 0.768; Fig. 1A inserts). Considering tumor suppressor p53 is mutated in the SW480 cell line but not in the HCT116 cell line, we next investigated whether p53 dysregulation contributed to the discrepancy of AKBA and curcumin-induced cytotoxicity between these cell lines using p53−/− HCT116 cells (HCT116p53−/−). While treatment of curcumin or AKBA resulted in a dose-dependent increase in cytotoxicity in HCT116p53−/− cell line, the combination of curcumin and AKBA showed synergistic enhancement in cytotoxicity (CI < 1; Fig. 1A insert), suggesting that AKBA complements cytotoxicity of curcumin in cell lines lacking active p53. In addition, to ensure that the combined botanicals exert synergistic enhancement in cytotoxicity in p53 mutated cell lines, we determined synergism between curcumin and AKBA in RKO (p53 WT), Caco3 and HT29 (both p53 mutant cell lines; Suppl. Fig. 2A). While RKO cells showed no synergistic cytotoxicity between curcumin and AKBA (CI = 1.21), the combined botanicals exerted synergistic cytotoxicity in both HT29 and Caco2 cell lines (CI = 0.989, 0.971 respectively). Next, we evaluated the effects of these botanicals on cell survival and proliferation using the clonogenic assays (Fig. 1B and Suppl. Fig. 2B). To our surprise, even at a low dose of 2.5 μM, curcumin significantly suppressed colony formation, while over a 10-fold higher concentration of AKBA was required to exert a similar effect (Fig. 1B), indicating that curcumin has superior inhibition of cell survival and proliferation compared to AKBA.
Figure 1. Curcumin and AKBA exert cytotoxicity and suppress colony formation on CRC cell lines.
(A) Cytotoxicity of different doses of curcumin and/or AKBA on HCT116, HCT116p53−/−, and SW480 cell lines. Insert: Synergy between curcumin and AKBA was calculated by use of the Combined Index (CI). (B) Colony formation assay of CRC cell lines treated with various concentrations of curcumin and/or AKBA.
Combination of curcumin and AKBA regulates cell death, proliferation and cell cycle
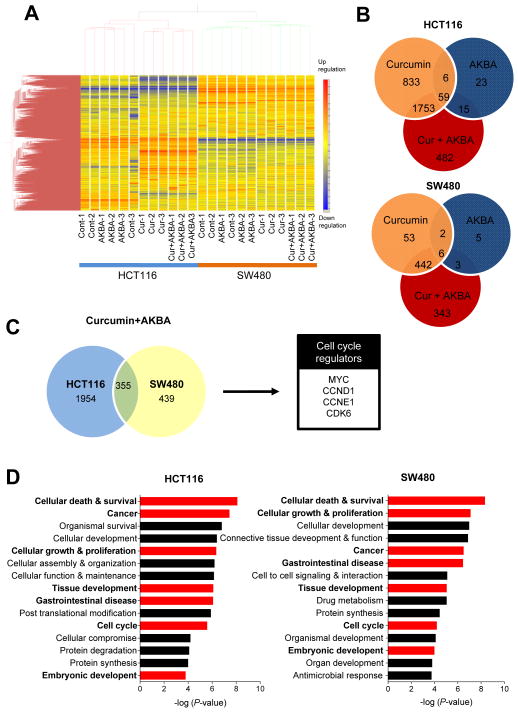
To identify cancer signaling pathways modulated by curcumin and AKBA in CRC, we used microarray analysis to examine gene-expression alterations caused by curcumin and AKBA individually, and in combination in the two CRC cell lines. Hierarchical clustering analysis showed that a markedly different cluster of genes were regulated by curcumin and AKBA in HCT116 and SW480 cell lines (Fig. 2A). Furthermore, gene-expression profiles of the combined treatments revealed that a large cluster of genes unaffected by curcumin treatment alone were regulated by the combined treatment with curcumin and AKBA (Fig. 2B), suggesting that these botanicals in combination modulate additional cluster of genes compared to individual treatments. We then assessed all genes regulated by the dual treatments in both CRC cell lines and identified 355 genes with overlapping expression alterations (Fig. 2C). Next we used Ingenuity Pathway Analysis (IPA) to determine potential molecular signaling pathways regulated by the combined curcumin and AKBA treatment (Fig 2D). Top cancer-related molecular functions common to both cell lines were: cell death and survival, cellular growth & proliferation, and cell cycle (Fig. 2D). Since cell cycle is related to both cell death and proliferation, we next focused on systematic evaluation of genes involved in cell cycle regulation among the subset of 355 differentially expressed genes. Subsequently we identified MYC, CCND1, CCNE1, and CDK6 as potential target genes of the combined curcumin and AKBA treatment (Fig. 2C).
Figure 2. Curcumin and AKBA modulate apoptosis, anti-proliferation and cell cycle regulation.
HCT116 and SW480 cell lines were treated with curcumin, AKBA alone or together followed by gene-expression microarray and bioinformatic analyses. (A) Heat map of gene expression in CRC cell lines treated with curcumin and/or AKBA. (B) Venn diagram showing number of commonly regulated genes shared by curcumin, AKBA and the combined treatment in HCT116 and SW480 cell lines. (C) Commonly regulated genes shared by the combined treatment for HCT116 and SW480. (D) Predicted molecular functions of genes regulated by curcumin and AKBA treated CRC cells determined by IPA.
Curcumin and AKBA induce cell cycle arrest, apoptosis and inhibit proliferation in 3D cultures
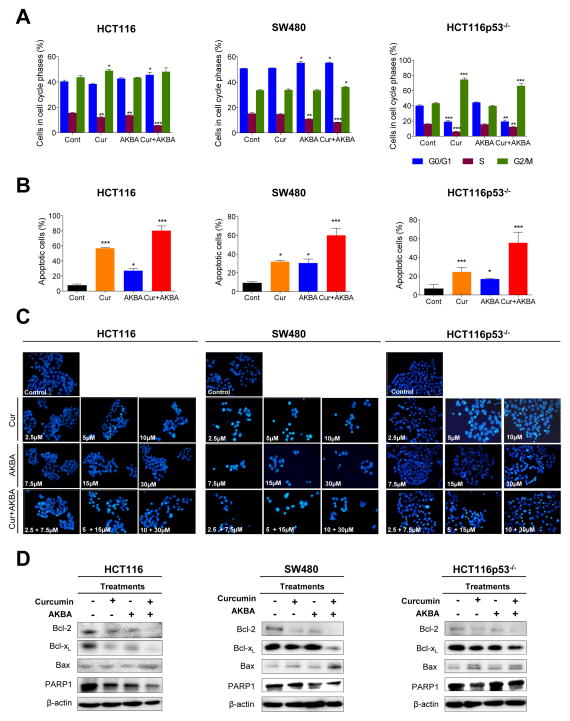
We next investigated the mechanism of cell cycle regulation by curcumin and AKBA alone and in combination in CRC cells. Curcumin treatment induced G2/M arrest in HCT116 and HCT116p53−/− cell lines, but not in the SW480 cell line; while AKBA induced G1 arrest in HCT116 and SW480 cell lines. When cell were treated with curcumin and AKBA together, G1 arrest was induced in HCT116 and SW480 cell lines, while G2/M arrest was predominantly observed in the HCT116p53−/− cells (Fig. 3A). These data indicate that combinatorial treatment with curcumin and AKBA exerts anti-tumorigenic effects through cell cycle regulation. Next, we determined whether curcumin and AKBA enhanced apoptosis in CRC cell lines. Both curcumin and AKBA treatment increased cellular apoptosis in all three cell lines, while the two botanicals together further elevated apoptotic cell population regardless of the cell line analyzed (Fig. 3B). We then used the DAPI nuclear staining to confirm that both curcumin and AKBA enhanced cellular apoptosis (Fig. 3C). In somatic cells, the Bax/Bcl ratio serves as a regulator for cell susceptibility to apoptosis (32), hence we first assessed whether curcumin and AKBA regulate cell survival proteins, Bcl-2 and Bcl-xL. While Bcl-2 and Bcl-xL were downregulated by both curcumin and AKBA alone, the effect of the dual treatment augmented Bcl-2 and Bcl-xL inhibition in all three CRC cell lines (Fig. 3D). We then showed that both curcumin and AKBA upregulated pro-apoptotic protein Bax, while the two treatments together further elevated the expression of Bax (Fig. 3D). In addition, poly (ADP-ribose) polymerase 1 (PARP1), a DNA single-strand breaks repair protein and a suppressor of Caspase pathway, was downregulated by curcumin and AKBA, both individually and in combination. Collectively, in line with microarray data, we confirmed that the combination of curcumin and AKBA results in increased cell cycle arrest and apoptosis. Additionally to confirm the anti-tumorigenic properties of these botanicals we used 3D cultures to determine whether curcumin and/or AKBA could interfere with CRC tumor growth (Suppl. Fig. 3). While both curcumin and AKBA inhibited cellular growth individually, combined treatment with curcumin and AKBA further inhibited the growth in HCT116 cells. Together we demonstrated that curcumin and AKBA exert anti-tumorigenic effects through cell cycle arrest and apoptosis, while suppressing cellular growth in both 2D and 3D in vitro models.
Figure 3. Curcumin and AKBA induce cell cycle arrest and apoptosis.
(A) Cell cycle analysis. Cells were treated with 10 μM curcumin and/or 30 μM AKBA and then stained with propidium iodide and subjected to flow cytometry analysis to determine DNA content for phase of the cell cycle. (B) Cells were stained with Annexin V and 7-AAD and apoptotic cell number was determined by flow cytometry. Flow cytometry graphs and the corresponding percentage of apoptotic cells are shown in bar graphs. (C) Images of apoptotic cells treated with increasing doses of curcumin and/or AKBA determined by DAPI staining. (D) Immunoblot analysis of Bcl-2, Bcl-xl, Bax and PARP1. *P< 0.05, ** P< 0.01 *** P< 0.001 compared to the corresponding control.
Curcumin and AKBA control cell cycle regulating miRNAs and their downstream target genes
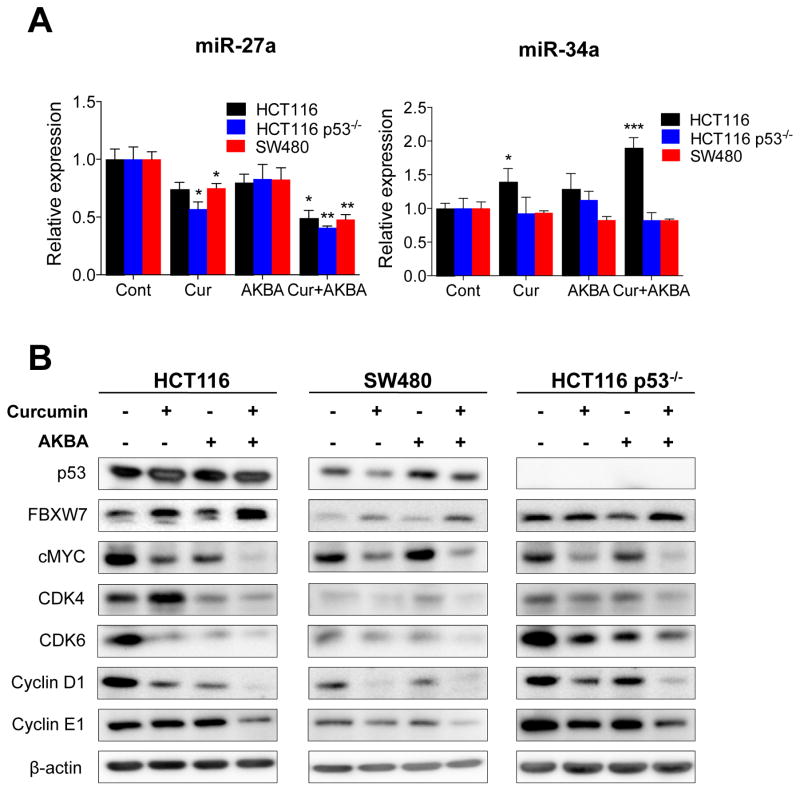
Using the genes identified by the microarray analysis, we utilized Targetscan (Ver 6.2) and miRTarBase to determine potential miRNAs regulated by curcumin and AKBA. We initially selected miR-34a, miR-145, and miR-16 as potential candidates based on their predicted target genes. miR-34a expression was upregulated by curcumin and further elevated by concurrent treatment with curcumin and AKBA in HCT116 cells (Fig. 4A), but had no significant effect in both SW480 and HCT116p53−/− cell lines. Considering that miR-34a has been shown to be primarily activated by p53 (33), these data indicate that curcumin and AKBA modulate miR-34a expression through p53. This finding was consistent in RKO (p53 wild type), Caco2 and HT29 (both p53 mutated) cell lines as well (Suppl. Fig. 4A). Next, we used western blot and qRT-PCR analyses to determine whether these botanicals suppressed expression of miR-34a target genes. Both curcumin and AKBA downregulated cMyc, CDK4, CDK6 and Cyclin D1 expression, while the combined treatment further increased the inhibitory effects in the HCT116 cell line (Fig. 4B). To our surprise, miR-34a target gene expression was also downregulated in cell lines with p53 mutation/deficiency indicating that these botanicals exert anti-tumorigenic effects only in part through miR-34a upregulation in CRC cells. Next, we investigated the expression of miR-145 and miR-16, both putative tumor suppressive miRNA involved in modulation of cell cycle (34, 35) in CRC cell lines. Although miR-145 expression was increased by AKBA alone and with the combined treatment in the HCT116 cell line, curcumin treatment alone did not alter miR-145 expression in any of the CRC cell lines (Suppl. Fig. 4B). The combination of curcumin and AKBA treatment resulted in a significant increase in miR-16 levels in the HCT116 p53−/− cells, while curcumin or AKBA alone did not significantly influence miR-16 expression in any cell lines (Suppl. Fig. 4B). Therefore, these data collectively indicate that not all tumor suppressive miRNAs are regulated coordinately by curcumin, and that AKBA and curcumin target different miRNAs to exert their anti-tumorigenic effects.
Figure 4. Curcumin and AKBA regulate miR-34a and miR-27a protein expression and their downstream targets.
(A) Expression of miR-27a and miR-34a in CRC cells treated with curcumin and/or AKBA. MiRNA expression was normalized to RNU6B. (B) Western blots of downstream targets of miRNAs. All CRC cell lines were treated with 10μM curcumin and/or 30 μM AKBA for 24 h. Cells were lyzed and western blot analyses were performed on putative downstream targets of miR-34a and miR-27a. β-actin was run as a loading control. *P< 0.05, ** P< 0.01 *** P< 0.001 compared to the corresponding control.
Since our initial focus was on the identification of putative tumor suppressive miRNAs, we investigated whether curcumin and AKBA can also regulate the expression of oncogenic miRNAs. Recent studies demonstrated that miR-27a, an oncogenic miRNA, was suppressed by curcumin in CRC cell lines (36, 37). While we confirmed that miR-27a was downregulated by curcumin treatment alone in all three CRC cell lines, its expression was further inhibited by the combined treatment. These data indicate that unlike miR-34a, curcumin and AKBA inhibit miR-27a independently of p53 activation (Fig. 4A). Furthermore, we confirmed downregulation of miR-27a expression by the combined curcumin and AKBA treatment in RKO, HT29 and Caco2 cell lines (Suppl. Fig. 4A). We then investigated whether inhibition of miR-27a by curcumin and AKBA resulted in alteration of FBXW7, a tumor suppressor and a direct target of miR-27a (38). While curcumin treatment alone upregulated FBXW7 expression, the combined treatment further enhanced FBXW7 expression (Fig. 4B & Suppl. Fig 5). In addition, we demonstrated that both curcumin and AKBA individually and in combination suppressed Cyclin D1 and cMyc, as well as downstream targets of FBXW7 (Fig. 4B & Suppl. Fig 5).
miR-34a over-expression/miR-27a knockdown induces apoptosis and cell cycle arrest and suppresses proliferation
To confirm that miR-34a upregulation contributes to the anti-tumorigenic effects of botanicals, we transiently over-expressed miR-34a and investigated its molecular function in the three CRC cell lines (Suppl. Fig. 6A). Over-expression of miR-34a resulted in an enhanced apoptotic cell population in all three cell lines (Suppl. Fig. 6B); however, miR-34a-induced apoptosis appeared to be less prominent in p53 mutated/deficient cell lines. These results support the idea that there is a positive feedback loop between miR-34a and p53 (33). Furthermore, miR-34a over-expression resulted in G1 arrest in all cell lines (Suppl. Fig. 6C), while it resulted in suppressed cell proliferation and colony formation (Suppl. Fig. 6D and 6E). Similarly, we investigated anti-tumorigenic activity of miR-27a inhibition in CRC cell lines. Transient knockdown of miR-27a enhanced cellular apoptosis in all three CRC cell lines (Suppl. Fig. 7A, 7B), while cell cycle analysis showed miR-27a knockdown resulted in an increase in G2/M phase arrest in HCT116 and HCT116 p53−/− cell lines, while prolonged S phase fraction in the SW480 cell line (Suppl. Fig. 7C). miR-27a knockdown resulted in suppression of cell growth and colony formation in all three cell lines (Suppl. Fig. 7D, 7E).
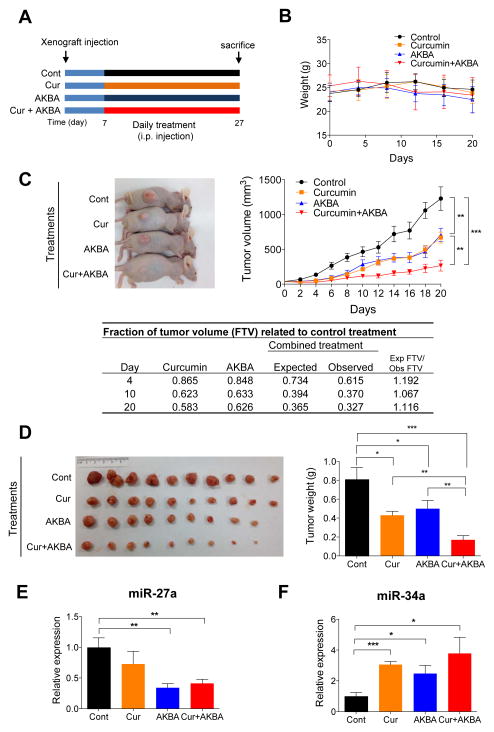
Curcumin and AKBA inhibit tumor progression in a mouse xenograft model
To confirm the therapeutic potential of curcumin and AKBA in vivo, we generated mouse xenograft tumors by injecting HCT116 cells subcutaneously into nude athymic mice. We subsequently treated the animals with curcumin (25 mg kg−1 b/w) and/or AKBA (75 mg kg−1 b/w) for 20 days (Fig. 5A). Although previous studies used 100 mg kg−1 curcumin to attenuate tumor growth in the mouse xenograft model (39, 40), we purposely chose a lower dose of curcumin to mimic a more reasonable and physiologically achievable clinical dose of curcumin. The body weight of the animals was unaffected by the treatment during the experiment (Fig. 5B). The progressive growth in tumor volume showed that treatment with curcumin or AKBA suppressed tumor growth at a similar rate (Fig. 5C). Interestingly, treatment with botanicals appeared to influence tumor growth immediately, because the average tumor volume of treatment groups deviated from the control group four days from the initiation of treatment. The combined curcumin and AKBA treatment resulted in further inhibition in the growth of the xenograft tumors. Confirming our measurement for tumor volume, tumor weight positively correlated with changes the tumor volume (Fig. 5D). In order to determine whether combined treatments resulted in an enhanced suppression of tumor growth, we calculated the expected tumor volume using fraction of tumor volume (FTV) of curcumin and AKBA (Fig. 5C). Interestingly, throughout the treatment period, curcumin and AKBA together resulted in synergistic tumor growth suppression (ratio of expected: observed FTV > 1). In addition, we wanted to ascertain whether these in vivo anti-tumorigenic effects of curcumin and AKBA corresponded with the expression alterations of miR-27a and miR-34a, as witnessed in cell culture studies. The expression of miR-27a was downregulated in tumors from mice treated with AKBA or curcumin and AKBA (Fig. 5E), while tumors from mice treated with curcumin and/or AKBA had increased miR-34a (Fig. 5F). In addition, we measured the expression of target genes of these miRNAs in the xenograft tumor tissues. We confirmed that FBXW7, cMyc, CDK6 and CyclinE1 were modulated by the combined treatment (Suppl. Fig 8). Collectively, these data indicate that changes in expression of these two miRNAs in tumors, at least in part, contributed to tumor growth inhibition.
Figure 5. Curcumin and AKBA suppress xenograft tumor growth.
(A) The schematic diagram of the curcumin and AKBA treatment protocol. (B) Body weight of animals during the 20 day treatment period. (C) Representative animals demonstrating tumor sizes according to the different treatments and a graph showing the progressive tumor volume increase during treatment period. Fraction of tumor volume (FTV) was calculated for both curcumin and AKBA treatment alone in the table. Expected FTV (Exp FTV) was calculated by multiplying the FTV of curcumin and AKBA then comparing it to the observed FTV (Obs FTV). Ratio of Exp FTV/Obs FTV > 1 indicates a synergistic effect. (D) Image of xenograft tumors collected from experimental animals and a graph depicting the average tumor weight by treatment (E) Graph of the relative expression of miR-27a in xenograft tumors by treatment (F) Graph of the relative expression of miR-34a in xenograft tumors by treatment (Normalized to RNU6B) *P< 0.05, ** P< 0.01 *** P< 0.001 compared to the corresponding control.
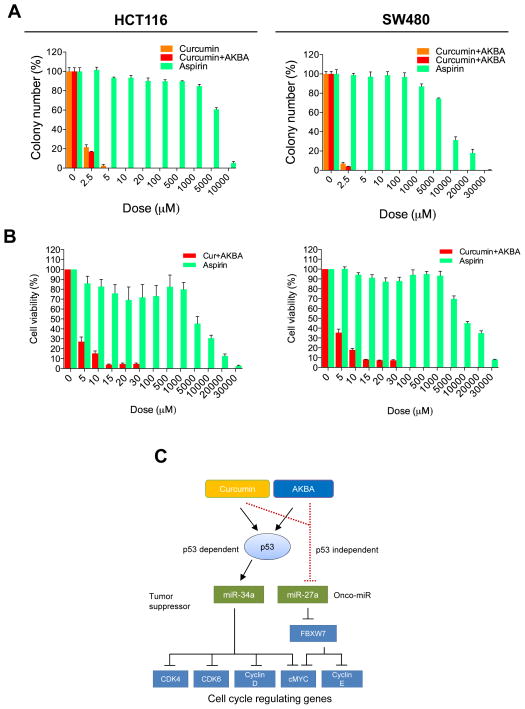
Curcumin and AKBA are significantly more cytotoxic against CRC cells than aspirin
Finally, in order to compare the anti-tumorigenic properties of both botanicals with a well-established chemopreventive drug, we used MTT and colony formation assays to compare the potency of curcumin and AKBA with aspirin, a non-steroidal anti-inflammatory drug (NSAID). A previous study showed that aspirin is more effective in PI3KCA mutated cancers (41), hence we compared the effects of these botanicals to aspirin in two cell lines HCT116 (PI3KCA mutated) and SW480 (PI3KCA wild type). While both curcumin and AKBA treatments significantly inhibited colony formation at 2.5 μM, we found 5,000 μM aspirin was required to moderately inhibit colony formation in both HCT116 and SW480 cell lines indicating that curcumin was significantly more effective in inhibiting colony formation than aspirin (Fig. 6A). Similarly, results of the MTT assay indicated that 20,000 μM aspirin was needed to exert a similar cellular cytotoxicity to the equivalent of the combined curcumin and AKBA treatment of 10 μM for HCT116 cell line, while almost 30,000 μM aspirin was needed for SW480 cell line (Fig. 6B). In addition, while PI3KA wild type SW480 cell line appeared to be more resistant to aspirin than HCT116 cell line, the combined botanicals were just as potent in both cell lines. Although there are other parameters contributing to drug efficacy such as bioavailability and drug retention time, these comparisons highlight the potency of these botanicals against CRC cells.
Figure 6. Comparison of the effects of curcumin and AKBA to aspirin on CRC cells.
(A) The effects of aspirin on colony formation was compared to curcumin alone, and curcumin and AKBA on HCT116 and SW480 cell lines. (B) The cytotoxic effects of aspirin compared to the combination of curcumin and AKBA treatment on HCT116 and SW480 cell lines. (C) Schematic diagram depicting the role of curcumin and AKBA on modulation of miR-34a and miR-27a and subsequent cell cycle regulation.
Discussion
Herein we demonstrate for the first time that curcumin and AKBA can act synergistically to exert anti-tumorigenic effects in CRC cells, in both in vitro and in vivo experimental models. Analysis of gene-expression microarrays identified cell cycle regulation, cellular apoptosis, and proliferation as the primary protective mechanisms by which curcumin and AKBA act in CRC cell lines; which were subsequently validated in a series of molecular and functional analyses during the course of this study. Based upon data obtained from gene-expression microarrays, we illustrate that curcumin and AKBA regulated the expression of miR-34a and miR-27a, two miRNAs involved in cell cycle regulation in cancer and modulated their downstream target genes. Finally, we used a mouse xenograft model to confirm our in vitro data and demonstrated that the combination of these botanicals resulted in a synergistic suppression of tumor growth.
MiRNAs are a class of small non-coding RNAs which play critical roles in the regulation of gene expression. MiR-34a is a well-established tumor suppressor which regulates both cell cycle and apoptosis pathways. Therefore, it is not surprising that miR-34a is primarily regulated by p53, a key cell cycle regulating tumor suppressor (33). We demonstrated that curcumin and AKBA only upregulated miR-34a in the HCT116 cell line and not HCT116p53−/− and SW480 cell lines suggesting that these botanicals control miR-34a expression through p53 activation. MiR-34 is one of the miRNAs identified for its chemotherapeutic use and it is currently being clinically analyzed with patients who have unresectable primary liver cancer and advanced or metastatic liver cancer (NCT01829971). We over-expressed miR-34a in CRC cell lines which resulted in inhibition of cell proliferation and colony formation; however, it was noted that the effect was less pronounced in p53 mutated/deficient cell lines. These results suggest that interference in the miR-34a and p53 positive feed-back loop may have contributed to the lack of efficacy of miR-34a-induced inhibition of cell proliferation and colony formation (33). Considering p53 mutation occurs in the latter stages of colorectal tumorigenesis (42), the role of botanicals in upregulating miR-34a during initiation and progression stages of CRC is of importance. With curcumin and AKBA suppressing validated miR-34a target genes including cMyc, Cyclin D1, CDK4, CDK6 and Bcl-2, our data imply that these botanicals could be used therapeutically to upregulate miR-34a in colonic epithelial cells.
In contrast, miR-27a has been identified recently as a putative oncogene in CRC (38). MiR-27a facilitates proliferation through Sp protein repressor ZBTB10 and FBXW7 (38, 43) and the present study confirmed the oncogeneic role of miR-27a in CRC through series of knockdown experiments. Previous studies have demonstrated that curcumin has been shown to downregulate miR-27a in CRC cell lines (36, 37). While we confirmed these findings, we also demonstrated that curcumin and AKBA in combination can further suppress miR-27a expression in CRC cell lines. One of the oncogenic functions of miR-27a in CRC is through direct inhibition of the tumor suppressor FBXW7 (38). FBXW7 is a member of F-box family of proteins which interacts with Skp1 and CUL1 to form a ubiquitin ligase complex (44) that play a pivotal role in the regulating the cell cycle by degrading key proteins in cell division and determination of cell fate including, cMyc, Cyclin E1, c-Jun, and Notch (45). The present study demonstrated that treatment of CRC cells with curcumin and AKBA upregulated FBXW7 resulting in downregulation of its downstream target genes. Collectively, our data indicate that these botanicals play an important role in regulation of the miR-27a/FBXW7 axis. On the basis of the findings from this study, we propose a mechanism by which curcumin and ABKA control cell cycle regulation in CRC cells (Fig. 6C). Curcumin and AKBA can modulate miRNAs such as miR-34a and miR-27a in the presence of p53 to control cell cycle regulation. However, these botanicals can still maintain cell cycle regulation through miRNA regulation in the absence of p53. Although additional investigations are required to fully understand the complex mechanisms involved in miRNA regulation by curcumin and AKBA, the present study highlights the therapeutic potential of these botanicals to coordinate modulation of cancer-related miRNAs.
Mutations in p53 are found in nearly all types of cancers and is the most frequently mutated gene in CRC (46). p53 is known for its role in maintaining genomic integrity by regulating cell cycle and cell death pathways (47). The present study showed that the combination of curcumin and AKBA induced synergistic cytotoxicity in p53 deficient/mutated cell lines, but not p53 wild type cell lines. Although curcumin has been shown to induce apoptosis through p53-independently, it primarily induces apoptosis through stabilization of p53 through inhibition of MDM2 (48). We suspect that the synergism we observed between curcumin and AKBA in this study is a result of AKBA compensating for lack of curcumin’s cytotoxicity in these cell lines. Considering all cancers are heterogeneous, combining anti-tumorigenic agents may increase effectiveness of these agents in various human tumors. While further investigation is needed to clarify how these botanicals interact to overcome mutations in CRC, these compounds have a promising potential to provide safe and cost effective adjunctive treatment alongside conventional therapies.
In order to confirm the anti-tumorigenic properties of curcumin and AKBA in vivo, we generated xenograft tumors using human CRC cells in mice and treated these mice with curcumin and/or AKBA. As expected, treatment of mice with curcumin or AKBA resulted in decreased tumor proliferation. However, to our surprise, the combined treatment resulted in synergistic suppression of tumor growth. Although the synergistic tumor suppressive effect observed for the combined treatment was modest, this finding is important considering that consumption of these two botanicals concurrently is extremely safe. Given that curcumin and AKBA are both readily available and affordable, there is a significant potential for use of these botanicals to prevent CRC development.
Finally, to highlight the potency of these botanicals with more conventional chemopreventive drugs, we compared the anti-tumorigenic properties of curcumin and AKBA to aspirin. Recently, a clinical observational study concluded that daily consumption of aspirin, a non-steroidal anti-inflammatory drug, lowers the risk of CRC (49). The cytotoxicity of curcumin was over 2,000 times more than aspirin in vitro, while it suppressed cellular proliferation at a significantly lower dose than aspirin demonstrating that anti-tumorigenic potential of these botanicals far exceeded that of aspirin. Although our data along with many preclinical studies confirmed the anti-tumorigenic effects of botanicals, the poor bioavailability associated with both curcumin and AKBA has been perceived as a potential hindrance for their use in prevention trials (50, 51). However, more recently there is increasing research focus on improving bioavailability of botanicals including curcumin through development of new formulations (52). In addition, in vivo studies have demonstrated that curcumin exerts anti-tumorigenic effects when consumed orally (25, 53). Similarly we have also demonstrated previously that gavaging of AKBA resulted in attenuation of tumor growth in a mouse xenograft model (23). While the present study focused on anti-tumorigenic synergism between these botanicals through intraperitoneal administration, our study provides strong evidence for these two botanicals as potential chemotherapeutic agents. Furthermore, unlike aspirin, high levels of curcumin can be consumed safely without increasing the risk of gastrointestinal bleeding and peptic ulcer - the risks associated with continuous administration of aspirin (49). Additionally, daily consumption of these botanicals can provide added health benefits as curcumin is effective against other diseases such as rheumatoid arthritis and depression (54, 55).
In summary, we for the first time demonstrate that individual and combined treatment with curcumin and AKBA exerted their anti-tumorigenic effects, at least in part, by regulation of miRNAs and their downstream target genes involved in cell cycle regulation. Furthermore, using a mouse xenograft model we confirmed that curcumin or AKBA suppressed tumor growth, while the combination resulted in synergistic tumor suppression. Collectively, the present study highlights the novel therapeutic potential of utilizing the combined treatment of two botanicals, curcumin and AKBA, to inhibit CRC tumor growth.
Supplementary Material
Acknowledgments
Funding: The present work was supported by the grants R01 CA72851, CA 181572 and U01 CA187956 from the National Cancer Institute, National Institutes of Health, and funds from the Baylor Research Institute to A. Goel.
We would like to acknowledge Ms. Patricia Kraehe for technical assistance. We would like to thank Margaret Hinshelwood, PhD, manager of the Office of Scientific Publications, Baylor Charles A. Sammons Cancer Center, Dallas, for critical suggestions and editing to further improve the quality of this article.
Abbreviations
- AKBA
3 acetyl-11-keto-β-boswellic acid
- CRC
colorectal cancer
- CI
combination index
- DAPI
4′, 6-diamidino-2-phenylindole
Footnotes
Conflict of interest: None of the authors have any potential conflicts of interests to disclose.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA: a cancer journal for clinicians. 2009;59:225–49. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Willett WC. Diet and cancer: one view at the start of the millennium. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2001;10:3–8. [PubMed] [Google Scholar]
- 3.Buhrmann C, Mobasheri A, Matis U, Shakibaei M. Curcumin mediated suppression of nuclear factor-kappaB promotes chondrogenic differentiation of mesenchymal stem cells in a high-density co-culture microenvironment. Arthritis Res Ther. 2010;12:R127. doi: 10.1186/ar3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rao CV, Simi B, Reddy BS. Inhibition by dietary curcumin of azoxymethane-induced ornithine decarboxylase, tyrosine protein kinase, arachidonic acid metabolism and aberrant crypt foci formation in the rat colon. Carcinogenesis. 1993;14:2219–25. doi: 10.1093/carcin/14.11.2219. [DOI] [PubMed] [Google Scholar]
- 5.Pereira MA, Grubbs CJ, Barnes LH, Li H, Olson GR, Eto I, et al. Effects of the phytochemicals, curcumin and quercetin, upon azoxymethane-induced colon cancer and 7,12-dimethylbenz[a]anthracene-induced mammary cancer in rats. Carcinogenesis. 1996;17:1305–11. doi: 10.1093/carcin/17.6.1305. [DOI] [PubMed] [Google Scholar]
- 6.Huang MT, Wang ZY, Georgiadis CA, Laskin JD, Conney AH. Inhibitory effects of curcumin on tumor initiation by benzo[a]pyrene and 7,12-dimethylbenz[a]anthracene. Carcinogenesis. 1992;13:2183–6. doi: 10.1093/carcin/13.11.2183. [DOI] [PubMed] [Google Scholar]
- 7.Rao CV, Rivenson A, Simi B, Reddy BS. Chemoprevention of colon carcinogenesis by dietary curcumin, a naturally occurring plant phenolic compound. Cancer research. 1995;55:259–66. [PubMed] [Google Scholar]
- 8.Sethi S, Li Y, Sarkar FH. Regulating miRNA by natural agents as a new strategy for cancer treatment. Current drug targets. 2013;14:1167–74. doi: 10.2174/13894501113149990189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005;120:15–20. doi: 10.1016/j.cell.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 10.Calin GA, Croce CM. MicroRNA signatures in human cancers. Nature reviews Cancer. 2006;6:857–66. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- 11.Subramaniam D, Ponnurangam S, Ramamoorthy P, Standing D, Battafarano RJ, Anant S, et al. Curcumin induces cell death in esophageal cancer cells through modulating Notch signaling. PloS one. 2012;7:e30590. doi: 10.1371/journal.pone.0030590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang CH, Yue J, Sims M, Pfeffer LM. The curcumin analog EF24 targets NF-kappaB and miRNA-21, and has potent anticancer activity in vitro and in vivo. PloS one. 2013;8:e71130. doi: 10.1371/journal.pone.0071130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali S, Ahmad A, Banerjee S, Padhye S, Dominiak K, Schaffert JM, et al. Gemcitabine sensitivity can be induced in pancreatic cancer cells through modulation of miR-200 and miR-21 expression by curcumin or its analogue CDF. Cancer research. 2010;70:3606–17. doi: 10.1158/0008-5472.CAN-09-4598. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Kronski E, Fiori ME, Barbieri O, Astigiano S, Mirisola V, Killian PH, et al. miR181b is induced by the chemopreventive polyphenol curcumin and inhibits breast cancer metastasis via down-regulation of the inflammatory cytokines CXCL1 and -2. Molecular oncology. 2014;8:581–95. doi: 10.1016/j.molonc.2014.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sreenivasan S, Thirumalai K, Danda R, Krishnakumar S. Effect of curcumin on miRNA expression in human Y79 retinoblastoma cells. Current eye research. 2012;37:421–8. doi: 10.3109/02713683.2011.647224. [DOI] [PubMed] [Google Scholar]
- 16.Liu JJ, Nilsson A, Oredsson S, Badmaev V, Zhao WZ, Duan RD. Boswellic acids trigger apoptosis via a pathway dependent on caspase-8 activation but independent on Fas/Fas ligand interaction in colon cancer HT-29 cells. Carcinogenesis. 2002;23:2087–93. doi: 10.1093/carcin/23.12.2087. [DOI] [PubMed] [Google Scholar]
- 17.Takada Y, Ichikawa H, Badmaev V, Aggarwal BB. Acetyl-11-keto-beta-boswellic acid potentiates apoptosis, inhibits invasion, and abolishes osteoclastogenesis by suppressing NF-kappa B and NF-kappa B-regulated gene expression. J Immunol. 2006;176:3127–40. doi: 10.4049/jimmunol.176.5.3127. [DOI] [PubMed] [Google Scholar]
- 18.Glaser T, Winter S, Groscurth P, Safayhi H, Sailer ER, Ammon HP, et al. Boswellic acids and malignant glioma: induction of apoptosis but no modulation of drug sensitivity. British journal of cancer. 1999;80:756–65. doi: 10.1038/sj.bjc.6690419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu M, Xia L, Hua H, Jing Y. Acetyl-keto-beta-boswellic acid induces apoptosis through a death receptor 5-mediated pathway in prostate cancer cells. Cancer research. 2008;68:1180–6. doi: 10.1158/0008-5472.CAN-07-2978. [DOI] [PubMed] [Google Scholar]
- 20.Yadav VR, Prasad S, Sung B, Gelovani JG, Guha S, Krishnan S, et al. Boswellic acid inhibits growth and metastasis of human colorectal cancer in orthotopic mouse model by downregulating inflammatory, proliferative, invasive and angiogenic biomarkers. International journal of cancer Journal international du cancer. 2012;130:2176–84. doi: 10.1002/ijc.26251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pang X, Yi Z, Zhang X, Sung B, Qu W, Lian X, et al. Acetyl-11-keto-beta-boswellic acid inhibits prostate tumor growth by suppressing vascular endothelial growth factor receptor 2-mediated angiogenesis. Cancer research. 2009;69:5893–900. doi: 10.1158/0008-5472.CAN-09-0755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park B, Sung B, Yadav VR, Cho SG, Liu M, Aggarwal BB. Acetyl-11-keto-beta-boswellic acid suppresses invasion of pancreatic cancer cells through the downregulation of CXCR4 chemokine receptor expression. International journal of cancer Journal international du cancer. 2011;129:23–33. doi: 10.1002/ijc.25966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Takahashi M, Sung B, Shen Y, Hur K, Link A, Boland CR, et al. Boswellic acid exerts antitumor effects in colorectal cancer cells by modulating expression of the let-7 and miR-200 microRNA family. Carcinogenesis. 2012;33:2441–9. doi: 10.1093/carcin/bgs286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu G, Ren G, Xu X, Yuan H, Wang Z, Kang L, et al. Combination of curcumin and green tea catechins prevents dimethylhydrazine-induced colon carcinogenesis. Food Chem Toxicol. 2010;48:390–5. doi: 10.1016/j.fct.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 25.Majumdar AP, Banerjee S, Nautiyal J, Patel BB, Patel V, Du J, et al. Curcumin synergizes with resveratrol to inhibit colon cancer. Nutrition and cancer. 2009;61:544–53. doi: 10.1080/01635580902752262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chou TC. Drug combination studies and their synergy quantification using the Chou-Talalay method. Cancer research. 2010;70:440–6. doi: 10.1158/0008-5472.CAN-09-1947. [DOI] [PubMed] [Google Scholar]
- 27.Link A, Shin SK, Nagasaka T, Balaguer F, Koi M, Jung B, et al. JC virus mediates invasion and migration in colorectal metastasis. PloS one. 2009;4:e8146. doi: 10.1371/journal.pone.0008146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jascur T, Fotedar R, Greene S, Hotchkiss E, Boland CR. N-methyl-N′-nitro-N-nitrosoguanidine (MNNG) triggers MSH2 and Cdt2 protein-dependent degradation of the cell cycle and mismatch repair (MMR) inhibitor protein p21Waf1/Cip1. The Journal of biological chemistry. 2011;286:29531–9. doi: 10.1074/jbc.M111.221341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shakibaei M, Mobasheri A, Lueders C, Busch F, Shayan P, Goel A. Curcumin enhances the effect of chemotherapy against colorectal cancer cells by inhibition of NF-kappaB and Src protein kinase signaling pathways. PloS one. 2013;8:e57218. doi: 10.1371/journal.pone.0057218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shakibaei M. Inhibition of chondrogenesis by integrin antibody in vitro. Exp Cell Res. 1998;240:95–106. doi: 10.1006/excr.1998.3933. [DOI] [PubMed] [Google Scholar]
- 31.Yokoyama Y, Dhanabal M, Griffioen AW, Sukhatme VP, Ramakrishnan S. Synergy between angiostatin and endostatin: inhibition of ovarian cancer growth. Cancer research. 2000;60:2190–6. [PubMed] [Google Scholar]
- 32.Oltvai ZN, Milliman CL, Korsmeyer SJ. Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell. 1993;74:609–19. doi: 10.1016/0092-8674(93)90509-o. [DOI] [PubMed] [Google Scholar]
- 33.Chen F, Hu SJ. Effect of microRNA-34a in cell cycle, differentiation, and apoptosis: a review. J Biochem Mol Toxicol. 2012;26:79–86. doi: 10.1002/jbt.20412. [DOI] [PubMed] [Google Scholar]
- 34.Pagliuca A, Valvo C, Fabrizi E, di Martino S, Biffoni M, Runci D, et al. Analysis of the combined action of miR-143 and miR-145 on oncogenic pathways in colorectal cancer cells reveals a coordinate program of gene repression. Oncogene. 2013;32:4806–13. doi: 10.1038/onc.2012.495. [DOI] [PubMed] [Google Scholar]
- 35.Hermeking H. MicroRNAs in the p53 network: micromanagement of tumour suppression. Nature reviews Cancer. 2012;12:613–26. doi: 10.1038/nrc3318. [DOI] [PubMed] [Google Scholar]
- 36.Noratto GD, Jutooru I, Safe S, Angel-Morales G, Mertens-Talcott SU. The drug resistance suppression induced by curcuminoids in colon cancer SW-480 cells is mediated by reactive oxygen species-induced disruption of the microRNA-27a-ZBTB10-Sp axis. Mol Nutr Food Res. 2013 doi: 10.1002/mnfr.201200609. [DOI] [PubMed] [Google Scholar]
- 37.Gandhy SU, Kim K, Larsen L, Rosengren RJ, Safe S. Curcumin and synthetic analogs induce reactive oxygen species and decreases specificity protein (Sp) transcription factors by targeting microRNAs. BMC cancer. 2012;12:564. doi: 10.1186/1471-2407-12-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jahid S, Sun J, Edwards RA, Dizon D, Panarelli NC, Milsom JW, et al. miR-23a promotes the transition from indolent to invasive colorectal cancer. Cancer Discov. 2012;2:540–53. doi: 10.1158/2159-8290.CD-11-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheng TS, Chen WC, Lin YY, Tsai CH, Liao CI, Shyu HY, et al. Curcumin-targeting pericellular serine protease matriptase role in suppression of prostate cancer cell invasion, tumor growth, and metastasis. Cancer prevention research. 2013;6:495–505. doi: 10.1158/1940-6207.CAPR-12-0293-T. [DOI] [PubMed] [Google Scholar]
- 40.Jutooru I, Chadalapaka G, Lei P, Safe S. Inhibition of NFkappaB and pancreatic cancer cell and tumor growth by curcumin is dependent on specificity protein down-regulation. The Journal of biological chemistry. 2010;285:25332–44. doi: 10.1074/jbc.M109.095240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liao X, Lochhead P, Nishihara R, Morikawa T, Kuchiba A, Yamauchi M, et al. Aspirin use, tumor PIK3CA mutation, and colorectal-cancer survival. The New England journal of medicine. 2012;367:1596–606. doi: 10.1056/NEJMoa1207756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fearon ER, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell. 1990;61:759–67. doi: 10.1016/0092-8674(90)90186-i. [DOI] [PubMed] [Google Scholar]
- 43.Mertens-Talcott SU, Chintharlapalli S, Li X, Safe S. The oncogenic microRNA-27a targets genes that regulate specificity protein transcription factors and the G2-M checkpoint in MDA-MB-231 breast cancer cells. Cancer research. 2007;67:11001–11. doi: 10.1158/0008-5472.CAN-07-2416. [DOI] [PubMed] [Google Scholar]
- 44.Wang Z, Inuzuka H, Zhong J, Wan L, Fukushima H, Sarkar FH, et al. Tumor suppressor functions of FBW7 in cancer development and progression. FEBS Lett. 2012;586:1409–18. doi: 10.1016/j.febslet.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Welcker M, Clurman BE. FBW7 ubiquitin ligase: a tumour suppressor at the crossroads of cell division, growth and differentiation. Nature reviews Cancer. 2008;8:83–93. doi: 10.1038/nrc2290. [DOI] [PubMed] [Google Scholar]
- 46.Hollstein M, Sidransky D, Vogelstein B, Harris CC. p53 mutations in human cancers. Science. 1991;253:49–53. doi: 10.1126/science.1905840. [DOI] [PubMed] [Google Scholar]
- 47.Levine AJ, Oren M. The first 30 years of p53: growing ever more complex. Nature reviews Cancer. 2009;9:749–58. doi: 10.1038/nrc2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Choudhuri T, Pal S, Das T, Sa G. Curcumin selectively induces apoptosis in deregulated cyclin D1-expressed cells at G2 phase of cell cycle in a p53-dependent manner. The Journal of biological chemistry. 2005;280:20059–68. doi: 10.1074/jbc.M410670200. [DOI] [PubMed] [Google Scholar]
- 49.Cook NR, Lee IM, Zhang SM, Moorthy MV, Buring JE. Alternate-day, low-dose aspirin and cancer risk: long-term observational follow-up of a randomized trial. Ann Intern Med. 2013;159:77–85. doi: 10.7326/0003-4819-159-2-201307160-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB. Bioavailability of curcumin: problems and promises. Molecular pharmaceutics. 2007;4:807–18. doi: 10.1021/mp700113r. [DOI] [PubMed] [Google Scholar]
- 51.Sterk V, Buchele B, Simmet T. Effect of food intake on the bioavailability of boswellic acids from a herbal preparation in healthy volunteers. Planta Med. 2004;70:1155–60. doi: 10.1055/s-2004-835844. [DOI] [PubMed] [Google Scholar]
- 52.Prasad S, Tyagi AK, Aggarwal BB. Recent Developments in Delivery, Bioavailability, Absorption and Metabolism of Curcumin: the Golden Pigment from Golden Spice. Cancer Res Treat. 2014;46:2–18. doi: 10.4143/crt.2014.46.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tu SP, Jin H, Shi JD, Zhu LM, Suo Y, Lu G, et al. Curcumin induces the differentiation of myeloid-derived suppressor cells and inhibits their interaction with cancer cells and related tumor growth. Cancer prevention research. 2012;5:205–15. doi: 10.1158/1940-6207.CAPR-11-0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chandran B, Goel A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytotherapy research: PTR. 2012;26:1719–25. doi: 10.1002/ptr.4639. [DOI] [PubMed] [Google Scholar]
- 55.Sanmukhani J, Satodia V, Trivedi J, Patel T, Tiwari D, Panchal B, et al. Efficacy and Safety of Curcumin in Major Depressive Disorder: A Randomized Controlled Trial. Phytotherapy research: PTR. 2013 doi: 10.1002/ptr.5025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.