Abstract
The purpose of the current study was to determine if, and how, Hispanic adolescents receiving clinical treatment differ from their peers who are not in treatment on the 8 domains (family economic stress, cultural or educational stress, acculturation-gap stress, immigration stress, discrimination stress, family immigration stress, community or gang related stress) of cultural stress (HSI-A), and if the relation between cultural stress domains and depressive symptomology differed by group membership (clinical versus non-clinical). The sample included 1,254 Hispanic adolescents. The clinical sample had significantly higher scores of cultural stress (p < .05) and mean depression scores (< .001). All 8 domains of HSI-A stress were correlated with depression (p < .05). In the GLM, only family economic, acculturation gap, family immigration, discrimination, and family drug stress had a unique effect on depression and effect varied by group. Acculturation gap stress was associated with depression for the non-clinical group but not the clinical group (p < .001) and community gang stress was more strongly related to depression for the clinical group (p < .05).
Keywords: Cultural Stress, Minority Stress, Hispanic Adolescents, Hispanic Stress Inventory-Adolescent Version
Hispanic adolescents report greater sadness, depressive symptoms, suicidal ideation and suicidal attempts than do their non-Hispanic peers (CDC, 2012; Nock et al., 2013; Zayas, Lester, Cabassas, & Fortuna, 2005). Depressive symptoms among Hispanic adolescent females are particularly alarming, with suicidal and self-harm behavior nearly three times higher than adolescents from the general population (Zayas, 2010). In recent years, a number of scholars have worked to understand the factors that contribute to depression and suicide among Hispanic adolescents and have found that racial and ethnic minorities are often exposed to a disproportionate number of acute and chronic stressors compared to non-Hispanic white adults in the U.S (Boardman, 2004; Boardman & Alexander, 2011; Schulz, Israel, Williams, Perker, Becker, & James, 2000). These findings are critical, as research suggests that individuals exposed to significant life stressors present with worse mental health outcomes (Boardman & Alexander, 2011; Kessler, 1997).
For Hispanics, these stressors are often “culturally based” and have been linked to depressive symptomology in Hispanic adolescents (e.g., Cervantes & Córdova, 2011; Lorenzo-Blanco et al., 2012; Zayas, 2010). Studies on cultural stress find that in addition to the normative strains of adolescence, such as changing family expectations, and planning for the future (Guinn & Vincent, 2002; Robson & Cook, 1995), Hispanic and other minority adolescents face non-normative stressors associated with their culture and minority status (Cordova & Cervantes, 2010; Garcia & Magnuson, 2005; Rice & Dolgin, 2002). These culturally specific stressors include reactions to anti-immigrant attitudes, familial separation related to immigrant status (McGuire & Martin, 2007), and the experience of negative public references toward their ethnic identity (Cervantes, Fisher, Córdova & Napper, 2011; Córdova & Cervantes, 2010). The stress associated with acculturation has also been related to negative mental health outcomes (Rogler, 1994; U.S. DHHS, 2001; Vega, Gil, Warheit, Zimmerman & Apospori, 1993; Vega, Kolody, Aguilar-Gaxiola, Alderete, Catalano & Caraveo-Anduaga, 1998) and suicide attempts (Fortuna, Perez, Canino, Sribney & Alegría, 2007; Zayas, Lester, Cabassa, & Fortuna, 2005) in Hispanic adolescents.
Efforts have been made to more accurately measure culturally specific constructs that seem to contribute to depressive symptoms and suicidal behavior in Hispanic youth. To that end, several validated measures of cultural stress have emerged over the past two decades including the Social, Attitudinal, Familial and Environmental (SAFE) Scale (Mena, Padilla & Maldonado, 1987), the Hispanic Stress Inventory (Cervantes, Padilla, & Salgado de Snyder, 1991) for adults and the Hispanic Stress Inventory-Adolescent Version (HSI-A) for Hispanic adolescents (Cervantes et al., 2011). A series of studies exploring stress among Hispanic adolescents was conducted with the intent of developing a Hispanic Stress Inventory, Adolescent Version (Cervantes et al., 2011; Cervantes, Goldbach & Padilla, 2012). This series of studies identified eight unique domains of cultural stress including: family economic stress, cultural and educational stress, acculturation-gap stress, immigration stress, discrimination stress, family immigration stress, drug-related stress and community/gang related stress,. Participants that reported higher levels of cultural stress experienced significantly higher internalizing symptoms (e.g., depression, anxiety) and externalizing behaviors (e.g., conduct problems) (Cervantes et al., 2011). Generational differences in cultural stress (Cervantes, Padilla, & Napper & Goldbach, 2013), school-related stress exposure (Cervantes & Shelby, 2013) and gender differences (Reynolds, Cervantes, Fisher, & Fagen, 2012) have also been explored using the HSI-A; each of these studies have found a relation between mental health outcomes and culturally based stress.
Assessment and Treatment of Hispanic Adolescents
There is little information available on how cultural stressors influence the mental health of youth receiving clinical treatment. Identifying and addressing the unique needs of Hispanic adolescents in clinical treatment settings is particularly important, as these youth often present with comorbid problems that include delinquency, substance use, distress, and depression (Garcia, 2010; Rew, 2005; Rodriguez, et al., 2009; Rodriguez et al., 2007; Zayas et al., 2005), and they more likely to drop-out of clinical treatment than are non-Hispanic white adolescents (Bluthenthal et al., 2007). Most clinical studies, however, have been unable to explore the unique role cultural stressors among youth receiving clinical treatment. The majority of clinical studies report outcomes based on DSM diagnostic categories, standardized measures of depression, anxiety or other behavioral problem checklists, or from simply translated versions of existing measures (Cervantes & Garcia, 1995; Cervantes & Bui, in press). Furthermore, research on Hispanic adolescents in clinical treatment has focused primarily on substance use treatment (Gil, Wagner & Tubman, 2004; Robbins et al., 2011) and does not include treatments of mental health concerns including depressive symptoms. A better understanding of the relation between cultural stress and depressive symptoms in a clinical sample of Hispanic youth has important implications for treatment.
The purpose of the current study was to determine if, and how, Hispanic adolescents receiving clinical treatment differ from their peers who are not in treatment on the 8 domains (family economic stress, cultural or educational stress, acculturation-gap stress, immigration stress, discrimination stress, family immigration stress, family drug-related stress, community or gang related stress) of cultural stress (HSI-A), and if the relation between cultural stress domains and depressive symptomology differed by group membership (clinical versus non-clinical). Thus, the questions guiding this research included:
How do scores on the 8 domains of cultural stress and depression symptoms differ for adolescents in clinical treatment compared to adolescents in non-clinical settings, controlling for age, gender, ethnicity, and parental employment?
What is the association between the 8 domains of stress and depression scores?
Does group membership moderate the association between cultural stress and depression scores?
What are the unique contributions of each stress subscale to depression symptoms for youth in the sample?
We expected that Hispanic adolescents who receive clinical treatment would have higher scores on the 8 domains of cultural stress, as well as greater depression symptomology. Additionally, given that acculturation related stress related to acculturation gap, discrimination, immigration, and family economic status, has been linked to mental health problems in Hispanic youth (Cervantes, Padilla, Goldbach & Napper, 2013), cultural stress scores are likely to have a stronger relation to Children’s Depression Inventory-2 (CDI) scores for adolescents in the clinical group. The research questions, and the analysis presented below, contribute to the knowledge in this area by articulating how and why youth in treatment may be more affected by culturally based stressors than their non-clinical peers. Results could better inform early screening, diagnosis and treatment planning, particularly in terms of symptoms related to depression.
Methods
Sample
Data were collected on 1,651 adolescents. To be included in the current study, adolescents had to self-report as Hispanic or Latino, be 11–19 years of age, and have a valid score on Hispanic Stress Inventory –Adolescent Version (n=1,187). Among the 1,187 youth in the sample, 987 adolescents were in the non-clinical group and 204 were in the clinical group. Clinic samples were drawn from 2 sites and included an outpatient, university based adolescent substance abuse treatment center (Miami) and a school based outpatient mental health counseling center (Los Angeles). Non-clinical youth were surveyed in a random classroom sampling design in 4 urban cities, each with a large and diverse ethnic, racial and immigrant compositions (Los Angeles, Miami, El Paso, and Lawrence), while youth receiving clinical behavioral health services were drawn from the Los Angeles, Miami and El Paso sites. Purposive sampling was used to obtain a diverse clinical group from both school based counseling centers, as well as community mental health and substance abuse treatment facilities. Adolescents in the clinic sample were being treated for a number of conditions ranging from: major depression (10.3%), depressive disorder not otherwise specified (4.7%), generalized anxiety disorder (17%), anxiety disorder not otherwise specified (2.7%), attention deficit hyperactivity (20.2%), oppositional defiant disorder (7.1%), language or other learning disorders (3.2%) and substance use disorders such as alcohol abuse (12.6%) and opioid abuse (2.1%). In addition, roughly 3% of the clinical sample received treatment but the diagnosis for such treatment was missing.
Measures
The primary independent variable of interest in the current study was cultural stress. Cultural stress was measured using the Hispanic Stress Inventory-Adolescent version (HSI-A). The HSI-A includes 71 items that measure exposure to life-event stressors related to minority status among Hispanics adolescents in the United States. If a participant reported experiencing the stressor, he or she was asked to appraise the severity of the stressor using a five-point Likert scale; 1= not at all worried or tense, 2= a little worried or tense, 3 = moderately worried or tense, 4 = very worried or tense, 5 = extremely worried or tense. In circumstances where the participant reported they had not experienced the stressor, the appraisal scores was coded to 1 = not at all worried or tense. The HSI-A was validated using factor analysis for both the Spanish and English version of the measure (see Cervantes et al., 2011 for more information about psychometric properties of the HSI-A). Eight unique domains of cultural stress (e.g. subscales) were identified, including family economic stress (12 items), cultural or educational stress (14 items), acculturation-gap stress, (12 items), immigration stress (7 items), discrimination stress (6 items), family immigration stress (7 items), community or gang related stress (8 items), and family and drug-related stress (5 items). Higher stress appraisal scores reflected greater intensity of the life-stress experiences.
The validity of the HSI-A scales was previously established with immigrant and U.S.-born Hispanic adolescents in the United States (see Cervantes et al., 2011). In the current study, the HSI-A total scale and subscales demonstrated strong reliability in both the clinical and non-clinical samples. In the clinical sample, the cronbach reliability for total HSI-A scale was strong, α = .96 and the stress subscales ranged from α = .93 to α= .56, with the lowest reliability in the family drug stress subscale. In the non-clinical group, cronbach reliability coefficients were similar to those previously reported (Cervantes et al., 2011), ranging from α = .66 to α = .85, with the lowest reliability in the nonclinical group also being the family drug stress subscale.
The dependent variable was depressive symptoms, as measured by the Children’s Depression Inventory 2 (CDI2; Kovacs & Multi-Health Systems Staff, 2011). The CDI2 was selected as a measure of depressive symptoms because of its previous use with Hispanic populations (Cowell, Gross, McNaughton, Ailey, & Fogg, 2005; Worchell, Hughes, Hall, Stanton, Stanton & Little, 1990). The CDI2 consists of 27 items that assess negative mood, interpersonal problems, ineffectiveness, anhedonia, and negative self-esteem. For each item, participants are asked to select the statement that best described their mood. CDI2 item is assigned a numerical value from 0 to 2, with the higher values attributed to more clinically severe behavior. In the current study, the total score for CDI2 was used. Cronbach reliability analysis for the sample revealed strong internal consistency in both the non-clinical (α= .89) and the clinical (α= .92) groups.
Child’s and parent’s characteristics were the two sets of covariates included in the models. Consistent with previous research, these included age (Nolen-Hoeksema & Girgus, 1994), gender (Zayas, Torres, & Kyriakakis, 2010), parental employment (White, Roosa, Weaver & Nair, 2009), parental or child nativity (Ng’andu & Ryan, 2011), and ethnicity (Walsemann, Gee & Geronimus, 2009). For child characteristics child gender was included as a covariate, 1= male and 2= female. Child age was a continuous variable, ranging from 11–19 years old. Child nativity was obtained from a single item question that asked youth, “Were you born in the United States” (0 = born outside of the United States, 1=born in the United States). Child ethnicity was obtained from a single item question that asked, “What is your specific Hispanic or Latino ethnicity?” Data were originally coded, 1 = Mexican or Mexican American, 2 = Central American, 3 = South American, 4 = Cuban, 5= Puerto Rican, 6= Dominican, 7= Mixed, 8= Other. Due to the large number of levels for this variable, we examined the differences between the clinical and non-clinical groups by child ethnicity. We found that most of the difference between the clinical and non-clinical group on ethnicity was accounted for with a dichotomous variable, 1= Mexican, Central American, Cuban and Mixed origin (91% in the clinical group and 74% in the nonclinical group) and 0 = Dominican, South American, Puerto Rican, and other origin (9% in the clinical group and 26% in the nonclinical group). Most of this difference was accounted for by the difference in the percentage of Dominican origin adolescents in each group.
Parent characteristics included nativity and employment status of the father and mother. Parental nativity was constructed using two single-item questions, asking the adolescent if their mother and or father was born in the United States (1= yes and 2= no). A single variable was computed combing the responses from both parents, 0= both parents born in the United States and 1= one or both parents born outside of the United States. The final covariate included in the model was parental employment. This variable was constructed using two single-item questions about maternal and paternal employment, 0= both parents work part-time or full-time and 1= Other. The Other category combined households with two unemployed parents, one unemployed parent, and single parents that were both employed and unemployed together in a single category. We dichotomized this variable to highlight differences between two-parent households, where both parents work, and families that may experience some economic hardship, such as single-parent families, families with one income, or families with two unemployed parents. A more sensitive marker of economic hardship, such as income, financial hardship, and material hardship, would have provided a stronger analysis of the influence of parental socioeconomic status on depression symptomology. No other measures of economic hardship were available in the dataset; as such, parental employment was used as a proxy to capture this construct.
Data analysis plan
Cross-tabulations, including frequencies and percentages and t-tests (means and standard deviations) were conducted to examine group in sample characteristics, such as gender, age, child nativity, parental nativity and unemployment, generally associated with depressive symptoms in Hispanic adolescents. To answer the first research question, “How do scores on the HSI-A domains of cultural stress differ for adolescents in clinical treatment compared to adolescents in non-clinical settings,” we conducted a univariate analysis of variance (ANOVA) on each dependent variable. We selected the ANOVA analysis over a multivariate analysis of variance because we were interested in the results for each dependent variables and not a weighted composite of dependent variables (Huberty & Morris, 1989). For each ANOVA analysis, the Benjamini-Hochberg procedure was applied to test the false discovery rate by correcting for multiple comparisons (Benjamini & Hochberg, 1995). The results were first sorted in the order by their uncorrected p-value, from lowest to highest. Then the false discovery rate was calculated by dividing the uncorrected p-value by position of the p-value (smallest is 0.125*.05, the next smallest is 0.25*.05, etc.). If the p-value retained its significance, then the null hypothesis was rejected and the difference in the stress domains between the clinical and non-clinical groups, controlling for the covariates, was assumed to be statistically significant (Benjamini & Hochberg, 1995). We controlled for covariates, including age, gender, child ethnicity and parental employment to provide a more sensitive analysis of between-group differences in the HSI-A stress domains.
To answer research questions 2–4, we conducted a series of general linear models (GLM). Prior to conducting GLM, we determined which covariates were significantly associated with depression. While gender was marginally related to depression in the sample (F = 2.89, p = .09), other covariates including child age (F = .06, p = .80), child ethnicity (F = .06, p = .9, p = .81), parental nativity (F = .00, p = .90), parental employment (F= 1.84, p = .18), and language (F = .09, p = .91) were not associated with depression. With the exception of gender, which was marginally significant, non-significant covariates were excluded from the analyses. Finally, HSI-A stress domains were centered at the mean and interaction variables between each stress domain and group membership were created (e.g., interaction effect).
Missing data
In the sample, 30% were missing one or more responses on the dependent variable, CDI2 depression survey tool. We compared demographic characteristics on observations missing the CDI2 variable to those with complete data. Results suggest these subsamples are statistically different from one another on key demographic variables. Observations with missing data on the CDI2 were significantly more likely to be female (X2=27.55, p < .001). In the sample, 17.4% of the missing data were in female observations to 12.6% male. Likewise, there were statistically significant differences in complete observations by age (t= 8.209 [df = 984.61], p <. 001). Participants with missing values on the CDI2 were younger (mean = 14.21 years) compared to complete cases (mean=14.97). Roughly 79% of the cases with missing data on the dependent variable were adolescents who identified as having Mexican origin. Furthermore, adolescents with fathers born in the United States were statistically more likely to having missing data on the CDI2 than were adolescents with foreign-born fathers (X2= 4.06, p < .05). However, neither nativity status of the adolescent nor nativity status of the adolescents’ mother was associated with a greater likelihood of missing data on the CDI2 variable.
Analyses revealed significant differences in demographic characteristics between participants with CDI2 scores compared to those with missing data on the CDI2 scores. As such, we assumed that data were not completely missing at random and therefore selected multiple imputation procedures to address the missing data on the CDI2 scores. Multiple imputation assumes that the data are missing at random but not completely at random. Using the PROC MI procedure in SAS, we performed multiple imputation with the Markov Chain Monte Carlo (MCMC) method. MCMC is commonly used in the social and behavioral sciences to address data that assumed to be missing at random (Horton & Kleinman, 2007).
To start the imputation process, we first identified other mental health variables that could be used to impute the missing values on the CDI2 depression scale. The Youth Self-Report (YSR) was selected to impute missing values for the CDI2 depression scores. The YSR is a validated screening measure used to assess mental health problems in youth, 11 years and older. The measure comprises 8 symptoms subscales, anxious/depressed, withdrawn/depressed and somatic symptoms, as well as social, thought, aggressive, attention, and rule-breaking problems. These scales were then combined to differentiate internalizing and externalizing symptoms in youth (CAMH, 2009). The internalizing and externalizing symptoms subscales were then used to facilitate the imputation. Ten datasets were generated for each of the ANOVA and GLM procedures and the final results were pooled to give an average of the imputed datasets.
RESULTS
Sample characteristics
Table 1 shows descriptive characteristics of the sample. There were marginally significant differences in gender by group membership (X2 = 3.66, p = .06). The percentage of male to female participants in the clinical subsample was slightly higher with males representing 53.0% of the clinical sample compared to 47.0% of females. The mean age of adolescents in the sample was 14.86 (SD = 1.79).
Table 1.
Sample characteristics of Hispanic adolescents and families in the sample by group membership
| Variable | Clinical sample (n=268) | Non-clinical sample (n=1197) | T/Chi-square statistic |
|---|---|---|---|
| Mean age (standard deviation) | 15.21 (1.61) | 14.80 (1.82) | 7.79** |
| Gender | 3.66 | ||
| Male | 104 (51.5%) | 432 (44.1%) | |
| Female | 98 (48.5%) | 547 (55.9%) | |
| National origin | 34.95*** | ||
| Mexican/Mexican American | 107 (53.8%) | 456 (47.4%) | |
| Central American | 17 (8.5%) | 52 (5.4%) | |
| South American | 5 (2.5%) | 35 (3.6%) | |
| Cuban | 30 (15.1%) | 118 (12.3%) | |
| Puerto Rican | 10 (5.0%) | 74 (7.7%) | |
| Dominican | 1 (0.5%) | 126 (13.1%) | |
| Mixed | 27 (13.6%) | 87 (9.0%) | |
| Other | 2 (1.0%) | 14 (1.5%) | |
| Adolescent born outside U.S. | 35 (17.2%) | 152 (15.5%) | .393 |
| One or both parents foreign-born | 168 (83.2%) | 833 (85.5%) | .733 |
| Both parents born inside the U.S. | 34 (16.8%) | 141 (14.5%) | |
| Language spoken at home | 5.04 | ||
| English | 49 (24.4%) | 232 (23.8%) | |
| Spanish | 68 (33.8%) | 263 (27.0%) | |
| Both English and Spanish | 84 (41.8%) | 478 (49.0%) | |
| Other | 0 (0%) | 2 (0.2%) | |
| Two parents employed | 82 (40.0%) | 541 (55.4%) | 14.91*** |
p<.001,
p<.01,
P<.05,
In the sample, nearly half of the participants were of Mexican origin. The remaining proportion of the sample was primarily of Central and South American and Caribbean origins. However, differences in ethnic background by clinical or nonclinical group membership were statistically significant. In the clinical sample there was a greater proportion of youth of Mexican, Cuban and Mixed backgrounds compared to the non-clinical sample. In the non-clinical sample, there were a greater proportion of South American, Dominican and Puerto Rican youth than in the clinical group. While most adolescents in the sample were born in the United States, the majority lived with at least one immigrant parent. Only about 16% of the adolescent sample was foreign born; however, roughly 85% of adolescents in the clinical and non-clinical sample had at least one immigrant parent. In both the clinical and non-clinical samples, most adolescents reported speaking both Spanish and English in the household. Differences in adolescents’ nativity, parental nativity, and preferred language by group membership were not statistically significant. Finally, there were significant group differences in parental employment by group. Adolescents in the non-clinical group were more likely to live in a household with two working parents than were youth in the clinical sample.
Analyses for each research questions
Research question 1: How do scores on the 8 domains of cultural stress differ for adolescents in clinical treatment compared to adolescents in non-clinical settings, controlling for child age, gender, ethnicity, and parental employment?
Findings from a series of ANOVA tests revealed group difference on 7 of the 8 HSI-A stress domains and depression scores between the clinical and non-clinical subsamples. Adolescents in the clinical group had significantly higher scores on the community gang, family economic stress, community or educational stress acculturation gap stress, family immigration, discrimination stress, and immigrant stress subscales. The group differences in stress on these subscales were significant even after the Benjamini-Hochberg test corrected for multiple tests. Group differences in stress on the family drug stress subscale did not meet the requirements for significance.
Also in Table 2 are results showing significant mean differences in the clinical and non-clinical group on depression scores. Adolescents in the clinical group had significantly higher depression scores, as measured by the CDI2, compared to adolescents in the non-clinical group. These mean differences remained significant even after child age, gender and ethnicity, and parental employment, were controlled for in the analysis.
Table 2.
Means (standard deviations) of HSI-A stress domains and depression, controlling for age, gender, ethnicity, and parental employment
| Independent variables | Clinical sample Mean (SD) |
Non-clinical sample Mean (SD) |
F-statistic | P=values |
|---|---|---|---|---|
| Community and gang stress | 1.43 (.68) | 1.19 (.38) | 39.79 | <. 0001 |
| Family economic stress | 1.45 (.78) | 1.22 (.44) | 35.58 | < .0001 |
| Culture and education stress | 1.19 (.46) | 1.09 (.26) | 19.60 | < .0001 |
| Acculturation gap stress | 1.48 (.63) | 1.35 (.51) | 13.63 | .0002 |
| Family immigration stress | 1.31 (.64) | 1.19 (.46) | 11.92 | .0006 |
| Child Depression Inventory-2 (DV) | 9.24 (.23) | 11.44 (.21) | 10.95 | .0009 |
| Discrimination stress | 1.23 (.56) | 1.13 (.37) | 10.94 | .001 |
| Immigration related stress | 1.25 (.66) | 1.17 (.48) | 6.84 | .009 |
| Family drug stress | 1.32 (.48) | 1.36 (.50) | 2.86 | .09 |
Note: Benjamini-Hochberg test was conducted to adjust for multiple tests. P-values are rank ordered. Alpha of .05 is divided by the order; for example, .05/1, .05/2, etc. If the p-value is smaller than the alpha the mean difference is statistically significant after Benjamini-Hochberg correction is applied.
DV= dependent variable
Research question 2: What is the association between HSI-A domains of cultural stress and depression scores?
Results from research question 1 indicated differences in depression scores and stress by group membership. In addition, gender is marginally related to depression scores. In order to examine the unique contribution of the stress domains on depression scores, we controlled for gender and group in this analysis.
Findings from the GLM model revealed that all 8 HSI-A domains of stress were significant and positively associated with depression scores, controlling for the effects of gender and group membership. Higher cultural stress scores were associated with higher depressive symptomology. In addition to the effects of each stress domain on depression scores, gender and group membership were significant predictors of depression in some models but not others. For example, the relation between gender and depressive scores was significant for 6 of the 8 domains of stress. Likewise, group membership predicted depression scores even with gender and cultural or educational, acculturation gap, immigration, discrimination, family immigration, family drug, and community gang stress domains were in the model. In sum, these results suggest that the stress domains were the stronger predictors of depression symptoms over and above the covariates.
Research question 3: Does group membership moderate the association between cultural stress and depressive symptoms?
To answer this question, we first centered each domain of stress at their mean values and then created a series of interaction effects with the new stress variable and group membership. In step 1 (the first two columns of Table 4), we ran 8 individual GLM models with gender, the stress domain, group membership and the interaction of each stress domain and group membership. In these analyses, significant interaction effects were found in three HSI-A domains: community or gang, cultural or educational and family immigration stress. Results suggest that the relation between these stress domains and depression is stronger for the clinical group. For the other five HSI-A domains (family economic, acculturation gap, family immigration, discrimination, and family drug stress), the relation between stress and depressive symptoms was positive for both adolescents in the clinical and non-clinical group, without a significant interaction by group (e.g., no group difference in the slopes).
Table 4.
Testing the moderating effect of group membership as an interaction between HSI-A stress domains and CDI2 depression scores.
| Step1: Individual models with gender and the group* stress interaction | Step 2: Full model with for gender and group* stress interaction | |||
|---|---|---|---|---|
|
| ||||
| B | Standard error | B | Standard error | |
|
|
||||
| Gender | --- | --- | .17 | .49 |
| Clinical/non-clinical interaction | --- | --- | .12 | .63 |
| Community and gang stress | .48*** | .09 | .02 | .09 |
| Community/gang stress* group membership | .30* | .14 | .36* | .17 |
| Family economic stress | .38*** | .05 | .13* | .06 |
| Family economic stress* group membership | .09 | .07 | .14 | .10 |
| Culture or educational stress | .48*** | .08 | −.08 | .09 |
| Cultural/educational stress * group membership | .23* | .12 | .06 | .18 |
| Acculturation gap stress | .48*** | 04 | .31*** | .05 |
| Acculturation gap stress* group membership | .03 | .09 | −.36** | .11 |
| Family immigration stress | .38*** | .08 | −.09 | .09 |
| Family immigration stress* group membership | .36* | .14 | .24 | .19 |
| Discrimination stress | 1.0*** | .11 | .53*** | .13 |
| Discrimination stress* group membership | .19 | .20 | .01 | .25 |
| Immigration related stress | .34*** | .08 | .18* | .08 |
| Immigration stress* group membership | .25 | .15 | −.12 | .16 |
| Family drug stress | .79*** | .11 | .23* | .11 |
| Family drug stress* group membership | .21 | .27 | −.01 | .29 |
p<.001,
p<.01,
P<.05
Research question 4: What are the unique contributions of each stress subscale to depression symptoms for youth in the sample?
Next, we ran a combined GLM model to test how each domain of stress uniquely predicts depression, above and beyond the other variables in the model (second set of columns in Table 4). When all of the domains of stress were included in the model, culture or education and family immigration stress were no longer significantly related to depression scores in either group. For culture or educational stress, in particular, both the direct effect of stress and the interaction of stress and group membership lost statistical significance in the full model. These findings suggest that the relations among these variables to depression scores did not add uniquely to the prediction of depression symptoms over and above the other measures of stress in the model.
In contrast, family economic, immigration, discrimination and family drug stress domains were positively related to depression scores, but the interaction between these stress domains and group were not significant. This suggests that these domains of stress were significant predictors of depressive symptoms in both the clinical and non-clinical sample of adolescents and the relation was not stronger in one group over the other. Two interaction effects were significant in the combined GLM model (step 2). The association between community gang stress and depressive scores was significant only for clinical sample (see Figure 1), whereas in the previous model it was significant in both groups—although the relation was stronger in the clinical group. Acculturation gap stress had a significant direct effect in the individual model, but the interaction effect was not significant (see Figure 2). This suggests that acculturation gap stress in not related to depression for the clinical group but is for the non-clinical group.
Figure 1.
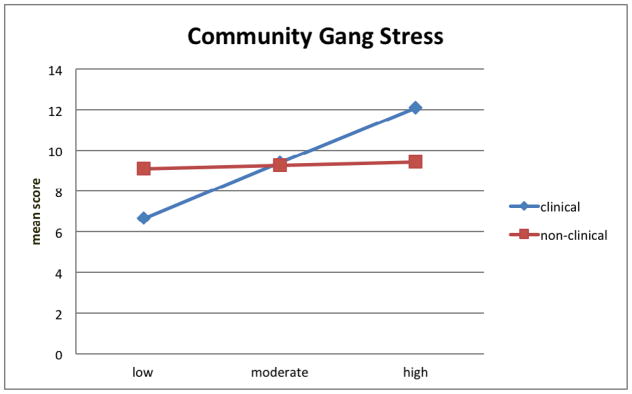
Interaction effects of predicted CDI2 by Community Gang Stress 251658240
Figure 2.
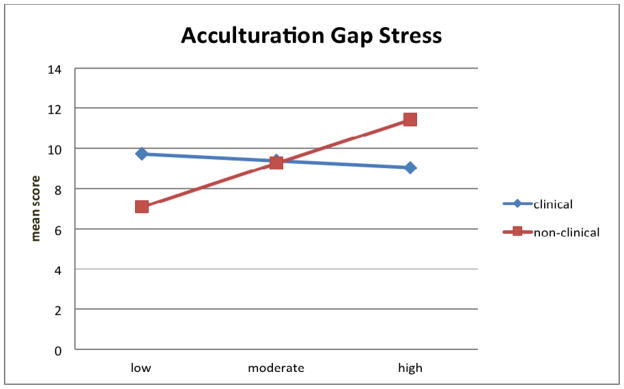
Interaction effects of predicted CDI2 by Acculturation Gap Stress 251658240
DISCUSSION
The aim of the current study was to understand the relation between cultural stress and depressive symptoms in a sample of clinical and non-clinical Hispanic adolescents. Depressive symptoms, including suicidal ideation and self-harm have been found to be more prevalent among Latina adolescents (Zayas, 2011; CDC, 2010). Further, researchers now point to disruptions in the family system, poor parent-child communication, and parent-child conflicts based on cultural stress as significant factors associated with depression in Hispanic adolescents (Santisteban & Mena, 2009). Albeit cross sectional in nature, this study represents one of the first quantitative assessments of cultural stress in conjunction with depressive symptomatology and addresses a significant gap in the literature by testing models of depression that account for cultural stress and group differences in Hispanic adolescents. Focusing on younger populations is important for diagnostic purposes (Boardman & Alexander, 2011; Eaton & Kessler, 1981) and provides opportunity for early intervention approaches that focus on stress and coping techniques.
Findings from this study suggest that youth in clinical treatment have significantly higher cultural stress scores on 7 of the 8 domains, as well as higher levels of depression symptomology compared to Hispanic youth in the general population. Although these findings seem somewhat intuitive, confirmation that higher cultural stressors in Hispanic adolescents in clinical treatment has implications for practice. Overlooking these cultural stress experiences, especially among youth in treatment, could contribute to less effective treatment outcomes, and at the extreme, higher dropout rates among these youth. Given that Hispanic families are generally more apprehensive to seek and remain in treatment (Bluthenthal et al., 2007), focusing on ways to keep them engaged in treatment is critical to addressing a large unmet need for mental health services in the community.
The effects of cultural stress scores on depression were robust, with higher stress associated with higher CDI2 depressive symptoms. Research by Boardman and Alexander (2011) found that high levels of stress were correlated to a higher prevalence of depression in African American youth and that these stressors were a potential source of health disparities between white and black adolescents. Yet, their study did not examine the stress experiences in Hispanic youth, and even in studies that include this population, no studies have used a validated measure of cultural stress that is relevant to the experiences of Hispanic families in the U.S. These findings contribute to a body literature that documents the stress-depression relation for minority adolescents and to the conversation about depression as a potential source of health disparities in this population.
A major focus of the study was examining how cultural stress domains relate to depression taking in to account the interaction of group membership. Recall that in the individual models, all of the domains of stress were positively related to depression for both groups, but this association was stronger in youth in the clinical group on community gang, cultural or education and family immigration stress domains. In the full model, family economic, discrimination, immigration, and family drug stress were uniquely related to depression above and beyond the other domains of stress and this relation was consistent for both the clinical and nonclinical group. This suggests that these four domains of stress are particularly important to our understanding of depression in Hispanic youth. For youth in clinical treatment, integrating culturally tailored intervention approaches that address the sociopolitical stressors (e.g., immigration related stress), as well as the family economic and social stressors (e.g., discrimination) may improve treatment outcomes and assist youth in dealing with these triggers post-treatment. For youth who are not yet receiving clinical treatment, intervening on these stressors may be a relevant area of prevention for future mental health problems. Clinicians should be acutely aware that cultural stressors may exacerbate mental health problems, and as such, assistance in helping clients develop healthy coping skills when faced with cultural stressors should be part of the treatment tailoring process as urged by Santisteban and colleagues (2011). At the same time, preventive interventions, such as Familia Adelante (Cervantes & Goldbach, 2012; Cervantes, Goldbach, & Santos, 2011) that incorporate cultural stress management skills may prevent clinical syndromes from developing. Specific learning modules that focus on domain specific stressors and that guide youth and parents toward effective stress-coping strategies are part of the Familia Adelante Program, as an example. Focusing on the acculturation gaps that exist within families is an important aspect of the tailoring process that occurs as part of the Culturally Informed Family Focused Treatment (CIFFTA) (Santisteban, et al 2011).
Our final research question uncovered two significant interaction effects between stress and group membership. Acculturation gap stress was significantly related to depression for the non-clinical but not the clinical group, whereas community gang stress was associated to depression in both groups, but the relation was stronger for youth in the clinical group. Factors such as the combination of community gang stress and depression may influence clinical levels of psychopathology, while acculturation gaps and depression combined appear to predict pre-clinical distress. Understanding which domains of stress uniquely predict depression in each group can assist with the adaptation of prevention intervention strategies to meet the unique needs of each population.
Study limitations and directions for future research
Despite several strengths in the current study, there are also several limitations that are worth noting. The data presented in the current study are not causal, and youth in the clinical sample who present with clinical problems, such as depressive symptoms, may have greater difficulty in coping with HSI-A cultural stressors and therefore rate these stressor events as more disturbing or disruptive (stressful). Longitudinal research on cultural stress and mental health is a critical next step so that we are able to identify which predisposing factors contribute to both stress and depression in U.S. Hispanic youth. More precise data on how cultural stress plays a role in the etiology of mental illness, including the expression of genes that may make youth more vulnerable, may better inform the development of culturally tailored prevention and treatment programs for this population.
In the parent study, purposive sampling was used to identify youth in the clinical sample and therefore this sample may not represent all youth in clinical treatment. We selected the clinical group from both school based counseling centers, as well as community mental health and substance abuse treatment facilities. However, because of sample size, we were unable to examine within-group differences by treatment setting or establish differences based on the presenting problem for treatment. Further, by aggregating the clinic samples to include youth with primary substance use disorders and youth who have emotional or stress based disorders, it is possible that the diverse treatment backgrounds of the adolescents skewed the scores for depression found in the clinical sample. A closer examination of how substance use disorders and emotional stress based disorders differ on the domains of cultural stress is needed to better understand the findings that are presented in the study. Future research could address these concerns by selecting more heterogeneous clinical population or ensuring an adequate sample size to facilitate multiple group analyses.
Finally, we recognize that the issue of immigration and its’ impact on development, stress exposure and mental health varies widely depending on a number of critical factors. Reasons for migration, the family migration experience, family legal status in the United States, and extent of fear of deportation faced by family members are all significant issues that can impact adolescent mental health. While both our clinic and non-clinic samples had sizeable proportions of immigrant adolescents (about 15%), our assessment tools and subsequent analysis did not measure or control for variables related to reasons for migration and this constitutes a limitation to our reported findings. While we attempted to control for some of these factors with demographic variables like child ethnicity and nativity status, we recognize that higher depression scores in the clinical group may influenced not only by the domains of cultural stress that we included in the model, but also by these unmeasured sociopolitical variables that were not accounted for in our statistical analyses. If this is the case, these unmeasured sociopolitical factors (e.g., pre-migration factors, documentation status, and experiences of macro/micro aggressions) may have skewed (likely inflated) the depression scores in both groups. In conclusion, research studies that isolate reasons for migration, the context of the settlement in the United States, and the impact of those varying reasons on youth mental health are sorely needed. Incorporating validated measures of cultural stress, as well as sociopolitical measures that capture the context of life for Hispanic adolescents, in longitudinal studies of mental health in Hispanic populations is the next step to understanding the nonclinical and clinical levels of mental health problems found in this population.
Table 3.
Generalized Linear Models examining individual stress domains regressed on depression, controlling for group membership and gender.
| B (SE) | P-value | |
|---|---|---|
| Gender | 1.1 (.51) | .02 |
| Group membership | 1.3 (.66) | .05 |
| Community and gang stress | .58 (.07) | < .0001 |
| Gender | .91 (.50) | .06 |
| Group membership | .58 (.65) | .40 |
| Family economic stress | .42 (.04) | < .0001 |
| Gender | 1.4 (.50) | .007 |
| Group membership | 1.4 (.65) | .03 |
| Cultural and education stress | .57 (.06) | < .0001 |
| Gender | −.00 (.50) | .98 |
| Group membership | 1.3 (.62) | .04 |
| Acculturation gap stress | .48 (.03) | < .0001 |
| Gender | 1.0 (.51) | .04 |
| Group membership | 1.6 (.67) | .02 |
| Family immigration stress | .50 (.06) | < .0001 |
| Gender | 1.1 (.50) | .03 |
| Group membership | 1.6 (.64) | .01 |
| Discrimination stress | 1.1 (.10) | < .0001 |
| Gender | 1.3 (.52) | .01 |
| Group membership | 2.0 (.68) | .002 |
| Immigration related stress | .42 (.07) | < .0001 |
| Gender | 1.0 (.52) | .04 |
| Group membership | 1.6 (.67) | .02 |
| Family drug stress | .51 (.07) | <.001 |
Acknowledgments
This research was supported by the National Institute of Mental Health, Grant No. 2R44MH073180-02 to Dr. Richard C. Cervantes. The authors would like to thank Paul Swank, at the School of Public Health, the University of Texas Health and Sciences Center for his assistance with the statistical analyses.
Contributor Information
Dr. Richard C. Cervantes, Behavioral Assessment, Incorporated
Dr. Jodi Berger Cardoso, University of Houston Graduate, Graduate College of Social Work
Dr. Jeremy T. Goldbach, University of Southern California, School of Social Work
References
- Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful approach to Multiple Testing. Journal of the Royal Statistical Society, Series B (Methodological) 1995;57(1):289–300. [Google Scholar]
- Bluthenthal RN, Anderson R, Flynn NM, Kral AH. Higher syringe Coverage is associated with lower odds of HIV risk and does not increase unsafe Disposal among syringe exchange program clients. Drug Alcohol Depend. 2007;89:214–222. doi: 10.1016/j.drugalcdep.2006.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boardman JD. Health pessimism among black and white adults: The role of interpersonal and institutional maltreatment. Social Science and Medicine. 2004;59:2523–2533. doi: 10.1016/j.socscimed.2004.04.014. [DOI] [PubMed] [Google Scholar]
- Boardman JD, Alexander KB. Stress trajectories, health behaviors, and the mental health of black and white young adults. Social Science and Medicine. 2011;72:1659–1666. doi: 10.1016/j.socscimed.2011.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Concurrent Substance Use and Mental Health Problems in Youth [CAMH] Screening for concurrent substance use and mental health problems in youth. Centre for Addition and Mental Health; 2009. Retrieved February 7, 2014 http://knowledgex.camh.net/amhspecialists/Screening_Assessment/screening/screen_CD_youth/Pages/YSR.aspx. [Google Scholar]
- [CDC] Centers for Disease Control and Prevention. Youth Suicide. 2012 Retrieved February 1, 2013, from http://www.cdc.gov/ViolencePrevention/suicide/youth_suicide.html.
- [CDC] Centers for Disease Control and Prevention National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) 2010 Retrieved September 21, 2013, from www.cdc.gov/injury/wisqars/index.html.
- Cervantes RC, Bui T. Culturally Informed Stress Assessments for Hispanics. In: Guisinger K, editor. Psychological Testing of Hispanics: Clinical and Intellectual Issues. American Psychological Association Press; in press. [Google Scholar]
- Cervantes RC, Córdova D. Life Experiences of Hispanic Adolescents: Developmental and Clinical Considerations in Acculturation Stress. Journal of Community Psychology. 2011;39(3):336–352. [Google Scholar]
- Cervantes RC, Fisher DG, Córdova D, Napper LE. The Hispanic Stress Inventory-Adolescent Version: A culturally informed psychosocial assessment. Psychological Assessment. 2011 doi: 10.1037/a0025280. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervantes RC, Garcia I. Alcohol Abuse Prevention in the Hispanic Community. In: Langton P, editor. The challenge of participatory research: Prevention of alcohol-related problems in ethnic communities. National Institute on Alcohol Abuse and Alcoholism/Center for Substance Abuse Prevention, SAMHSA; Washington, D.C: 1995. [Google Scholar]
- Cervantes RC, Goldbach J. Adapting Evidence-Based Prevention Approaches for Latino Adolescents: The Familia Adelante Program – Revised. Journal of Psychosocial Intervention. 2012;21(3):281–290. [Google Scholar]
- Cervantes RC, Goldbach J, Padilla A. Using Qualitative Methods for Revising the Hispanic Stress Inventory. Hispanic Journal of Behavioral Sciences. 2012;34(2):208–231. [Google Scholar]
- Cervantes RC, Goldbach J, Santos S. Familia Adelante: A Multi-Risk Prevention Intervention for Latino Youth. Journal of Primary Prevention. 2011;32(3–4):225–234. doi: 10.1007/s10935-011-0251-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervantes RC, Padilla AM, Napper LE, Goldbach J. Acculturation Related-Stress and Mental Health Outcomes among Three Generations of Hispanic Adolescents. American Journal of Community Psychology 2013 [Google Scholar]
- Cervantes RC, Padilla AM, Salgado de Snyder NS. The Hispanic Stress Inventory: A culturally relevant approach to psychosocial assessment. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3(3):438–447. [Google Scholar]
- Cervantes RC, Shelby TM. Mental health issues for immigrant Adolescents: Research and practice. In: Grigorenko EL, editor. Handbook of US Immigration and Education. New York: Springer Publishing Company; 2013. pp. 163–178. [Google Scholar]
- Córdova D, Cervantes RC. Intergroup and within group perceived discrimination among U.S. born and Foreign born Latino youth. Hispanic Journal of Behavioral Sciences. 2010;32(2):259–274. [Google Scholar]
- Cowell JM, Gross D, McNaughton D, Ailey S, Fogg L. Depression and suicidal ideation among Mexican American school-aged children. Research and Theory for Nursing Practice. 2005;19(1):77–94. doi: 10.1891/rtnp.19.1.77.66337. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Kessler LG. Rates of symptoms of depression in a national sample. American Journal of Epidemiology. 1981;114:528–538. doi: 10.1093/oxfordjournals.aje.a113218. [DOI] [PubMed] [Google Scholar]
- Fortuna L, Perez D, Canino G, Sribney W, Alegría M. Prevalence and Correlates of Lifetime Suicidal Ideation and Attempts among Latino Subgroups in the United States. Journal of Clinical Psychiatry. 2007;68(4):572–581. doi: 10.4088/jcp.v68n0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia C. Coping with the Conceptualization and Measurement of Coping during Adolescence: A Review of the Literature. Journal of Nursing Scholarship. 2010;42(2):166–185. doi: 10.1111/j.1547-5069.2009.01327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia C, Magnuson K. The Psychological Experience of Immigration: A Developmental Perspective. In: Suarez-Orozco M, Qin DB, editors. The New Immigration: An Interdisciplinary Reader. New York: Routledge; 2005. [Google Scholar]
- Gil AG, Wagner EF, Tubman JG. Young adult consequences of early adolescent substance use: Substance use and psychiatric disorders in a multiethnic sample of males. American Journal of Public Health. 2004;94(9):1603–1609. doi: 10.2105/ajph.94.9.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guinn B, Vincent V. Determinants of coping responses among Mexican American adolescents. Journal of School Health. 2002;72(4):152–156. doi: 10.1111/j.1746-1561.2002.tb06536.x. [DOI] [PubMed] [Google Scholar]
- Horton NJ, Kleinman KP. Much Ado About Nothing: A comparison of missing data methods and software to fit incomplete data regression models. American Statistical Association. 2007;67(1):79–90. doi: 10.1198/000313007X172556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huberty CJ, Morris JD. Multivariate analyses versus multiple univariate analyses. Psychological Bulletin. 1989;105:302–308. [Google Scholar]
- Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychol Med. 1997;27(4):861–873. doi: 10.1017/s0033291797004807. [DOI] [PubMed] [Google Scholar]
- Kovacs M Multi-Health Systems Staff. CDI-2: Children’s Depression Inventory. 2. Toronto (ON): Multi-Health Systems Inc; 2011. Technical Manual. [Google Scholar]
- Lorenzo-Blanco EI, Unger JB, Baezconde-Garbanati L, Ritt-Olson A, Soto D. Acculturation, enculturation, and symptoms of depression in Hispanic youth: The roles of gender, Hispanic cultural values, and family functioning. Journal of Youth Adolescence. 2012;41:1350–1365. doi: 10.1007/s10964-012-9774-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire S, Martin K. Fractured Migrant Families: Paradoxes of Hope and Devastation. Family and Community Health. 2007;30:178–188. doi: 10.1097/01.FCH.0000277761.31913.f3. [DOI] [PubMed] [Google Scholar]
- Mena FJ, Padilla AM, Maldonado M. Acculturative stress and specific coping strategies among immigrant and later generation college students. Hispanic Journal of Behavioral Science. 1987;9:207–225. [Google Scholar]
- Ng’andu J, Ryan KD. Fast Facts: Immigrants and Health Care. Facts and Figures about immigrants’ access to the U.S. health care system. National Council of La Raza (NCLR) 2011 Retrieved January 15, 2013, from http://www.nclr.org/images/uploads/publications/FastFacts_ImmigrantsandHealthCare2012.pdf.
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, Correlates, and Treatment of Lifetime Suicidal Behavior Among Adolescents: Results From the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression in adolescence. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Reynolds GL, Cervantes RC, Fisher DG, Fagen D. Measuring gender differences in stress in Latina/o adolescents. Abstract presented at the annual meeting of the American Public Health Association; San Francisco, CA. 2012. [Google Scholar]
- Rew L. Adolescent Health: A multidisciplinary approach to theory, research, and intervention. Thousand Oaks, CA: Sage; 2005. [Google Scholar]
- Rice FP, Dolgin KG. The Adolescent: Development, Relationships, and Culture. Boston: Allyn and Bacon; 2002. [Google Scholar]
- Robbins MS, Feaster DJ, Horigian V, Rohrbaugh M, Shoham V, Bachrach K, Miller M, Burlew K, Hodgkins C, Carrion I, Vandermark N, Schindler E, Werstlein &, Scapocznik J. Brief Strategic Family Therapy versus treatment as usual: Results of a multisite randomized trial for substance using adolescents. Journal of Consulting and Clinical Psychology. 2011;79(6):713–727. doi: 10.1037/a0025477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robson M, Cook P. Helping children manage stress. British Educational Research Journal. 1995;21(2):265–175. [Google Scholar]
- Rodriguez ET, Tamis-LeMonda CS, Spellmann ME, Pan BA, Raikes H, Lugo-Gil J, Luze G. The formative role of home literacy experiences across the first three years of life in children from low-income families. Journal of Applied Developmental Psychology. 2009;30:677–694. [Google Scholar]
- Rodriguez RA, Henderson CE, Rowe CL, Burnett KF, Dakof GA, Liddle HA. Acculturation and drug use among dually diagnosed Hispanic adolescents 21st. Century Research on Drugs and Ethnicity. 2007;6(2):97–113. doi: 10.1300/J233v06n02_07. [DOI] [PubMed] [Google Scholar]
- Rogler LH. International Migrations: A framework for directing research. American Psychologist. 1994;49(8):701–708. doi: 10.1037//0003-066x.49.8.701. [DOI] [PubMed] [Google Scholar]
- Santisteban D, Mena MP. Culturally informed and flexible family-based treatment for adolescents: A tailored and integrative treatment for Hispanic youth. Family Process. 2009;48:253–268. doi: 10.1111/j.1545-5300.2009.01280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santisteban DA, Mena MP, McCabe BE. Preliminary results for an adaptive family treatment for drug abuse in Hispanic youth. Journal of Family Psychology. 2011;25(4):610–614. doi: 10.1037/a0024016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz A, Israel B, Williams D, Perker E, James S. Social inequalities, stressors, and self-reported health status among African American and white women in the Detroit metropolitan area. Social Science and Medicine. 2000;51:1639–1653. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. A supplement to mental health: A report of the surgeon general. Rockville: Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2001. Mental health: Culture, race, and ethnicity; pp. 1–204. [PubMed] [Google Scholar]
- Vega WA, Gil AG, Warheit W, Zimmerman RS, Apospori E. Acculturation and delinquent behavior among Cuban American adolescents: Toward an empirical model. American Journal of Community Psychology. 1993;21:113–125. doi: 10.1007/BF00938210. [DOI] [PubMed] [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry. 1998;55(9):771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- Walsemann KM, Gee GC, Geronimus AT. Ethnic Differences in Trajectories of Depressive Symptoms: Disadvantage in Family Background, High School Experiences, and Adult Characteristics. Journal of Health and Social Behavior. 2009;50(1):82–98. doi: 10.1177/002214650905000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White RMB, Roosa MW, Weaver SR, Nair RL. Cultural and contextual influences on parenting in Mexican American families. Journal of Marriage and Family. 2009;71:61–79. doi: 10.1111/j.1741-3737.2008.00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worchel FF, Hughes JN, Hall BM, Stanton SB, Stanton H, Little VZ. Evaluation of subclinical depression in children using self-, peer-, and teacher-report measures. Journal of Abnormal Child Psychology. 1990;18(3):271–282. doi: 10.1007/BF00916565. [DOI] [PubMed] [Google Scholar]
- Zayas LH. Seeking models and methods for cultural adaptation of interventions: Commentary on the special section. Cognitive and Behavioral Practice. 2010;17:198–202. doi: 10.1016/j.cbpra.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas LH, Torres LR, Kyriakakis S. Culturally competent assessment of Latino clients. In: Furman R, Negi N, editors. Social Work Practice with Latinos: Key Issues and Emerging Themes. Chicago, IL: Lyceum Books; 2010. pp. 161–183. [Google Scholar]
- Zayas LH. Latinas attempting suicide: When cultures, families, and daughters collide. New York: Oxford University Press; 2011. [Google Scholar]
- Zayas LH, Lester RJ, Cabassa LJ, Fortuna LR. Why do so many Latina teens attempt suicide? A conceptual model for research. American Journal of Orthopsychiatry. 2005;75(2):275–287. doi: 10.1037/0002-9432.75.2.275. [DOI] [PubMed] [Google Scholar]


