Abstract
Diabetic cardiomyopathy entails a serious cardiac dysfunction induced by alterations in structure and contractility of the myocardium. This pathology is initiated by changes in energy substrates and occurs in the absence of atherothrombosis, hypertension, or other cardiomyopathies. Inflammation, hypertrophy, fibrosis, steatosis, and apoptosis in the myocardium have been studied in numerous diabetic experimental models in animals, mostly rodents. Type I and type II diabetes were induced by genetic manipulation, pancreatic toxins, and fat and sweet diets, and animals recapitulate the main features of human diabetes and related cardiomyopathy. In this review we update and discuss the main experimental models of diabetic cardiomyopathy, analysing the associated metabolic, structural, and functional abnormalities, and including current tools for detection of these responses. Also, novel experimental models based on genetic modifications of specific related genes have been discussed. The study of specific pathways or factors responsible for cardiac failures may be useful to design new pharmacological strategies for diabetic patients.
1. Main Models of Diabetic Cardiomyopathy (DCM)
Experimental models of both type I and type II diabetes (T1DM and T2DM) consistently exhibit alterations in the circulating levels of glucose and in the lipid profile (Table 1). Main T1DM and T2DM animals show both hyperglycemia (early after pancreas-toxin or fat/sweet-diet administration, resp., and later after genetic mutations) and hyperlipidemia, represented by elevated levels of TAG, cholesterol, and lipoproteins. More interestingly, these models also exhibit functional, structural, and metabolic abnormalities that recapitulate the human DCM pathology.
Table 1.
Main experimental models of T1DM and T2DM and related plasma and cardiac characteristics.
| Type I diabetes | Type II diabetes | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Toxics | Genetics | Genetics | DIO | |||||||||||
| STZ | Alloxan | OVE26 | Akita | NOD | BB rat | ob/ob | db/db | ZDF | KK Ay | OLETF | GK | Fat | Sweet | |
| (Antibiotic toxicity) | (Uric acid derivative toxicity) | (Calmodulin overexpression) | (Ins2+/−) | (Nonobese diabetic mouse) | (Nonobese diabetic rat) |
(Lep −/−) | (Lepr −/−) | (Lepr −/−) | (Polygenic obese + A y) | (Polygenic obese) | (Polygenic nonobese) |
(Diet-induced obesity and diabetes) |
||
| Serum profile | ||||||||||||||
| Hyperglycemia onset (d: days; w: weeks) |
2 d after injection [123] |
5 d after injection [123] | 2-3 w [79] | 5-6 w [71] | 30 w [51] | 12 w [124] | 8–15 w [125] | 4–8 w [125] | 14 w [126] | 16 w [127] | 18 w [128] | 3 w [129] | 1 w [130] | 1 w [14] |
| Hyperlipidemia | TG, Ch [123] LDL, HDL [131] |
TG, Ch [123] | TG [79] | TG [71] | TG [132] Ch, HDL [133] |
FFA [124] | TG, FFA [64] LDL, HDL [134] |
TG, LDL, HDL [135] | TG, VLDL, LDL, HDL [136] | TG [137] | TG, Ch [11] | TG, FFA, LDL, HDL [12] | TG, FFA, Ch [138, 139] | TG, Ch [14] |
|
| ||||||||||||||
| Cardiac abnormalities | ||||||||||||||
| Functional | ||||||||||||||
| Diastolic function | ↓[140] | ↓[141] | ↓[90] | ↓[24] | ↓[142] | ↓[143] | ↓[5] | ↓[144] | ↓[8–10] | ↓[11] | ↓[12] | ↓[13, 144] | ↓[14] | |
| Systolic function | ↓[140] | ↓[141] | ↓[90] | ↓[145]/ ~[24, 71] |
↓[146] | ↓[147] | ~[5] | ↓[142]/ ~[148] |
↓[8]/ ~[9, 10] |
~[11] | ~[12] | ↓[13, 144] | ↓[14] | |
| Structural | ||||||||||||||
| Hypertrophy | ↑[20] | ↑[22, 23] | ~[24] | ↑[46, 149] | ↑[64] | ↑[26]/ ~[27] |
↑[10, 28] | ↑[12, 30] | ↑[13] | ↑[32] | ||||
| Inflammation | ~[21] | ↑[22] | ↑[40] | ↑[150] | ↑[41] | ↑[42] | ↑[44] | ~[32] | ||||||
| Fibrosis | ↑[21] | ↑[22, 23] | ~[24] | ~[25] | ↑[41]/ ~[25] |
↑[10, 29] | ↑[151] | ↑[11, 47] | ↑[12] | ↑[43] | ~[32] | |||
| Steatosis | ↑[21] | ↑[24] | ↑[51] | ↑[5] | ↑[5] | ↑[8, 10] | ↑[144] | ↑[53] | ||||||
| Apoptosis | ↑[21] | ↑[58] | ↑[52] | ↑[59] | ↑[10, 60] | ↑[12] | ↑[13, 65] | ~[32] | ||||||
|
| ||||||||||||||
| Metabolic alterations | ||||||||||||||
| Glucose oxidation | ↓[70] | ↓[24, 71] | ↓[5, 64] | ↓[26] | ↓[10, 72] | ↓[31, 80] | ↓[74] | |||||||
| FA oxidation | ↑[70] | ↑[62] | ↑[24, 71] | ↑[5, 64] | ↑[63] | ↑[10, 86] | ↑[31] | ~[74]/↑[73] | ↑[53] | |||||
| Mitoch. function | ↓[70] | ↓[62] | ↓[71] | ↓[81] | ↓[152] | ↓[10] | ↓[151] | ↓[83] | ↓[84] | ↓[73] | ||||
| Oxidative stress | ↑[70, 76] | ↑[153] | ↑[78, 79] | ~[71] | ↑[92] | ↑[152] | ↑[10, 86] | ↑[47, 83] | ↑[84, 85] | ↑[34] | ↑[53] | |||
| Ca2+ mobilization | ↓[70] | ↓[90] | ↓[24] | ↓[91] | ↓[25] | ↓[93] | ~[72] | ↓[94] | ↓[13, 95] | ↓[14] | ||||
T1DM was induced by toxins [streptozotocin (STZ) or alloxan] or genetic mutations (OVE26, calmodulin transgenic; Akita, insulin-2 deficient; NOD, nonobese diabetic or BB, BioBreeding diabetes-prone mice). T2DM models were produced by genetic alterations [ob/ob, leptin deficient mice; db/db, leptin receptor deficient mice; ZDF, Zucker Diabetic Fatty rats; KK Ay, yellow obese gene transgenic KK mice; OLEFT, Otsuka Long-Evans Tokushima fatty rats; GK, Goto-Kakizaki rats or DIO, diet-induced (fat, sweet) obesity].
Dysfunction in Cardiac Mechanics. In patients, early stages of DCM are marked by a deterioration of longitudinal systolic function, a compensative elevated radial function, and diastolic dysfunction [1]. DCM progression is characterized by reduced ejection fraction (EF) and ventricular dilatation and, later, mimicking dilative cardiomyopathy. Experimental T1DM and T2DM animals are prone to develop diastolic and/or systolic dysfunction, as demonstrated in numerous in vivo studies using echocardiography, magnetic resonance imaging (MRI), and hemodynamic measurements [2, 3]. Diastolic dysfunction usually precedes the alteration of cardiac contractility. As recently updated [4], a broad analysis of diastolic performance should include several Doppler indexes: ratio of peak velocity of early to late filling of mitral inflow (E/A) and deceleration time of early filling of mitral inflow, as well as the isovolumetric relaxation/contraction time. Given the subjectivity of visual echocardiographic estimations and the frequent coexistence of different Doppler severity patterns, measurement of left ventricular (LV) diastolic pressures by catheterization is also highly valuable. The main systolic parameters include LV septum thicknesses, LV internal dimensions, posterior wall (PW) thicknesses at diastole and systole, LV mass, LVEF, LV fractional shortening (FS), and ventricular contractility assessment (dP/dt). Regardless of rather inconstant particularities mainly displayed by Akita mice, all T1DM models have been reported to meet most of these criteria (Table 1). Cardiac performance has also been extensively studied in T2DM experimental models. Genetically obese mice displayed severe diastolic dysfunction, as evidenced by diminished E/A velocities in ob/ob and db/db mice [5, 6]. Contractile properties are yet marginally affected in ob/ob mice [5]. On the contrary, db/db mice exhibited a reduced FS and velocity of circumferential fibre shortening at age 12 weeks [6]. Van den Bergh et al. also reported in db/db a decreased preload recruitable stroke work, end-systolic elastance, and dP/dt from age 24 weeks onwards but found preserved cardiac output, EF, and dP/dt [7] (Table 1). Other T2DM models presented heterogeneous data regarding cardiac performance. In ZDF rats, impaired diastolic function has been extensively described [8–10]. However, Zhou's work initially reported a decrease of FS at age 20 weeks [8], and we and others found no evidence of systolic dysfunction by both echocardiographic and MRI determinations at ages 16 and 44 weeks, respectively [9, 10]. Similarly, OLETF and GK rats preserved contractile function while displaying abnormalities of ventricular relaxation, as suggested by a prolonged deceleration time, decreased peak velocity, and reduced LV diameters associated with increased LVPW thickness and LV mass [11, 12]. In contrast, diet-induced obesity appears to invariably associate both diastolic and systolic dysfunctions. High-fat diet increased LV mass and reduced dP/dt and FS after 6 weeks [13]. Alike, sucrose fed rats exhibited early abnormalities in LV fillings, as demonstrated by reduced E/A ratios, together with depressed FS and EF after 10 weeks [14]. Consistently, echocardiographic findings in other high-fat and high-sucrose fed mice revealed decreased FS, EF, and velocity of circumferential fibre shortening, as well as dramatically impaired parameters of diastolic function after 16 weeks [15].
Thus, cardiac dysfunction in T1DM patients could be roughly reproduced in all conventional models (induced by toxins and genetic alterations). In T2DM, diet-induced models may represent the human pathology more appropriately, at least in the advanced states of the disease.
(1) Alterations of Cardiac Structure. Maladaptive structural modifications underlie both the diastolic and systolic impairments that eventually lead to heart failure. Although the progression of these events has not been fully established, the hallmark of changes includes cell hypertrophy, local inflammation, and interstitial fibrosis promoted by steatosis and cell-death processes in the injured myocardium.
(a) Hypertrophy. Undiagnosed cardiac hypertrophy is prevalent in asymptomatic T2DM patients, reaching up to 56% in recent reports [16]. Myocyte hypertrophy is common in biopsy of diabetic hearts and is induced by long-standing metabolic imbalances and microcirculation anomalies. However, the contribution of cardiomyocyte hypertrophy to the development of ventricular hypertrophy is still unclear [17]. Most models of DCM display progressive concentric or eccentric hypertrophy, which is directly associated with diastolic and systolic derangement, respectively. Indicative parameters include LV mass and heart-to-body weight (or femur length) ratio, LVPW and septum thicknesses, LV internal diameters, and cardiomyocyte size. In addition, complementary plasma levels of brain natriuretic peptide (BNP), atrial natriuretic peptide (ANP), and β-myosin heavy chain (β-MHC) have traditionally been considered supportive [18]. However, a recent systematic analysis of hypertrophic biomarkers in diabetic rodents revealed that most commonly measured genes are confounded by diabetogenic methods and do not correlate with cardiac hypertrophy [19]. In STZ-induced models, reduced wall thicknesses and increased LV internal diameters are prominent features, accounting for extensive ventricular dilatational remodeling [20] (Table 1). We observed cardiomyocyte size enlargement in long-term T1DM (22 weeks), reproduced to a lesser extent in short-term counterparts (6 weeks) [21]. Similar histological findings have been reported in OVE26 mice together with the upregulation of ANP and β-MHC [22, 23]. Conversely, no evidence of myocardial hypertrophy has been found in Akita mice [24]. In T2DM mice models, though systolic dysfunction is developed as a late event, myocardial mass may increase earlier. A higher heart weight has been reported in ob/ob and db/db mice at ages 12 and 9 weeks, respectively [25, 26]. A comprehensive MRI analysis of db/db hearts by Yue et al. revealed a significant increase in LV mass and LVPW, and septum thicknesses, as soon as age 13 weeks [26]. However, early architectural changes are subtle and not consistently identified. In this line, echocardiographic and cell dimension assessments did not find hypertrophy in 15-week-old db/db mice, despite evidence of systolic compromise [27]. In contrast, ZDF and GK rats usually exhibited a significant increase of the septum and LVPW thicknesses, reduced LV diastolic and systolic diameters, enlarged cardiomyocyte volume, and higher expression rates of ANP, in spite of the fact that contractile function was frequently preserved [10, 12, 28–31]. Finally, the limited body of evidence on diet-induced T2DM rather pointed hypertrophy as the only morphological alteration constantly present, independently of its high-fat of high-sugar diet origin [13, 32–34]. However, a recent work reported no difference in heart weight and cardiomyocyte size but overexpression of ANP, BNP, and β-MHC after a 16-week-long high-fat diet [35].
(b) Inflammation. Chronic low-grade inflammation has been recently added to the features of DCM in human patients [36]. Inflammatory signaling in cardiomyocytes usually occurs as an early response to myocardial injury and entails an activation of the proinflammatory nuclear transcription factor-κB (NF-κB) and the related expression of cytokines (i.e., tumour necrosis factor-α (TNFα), interleukins (IL-1β, IL-6), and chemokines (i.e., MCP-1)), and adhesion molecules (i.e., intracellular and vascular cell adhesion molecule-1 (ICAM-1, VCAM-1, resp.)) [37, 38]. Toll-like receptors and inflammasome signalling platforms may also be key participants in DCM-associated inflammation [39]. In STZ-treated hearts, both macrophage and lymphocyte infiltration and increased expression of proinflammatory cytokines and adhesion molecules were detected at 22 weeks, but not 6 weeks, after injection [21] (Table 1). Likewise, Li's paper reported an augmented NF-κB activity in OVE26 mice [22]. A comprehensive approach to myocardial inflammation in Akita mice was recently available, indicating the upregulation of TNFα and the attenuation of anti-inflammatory IL-10 [40]. However, data from T2DM models is more variable. Ob/ob and db/db mice displayed inflammation and increased myocardial proinflammatory factors [41], whereas we are not aware of any work addressing inflammation in the heart of GK and OLETF rats or KK Ay mice. ZDF myocardia showed either absence of inflammatory cell infiltrates at ages 9 and 13 months or higher levels of proinflammatory cytokines at age 22 weeks [42]. Inflammation is also present in diet-induced models of obesity and diabetes. Several studies on high-fat fed mice showed upregulation of proinflammatory factors, together with lower measurements of anti-inflammatory adiponectin and IFNγ [35, 43, 44]. In turn, high-sucrose fed mice did not present inflammation [32].
(c) Fibrosis. Interstitial fibrosis is the histologic hallmark of human DCM as a result of both replacement of focal myocyte death and response to inflammatory infiltrate. Accelerated extracellular matrix (ECM) deposition leads to ventricular stiffness in the diabetic heart, which also stimulates a local increase of cytokines and NF-κB [45]. Collagen type I and type III fibres accumulate in the epicardial and perivascular domains, whereas type IV is mostly found in the endocardium. Collagen can further undergo glycation by advanced glycation end-products (AGEs) and impair its degradation, leading to fibrosis, myocardial stiffness, and decreased cardiac relaxation. Quantification of interstitial fibrosis may be evaluated by histological staining (Masson's trichrome, Azan, and Sirius red) and gene/protein expression of ECM components. Valuable insight into the molecular substrate of ECM deposition is provided by the analysis of TGFβ-Smad-AP1 axis, poly(ADP-ribose) polymerase-1 (PARP-1), and matrix metalloproteinases (MMP) activity (MMP/TIMP (tissue inhibitor metalloproteinase) ratio). We reported that the myocardium of both short-term and long-term STZ-treated rats undergoes intense fibrotic remodeling, mainly at the expense of interstitial and perivascular ECM deposits and TGFβ axis [21] (Table 1). OVE26 mice and BB rats also displayed myocardial fibrosis, as determined by increases in collagen accumulation and reduced MMP activity [22, 46]. As with hypertrophy, histological study of Akita mice showed no evidence of fibrosis and elevated levels of ECM proteins [24]. In T2DM, most models exhibited extensive myocardial collagen deposits. In ZDF rats, we and others described an enlarged interstitial space mostly confined to the subendocardial domain [10, 29]. Similarly, we recently reported increased ECM deposition and upregulated expression profibrotic factors in the GK myocardium [12]. Other models in which fibrosis has been clearly detected include db/db and ob/ob mice and OLETF rats [18, 26, 47]. On the contrary, several groups pointed the absence of increased collagen deposition and ventricular stiffness in ob/ob despite strong evidence of other DCM traits such as hypertrophy and apoptosis [5, 25]. Much less has been done so far to assess fibrosis in diet-induced obesity models, in which a complete histological examination is lacked. High-fat fed mice presented overexpression of TGFβ axis and downregulation of antifibrotic p-Smad1/5 and bone morphogenetic protein-2 (BMP-2) [34, 43]. However, Nunes et al. found no differences in perivascular and interstitial fibrosis in high-sucrose fed mice compared to controls [32].
(d) Steatosis. Accumulation of fat in nonadipose tissues in human diabetes may be a protective response to provide a store of fuel for subsequent oxidation and to prevent exposure to toxic lipid metabolites such as ceramides [48]. However, a chronic imbalance of lipid storage versus lipid oxidation may lead to mechanical dysfunction. Insulin resistance and high levels of intramyocardial triacylglycerol (TAG), long-chain fatty acid (FA), TAG derivatives (i.e., diacylglycerols (DAG) and phospholipids), and ceramides are main triggers of heart disease in obesity and T2DM [49]. Also, ceramide and DAG can reduce insulin-stimulated signalling through the activation of PKC and NF-κB. Surprisingly, myocardial steatosis is a common feature among T1DM models (Table 1). STZ-treated mice showed a 50% increase in cardiac content of FA [50], and both FA and ceramide deposits have been reported in NOD and Akita mice already at age 3 months [24, 51]. An association between increased myocardial lipid content and cardiac dysfunction has also been observed in rodent models of obesity and T2DM. Interestingly, Zhou's lab described that cardiac steatosis was evident in ZDF at 6 weeks even before the reduction of FS [8]. Also, ob/ob and db/db showed significantly elevated contents of phospholipids, whereas ceramides, cardiolipin, and unesterified cholesterol remained unaltered [5, 41, 52]. As expected, both high-fat and high-fructose-induced obesity models also displayed extensive myocardial steatosis [15, 53].
(e) Apoptosis. Myocardial cell death is recognized as a major event in the progression of DCM. Biopsies from diabetic patients revealed that cardiomyocytes are more susceptible to diabetes-induced apoptosis than endothelial cells or fibroblasts [54]. Standard methods to study apoptosis include TUNEL staining, phosphatidylserine exposure in cell membrane, and analysis of caspase-3 and other components of the extrinsic (i.e., Fas, FasL) and intrinsic (i.e., Bax/Bcl-2 ratio, cytochrome-C) apoptotic pathways. Of note, the DNA repairing enzyme PARP-1, which is also recognized as an apoptotic marker, has been recently shown to be central in a genuine type of cell death termed parthanatos [55], and its potential role in DCM has already been stated [56]. STZ-treated hearts displayed a significant increase in cardiomyocyte apoptosis already at 3 days after injection. A progressive decrease of apoptosis was reported from 4 to 24 weeks after the induction of diabetes [57] (Table 1). In this line, we showed that apoptosis is more severe in long-standing STZ-treated hearts than in short-term ones [21]. Similarly, apoptosis was stimulated in OVE26 [58]. T2DM hearts also augmented rates of cell death. Comprehensive studies on ob/ob and db/db mice reported marked pro-apoptotic molecules and apoptosis [59, 60]. Moreover, cell death became more accentuated with aging [46, 61–63]. Likewise, we and others have described spread apoptosis in ZDF and GK myocardia [10, 12, 64]. Finally, most of the works on high-fat and high-sugar fed mice reported increased myocardial apoptosis [13, 43, 61, 65]. However, no change in apoptosis markers was identified in a more recent contribution in high-sucrose fed mice [66].
In summary, inflammation in human DCM usually occurs in early stages of the disease. Main established T1DM and T2DM models could emulate this response when analysed soon after the onset of the pathology. Also, most of them (but Akita) can exhibit myocardial hypertrophy, fibrosis, steatosis and apoptosis, preferentially at late stages of the disease. Thus, these models may be used to reproduce specific human responses to DCM, in particular when obesity coexists in the patients.
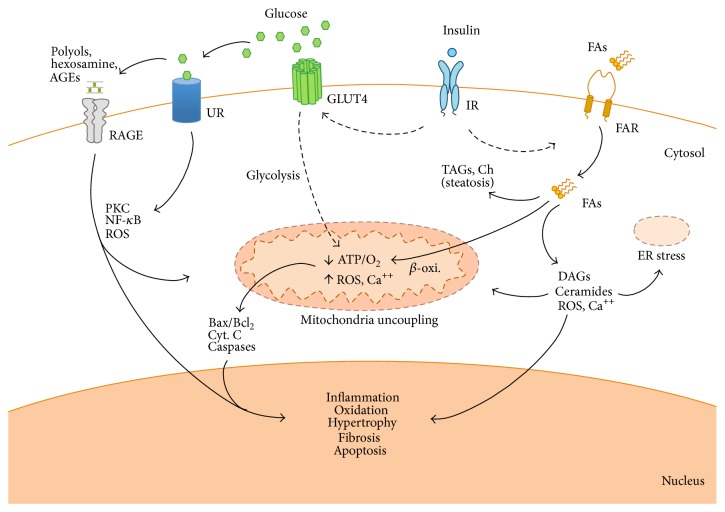
(2) Alterations in Cardiac Metabolism and Calcium Handling. The structural alterations in DCM may be originated by disruptions in energetic metabolism, which almost completely relies on FA and requires higher rates of O2 consumption. This scenario induces a progressive loss of cardiac efficiency by mitochondrial uncoupling and endoplasmic reticulum stress, and subsequent apoptosis and cardiac dysfunction [67] (Figure 1).
Figure 1.
The diabetic milieu at the myocardium. Thickened lines represent activated pathways, and dotted lines denote reduced pathways. The absence of insulin response by defect in its secretion (T1DM) or sensibility (T2DM) promotes a lack of glucose assimilation for energy demand in the cardiomyocytes and extracellular glucose accumulation. Thus, FA may be the unique energetic substrate but β-oxidation may saturate and lipid can accumulate and cause steatosis and lipotoxicity by DAG, ceramide, and ROS formation. These metabolites together with glucose derivatives (i.e., polyols, AGEs) damage the mitochondria and endoplasmic reticulum (ER) and regulate the expression of proinflammatory, hypertrophy, fibrotic, and apoptotic genes. RAGE, receptor for advanced glycation end products; UR, unspecific receptors; IR, insulin receptor; FAR, fatty acid receptors. Ch: cholesterol; Cyt. C: cytochrome-C.
(a) Energetic Imbalance. In human DCM, FA constitute principally the unique energy source of fuel due to the insulin inefficiency and reduction of glucose transporters and glucose oxidation enzymes [68]. As a consequence, PPAR(α, β, and γ) transcription factors are stimulated to increase gene expression of those proteins involved in FA-uptake, -transport, and -oxidation (FAO) and ceramide production, in both peroxisomes and mitochondria [69]. Main models of T1DM [62, 70, 71] exhibited a reduced expression of GLUT1 and GLUT4, and higher levels of the glucose oxidation inhibitor pyruvate dehydrogenase kinase 4 (PDK4) (Table 1). Upregulation of PPARα and FAO proteins has also been extensively described [62]. Likewise, Akita mice hearts showed lower glucose degradation and greater palmitate oxidation and expression of FA-transporters [24]. Nevertheless, most of the experimental data regarding metabolic abnormalities of the diabetic heart derive from T2DM models. Insulin resistance and higher FA utilization have been observed in ob/ob mice. As a result, myocardial O2 consumption rose, and cardiac performance substantially declined [64]. In the same model, a consistent decrease of key regulators of glucose metabolism such as phosphofructokinase (PFK) and GLUT-4 and increased expression of a set of PPARα and PPARγ independent genes involved in FA metabolism was reported [5]. In like fashion, db/db mice displayed a 40% decrease in glucose uptake, together with a considerable reduction in carbohydrate oxidation from age 10 weeks onwards. At this age, palmitate oxidation was shown to contribute over 90% to the cardiac FA production [26, 63]. In addition, we and others demonstrated the abnormal lipid metabolism of ZDF hearts, which include upregulation of genes involved in FA uptake, lipid reesterification, and β-oxidation [8, 10, 72]. Several studies ranging from gene expression assessment to quantitative positron emission tomography imaging have recently uncovered similar alterations in OLETF and GK rats [11, 31]. Diet-induced models have also disclosed similar disturbances. A recent work described an excessive FA metabolism in high-fat fed mice, supported also by upregulated PPARα [15]. In the same model, Cole et al. found increased FAO rates [73], though Ussher's group observed no association between lipid accumulation and insulin sensitivity [74].
(b) Mitochondrial Dysfunction and Oxidative Stress. Energetic imbalance triggers defects of mitochondrial respiration and ROS overload in human diabetes. In both T1DM and T2DM, metabolic maladaptation contributes to ROS imbalance by affecting multiple enzymatic systems including NADH oxidase (NOX), endothelial NO synthase, and, mainly, the mitochondrial respiratory chain [68, 75]. In STZ-treated rats, mitochondrial damage was evidenced by loss of membrane potential, increases in ROS production, and reduction in antioxidant glutathione [76] (Table 1). Further proteomic analysis revealed marked alterations in the expression of 24 different cardiac proteins implicated in metabolic derangement and ROS excess, half of them located in the mitochondria [77]. Likewise, OVE26 mice showed altered mitochondrial function, reduced glutathione, and increased mitochondrial biogenesis [62, 78, 79]. A comprehensive study pointed that mitochondria of Akita mice also displayed respiratory defects, reduced cristae density, and increased volume at the mitochondria. However, despite morphological aberrations, mitochondrial number and antioxidant defences remained unchanged, and the absence of mitochondrial uncoupling was evidenced by unaffected ATP-to-O2 ratio [71]. In T2DM, db/db mice exhibited increased O2 consumption, mitochondrial ROS generation, and lipid peroxidation. Mitochondrial uncoupling was associated with upregulated FAO genes and electron transfer flavoproteins [80]. Ob/ob mice and OLETF maintain unchanged levels of uncoupled proteins despite signal of mitochondrial dysfunction [81, 82]. Higher mitochondrial ROS production and lipid peroxidation rates have been also described in ZDF, OLETF, and GK rats [10, 83–85]. In addition, an elevation in antioxidant levels was demonstrated in ZDF rats [86]. Interestingly, ZDF rats neither displayed increased myocardial O2 consumption nor showed a significant reduction of mitochondrial biogenesis-related factors [10, 87]. Finally, mitochondrial uncoupling appears to be invariably present in cardiomyocytes from diet-induced obese mice. High-fat intake is associated with an increased burden of oxidized proteins, NOX and uncoupling-related factors, and antioxidant responses [43, 65, 73].
(c) Altered Ca 2+ Mobilization. A progressive dysregulation of Ca2+ handling underlies the relaxation-contraction defects in human DCM. Impaired Ca2+ signaling may be the consequence of altered sarcolemmal or sarcoplasmic Ca2+ pumps and channels and ryanodine receptors [88]. Cardiac mitochondria from STZ-treated rats decreased the capacity to stimulate ATP synthesis via stimulation of Ca2+ pumps, and, consequently, it abridged the relaxation during work load [89] (Table 1). Impaired contractility and reuptake of Ca2+ in cardiomyocytes from OVE26 mice were associated with reduced Ca2+ ATPase-60A (SERCA2a) levels and cytoplasmic Ca2+ clearance [90]. BB rats and Akita mice reported altered cardiac excitation-contraction coupling as well [24, 91]. In experimental T2DM models, the mechanisms explaining decreased Ca2+ uptake are not yet fully resolved. In ob/ob, Li et al. noted that SERCA2a was markedly modified by oxidation [92], whereas Van Den Bergh et al. showed increased SERCA2a levels with less affinity for Ca2+, which reduced contractile capacity [25]. In db/db mice, Belke's lab did not report significant variance in ryanodine receptor levels but lessened SERCA2a [93]. However, unchanged expression of SERCA2a has been described in ZDF [72] and intracellular Ca2+ transient was unaltered in GK cardiomyocytes [94]. In addition, cardiomyocytes from high-fat fed mice displayed a significantly elevated baseline intracellular Ca2+ and reduced Ca2+ decay rate, together with a marked decrease in SERCA2a expression [13, 65]. Further, sucrose fed rats showed reduced Ca2+ uptake [14], and fructose fed mice exhibited an attenuation of diastolic Ca2+ and Ca2+ transient amplitude, as well as SERCA2a expression [95].
Thus, the main T1DM and T2DM experimental models could replicate the metabolic alterations occurring in human hearts, including the energetic imbalance and mitochondrial and Ca2+ defects.
2. Cardiac Responses of DCM-Like Models Induced by Genetic Modification
Specific target genes have been modulated to create DCM-like models in rodents (Table 2). As detected in T1DM patients, cardiac dysfunction, hypertrophy, and fibrosis were demonstrated by upregulation of PKCβ [96] or by downregulation of GLUT4 [97–99], phosphoinositide dependent kinase-1 (PDK1) [100], phosphoinositide-3 kinase (PI3K) [101], or glucokinase (GCK) [102] genes (Table 2). Apoptosis and inflammation were less common (only in PKCβ and/or PI3K), and some metabolic controversies were described. For example, the lack of GLUT4 or the cardiac-specific insulin receptor (CIRKO) [103, 104] decreased both FA and glucose metabolisms, but it intriguingly elevated oxidative stress without reducing mitochondrial function. On the other hand, as observed in T2DM patients, a decline of cardiac function and increased myocardial hypertrophy, fibrosis, and steatosis were predominantly found in PPARα [105, 106], PPARγ [107, 108], long-chain acyl-CoA synthetase-1 (LCACS1) [109, 110], lipoprotein lipase (LPL) [111, 112], and fatty acid transport protein-1 (FATP1) [113, 114] overexpressed mice. Apoptosis was also presented in PPARγ, LCACS1, and, perhaps, LPL null mice. Interestingly, all these responses were exhibited by adipose triglyceride lipase (ATGL) deletion [115, 116]. Also, by ablation of the brown adipose tissue in the transgenic model of uncoupling protein-diphtheria toxin A (UCPDTA) [117, 118], mice exhibited a T2DM-like phenotype though a potential rise of related cardiac steatosis and apoptosis was not assessed. However, metabolic changes in all these models were principally represented by an increase of FA oxidation. The glucose metabolism, mitochondrial function, and Ca2+ mobilization were unpredictably changed or were not analysed.
Table 2.
Genetic models of DCM and related cardiac responses.
| Upregulation | Downregulation | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PPARα | PPARγ | LCACS1 | LPL | FATP1 | PKCβ | UCPDTA | CIRKO | GLUT4 | ATGL | PDK1 | PI3K | GCK | |
| Heart failure markers | ↑ANP, BNP | ↑ANP, BNP | ↑ANP, BNP | ↑ANP, BNP | ↑ANP, BNP | ↑ANP, BNP | |||||||
|
| |||||||||||||
| Cardiac abnormalities | |||||||||||||
| Functional | |||||||||||||
| Diastolic function | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓/~ | ↓ | ↓ | ↓ | ↓ |
| Systolic function | ↓ | ↓ | ↓ | ↓ | ~ | ↓ | ~ | ↓ | ↓/~ | ↓ | ↓ | ~ | |
| Structural | |||||||||||||
| Hypertrophy | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↓ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Inflammation | ↑ | ~ | |||||||||||
| Fibrosis | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ~ | ↑/~ | ↑ | ↑ | ↑ | ↑ | |
| Steatosis | ↑ | ↑ | ↑ | ↑ | ↑ | ~ | ~ | ↑ | |||||
| Apoptosis | ↑ | ↑ | ↑/~ | ↑ | ↑ | ~ | ↑ | ||||||
|
| |||||||||||||
| Metabolic alterations | |||||||||||||
| Glucose oxidation | ↓ | ~ | ↓ | ↓ | ↓/~ | ↑ | ↓ | ↓ | |||||
| FA oxidation | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↓ | ↓ | ↓ | ↑ | ↑ | ||
| Mitochondrial function | ↑ | ↑ | ↑ | ↑ | ↑ | ↓ | ↑ | ↑ | |||||
| Oxidative stress | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ||||||
| Ca2+ mobilization | ~ | ~ | ↓ | ~ | |||||||||
|
| |||||||||||||
| References | [105, 106] | [107, 108] | [109, 110] | [111, 112] | [113, 114] | [96] | [117, 118] | [103, 104] | [97–99] | [115, 116] | [100] | [101] | [102] |
Genetic overexpression of PPARα, PPARγ, long-chain acyl-CoA synthetase-1 (LCACS1), lipoprotein lipase (LPL), fatty acid transport protein-1 (FATP1), PKCβ and uncoupling protein-diphtheria toxin A (UCPDTA), or ablation of cardiac-specific insulin receptor (CIRKO), GLUT4, adipose triglyceride lipase (ATGL), phosphoinositide dependent kinase-1 (PDK1), phosphoinositide-3 kinase (PI3K), and glucokinase (GCK) were forced in rodents for DCM. The associated cardiac effects and the levels of natriuretic peptides in plasma are also highlighted for each model. ↑, ↓ and ~ stand for increased, decreased, or not modified effect, respectively.
3. Major Animal Models Recapitulating the Human DCM Pathology
3.1. T1DM Associated DCM-Like Models
The STZ-administration could recapitulate the most human DCM features associated with T1DM (Table 1). The injection of this β-cell killer can induce cardiac dysfunction in parallel with typical myocardial alterations in the structure and metabolism. However, STZ may also injure nonpancreatic tissues such as brain, and the rapid and accentuated onset of T1DM (i.e., robust hyperglycemia, lipotoxicity, and cardiac apoptosis after only 2-3 days of injection) can diverge from the human nature. In this regard, an upregulation of calmodulin in OVE26 mice may develop a slower and more humanized T1DM-associated DCM, though the energetic imbalance should be further examined. However, this point mutation disagrees with the patient aetiology, in which an autoimmune response is usually the origin of the disease. In addition, the lack of insulin production in Akita leads to some uncommon responses in the myocardium such as the absence of hypertrophy and fibrosis and unchanged levels of oxidation in spite of mitochondrial dysfunction. Nonconventional T1DM models may also emulate the human disorder (Table 2). Aside CIRKO and GLUT4 metabolic controversies, the absence of other mediators for glucose assimilation as GCK may mirror the T1DM phenotype in patients. Also, the lack of PDK1 might reduce the activation of PI3K-dependent insulin signaling [119], leading to a useful T1DM-associated DCM model.
3.2. T2DM Associated DCM-Like Models
Traditional models of T2DM are those with an abolished leptin-system activity (Table 1). Considering leptin activities other than satiety control, these models develop obesity and an average onset of T2DM pathology, with increased hyperglycemia, insulin resistance, and hyperlipidemia, in parallel with cardiac dysfunction. They mostly show expected structural alterations as in the human disorder. However, a polygenic model could be more representative. In this regard, GK rats trigger similar responses but the lack of obesity and steatosis is not usually observed in clinic. More valid models of T2DM-associated DCM can be the DIO. In particular, high-fat diet emulates responses of the leptin-system defect, including obesity and steatosis, but not as a consequence of a single mutation. These effects can be additionally enhanced by coadministration of STZ [120], though tissue toxicity may be increased. Other nonconventional approaches may mimic human DCM in T2DM (Table 2). The upregulation of PPARα or PPARγ unexpectedly leads to similar actions to the lack of leptin stimulation. In spite of increased FA-transporters and FAO enzymes, the myocardium accumulates lipids and ROS. Likely, the level of other PPAR-regulated genes such as reesterification enzymes, glucose transporters, and proinflammatory cytokines could also explain those actions [121]. Moreover, ATGL, LPL, and FATP1 are involved in FA uptake and accumulation in the cardiomyocytes, and LCACS1 catalyses the first step of lipid biosynthesis. In this regard, an excess of FA and lipid content could increase lipotoxicity and subsequent cardiac failure, as occurs in T2DM patients.
4. Conclusions and Future Remarks
Since human trials focused on identifying the cardiovascular outcomes of tight glycemic control failed to show significant benefit [122], the prevention and treatment of DCM may not be limited to the restoration of systemic parameters. It should also include the preservation of cardiac structure and function along with the local metabolic balances (Figure 1). Thus, the knowledge and manipulation of specific key pathways and mediators in appropriate experimental models may be useful for studying new approaches for diabetic patients. Although the experimental milieu (genetic background, diets, and animal location) must be obviously considered, we may have valuable armamentarium to investigate key factors for DCM pathology. In relation with current data, the most appropriate T1DM-model induced by pancreas toxicity is achieved by STZ. However, unique (nontoxic) mutations on glucose-related genes (not on insulin) have demonstrated a DCM-like T1DM phenotype, as occurs with GCK. In addition, due to its possible origin as an autoimmune failure, T1DM could be ideally produced by triggers of specific autoimmune reactions or β-cell death (i.e., virus, modified genes). For T2DM-linked DCM, we may have more working options, including both T2DM-obesity and T2DM aetiologies. Since human T2DM is usually acquired with an unhealthy lifestyle and/or unknown polygenic mutations, high-fat fed models can be closer to that point mutations on leptin system or in lipid storage. Polygenetic mutations of obesity, such as KK Ay, and OLETF, should be further characterized, and nonobese polygenetic mutated GK rats could facilitate the study of T2DM per se. However, we probably need diet-conditioned models of polygenetic mutations of T2DM to exemplify a bona fide approach to a related DCM.
Acknowledgments
This work was supported by national grants from Ministerio de Educación y Ciencia (SAF2009-08367) and Comunidad de Madrid (CCG10-UAM/BIO-5289).
Abbreviations
- AGEs:
Advanced glycation end products
- ANP:
Atrial natriuretic peptide
- AP-1:
Activating protein-1
- ATGL:
Adipose triglyceride lipase
- Bax:
Bcl-2-associated X protein
- Bcl2:
B-cell lymphoma 2
- BMP-2:
Bone morphogenetic protein-2
- BNP:
Brain natriuretic peptide
- DCM:
Diabetic cardiomyopathy
- ECM:
Extracellular matrix
- EF:
Ejection fraction
- FA:
Fatty acid
- FAO:
Fatty acid oxidation
- FasL:
Fas ligand
- FATP1:
Fatty acid transport protein-1
- FS:
Fractional shortening
- GCK:
Glucokinase
- GLUT:
Glucose transporter
- ICAM-1:
Intercellular adhesion molecule-1
- IFNγ:
Interferon-γ
- IL:
Interleukin
- LCACS1:
Long-chain acyl-CoA synthetase-1
- LV:
Left ventricular
- MCP-1:
Monocyte chemoattractant protein-1
- MMP:
Matrix metalloproteinase
- MRI:
Magnetic resonance imaging
- NFκB:
Nuclear factor of κ-light polypeptide gene enhancer in B-cells
- NOX:
NADH oxidase
- PARP-1:
Poly(ADP-ribose) polymerase 1
- PDK:
Phosphoinositide dependent kinase
- PI3K:
Phosphatidylinositol 3-kinase
- PKC:
Protein kinase C
- PPAR:
Peroxisome proliferator-activated receptor
- PW:
Posterior wall
- ROS:
Reactive oxygen species
- SERCA2a:
Sarco(endo)plasmic reticulum calcium ATPase
- TAG:
Triacylglyceride
- TGFβ:
Transforming growth factor β
- TIMP:
Tissue inhibitor of metalloprotease
- TNFα:
Tumor necrosis factor α
- TUNEL:
Terminal deoxynucleotidyl transferase- (TdT-) mediated dUTP nick end labelling
- UCPDTA:
Uncoupling protein- (UCP-) promoter-driven diphtheria toxin A
- VCAM-1:
Vascular cell adhesion molecule-1
- β-MHC:
β-Myosin heavy chain.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Niemann M., Herrmann S., Ertl G., Weidemann F. Echocardiography in diabetic cardiomyopathy. Herz. 2013;38(1):42–47. doi: 10.1007/s00059-012-3726-6. [DOI] [PubMed] [Google Scholar]
- 2.Khan J. N., Wilmot E. G., Leggate M., et al. Subclinical diastolic dysfunction in young adults with Type 2 diabetes mellitus: a multiparametric contrast-enhanced cardiovascular magnetic resonance pilot study assessing potential mechanisms. European Heart Journal—Cardiovascular Imaging. 2014;15(11):1263–1269. doi: 10.1093/ehjci/jeu121. [DOI] [PubMed] [Google Scholar]
- 3.Jellis C., Wright J., Kennedy D., et al. Association of imaging markers of myocardial fibrosis with metabolic and functional disturbances in early diabetic cardiomyopathy. Circulation: Cardiovascular Imaging. 2011;4(6):693–702. doi: 10.1161/circimaging.111.963587. [DOI] [PubMed] [Google Scholar]
- 4.Gao S., Ho D., Vatner D. E., Vatner S. F. Echocardiography in mice. Current Protocols in Mouse Biology. 2011;1:71–83. doi: 10.1002/9780470942390.mo100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christoffersen C., Bollano E., Lindegaard M. L. S., et al. Cardiac lipid accumulation associated with diastolic dysfunction in obese mice. Endocrinology. 2003;144(8):3483–3490. doi: 10.1210/en.2003-0242. [DOI] [PubMed] [Google Scholar]
- 6.Semeniuk L. M., Kryski A. J., Severson D. L. Echocardiographic assessment of cardiac function in diabetic db/db and transgenic db/db-hGLUT4 mice. American Journal of Physiology—Heart and Circulatory Physiology. 2002;283(3):H976–H982. doi: 10.1152/ajpheart.00088.2002. [DOI] [PubMed] [Google Scholar]
- 7.van den Bergh A., Flameng W., Herijgers P. Type II diabetic mice exhibit contractile dysfunction but maintain cardiac output by favourable loading conditions. European Journal of Heart Failure. 2006;8(8):777–783. doi: 10.1016/j.ejheart.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Zhou Y.-T., Grayburn P., Karim A., et al. Lipotoxic heart disease in obese rats: implications for human obesity. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(4):1784–1789. doi: 10.1073/pnas.97.4.1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daniels A., Linz D., van Bilsen M., et al. Long-term severe diabetes only leads to mild cardiac diastolic dysfunction in Zucker diabetic fatty rats. European Journal of Heart Failure. 2012;14(2):193–201. doi: 10.1093/eurjhf/hfr166. [DOI] [PubMed] [Google Scholar]
- 10.Ramírez E., Klett-Mingo M., Ares-Carrasco S., et al. Eplerenone attenuated cardiac steatosis, apoptosis and diastolic dysfunction in experimental type-II diabetes. Cardiovascular Diabetology. 2013;12(1, article 172) doi: 10.1186/1475-2840-12-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mizushige K., Yao L., Noma T., et al. Alteration in left ventricular diastolic filling and accumulation of myocardial collagen at insulin-resistant prediabetic stage of a type II diabetic rat model. Circulation. 2000;101(8):899–907. doi: 10.1161/01.cir.101.8.899. [DOI] [PubMed] [Google Scholar]
- 12.Picatoste B., Ramírez E., Caro-Vadillo A., et al. Sitagliptin reduces cardiac apoptosis, hypertrophy and fibrosis primarily by insulin-Dependent mechanisms in experimental type-II diabetes. Potential roles of GLP-1 isoforms. PLoS ONE. 2013;8(10) doi: 10.1371/journal.pone.0078330.e78330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fang C. X., Dong F., Thomas D. P., Ma H., He L., Ren J. Hypertrophic cardiomyopathy in high-fat diet-induced obesity: role of suppression of forkhead transcription factor and atrophy gene transcription. The American Journal of Physiology—Heart and Circulatory Physiology. 2008;295(3):H1206–H1215. doi: 10.1152/ajpheart.00319.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vasanji Z., Cantor E. J. F., Juric D., Moyen M., Netticadan T. Alterations in cardiac contractile performance and sarcoplasmic reticulum function in sucrose-fed rats is associated with insulin resistance. The American Journal of Physiology—Cell Physiology. 2006;291(4):C772–C780. doi: 10.1152/ajpcell.00086.2005. [DOI] [PubMed] [Google Scholar]
- 15.Pulinilkunnil T., Kienesberger P. C., Nagendran J., Sharma N., Young M. E., Dyck J. R. B. Cardiac-specific adipose triglyceride lipase overexpression protects from cardiac steatosis and dilated cardiomyopathy following diet-induced obesity. International Journal of Obesity. 2014;38(2):205–215. doi: 10.1038/ijo.2013.103. [DOI] [PubMed] [Google Scholar]
- 16.Somaratne J. B., Whalley G. A., Poppe K. K., et al. Screening for left ventricular hypertrophy in patients with type 2 diabetes mellitus in the community. Cardiovascular Diabetology. 2011;10, article 29 doi: 10.1186/1475-2840-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dei Cas A., Spigoni V., Ridolfi V., Metra M. Diabetes and chronic heart failure: from diabetic cardiomyopathy to therapeutic approach. Endocrine, Metabolic and Immune Disorders—Drug Targets. 2013;13(1):38–50. doi: 10.2174/1871530311313010006. [DOI] [PubMed] [Google Scholar]
- 18.Zibadi S., Cordova F., Slack E. H., Watson R. R., Larson D. F. Leptin's regulation of obesity-induced cardiac extracellular matrix remodeling. Cardiovascular Toxicology. 2011;11(4):325–333. doi: 10.1007/s12012-011-9124-0. [DOI] [PubMed] [Google Scholar]
- 19.Cox E. J., Marsh S. A. A systematic review of fetal genes as biomarkers of cardiac hypertrophy in rodent models of diabetes. PLoS ONE. 2014;9(3) doi: 10.1371/journal.pone.0092903.e92903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nemoto O., Kawaguchi M., Yaoita H., Miyake K., Maehara K., Maruyama Y. Left ventricular dysfunction and remodeling in streptozotocin-induced diabetic rats. Circulation Journal. 2006;70(3):327–334. doi: 10.1253/circj.70.327. [DOI] [PubMed] [Google Scholar]
- 21.Ares-Carrasco S., Picatoste B., Benito-Martín A., et al. Myocardial fibrosis and apoptosis, but not inflammation, are present in long-term experimental diabetes. The American Journal of Physiology—Heart and Circulatory Physiology. 2009;297(6):H2109–H2119. doi: 10.1152/ajpheart.00157.2009. [DOI] [PubMed] [Google Scholar]
- 22.Li Y., Ma J., Zhu H., et al. Targeted inhibition of calpain reduces myocardial hypertrophy and fibrosis in mouse models of type 1 diabetes. Diabetes. 2011;60(11):2985–2994. doi: 10.2337/db10-1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Y., Sun W., Du B., et al. Therapeutic effect of MG-132 on diabetic cardiomyopathy is associated with its suppression of proteasomal activities: roles of Nrf2 and NF-κB. American Journal of Physiology—Heart and Circulatory Physiology. 2013;304(4):H567–H578. doi: 10.1152/ajpheart.00650.2012. [DOI] [PubMed] [Google Scholar]
- 24.Basu R., Oudit G. Y., Wang X., et al. Type 1 diabetic cardiomyopathy in the Akita (Ins2WT/C96Y) mouse model is characterized by lipotoxicity and diastolic dysfunction with preserved systolic function. The American Journal of Physiology—Heart and Circulatory Physiology. 2009;297(6):H2096–H2108. doi: 10.1152/ajpheart.00452.2009. [DOI] [PubMed] [Google Scholar]
- 25.Van Den Bergh A., Vanderper A., Vangheluwe P., et al. Dyslipidaemia in type II diabetic mice does not aggravate contractile impairment but increases ventricular stiffness. Cardiovascular Research. 2008;77(2):371–379. doi: 10.1093/cvr/cvm001. [DOI] [PubMed] [Google Scholar]
- 26.Yue P., Arai T., Terashima M., et al. Magnetic resonance imaging of progressive cardiomyopathic changes in the db/db mouse. American Journal of Physiology: Heart and Circulatory Physiology. 2007;292(5):H2106–H2118. doi: 10.1152/ajpheart.00856.2006. [DOI] [PubMed] [Google Scholar]
- 27.Pereira L., Matthes J., Schuster I., et al. Mechanisms of [Ca2+]i transient decrease in cardiomyopathy of db/db type 2 diabetic mice. Diabetes. 2006;55(3):608–615. doi: 10.2337/diabetes.55.03.06.db05-1284. [DOI] [PubMed] [Google Scholar]
- 28.Fredersdorf S., Thumann C., Ulucan C., et al. Myocardial hypertrophy and enhanced left ventricular contractility in Zucker diabetic fatty rats. Cardiovascular Pathology. 2004;13(1):11–19. doi: 10.1016/s1054-8807(03)00109-1. [DOI] [PubMed] [Google Scholar]
- 29.Conti M., Renaud I. M., Poirier B., et al. High levels of myocardial antioxidant defense in aging nondiabetic normotensive Zucker obese rats. The American Journal of Physiology—Regulatory Integrative and Comparative Physiology. 2004;286(4):R793–R800. doi: 10.1152/ajpregu.00521.2002. [DOI] [PubMed] [Google Scholar]
- 30.Desrois M., Sidell R. J., Gauguier D., Davey C. L., Radda G. K., Clarke K. Gender differences in hypertrophy, insulin resistance and ischemic injury in the aging type 2 diabetic rat heart. Journal of Molecular and Cellular Cardiology. 2004;37(2):547–555. doi: 10.1016/j.yjmcc.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 31.Devanathan S., Nemanich S. T., Kovacs A., Fettig N., Gropler R. J., Shoghi K. I. Genomic and metabolic disposition of non-obese type 2 diabetic rats to increased myocardial Fatty Acid metabolism. PLoS ONE. 2013;8(10) doi: 10.1371/journal.pone.0078477.e78477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nunes S., Soares E., Fernandes J., et al. Early cardiac changes in a rat model of prediabetes: brain natriuretic peptide overexpression seems to be the best marker. Cardiovascular Diabetology. 2013;12, article 44 doi: 10.1186/1475-2840-12-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Axelsen L. N., Lademann J. B., Petersen J. S., et al. Cardiac and metabolic changes in long-term high fructose-fat fed rats with severe obesity and extensive intramyocardial lipid accumulation. The American Journal of Physiology—Regulatory Integrative and Comparative Physiology. 2010;298(6):R1560–R1570. doi: 10.1152/ajpregu.00392.2009. [DOI] [PubMed] [Google Scholar]
- 34.Tarikuz Zaman A. K. M., McLean D. L., Sobel B. E. The efficacy and tolerability of azilsartan in obese insulin-resistant mice with left ventricular pressure overload. Journal of Cardiovascular Pharmacology. 2013;62(4):381–387. doi: 10.1097/FJC.0b013e31829f0c1b. [DOI] [PubMed] [Google Scholar]
- 35.Noyan-Ashraf M. H., Shikatani E. A., Schuiki I., et al. A glucagon-like peptide-1 analog reverses the molecular pathology and cardiac dysfunction of a mouse model of obesity. Circulation. 2013;127(1):74–85. doi: 10.1161/circulationaha.112.091215. [DOI] [PubMed] [Google Scholar]
- 36.Schilling J. D., Mann D. L. Diabetic cardiomyopathy: bench to bedside. Heart Failure Clinics. 2012;8(4):619–631. doi: 10.1016/j.hfc.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mann D. L. Inflammatory mediators and the failing heart: past, present, and the foreseeable future. Circulation Research. 2002;91(11):988–998. doi: 10.1161/01.res.0000043825.01705.1b. [DOI] [PubMed] [Google Scholar]
- 38.Huang W., Glass C. K. Nuclear receptors and inflammation control: molecular mechanisms and pathophysiological relevance. Arteriosclerosis, Thrombosis, and Vascular Biology. 2010;30(8):1542–1549. doi: 10.1161/atvbaha.109.191189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fuentes-Antrás J., Ioan A. M., Tuñón J., Egido J., Lorenzo Ó. Activation of toll-like receptors and inflammasome complexes in the diabetic cardiomyopathy-associated inflammation. International Journal of Endocrinology. 2014;2014:10. doi: 10.1155/2014/847827.847827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chavali V., Tyagi S. C., Mishra P. K. Differential expression of dicer, miRNAs, and inflammatory markers in diabetic Ins2+/- akita hearts. Cell Biochemistry and Biophysics. 2014;68(1):25–35. doi: 10.1007/s12013-013-9679-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mori J., Patel V. B., Abo Alrob O., et al. Angiotensin 1-7 ameliorates diabetic cardiomyopathy and diastolic dysfunction in db/db mice by reducing lipotoxicity and inflammation. Circulation. Heart Failure. 2014;7(2):327–339. doi: 10.1161/circheartfailure.113.000672. [DOI] [PubMed] [Google Scholar]
- 42.Jadhav A., Tiwari S., Lee P., Ndisang J. F. The heme oxygenase system selectively enhances the anti-inflammatory macrophage-m2 phenotype, reduces pericardial adiposity, and ameliorated cardiac injury in diabetic cardiomyopathy in zucker diabetic fatty rats. Journal of Pharmacology and Experimental Therapeutics. 2013;345(2):239–249. doi: 10.1124/jpet.112.200808. [DOI] [PubMed] [Google Scholar]
- 43.Wang H.-T., Liu C.-F., Tsai T.-H., et al. Effect of obesity reduction on preservation of heart function and attenuation of left ventricular remodeling, oxidative stress and inflammation in obese mice. Journal of Translational Medicine. 2012;10(1, article 145) doi: 10.1186/1479-5876-10-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Álvarez-Guardia D., Palomer X., Coll T., et al. PPARβ/δ activation blocks lipid-induced inflammatory pathways in mouse heart and human cardiac cells. Biochimica et Biophysica Acta. 2011;1811(2):59–67. doi: 10.1016/j.bbalip.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 45.Way K. J., Isshiki K., Suzuma K., et al. Expression of connective tissue growth factor is increased in injured myocardium associated with protein kinase C β2 activation and diabetes. Diabetes. 2002;51(9):2709–2718. doi: 10.2337/diabetes.51.9.2709. [DOI] [PubMed] [Google Scholar]
- 46.Katayama S., Abe M., Negishi K., Takahashi K., Ishii J., Komeda K. Reciprocal changes in left ventricular collagen α1 chain gene expression between types I and IV in spontaneously diabetic rats. Diabetes Research and Clinical Practice. 1994;26(3):163–169. doi: 10.1016/0168-8227(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 47.Lee J. E., Yi C.-O., Jeon B. T., et al. α-lipoic acid attenuates cardiac fibrosis in Otsuka Long-Evans Tokushima Fatty rats. Cardiovascular Diabetology. 2012;11, article 111 doi: 10.1186/1475-2840-11-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lewis G. F., Carpentier A., Adeli K., Giacca A. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. Endocrine Reviews. 2002;23(2):201–229. doi: 10.1210/er.23.2.201. [DOI] [PubMed] [Google Scholar]
- 49.Korosoglou G., Humpert P. M., Ahrens J., et al. Left ventricular diastolic function in type 2 diabetes mellitus is associated with myocardial triglyceride content but not with impaired myocardial perfusion reserve. Journal of Magnetic Resonance Imaging. 2012;35(4):804–811. doi: 10.1002/jmri.22879. [DOI] [PubMed] [Google Scholar]
- 50.Ueno M., Suzuki J., Zenimaru Y., et al. Cardiac overexpression of hormone-sensitive lipase inhibits myocardial steatosis and fibrosis in streptozotocin diabetic mice. The American Journal of Physiology—Endocrinology and Metabolism. 2008;294(6):E1109–E1118. doi: 10.1152/ajpendo.00016.2008. [DOI] [PubMed] [Google Scholar]
- 51.Dong B., Qi D., Yang L., et al. TLR4 regulates cardiac lipid accumulation and diabetic heart disease in the nonobese diabetic mouse model of type 1 diabetes. The American Journal of Physiology—Heart and Circulatory Physiology. 2012;303(6):H732–H742. doi: 10.1152/ajpheart.00948.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barouch L. A., Gao D., Chen L., et al. Cardiac myocyte apoptosis is associated with increased DNA damage and decreased survival in murine models of obesity. Circulation Research. 2006;98(1):119–124. doi: 10.1161/01.res.0000199348.10580.1d. [DOI] [PubMed] [Google Scholar]
- 53.Diniz Y. S., Santos P. P., Assalin H. B., et al. Conjugated linoleic acid and cardiac health: oxidative stress and energetic metabolism in standard and sucrose-rich diets. European Journal of Pharmacology. 2008;579(1–3):318–325. doi: 10.1016/j.ejphar.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 54.Frustaci A., Kajstura J., Chimenti C., et al. Myocardial cell death in human diabetes. Circulation Research. 2000;87(12):1123–1132. doi: 10.1161/01.res.87.12.1123. [DOI] [PubMed] [Google Scholar]
- 55.Andrabi S. A., Dawson T. M., Dawson V. L. Mitochondrial and nuclear cross talk in cell death: parthanatos. Annals of the New York Academy of Sciences. 2008;1147:233–241. doi: 10.1196/annals.1427.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Puthanveetil P., Zhang D., Wang Y., et al. Diabetes triggers a PARP1 mediated death pathway in the heart through participation of FoxO1. Journal of Molecular and Cellular Cardiology. 2012;53(5):677–686. doi: 10.1016/j.yjmcc.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 57.Fiordaliso F., Li B., Latini R., et al. Myocyte death in streptozotocin-induced diabetes in rats is angiotensin II- dependent. Laboratory Investigation. 2000;80(4):513–527. doi: 10.1038/labinvest.3780057. [DOI] [PubMed] [Google Scholar]
- 58.Xie Z., Lau K., Eby B., et al. Improvement of cardiac functions by chronic metformin treatment is associated with enhanced cardiac autophagy in diabetic OVE26 mice. Diabetes. 2011;60(6):1770–1778. doi: 10.2337/db10-0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shen E., Li Y., Shan L., et al. Rac1 is required for cardiomyocyte apoptosis during hyperglycemia. Diabetes. 2009;58(10):2386–2395. doi: 10.2337/db08-0617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guleria R. S., Choudhary R., Tanaka T., Baker K. M., Pan J. Retinoic acid receptor-mediated signaling protects cardiomyocytes from hyperglycemia induced apoptosis: role of the renin-angiotensin system. Journal of Cellular Physiology. 2011;226(5):1292–1307. doi: 10.1002/jcp.22457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Matsui H., Yokoyama T., Sekiguchi K., et al. Stearoyl-CoA desaturase-1 (SCD1) augments saturated fatty acid-induced lipid accumulation and inhibits apoptosis in cardiac myocytes. PLoS ONE. 2012;7(3) doi: 10.1371/journal.pone.0033283.e33283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shen X., Zheng S., Thongboonkerd V., et al. Cardiac mitochondrial damage and biogenesis in a chronic model of type 1 diabetes. American Journal of Physiology—Endocrinology and Metabolism. 2004;287(5):E896–E905. doi: 10.1152/ajpendo.00047.2004. [DOI] [PubMed] [Google Scholar]
- 63.Aasum E., Hafstad A. D., Severson D. L., Larsen T. S. Age-dependent changes in metabolism, contractile function, and ischemic sensitivity in hearts from db/db mice. Diabetes. 2003;52(2):434–441. doi: 10.2337/diabetes.52.2.434. [DOI] [PubMed] [Google Scholar]
- 64.Mazumder P. K., O'Neill B. T., Roberts M. W., et al. Impaired cardiac efficiency and increased fatty acid oxidation in insulin-resistant ob/ob mouse hearts. Diabetes. 2004;53(9):2366–2374. doi: 10.2337/diabetes.53.9.2366. [DOI] [PubMed] [Google Scholar]
- 65.Ballal K., Wilson C. R., Harmancey R., Taegtmeyer H. Obesogenic high fat western diet induces oxidative stress and apoptosis in rat heart. Molecular and Cellular Biochemistry. 2010;344(1-2):221–230. doi: 10.1007/s11010-010-0546-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nunes S., Soares E., Fernandes J., et al. Early cardiac changes in a rat model of prediabetes: brain natriuretic peptide overexpression seems to be the best marker. Cardiovascular Diabetology. 2013;12(1, article 44) doi: 10.1186/1475-2840-12-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fang Z. Y., Prins J. B., Marwick T. H. Diabetic cardiomyopathy: evidence, mechanisms, and therapeutic implications. Endocrine Reviews. 2004;25(4):543–567. doi: 10.1210/er.2003-0012. [DOI] [PubMed] [Google Scholar]
- 68.Bugger H., Abel E. D. Mitochondria in the diabetic heart. Cardiovascular Research. 2010;88(2):229–240. doi: 10.1093/cvr/cvq239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee T.-I., Kao Y.-H., Chen Y.-C., Huang J.-H., Hsiao F.-C., Chen Y.-J. Peroxisome proliferator-activated receptors modulate cardiac dysfunction in diabetic cardiomyopathy. Diabetes Research and Clinical Practice. 2013;100(3):330–339. doi: 10.1016/j.diabres.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 70.Flarsheim C. E., Grupp I. L., Matlib M. A. Mitochondrial dysfunction accompanies diastolic dysfunction in diabetic rat heart. The American Journal of Physiology—Heart and Circulatory Physiology. 1996;271(1, part 2):H192–H202. doi: 10.1152/ajpheart.1996.271.1.H192. [DOI] [PubMed] [Google Scholar]
- 71.Bugger H., Boudina S., Hu X. X., et al. Type 1 diabetic akita mouse hearts are insulin sensitive but manifest structurally abnormal mitochondria that remain coupled despite increased uncoupling protein 3. Diabetes. 2008;57(11):2924–2932. doi: 10.2337/db08-0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Golfman L. S., Wilson C. R., Sharma S., et al. Activation of PPARγ enhances myocardial glucose oxidation and improves contractile function in isolated working hearts of ZDF rats. American Journal of Physiology—Endocrinology and Metabolism. 2005;289(2):E328–E336. doi: 10.1152/ajpendo.00055.2005. [DOI] [PubMed] [Google Scholar]
- 73.Cole M. A., Murray A. J., Cochlin L. E., et al. A high fat diet increases mitochondrial fatty acid oxidation and uncoupling to decrease efficiency in rat heart. Basic Research in Cardiology. 2011;106(3):447–457. doi: 10.1007/s00395-011-0156-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ussher J. R., Koves T. R., Jaswal J. S., et al. Insulin-stimulated cardiac glucose oxidation is increased in high-fat diet–induced obese mice lacking malonyl CoA decarboxylase. Diabetes. 2009;58:1766–1775. doi: 10.2337/db09-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ilkun O., Boudina S. Cardiac dysfunction and oxidative stress in the metabolic syndrome: an update on antioxidant therapies. Current Pharmaceutical Design. 2013;19(27):4806–4817. doi: 10.2174/1381612811319270003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ghosh S., Pulinilkunnil T., Yuen G., et al. Cardiomyocyte apoptosis induced by short-term diabetes requires mitochondrial GSH depletion. American Journal of Physiology—Heart and Circulatory Physiology. 2005;289(2):H768–H776. doi: 10.1152/ajpheart.00038.2005. [DOI] [PubMed] [Google Scholar]
- 77.Hamblin M., Friedman D. B., Hill S., Caprioli R. M., Smith H. M., Hill M. F. Alterations in the diabetic myocardial proteome coupled with increased myocardial oxidative stress underlies diabetic cardiomyopathy. Journal of Molecular and Cellular Cardiology. 2007;42(4):884–895. doi: 10.1016/j.yjmcc.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Song Y., Du Y., Prabhu S. D., Epstein P. N. Diabetic cardiomyopathy in OVE26 mice shows mitochondrial ROS production and divergence between in vivo and in vitro contractility. Review of Diabetic Studies. 2007;4(3):159–168. doi: 10.1900/RDS.2007.4.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liang Q., Carlson E. C., Donthi R. V., Kralik P. M., Shen X., Epstein P. N. Overexpression of metallothionein reduces diabetic cardiomyopathy. Diabetes. 2002;51(1):174–181. doi: 10.2337/diabetes.51.1.174. [DOI] [PubMed] [Google Scholar]
- 80.Boudina S., Sena S., Theobald H., et al. Mitochondrial energetics in the heart in obesity-related diabetes: direct evidence for increased uncoupled respiration and activation of uncoupling proteins. Diabetes. 2007;56(10):2457–2466. doi: 10.2337/db07-0481. [DOI] [PubMed] [Google Scholar]
- 81.Boudina S., Sena S., O'Neill B. T., Tathireddy P., Young M. E., Abel E. D. Reduced mitochondrial oxidative capacity and increased mitochondrial uncoupling impair myocardial energetics in obesity. Circulation. 2005;112(17):2686–2695. doi: 10.1161/CIRCULATIONAHA.105.554360. [DOI] [PubMed] [Google Scholar]
- 82.Boudina S., Abel E. D. Diabetic cardiomyopathy revisited. Circulation. 2007;115(25):3213–3223. doi: 10.1161/CIRCULATIONAHA.106.679597. [DOI] [PubMed] [Google Scholar]
- 83.Vázquez-Medina J. P., Popovich I., Thorwald M. A., et al. Angiotensin receptor-mediated oxidative stress is associated with impaired cardiac redox signaling and mitochondrial function in insulin-resistant rats. American Journal of Physiology—Heart and Circulatory Physiology. 2013;305(4):H599–H607. doi: 10.1152/ajpheart.00101.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Santos D. L., Palmeira C. M., Seiça R., et al. Diabetes and mitochondrial oxidative stress: a study using heart mitochondria from the diabetic Goto-Kakizaki rat. Molecular and Cellular Biochemistry. 2003;246(1-2):163–170. doi: 10.1023/a:1023475022025. [DOI] [PubMed] [Google Scholar]
- 85.Grijalva J., Hicks S., Zhao X., et al. Exercise training enhanced myocardial endothelial nitric oxide synthase (eNOS) function in diabetic Goto-Kakizaki (GK) rats. Cardiovascular Diabetology. 2008;7, article 34 doi: 10.1186/1475-2840-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Vincent H. K., Powers S. K., Dirks A. J., Scarpace P. J. Mechanism for obesity-induced increase in myocardial lipid peroxidation. International Journal of Obesity. 2001;25(3):378–388. doi: 10.1038/sj.ijo.0801536. [DOI] [PubMed] [Google Scholar]
- 87.Wang P., Lloyd S. G., Zeng H., Bonen A., Chatham J. C. Impact of altered substrate utilization on cardiac function in isolated hearts from Zucker diabetic fatty rats. American Journal of Physiology—Heart and Circulatory Physiology. 2005;288(5):H2102–H2110. doi: 10.1152/ajpheart.00935.2004. [DOI] [PubMed] [Google Scholar]
- 88.Turan B., Vassort G. Ryanodine receptor: a new therapeutic target to control diabetic cardiomyopathy. Antioxidants and Redox Signaling. 2011;15(7):1847–1861. doi: 10.1089/ars.2010.3725. [DOI] [PubMed] [Google Scholar]
- 89.Flarsheim C. E., Grupp I. L., Matlib M. A. Mitochondrial dysfunction accompanies diastolic dysfunction in diabetic rat heart. The American Journal of Physiology—Heart and Circulatory Physiology. 1996;271(1):H192–H202. doi: 10.1152/ajpheart.1996.271.1.H192. [DOI] [PubMed] [Google Scholar]
- 90.Kralik P. M., Ye G., Metreveli N. S., Shen X., Epstein P. N. Cardiomyocyte dysfunction in models of type 1 and type 2 diabetes. Cardiovascular Toxicology. 2005;5(3):285–292. doi: 10.1385/ct:5:3:285. [DOI] [PubMed] [Google Scholar]
- 91.Ren J., Bode A. M. Altered cardiac excitation-contraction coupling in ventricular myocytes from spontaneously diabetic BB rats. American Journal of Physiology: Heart and Circulatory Physiology. 2000;279(1):H238–H244. doi: 10.1152/ajpheart.2000.279.1.H238. [DOI] [PubMed] [Google Scholar]
- 92.Li S.-Y., Yang X., Ceylan-Isik A. F., Du M., Sreejayan N., Ren J. Cardiac contractile dysfunction in Lep/Lep obesity is accompanied by NADPH oxidase activation, oxidative modification of sarco(endo)plasmic reticulum Ca2+-ATPase and myosin heavy chain isozyme switch. Diabetologia. 2006;49(6):1434–1446. doi: 10.1007/s00125-006-0229-0. [DOI] [PubMed] [Google Scholar]
- 93.Belke D. D., Swanson E. A., Dillmann W. H. Decreased sarcoplasmic reticulum activity and contractility in diabetic db/db mouse heart. Diabetes. 2004;53(12):3201–3208. doi: 10.2337/diabetes.53.12.3201. [DOI] [PubMed] [Google Scholar]
- 94.Salem K. A., Adrian T. E., Qureshi M. A., Parekh K., Oz M., Howarth F. C. Shortening and intracellular Ca2+ in ventricular myocytes and expression of genes encoding cardiac muscle proteins in early onset type 2 diabetic Goto-Kakizaki rats. Experimental Physiology. 2012;97(12):1281–1291. doi: 10.1113/expphysiol.2012.066639. [DOI] [PubMed] [Google Scholar]
- 95.Mellor K. M., Wendt I. R., Ritchie R. H., Delbridge L. M. D. Fructose diet treatment in mice induces fundamental disturbance of cardiomyocyte Ca2+ handling and myofilament responsiveness. The American Journal of Physiology—Heart and Circulatory Physiology. 2012;302(4):H964–H972. doi: 10.1152/ajpheart.00797.2011. [DOI] [PubMed] [Google Scholar]
- 96.Wakasaki H., Koya D., Schoen F. J., et al. Targeted overexpression of protein kinase C β2 isoform in myocardium causes cardiomyopathy. Proceedings of the National Academy of Sciences of the United States of America. 1997;94(17):9320–9325. doi: 10.1073/pnas.94.17.9320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Abel E. D., Kaulbach H. C., Tian R., et al. Cardiac hypertrophy with preserved contractile function after selective deletion of GLUT4 from the heart. The Journal of Clinical Investigation. 1999;104(12):1703–1714. doi: 10.1172/jci7605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Domenighetti A. A., Danes V. R., Curl C. L., Favaloro J. M., Proietto J., Delbridge L. M. D. Targeted GLUT-4 deficiency in the heart induces cardiomyocyte hypertrophy and impaired contractility linked with Ca2+ and proton flux dysregulation. Journal of Molecular and Cellular Cardiology. 2010;48(4):663–672. doi: 10.1016/j.yjmcc.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 99.Li Y., Wende A. R., Nunthakungwan O., et al. Cytosolic, but not mitochondrial, oxidative stress is a likely contributor to cardiac hypertrophy resulting from cardiac specific GLUT4 deletion in mice. FEBS Journal. 2012;279(4):599–611. doi: 10.1111/j.1742-4658.2011.08450.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mora A., Davies A. M., Bertrand L., et al. Deficiency of PDK1 in cardiac muscle results in heart failure and increased sensitivity to hypoxia. The EMBO Journal. 2003;22(18):4666–4676. doi: 10.1093/emboj/cdg469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ritchie R. H., Love J. E., Huynh K., et al. Enhanced phosphoinositide 3-kinase(p110α) activity prevents diabetes-induced cardiomyopathy and superoxide generation in a mouse model of diabetes. Diabetologia. 2012;55(12):3369–3381. doi: 10.1007/s00125-012-2720-0. [DOI] [PubMed] [Google Scholar]
- 102.Li H., Wang X., Mao Y., et al. Long term liver specific glucokinase gene defect induced diabetic cardiomyopathy by up regulating NADPH oxidase and down regulating insulin receptor and p-AMPK. Cardiovascular Diabetology. 2014;13(1, article 24) doi: 10.1186/1475-2840-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Belke D. D., Betuing S., Tuttle M. J., et al. Insulin signaling coordinately regulates cardiac size, metabolism, and contractile protein isoform expression. Journal of Clinical Investigation. 2002;109(5):629–639. doi: 10.1172/jci200213946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Boudina S., Bugger H., Sena S., et al. Contribution of impaired myocardial insulin signaling to mitochondrial dysfunction and oxidative stress in the heart. Circulation. 2009;119(9):1272–1283. doi: 10.1161/CIRCULATIONAHA.108.792101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Finck B. N., Han X., Courtois M., et al. A critical role for PPARα-mediated lipotoxicity in the pathogenesis of diabetic cardiomyopathy: modulation by dietary fat content. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(3):1226–1231. doi: 10.1073/pnas.0336724100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Finck B. N., Lehman J. J., Leone T. C., et al. The cardiac phenotype induced by PPARα overexpression mimics that caused by diabetes mellitus. Journal of Clinical Investigation. 2002;109(1):121–130. doi: 10.1172/jci200214080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Son N.-H., Park T.-S., Yamashita H., et al. Cardiomyocyte expression of PPARγ leads to cardiac dysfunction in mice. Journal of Clinical Investigation. 2007;117(10):2791–2801. doi: 10.1172/jci30335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Son N.-H., Yu S., Tuinei J., et al. PPARγ-induced cardiolipotoxicity in mice is ameliorated by PPARα deficiency despite increases in fatty acid oxidation. Journal of Clinical Investigation. 2010;120(10):3443–3454. doi: 10.1172/jci40905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chiu H.-C., Kovacs A., Ford D. A., et al. A novel mouse model of lipotoxic cardiomyopathy. Journal of Clinical Investigation. 2001;107(7):813–822. doi: 10.1172/jci10947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liu L., Shi X. J., Bharadwaj K. G., et al. DGAT1 expression increases heart triglyceride content but ameliorates lipotoxicity. The Journal of Biological Chemistry. 2009;284(52):36312–36323. doi: 10.1074/jbc.m109.049817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yagyu H., Chen G., Yokoyama M., et al. Lipoprotein lipase (LpL) on the surface of cardiomyocytes increases lipid uptake and produces a cardiomyopathy. Journal of Clinical Investigation. 2003;111(3):419–426. doi: 10.1172/JCI200316751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yokoyama M., Yagyu H., Hu Y., et al. Apolipoprotein B production reduces lipotoxic cardiomyopathy. Studies in heart-specific lipoprotein lipase transgenic mouse. The Journal of Biological Chemistry. 2004;279(6):4204–4211. doi: 10.1074/jbc.m311995200. [DOI] [PubMed] [Google Scholar]
- 113.Chiu H.-C., Kovacs A., Blanton R. M., et al. Transgenic expression of fatty acid transport protein 1 in the heart causes lipotoxic cardiomyopathy. Circulation Research. 2005;96(2):225–233. doi: 10.1161/01.res.0000154079.20681.b9. [DOI] [PubMed] [Google Scholar]
- 114.Flagg T. P., Cazorla O., Remedi M. S., et al. Ca2+-independent alterations in diastolic sarcomere length and relaxation kinetics in a mouse model of lipotoxic diabetic cardiomyopathy. Circulation Research. 2009;104(1):95–103. doi: 10.1161/circresaha.108.186809. [DOI] [PubMed] [Google Scholar]
- 115.Haemmerle G., Lass A., Zimmermann R., et al. Defective lipolysis and altered energy metabolism in mice lacking adipose triglyceride lipase. Science. 2006;312(5774):734–737. doi: 10.1126/science.1123965. [DOI] [PubMed] [Google Scholar]
- 116.Kienesberger P. C., Pulinilkunnil T., Nagendran J., et al. Early structural and metabolic cardiac remodelling in response to inducible adipose triglyceride lipase ablation. Cardiovascular Research. 2013;99(3):442–451. doi: 10.1093/cvr/cvt124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cittadini A., Mantzoros C. S., Hampton T. G., et al. Cardiovascular abnormalities in transgenic mice with reduced brown fat: an animal model of human obesity. Circulation. 1999;100(21):2177–2183. doi: 10.1161/01.cir.100.21.2177. [DOI] [PubMed] [Google Scholar]
- 118.Duncan J. G., Fong J. L., Medeiros D. M., Finck B. N., Kelly D. P. Insulin-resistant heart exhibits a mitochondrial biogenic response driven by the peroxisome proliferator-activated receptor-α/PGC-1α gene regulatory pathway. Circulation. 2007;115(7):909–917. doi: 10.1161/circulationaha.106.662296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cho J. Y., Park J. Contribution of natural inhibitors to the understanding of the PI3K/PDK1/PKB pathway in the insulin-mediated intracellular signaling cascade. International Journal of Molecular Sciences. 2008;9(11):2217–2230. doi: 10.3390/ijms9112217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Marsh S. A., Dell'Italia L. J., Chatham J. C. Interaction of diet and diabetes on cardiovascular function in rats. American Journal of Physiology—Heart and Circulatory Physiology. 2009;296(2):H282–H292. doi: 10.1152/ajpheart.00421.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fuentes-Antrás J., Picatoste B., Ramírez E., Egido J., Tuñón J., Lorenzo Ó. Targeting metabolic disturbance in the diabetic heart. Cardiovascular Diabetology. 2015;14, article 17 doi: 10.1186/s12933-015-0173-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mazzone T. Intensive glucose lowering and cardiovascular disease prevention in diabetes: reconciling the recent clinical trial data. Circulation. 2010;122(21):2201–2211. doi: 10.1161/circulationaha.109.913350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Islas-Andrade S., Monsalve M. C. R., De La Peña J. E., Polanco A. C., Palomino M. A., Velasco A. F. Streptozotocin and alloxan in experimental diabetes: comparison of the two models in rats. Acta Histochemica et Cytochemica. 2000;33(3):201–208. doi: 10.1267/ahc.33.201. [DOI] [Google Scholar]
- 124.Lopaschuk G. D., Tsang H. Metabolism of palmitate in isolated working hearts from spontaneously diabetic ‘BB’ Wistar rats. Circulation Research. 1987;61(6):853–858. doi: 10.1161/01.res.61.6.853. [DOI] [PubMed] [Google Scholar]
- 125.Buchanan J., Mazumder P. K., Hu P., et al. Reduced cardiac efficiency and altered substrate metabolism precedes the onset of hyperglycemia and contractile dysfunction in two mouse models of insulin resistance and obesity. Endocrinology. 2005;146(12):5341–5349. doi: 10.1210/en.2005-0938. [DOI] [PubMed] [Google Scholar]
- 126.Forcheron F., Basset A., Abdallah P., Carmine P. D., Gadot N., Beylot M. Diabetic cardiomyopathy: effects of fenofibrate and metformin in an experimental model—the Zucker diabetic rat. Cardiovascular Diabetology. 2009;8, article 16 doi: 10.1186/1475-2840-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Iwatsuka H., Shino A., Suzuoki Z. General survey of diabetic features of yellow KK mice. Endocrinologia Japonica. 1970;17(1):23–35. doi: 10.1507/endocrj1954.17.23. [DOI] [PubMed] [Google Scholar]
- 128.Kawano K., Hirashima T., Mori S., Saitoh Y., Kurosumi M., Natori T. Spontaneous long-term hyperglycemic rat with diabetic complications: Otsuka Long-Evans Tokushima Fatty (OLETF) strain. Diabetes. 1992;41(11):1422–1428. doi: 10.2337/diab.41.11.1422. [DOI] [PubMed] [Google Scholar]
- 129.Tourrel C., Bailbe D., Lacorne M., Meile M.-J., Kergoat M., Portha B. Persistent improvement of type 2 diabetes in the Goto-Kakizaki rat model by expansion of the β-cell mass during the prediabetic period with glucagon-like peptide-1 or exendin-4. Diabetes. 2002;51(5):1443–1452. doi: 10.2337/diabetes.51.5.1443. [DOI] [PubMed] [Google Scholar]
- 130.Winzell M. S., Ahrén B. The high-fat diet-fed mouse: a model for studying mechanisms and treatment of impaired glucose tolerance and type 2 diabetes. Diabetes. 2004;53(supplement 3):S215–S219. doi: 10.2337/diabetes.53.suppl_3.s215. [DOI] [PubMed] [Google Scholar]
- 131.Bar On H., Roheim P. S., Eder H. A. Serum lipoproteins and apolipoproteins in rats with streptozotocin induced diabetes. Journal of Clinical Investigation. 1976;57(3):714–721. doi: 10.1172/jci108329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Altomonte J., Cong L., Harbaran S., et al. Foxo1 mediates insulin action on apoC-III and triglyceride metabolism. The Journal of Clinical Investigation. 2004;114(10):1493–1503. doi: 10.1172/jci200419992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tang C., Kanter J. E., Bornfeldt K. E., Leboeuf R. C., Oram J. F. Diabetes reduces the cholesterol exporter ABCA1 in mouse macrophages and kidneys. Journal of Lipid Research. 2010;51(7):1719–1728. doi: 10.1194/jlr.m003525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Naveilhan P., Svensson L., Nyström S., Ekstrand A. J., Ernfors P. Attenuation of hypercholesterolemia and hyperglycemia in ob/ob mice by NPY Y2 receptor ablation. Peptides. 2002;23(6):1087–1091. doi: 10.1016/S0196-9781(02)00042-6. [DOI] [PubMed] [Google Scholar]
- 135.Kobayashi K., Forte T. M., Taniguchi S., Ishida B. Y., Oka K., Chan L. The db/db mouse, a model for diabetic dyslipidemia: Molecular characterization and effects of western diet feeding. Metabolism: Clinical and Experimental. 2000;49(1):22–31. doi: 10.1016/s0026-0495(00)90588-2. [DOI] [PubMed] [Google Scholar]
- 136.Sparks J. D., Phung T. L., Bolognino M., et al. Lipoprotein alterations in 10- and 20-week-old Zucker diabetic fatty rats: hyperinsulinemic versus insulinopenic hyperglycemia. Metabolism: Clinical and Experimental. 1998;47(11):1315–1324. doi: 10.1016/s0026-0495(98)90298-0. [DOI] [PubMed] [Google Scholar]
- 137.Shimizugawa T., Ono M., Shimamura M., et al. ANGPTL3 decreases very low density lipoprotein triglyceride clearance by inhibition of lipoprotein lipase. The Journal of Biological Chemistry. 2002;277(37):33742–33748. doi: 10.1074/jbc.m203215200. [DOI] [PubMed] [Google Scholar]
- 138.Calligaris S. D., Lecanda M., Solis F., et al. Mice long-term high-fat diet feeding recapitulates human cardiovascular alterations: an animal model to study the early phases of diabetic cardiomyopathy. PLoS ONE. 2013;8(4) doi: 10.1371/journal.pone.0060931.e60931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Oliveira-Junior S. A., Martinez P. F., Guizoni D. M., et al. AT1 receptor blockade attenuates insulin resistance and myocardial remodeling in rats with diet-induced obesity. PLoS ONE. 2014;9(1) doi: 10.1371/journal.pone.0086447.e86447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Joffe I. I., Travers K. E., Perreault-Micale C. L., et al. Abnormal cardiac function in the streptozotocin-induced, non-insulin-dependent diabetic rat: noninvasive assessment with Doppler echocardiography and contribution of the nitric oxide pathway. Journal of the American College of Cardiology. 1999;34(7):2111–2119. doi: 10.1016/s0735-1097(99)00436-2. [DOI] [PubMed] [Google Scholar]
- 141.Fein F. S., Miller-Green B., Sonnenblick E. H. Altered myocardial mechanics in diabetic rabbits. American Journal of Physiology—Heart and Circulatory Physiology. 1985;248(5, part 2):H729–H736. doi: 10.1152/ajpheart.1985.248.5.H729. [DOI] [PubMed] [Google Scholar]
- 142.Semeniuk L. M., Kryski A. J., Severson D. L. Echocardiographic assessment of cardiac function in diabetic db/db and transgenic db/db-hGLUT4 mice. American Journal of Physiology: Heart and Circulatory Physiology. 2002;283(3):H976–H982. doi: 10.1152/ajpheart.00088.2002. [DOI] [PubMed] [Google Scholar]
- 143.Rodrigues B., McNeill J. H. Cardiac dysfunction in isolated perfused hearts from spontaneously diabetic BB rats. Canadian Journal of Physiology and Pharmacology. 1990;68(4):514–518. doi: 10.1139/y90-073. [DOI] [PubMed] [Google Scholar]
- 144.Pulinilkunnil T., Kienesberger P. C., Nagendran J., Sharma N., Young M. E., Dyck J. R. B. Cardiac-specific adipose triglyceride lipase overexpression protects from cardiac steatosis and dilated cardiomyopathy following diet-induced obesity. International Journal of Obesity. 2014;38(2):205–215. doi: 10.1038/ijo.2013.103. [DOI] [PubMed] [Google Scholar]
- 145.Lu Z., Jiang Y.-P., Xu X.-H., Ballou L. M., Cohen I. S., Lin R. Z. Decreased L-type Ca2+ current in cardiac myocytes of type 1 diabetic akita mice due to reduced phosphatidylinositol 3-kinase signaling. Diabetes. 2007;56(11):2780–2789. doi: 10.2337/db06-1629. [DOI] [PubMed] [Google Scholar]
- 146.Pacher P., Liaudet L., Soriano F. G., Mabley J. G., Szabó É., Szabó C. The role of poly(ADP-ribose) polymerase activation in the development of myocardial and endothelial dysfunction in diabetes. Diabetes. 2002;51(2):514–521. doi: 10.2337/diabetes.51.2.514. [DOI] [PubMed] [Google Scholar]
- 147.Broderick T. L., Hutchison A. K. Cardiac dysfunction in the euglycemic diabetic-prone BB Wor rat. Metabolism: Clinical and Experimental. 2004;53(11):1391–1394. doi: 10.1016/j.metabol.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 148.Van den Bergh A., Flameng W., Herijgers P. Type II diabetic mice exhibit contractile dysfunction but maintain cardiac output by favourable loading conditions. European Journal of Heart Failure. 2006;8(8):777–783. doi: 10.1016/j.ejheart.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 149.Hsiao Y.-C., Suzuki K.-I., Abe H., Toyota T. Ultrastructural alterations in cardiac muscle of diabetic BB Wistar rats. Virchows Archiv A. 1987;411(1):45–52. doi: 10.1007/bf00734513. [DOI] [PubMed] [Google Scholar]
- 150.Li L., Hua Y., Dong M., et al. Short-term lenalidomide (Revlimid) administration ameliorates cardiomyocyte contractile dysfunction in ob/ob obese mice. Obesity. 2012;20(11):2174–2185. doi: 10.1038/oby.2012.106. [DOI] [PubMed] [Google Scholar]
- 151.Saito K., Nishi S., Kashima T., Tanaka H. Histologic and ultrastructural studies on the myocardium in spontaneously diabetic KK mice: a new animal model of cardiomyopathy. The American Journal of Cardiology. 1984;53(2):320–323. doi: 10.1016/0002-9149(84)90446-6. [DOI] [PubMed] [Google Scholar]
- 152.Boudina S., Sena S., Theobald H., et al. Mitochondrial energetics in the heart in obesity-related diabetes: direct evidence for increased uncoupled respiration and activation of uncoupling proteins. Diabetes. 2007;56(10):2457–2466. doi: 10.2337/db07-0481. [DOI] [PubMed] [Google Scholar]
- 153.Akhileshwar V., Patel S. P., Katyare S. S. Diabetic cardiomyopathy and reactive oxygen species (ROS) related parameters in male and female rats: a comparative study. Indian Journal of Clinical Biochemistry. 2007;22(1):84–90. doi: 10.1007/bf02912887. [DOI] [PMC free article] [PubMed] [Google Scholar]