Dear Editor,
Brain metastases from malignant melanoma are common, and it result in severe morbidity and mortality.[1] Approximately, 10–40% of patients with melanoma develop brain metastasis (autopsy rates are much higher), and 50% of melanoma brain metastases (MBM) turn hemorrhagic.[2] Invasion of brain blood vessels, rapid growth, hemorrhagic infarction, leaky endothelium, and fragile blood vessels are postulated resulting in hemorrhage.[2]
A 55-year-old male presented with altered sensorium, headache, and weakness of right upper and lower limb since 1 day. Patient was a known alcoholic and smoker for 35 years. He had recent complaints of decreased appetite and irregular bowel, bladder habits. On examination, he was drowsy and arousable, pupils were sluggish and reactive to light. Motor examination revealed 3/5 power in right upper and lower limbs. He was localizing on the left side. On chest examination, he had bilateral crepitation and conducted sounds. In view of poor neurological status, the patient was intubated. Plain computed tomography (CT) scan brain showed a well-defined heterogeneous mass with hemorrhage in the left parieto-occipital region with adjacent vasogenic edema and mass effect [Figure 1a-c, upper row]. His chest X-ray was normal. A differential diagnosis of tumor with bleed and hypertensive bleed was considered. The patient was started on anti-edema measures and anti-epileptics. The patient underwent left parieto-occiptial craniotomy and total decompression of the lesion. Intraoperatively, there thick dark color clotted blood with tumor tissue. The patient was kept on elective ventilation and could be weaned off on day 2 post-surgery. The patient became conscious, and his power improved to almost normal. Histopathology showed metastatic carcinomatous deposit showing dispersed tumor cells having hyperchromatic nuclei of varying sizes, prominent eosinophilic nuclei, cytoplasm was showing brown to black pigment [Figure 1a-c, lower row].
Figure 1.
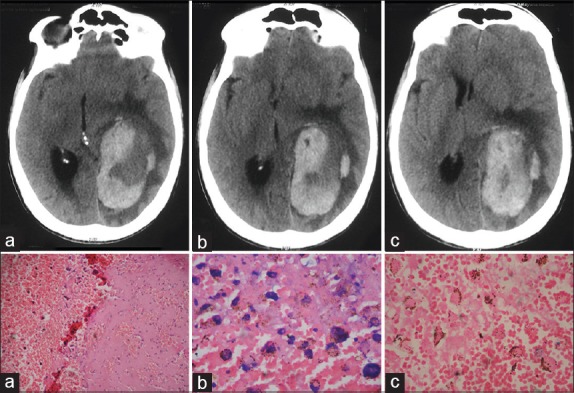
(Upper row) Well-defined hyperattenuating hemorrhagic mass in the left parieto-occipital region with adjacent vasogenic edema and mass effect as described, lower row (a) Hemorrhagic material with dispersed tumor cells (H and E, ×100), (b) tumor cell having hyperchromatic nuclei and cytoplasm with brown-black pigment (H and E, ×400) and (c) Hemorrhagic material with dispersed hemosiderin-laden macrophages (H and E, ×400)
High neurotropism of malignant melanoma cells makes the brain one of the frequent site of metastases.[3] It has been postulated that neurotrophins or chemokines co-ordinate with receptors on melanoma cells which create an environment for their survival.[3] Once tumor cells arrive into the target brain circulation, they are seized in the capillary bed depending on the size, few tumor cells cross the endothelial barrier and interact with astrocytes and microglia, and establish neovascularization which is necessary for sustained tumor growth.[4] Clinical symptoms include frequent headaches and other symptoms of raised intracranial pressure, seizures, and focal neurological deficits.[1,3] Although magnetic resonance imaging is the gold standard in diagnosing metastases from melanoma as it can differentiate amelanotic pattern from the melanotic pattern of metastases and metastases with tumoral hemorrhage, CT brain with contrast can detect melanoma metastases of approximate size of 1 cm and most hemorrhagic lesions.[1] Variegated appearance, heterogeneous enhancement should help us diagnosis tumoral hemorrhage.[1] Prime role of surgery is to do debulk the tumor and reduce vasogenic edema, mass effect, local recurrence can be treated with surgery and adjuvant whole brain radiotherapy.[3] MBM'S have extremely grave prognosis and the reported median survival rate for patients treated with surgery and radiotherapy is 8.9 months.[5] Recently, novel treatments such as monoclonal BRAF inhibitors and immunotherapies have been introduced, and they have been showing good improvement in survival rates.[3,6]
Although approximately 50% of MBM turn hemorrhagic but melanoma presenting with neurological deficits and focal weakness is an uncommon first manifestation. In such cases, removal of intracranial mass may not increase the survival; however, it can improve the quality-of-life of the survivors.
References
- 1.Sloan AE, Nock CJ, Einstein DB. Diagnosis and treatment of melanoma brain metastasis: A literature review. Cancer Control. 2009;16:248–55. doi: 10.1177/107327480901600307. [DOI] [PubMed] [Google Scholar]
- 2.Yoo H, Jung E, Gwak HS, Shin SH, Lee SH. Surgical outcomes of hemorrhagic metastatic brain tumors. Cancer Res Treat. 2011;43:102–7. doi: 10.4143/crt.2011.43.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kenchappa RS, Tran N, Rao NG, Smalley KS, Gibney GT, Sondak VK, et al. Novel treatments for melanoma brain metastases. Cancer Control. 2013;20:298–306. doi: 10.1177/107327481302000407. [DOI] [PubMed] [Google Scholar]
- 4.Peres MF, Forones NM, Malheiros SM, Ferraz HB, Stávale JN, Gabbai AA. Hemorrhagic cerebral metastasis as a first manifestation of a hepatocellular carcinoma. Case report. Arq Neuropsiquiatr. 1998;56:658–60. doi: 10.1590/s0004-282x1998000400023. [DOI] [PubMed] [Google Scholar]
- 5.Sampson JH, Carter JH, Jr, Friedman AH, Seigler HF. Demographics, prognosis, and therapy in 702 patients with brain metastases from malignant melanoma. J Neurosurg. 1998;88:11–20. doi: 10.3171/jns.1998.88.1.0011. [DOI] [PubMed] [Google Scholar]
- 6.Papadatos-Pastos D, Soultati A, Harries M. Targeting brain metastases in patients with melanoma. Biomed Res Int 2013. 2013 doi: 10.1155/2013/186563. 186563. [DOI] [PMC free article] [PubMed] [Google Scholar]


