Abstract
Background:
Early tracheostomy (ET) has been shown to be effective in reducing complications associated with prolong mechanical ventilation. The study was carried out to evaluate the role of ET in reducing the duration of mechanical ventilation, duration of intensive care unit (ICU) stay, ICU-related morbidities, and its overall effect on outcome, in patients with isolated severe traumatic brain injury (TBI).
Methods:
This 7-year review included 100 ICU patients with isolated severe TBI requiring mechanical ventilation. ET was defined as tracheostomy within 7 days of TBI, and prolonged endotracheal intubation (EI) as EI exceeding 7 days of TBI. Of 100 patients, 49 underwent ET and 51 remained on prolong EI for ventilation. All patients were comparable in term of age and initial Glasgow Coma Scale (GCS). We evaluated groups regarding clinical outcome in terms of ventilator-associated pneumonia (VAP), ICU stay, and Glasgow Outcome Score (GOS).
Results:
The frequency of VAP was higher in EI group relative to ET group (63% vs. 45%, P value 0.09). ET group showed significantly less ventilator days (10 days vs. 13 days, P value 0.031), ICU stay (11 days vs. 13 days, P value 0.030), complication rate (14% vs. 18%), and mortality (8.2% vs. 17.6%). Clinical outcome assessed on the basis of GOS was also better in the ET group. Total inpatient cost was also considerably less (USD $8027) in the ET group compared with the EI group (USD $9961).
Conclusions:
In patients with severe TBI, ET decreases total days of ventilation and ICU stay, and is associated with a decrease in the frequency of VAP. ET should be considered in severe head injury patients requiring prolong ventilatory support.
Keywords: Early tracheostomy, prolonged endotracheal intubation, severe traumatic brain injury
INTRODUCTION
There is sufficient literature to support early tracheostomy (ET) in intensive care unit (ICU) patients who fail to wean off the ventilator easily.[16] Tracheostomy not only provides a relatively stable and a well tolerated airway but also provides access for good pulmonary toilet, makes oral feeding possible and permits earlier ambulation in turn preventing orthostatic and ventilator-associated pneumonia (VAP).[9] It also avoids any oropharangeal and/or laryngeal injury usually observed with endotracheal intubation (EI).[2,3,6] Although several complications, such as hemorrhage, tracheal stenosis, stomal infection, have been reported, these are relatively infrequent.[8] Despite ET being a standard part in the clinical algorithm for management of patients requiring prolonged ventilation, comparatively little data are available that defines its significance in patients with isolated severe traumatic brain injury (TBI). This present study was designed in order to identify the impact of ET on the duration of mechanical ventilation, ICU stay, VAP, and mortality compared with prolonged EI, specifically for patients with isolated severe TBI.
MATERIALS AND METHODS
The study included all the inpatients fulfilling the inclusion criteria, presenting at the Aga Khan University Hospital from January 2002 to December 2009. A review of prospectively collected data from July 2004 to December 2009, in addition to some retrospectively collected data from January 2002 to June 2004 was analyzed.
The Aga Khan University Hospital is a 577-bed, Level 1 trauma center and currently has the largest ICU center in the metropolitan city of Karachi. It is a referral center for trauma patients in the city. The hospital runs a neurosurgery residency program that deals with patients of all age groups, without subspecialty sections for pediatric and adult TBI. The intensive care teams for pediatric and adult patients, however, are separate. As an institutional protocol, every patient with a TBI arriving to the emergency department with a Glasgow Coma Scale (GCS) score of 8 or less immediately receives EI; the remaining patients are managed without intubation. We do not routinely perform intracranial pressure monitoring for patients with TBI. Patients with mass lesions, such as extradural or subdural hematoma, fulfilling Brain Trauma Foundation guidelines, are brought to the operating room for decompressive surgery with or without replacement of the bone flap, depending on intraoperative findings. Patients without obvious mass lesions but with intracranial hypertension and persistently low GCS scores undergo ventilation in the ICU and are treated on the basis of Lund protocol and undergo serial neurological examinations and neuroimaging.
Patients were included in the study if they had isolated severe TBI (defined as a GCS <8) requiring airway control and ventilation. For the purpose of this study ET was defined as tracheostomy performed within 7 days of intubation and patients who were kept on ventilation through translaryngeal intubation for more than 7 days were included in prolonged EI group. We excluded pediatric patients and those adult patients who had polytrauma with systemic injuries requiring mechanical ventilation. All tracheostomy procedures were performed by the Neurosurgery team in the operating room.
There is no defined protocol to decide the mode of ventilation for such patients. The choice to proceed with an ET compared with EI was the decision of the attending neurosurgeon on call, based on the presentation of the patient. Our institutional data suggests that abnormal pupillary response on arrival, preoperative neurological worsening during hospital stay, presence of preexisting medical comorbid conditions, and delay in emergency room arrival exceeding 1.5 h are all independently predictive of tracheostomy in patients of severe TBI. All of the above factors in addition to a low GCS and presumed prolonged intubation were strongly considered in each patient.
Clinical outcome
The duration of intubation, ventilation, intensive care stay, and mortality in each group was recorded. All intraoperative and postoperative complications of tracheostomy, as well as prolonged EI, were also recorded. Both groups were compared in terms of incidence of VAP and acute respiratory distress syndrome (ARDS). Clinical outcome of patients in both groups was compared on the basis of Glasgow Outcome Score (GOS).
Cost of treatment
All cost data was calculated in Pakistani Rupee (PKR) and then converted to US Dollar (USD) (the conversion factor of $1 = PKR 85 was used as of 2009). The cost of treatment for each patient was calculated to evaluate the expenses incurred during the time spent as an inpatient. This included cost of initial hospital stay including the time spent in the emergency room, ICU bed occupancy, special care bed occupancy, regular hospital bed, laboratory tests and imaging studies and the cost of any neurosurgical procedure performed. The total cost was obtained from the billing department of the institution. All cost data are presented in PKR and USD. It should be noted that the cost does not include any expenditure that might have occurred due to additional hospitalizations or rehabilitation at the Aga Khan University Hospital or any other institution after discharge, or any expected expenditures regarding future procedures.
Statistical analysis
All the data was entered into and analyzed using Statistical Package of Social Sciences (SPSS) v17.0 for Microsoft Windows 7. Outcome variables were analyzed by a simple categorical frequency comparison with the Chi-square (X2). Continuous variables were analyzed as means ± SDs, and the Student t-test was used to compare the two groups. A P <0.05 was considered statistically significant.
RESULTS
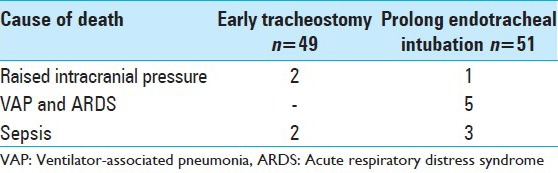
This 8-year review included 100 ICU patients with severe traumatic head injury requiring mechanical ventilation and tracheostomy. Of 100 patients, 49 underwent ET and 51 remained on prolonged EI for ventilation. The two groups were comparable in terms of age, gender, and arrival GCS. The mean time of mechanical ventilation was 10 days in ET group and 13 days for patients who were kept on endotracheal tube. The incidence of VAP was significantly higher in EI group, relative to ET group (63% vs. 45%, respectively). Gram-negative bacilli, especially Acinetobacter and Pseudomonas, were the most frequently isolated bacteria in tracheal cultures of patients with VAP. Due to shorter ventilation and decreased incidence of VAP, patients in ET group were shifted out of ICU earlier as compared with EI group. The average ICU stay was 11 and 13 days in the ET and EI groups, respectively. There was no case of tracheal stenosis. However, two patients had nonlethal stomal bleed and three stomal infections were noted in the ET group. Four cases of labial and tongue lacerations were present in the prolonged EI group. Out of 51 patients, 2 had accidental extubations in EI group. In contrary to ICU stay, total hospital stay was longer in ET group, that is, 29 days [Table 1]. Clinical outcome was assessed on the basis of GOS. Patients who underwent ET showed a better clinical outcome as compared with prolonged EI group [Table 2]. Mortality rate was higher in prolonged EI group (17.6%) due to the longer ICU stay and increased incidence of VAP. Intracranial hypertension and sepsis were the cause of death in ET group, while ARDS and sepsis were the major causes of death for the EI group [Table 3].
Table 1.
Comparison of baseline characteristics, mechanical ventilation, ICU, and total hospital stay between the two groups
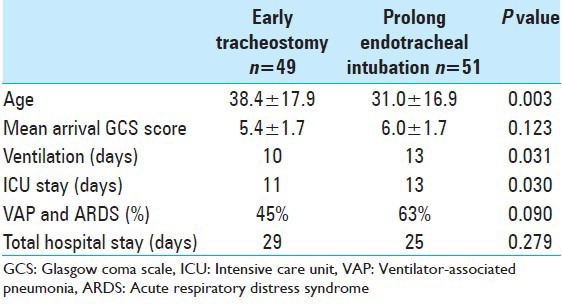
Table 2.
Clinical outcome on basis of glasgow outcome score
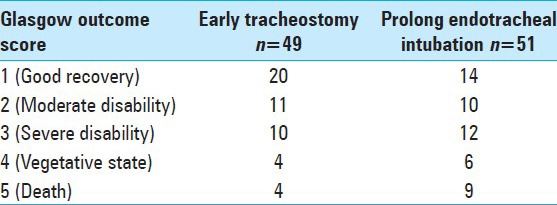
Table 3.
Cause of death
Out of 49 patients in ET group, 4 had an in-hospital mortality and 45 were followed after discharge. The average follow-up was 6 months. Tracheostomy decannulation was carried out after 2 months. No delayed complications were noted.
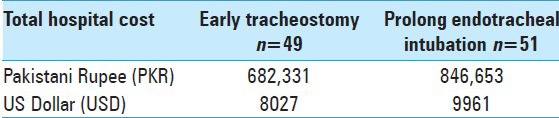
On comparison of the cost of stay, there was a considerable difference between the two groups. The average total inpatient cost of the ET group was USD $8027, which was significantly less than the EI group (USD $9961). The ICU stay of the patients in the ET group was significantly shorter (15.4% shorter than the EI group). The decrease in ICU bed cost accompanied with the reduction in rigorous clinical monitoring and laboratory investigations contributed to this [Table 4].
Table 4.
Total hospital cost
DISCUSSION
Preventing secondary injury, which might either delay the recovery of the healing portion of the injured brain or cause further deterioration, is the prime focus of the intense ICU support. After surviving the critical 48-h period of initial injury, most patients with severe head trauma are at a high risk of developing the morbidities and possibly mortality associated with a prolonged ICU stay.[5,6] High sedation is used in these patients to control agitation and an elevated intracranial pressure. An already depressed mental status secondary to injury combined with the depressant effect of the sedatives and various narcotics mandates airway patency be maintained via EI. However, for a comatose patient, the endotracheal tube is extremely noxious and to control the agitation, sedation is usually increased, leading to a further decline in mental status.[10] Thus intensive unit care after a head trauma is a profound clinical challenge, even with the current advancements in critical care.
EI not only provides better airway protection but also allows easy mechanical ventilation and endotracheal/pulmonary toilet.[12] Most patients, however, might not require the latter for a long time therefore tracheostomy becomes a viable alternative. It provides an early alternative for airway protection and decreases the need for prolonged mechanical ventilation support. Also, since most of these patients have suboptimal airway protective reflexes throughout the course of their recovery period, aspirations are common. Airway protection therefore becomes necessary, as enforced by studies in which reported patients who were extubated but did not undergo tracheostomy had a high frequency of reintubation due to poor control of aspiration.[7]
Due to pooling of the secretions above the endotracheal cuff in patients on translaryngeal ventilation, constant opening of vocal cords by the tube, along with a decreased conscious level with high sedation, the frequency of aspiration into the distal airway is high. This predisposes patients on ventilators to a greater risk of VAP and ARDS. The developing biofilm in the inner part of the tube often becomes colonized[15] and the frequent suctioning and ventilation allows contaminated secretions to disperse further into the lungs.[4] The removable inner cannula of the tracheostomy tube proves to be a vital asset in these circumstances. It can be removed and cleaned regularly, which prevents buildup of the biofilm. In addition to this, it also provides an excellent route for easy and efficient pulmonary toilet. With a secure airway patients can be ambulated early and along with frequent chest therapy an overall reduction in the risk of orthostatic and VAP can be observed.[14]
The decrease in dead space, better lung mechanics and function, less sedation and lesser breathing work explains the decrease in ventilation time as seen in our patients of the ET group in which the total ventilation days and ICU stay were considerably less.[7,15] It is also essential to take into consideration the financial benefit of this. As most of the patients in a country like Pakistan do not have health insurance, it is a massive financial constraint. Cutting down the length of ICU stay, which is the most expensive part of the treatment, reduces the load considerably. The decrease in the incidence of VAP also allows cutting the cost of broad spectrum antibiotics needed to treat these nosocomial infections. With the scarcity of intensive care facilities in Pakistan this allows a much more efficient utilization of these resources as well.
There are various factors when considering the timing of tracheostomy. Perhaps the most important ones are the risk of larynogotracheal injury and the duration of ventilation. As reported by a study, the risk of severe tracheal complications was considerably higher in patients who were intubated for >14 days.[11] We therefore assessed a need for ET before larynogotracheal injury becomes a point of concern.
It is a paradox that although tracheostomy is frequently recommended in head injury patients, there have been few studies conducted strictly on such a group. Rodriguez et al. reported a reduction in duration of mechanical ventilation, ICU, and hospital stay after ET.[13] But their study population included patients with diverse surgical problems instead of a homogenous cohort of head injury patients. In our study, hospital stay is more in tracheostomy group because of increased time needed by care providers to learn the different protocols of managing a patient with tracheostomy. It is important to teach them tracheostomy care, daily dressings, regular suctioning, feeding, and usage of speaking valves for communication. In one retrospective study on 101 patients who were admitted after blunt injuries, 32 had tracheostomy within the first 4 days and 69 underwent tracheostomy after 4 days. The authors found that the mean duration of ventilatory support was 6 days in early group versus 20 days in late tracheostomy group.[9] Both of these studies did not compare outcome and complications in prolonged intubation versus ET patients. There is a prospective study in which authors have randomized patients to ET (n = 31) and prolonged EI group (n = 31). They found that ET decreases the total days of ventilator but did not reduce either ICU stay or frequency of VAP.[1] The study did not look into the clinical outcome. In our study clinical outcome of patients was assessed on the basis of GOS to provide us a better understanding of pros and cons of ET.
CONCLUSION
In isolated severe head injury, ET decreases total days of ventilation and ICU stay. Tracheostomy is associated with a decrease in the incidence of VAP. ET should be considered in severe head injury patients requiring prolong ventilatory support.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2015/6/1/65/155757
Contributor Information
Usman Tariq Siddiqui, Email: usmantsiddiqui@hotmail.com.
Muhammad Zubair Tahir, Email: zubair.tahir@aku.edu.
Muhammad Shahzad Shamim, Email: shahzad.shamim@aku.edu.
Syed Ather Enam, Email: ather.enam@aku.edu.
REFERENCES
- 1.Bouderka MA, Fakhir B, Bouaggad A, Hmamouchi B, Hamoudi D, Harti A. Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma. 2004;57:251–4. doi: 10.1097/01.ta.0000087646.68382.9a. [DOI] [PubMed] [Google Scholar]
- 2.Colice GL, Stukel TA, Dain B. Laryngeal complications of prolonged intubation. Chest. 1989;96:877–84. doi: 10.1378/chest.96.4.877. [DOI] [PubMed] [Google Scholar]
- 3.Davis K, Jr, Campbell RS, Johannigman JA, Valente JF, Branson RD. Changes in respiratory mechanics after tracheostomy. Arch Surg. 1999;134:59–62. doi: 10.1001/archsurg.134.1.59. [DOI] [PubMed] [Google Scholar]
- 4.Feldman C, Kassel M, Cantrell J, Kaka S, Morar R, Goolam Mahomed A, et al. The presence and sequence of endotracheal tube colonization in patients undergoing mechanical ventilation. Eur Respir J. 1999;13:546–51. doi: 10.1183/09031936.99.13354699. [DOI] [PubMed] [Google Scholar]
- 5.Gurkin SA, Parikshak M, Kralovich KA, Horst HM, Agarwal V, Payne N. Indicators for tracheostomy in patients with traumatic brain injury. Am Surg. 2002;68:324–8. discussion 328-9. [PubMed] [Google Scholar]
- 6.Heffner JE, Miller KS, Sahn SA. Tracheostomy in the intensive care unit. Part 2: Complications. Chest. 1986;90:430–6. doi: 10.1378/chest.90.3.430. [DOI] [PubMed] [Google Scholar]
- 7.Koh WY, Lew TW, Chin NM, Wong MF. Tracheostomy in a neuro-intensive care setting: Indications and timing. Anaesth Intensive Care. 1997;25:365–8. doi: 10.1177/0310057X9702500407. [DOI] [PubMed] [Google Scholar]
- 8.Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med. 2000;342:1471–7. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]
- 9.Lesnik I, Rappaport W, Fulginiti J, Witzke D. The role of early tracheostomy in blunt, multiple organ trauma. Am Surg. 1992;58:346–9. [PubMed] [Google Scholar]
- 10.Major KM, Hui T, Wilson MT, Gaon MD, Shabot MM, Margulies DR. Objective indications for early tracheostomy after blunt head trauma. Am J Surg. 2003;186:615–9. doi: 10.1016/j.amjsurg.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 11.Nowak P, Cohn AM, Guidice MA. Airway complications in patients with closed-head injuries. Am J Otolaryngol. 1987;8:91–6. doi: 10.1016/s0196-0709(87)80030-3. [DOI] [PubMed] [Google Scholar]
- 12.Qureshi AI, Suarez JI, Parekh PD, Bhardwaj A. Prediction and timing of tracheostomy in patients with infratentorial lesions requiring mechanical ventilatory support. Crit Care Med. 2000;28:1383–7. doi: 10.1097/00003246-200005000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez JL, Steinberg SM, Luchetti FA, Gibbons KJ, Taheri PA, Flint LM. Early tracheostomy for primary airway management in the surgical critical care setting. Surgery. 1990;108:655–9. [PubMed] [Google Scholar]
- 14.Rumbak MJ. Pneumonia in patients who require prolonged mechanical ventilation. Microbes Infect. 2005;7:275–8. doi: 10.1016/j.micinf.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 15.Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med. 2004;32:1689–94. doi: 10.1097/01.ccm.0000134835.05161.b6. [DOI] [PubMed] [Google Scholar]
- 16.Whited RE. A prospective study of laryngotracheal sequelae in long-term intubation. Laryngoscope. 1984;94:367–77. doi: 10.1288/00005537-198403000-00014. [DOI] [PubMed] [Google Scholar]


