Abstract
Objective:
The objective was to assess the frequency of polypharmacy and potential complications among local seniors.
Methods:
A cross-sectional convenience sample of 59 adults aged above 65 years was interviewed at Cuyahoga county (U.S. state of Ohio) senior programs. Polypharmacy was defined as more than five prescribed medications. Primary outcomes were frequent missed doses, one or more duplicate drug/s, and equal or more than one contraindicated drug combinations.
Findings:
Among seniors with the mean age of 76.9 years (25.4% male), 40.6% used multiple pharmacies and 35.6% had polypharmacy. Of all seniors with polypharmacy, about 57% had contraindicated drug combinations. Polypharmacy was associated with duplication (P = 0.02), but not frequent missed doses (P = 0.20).
Conclusion:
As shown by this study, polypharmacy was associated with duplicated therapy and contraindicated drug combinations. Improved communications among seniors, physicians, and pharmacists is necessary to minimize adverse consequences of polypharmacy.
Keywords: Elderly, drug adherence, polypharmacy
INTRODUCTION
The use of multiple drugs, often termed polypharmacy is commonly defined as using from 5 to 10 prescription drugs.[1,2,3] This polypharmacy is sometimes necessary, but may be associated with an increased risk of adverse outcomes.[2] The U.S. Center for Medicare and Medicaid Services estimated the annual costs of polypharmacy at over 50 billion dollars.[1]
Polypharmacy is especially common in elderly patients. Although elderly patients comprise <13% of the U.S. population, they almost 33% of prescription medications annually.[1] Because individuals are living longer with chronic diseases, elderly patients also tend to have more complicated chronic conditions, may respond differently to medication therapy or experience more severe adverse reactions due to differences in pharmacokinetic and pharmacodynamic characteristics, compared with younger patients. They may also visit multiple prescribers and use multiple pharmacies that will lead to increased risk of medication-related problems through poorly coordinated or duplicated care.[3,4]
The potential for medication nonadherence rises with increased numbers of prescribed medications.[4,5,6] Nonadherence to prescribed medication is estimated at 79%, 69%, 65%, and 51%, for once, twice, three, and four times daily administration, respectively.[4,5,6] It can be associated with subsequent reduced effectiveness.[4,5] Medication nonadherence could be linked to 125,000 deaths in America annually and results in approximately 177 billion dollars increased costs of health care.[5]
Based on the Ohio Medicaid data report, the rate of psychotropic polypharmacy increased significantly since 2002 in younger adults, however, there are few data available for a general elderly population.[7] Most previous studies focused on cardiac patients, hospital-based or posthospital patients.[8,9]
The objective of this study was to evaluate the frequency of polypharmacy and to assess the relationship between polypharmacy and potential adverse outcomes within a sample of elderly population served by the Cuyahoga County Board of Health (CCBH), Cleveland, Ohio, USA. These data were needed to inform a set of recommendations for the CCBH, to improve prescribing outcomes for Cuyahoga county senior residents.
METHODS
This cross-sectional study took place in three senior community centers in Cleveland, Ohio that are served by CCBH. As Ohio's largest health district by population, servicing a major metropolitan area since 1919, the Board of Health provides a broad range of quality driven public health services. A convenience sample of residents participating in CCBH senior citizens programs during the time period of October 2010 to January 2011 was recruited for participation in this study. Inclusion criteria consisted of subjects aged more than 65 years who can understand the English language. Seniors were encouraged to bring medication lists and pill containers for medication management visits with the pharmacist.
The study questionnaire included demographics: Age, gender, self-identified race and ethnicity, and level of education. Subjects were asked to list their health conditions, and all of their current prescription and over-the-counter (OTC) medications, their prescribers, doses, administration times, and an estimate of whether they “frequently” (defined as they chose) missed medication doses and their pharmacy.
The exposure of interest was polypharmacy, defined as self-reported concurrent use of at least five different prescribed medications. The primary outcomes were: Self-reported missed doses of prescribed drugs, at least one duplicate drug therapy, at least one contraindicated drug combinations, as defined by the Drug Facts and Comparisons,[10] and multiple pharmacies to obtain prescribed medications.
Stata SE 10.1 for Windows (StataCorp LP, College Station, TX, USA) was used for analysis. Fisher's exact test was used to compare frequencies between groups. Multivariable logistic regression was used to adjust for possible confounders in the relationship between contraindicated drug combinations and drug duplication and polypharmacy. Covariates were retained in the model if they had an independent association with polypharmacy and the outcome of interest and if removing them from the model would change the point estimate by ≥10%. This study was approved by the Case Western Reserve University Institutional Review Board.
RESULTS
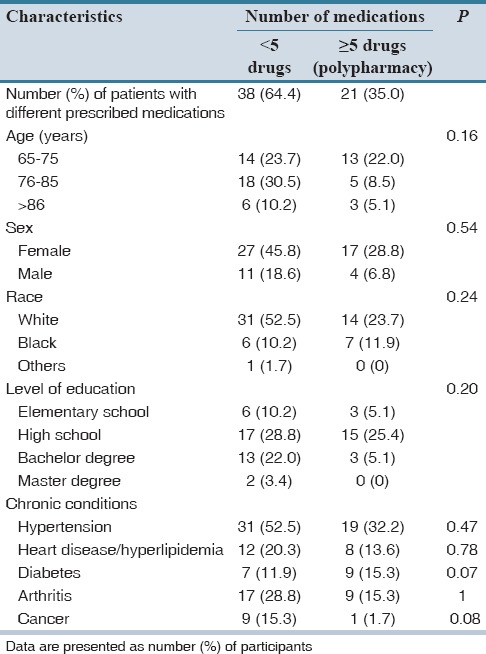
A total of 59 seniors enrolled from three different senior community centers in CCBH. Age range was 65–90 with a mean of 76.9 years. Of these, 45 (76.3%) were self-identified white, 13 (22.0%) were black and 1 (1.7%) was Asian. Of the 59 seniors, 21 (35.6%) were prescribed more than five medications [Table 1]. Polypharmacy was not associated with age (P = 0.16), sex (P = 0.54), level of education (P = 0.20) or race (P = 0.24).
Table 1.
Seniors’ use of prescribed medication (n=59)
24 (40.6%) of seniors used multiple pharmacies. 49 seniors (83.0%) were using OTC medications, 21 of these had duplicate use of OTC medications for the same indication. The mean number of prescription medications taken was 5.1 and the mean number of OTC drugs taken was 2.0. There was no association between duplicate use of OTC medications and the presence of polypharmacy of prescription medications (P = 0.94) or the use of multiple pharmacies (P = 0.51).
Thirteen seniors (22.0%) admitted frequently missed doses, 11 (18.6%) had duplicated therapy, and 12 (20.3%) had contraindicated drug combinations. 12 seniors with polypharmacy and none without polypharmacy had contraindicated prescription drug combinations (P < 0.001). Duplication of therapy was associated with polypharmacy when models adjusted for race and education (odds ratio: 10.7, 95% confidence interval: 1.5–76.7, P = 0.02). There were no significant associations between polypharmacy and any other specific chronic condition, including hypertension, heart disease/hyperlipidemia, diabetes, arthritis and cancer.
15 (25.4%) seniors carried a medication list for the study interview. Seniors’ level of education was associated with having this list (P = 0.01), however not the presence of polypharmacy (P = 0.30), inappropriate drug combination (P = 0.48) or self-reported frequent missed doses (P = 0.34).
DISCUSSION
Medication adherence and drug safety continue to be important problems, especially for seniors. This study found that, polypharmacy was common in over one-third of our subjects; previous studies found a somewhat lower prevalence of 20–30%.[2,7] Polypharmacy was associated with duplicate prescribed drugs and contraindicated prescribed drug combinations. This can potentially increase the risk of adverse drug reactions.[2,3] The use of multiple medications, and their associated risks, might be medically indicated for patients with numerous and/or complex co-morbid conditions; this will be increasingly prevalent with the expected demographic trend toward a progressively elderly U.S. population.[11,12] In this study, only prescription medications were considered in the definition of polypharmacy. Some earlier studies considered both prescription and nonprescription-OTC-medications in their polypharmacy definitions.[12]
This study found no association between polypharmacy and age, sex, educational level, or number of comorbidities. Previous studies reported an association between polypharmacy and sex,[3] level of education, and/or a history of diabetes or hypertension.[12] These differences could be the result of differences in the characteristics of the populations studied and/or sample size.
Medication nonadherence increases the risk of suboptimal drug treatment and its further consequences. Other studies also reported that polypharmacy was associated with poor adherence.[13] The scope of this study precluded access to seniors’ pharmacy records. Thus this study was not able to fully address medication adherence.
Many seniors used multiple pharmacies. Switching between pharmacies may exacerbate communication among patients, pharmacists, and physicians, increase the risk of inappropriate medication use and potential adverse consequences. Utilization of mail order pharmacies is increasing rapidly in the U.S. Medicare part D, which covers most seniors’ medications in America, promotes the use of this service to provide seniors with maintenance medications for 90 days. Barriers to pharmacy consultation and decreased direct personal interaction with consultant pharmacists may potentially increase the risk of inappropriate medication use.[14] The promotion of mail-order pharmacy services may be counter-productive if it interferes with communication. These issues need further careful study.
Limitations of this study include that results may not be generalizable to seniors who chose not to participate and attending different centers, or to seniors in different counties. Cuyahoga county seniors have similar rates of chronic health conditions and health care utilization as those of Ohio and the U.S. as a whole. Conclusions regarding this study are also limited by its relatively small sample size. The paucity of previous data available for the general elderly population in the community heightens its potential value to inform future studies, which can include more subjects from more diverse environments, examine the effect of mail-order prescriptions, and include cost-benefit analysis of interventions to minimize polypharmacy.
Further patient education on the disease, treatment goals, medication risks and benefits, and interventions to improve drug coordinated communication may help improve drug adherence and minimize polypharmacy. Based on the findings of this project, authors developed recommendations for the CCBH to help further improve seniors’ medication use and associated health outcomes, designed to minimize unnecessary polypharmacy, improve prescribing, and promote coordination and communication between County prescribers, pharmacists, and elderly residents.
In conclusion, this study found that polypharmacy was frequent among Cuyahoga county seniors and associated with duplicated therapy and inappropriate drug combinations. These results can potentially inform future research and policy recommendations to help improve seniors’ medication use at the societal level. As medical care becomes increasingly complex in our aging population, it is particularly important to improve cooperation, coordination, and communication between patients, physicians, and pharmacists. These efforts can complement current national endeavors toward a more patient-centered approach to health care and promoting the concept of the medical home.
AUTHORS’ CONTRIBUTION
Dr. Golchin designed the intervention, evaluation and data collection, collected the data, planned and carried out the analysis, drafted the initial manuscript, reviewed and revised the manuscript, and approved the final manuscript submitted. Dr. Frank advised and assisted in study design and analysis, reviewed and contributed to the analysis, reviewed and revised the manuscript and approved the final manuscript submitted. Ms. Isham assisted with study design, reviewed the analysis, reviewed and revised the manuscript and approved the final manuscript as submitted. Ms. Vince assisted with study design, reviewed the analysis, reviewed and revised the manuscript and approved the final manuscript as submitted. Dr. Meropol advised and assisted with design of the study, intervention, and the analysis, assisted with the analysis, reviewed and revised the manuscript and approved the final manuscript submitted
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Fillit HM, Futterman R, Orland BI, Chim T, Susnow L, Picariello GP, et al. Polypharmacy management in medicare managed care: Changes in prescribing by primary care physicians resulting from a program promoting medication reviews. Am J Manag Care. 1999;5:587–94. [PubMed] [Google Scholar]
- 2.Bushardt RL, Massey EB, Simpson TW, Ariail JC, Simpson KN. Polypharmacy: Misleading, but manageable. Clin Interv Aging. 2008;3:383–9. doi: 10.2147/cia.s2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linjakumpu T, Hartikainen S, Klaukka T, Veijola J, Kivelä SL, Isoaho R. Use of medication and polypharmacy are increasing among the elderly. J Clin Epidemiol. 2002;55:809–81. doi: 10.1016/s0895-4356(02)00411-0. [DOI] [PubMed] [Google Scholar]
- 4.Strom BL, Kimmel SE. In: Textbook of Pharmacoepidemiology. 4th ed. Ch. 4. West Sussex, England: Wiley; 2007. Basic principles of clinical pharmacology related to pharmacoepidemiology studies; pp. 35–55. [Google Scholar]
- 5.Veehof L, Stewart R, Haaijer-Ruskamp F, Jong BM. The development of polypharmacy. A longitudinal study. Fam Pract. 2000;17:261–7. doi: 10.1093/fampra/17.3.261. [DOI] [PubMed] [Google Scholar]
- 6.Callahan CM, Weiner M, Counsell SR. Defining the domain of geriatric medicine in an urban public health system affiliated with an academic medical center. J Am Geriatr Soc. 2008;56:1802–6. doi: 10.1111/j.1532-5415.2008.01941.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fontanella CA, Warner LA, Phillips GS, Bridge JA, Campo JV. Trends in psychotropic polypharmacy among youths enrolled in Ohio medicaid, 2002-2008. Psychiatr Serv. 2014;65:1332–40. doi: 10.1176/appi.ps.201300410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morandi A, Vasilevskis E, Pandharipande PP, Girard TD, Solberg LM, Neal EB, et al. Inappropriate medication prescriptions in elderly adults surviving an intensive care unit hospitalization. J Am Geriatr Soc. 2013;61:1128–34. doi: 10.1111/jgs.12329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruwald MH, Hansen ML, Lamberts M, Hansen CM, Numé AK, Vinther M, et al. Comparison of incidence, predictors, and the impact of co-morbidity and polypharmacy on the risk of recurrent syncope in patients <85 versus = 85 years of age. Am J Cardiol. 2013;112:1610–5. doi: 10.1016/j.amjcard.2013.07.041. [DOI] [PubMed] [Google Scholar]
- 10.St. Loise, Missori, USA: Published by Facts and Comparisons, Hardbound, Lippincott; 2010. Facts and Comparisons. Drug Facts and Comparisons. [Google Scholar]
- 11.Hilmer SN, Shenfield GM, Le Couteur DG. Clinical implications of changes in hepatic drug metabolism in older people. Ther Clin Risk Manag. 2005;1:151–6. doi: 10.2147/tcrm.1.2.151.62914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moen J, Antonov K, Larsson CA, Lindblad U, Nilsson JL, Råstam L, et al. Factors associated with multiple medication use in different age groups. Ann Pharmacother. 2009;43:1978–85. doi: 10.1345/aph.1M354. [DOI] [PubMed] [Google Scholar]
- 13.Esserman DA, Moore CG, Roth MT. Analysis of binary adherence data in the setting of polypharmacy: A comparison of different approaches. Stat Biopharm Res. 2009;1:201–212. doi: 10.1198/sbr.2009.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Medicare Part D Manual. 2013. [Last visit on 2014 Feb 17, Last accessed on 2014 Apr 24]. Available from: http://www.healthplus.org/uploadedFiles/PDFs/Medicare/PDBMChap6FormularyReqrmts_03.09.07.pdf . Available from: http://www.Dartmouthatlas.org .


