Abstract
Objective:
Ketamine administration is known to induce hemodynamic pressor response and psychomimetic effects which could be attenuated by appropriate premedication. The present study was designed to evaluate the effect of midazolam on hemodynamic stability and postoperative emergence phenomenon following ketamine anesthesia.
Methods:
This was a prospective observational study including 30 adult patients with American Society of Anesthesiologists physical grades I and II scheduled for elective short surgeries under ketamine anesthesia. Patients were premedicated with midazolam (0.02 mg/kg intravenously) before the ketamine induction (1 mg/kg intravenously). Demographic data and hemodynamic variables were observed during the perioperative period. Pain score by visual analog scale score and psychomimetic effects were recorded postoperatively.
Findings:
The mean ± standard deviation of heart rate, systolic blood pressure, diastolic blood pressure, and respiratory rate were decreased postoperatively (85.3 ± 11.4, 120.7 ± 8.2, 79.2 ± 5.5, 13.5 ± 1.8, respectively) compared to intraoperative period (88.53 ± 14.1, 123.83 ± 13.8, 83 ± 9.1, 14.13 ± 2.0, respectively). There was statistically significant decrease in systolic (P = 0.03) and diastolic (P = 0.002) blood pressure, but not with heart rate and respiratory rate. Eighty percent of patients had no pain at ½ hour and 1 hour, while this increased to 90% at 2 hours postoperatively. Mild emergence delirium was noted in 13.3% and 16.7% at ½ hour and 1 hour, respectively, which decreased to 13.3% at 2 hours. Dreams were noticed in 20%, 27% and 10% of patients at ½ hour, 1 and 2 hours after surgery, respectively.
Conclusion:
Midazolam premedication in ketamine anesthesia effectively attenuated the hemodynamic pressor response and postoperative emergence phenomenon. Hence, the combination of midazolam with ketamine can be safely used for short surgical painful procedures in adults.
Keywords: Emergence phenomenon, Ketamine anesthesia, Midazolam, premedication
INTRODUCTION
Ketamine is a rapidly acting dissociative anesthetic agent commonly used for short surgical procedures which has the properties of rapid induction, good analgesia, and amnesia with a short recovery period. But it has the limitations of intraoperative cardiovascular stimulation, muscular hypertonia and recovery is often associated with postoperative psychomimetic effects (emergence delirium, unpleasant dreams, and hallucinations).[1] The incidence ranges from 5% to 30% which is mostly dose related.[2] Hence, there is an ever-increasing quest to overcome these adverse effects with appropriate medication. Drugs including opiates, neuroleptics, benzodiazepines, physostigmine, and alpha-2 adrenoceptor agonists have been used with varying success to prevent these emergence reactions associated with ketamine administration.[3]
Among the above premedication drugs, concomitant use of benzodiazepines has been proven to be satisfactory in alleviating the undesirable effects during the perioperative period. But every benzodiazepine has its own disadvantage: More prolonged impairment of mental activity and amnesia with flunitrazepam; slower onset of action and delayed recovery with lorazepam; higher incidence of unpleasant dreams with diazepam.[3] Midazolam has potent anxiolytic effect with amnesia, sedation, skeletal muscle relaxant activity, and good hemodynamic stability with lack of significant side effects in doses <0.5 mg/kg.[4] Midazolam when combined with intravenous ketamine found to be safe and effective for relief of anxiety and sedation for diagnostic and therapeutic procedures. Literature suggests that compared with a combination of ketamine with other benzodiazepines (diazepam, lorazepam), midazolam premedication results in fewer emergence reactions.[5] Though studies are available with other premedication drugs used for ketamine anesthesia, limited data are available regarding the usefulness of the low dose midazolam combined with low-dose ketamine in preventing ketamine-induced hemodynamic instability and postanesthetic emergence phenomenon. In view of these attributes, the present study was designed to evaluate the effect of low dose intravenous midazolam as premedication in attenuating ketamine-induced hemodynamic instability and postanesthetic emergence delirium.
METHODS
This study was an open-label, prospective, observational study conducted at Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India, by the Department of Pharmacology in collaboration with Department of Anesthesia between March and August 2014. Thirty patients posted for elective short surgeries from Departments of Obstetrics and Gynaecology, general surgery and Orthopaedics receiving ketamine with midazolam as an anesthetic agent were enrolled in our study. Institutional Ethical Committee approval (IEC No: SMVMCH/IEC/DAO/239/2014) and informed written consent from all the patients were obtained before the commencement of the study.
Patients aged between 18 and 45 years of either sex with the American society of Anesthesiologists physical grades I and II were included in the study. The duration of surgery was equal to or <30 min in all the cases. Patients with a previous history of systemic illness, organ dysfunction, raised intraocular and intracranial pressure, known drug hypersensitivity and difficult airway were excluded from the study. Complete preanesthetic assessment with history, general and systemic examination, and review of biochemical investigations by the anesthetist were done prior to enrollment in the study. Demographic and clinical data such as age, gender, weight, and the surgical procedure (type and duration) were collected preoperatively.
Patients were premedicated with intravenous metoclopramide (10 mg), glycopyrrolate (0.2 mg) followed by intravenous midazolam at a dose of 0.02 mg/kg[6] which was given slowly over a period of 10 min. After preoxygenation with 100% oxygen, anesthesia was induced with intravenous ketamine (1% solution) at a dose of 1 mg/kg slowly over 30 s.[7] Anesthetic and surgical techniques were standardized for all the patients. No additional dose of ketamine or midazolam was required for any of the patients throughout the study. Baseline heart rate, blood pressure, and respiratory rate were recorded pre-, intra-, and post-operatively. All patients were on continuous monitoring of electrocardiography and oxygen saturation throughout the study period. They were also observed closely and assessed for presence or absence of psychomimetic effects during ½ h, 1 h, and 2 h in the postoperative period. The various postoperative events assessed were as following: Modified visual analog scale (VAS) for pain,[8] emergence delirium (mild or severe), dreams, nausea, vomiting, and salivation.
Modified VAS is a nonverbal pain assessment method for adults which include five observations with a subjective scoring from 0 to 10. Patients with purposeless and hallucinatory movements were termed as mild emergence delirium. Those with screaming, violent involuntary movements were classed as severe emergence delirium.[3] A special case record form was used to collect the above data from the patients.
Sample size was calculated using mean and standard deviation (SD) for diastolic blood pressure (value 78 ± 13)[9] by the formula 4× (σ)2/(d)2, which was determined to be 27 patients. Considering the nonresponse rate of 10%, the derived sample size was set at 30. Data were analyzed using Statistical Package for the Social Sciences (SPSS) software (version 11.5, SPSS Inc., Chicago, IL). Hemodynamic parameters were analyzed using one-way analysis of variances and expressed as mean and SD. Postoperative events were analyzed using descriptive statistics and Chi-square test to test the level of significance. P < 0.05 was considered statistically significant.
RESULTS
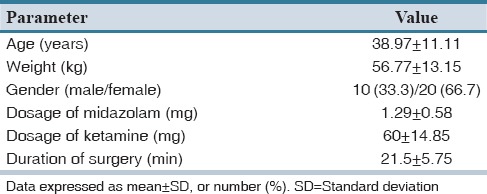
A total of 30 patients were enrolled in our study among which female patients were predominant (66.7%). Demographic data, mean dose of the drugs used, and surgery duration are shown in Table 1.
Table 1.
Demographic characteristics of the study patients (n=30)
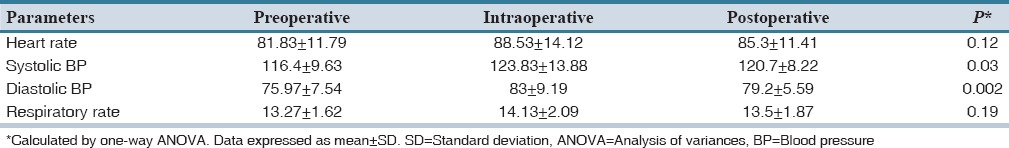
The hemodynamic parameters namely heart rate, systolic and diastolic blood pressure, and respiratory rate were monitored during the perioperative period (pre-, intra-, and post-operative). The mean heart rate observed during the intraoperative period was 88.53 ± 14.12 which decreased to 85.3 ± 11.41 postoperatively which was not statistically significant (P = 0.12). Moreover, there was no significant change in respiratory rate during this period. However, significant change in the systolic (P = 0.03) and diastolic (P = 0.002) blood pressure was observed postoperatively when compared to intraoperative period as given in Table 2. Postoperative recovery time was not recorded, but all the patients were monitored for respiratory depression, hypoxia, apnea, and nystagmus in the postoperative period. None of the patients had the above clinical findings except for nystagmus in one patient.
Table 2.
Effect of midazolam premedication on various hemodynamic parameters during the perioperative period
The preoperative administration of midazolam with ketamine virtually abolished pain in majority of the cases at ½ h (80%), 1 h (80%), and 2 h (90%) after surgery as assessed by modified VAS.[8] Mild pain was experienced in 16.7% of patients at ½ h and 1 h which was reduced to 10% at 2 h period as depicted in Table 3. Satisfactory control over emergence delirium was noticed at ½ h (83.3%), 1 h (80%) and 2 h (86.7%) postoperatively. Mild delirium was observed in 13.3% of patients at ½ h and 2 h, 16.7% at 1 h period whereas severe delirium was observed with only one patient (3.3%) at ½ and 1 h after surgery [Table 3]. Though the percentage of delirium seems to be higher in the orthopedic surgeries (40%) than compared to other departments (data not shown), hence, in order to address the effect of confounders, the stratified analysis done showed nonsignificant (P = 0.4895).
Table 3.
Assessment of postoperative pain (evaluated by modified VAS), emergence delirium, and other undesirable effects among the study subjects (n=30)
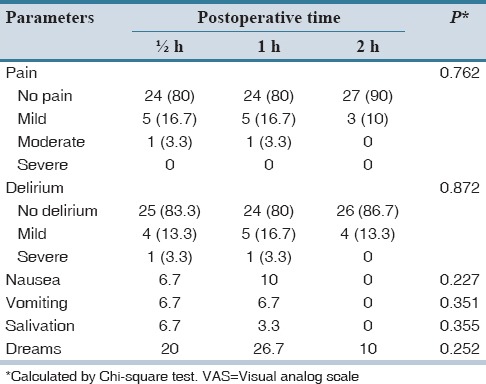
Postoperative adverse effects like dreams were not seen with 90% of the patients at 2 h, 80% at ½ h and 73.3% at 1 h period in patients who received ketamine with midazolam. All the patients were completely devoid of subjective symptoms such as nausea, vomiting, and salivation at 2 h postoperatively as shown in Table 3. No statistical significant difference was observed within the time period (Chi-square test). All the patients universally accepted the midazolam premedication with ketamine anesthesia.
DISCUSSION
Ketamine-induced sedation and analgesia differ from that of other agents as it causes dissociative anesthesia being preferred for the majority of short surgeries. This potent analgesic, anesthetic effect has been suggested to be mediated by different mechanism. It has a high margin of safety, no irritation of the injected veins with main disadvantage of increasing blood pressure and precipitation of psychomimetic emergence phenomenon.[10,11] This limitation was reported to be due to its noncompetitive binding and modification of phencyclidine site of N-methyl-D-aspartate receptors in the thalamus and limbic areas.[12] Various other neurochemicals such as opiates, dopamine, and acetylcholine have also been implicated in its action. In addition, it also inhibits the reuptake of catecholamines leading to mild to moderate increase in hemodynamic parameters.[13] Hence, several adjuncts have been used as preanesthetic medication to attenuate this pressor response and undesirable emergence phenomenon.
An ideal premedication should be easily administered, acceptable, act rapidly, do not prolong emergence from anesthesia and have fewer side effects. In our study midazolam, a benzodiazepine which is a rapid onset, short-acting, and water soluble drug having anxiolytic and amnestic effect thus making it as a good preanesthetic agent.[14] Hence in our study, single dose (0.02 mg/kg) of midazolam with ketamine had shown desirable effect on hemodynamic stability and in mitigating postoperative emergence reactions. Present study showed that concurrent medication of midazolam with ketamine had abolished the rise in respiratory rate and heart rate. In addition, statistical significant reduction of systolic (P = 0.03) as well as diastolic (P = 0.002) blood pressure was observed postoperatively which can be related to its ability to abolish the pressor response of ketamine. Similar effects were observed with study done by Gupta K et al.[6] who compared the effect of dexmedetomidine with midazolam in ketamine anesthesia. Our study results on hemodynamic parameters were similar to yet another study done by Kolhe et al.[15] However, in his study, midazolam was compared with diazepam premedication in orthopedic surgeries. Ketamine-induced cardiostimulatory effects may be blunted with concurrent administration of midazolam due to its known action on decreasing the peripheral vascular resistance thereby reducing the raised blood pressure.[16]
In our study, we found midazolam premedication also had considerably abolished the pain in the majority of cases (80–90%) as assessed by modified VAS. 16.7% of patients experienced only mild pain at ½ h and 1 h which was later reduced to 10% at 2 h period; Only one patient (3.3%) reported to have moderate pain at ½ h and 1 h postoperatively. Our study goes in accordance with that of another study conducted by Gupta R et al.[17] who compared the pain scores among two groups of patients with and without midazolam in ketamine anesthesia. One study done by Gündüz et al. reported that there was no statistically significant difference between two groups of adult burns patients (intravenous ketamine alone and ketamine with midazolam coadministration) when pain was assessed by VAS self-rating method.[18] The present study appeared encouraging as midazolam premedication virtually reduced the incidence of emergence delirium which is especially appreciable 2 h after surgery. Occurrence of delirium in our study was comparable with other studies.[3,15] But complete abolition of delirium was also observed by Lohit et al. who used the midazolam with ketamine in all periods of observation postoperatively.[19] Only two patients had nausea, vomiting, and salivation at ½ h after procedure, and neither of them had any aspiration or other complications. This may be explained by the preservation of protective airway reflexes by ketamine administration. Moreover, we did not observe respiratory depression, hypoxia or apnea in any of the patients in our study which may be due to single, low dose (0.02 mg/kg) usage of midazolam along with ketamine.[20] Study done by Gündüz et al. demonstrated that the occurrence of postoperative events (nausea, vomiting) were similar to our study at ½ h and 1 h period (<10% of the patients). Moreover, our study also recorded that there were no untoward effects observed at 2 h postoperative period. However, Lohit et al. study showed that there were no adverse events noticed during the entire postoperative period in midazolam premedicated patients than compared to ketamine only treated group.[19]
In the present study, only six patients (20%) at ½ h, eight patients (26.7%) at 1 h, and three patients (10%) at 2 h experienced dreams postoperatively which were also not distressing. The frequency of dreams was similar to another study done by Chudnofsky et al. in his procedural sedation and analgesia in adult emergency department patients.[9] Patient tolerance for the combination treatment was satisfactory except in one patient who experienced a mild nystagmus which completely recovered after 2 h.
The limitation of our present study was the lack of a control group with a small population. However, the effectiveness of midazolam as a premedicant in reducing the emergence reactions has been well-documented as per our study. However, the study should be done using a larger number of population. From the above observation, administration of intravenous ketamine at a dose of 1 mg/kg had significant effect on cardiovascular stability and alleviated the occurrence of postoperative events when combined with intravenous midazolam at a dose of 0.02 mg/kg which can be recommended for short surgical procedures.
It was concluded that midazolam premedication with ketamine had effectively attenuated the hemodynamic pressor response and postanesthetic emergence phenomenon. Hence, we suggest that the combination of midazolam and ketamine at low doses can be safely used for short surgical painful procedures in adults.
AUTHORS’ CONTRIBUTION
DKP and MA : Study Design and Manuscript writing. NS: Manuscript editing and analysis. DKP and SPL: Data collection. MA and MAR : Expert review.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sawhney S, Agarwal RP. Combination of low dose ketamine and pentazocine – A clinical experience. Indian J Anaesth. 2003;47:439–42. [Google Scholar]
- 2.White PF, Ham J, Way WL, Trevor AJ. Pharmacology of ketamine isomers in surgical patients. Anesthesiology. 1980;52:231–9. doi: 10.1097/00000542-198003000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Somashekara SC, Govindadas D, Devashankaraiah G, Mahato R, Deepalaxmi S, Srinivas V, et al. Midazolam premedication in attenuating ketamine psychic sequelae. J Basic Clin Pharm. 2010;1:209–13. [PMC free article] [PubMed] [Google Scholar]
- 4.Kain ZN, Mayes LC, Bell C, Weisman S, Hofstadter MB, Rimar S. Premedication in the United States: A status report. Anesth Analg. 1997;84:427–32. doi: 10.1097/00000539-199702000-00035. [DOI] [PubMed] [Google Scholar]
- 5.Deng XM, Xiao WJ, Luo MP, Tang GZ, Xu KL. The use of midazolam and small-dose ketamine for sedation and analgesia during local anesthesia. Anesth Analg. 2001;93:1174–7. doi: 10.1097/00000539-200111000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Gupta K, Gupta A, Gupta PK, Rastogi B, Agarwal S, Lakhanpal M. Dexmedetomidine premedication in relevance to ketamine anesthesia: A prospective study. Anesth Essays Res. 2011;5:87–91. doi: 10.4103/0259-1162.84193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tobias JD. Dexmedetomidine and ketamine: An effective alternative for procedural sedation? Pediatr Crit Care Med. 2012;13:423–7. doi: 10.1097/PCC.0b013e318238b81c. [DOI] [PubMed] [Google Scholar]
- 8.Warden V, Hurley AC, Volicer L. Development and psychometric evaluation of the Pain Assessment in Advanced Dementia (PAINAD) scale. J Am Med Dir Assoc. 2003;4:9–15. doi: 10.1097/01.JAM.0000043422.31640.F7. [DOI] [PubMed] [Google Scholar]
- 9.Chudnofsky CR, Weber JE, Stoyanoff PJ, Colone PD, Wilkerson MD, Hallinen DL, et al. A combination of midazolam and ketamine for procedural sedation and analgesia in adult emergency department patients. Acad Emerg Med. 2000;7:228–35. doi: 10.1111/j.1553-2712.2000.tb01064.x. [DOI] [PubMed] [Google Scholar]
- 10.Kurdi MS, Theerth KA, Deva RS. Ketamine: Current applications in anesthesia, pain, and critical care. Anesth Essays Res. 2014;8:283–90. doi: 10.4103/0259-1162.143110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mion G, Villevieille T. Ketamine pharmacology: An update (pharmacodynamics and molecular aspects, recent findings) CNS Neurosci Ther. 2013;19:370–80. doi: 10.1111/cns.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orser BA, Pennefather PS, MacDonald JF. Multiple mechanisms of ketamine blockade of N-methyl-D-aspartate receptors. Anesthesiology. 1997;86:903–17. doi: 10.1097/00000542-199704000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Levänen J, Mäkelä ML, Scheinin H. Dexmedetomidine premedication attenuates ketamine-induced cardiostimulatory effects and postanesthetic delirium. Anesthesiology. 1995;82:1117–25. doi: 10.1097/00000542-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Sener S, Eken C, Schultz CH, Serinken M, Ozsarac M. Ketamine with and without midazolam for emergency department sedation in adults: A randomized controlled trial. Ann Emerg Med. 2011;57:109–14.e2. doi: 10.1016/j.annemergmed.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Kolhe EP, Dhumal PR, Kurhekar VA. Comparative study of midazolam and diazepam to supplement ketamine as total intravenous anaesthesia in short orthopedic procedures. Int J Pharm Biomed Res. 2013;4:15–20. [Google Scholar]
- 16.Mihic JS, Harris RA. Hypnotics and sedatives. In: Brunton LL, Chabner BA, Knollman BC, editors. Goodman and Gilman's Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill; 2011. pp. 457–80. [Google Scholar]
- 17.Gupta R, Sharma K, Dhiman UK. Effect of a combination of oral midazolam and low-dose ketamine on anxiety, pain, swelling, and comfort during and after surgical extractions of mandibular third molars. Indian J Dent Res. 2012;23:295–6. doi: 10.4103/0970-9290.100460. [DOI] [PubMed] [Google Scholar]
- 18.Gündüz M, Sakalli S, Günes Y, Kesiktas E, Ozcengiz D, Isik G. Comparison of effects of ketamine, ketamine-dexmedetomidine and ketamine-midazolam on dressing changes of burn patients. J Anaesthesiol Clin Pharmacol. 2011;27:220–4. doi: 10.4103/0970-9185.81823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lohit K, Srinivas V, Kulkarni C, Shaheen A clinical evaluation of the effects of administration of midazolam on ketamine-induced emergence phenomenon. J Clin Diagn Res. 2011;5:320–3. [Google Scholar]
- 20.Ramoska EA, Linkenheimer R, Glasgow C. Midazolam use in the emergency department. J Emerg Med. 1991;9:247–51. doi: 10.1016/0736-4679(91)90421-b. [DOI] [PubMed] [Google Scholar]


