Abstract
Background
Studies indicate that women victims of intimate partner violence are at increased risk for poor mental health. This research disentangled the effect of partner violence on new-onset depression and psychosis spectrum symptoms from effects of child maltreatment and other confounding factors, including substance abuse and antisocial personality.
Methods
Participants were 1,052 mothers involved in the Environmental Risk (E-Risk) Longitudinal Twin Study, a nationally representative cohort of families followed prospectively. To test the directionality of associations between partner violence and depression, only women without a history of depression at the beginning of the study were considered (n = 978). Partner violence and mental health were assessed during face-to-face interviews with women across three time points.
Results
Four of 10 women reported being the victim of violence from their partner in a 10-year period. They represent 33% of our cohort and they account for 51% of new-onset depression. These women had a twofold increase in their risk of suffering from new-onset depression once the effect of childhood maltreatment, socioeconomic deprivation, antisocial personality, and young motherhood were controlled. Women who were abused both in childhood and adulthood were four to seven times more likely to suffer from depression than never-abused women. We observed similar associations with psychosis spectrum symptoms.
Conclusions
Women victims of partner violence account for more than their share of depression. Findings strengthen existing evidence that partner violence independently contributes to women’s poor mental health. Psychological difficulties among a considerable number of women could be reduced by stopping partner violence.
Keywords: depression, partner violence, interpersonal violence, victimization, women, longitudinal study
Violence experienced in the context of an intimate relationship (hereafter partner violence) is one of the most prevalent types of violence directed against women; in the United States, one in three women has reported rape, physical violence, or stalking by a current or former boyfriend, partner, or spouse in her lifetime.[1] The economic burden is estimated at $4 billion yearly just in direct medical costs.[2] Partner violence is a public health concern because the consequences on mental health persist after the violence has ceased and the acute physical injuries have healed. Depression, posttraumatic stress disorder (PTSD) and anxiety are, on average, two to four times more prevalent in victims of partner violence than in the general population.[3, 4] However, whether partner violence is a causal factor associated with women’s mental health problems remains unclear;[5] only a few studies have disentangled the effect of partner violence from other forms of victimization, including childhood abuse, and other risk factors,[6, 7] and controlled for mental illnesses prior to experiencing partner violence.[5] A closer examination of the magnitude and directionality of the association between partner violence and women’s mental health disorders, while controlling for known correlates, would strengthen the empirical basis of this problem and the clinical relevance for mental health services.
The aim of this study was to provide further support to the association between partner violence and women’s poor mental health using data from a population-based sample followed prospectively. First, we tested the association focusing on women who initially reported no history of depression. The directionality of the association between partner violence and women’s mental health problems has been more often assumed from cross-sectional studies rather than being empirically tested with longitudinal designs.[5, 8–10] Many women involved in abusive relationships have mental health conditions before becoming a victim.[11] By excluding these women, longitudinal studies can rule out the possibility that the association between partner violence and mental health problems is solely attributable to the risk of depressed women becoming the victim of a violent partner.
Second, we tested for the association between partner violence and new-onset depression controlling for the confounding effect of a history of childhood maltreatment. People who have been maltreated in childhood are at increased risk of revictimization and partner violence.[12, 13] Given the well-known association between childhood maltreatment and later poor mental health,[14] controlling for prior abuse is required to estimate the magnitude of the association between partner violence and depression, net of the effect of childhood violence.[6, 7] Third, we controlled for a number of known correlates of partner violence to estimate the independent contribution of partner violence to depression. Such a stringent level of control is required, although rarely used. These omissions could bias the magnitude of the association between partner violence and women’s poor mental health because victims of partner violence are disproportionally represented in groups living in socioeconomic hardship[5] and at increased risk for abusing alcohol and drugs, having antisocial traits, and giving birth to their first child at a young age,[7] all of which elevate the risk for depression.
Fourth, we looked for a dose–response relationship between partner violence and women’s new-onset depression as suggested by others.[4, 15–18] Fifth, we investigated whether childhood maltreatment and partner violence had a cumulative impact on the incidence of mental health problems, over and above the effect of other risk factors. We expected high prevalence of depression in women exposed to both childhood maltreatment and partner violence and for those who experienced a wide range of abusive acts.
Sixth, we verified whether the effect of partner violence was limited to women’s depression or whether it could be generalized to other indicators of mental health problems such as psychosis spectrum symptoms. Cross-sectional studies suggest that victims of partner violence are at increased risk of reporting psychotic symptoms (e.g., hearing voices),[19–23] although strong empirical evidence supporting this association is still limited.[24, 25] These findings are, however, consistent with high prevalence of partner violence in psychiatric populations (ranging from 34 to 92%),[24] which suggests that such abuse may also carry risk for less common and more severe psychiatric disorders.[25]
METHODS
Participants were mothers involved in the Environmental Risk (E-Risk) Longitudinal Twin Study, which tracks the development of a nationally representative birth cohort of British children selected from a larger birth register of women who gave birth to twins in England and Wales in 1994–1995.[26] The original sample (n = 1,116 families) was constructed using a high-risk stratification sampling procedure to represent the U.K. population of mothers having children in the 1990s by oversampling women who gave birth to their first child when 20 years old or younger to replace those selectively lost to the register due to nonresponse and undersampling older, well-educated mothers having twins via assisted reproduction. Women were, on average, 33 years old (range 20–48) at the initial assessment (thereafter referred to as T1; Supporting Information Fig. 1). Two additional assessments were undertaken when they were, on average, 38 and 40 years old (T2 and T3), thus representing a 7-year follow-up period. The attrition was minimal and the last assessment included 96% of the women. This sample comprised 1,052 mothers with valid data on partner violence. Participants gave written informed consent after a complete description of the study. Ethical approval was granted by the Joint South London and Maudsley and the Institute of Psychiatry NHS Ethics Committee (U.K.).
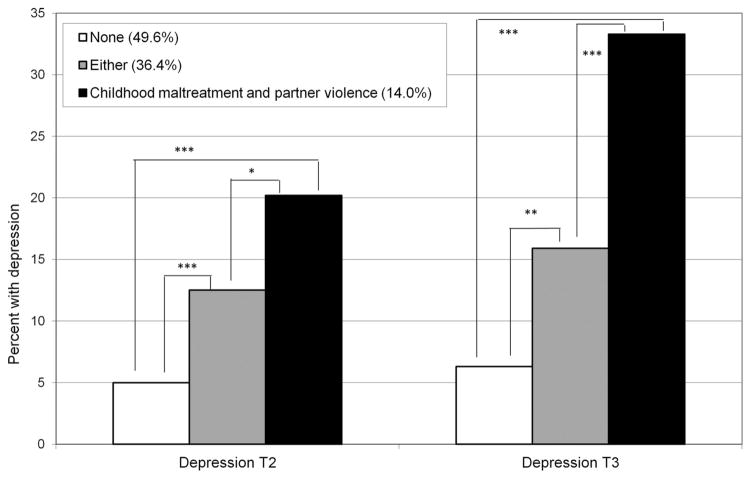
Figure 1.
Proportion of women with new-onset depression as a function of cumulative experiences of childhood maltreatment and partner violence in adulthood. Note: *P < .05; **P < .01; ***P < .001.
PARTNER VIOLENCE
We asked women about their experiences of partner violence using the Conflict Tactics Scale-Form R.[27] Participants responded “not true” or “true” to all 12 questions. Questions regarding partner violence were asked at T1, covering the period of 5 years since the twins’ birth and again at T2, 5 years later. The internal consistency reliability was .97 at T1 and .98 at T2. We identified 389 women who reported being a victim of partner violence at either time point (39.8%). We also derived an index of a variety of partner’s abusive acts representing the sum of abusive acts assessed across T1 and T2 (from 0 to 20; mean = 2.5, SD = 3.7). We created four categories corresponding to the experience of “none” (47.8%), “limited” (1 or 2; 19.2%), “moderate” (3–6; 18.5%), and a “wide” (7 or more; 14.5%) range of different types of abusive acts.
MENTAL HEALTH PROBLEMS
Depressive disorders were diagnosed using the Diagnostic Interview Schedule (DIS)[28] according to the Diagnostic and Statistical Manual of Mental Disorders-IV criteria (DSM-IV).[29] We excluded participants with a lifetime history of depression prior to T1 (6.9%, n = 72) and prospectively enquired about depressive symptoms at T2 and T3, with a reporting period of 2 years. A total of 94 women (9.8%) met DSM-IV diagnostic criteria for a major depressive episode at T2, and 125 at T3 (13.5%).
Psychosis spectrum symptoms were assessed at T3 using the Psychosis Screening Questionnaire (PSQ).[30] The PSQ consists of five probe questions enquiring about mania, thought insertion, paranoia, strange experiences, and hallucinations. Probe questions were followed, when endorsed, by secondary questions. We classified women as having psychosis spectrum symptoms if they reported at least one symptom (initial probe plus secondary questions).[31] Our goal was not to diagnose schizophrenia or other psychotic disorders but to identify women who endorsed psychotic-like experiences and beliefs bearing in mind evidence that psychotic symptoms are more prevalent in the general population than diagnosed cases of psychotic disorders.[32] In this sample, 45 women (4.7%) had at least one psychosis spectrum symptom.
CONFOUNDERS
Women’s history of childhood maltreatment was retrospectively assessed at T3 using the short form of the Childhood Trauma Questionnaire (CTQ-SF),[33] which inquires about emotional, physical, and sexual abuse and emotional and physical neglect. The validity of the CTQ’s original and brief versions has been demonstrated in community samples.[33, 34] Using the manual’s recommended classification scores,[34] we identified 235 women (24.9%) with a history of at least one type of maltreatment.
Socioeconomic deprivation was constructed from a standardized composite of family income, education, and social class collected at T1. These indicators were highly correlated (correlations ranged from .57 to .67, P’s < .05) and loaded significantly onto one latent factor (factor loadings were .80, .70, and .83 for income, education, and social class, respectively). The population-wide distribution of the latent factor was divided into three groups. One woman in three (33.5%) was living in socioeconomically deprived conditions.
Young motherhood was identified if the participants gave birth to their first child when they were 20 years old or younger. We used the information available in the U.K. register of twin birth and corroborated it during interviews conducted with mothers at T1. Half of the sample was composed of young mothers (n = 487, 49.8%).
Substance abuse was derived from the short Michigan Alcoholism Screening Test[35] and the Drug Abuse Screening Test[36] completed at T1. Internal consistency reliability was above .73. A symptom was considered to be present if the participants endorsed it as being “very true or often true.” A cut-off score of four symptoms showed good agreement with clinical diagnoses of alcoholism.[37] In this sample, 74 women (7.6%) reported substance abuse.
Antisocial personality was assessed at T1 by asking women to answer questions taken from the Young Adult Self-Report,[38] modified to obtain past reports and supplemented with questions from the DIS[28] to assess lifetime presence of DSM-IV symptoms of Conduct Disorder and Antisocial Personality Disorder (e.g., deceitfulness).[29] A symptom was considered to be present if participants endorsed it as being “very true or often true.” Women with three or more symptoms were identified as having an antisocial personality style (n = 99, 10.1%).
STATISTICAL ANALYSES
We tested our hypotheses in five steps. First, we used bivariate logistic regressions to replicate earlier reports that victims of partner violence were at increased risk for having been maltreated during their childhood and for experiencing difficulties in adulthood (socioeconomic deprivation, substance abuse, antisocial personality, and young motherhood). We then carried out a multivariate logistic regression to identify risk factors that were uniquely associated with partner violence. Second, we tested in a series of logistic regressions whether women victims of partner violence had an increased risk of new-onset depression at T2 and T3. We examined the bivariate associations (Model 1) to which we subsequently added, in separate steps, childhood maltreatment (Model 2) and the remaining confounders (Model 3).
Third, we examined the cumulative effect of childhood maltreatment and partner violence on new onsets of depression using logistic regressions. Fourth, we tested whether women exposed to a greater variety of abusive acts had an increased risk of suffering from depression using logistic regressions. In the fifth step, we repeated all the analyses using psychosis spectrum symptoms as the mental health outcome.
RESULTS
IS PARTNER VIOLENCE ASSOCIATED WITH KNOWN RISK FACTORS OF POOR MENTAL HEALTH?
Women who experienced partner violence were more likely to report childhood maltreatment, social deprivation, substance abuse, and antisocial personality, and also to have had their first child when they were young (Table 1). Each risk factor was associated with at least a twofold increase in odds of experiencing partner violence. Women with an antisocial personality had a 4.5-fold increase in their odds of experiencing partner violence, the highest odds associated with any risk factor. The multivariate analysis indicated that, aside from substance abuse, all factors were uniquely associated with partner violence (Table 1).
TABLE 1.
Prevalence of partner violence according to risk factors for poor mental health among 978 British women
| Covariates | Partner violence
|
||
|---|---|---|---|
| Women who experienced partner violence N (%) | Models
|
||
| Bivariate OR (95% CI) | Multivariate OR (95% CI) | ||
| Childhood maltreatment | |||
| Yes | 132 (56.2) | 2.49 (1.85–3.37) | 1.90 (1.38–2.63) |
| No | 241 (33.9) | ||
| Socioeconomic deprivation | |||
| Yes | 184 (56.1) | 2.77 (2.11–3.65) | 1.82 (1.33–2.50) |
| No | 205 (31.5) | ||
| Substance abuse | |||
| Yes | 45 (60.8) | 2.53 (1.56–4.12) | 1.06 (0.59–1.89) |
| No | 343 (38.0) | ||
| Antisocial personality | |||
| Yes | 71 (71.7) | 4.47 (2.83–7.08) | 2.41 (1.43–4.07) |
| No | 318 (36.2) | ||
| Young motherhood | |||
| Yes | 252 (51.7) | 2.77 (2.13–3.61) | 1.80 (1.32–2.45) |
| No | 137 (27.9) | ||
Note: OR, odds ratio; CI, confidence intervals. The multivariate model included all covariates in a single regression model to document their unique association with partner violence.
IS PARTNER VIOLENCE ASSOCIATED WITH NEW-ONSET DEPRESSION?
Women who experienced partner violence were more likely to report new-onset depression compared to those who had not, both at the end of the partner violence reporting period (T2) and 2 years later at T3 (Table 2, Panel A). These associations remained significant, but of smaller magnitude, once childhood maltreatment and other confounders were accounted for (18.1 and 33.6% decrease in odds ratio, respectively). Childhood maltreatment also uniquely contributed to new-onset depression at both time points.
TABLE 2.
Associations between partner violence and women’s new onset of depression
| Time | Risk factors | Model 1 unadjusted
|
Model 2 adjusted for child maltreatment
|
Model 3 adjusted for all confounders
|
|||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Panel A
|
Risk associated with exposure to violence
|
||||||
| T2 | Partner violence | 2.59 | 1.67–4.00 | 2.12 | 1.35–3.33 | 1.72 | 1.07–2.77 |
| Childhood maltreatment | 2.28 | 1.45–3.60 | 2.01 | 1.25–3.22 | |||
| T3 | Partner violence | 2.66 | 1.81–3.91 | 2.25 | 1.51–3.37 | 1.61 | 1.05–2.48 |
| Childhood maltreatment | 3.27 | 2.19–4.89 | 2.64 | 1.74–4.01 | |||
| Panel B
|
Cumulative risk associated with exposure to violence
|
||||||
| T2 | Either | 2.71 | 1.59–4.59 | — | — | 2.25 | 1.31–3.89 |
| Both | 4.80 | 2.63–8.75 | — | — | 3.43 | 1.79–6.57 | |
| T3 | Either | 2.78 | 1.73–4.49 | — | — | 2.09 | 1.27–3.44 |
| Both | 7.38 | 4.35–12.51 | — | — | 4.30 | 2.43–7.60 | |
| Panel C
|
Risk associated with a variety index of abusive acts
|
||||||
| T2 | Limited (1 or 2) | 0.31 | 0.67–2.55 | 1.16 | 0.59–2.29 | 1.06 | 0.53–2.10 |
| Moderate range (3 to 6) | 2.25 | 1.25–4.07 | 1.99 | 1.09–3.63 | 1.65 | 0.88–3.09 | |
| Wide range (≥ 7) | 4.71 | 2.70–8.24 | 3.44 | 1.91–6.18 | 2.53 | 1.33–4.82 | |
| T3 | Limited (1 or 2) | 2.20 | 1.28–3.79 | 1.96 | 1.12–3.42 | 1.70 | 0.96–3.02 |
| Moderate range (3 to 6) | 2.75 | 1.62–4.65 | 2.41 | 1.40–4.14 | 1.69 | 0.95–3.00 | |
| Wide range (≥ 7) | 4.33 | 2.56–7.34 | 3.48 | 2.01–6.04 | 1.88 | 1.02–3.47 | |
Note: Model 3; Panel A controlled for childhood maltreatment, socioeconomic deprivation, antisocial personality, and young motherhood. Model 3; Panel B controlled for socioeconomic deprivation, antisocial personality, and young motherhood. Comparison groups are the absence of both childhood maltreatment and partner violence for Panel B and the absence of partner violence for Panel C. OR, odds ratio; CI, confidence intervals.
IS THERE A DOSE–RESPONSE RELATIONSHIP BETWEEN CUMULATIVE VIOLENCE VICTIMIZATION AND NEW-ONSET DEPRESSION?
Figure 1 shows that the prevalence of depression increased as the experiences of abuse accumulated over time. Compared to nonvictims, women who were exposed to either childhood maltreatment or partner violence in adulthood were approximately 2.5 times more likely to report depression at T2 and T3 (Table 2, Panel B). As expected, these risks were greater for women who experienced both types of abuse. Women who experienced one type of abuse were less likely to report depression than those who were exposed to both [T2: OR (95% CI) = 0.56 (0.33–0.97); T3: OR (95% CI) = 0.38 (0.24–0.61)], indicating a dose–response relationship with violence exposure. The cumulative impact of abuse in childhood and adulthood remained significant, but of smaller magnitude, once the effect of confounders was controlled for (17.0–41.7% decrease in odds ratio).
IS THERE A DOSE–RESPONSE RELATIONSHIP BETWEEN THE VARIETY OF PARTNER’S ABUSIVE ACTS AND NEW-ONSET DEPRESSION?
We observed partial evidence for a dose–response relationship between an index of various abusive acts and new-onset depression (Table 2, Panel C). Women exposed to a limited range of abusive acts did not have an increased risk of depression at the end of the reporting period (T2), although a significant association emerged 2 years later (T3). Women exposed to a wide range of abusive acts did not show a significantly greater risk of depression in comparison to those who experienced a moderate range of violent abuse. Altogether, the findings suggest a dose–response relationship between the variety of abusive acts and new-onset depression, albeit not present between each point of the distribution or across assessments. These effects remained when childhood maltreatment was controlled for, although only women exposed to a wide range of abusive acts remained at increased risk of new-onset depression when all confounders were taken into account (Model 3).
CAN THE HARMFUL IMPACT OF PARTNER VIOLENCE EXTEND TO PSYCHOSIS SPECTRUM SYMPTOMS?
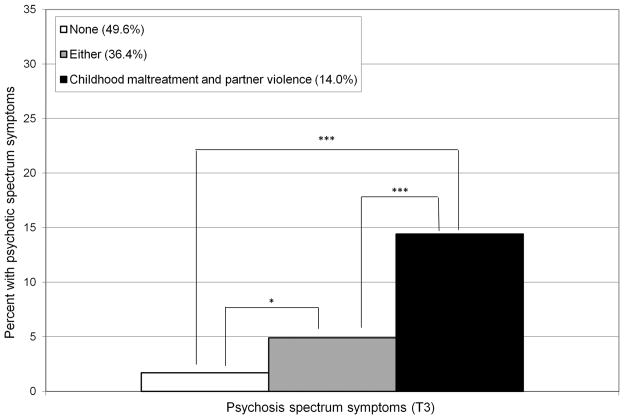
Similarly to depression, partner violence was associated with a 4.5-fold increase of reporting psychosis spectrum symptoms, which remained significant once the confounding effects of childhood maltreatment and other risk factors were controlled for (Table 3, Panel A). Figure 2 illustrates the increased prevalence of psychosis spectrum symptoms as a function of cumulative experiences of childhood maltreatment and partner violence in adulthood. Consistent with our findings on depression, the risk of psychosis spectrum symptoms was three times greater for women exposed to either childhood maltreatment or partner violence, and 10 times greater when they reported both types of abuse (Panel B). This association remained significant once the effects of all confounders were controlled for. Women exposed to one type of abuse were at lesser risk of psychosis spectrum symptoms than those who experienced both types of abuse [OR (95% CI) = 0.31 (0.16–0.62)]. Finally, women exposed to a moderate or a wide range of abusive acts had an increased risk of psychosis spectrum symptoms, but only those exposed to a wide variety of abuse remained at risk when childhood maltreatment and all other confounders were controlled for (48.5% of decrease in odds ratio).
TABLE 3.
Associations between partner violence and psychosis spectrum symptoms
| Time | Risk factors | Model 1 unadjusted
|
Model 2 adjusted for child maltreatment
|
Model 3 adjusted for all confounders
|
|||
|---|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | ||
| Panel A
|
Risk associated with exposure to violence
|
||||||
| Partner violence | 4.47 | (2.28–8.77) | 3.61 | (1.81–7.21) | 2.75 | (1.33–5.65) | |
| Childhood maltreatment | 2.76 | (1.48–5.17) | 2.25 | (1.18–4.31) | |||
| Panel B
|
Cumulative risk associated with childhood maltreatment and partner violence
|
||||||
| Either | 2.99 | (1.28–7.01) | — | — | 2.34 | (0.98–5.62) | |
| Both | 9.67 | (4.13–22.65) | — | — | 5.99 | (2.39–15.00) | |
| Panel C
|
Risk associated with a variety index of abusive acts
|
||||||
| Limited (1 or 2) | 1.39 | (0.46–4.20) | 1.20 | (0.39–3.67) | 1.09 | (0.36–3.37) | |
| Moderate range (3 to 6) | 2.66 | (1.04–6.82) | 2.28 | (0.88–5.90) | 1.82 | (0.68–4.89) | |
| Wide range (≥ 7) | 9.34 | (4.19–20.82) | 6.99 | (3.05–16.02) | 4.81 | (1.94–11.95) | |
Note: Model 3 controlled for childhood maltreatment, socioeconomic deprivation, antisocial personality, and young motherhood. Comparison groups are the absence of both childhood maltreatment and partner violence for Panel B and the absence of partner violence for Panel C. OR, odds ratio; CI, confidence intervals.
Figure 2.
Proportion of women with psychosis spectrum symptoms as a function of cumulative experiences of childhood maltreatment and partner violence in adulthood. Note: *P < .05; ***P < .001.
DISCUSSION
In our population-based sample of mothers in the United Kingdom, four of 10 women reported being the victim of violence at the hands of their partner in a period of nearly 10 years. This study demonstrates the far-reaching impact of partner violence on women’s mental health. Our findings show that women exposed to partner violence carry a two- to threefold increased risk of developing new-onset depression and psychosis spectrum symptoms. These increased risks are net of the effect of the experience of childhood maltreatment and several other known factors associated with poor mental health. Women who engage in intimate relationships with violent partners are at risk not only of physical injuries but also of later psychological problems.
Four findings from this longitudinal study stand out. First, the observed associations between partner violence and women’s depression survived the test of confounding. It is crucial to take into consideration a number of risk factors shown to have a higher prevalence in women victims of partner violence to avoid reporting erroneously inflated associations. For example, women may try to alleviate the stress and emotional burden of partner violence through the use of alcohol or drugs,[15] which may contribute to their fragile mental health. A similar argument can be put forward for antisocial personality, which was shown to be the strongest risk factor for partner abuse in this study and others.[39] Partner violence takes place between two persons who may alternate between the roles of victim and perpetrator.[40, 41] Women’s perpetration of abuse could represent a manifestation of prior antisocial lifestyle.[41] Assortative partnering, whereby women with depressive and antisocial histories tend to couple with antisocial men, also requires rigorous methodological control. Past studies could not rule out the possibility that substance abuse, assortative mating, and previous history of depression were the driving force behind the association between partner violence and women’s mental health problems because the majority controlled for socioeconomic factors only,[15] while a few also considered child maltreatment[8–10] and/or substance abuse.[42] Rarely have antisocial personality and young motherhood been included as additional confounders, thus limiting the ascertainment of these complex associations.[5]
Second, the exclusion of participants with a history of depression further strengthened the directionality of the association between partner violence and women’s poor mental health. The fact that small decreases in the estimated risks were noted once stringent control for directionality and confounders was exerted underlines the robustness of this association.[3, 16] Stress-related mechanisms could be a common denominator involved in this association; ruminating about the abuse, using poor coping strategies (e.g., social withdrawal), and manifesting a distorted sense of self-value, could increase later risks of victimization and disrupt neuroendocrine activity relevant to depression.[23, 43, 44]
Third, the risk of new-onset depression in victims of partner violence remained of similar magnitude over a 2-year period. This finding may be interpreted in two different ways. One possibility is that the impact of partner violence on women’s mental health is indeed long lasting. Previous investigations have shown that victims of partner violence had persisting mental health difficulties irrespective of whether they left or stayed in the abusive relationship.[45] Another possibility is that what may look like a persisting impact of partner violence may arise because some women had experienced recurrent violence over the course of 2 years. In our sample, half of the women who reported partner violence during the first interview were also in an abusive relationship 5 years later. The increased risk of poor mental health in women exposed to severe abuse may also be maintained by their tendency to engage in new abusive relationships.[46]
Fourth, our findings are consistent with a dose–response relationship between partner violence and women’s poor mental health, as shown by the cumulative effect of childhood maltreatment and partner violence, and also by the increasing prevalence of depression and psychosis spectrum symptoms in women exposed to a wider variety of abusive acts.[9, 24, 42] Controlling for the confounders was imperative in this endeavor as women who experienced distinct types of abuse (childhood maltreatment, partner violence) or more severe forms of exposure (variety index) showed an increased number of risk factors.[16, 17] It is noteworthy that childhood maltreatment increased the risk of women’s poor mental health over and above other risk factors, including partner violence. This finding is consistent with current conceptualizations of the early roots of physical and mental health inequalities.[47]
The present findings should be considered in light of some limitations. First, we relied on retrospective self-reports of childhood maltreatment and partner violence, which are vulnerable to recall bias. However, the long-term relationship developed with the participants of this longitudinal study supports disclosure. The use of life event calendars as reference points to report partner abuse also likely minimized memory-related errors. High test–retest and interpartner agreement obtained with a similar method supports this idea,[48] and minimizes the possibility that our measure is limited by its gender neutrality, as discussed elsewhere.[25]
Second, we did not assess the duration of the abuse, but we examined the number of different violent acts women were victims of. Future studies exploring the enduring patterns of abuse are needed to examine whether similar effects are present in different contexts. Third, our measure of partner violence mainly referred to physical abuse (e.g., slapping, kicking, choking). The inclusion of other types of abuse (e.g., sexual, emotional) would have helped to capture all instances of partner violence.
Fourth, we cannot be certain that our findings, based on a sample of twins’ mothers in England and Wales, generalize to mothers of singletons or women living elsewhere. However, our prevalence estimates of depression and the magnitude of the associations between partner violence and depression are comparable to epidemiological studies in other countries.[15, 49] Fifth, we did not ask participants about their history of psychosis spectrum symptoms before the study began, which precluded a level of control for directionality as strict as that exerted for new-onset depression.
CONCLUSIONS AND IMPLICATIONS
Our study provides strong empirical evidence supporting the directionality and magnitude of the association between partner violence and women’s new-onset depression and psychosis spectrum symptoms. These robust and long-lasting effects emphasize that it is important for mental health professionals to investigate past and current experiences of abuse in women reporting poor mental health, ideally using self-reported measures.[50] Diagnostic and subsequent care may be improved as a result of this.[51] Immediate support taking the forms of advocacy and psychological interventions would be beneficial to women who disclose violence.[24, 52, 53] Taking a history of violence and providing advice about mobilizing social support to activate their resources in dealing with severe stress should also be prioritized.[51] To do so, frontline staff should be trained to recognize the indicators of partner violence, to ask relevant questions for easier disclosure, and to create a comfortable environment where women feel safe and treated in a kind, sensitive manner.[54] More generally, considering that more than half of victims of partner violence reported new-onset depression, reducing this form of abuse in our society may be a valuable strategy to prevent the onset of mental health problems in women.
Acknowledgments
Contract grant sponsor: Medical Research Council; Contract grant numbers: G9806489, 61002190; Contract grant sponsor: Economic and Social Research Council; Contract grant number: RES-177-25-0013; Contract grant sponsor: NICHD; Contract grant number: HD061298.
We are grateful to the Study families and teachers for their participation. We thank Michael Rutter, Robert Plomin, and members of the E-Risk team for their dedication, hard work, and insights. The E-Risk Study is funded by the Medical Research Council (grant G9806489 and 61002190). Additional support was provided by funds from the Economic and Social Research Council (RES-177-25-0013) and NICHD (HD061298). Isabelle Ouellet-Morin is a Canadian Institute of Health Research New Investigator.
Footnotes
Conflict of interest. The authors report no conflict of interest.
References
- 1.Black MC, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Costs of Intimate Partner Violence Against Women in the United States. Altlanta: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 3.Golding JM. Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J Fam Violence. 1999;14:99–132. [Google Scholar]
- 4.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359:1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 5.Devries KM, Mak JY, Bacchus LJ, et al. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med. 2013;10:e1001439. doi: 10.1371/journal.pmed.1001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jordan CE, Campbell R, Follingstad D. Violence and women’s mental health: the impact of physical, sexual, and psychological aggression. Ann Rev Clin Psychol. 2010;6:607–628. doi: 10.1146/annurev-clinpsy-090209-151437. [DOI] [PubMed] [Google Scholar]
- 7.Briere J, Jordan CE. Violence against women: outcome complexity and implications for assessment and treatment. J Interpers Violence. 2004;19:1252–1276. doi: 10.1177/0886260504269682. [DOI] [PubMed] [Google Scholar]
- 8.Coker AL, Smith PH, Bethea L, et al. Physical health consequences of physical and psychological intimate partner violence. Arch Fam Med. 2000;9:451–457. doi: 10.1001/archfami.9.5.451. [DOI] [PubMed] [Google Scholar]
- 9.Carlson BE, McNutt LA, Choi DY. Childhood and adult abuse among women in primary health care: effects on mental health. J Interpers Violence. 2003;18:924–941. doi: 10.1177/0886260503253882. [DOI] [PubMed] [Google Scholar]
- 10.Hegarty K, Gunn J, Chondros P, et al. Association between depression and abuse by partners of women attending general practice: descriptive, cross sectional survey. BMJ. 2004;328:621–624. doi: 10.1136/bmj.328.7440.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moffitt TE, Caspi A. Annotation: implications of violence between intimate partners for child psychologists and psychiatrists. J Child Psychol Psychiatry. 1998;39:137–144. [PubMed] [Google Scholar]
- 12.Widom CS, Czaja SJ, Dutton MA. Childhood victimization and lifetime revictimization. Child Abuse Negl. 2008;32:785–796. doi: 10.1016/j.chiabu.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whitfield CL, Anda RF, Dube SR, et al. Violent childhood experiences and the risk of intimate partner violence in adults. J Interpers Violence. 2003;18:166–185. [Google Scholar]
- 14.Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- 15.Coker AL, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23:260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 16.Dillon G, Hussain R, Loxton D, et al. Mental and physical health and intimate partner violence against women: a review of the literature. Int J Family Med. 2013;2013:313909–313914. doi: 10.1155/2013/313909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ludermir AB, Schraiber LB, D’Oliveira AF, et al. Violence against women by their intimate partner and common mental disorders. Soc Sci Med. 2008;66:1008–1018. doi: 10.1016/j.socscimed.2007.10.021. [DOI] [PubMed] [Google Scholar]
- 18.Dutton MA, Green BL, Kaltman SI, et al. Intimate partner violence, PTSD, and adverse health outcomes. J Interpers Violence. 2006;21:955–968. doi: 10.1177/0886260506289178. [DOI] [PubMed] [Google Scholar]
- 19.Meekers D, Pallin SC, Hutchinson P. Intimate partner violence and mental health in Bolivia. BMC Womens Health. 2013;13:28. doi: 10.1186/1472-6874-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danielson KK, Moffitt TE, Caspi A, et al. Comorbidity between abuse of an adult and DSM-III-R mental disorders: evidence from an epidemiological study. Am J Psychiatry. 1998;155:131–133. doi: 10.1176/ajp.155.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neria Y, Bromet EJ, Carlson GA, et al. Assaultive trauma and illness course in psychotic bipolar disorder: findings from the Suffolk county mental health project. Acta Psychiatr Scand. 2005;111:380–383. doi: 10.1111/j.1600-0447.2005.00530.x. [DOI] [PubMed] [Google Scholar]
- 22.Friedman SH, Loue S. Incidence and prevalence of intimate partner violence by and against women with severe mental illness. J Womens Health. 2007;16:471–480. doi: 10.1089/jwh.2006.0115. [DOI] [PubMed] [Google Scholar]
- 23.Jonas S, Khalifeh H, Bebbington PE, et al. Gender differences in intimate partner violence and psychiatric disorders in England: results from the 2007 adult psychiatric morbidity survey. Epidemiol Psychiatr Sci. 2014;23:189–199. doi: 10.1017/S2045796013000292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howard LM, Trevillion K, Khalifeh H, et al. Domestic violence and severe psychiatric disorders: prevalence and interventions. Psychol Med. 2010;40:881–893. doi: 10.1017/S0033291709991589. [DOI] [PubMed] [Google Scholar]
- 25.Trevillion K, Oram S, Feder G, et al. Experiences of domestic violence and mental disorders: a systematic review and meta-analysis. PLoS One. 2012;7:e51740. doi: 10.1371/journal.pone.0051740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moffitt TE E-Risk Study Team. Teen-aged mothers in contemporary Britain. J Child Psychol Psychiatry. 2002;43:727–742. doi: 10.1111/1469-7610.00082. [DOI] [PubMed] [Google Scholar]
- 27.Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) Scales. In: Straus MA, Gelles RJ, editors. Physical violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. New Brunswick: Transaction Press; 1990. pp. 403–424. [Google Scholar]
- 28.Robins L, Cottler L, Bucholz K, et al. Diagnostic Interview Schedule for DSM-IV. St. Louis: Washington University School of Medicine; 1996. [Google Scholar]
- 29.American Psychiatric Association. Diagnostic and Statistical Manual. 4. Washington, DC: 1994. [Google Scholar]
- 30.Bebbington P, Nayani T. The Psychosis Screening Questionnaire. Int J Methods Psychiatr Res. 1995;5:11–19. [Google Scholar]
- 31.Johns LC, Cannon M, Singleton N, et al. Prevalence and correlates of self-reported psychotic symptoms in the British population. Br J Psychiatry. 2004;185:298–305. doi: 10.1192/bjp.185.4.298. [DOI] [PubMed] [Google Scholar]
- 32.Myin-Germeys I, Krabbendam L, van Os J. Continuity of psychotic symptoms in the community. Curr Opin Psychiatry. 2003;16:443–449. [Google Scholar]
- 33.Bernstein D, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 34.Bernstein D, Fink L. Childhood Trauma Questionnaire Manual. San Antonio: The Psychological Corporation; 1998. [Google Scholar]
- 35.Selzer ML, Vinokur A, van Rooijen L. A self-administered Short Michigan Alcoholism Screening Test (SMAST) J Stud Alcohol. 1975;36:117–126. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- 36.Skinner HA. The drug abuse screening test. Addict Behav. 1983;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 37.Crews TM, Sher KJ. Using adapted short MASTs for assessing parental alcoholism: reliability and validity. Alcohol Clin Exp Res. 1992;16:576–584. doi: 10.1111/j.1530-0277.1992.tb01420.x. [DOI] [PubMed] [Google Scholar]
- 38.Achenbach TM. Manual for the Young Adult Self-Report and Young Adult Behavior Checklist. Burlington: University of Vermont Department of Psychiatry; 1997. [Google Scholar]
- 39.Kim H, Laurent H, Capaldi D, et al. Men’s aggression toward women: a 10-year panel study. J Marriage Fam. 2008;70:1169–1187. doi: 10.1111/j.1741-3737.2008.00558.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Archer J. Sex differences in aggression between heterosexual partners: a meta-analytic review. Aggr Viol Behav. 2002;7:313–351. doi: 10.1037/0033-2909.126.5.651. [DOI] [PubMed] [Google Scholar]
- 41.Ehrensaft MK, Moffitt TE, Caspi A. Clinically abusive relationships in an unselected birth cohort: men’s and women’s participation and developmental antecedents. J Abnorm Psychol. 2004;113:258–270. doi: 10.1037/0021-843X.113.2.258. [DOI] [PubMed] [Google Scholar]
- 42.Nicolaidis C, Curry M, McFarland B, et al. Violence, mental health, and physical symptoms in an academic internal medicine practice. J Gen Intern Med. 2004;19:819–827. doi: 10.1111/j.1525-1497.2004.30382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nemeroff CB, Vale WW. The neurobiology of depression: inroads to treatment and new drug discovery. J Clin Psychiatry. 2005;66(Suppl 7):5–13. [PubMed] [Google Scholar]
- 44.Howard LM, Trevillion K, Agnew-Davies R. Domestic violence and mental health. Int Rev Psychiatry. 2010;22:525–534. doi: 10.3109/09540261.2010.512283. [DOI] [PubMed] [Google Scholar]
- 45.Zlotnick C, Johnson DM, Kohn R. Intimate partner violence and long-term psychosocial functioning in a national sample of American women. J Interpers Violence. 2006;21:262–275. doi: 10.1177/0886260505282564. [DOI] [PubMed] [Google Scholar]
- 46.Carbone-Lopez K, Rennison C-M, Macmillan R. The transcendence of violence across relationships: new methods for understanding men’s and women’s experiences of intimate partner violence across the life course. J Quant Criminol. 2012;28:319–346. [Google Scholar]
- 47.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 48.Moffitt TE, Caspi A, Krueger RF, et al. Do partners agree about abuse in their relationship? A psychometric evaluation of interpartner agreement. Psychol Assess. 1997;9:47–56. [Google Scholar]
- 49.Ehrensaft MK, Moffitt TE, Caspi A. Is domestic violence followed by an increased risk of psychiatric disorders among women but not among men? A longitudinal cohort study. Am J Psychiatry. 2006;163:885–892. doi: 10.1176/ajp.2006.163.5.885. [DOI] [PubMed] [Google Scholar]
- 50.MacMillan HL, Wathen CN, Jamieson E, et al. Approaches to screening for intimate partner violence in health care settings: a randomized trial. JAMA. 2006;296:530–536. doi: 10.1001/jama.296.5.530. [DOI] [PubMed] [Google Scholar]
- 51.World Health Organization. Responding to Intimate Partner Violence and Sexual Violence Against Women: WHO Clinical and Policy Guidelines. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 52.Feder G, Davies RA, Baird K, et al. Identification and Referral to Improve Safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: a cluster randomised controlled trial. Lancet. 2011;378:1788–1795. doi: 10.1016/S0140-6736(11)61179-3. [DOI] [PubMed] [Google Scholar]
- 53.Ramsay J, Carter Y, Davidson L, et al. Advocacy interventions to reduce or eliminate violence and promote the physical and psychosocial well-being of women who experience intimate partner abuse. Cochrane Database Syst Rev. 2009;3 doi: 10.1002/14651858.CD005043.pub2. [DOI] [PubMed] [Google Scholar]
- 54.NICE. Domestic Violence and Abuse: How Health Services, Social Care and the Organisations They Work With Can Respond Effectively. London: National Institute for Health and Care Excellence; 2014. [Google Scholar]