Abstract
Background
In El Salvador, about 200 new cases of pediatric cancer are diagnosed each year, and survival rates approach 70%. Although treatment is available at no cost, abandonment of therapy has remained at a steady yearly rate of 13% during the past decade. A time sensitive adherence tracking procedure (TS-ATP) was recently implemented to detect missed appointments, identify their causes, and intervene promptly.
Procedure
The study team was informed daily of patient/family failure to attend medical appointments in the pediatric oncology unit; the families were contacted and interviewed to ascertain and address the reasons. Patients who did not return after this initial contact were contacted again through local health clinics and municipalities. Law enforcement was a last resort for patients undergoing frontline treatment with a good prognosis., The system was adapted to clinical urgency: families of patients undergoing induction therapy were contacted within 24 hours, those in other therapy phases, within 48 hours, and those who had completed treatment, within one week. Reasons for absence were obtained by telephone or in person.
Results
The annual rate of abandonment was reduced from 13% to 3% during the 2-year period. There were 1111 absences reported and 1472 contacts with caregivers and institutions. The three main reasons for absences were financial needs (165, 23%), unforeseen barriers (116, 16%), and domestic needs (86, 12%).
Conclusions
Use of the treatment adherence tracking system to locate and communicate with patients/families after missed appointments and the allocated aid stemming from these interviews substantially reduced abandonment and non-adherence.
Keywords: childhood cancer, treatment abandonment, adherence, patient tracking, developing countries
BACKGROUND
Abandonment of therapy, defined as either missing at least 4 consecutive weeks of scheduled treatment or not starting therapy after a cancer diagnosis (1), is a major cause of pediatric cancer mortality in low- and mid-income countries(2–5). Although less clearly documented, more general non-adherence to treatment (such as intermittently missing medication doses or appointments) can also reduce the effectiveness of therapy(6) and may predict a greater risk of abandoning treatment. The World Health Organization defines adherence as “the extent to which a person’s behavior … corresponds with agreed recommendations from a health care provider”(7). Parents or caregivers are generally responsible for adherence to their child’s therapy appointments and therefore can provide insight into the causes of non-adherence and abandonment of therapy.
Low adherence to medication, such as missing chemotherapy appointments, has been observed in young patients with cancer(8, 9); they may experience lower cure rates as a consequence (8–10), including the relapse of highly curable malignancies. The impact of poor therapy adherence on survival has not been reported in children with cancer, but it may partially explain their relatively low survival rates in low- and mid-income countries.
Medications, diagnostic procedures, and treatment for childhood cancer are provided free of charge at El Salvador’s national pediatric hospital in San Salvador, and psychosocial and financial support, food and shelter are available to families. Although these measures have substantially reduced abandonment, it has remained at approximately 13% over the past decade and is still an important cause of treatment failure (11). Therefore, additional factors in the abandonment of treatment remain to be identified.
Focusing adherence to treatment appointments, we reasoned that a first missed appointment could be interpreted as a “cry for help” and could provide important information about the unaddressed barriers to treatment. The systematic documentation of missed therapy appointments recently became possible in our unit, when an electronic tracking system was implemented for follow-up of all patient care, including admission, clinic visits, clinical examination, and chemotherapy prescription, preparation, and administration. This system also allowed the prompt detection of failure to appear for scheduled clinical visits. When a patient was considered a “no show,” the psychosocial team made family contact, obtained the reasons for the absence, and discussed possible options of help. In a similar initiative to the one we are reporting here, Kumar et al. (12) showed that interventions are more effective in a preventive frame instead of after an event of abandonment, which supports our methodology departing point of delivering tailored counseling and solutions once the first signs of discontinuity were detected. Here we describe the implementation and results of the time-sensitive adherence tracking procedure (TS-ATP) over a period of 2 years. The procedure was prospectively designed to allow (1) systematic detection and recording of absences, (2) contact with the patient’s caregivers, (3) documentation of reasons for the absence, (4) instruction of parents about the importance of adherence, and (5) appropriate interventions to overcome barriers to a prompt return and prevent further absences.
PATIENTS AND METHODS
Patients and Setting
El Salvador has approximately six million inhabitants, of which 29% are children less than14 years of age (13). About 200 new cases of childhood cancer are diagnosed each year at the oncology unit within the national children’s hospital (Hospital Nacional de Niños Benjamin Bloom), in San Salvador. This is the only referral center for childhood cancer treatment in the country. According to hospital data, approximately 70% of patients’ families live in extreme poverty, having no fixed income; they survive on informal, temporary work and have a monthly income below $50. Sixteen percent live in poverty (monthly income < $250), and only 14% live above the poverty level. Despite high poverty levels among the population, all Salvadorans own a cellular phone or have a family member who owns one, which allowed the tracking procedure to function. All children with cancer under age 12 years are treated in the pediatric oncology unit. All patients in active treatment must visit the hospital at least once weekly, although about half reside in rural areas.
An undetermined number of patients’ missed appointments were undetected until the TS ATP was implemented to reduce absences by early detection, investigation of the reasons for absence, and provision of appropriate economic, emotional, and educational support. Our analysis included all newly diagnosed patients as well as those undergoing treatment prior to the implementation of the TS-ATP, who missed one or more appointments between January 2011 and December 2012, for solid or hematological malignancies, who were on or off treatment, receiving palliative care, or undergoing diagnostic confirmation.
Procedure
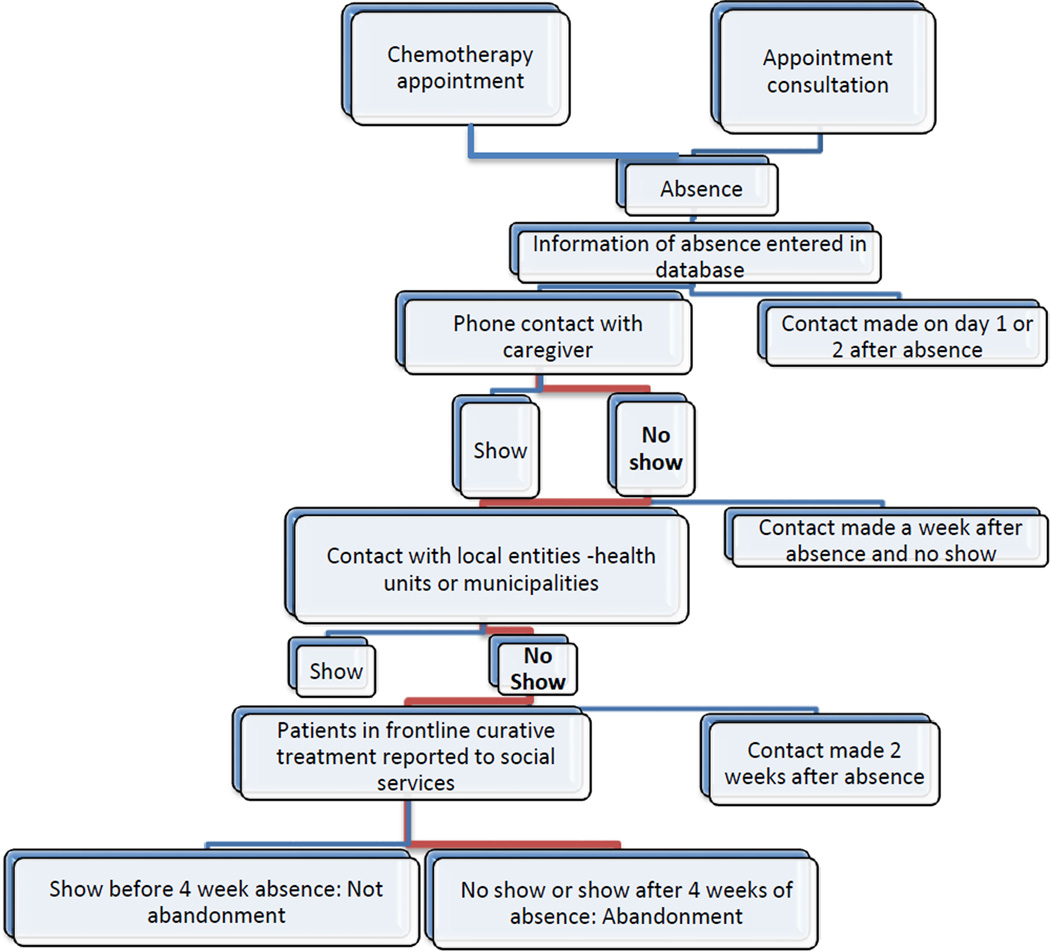
Adherence tracking was conducted by a psychosocial team comprising two psychologists, a social worker, and a nurse educator. Absences were detected by two routes. For clinical appointments, the charts of absent patients were collected; for chemotherapy appointments, the electronic system showed which scheduled patients’ chemotherapy had not been prepared in pharmacy, identifying a no show. The team initiated an entry in a database created for this purpose at the time a patient failed to appear for a scheduled appointment. Patients’ names were highlighted in the database to indicate that contact with the family was pending. The TS-ATP procedure is shown in Figure 1.
Figure 1.
Procedure of TS ATP
Patient/Family Contact and Interviews
The intervention process began with attempted telephone or personal contact with the child’s caregiver to ascertain the reasons for the absence (by open-ended questions), emphasize the importance of therapy adherence, and discuss options that might quickly return the child to the hospital. The call/interview and its contents were reported in the database. Patients with ALL in the induction phase were contacted within 24 hours, all other patients in treatment within 48 hours, and patients off treatment within a week. We intentionally focused the tone of the calls and interviews more on concern and willingness to help than on reprimanding the caregivers. After the patient arrived at the hospital, the entry highlight was removed but information about the absence, and the intervention process remained in the database. If no reasons were given for the absence or if a more in-depth interview was needed, for example for families experiencing greater difficulty, a member of the psychosocial team interviewed the caregivers after their return to the hospital.
Importantly, we categorized the act of contacting the parent/caregiver in itself as an intervention, reflecting the profound effect that personal attention from a clinical professional can have on the average parent in this setting. Most patients’ families live in deep poverty and lack even basic education, creating a great economic and sociocultural divide between these families and the educated professionals who care for them. This almost “god-like” effect is difficult to convey in a journal context, but the effort of a clinician to reach out in a caring manner can deeply impress and motivate a child’s caregivers. The information obtained from the interviews and the discussion of options was promptly entered into the database and was available to all team members.
These reasons for absences were later assigned categories.
Specific interventions were devised according to the reasons stated for the absences. If a patient failed to appear at the hospital for several days after initial retrieval attempts, the health unit (within the national health care system) nearest to the patient’s residence was contacted, and local nurses or health workers visited the caregivers’ home to check on patients and persuade the parents to take the child to the hospital. If this effort proved unsuccessful for a patient undergoing frontline treatment with curative intent, the case was referred to social services to be pursued according to a law introduced in 2010 to protect the welfare of children. This law states that when a child requires treatment for a life-threatening condition, the medical instructions must be followed. The hospital´s social services report the child´s case to the pertinent state authorities and locate the patient to return him to the hospital. When the child was not located before the 4 week hiatus from treatment, the case was entered in the database as abandonment. The disruptive nature of this procedure for the family unit is the reason why the hospitals team resorts to this measure as a last option. For missed appointments of patients off treatment with no contact information, their last attendance was verified in an online internal database of the hospital.
Information entered into the database included patient identification, treatment phase, contact information, date and type of absence, date and type of attempt made to contact the parents, time required for each attempt or contact, reasons given for the absence, team member who made the contact, travel distance to the hospital, and monthly family income which was available from the initial diagnosis interview of all patients. All members of the team updated the database daily. The psychologists categorized the stated reasons for absence on the basis of information from the interviews, together with parents’ past interviews and psychosocial records.
Specific Interventions
Specific interventions were devised to address the reasons given for absence and could include financial aid, food, and/or shelter (if not previously offered), counseling for emotional hardship, and instruction to improve understanding of or adjustment to the treatment regimen or hospital routine. Although assistance might have been available earlier for these families, their level of need might not have been fully appreciated. The assessment of the patient´s needs and provision of any type of aid was based on the criteria of the social worker and the psychologists. The social worker has ample knowledge of the cost of travel expenses from all over the country and allocated financial aid to those with a greater financial burden in terms of travel expenses.
RESULTS
Patients and Missed Appointments
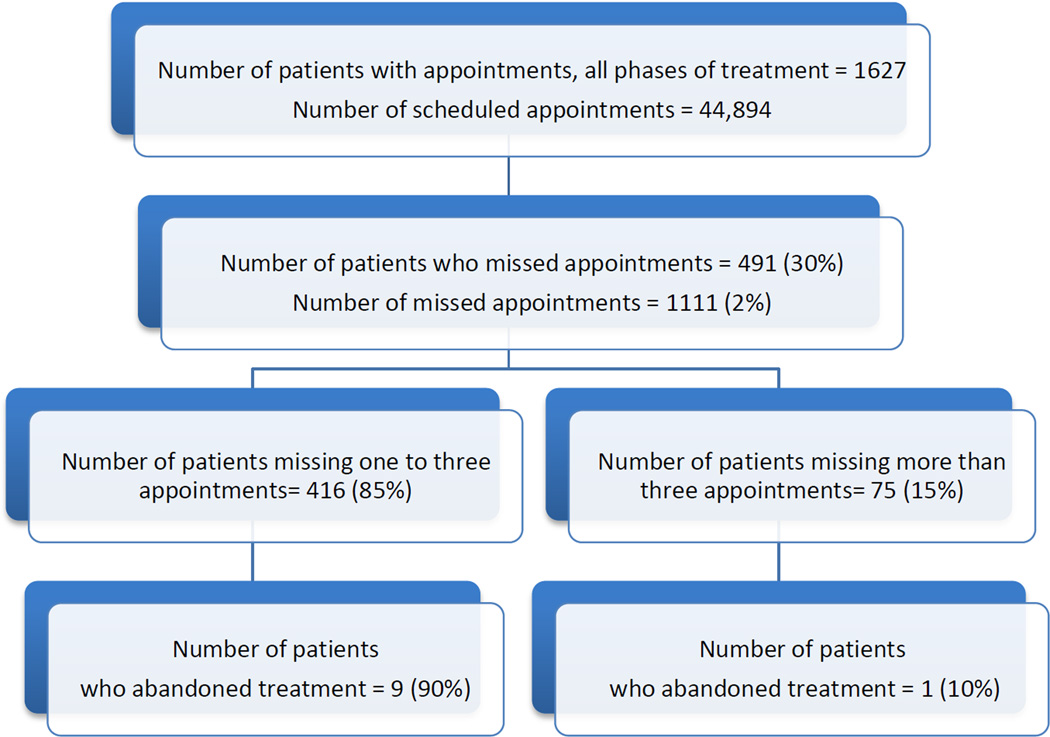
During the 2-year period, 25,953 physician appointments and 18,941 ambulatory chemotherapy appointments were scheduled (Figure 2). Of these, 1,313 appointments were missed by patients in any phase of treatment; 202 (15%) were erroneously reported as absences due to scheduling changes not registered in the electronic system or patients’ arrival after the day’s attendance had been documented. The remaining 1,111 absences reflected appointments for 491 patients, some of whom had numerous absences sometimes at different phases of treatment. There were 1–18 absences per patient. Most patients (416/491, 85%) had 1 to 3 absences, accounting for 53% (588/1,111) of absences. The remaining 75/491 (15%) patients had 4–18 absences. Missed appointments increased during the rainy season (May through October). During year 1, 23% of all absences were counted in October, when a tropical storm paralyzed public transportation for 2 weeks. Absences were relatively uniform during the dry season. Phase of treatment at the time of absence is shown in Table I.
Figure 2.
Flow chart of appointments made and missed in the pediatric oncology unit during the 2-year study period, showing the rate of abandonment of therapy in patients who missed 1–3 visits (0.022) and in those who missed more than 3 visits (0.013). Two patients who refused treatment and had no absences are excluded from flow chart.
Table I.
Absences and Interventions According to Phase of Treatment
| All Phases of Treatment, n (%) | In Treatment, n (%) | |||
|---|---|---|---|---|
| Number of Absences | 1,111 | 704 | ||
| •In treatment | 704 (63) | |||
| •Off treatment | 326 (29) | |||
| •Palliative Care | 61 (6) | |||
| •Pending Diagnosis | 20 (2) | |||
| Absences with No Intervention* | 305 (27) | 108 (15) | ||
| Total Number of Interventions | 1,472 | 1098 | ||
| •Telephone Calls | 1,005 (68) | •Telephone Calls | 790 (72) | |
| •Interviews | 374 (26) | •Interviews | 301 (27) | |
| •Database Searches | 93 (6) | •Database Searches | 7 (1) | |
Refers to either no attempt to contact or no answer obtained from attempted contact.
Contact with Caregivers
Of the 1111 absences, 806 (73%) had successful contacts. Contact with patients who had missed appointments or verify their return to the hospital after an absence resulted in 1472 attempts. Some patients had several attempts to contact. Of these 1472 attempts, 1379 (94%) resulted in interviews. Most were conducted by telephone (1,005; 68%) and the rest in person (374; 25%). The remaining 93 (6%) were patients off treatment and a treatment protocol database was used to search for their last attended appointment in case they had shown up and it was not detected. (Table I).
No contact with the parent/caregiver was made for 305 (27%) absences. Of these, 183 (60%) were absences of patients off treatment whose contact information was outdated. The remaining 122 absences (40%) were of patients in treatment, palliative care, or pending diagnosis. This category included patients who had already returned to the hospital prior to a contact attempt or with whom attempted contact was unsuccessful (e.g., unanswered calls, disconnected telephones).
Patients in Active Treatment
The 269 patients in active treatment had 704 absences. Of these, 486 absences (69%) were of children with acute lymphoblastic leukemia (ALL), 34 (5%) were of children with CNS neoplasms, 62 (9%) were of children with lymphomas, and the remaining 137 (19%) corresponded to other neoplasms. Of these 269 patients, 128 (48%) had one absence, 59 (22%) had two absences, and 29 (11%) had three absences. The remaining 53 (19%) patients had 4 to 18 absences.
The 704 absences during active treatment prompted 1,098 attempts at contact, representing 75% of the 1,472 total attempted contacts: 790 (72%) telephone calls, 301 (27%) interviews, and 7 (1%) searches for last attended appointment. Seven patients undergoing frontline treatment with curative intent had caregivers who declined to return to the hospital; meetings of the pediatric oncology interdisciplinary team resulted in a decision to report these cases to social services for legal action. Four of the seven children were returned for treatment within 4 weeks. The remaining three were returned later and were classified as having abandoned treatment. Table I shows absence rates and contact interventions during all phases of treatment and during active treatment.
Abandonment of Treatment
During these 2 years of adherence tracking, the annual rate of abandonment was reduced to 3%. Twelve of the 269 patients on active therapy did not return to the hospital within 4 weeks despite telephone contact and were classified as having abandoned treatment. Two patients’ caregivers refused curative treatment outright; 7 patients abandoned treatment with no prior absences, while 3 patients had had 2, 3, and 6 absences, respectively, before abandoning treatment. Of these 12 patients, 7 (59%) were male. Five of the 12 patients required amputation or other complex surgery, and parents attributed their refusal or abandonment of therapy in part on their fear of or disagreement with the child’s surgery. Attempts were made to contact and bring back all children as quickly as feasible after their absence was detected, except in three cases: one child with retinoblastoma whose caregiver refused enucleation outright, one child who had an undetected absence of one month before returning, and a patient with ALL who had a complex constitutional medical condition and whose caregiver refused curative treatment for ALL. Ten of the 12 cases of abandonment occurred within 6 months of beginning therapy, and six occurred during the first two months. The cases of patients who abandoned therapy are characterized in Table II.
Table II.
Characteristics of the 12 Cases of Abandonment of Treatment
| Case | Diagnosis | Age at Diagnosis (years) |
Sex | Time since Diagnosis at Time of Abandonmenta (years) |
Number of Previous Absences |
Legal Intervention |
|---|---|---|---|---|---|---|
| 1 | ALL | 2.5 | Female | 0 | Refusedb | No |
| 2 | Retinoblastoma | 2.2 | Male | .36 | 0 | No |
| 3 | Ewing Sarcoma | 3.4 | Female | .6 | 0 | No |
| 4 | CNS Tumor | 2.7 | Male | 1.3 | Refusedb | No |
| 5 | Ewing Sarcoma | 11.3 | Male | 1.8 | 0 | No |
| 6 | ALL | 3.0 | Female | 2.3 | 0 | Yes |
| 7 | Sarcoma | 12.2 | Male | 3 | 0 | No |
| 8 | Wilms Tumor | 4.1 | Male | 4.3 | 0 | No |
| 9 | Wilms Tumor | 2.1 | Female | 5.2 | 0 | No |
| 10 | Hodgkin Lymphoma | 6.8 | Male | 6.4 | 6 | No |
| 11 | Histiocytosis | 4.2 | Female | 7.9 | 3 | Yes |
| 12 | ALL | 6.8 | Male | 12.3 | 2 | Yes |
ALL, acute lymphoblastic leukemia; CNS Central Nervous System
Abandonment was defined as failure to start or complete medically indicated curative therapy.
Patients listed as “refused” attended treatment appointments but never began curative therapy. Therefore, they abandoned therapy despite not missing appointments.
Reasons Given for Absence
Table III categorizes the reasons given by caregivers for the patient’s absence. Lack of funds was most common (165; 23%). The Domestic Needs category (86; 12%) included illness of the primary caregiver (53%) or another family member (22%) and the primary caregiver’s conflicting responsibility for the care of other family members. Fourteen of these caregivers (12%) stated that no one else was available to take the child to the hospital. The Unforeseen Events category (116; 16%) included weather conditions (71 absences, 61%) and transportation problems (28 absences, 24%). Finances, domestic needs, and unforeseen events accounted for 52% of patient absences.
Table III.
Post-hoc Categorization of Caregivers’ Reported Reasons for Absence
| Category | Description | Number of Absences (%) |
|---|---|---|
| Financial Need |
|
165 (23) |
| Unforeseen Barriers |
|
116 (16) |
| Domestic Needs |
|
86 (12) |
| Caregiver Decided Against Treatment |
|
69 (10) |
| Caregiver Error |
|
56 (8) |
| Ongoing Demands |
|
48 (7) |
| Missing Information |
|
34 (5) |
| Caregiver Disagreed with Treatment |
|
16 (2) |
| Miscellaneous |
|
6 (1) |
| Palliative Care |
|
0 (0) |
DISCUSSION
We have described the first two years of application of the TS ATP, an intervention to address patients’ missed appointments. The absences were detected during the scheduled appointment day and the parent/caregiver was contacted within the following 24 to 48 hours. Prompt contact and the process of interviews and actions allowed us to obtain most parents’ reasons for absence and to provide appropriate aid to prevent or reduce further absences. The main reported barrier to keeping appointments was lack of funds, either sporadic or continuous; the distribution of family tasks and support also played a role. To address these problems, financial assistance was given or increased, and options for temporary housing were coordinated. The annual abandonment rate fell from 13% to 3% during the two years of this intervention.
Understanding the causes of missed therapy appointments is crucial for proper resource allocation to reduce or prevent abandonment. Our procedure was highly effective in the prompt detection and follow-up of missed appointments. Our success in improving treatment adherence was attributable to the daily commitment of the monitoring team to contact parents and to ascertain and address their specific needs, which in many cases enhanced the parent–care team relationship. The availability of a computer-based system that facilitated prompt detection was the starting point of this intervention, allowing information to be accessed and updated at any time by any member of the group; however, the effort and commitment of the team in locating the patient/family, obtaining the information, and following a procedure to reduce or prevent absences was the decisive factor for success.
Despite free treatment and hospitalization and subsidies for housing, food, and transportation, financial need remained a significant cause of missing appointments. In some cases, patients who had missed several appointments were retained in therapy by provision of financial aid and psychosocial support. Contact by the care team was highly meaningful to parents in itself and increased their willingness to continue treatment despite great adversity. However, the parents’ explanations showed that more complex issues, mainly lack of help in meeting family demands, also affected their ability to appear for appointments.
We found no clear relation of the number of missed appointments to the likelihood of abandonment. The fact that some patients who abandoned treatment had missed no previous appointments, or missed only a few, suggests that immediate attention should be given to each absence, even if only one appointment is missed.
Parents’ need for additional financial aid to comply with treatment raises several questions. It is possible that parents who have multiple absences despite financial support for transportation may have become dependent on these funds to comply with treatment responsibilities. These parents expressed the lack of availability of this financial aid on the expected date as an impediment to comply adherently to treatment. This increases the need for the institution to secure these means to be always available. Future research should examine where the parents perceive their responsibility to lie after an institution begins to facilitate or underwrite travel. Although it was not systematically documented, some interviews with parents suggested that during the often lengthy process of treatment, parents began to consider it the hospital’s responsibility to provide the necessary means for the child to receive treatment as planned and became less concerned about adherence to treatment.
Ten percent of missed appointments were attributed to lack of a second adult to take over domestic needs, even during a patient’s medical emergencies. A significant number of families live at the limits of their capacity to manage domestic and job demands and cannot accommodate unexpected burdens. Similarly, interviews and focus groups with parents of children undergoing cancer treatment in Malawi showed that immediate family members would help with tasks at home to facilitate a parent’s travel to the hospital, but community commitment was not strong (14). Further studies should explore to what extent this type of family isolation is inescapable and to what extent it could be remedied by seeking alternative options for assistance.
All but one case of abandonment occurred during the first year of treatment, with the highest incidence during the first months, as reported in other studies (11, 15, 16), confirming that surveillance of treatment adherence and prompt guidance of parents is vital during this time. We demonstrated that such monitoring and immediate intervention reduces abandonment. Similarly, Brown et al. found in Saudi Arabia that close monitoring increased treatment adherence in a comparable group of patients (17). Moreover, a report from Recife, Brazil described how immediate tracking of patients’ absences, together with psychosocial support integrated in the medical care, can substantially reduce abandonment (18). As in Recife, El Salvador’s pediatric cancer program provides several types of psychosocial intervention, and addition of the treatment adherence tracking program appears to be reducing abandonment to an extent similar to that in Brazil.
Team members perceived that most caregivers and family members were surprised and impressed by the professionals’ attention and appreciative of their concern after a missed appointment; we intend to further analyze the implications of this effect. However, we believe that the involvement and support of local groups in helping to locate patients also helped to persuade the parents to continue their child’s treatment. It is possible that the parents realize that others care and are aware of their decisions regarding their child’s health.
Despite the many effective interventions that quickly located and retrieved absent patients, there remained at the time of this report room for improvement in updating patients’ contact information and inability to respond to an absence on the same day it occurred. Additionally, time could be saved by improving clerical procedures and clinician communication to prevent erroneous absence notifications. Other difficulties included the unavailability of a team member to perform interviews at all times, subjective differences in implementation of the routine, and the accuracy of the registered information. Although tracking of missed appointments and subsequent intervention were time consuming, such a project is feasible and worthwhile.
Immediate detection and remediation of absences was successful in securing patients’ prompt return to the hospital, reducing the decade-long 13% rate of abandonment to 3% in both study years. Interviews and supportive contact with caregivers allowed us to identify their immediate needs and intervene as warranted to reduce absences. Interventions typically involved financial assistance, emotional support, and instruction about the importance of treatment adherence. Rarely, law enforcement measures were necessary.
Acknowledgments
We thank Sharon Naron for expert scientific review. This work was supported in part by Cancer Center Support (CORE) grant P30 CA021765-30 from the National Institutes of Health, by a Center of Excellence Grant from the State of Tennessee, and by the American Lebanese Syrian Associated Charities (ALSAC).
Glossary
- TS ATP
Time Sensitive Adherence Tracking Procedure
- ALL
Acute Lymphoblastyc Leukemia
Footnotes
Conflict of interest statement: The authors have no conflict of interest to declare.
REFERENCES
- 1.Mostert S, Arora RS, Arreola M, Bagai P, Friedrich P, Gupta S, Kaur G, Koodiyedath B, Kulkarni K, Lam CG, Luna-Fineman S, Pizer B, Rivas S, Rossell N, Sitaresmi MN, Tsimicalis A, Weaver M, Ribeiro RC. Abandonment of treatment for childhood cancer: position statement of a SIOP PODC Working Group. The Lancet Oncology. 2011;12(8):719–720. doi: 10.1016/S1470-2045(11)70128-0. [DOI] [PubMed] [Google Scholar]
- 2.Spinetta J, Masera G, Eden T, Oppenheim D, Martins A, van Dongen Melman J, Siegleret M, Eiser C, Weyl Ben Arush M, Kosmidis HV, Jankovic M. Refusal, non compliance, and abandonment of treatment in children and adolescents with cancer. A report of the SIOP Working Committee on Phychosocial Issues in Pediatric Oncology. Medical and Pediatric Oncology. 2002;38(2):114–117. doi: 10.1002/mpo.1283. [DOI] [PubMed] [Google Scholar]
- 3.Lam C, Rossell N, Ribeiro R. Global snapshots of treatment abandonment in children and adolescents with cancer: social factors, implications and priorities. Journal of Healthcare, Science and the Humanities. 2012;2:81–110. [Google Scholar]
- 4.Arora RS, Pizer B, Eden T. Understanding refusal and abandonment in the treatment of childhood cancer. Indian Pediatrics. 2010;47:1005–1010. doi: 10.1007/s13312-010-0172-5. [DOI] [PubMed] [Google Scholar]
- 5.Mostert S, Gunawan S, Wolters E, van de Ven P, Sitaresmi M, van Dongen J, Veerman A, Mantik M, Kaspers G. Socio-economic status plays important role in childhood cancer treatment outcome in Indonesia. Asian Pacific Journal of Cancer Prevention. 2012;13(12):6491–6496. doi: 10.7314/apjcp.2012.13.12.6491. [DOI] [PubMed] [Google Scholar]
- 6.Butow P, Palmer S, Pai A, Goodenough B, Luckett T, King M. Review of adherence-related issues in adolescents and young adults with cancer. Journal of Clinical Oncology. 2010;28(32):4800–4809. doi: 10.1200/JCO.2009.22.2802. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Adherence to long-term therapies: evidence for action. In: Sabaté E, editor. Switzerland: World Health Organization; 2003. p. 194. [PubMed] [Google Scholar]
- 8.Coccia PF, Altman J, Bhatia S, Borinstein SC, Flynn J, George S, Goldsby R, Hayashi R, Huang MS, Johnson RH, Beaupin LK, Link MP, Oeffinger KC, Orr KM, Pappo AS, Reed D, Spraker HL, Thomas DA, von Mehren M, Wechsler DS, et al. Adolescent and young adult oncology. Journal of the National Comprehensive Cancer Network. 2012;10(9):1112–1150. doi: 10.6004/jnccn.2012.0117. [DOI] [PubMed] [Google Scholar]
- 9.Kondryn HJ, Edmondson CL, Hill J, Eden TO. Treatment non-adherence in teenage and young adult patients with cancer. The Lancet Oncology. 2011;12(1):100–108. doi: 10.1016/S1470-2045(10)70069-3. [DOI] [PubMed] [Google Scholar]
- 10.Castellano JM, Copeland-Halperin R, Fuster V. Aiming at strategies for a complex problem of medical nonadherence. Global Heart. 2013;8(3):263–271. doi: 10.1016/j.gheart.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Bonilla M, Rossell N, Salaverria C, Gupta S, Barr R, Sala A, Metzger ML, Sung L. Prevalence and predictors of abandonment of therapy among children with cancer in El Salvador. International Journal of Cancer. 2009;125(9):2144–2146. doi: 10.1002/ijc.24534. [DOI] [PubMed] [Google Scholar]
- 12.Kumar A, Moulik NR, Mishra RK, Kumar D. Causes, outcome and prevention of abandonment in retinoblastoma in India. Pediatric Blood & Cancer. 2013;60(5):771–775. doi: 10.1002/pbc.24454. [DOI] [PubMed] [Google Scholar]
- 13.Central Intelligence Agency. The world factbook. [[cited 2013 19 October]]; Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/es.html.
- 14.Israëls T, Chirambo C, Caron H, de Kraker J, Molyneux E, Reis R. The guardians' perspective on paediatric cancer treatment in Malawi and factors affecting adherence. Pediatric Blood & Cancer. 2008;51(5):639–642. doi: 10.1002/pbc.21703. [DOI] [PubMed] [Google Scholar]
- 15.Metzger M, Howard S, Fu L, Peña A, Stefan R, Hancock M, Zhang Z, Pui CH, Wilimas J, Ribeiro RC. Outcome of childhood acute lymphoblastic leukaemia in resource-poor countries. The Lancet. 2003;362(9385):706–708. doi: 10.1016/S0140-6736(03)14228-6. [DOI] [PubMed] [Google Scholar]
- 16.Li E, Jin R. Causes for refusal or abandonment during treatment of pediatric acute promyelocytic leukemia. Leukemia Research. 2012;36(9):E193–E194. doi: 10.1016/j.leukres.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 17.Brown S, Belgaumi A, Kofide A, Littlechild B, Sabbah R, Ezzat A, Shoukri M, Barr R, Levin A. Failure to attend appointments and loss to follow-up: a prospective study of patients with malignant lymphoma in Riyadh, Saudi Arabia. European Journal of Cancer Care. 2009;18(3):313–317. doi: 10.1111/j.1365-2354.2008.01037.x. [DOI] [PubMed] [Google Scholar]
- 18.Howard SC, Pedrosa M, Lins M, Pedrosa A, Pui C-H, Ribeiro RC, Pedrosa F. Establishment of a pediatric oncology program and outcomes of childhood acute lymphoblastic leukemia in a resource-poor area. JAMA: Journal of the American Medical Association. 2004;291(20):2471–2475. doi: 10.1001/jama.291.20.2471. [DOI] [PubMed] [Google Scholar]