Abstract
Purpose:
To present the descriptive data on the frequency of medical and psychiatric morbidity and also to discuss various pertinent issues relevant to the disaster management, the future challenges and psychosocial needs of the 2013 floods in Uttarakhand, India.
Materials and Methods:
Observation was undertaken by the disaster management team of National Institute of Mental Health and Neurosciences in the worst affected four districts of Uttarakhand. Qualified psychiatrists diagnosed the patients using the International Classification of Diseases-10 criteria. Data were collected by direct observation, interview of the survivors, group sessions, individual key-informant interview, individual session, and group interventions.
Results:
Patients with physical health problems formed the majority of treatment seekers (39.6%) in this report. Only about 2% had disaster induced psychiatric diagnoses. As was expected, minor mental disorders in the form of depressive disorders and anxiety disorders formed majority of the psychiatric morbidity. Substance use disorders appear to be very highly prevalent in the community; however, we were not able to assess the morbidity systematically.
Conclusions:
The mental health infrastructure and manpower is abysmally inadequate. There is an urgent need to implement the National Mental Health Program to increase the mental health infrastructure and services in the four major disaster-affected districts.
Keywords: Disaster, Uttarakhand, psychiatric morbidity
INTRODUCTION
Disasters not only have impact on the morbidity and mortality of the local population but also disrupt progress and destroy the outcome of developmental efforts over several years, often pushing nations’ quest for progress back by several decades.[1] A typical pattern of mental, emotional, and physical response is observed in the majority of people after exposure to any disaster.[2,3] Disasters threaten personal safety, overwhelm defense mechanisms and disrupt community and family structure.[4]
When it comes to the Indian literature on disaster-affected populations, there are few reports from tsunami affected areas of Southern India. For example, psychiatric morbidity was found to be highest in the displaced population after a major disaster. Cohesive community, family systems, social support, altruistic behavior of the community leaders, and religious faith and spirituality were resilience factors that helped survivors cope during the early phase of the disaster.[5,6] Viswanath et al. in 2012[7] reported that the medical and mental health needs of geriatric survivors deserve special consideration and allocation of resources on a priority basis. Another report concludes that women may need to be rehabilitated in their own habitats after major disasters.[8] Pediatric population is another high risk group for development of both physical and mental health morbidity. Math et al.[9] had reported that interventions such as art therapy, informal education, group discussions, dramas, story-telling, activity scheduling, yoga, relaxation, sports/games, providing factual information, and educating parents and teachers can help in a number of ways. These kinds of activities are simple, easy to implement using local resources, effective in all groups and provide important components of psychosocial rehabilitation such as normalizing, stabilizing, socializing, defusing emotions and feelings, sense of identification with others, restoring sense of safety and security, allowing normal healing process and hope for the future. This kind of approach should be started at the earliest targeting almost all the children and adolescents affected by any disaster in developing countries.
Context of the study
The combination of cloud bursts, floods, and landslides triggered on 16 and 17 June 2013 affected most of the 13 districts in Uttarakhand. Magnitude of the disaster prompted people to coin the term Himalayan tsunami for this disaster. Worst hit places were very important Hindu pilgrimage districts namely Rudraprayag, Chamoli, Uttarakashi, and Pithoragarh.
The Government of India designated National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, as the nodal agency for assessing and coordinating the psychosocial relief in this Himalayan tsunami affected region. Accordingly, a multidisciplinary team was deputed to Uttarakhand with the mandate of identifying and treating persons needing immediate interventions and for assessing psychiatric/psychosocial morbidity. The data presented in this study is a part of this community assessment and intervention program during the emergency relief work. It is not a research work, but an observational based report. Post-hoc ethical clearance was obtained for the manuscript from the NIMHANS Ethics Committee.
MATERIALS AND METHODS
Affected population
The disaster management team undertook observation mainly in the worst affected four districts (Rudraprayag, Chamoli, Uttarakashi and Pithoragarh). The team worked for nearly 3 weeks in various districts providing mental health care. Assessments were done considering logistics such as accessibility and representation ability of the affected population. It is to be noted that the affected population can be classified into three groups:
“Pilgrims” visiting the holy places of Uttarakhand from various parts of India
“Local population” who live in these areas and
“Local business population” who visit and stay in these places only during the pilgrimage season for business purposes, but return back to an independent residential places in the planes.
Case-identification
This disaster was unique as substantial proportions of the affected population were pilgrims. Since they were evacuated on a high-priority basis, majority of this population could not be assessed. Considering the logistics, the team visited and did the assessment in all the affected (four) district hospitals, at least one Community Health Center (CHC), Primary Health Centers (PHCs), evacuation centers, relief camps, schools and also communities (visiting the affected villages, which were inaccessible by road). The team used to approach relief camps and contact the medical officer in charge with the request to make an announcement to the inhabitants about the availability of mental health professionals and that the needy could avail clinical services. In the communities, key-informants such as community leaders were approached with the similar request. Their consent and cooperation of the community leaders were essential for community participation and acted as an entry point into the community. The community leaders and local staff announced the availability of mental health professionals. While doing so, they used to give descriptions of common symptoms of psychopathology. During the consultations with the survivors, attempts were also made to identify other cases using the snowball technique. The snowball technique is a special nonprobability method that relies on referrals from initial subjects to generate additional subjects.
Diagnoses
Qualified psychiatrists diagnosed the patients using the International Classification of Diseases-10 criteria. Informed oral consent was obtained from all the subjects. To gather both quantitative and qualitative data, the following strategies were used: Direct observation, interview of the survivors, group sessions, individual key-informant interview, individual session and group interventions. Psychiatrists, psychologists, and psychiatric social workers conducted sessions. The method adopted was mixed to suit the vast nature of the disaster and highly mobile and volatile survivors’ groups. Another issue of note is that this report describes only about axis-1 psychiatric disorders. Various sub-syndromal psychosocial issues have not been included.
RESULTS
In total, 825 subjects were interviewed. Males formed 45% (n = 371) among these. Children (age <12 years) formed 18% (n = 153) of the sample. Mean age (standard deviation) of the entire sample was 30.3 (17.9) years, while it ranged between 6 months and 85 years. 419 of the interviewed persons did not have any diagnosable psychiatric or medical diagnosis.
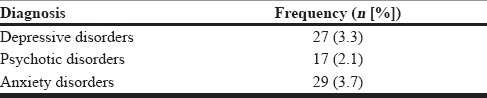
Table 1 gives details of the diagnostic break up among the entire sample. As can be seen, physical health problems were the main concerns for consulting our team. As regards the psychiatric diagnoses, 73/825 (9%) out of the total 825 had axis-1 problems. Depressive disorders (including dysthymia and depressive episodes; n = 27) formed 3.3% of the total diagnoses. Anxiety disorders (including adjustment disorders and posttraumatic stress disorders [PTSD], panic disorder, mixed anxiety and depressive disorder, generalized anxiety disorder, somatoform disorder, obsessive compulsive disorder, dissociative disorder and unspecified anxiety disorder) formed 3.5% (n = 29) of the total, while psychotic disorders (n = 17; including schizophrenia, mania, bipolar affective disorders, cannabis dependence with schizophrenia and unspecified psychosis) accounted for 2.1% of the entire sample. Notably, adjustment disorders and PTSD accounted only for 1.7% of diagnoses of the entire sample and 19% of the psychiatric diagnoses. Table 2 gives details regarding the distribution of psychiatric diagnostic categories. As can be made out, depressive disorders and anxiety disorders were commoner.
Table 1.
Distribution of the diagnoses in the entire sample (n = 825)
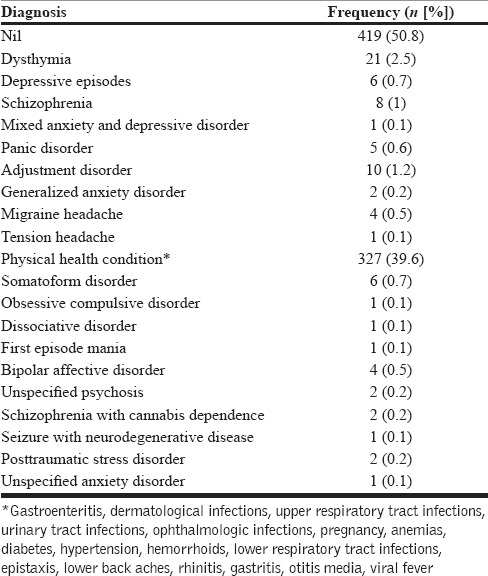
Table 2.
Psychiatric diagnostic categories among the entire sample (n = 825)
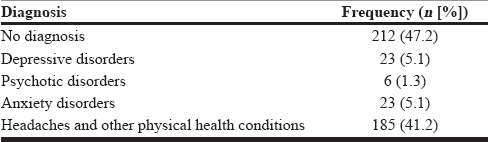
Females significantly outnumbered males in having depressive disorders (23 females; 85% vs. 4 males; 14.8%) as well as anxiety disorders (23 females; 79.3% vs. 6 males; 20.7%) (χ2 = 20.27; P < 0.001). Table 3 gives details for female patients only. Depressive disorders and anxiety disorders together accounted for 10% (46/449) of all the diagnoses and among the psychiatric diagnoses, this group accounted for 75% (52/69) of the cases. Depressive disorders and anxiety disorders were actually present even before the onset of this disaster. Multiple psychosocial issues were acting as the maintaining factors for these: Financial difficulties, substance use in their spouses, lack of stable income, the imminent danger of evacuation every year, no stable arrangements for their children's education, loss of private property, including the household materials, unstable housing arrangements, etc. The disaster had only worsened their problems.
Table 3.
diagnostic categories among female patients (n = 449)
When only children were analyzed, out of the 153, 72 (47.1%) had physical conditions and one child had a neurodegenerative disorder associated with seizures. Notably, none of the children had any diagnosable axis-1 psychiatric disorder.
DISCUSSION
Important findings of this observational report were: The disaster-affected population had considerable physical and mental morbidity. With regard to mental health morbidity, disaster had a causal effect in only a minority of the proportion of the mental disorders (adjustment disorder and PTSD accounted for only about 2% of the entire sample). We would like to discuss further taking into account, the definition of “health” as given by World Health Organization.
Physical health
Patients with physical health problems formed the majority of treatment seekers in this report. This is understandable, considering the nature of the disaster and the living arrangements these people had during the time of the assessments: Immediate aftermath of the disaster, ravaged homes, prevailing psychosocioeconomic situation of the majority of locals, make-shift relief camps, over-crowding of these camps, lack of hygienic supply of potable water, etc.: Understandably, majority of these physical health conditions were infective in origin affecting the respiratory and gastrointestinal system. No efforts should be left behind in reaching out to those in needs, considering the eminently preventable and treatable nature of these physical problems. Efficient public health methods in collaboration with the local community team members such as ASHA workers and PHC staff can effectively handle this menace.
Mental health
As was expected, minor mental disorders formed the majority. Though, the percentages do not compare with the epidemiological data, the nature of sampling and the timing of the assessment precludes such strict comparisons. Nevertheless, the pattern of psychiatric morbidity points towards the same direction as given by the psychiatric epidemiology findings.[10,11] Another point is that these disorders were preexistent and the disaster had only worsened the situation. Only about 2% had disaster induced psychiatric diagnoses. There could be a couple of reasons for this particular phenomenon: First, the disaster was not totally unexpected for the local population as some life and property loss is an occurrence every year during the monsoon. Furthermore, this time, the timing of the disaster was during morning time giving enough time for people to escape. This was in contrast to the situation last year where the disaster struck during midnight causing considerably more deaths of the locals. Second, our sample consisted of locals while significant life damage might have occurred among the pilgrimage population. Since these were evacuated, our estimate could be an underestimate. This does not mean that the locals did not have any psychosocial morbidity induced by the disaster. Many in fact had sub-syndromal symptoms, which were not systematically collected. Third, many protective factors such as resilience, spirituality etc., could have played a part. Fourth, the team observed that a considerable minority of the people from the riverbeds had moved on to another of their abodes at a safer distance (in the planes). This issue led to a situation where in the survivors we interviewed comprised predominantly of the economically weaker section of the society which did not have the resources to construct extra homes/places of living. These persons had morbidity even from the beginning secondary to various other life-situations rather than getting affected exclusively by the disaster. Whatever the situation, the most striking issue was the severe dearth of mental health manpower in the entire state. This issue requires urgent attention. Another important issue about this report is the absence of data on substance use disorders (SUDs). Though, SUDs appear to be very highly prevalent in the community (this conjecture is derived from speaking to the all grades of stake holders such as women and children in the community, village health workers, doctors in PHCs, CHCs, pharmacists, community leaders and officials from the taluk and district health administration), we were not able to assess the morbidity as the information was extremely unreliable and invalid. Most of them used to deny substance use, while other sources of information regarding the same individual indicated otherwise. In this connection, it is to be noted that there are no intervention or treatment or rehabilitation centers available across the entire state of Uttarakhand. There are only few de-addiction centers run by NGOs or private bodies. There is an urgent need to open de-addiction centers in the district hospitals and expand mental health services through General Hospital Psychiatric Units. Regarding people with severe mental disorders, a large number of wandering mentally ill were seen in the villages and also near these religious places. Use of cannabis seems to be particularly high among the local population. Anti-epileptics, anti-psychotics, anti-depressants and mood stabilizers were not available in any of the district hospitals in the state. This nonavailability of mental health care in district hospitals may have contributed to the wandering mentally ill. The NIMHANS team had a major problem of initiating pharmacotherapy for these persons as there is no system for follow-up and continuation of care for these persons. Strengthening of mental health services for the state needs to give a high-priority in the rehabilitation phase of the disaster.
The mental health infrastructure and manpower is abysmally inadequate as. There is an urgent need to upgrade the current 30 bedded mental hospital to a 100 bedded mental health institution with teaching facility in mental health.
Further, National Mental Health Program (NMHP) has not implemented even in a single district of the state. This issue also needs to see the light of the hour.
Social well-being
One major issue in this disaster is the landslide and the consequent damages caused to the roads, which makes the connectivity to various forward areas a major problem. In the initial days after the disaster, the entire connectivity was cut off. Choppers were the only means of connectivity through which relief and rehabilitation materials were supplied. For the locals, the issue of continuous connectivity (to the outside world) is the only means of survival as all aspects of life is dependent on this connectivity and each and every dimension of their life would get affected adversely otherwise. Basic life requirements such as regular supply of ration, cooking gas, petrol and other essentials also get hit if the connectivity is lost. Most of the houses on the banks of the river were fully or partially destroyed. Some of the hotels were totally washed away. The loss in terms of the houses and the livelihood would never ever be recovered. It would be better to think on long-term soft loans with low interest for them to rebuild the lives.
The event has a major impact on the education of the children. There is a need to assist these children to continue education in spite of the difficult situation they have gone through. The girl children need to be concentrated as the families are thinking of them to drop out to assist the boys going to school. Most of these families are sending the child to the valley for higher education with larger fees and other financial implications. Waiver of the fee for the children in both the government and private schools would do a lot better for these children to continue education.
Major income of the Uttarakhand state is through religious tourism. Drastic decline in the number of pilgrims would cause a large of impact and distress among the local population. There is a need for NGO-involvement in providing support to alternative livelihood for these survivors.
Limitations
This observational report has certain limitations: Information was derived from records of clinical interventions and assessment carried out during the early phase of the disaster. The assessments using structured instruments and rigorous sampling methods could not be carried out. The nature of the study is observational, which overrules the measure of actual research design results. Only patterns of morbidity have been identified. However, the main strength of the results is that qualitative reporting, individual case based reporting and involvement of the community leaders and the survivors
Future plans
Families with life loss among the pilgrims need to be followed-up for prevention of emergence of long-term mental health issues through the Institutes of Mental Health in the respective states. Dedicated telemedicine services needs to be installed across the state in all district hospitals, CHCs and PHCs. The aim should be to provide specialist consultation, monitoring national programs, health services and training purposes. Implementation of NMHP and life skills education for school children with disaster preparedness is highly essential. Initiation of de-addiction units across the state in district hospital is a must. There are large number of altruistic religious service providers in the form of ashrams and temple committees in various religious places of the state. These need to be screened and bought into the mainstream psychosocial support care network.
ACKNOWLEDGMENTS
Disaster team members are thankful to Departments of Health and Family Welfare, New Delhi for deputing and providing logical support for providing relief work for the survivors. We also thank the staff of National Disaster Management Authority, New Delhi for their constant support. The authors are grateful to the Departments of Health and Family Welfare, and Social Welfare of the Uttarakhand.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.New Delhi: Published by Ministry of Home Affairs, Government of India; 2013. [Last visited on 2013 Nov 02]. NDMA G. State Level Programmes for Strengthening Disaster Management in India, 2011. Available from: http://www.ndmindia.nic.in/DMBooklet-080211.pdf . [Google Scholar]
- 2.Carol SN. Psychiatric epidemiology of disaster responses. In: Ursano RJ, Norwood AE, editors. Trauma and Disaster, Responses and Management. Review of Psychiatry Series. Vol. 22, No. 1. Washington, DC: American Psychiatric Publishing, Inc; 2003. pp. 35–62. [Google Scholar]
- 3.Geneva: WHO; 1992. World Health Organization. Psychosocial Consequences of Disaster – Prevention and Management. WHO. MNH/PSF/91.3 Rev.1. [Google Scholar]
- 4.Lubit R, Eth S. Children, disasters, and the september 11th world trade center attack. In: Ursano RJ, Norwood AE, editors. Trauma and Disaster, Responses and Management, Review of Psychiatry Series. Vol. 22. No. 1. Washington DC: American Psychiatric Publishing, Inc; 2003. pp. 63–96. [Google Scholar]
- 5.Math SB, John JP, Girimaji SC, Benegal V, Sunny B, Krishnakanth K, et al. Comparative study of psychiatric morbidity among the displaced and non-displaced populations in the Andaman and Nicobar Islands following the tsunami. Prehosp Disaster Med. 2008;23:29–34. doi: 10.1017/s1049023x00005513. [DOI] [PubMed] [Google Scholar]
- 6.Sundram S, Karim ME, Ladrido-Ignacio L, Maramis A, Mufti KA, Nagaraja D, et al. Psychosocial responses to disaster: An Asian perspective. Asian J Psychiatr. 2008;1:7–14. doi: 10.1016/j.ajp.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Viswanath B, Maroky AS, Math SB, John JP, Benegal V, Hamza A, et al. Psychological impact of the tsunami on elderly survivors. Am J Geriatr Psychiatry. 2012;20:402–7. doi: 10.1097/JGP.0b013e318246b7e9. [DOI] [PubMed] [Google Scholar]
- 8.Viswanath B, Maroky AS, Math SB, John JP, Cherian AV, Girimaji SC, et al. Gender differences in the psychological impact of tsunami. Int J Soc Psychiatry. 2013;59:130–6. doi: 10.1177/0020764011423469. [DOI] [PubMed] [Google Scholar]
- 9.Math SB, Tandon S, Girimaji SC, Benegal V, Kumar U, Hamza A, et al. Psychological impact of the tsunami on children and adolescents from the Andaman and Nicobar islands. Prim Care Companion J Clin Psychiatry. 2008;10:31–7. doi: 10.4088/pcc.v10n0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Math SB, Chandrashekar CR, Bhugra D. Psychiatric epidemiology in India. Indian J Med Res. 2007;126:183–92. [PubMed] [Google Scholar]
- 11.Chandrashekar CR, Math SB. Psychosomatic disorders in developing countries: Current issues and future challenges. Curr Opin Psychiatry. 2006;19:201–6. doi: 10.1097/01.yco.0000214349.46411.6a. [DOI] [PubMed] [Google Scholar]


