Abstract
Background:
Resistance to pharmacotherapy is one of the major challenges in the management of obsessive-compulsive disorder (OCD). OCD being a quite prevalent disorder, this resistance adds to the disability. Different strategies are being employed to counter this resistance, one of them being augmentation with glutamatergic modulators. Lamotrigine is being used for same since the recent past with mixed results.
Objective:
The aim was to study the role of lamotrigine augmentation in serotonin reuptake inhibitor (SRI) resistant OCD patients.
Methodology and Results:
This study was carried by studying the case sheets of SRI resistant cases having already completed the treatment. A total of 22 cases sheets over 2 years met the study criteria with a mean age of mean age of 34.14 years. Over a period of 16 weeks, with a mean lamotrigine dose of 150 mg/day, 20 out of 22 patients had shown a significant response. The mean decrease in Yale-Brown Obsessive Compulsive Scale score was 67.23% with a baseline score of 28.87. There was a similar change on different domains of World Health Organization quality of life (P = 0.00564).
Conclusion:
Lamotrigine augmentation to on-going treatment with SRIs may be an effective move in case of SRI resistant OCD patients.
Keywords: Augmentation, lamotrigine, obsessive-compulsive disorder, serotonin reuptake inhibitor resistance
INTRODUCTION
Obsessive-compulsive disorder (OCD) is a chronic, disabling disorder affecting 2-3% of the general population.[1] Serotonin reuptake inhibitors (SRIs) which include clomipramine and selective SRIs (SSRIs), are being considered the first line of pharmacological treatment in this disorder as is supported by the literature.[2,3,4] However, the majority (40-50%) of patients are resistant to this mono-therapeutic treatment approach which poses a major issue in the management of OCD.[5] Current options for such treatment-resistant OCD include switching to an alternative SSRI or augmentation with dopamine antagonists or other agents or cognitive-behavioural therapy.[6] When such options are not suitable, available or effective, augmentation of the on-going SSRI with another compound represents the preferable strategy.[5]
Apart from the monoaminergic dysfunction that forms the basis of present day treatments in OCD, several evidences suggest that abnormalities of other neurotransmitters may have a role in the pathophysiology of OCD. Evidence from genetic, behavioral, and neuroimaging studies have shown the abnormally high glutamatergic concentrations in caudate nucleus of patients in OCD.[7] Moreover this evidence has led to the hypothesis that glutamate modulating drugs may be a suitable treatment option for patients with SRI-resistant OCD.[8,9]
Lamotrigine, an antiepileptic drug and a mood stabilizer, also having anti-glutamanergic properties has been occasionally has been occasionally used in OCD treatment.[10] Two small open studies used lamotrigine for treating obsessive symptoms, one in schizophrenia and another in bipolar disorder.[11,12] A small open study of augmentation of SRIs with 100 mg/day of lamotrigine in eight patients reported negative results.[13] A case report of lamotrigine augmentation using up to 150 mg/day in a patient with a stable dose of clomipramine (225 mg/day) described a remarkable improvement.[14] A 16 weeks double-blind, randomized, and placebo-controlled trial of lamotrigine augmentation (up to 100 mg/day) in patients receiving SSRIs has shown positive results at large.[15]
To the best of our knowledge, there is no study from South Asia contesting the role of lamotrigine augmentation in SRI resistant OCD. With this aim in mind and the recent data showing an association between decreased caudate glutamatergic concentrations and a reduction in OCD symptoms, we initiated an investigation of adjunctive lamotrigine in treatment-resistant OCD.
MATERIALS AND METHODS
The study included a retrospective chart review of a consecutive series of patients over a period of 2 years diagnosed with Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) OCD, and was treated at the Department of Psychiatry, Government Medical College, Srinagar, Jammu and Kashmir, India. Only those case sheets were reviewed, which were complete and met the requirements of the review. All patients were evaluated by a consultant psychiatrist using a semi-structured clinical interview for DSM-IV diagnosis to determine Axis I diagnoses. Patients were considered to be treatment-resistant if they were nonresponsive or partially responsive to an adequate trial (14 weeks) of open, flexible-dose treatment of an SRI at maximal doses (fluoxetine 80 mg/day, paroxetine 60 mg/day, fluvoxamine 300 mg/day, clompiramine 250 mg/day, or sertraline 200 mg/day) or to highest dose tolerated.[15]
Patients having any other primary Axis I psychiatric diagnosis were not included in this review; that is, OCD must be the disorder that caused the most disability and impairment to the patient. Patients taking concurrent benzodiazepines, antipsychotics, sedative hypnotics, or antidepressant medications were not excluded from this case series provided that they had been on a stable dose of these medications for at least 8 weeks prior, and had not changed the dose of the concurrent medication over the course of the treatment period. Lamotrigine was started at dose of 25 mg/day and gradually increased to 200 mg by 8 weeks with weekly increment of 25 mg. The SRI was continued, and the doses were changed minimally were needed. Lamotrigine was stopped in some patients owing to the development of rash. In total 22 patients who had completed follow-up for a minimum of 16 weeks were assessed for this study. This study included in-patients as well as out-door patients.
The progress of symptoms was assessed using Yale-Brown Obsessive Compulsive Scale (YBOCS) symptom checklist and severity rating scale which is a 10 item scale with scores varying from 0 to 4 for each item with a high validity and reliability.[16]
The general wellbeing and quality-of-life (QoL) was assessed using the World Health Organization (WHO)-QoL (BREF version). The WHO-QoL (BREF version) is a 26-item self-administered questionnaire, which emphasizes the subjective responses of patients in physical, psychological, environmental and social domains. The score for each domain was computed on a 0-100 scale. The psychometric property is comparable to that of the full version of WHO-QoL.[17]
The data were tabulated, and the individual results of the cases were studied statistically. Mean/average and the deviations were calculated using the latest version of Statistical Package for Social Sciences. Chi-square tests were applied to study the change in scores. Statistical significance was set at P < 0.05.
RESULTS
Twenty-two patients met the selection criteria, having a complete follow-up with fully maintained case sheets along with relevant rating scales. The sample included 14 males and 6 females with a mean age of 34.14 ± 5.66 years (22-52 years). The mean duration of illness was 15.82 ± 5.87 years (5-30 years). Before the initiation of lamotrigine, the mean YBOCS score was 28.87 suggesting a severely ill state of most of these patients [Table 1]. This was further evident from the mean baseline score of the different domains of WHO-QoL viz., 51.77, 51.45, 53.95, 56 for physical, psychological, social, environmental respectively [Table 2]. Other variables, treatment history and treatment response, are noted in Table 1.
Table 1.
Clinical profile and YBOCS score
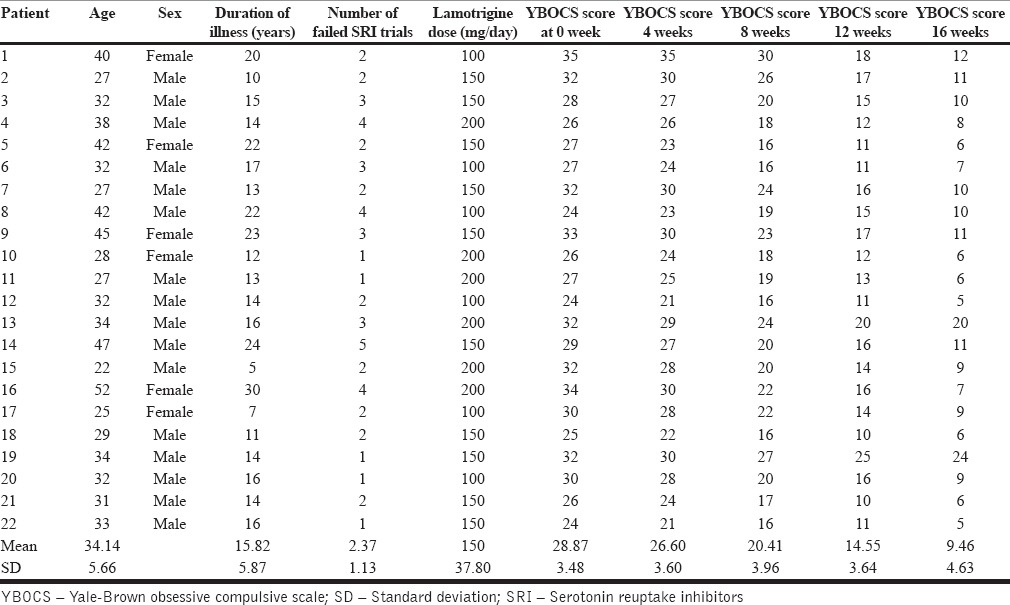
Table 2.
WHO-QoL scores
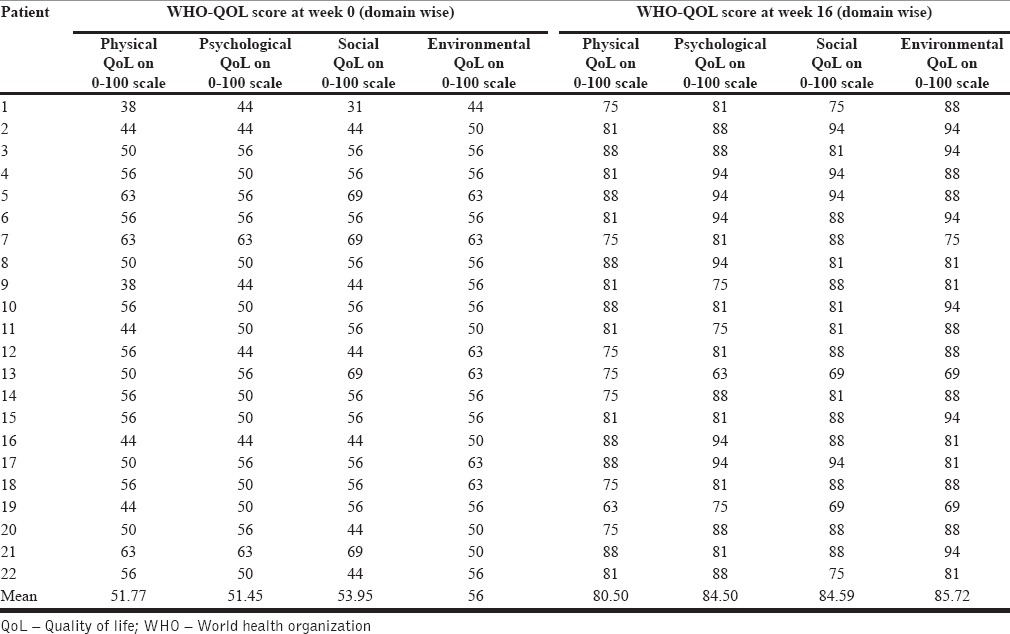
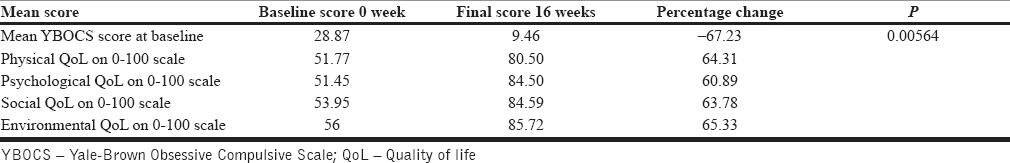
All the patients were treated at least 16 weeks of lamotrigine augmentation among whom twenty showed a significant response and two of them did not respond. A significant change of more than 60% was seen both in YBOCS and WHO-QoL (P = 0.00564) [Table 3]. The endpoint mean score for YBOCS was 9.46 and the mean score for physical, psychological, social and environmental domains of WHO-QoL was 80.50, 84.50, 84.59 and 85.72, respectively. Both YBOCS and WHO-QoL showed a significant improvement in overall state of health of these patients.
Table 3.
Change in severity scores
The mean time for responders to achieve a 25% reduction on YBOCS score was 9.2 ± 2.2 weeks at a mean dose of 150 mg/day of lamotrigine. The mean dose of lamotrigine at endpoint was 150 ± 37.8 mg/day, with a dose range of 100-200 mg/day with a 67.23% decline in YBOCS score with 20 (out 22) patients showing a full response of more than 35% reduction in scores.
Augmentation of lamotrigine was carried on the different SRIs, which included fluvoxamine, sertaline, clomipramine and escitalopram, but due to the small number of subjects, statistical analyses were not feasible to evaluate differences between subgroups. The combination of lamotrigine-SRIs was generally well-tolerated. A few adverse effects were documented which included headache (three patients), sedation (four patients), fatigue (one patient), and benign skin rash (one patient). These effects were generally mild and transient and did not force discontinuation.
DISCUSSION
This case series provides a basic evidence for the potential effectiveness of lamotrigine augmentation in patients with OCD who are refractory to standard SRI therapy. There are, however, obvious limitations to the presented data, including a retrospective case series design, small sample size, and reliance on case sheets. However, the use of a specific scale for OCD (YBOCS), WHO-QoL and continuous follow-up make a strong case to bet on its results.
The results obtained from the present study indicate that lamotrigine added to stable SRIs treatment substantially improved obsessive-compulsive symptoms in patients who were resistant to SRI alone. A mean 67.23% reduction in YBOCS total score was observed at the end of 16 weeks of adjunctive lamotrigine. The rate of responders in our sample was 90.9% when the response criterion of 25% improvement or greater in YBOCS total score was considered; a full response (>35% YBOCS total score reduction) was also observed in the same percentage. The percentage of full responders was more than observed in previously conducted studies.[11,15] The probable reasons of this high response was higher dose of lamotrigine used for a longer duration of time than in the previous attempts. However, a trial of eight patients with OCD refractory to SRI treated with adjunctive lamotrigine, had not shown benefit.[13] However, this negative result could be due to the low doses of lamotrigine used in that study.
There is some evidence that glutamate dysregulation and the subsequent glutamanergic modulation by lamotrigine may explain this therapeutic relationship. There are similar evidences with regard to efficacy of other glutamanergic modulators such as riluzole and topiramate in the management of refractory OCD.[8,18,19] Further the augmenting role of lamotrigine by glutamanergic modulation is supported indirectly by the fact that SRIs may indirectly attenuate glutamatergic activity through inhibitory effect of serotonin on corticostriatal glutamate release.[9]
The clinical phenomenology of OCD in these resistant cases could provide another plausible explanation of this therapeutic benefit. As was observed by authors, features such as diurnal variation in symptom severity, family history of mood disorder, rapid mood changes, rapid popping out from severe illness and predominance of religious and blasphemous obsessions. The response at bipolar doses of lamotrigine further points toward the affect of some of these clinical features in this response-relationship. However, this needs to be studied separately and at a wider clinical sample.
Our study provides evidence that the lamotrigine augmentation to on-going treatment with SRIs may be a beneficial strategy for SRI resistant OCD patients. The mechanism behind this anti-obsessional activity looks likely to be multi-pronged synergistic action on neurotransmitter systems involved in obsessional symptoms.[20] However, these results may be interpreted cautiously in view of weakness and strengths already discussed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Koran LM. Quality of life in obsessive-compulsive disorder. Psychiatr Clin North Am. 2000;23:509–17. doi: 10.1016/s0193-953x(05)70177-5. [DOI] [PubMed] [Google Scholar]
- 2.Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB. American Psychiatric Association. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry. 2007;164:5–53. [PubMed] [Google Scholar]
- 3.Soomro GM, Altman D, Rajagopal S, Oakley-Browne M. Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for obsessive compulsive disorder (OCD) Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD001765.pub3. CD001765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stein DJ, Koen N, Fineberg N, Fontenelle LF, Matsunaga H, Osser D, et al. A 2012 evidence-based algorithm for the pharmacotherapy for obsessive-compulsive disorder. Curr Psychiatry Rep. 2012;14:211–9. doi: 10.1007/s11920-012-0268-9. [DOI] [PubMed] [Google Scholar]
- 5.Albert U, Bergesio C, Pessina E, Maina G, Bogetto F. Management of treatment resistant obsessive-compulsive disorder. Algorithms for pharmacotherapy. Panminerva Med. 2002;44:83–91. [PubMed] [Google Scholar]
- 6.Pallanti S, Hollander E, Goodman WK. A qualitative analysis of nonresponse: Management of treatment-refractory obsessive-compulsive disorder. J Clin Psychiatry. 2004;65(Suppl 14):6–10. [PubMed] [Google Scholar]
- 7.Arnold PD, Rosenberg DR, Mundo E, Tharmalingam S, Kennedy JL, Richter MA. Association of a glutamate (NMDA) subunit receptor gene (GRIN2B) with obsessive-compulsive disorder: A preliminary study. Psychopharmacology (Berl) 2004;174:530–8. doi: 10.1007/s00213-004-1847-1. [DOI] [PubMed] [Google Scholar]
- 8.Coric V, Taskiran S, Pittenger C, Wasylink S, Mathalon DH, Valentine G, et al. Riluzole augmentation in treatment-resistant obsessive-compulsive disorder: An open-label trial. Biol Psychiatry. 2005;58:424–8. doi: 10.1016/j.biopsych.2005.04.043. [DOI] [PubMed] [Google Scholar]
- 9.Pittenger C, Krystal JH, Coric V. Glutamate-modulating drugs as novel pharmacotherapeutic agents in the treatment of obsessive-compulsive disorder. NeuroRx. 2006;3:69–81. doi: 10.1016/j.nurx.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burstein AH. Lamotrigine. Pharmacotherapy. 1995;15:129–43. [PubMed] [Google Scholar]
- 11.Poyurovsky M, Glick I, Koran LM. Lamotrigine augmentation in schizophrenia and schizoaffective patients with obsessive-compulsive symptoms. J Psychopharmacol. 2010;24:861–6. doi: 10.1177/0269881108099215. [DOI] [PubMed] [Google Scholar]
- 12.Bisol LW, Lara DR. Improvement of obsessive-compulsive disorder with divalproex and lamotrigine in two patients with bipolar II disorder. Pharmacopsychiatry. 2009;42:37–9. doi: 10.1055/s-0028-1085439. [DOI] [PubMed] [Google Scholar]
- 13.Kumar TC, Khanna S. Lamotrigine augmentation of serotonin re-uptake inhibitors in obsessive-compulsive disorder. Aust N Z J Psychiatry. 2000;34:527–8. doi: 10.1080/j.1440-1614.2000.0751c.x. [DOI] [PubMed] [Google Scholar]
- 14.Uzun O. Lamotrigine as an augmentation agent in treatment-resistant obsessive-compulsive disorder: A case report. J Psychopharmacol. 2010;24:425–7. doi: 10.1177/0269881108098809. [DOI] [PubMed] [Google Scholar]
- 15.Bruno A, Micò U, Pandolfo G, Mallamace D, Abenavoli E, Di Nardo F, et al. Lamotrigine augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: A double-blind, placebo-controlled study. J Psychopharmacol. 2012;26:1456–62. doi: 10.1177/0269881111431751. [DOI] [PubMed] [Google Scholar]
- 16.Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–11. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 17.Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 18.Van Ameringen M, Mancini C, Patterson B, Bennett M. Topiramate augmentation in treatment-resistant obsessive-compulsive disorder: A retrospective, open-label case series. Depress Anxiety. 2006;23:1–5. doi: 10.1002/da.20118. [DOI] [PubMed] [Google Scholar]
- 19.Ting JT, Feng G. Glutamatergic synaptic dysfunction and obsessive-compulsive disorder. Curr Chem Genomics. 2008;2:62–75. doi: 10.2174/1875397300802010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGrath MJ, Campbell KM, Parks CR, Burton FH. Glutamatergic drugs exacerbate symptomatic behavior in a transgenic model of comorbid Tourette's syndrome and obsessive-compulsive disorder. Brain Res. 2000;877:23–30. doi: 10.1016/s0006-8993(00)02646-9. [DOI] [PubMed] [Google Scholar]


