Abstract
Rationale: Physicians self-report high adherence rates for Ask and Advise behaviors of tobacco dependence treatment but are much less likely to engage in “next steps” consistent with sophisticated management of chronic illness. A variety of potential explanations have been offered, yet each lacks face validity in light of experience with other challenging medical conditions.
Objective: Conduct a preliminary exploration of the behavioral economics of tobacco treatment decision-making in the face of uncertain outcomes, seeking evidence that behaviors may be explained within the framework of Prospect Theory.
Methods: Four physician cohorts were polled regarding their impressions of the utility of tobacco use treatment and their estimations of “success” probabilities. Contingent valuation was estimated by asking respondents to make monetary tradeoffs relative to three common chronic conditions.
Measurements and Main Results: Responses from all four cohorts showed a similar pattern of high utility of tobacco use treatment but low success probability when compared with the other chronic medical conditions. Following instructional methods aimed at controverting cognitive biases related to tobacco, this pattern was reversed, with success probabilities attaining higher valuation than for diabetes.
Conclusions: Important presuppositions regarding the potential “success” of tobacco-related patient interactions are likely limiting physician engagement by favoring the most secure visit outcome despite the limited potential for health gains. Under these conditions, low engagement rates would be consistent with Prospect Theory predictions. Interventions aimed at counteracting the cognitive biases limiting estimations of success probabilities seem to effectively reverse this pattern and provide clues to improving the adoption of target clinical behaviors.
Keywords: tobacco dependence treatment, physician education, behavioral economics, cognitive bias, prospect theory
The evidence that the advice and support delivered by healthcare professionals to smokers achieves abstinence rates of 5 to 10% with minimal interventions and 15 to 30% with more intense interventions is well established (1–3). Given that the United States suffers 480,000 annual deaths related to tobacco and that nearly 80% of adults have contact with the healthcare system each year, a more seamless integration of tobacco use treatment principles into the healthcare context has enormous potential to affect the health of the population (4–6). However, the degree to which physicians have adopted evidence-based treatment recommendations has been suboptimal (7–10).
Primary care physicians self-report high adherence rates for Ask and Advise behaviors (11, 12). However, even when these steps are confirmed, physicians do not generally engage in the “next steps” consistent with the sophisticated management of a chronic illness (13). A variety of potential explanations have been offered, including prohibitive time requirements, perceived treatment ineffectiveness, disinterest among patients, lack of self-efficacy, an unestablished moral responsibility to treat, and absent reimbursement (14–16). These appear to have been accepted as intransigent barriers to practice change, despite lacking face validity, given that they have not been claimed as relevant to other, even more challenging aspects of medical care (17–20).
It is clear that physicians understand tobacco use to be a significant contributor to disease and disability and that they recognize their unique role in promoting abstinence (11, 21). If this is the case, classical economic theories of decision-making based on “maximized utility” would predict very high rates of physician engagement (22). An alternative proposition might account more fully for the impact of emotions and presuppositions on the physician’s decision-making, particularly under conditions of uncertainty (Box 1) (23). When decisions are made in the face of uncertain outcomes, decision-makers balance the need to minimize the risk of losing their “investment” against the need to maximize the probability of a successful outcome (24). Tversky and Kahneman’s Prospect Theory further refines the role of context in decision-making, suggesting that people are intuitively attracted to secure, highly likely outcomes when considering the value of a proposition to themselves while conversely reporting attraction to high gain options, despite lower probabilities of success, when considering the expected value to the community at large (25). Within this framework, decision-making can be viewed as the complex product of the counterbalancing concerns of utility (U) (i.e., the perceived value to self or others) and probability (P) of success or reward.
Box 1: An example of prospect theory in practice
Imagine a circumstance of finite resources, a budgetary restriction that limits spending for clinical equipment, for example. Suppose further that meeting all of your clinic’s equipment needs would require spending an amount in excess of the budget limit. How would you choose which piece(s) of equipment to buy? Earlier economic theory of “choice”—in this case consumer choice—was based on the notion that decision makers in this situation would create a list of required items, existing solely within the individual’s mind and rank-ordered by the degree to which the commodity was essential to the operation of the clinic, and would proceed to invest equipment resources in the order that maximizes the clinic’s productivity. The equipment with the greatest utility would be the logical first investment.
Now suppose that your familiarity with each of the required equipment pieces is not equal. Suppose it differs enough to make you concerned about your ability to use a given piece effectively. Introducing uncertainty into the purchasing decision has the potential to significantly alter your investment choice. Under these conditions, you might forego the piece with the greatest utility and instead choose to invest in the piece with the highest success probability because this choice is likely to have the best potential return on investment for your clinic. This reversal in position is likely to have a substantive effect on outcome.
The value placed on each piece of equipment is a complex internal integration of the balance between perceived utility and success probability. Because both utility and success probability are only internally known, it is difficult for an outside observer to predict in advance how real-life decisions will end. Prospect Theory states that people make decisions based on perceived losses and gains, rather than on final outcome, and that their estimations of loss/gain are influenced by predictable heuristics or mental shortcuts. Cognitive biases are commonly used heuristics, which are often adaptive but can sometimes lead to maladaptive distortions in judgment.
We hypothesize that a physician’s decision to cross the threshold of engagement during an office visit may be best understood within the framework of Prospect Theory rather than as a maximized utility function. If true, we would expect to see a pattern of high perceived success probability for conditions that are routinely treated in the clinic but low success probability estimates for conditions that are not, despite the relative perceived utility of these treatments to the community. We conducted a preliminary exploration of the behavioral economics of tobacco treatment decision-making and evaluated the potential for an educational approach based on these insights to influence these elements of choice construction.
Methods
In preparation for The Philadelphia COPD Initiative, a Department of Public Health effort to disseminate resources to physicians and patients promoting the treatment of tobacco dependence among primary care practitioners in Philadelphia’s low-income communities, four mutually exclusive, convenience samples of physicians (sample cohorts) were polled in an effort to understand their impressions of the baseline utility of tobacco use treatment and their perceptions of “success” probabilities (26). Because money is a universal medium of exchange, one traditional way of measuring value is to ask respondents to provide monetary figures as an expression of their values. Monetary values for nonmarket items, such as change in disease burden within a community, are usually elicited using contingent valuation (i.e., asking respondents to make tradeoffs within a hypothetical market situation) (27). Hypertension (HTN) and type II diabetes mellitus (DM) were chosen as tobacco use (TOB) comparator conditions because of their universal familiarity and their similar requirements for chronic management and control.
Beliefs regarding illness causation and patient culpability in the matter can influence willingness to invest effort in help giving (28). To help control for this effect, we standardized valuations for both HTN and TOB against the DM referent because, of the three conditions, DM and TOB were most likely to be subject to similar presumptions of controllability. In this manner, standardized values for the utility and success probability of TOB (UTOB/DM and PTOB/DM) and HTN (UHTN/DM and PHTN/DM) could be calculated. Standardized valuation can then be interpreted as though respondents reported “For every dollar of value I assigned to diabetes, I assigned ____ dollars of greater/lesser value to tobacco (or hypertension).”
Two of the four cohorts were also exposed to training regarding principles of tobacco dependence treatment to estimate the impact of education on valuations. Training content included standard instructional material derived from U.S. Public Health Service treatment guidelines (1). In addition, four important cognitive biases were identified a priori as having the potential to affect perceptions of success probabilities. Instructional methods were designed to directly controvert the influence of focusing effect bias, impact bias, omission bias, and availability bias in the process of delivering guideline instruction (Table 1) (23, 29–31). Delivery of instructional content was via 1-hour didactic lectures for cohort 3 and via academic detailing methods for field-based instruction previously described by Soumerai and Avorn (32) and others (34) for cohort 4.
Table 1.
Experience-based techniques for problem solving (heuristics), potentially leading to suboptimal judgments or outcomes related to the treatment of tobacco dependence
| Heuristic | Description | Example |
|---|---|---|
| Availability bias | Recent or memorable events hold exceptional sway in decision-making. | A prior frustration with a patient, reluctant to quit despite significant tobacco-related morbidity, influences the clinician’s subsequent assessment of patients’ likelihood of quitting. |
| Focusing effect bias | Decisions are influenced more by short-term concerns than by long-term goals. | A patient with a history of active smoking and poorly controlled hypertension requires an adjustment to his medication regimen. Initiation of tobacco dependence treatment is forgone in favor of ensuring proper understanding and adherence to antihypertensive medications. |
| Impact bias | Decisions are unduly influenced by inaccurate projections of future states. | A discussion of available tobacco dependence treatments is avoided out of concern over the potential time commitment required or because of the perceived risk of alienating the patient. |
| Omission bias | There was a tendency to prefer inaction in an effort to avoid harm, even when inaction may cause greater harm than action. | Treatment with tobacco dependence pharmacotherapy is avoided because of concerns for possible depressed mood side effects. |
Analysis used a χ2 test of proportions for categorical data, a two-sided paired t test and ANOVA for continuous outcomes, and the Wilcoxon test of paired differences to evaluate pre–post results. Testing was performed using SPSS 21, with P values <0.05 considered statistically significant. No corrections for multiple comparisons were made. The analysis was deemed exempt from review requirements by University and Department of Public Health Institutional Review Boards.
Results
Cohort 1
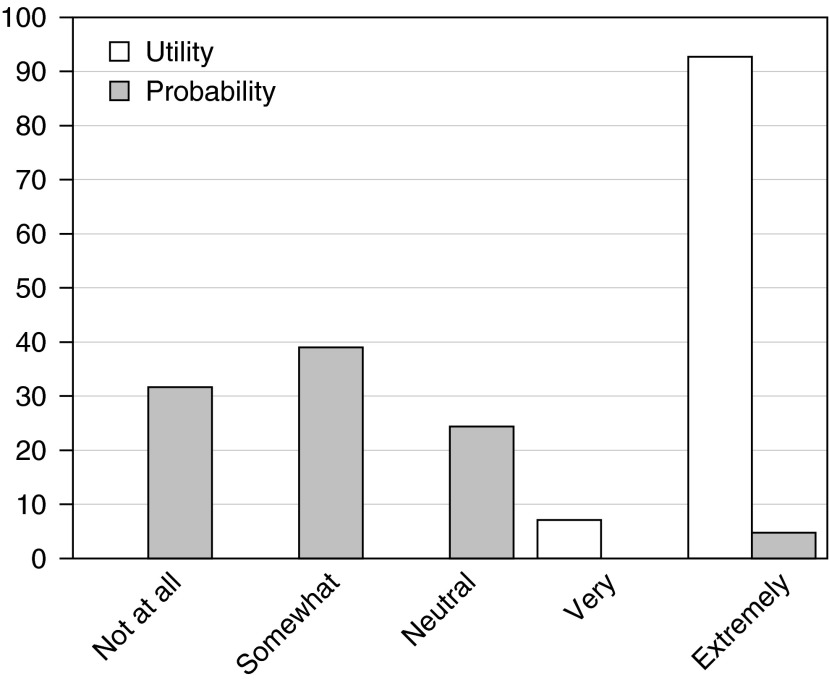
A convenience sample of 42 primary care clinicians from a single academic institution in California were presented with a simple case scenario of an obese, white, 65-year-old woman with chronic obstructive pulmonary disease, hypertension, and type II diabetes. The scenario included a photograph of a well appearing woman wearing nasal cannula oxygen. Clinicians were asked to rate the utility of tobacco use treatment in terms of the importance to the patient’s overall health on a five-point Likert scale, ranging from “not at all important” to “extremely important.” Utility scores averaged 4.95 (range, 4–5), suggesting that clinicians felt tobacco use was extremely important in determining the patient’s outcome (Figure 1). Using the same case details, clinicians were then asked to rate how likely they were to achieve a “successful tobacco interaction” with this patient and were instructed to use any definition of success that they desired. Responses were again collected on a five-point Likert scale, ranging from “not at all likely” to “extremely likely.” Success probability scores averaged only 2.07 (range, 1–5), corresponding to the “somewhat likely” Likert category (P = 0.03)
Figure 1.
Cohort 1 categorical valuation of utility and success probability of a tobacco treatment intervention. Data show a reversal of valuation, with utility rated as “extremely important” (mean score, 4.95) but with success probability rated only “somewhat likely” (mean score, 2.07) (P = 0.03).
Cohort 2
Using a similar case scenario, a second cohort of 63 English-speaking primary care physicians were selected randomly from attendees of an international professional society conference and were asked to distribute a fixed hypothetical investment of $100,000 across three public health priorities in proportion to their anticipated impact on the health of the respondent’s community. Mean utility values (in thousands) assigned were $24.8 for HTN, $35.2 for DM, and $40.2 for TOB (P < 0.001). Respondents were then challenged to “Imagine there are three new patients on your schedule. You are given $100 to bet on the ‘likelihood of a successful interaction’ during this visit. How much would you bet on each patient if the problem is…” and asked to assign a dollar value bet to each of the three conditions. Mean success probability values (in dollars) assigned were $45.4 for HTN, $37.4 for DM, and $16.5 for TOB (within-group ANOVA, P < 0.001; between group χ2, P < 0.001).
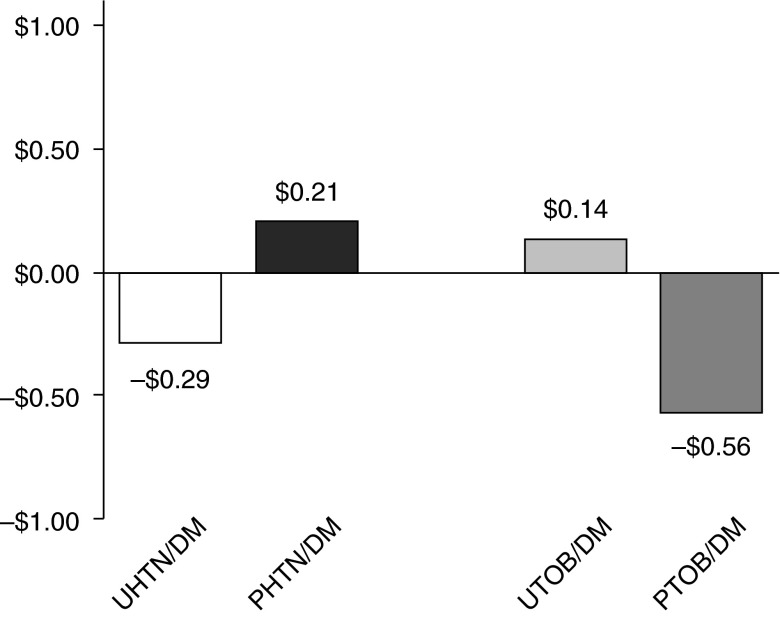
Standardized valuations were calculated and are presented in Figure 2. UTOB was valued at $1.14 for every $1.00 value assigned to UDM (a standardized UTOB/DM value of +$0.14). Conversely, PTOB was valued at only $0.44 for every $1.00 value assigned to PDM (a standardized PTOB/DM value of −$0.56). To ensure that the observed drop in success probability was not a function of chronic illness treatment in general, similar standardized values were calculated for HTN. In comparison, UHTN was valued at $0.71 for every $1.00 value assigned to UDM (a standardized UHTN/DM value of −$0.29), whereas PHTN was valued at $1.21 for every $1.00 value assigned to PDM (a standardized PHTN/DM value of +$0.21) (P < 0.001). The pattern of significantly reduced success probability for tobacco relative to the perceived utility suggests an important reversal may be operant for tobacco but not for hypertension.
Figure 2.
Cohort 2 standardized monetary valuation of utility (U) and success probability (P) for tobacco treatment interventions (TOB) and comparitor hypertension interventions (HTN). Standardized valuation can be interpreted as: “For every dollar of value assigned to diabetes, respondents assigned ____ dollars of greater/lesser value to tobacco (or hypertension).” Mean utility of tobacco interventions was valued 14% higher, and probability of success valued 56% lower, than interventions for diabetes. Data show a reversal of valuation for tobacco interventions, a pattern opposite that observed with hypertension (P < 0.001). DM = type II diabetes mellitus.
Cohort 3
The third cohort consisted of a convenience sample of 12 pulmonologists responsible for the management of chronic obstructive pulmonary disease within an urban academic setting located in the southern United States. Using the same methods used to evaluate cohort 2, this group of pulmonologists revealed a very similar, and significant, reversal. Standardized mean valuations (Figure 3A) were as follows: UTOB/DM +$0.66 while PTOB/DM −$0.14 and UHTN/DM −$0.12 while PHTN/DM +$0.58 (P < 0.001). Two weeks after receiving a 1-hour didactic lecture that included cognitive bias instruction (Figure 3B), the third cohort’s valuation of PTOB/DM had improved significantly to +$0.35 (P < 0.001), becoming statistically indistinguishable from PHTN/DM, which remained steady at +$0.59 (P = 0.66).
Figure 3.
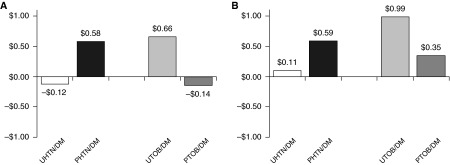
Cohort 3 standardized monetary valuations again show the anticipated reversal of valuation at baseline (A). However, 2 weeks after an educational intervention aimed at overcoming four key cognitive biases (B), valuation reversal for tobacco was no longer apparent (P = 0.66). The educational intervention resulted in a valuation of success probability for tobacco 35% higher than for diabetes and equivalent to that of hypertension. DM = type II diabetes mellitus; HTN = hypertension interventions; P = success probability; TOB = tobacco treatment interventions; U = utility.
Cohort 4
Two academic detailers with experience in public health education were tasked with disseminating high-priority messages about smoking cessation to a group of physicians caring for patients within high smoking prevalence areas of Philadelphia (34, 35). Cohort 4 consisted of the first 100 primary care physicians to receive an academic detailing visit as part of this effort. Seventy-six physicians (76%) completed follow-up assessments 2 months after receiving academic detailing instruction. Respondents estimated the prevalence of tobacco use in their communities to be 41% on average. Valuations made before instruction (Figure 4A) again confirmed a significant reversal, with mean UTOB/DM +$2.23 while PTOB/DM −$0.01 and UHTN/DM −$0.03 while PHTN/DM +$1.54 (P < 0.001).
Figure 4.
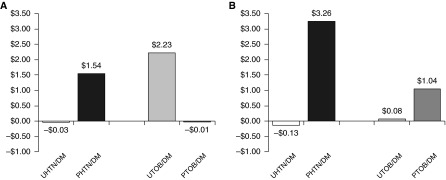
Cohort 4 physicians displayed a similar reversal pattern, with magnitudes of the standardized monetary valuations much higher than in previous cohorts (A). Two months after an academic detailing intervention aimed at overcoming four key cognitive biases (B), reversal was no longer apparent (P = 0.45). The educational intervention resulted in a valuation of success probability for tobacco more than double that for diabetes. DM = type II diabetes mellitus; HTN = hypertension interventions; P = success probability; TOB = tobacco treatment interventions; U = utility.
After instruction (Figure 4B), standardized PTOB/DM values rose dramatically to +$1.04 and were no longer statistically different from mean PHTN/DM, which had risen to +$3.26 (P = 0.45). The precipitous drop in success probability for tobacco relative to utility observed before instruction was no longer observed at follow-up 2 months later. Results were not associated with geographic location of practice, practice type, or the physician’s a priori estimate of tobacco use prevalence within the practice community.
Conclusions
In general, the complex executive functions of medicine make reliance on intuition for decision-making highly likely (36). Although intuitive thinking may be useful, there are a number of identified ways in which intuition may lead to decisions that may be counterproductive (37). Our experience appears to shed an important light on the factors that may be underpinning decisions about tobacco use treatment in the clinic and may provide useful clues as to how to improve rates of behavior change and guideline uptake.
First, prior observations that physicians see the value of tobacco use treatment to the community was confirmed in all four cohorts. Furthermore, we have identified that physicians value TOB quite highly, even when considered relative to the impact of DM on their community. One of the most surprising findings was the UTOB/DM value of $2.23 identified in cohort 4. This is an astounding figure that suggests this cohort feels that tobacco interventions could have over three times the health impact on their community as diabetes interventions.
Second, our observations suggest that physicians value the probability of success for tobacco treatment interventions quite a bit lower. This may be because tobacco use treatment requires input and cooperation from the patient—factors that the physician cannot control. However, the low valuation persists even when responses are standardized against diabetes, another condition that requires significant patient input. If physicians’ presupposed values for PTOB really are this low, then Prospect Theory would predict that physicians would preferentially pursue the most secure outcomes despite recognition of the lower expected gain. We believe that the observed consistency of direction and magnitude of the “flipped” relationship between utility and success probability is likely a crucial point, which must be better understood if progress is to be made helping clinicians adopt complex tobacco treatment behaviors required for longitudinal, adaptive models of chronic illness management.
Finally, it appears that educational training may be used to resolve low expectations for successful tobacco treatment interventions. Our training methods focused on undermining four cognitive biases identified a priori as having the greatest potential to affect estimates of success probability. It remains to be seen which biases have the greatest impact on valuation or whether alternative educational objectives are equally effective. Our observations suggest that the effect of bias training may be scalable and deliverable to large numbers of practicing physicians in the field by nonphysician academic detailers. The effect of bias training appears to be significant, predictable, and sustainable. It also remains to be seen, however, whether the improvement in perceived success probabilities translates directly into behavior change or whether additional training elements are required to effect change.
Should future studies confirm the behavioral economics of tobacco treatment decision-making, perhaps using a range of methods within a variety of contexts, these insights might inform a novel approach to ensuring healthcare systems reach their fullest potential in the worldwide effort to eradicate the tobacco epidemic.
Footnotes
This work was supported in part by National Institutes of Health grants R01 CA136888 and P30 CA016520 and by grants from the Pennsylvania Master Settlement Agreement through the PA Department of Health.
Author Contributions: F.T.L. was responsible for conception and execution of the study and manuscript preparation. S.E.-C. was responsible for conception and execution of the study and manuscript preparation. S.G. was responsible for execution of the study and data collection. R.S. was responsible for conception of the study and manuscript preparation.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Fiore M, Jaén CR, Baker TB, Bailey WC, Bennett G, Benowitz NL, Christiansen BA, Connell M, Curry SJ, Dorfman SF, et al. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. [Google Scholar]
- 2.Russell MA, Wilson C, Taylor C, Baker CD. Effect of general practitioners’ advice against smoking. BMJ. 1979;2:231–235. doi: 10.1136/bmj.2.6184.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kottke TE, Battista RN, DeFriese GH, Brekke ML. Attributes of successful smoking cessation interventions in medical practice: a meta-analysis of 39 controlled trials. JAMA. 1988;259:2883–2889. doi: 10.1001/jama.259.19.2883. [DOI] [PubMed] [Google Scholar]
- 4.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health The health consequences of smoking—50 years of progress: a report of the Surgeon General Atlanta (GA)Centers for Disease Control and Prevention; 2014[updated 2014; accessed 2014 Apr 13]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK179276/ [PubMed] [Google Scholar]
- 5.Silagy C, Muir J, Coulter A, Thorogood M, Yudkin P, Roe L. Lifestyle advice in general practice: rates recalled by patients. BMJ. 1992;305:871–874. doi: 10.1136/bmj.305.6858.871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Fam Pract. 1997;14:160–176. doi: 10.1093/fampra/14.2.160. [DOI] [PubMed] [Google Scholar]
- 7.Mowat DL, Mecredy D, Lee F, Hajela R, Wilson R. Family physicians and smoking cessation: survey of practices, opinions, and barriers. Can Fam Physician. 1996;42:1946–1951. [PMC free article] [PubMed] [Google Scholar]
- 8.Wechsler H, Levine S, Idelson RK, Schor EL, Coakley E. The physician’s role in health promotion revisited: a survey of primary care practitioners. N Engl J Med. 1996;334:996–998. doi: 10.1056/NEJM199604113341519. [DOI] [PubMed] [Google Scholar]
- 9.McEwen A, Akotia N, West R. General practitioners’ views on the English national smoking cessation guidelines. Addiction. 2001;96:997–1000. doi: 10.1046/j.1360-0443.2001.9679978.x. [DOI] [PubMed] [Google Scholar]
- 10.McEwen A, West R, Owen L. General practitioners’ views on the provision of nicotine replacement therapy and bupropion. BMC Fam Pract. 2001;2:6. doi: 10.1186/1471-2296-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evers-Casey S. Scottsdale, AZ: Society for Research on Nicotine and Tobacco; 2004. Tobacco-related knowledge and attitudes do not relate to provider self-efficacy. [Google Scholar]
- 12.Association of American Medical CollegesPhysician behavior and practice patterns related to smoking cessation. Washington, DC; c2007[updated 2015; accessed 2015 Mar 8]. Available from: http://www.legacyforhealth.org/4233.aspx
- 13.An LC, Bernhardt TS, Bluhm J, Bland P, Center B, Ahluwalia JS, Foldes SS, Magnan S, Manley M. Treatment of tobacco use as a chronic medical condition: primary care physicians’ self-reported practice patterns. Prev Med. 2004;38:574–585. doi: 10.1016/j.ypmed.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 14.Vogt F, Hall S, Marteau TM. General practitioners’ and family physicians’ negative beliefs and attitudes towards discussing smoking cessation with patients: a systematic review. Addiction. 2005;100:1423–1431. doi: 10.1111/j.1360-0443.2005.01221.x. [DOI] [PubMed] [Google Scholar]
- 15.Park E, Eaton CA, Goldstein MG, DePue J, Niaura R, Guadagnoli E, MacDonald Gross N, Dube C. The development of a decisional balance measure of physician smoking cessation interventions. Prev Med. 2001;33:261–267. doi: 10.1006/pmed.2001.0879. [DOI] [PubMed] [Google Scholar]
- 16.Fiore MC, Baker TB. Smoking cessation treatment and the good doctor club. Am J Public Health. 1995;85:161–163. doi: 10.2105/ajph.85.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smolders M, Laurant M, Verhaak P, Prins M, van Marwijk H, Penninx B, Wensing M, Grol R. Which physician and practice characteristics are associated with adherence to evidence-based guidelines for depressive and anxiety disorders? Med Care. 2010;48:240–248. doi: 10.1097/MLR.0b013e3181ca27f6. [DOI] [PubMed] [Google Scholar]
- 18.Price RA. Association between physician specialty and uptake of new medical technologies: HPV tests in Florida Medicaid. J Gen Intern Med. 2010;25:1178–1185. doi: 10.1007/s11606-010-1415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anonymous; Evidence-Based Care Resource Group. Evidence-based care: 1. Setting priorities: how important is the problem? CMAJ. 1994;150:1249–1254. [PMC free article] [PubMed] [Google Scholar]
- 20.Eisenberg JM. Physician utilization: the state of research about physicians’ practice patterns. Med Care. 2002;40:1016–1035. doi: 10.1097/01.MLR.0000032181.98320.8D. [DOI] [PubMed] [Google Scholar]
- 21.McIlvain HE, Backer EL, Crabtree BF, Lacy N. Physician attitudes and the use of office-based activities for tobacco control. Fam Med. 2002;34:114–119. [PubMed] [Google Scholar]
- 22.Edwards W. The theory of decision making. Psychol Bull. 1954;51:380–417. doi: 10.1037/h0053870. [DOI] [PubMed] [Google Scholar]
- 23.Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185:1124–1131. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- 24.Slovic P. The construction of preference. Am Psychol. 1995;50:364–371. [Google Scholar]
- 25.Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica. 1979;47:263–292. [Google Scholar]
- 26.The Philadelphia COPD Initiative. c2011 [updated 2014; accessed 2012 Dec 12]. Available from: http://www.phillycopd.com
- 27.Irwin JR. Buying/selling price preference reversals: preference for environmental changes in buying versus selling modes. Organ Behav Hum Decision Process. 1994;60:431–457. [Google Scholar]
- 28.Weiner B. On sin versus sickness: a theory of perceived responsibility and social motivation. Am Psychol. 1993;48:957–965. doi: 10.1037//0003-066x.48.9.957. [DOI] [PubMed] [Google Scholar]
- 29.Lutfey KE, Eva KW, Gerstenberger E, Link CL, McKinlay JB. Physician cognitive processing as a source of diagnostic and treatment disparities in coronary heart disease: results of a factorial priming experiment. J Health Soc Behav. 2010;51:16–29. doi: 10.1177/0022146509361193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78:775–780. doi: 10.1097/00001888-200308000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Mamede S, van Gog T, van den Berge K, Rikers RMJP, van Saase JLCM, van Guldener C, Schmidt HG. Effect of availability bias and reflective reasoning on diagnostic accuracy among internal medicine residents. JAMA. 2010;304:1198–1203. doi: 10.1001/jama.2010.1276. [DOI] [PubMed] [Google Scholar]
- 32.Soumerai SB, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA. 1990;263:549–556. [PubMed] [Google Scholar]
- 33.O’Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard-Jensen J, Kristoffersen DT, Forsetlund L, Bainbridge D, Freemantle N, Davis DA, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007;(4):CD000409. doi: 10.1002/14651858.CD000409.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Philadelphia Department of Public HealthGet healthy Philly, Tobacco Policy and Control Program, annual report, 2011–2012. c2013[updated 2015; cited 2014 July 21]. Available from: http://www.phila.gov/health/pdfs/commissioner/2012AnnualReport_Tobacco.pdf
- 35.Lai J.Philly smoking rates at lowest level in years. Philadelphia Inquirer, November 17, 2012 [updated 2012; accessed 2015 Mar 8]. Available from: http://articles.philly.com/2012–11–17/news/35157719_1_threat-of-secondhand-smoke-private-workplaces-cigarette-prices
- 36.Chugh D. Societal and managerial implications of implicit social cognition: why milliseconds matter. Soc Justice Res. 2004;17:203–222. [Google Scholar]
- 37.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]