Abstract
Rationale: Although expert communication between intensive care unit clinicians with patients or surrogates improves patient- and family-centered outcomes, fellows in critical care medicine do not feel adequately trained to conduct family meetings.
Objectives: We aimed to develop, implement, and evaluate a communication skills program that could be easily integrated into a U.S. critical care fellowship.
Methods: We developed four simulation cases that provided communication challenges that critical care fellows commonly face. For each case, we developed a list of directly observable tasks that could be used by faculty to evaluate fellows during each simulation. We developed a didactic curriculum of lectures/case discussions on topics related to palliative care, end-of-life care, communication skills, and bioethics; this month-long curriculum began and ended with the fellows leading family meetings in up to two simulated cases with direct observation by faculty who were not blinded to the timing of the simulation. Our primary measures of effectiveness were the fellows’ self-reported change in comfort with leading family meetings after the program was completed and the quality of the communication as measured by the faculty evaluators during the family meeting simulations at the end of the month.
Measurements and Main Results: Over 3 years, 31 critical care fellows participated in the program, 28 of whom participated in 101 family meeting simulations with direct feedback by faculty facilitators. Our trainees showed high rates of information disclosure during the simulated family meetings. During the simulations done at the end of the month compared with those done at the beginning, our fellows showed significantly improved rates in: (1) verbalizing an agenda for the meeting (64 vs. 41%; Chi-square, 5.27; P = 0.02), (2) summarizing what will be done for the patient (64 vs. 39%; Chi-square, 6.21; P = 0.01), and (3) providing a follow-up plan (60 vs. 37%; Chi-square, 5.2; P = 0.02). More than 95% of our participants (n = 27) reported feeling “slightly” or “much” more comfortable with discussing foregoing life-sustaining treatment and leading family discussions after the month-long curriculum.
Conclusions: A communication skills program can be feasibly integrated into a critical care training program and is associated with improvements in fellows’ skills and comfort with leading family meetings.
Keywords: communication skills, medical education, critical illness
Expert clinician–family communication is an integral part of the care of critically ill patients both in and outside of the intensive care unit (ICU). Delivering bad news, explaining critical care interventions, discussing prognosis in the face of uncertainty, and negotiating agreement on the withdrawal of life-sustaining treatments are examples of common communication challenges that critical care clinicians face. Clinician communication with critically ill patients and their surrogate decision makers has consistently been identified as one of the more important aspects of high-quality care in the ICU (1). Proactive communication strategies in the ICU have been associated with improvements in patient- and family-centered outcomes and improvements in the frequency and timing of decisions about major treatments (2).
Despite the importance of communication skills, research continues to suggest that communication with families in the ICU is often insufficient and of poor quality (3, 4). Critical care fellows, who traditionally learned communication skills from senior colleagues, often do not feel adequately trained to conduct family meetings (5). Previous research suggests that fellows value practical communication skills training with opportunities for structured feedback (5, 6). Simulation methodologies have been an effective way to improve the teaching of communication skills to medical trainees in a variety of settings (7) but often require trainees to miss multiple continuous days on clinical service, making it impractical for most critical care fellowship in the United States to integrate these methods into their fellowship training programs.
Recognizing the gap between the importance of communication skills in critical care and the lack of structured educational programs to improve critical care fellows’ comfort and skill in these areas, we aimed to develop a communication skills program that could be integrated into our Critical Care Medicine fellowship program. The overall objective was to provide critical care fellows with opportunities to practice and improve their skills in communicating with families of critically ill patients. This article describes the design, content, and evaluation of this communication skills program.
Methods
Setting
This program was developed in the Division of Critical Care Medicine, in collaboration with the Palliative Care Program, at the Montefiore Medical Center at Albert Einstein College of Medicine. Montefiore Medical Center is a large healthcare system composed of three urban tertiary care hospitals located in Bronx, New York. There are 72 critical care beds staffed by full-time critical care medicine attending physicians and a robust 24-hour critical care outreach service. The majority of the critical care fellows rotate through our division for 1 or 2 years of clinical training: the majority come for 1 year after completing previous training in pulmonary medicine or other internal medicine subspecialties; others come for 2 years after previous training in general internal medicine or emergency medicine. Fellows from a separate 3-year pulmonary/critical care fellowship also located at Montefiore Medical Center rotate through our division during the second year of their 3-year fellowship. The targeted learners for the course were the critical care fellows who were rotating through our division. The Institutional Review Board at Albert Einstein College of Medicine and Montefiore Medical Center reviewed this project, and it was found to be exempt under institutional and federal governmental policies.
Needs Assessment
Before we developed the program, we surveyed attending physicians in the Division of Critical Care Medicine asking about their clinical experiences and attitudes regarding communication in the critical care setting and their perceptions regarding the amount and quality of the communication skills teaching during the fellowship. Each year before the start of the program, we obtained potential participants’ demographic characteristics, their opinions regarding the amount and quality of communication skills teaching during the fellowship, and their attitudes and perceptions on the role of communication skills in the critical care setting.
Program Development
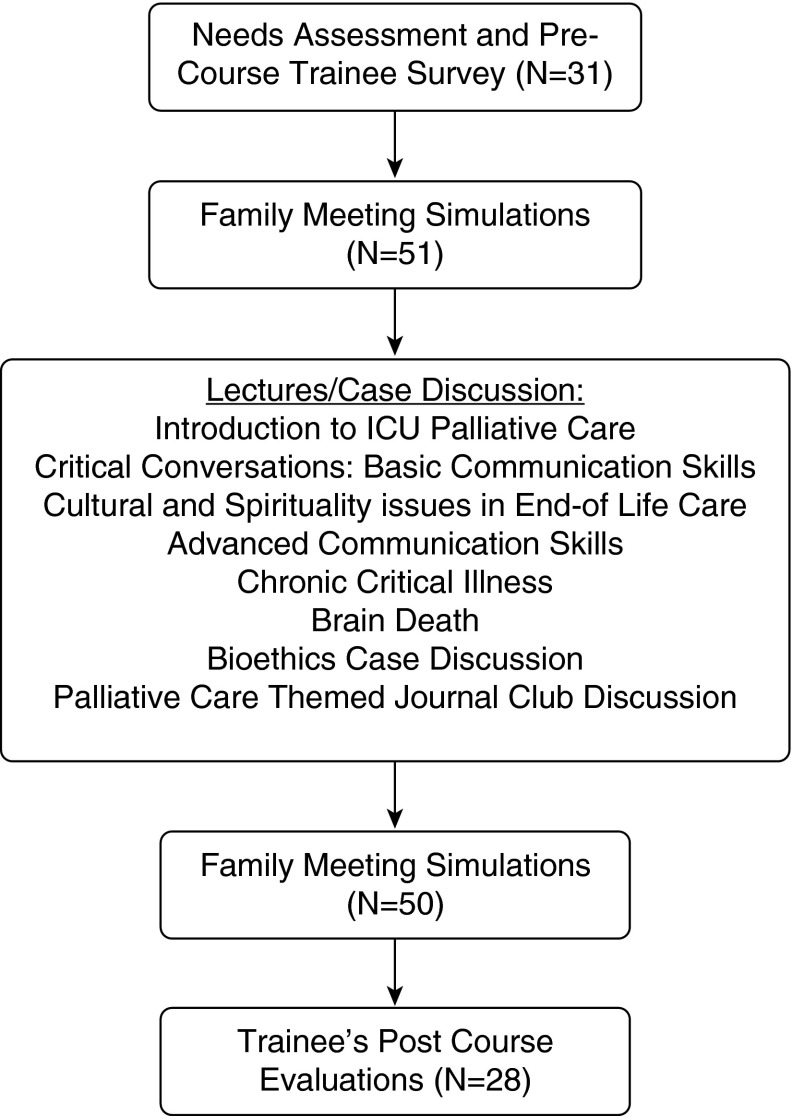
We reviewed the published literature on communication skills training for medical trainees and identified some key principles to integrate into the design of the program (8). First, we wanted to integrate some of the tenets of effective communication training programs like Oncotalk by giving the fellows opportunities for skills practice with direct observation and feedback using simulation cases (9–11). Second, we wanted to use diverse educational methods and provide our fellows with opportunities for repetition and reinforcement, so we designed a month-long curriculum of cases/lectures focused on communication skills, palliative care, and bioethics in the ICU (Figure 1).
Figure 1.
Structure and flow of the communication skills program. Fellows started the month with an opportunity for up to two simulated family meetings with directed feedback and then attended lectures and case-based discussions around palliative care, bioethics, and end-of-life care in the intensive care unit (ICU). At the end of the month, the fellows were given another opportunity to participate in up to two family meeting simulations with directed feedback.
We selected four paradigmatic cases that we believed represented distinct points along the hospital trajectory for critically ill patients and provided common communication challenges our fellows face (see Table E1 in the online supplement). We developed a list of observable communication tasks for each case (see Table E2 for an example), and we (A.A.H., J.A.F., A.B.K., M.N.G., and J.M.H.) reached consensus regarding the skill level of each task: level 1 skills were considered necessary for effective communication (e.g., introducing self, mentioning role on the clinical team), level 2 skills were considered intermediate communication skills that could be used to enhance communication and rapport building (e.g., checking for family member’s understanding of the illness before providing an update or eliciting concerns from the families regarding the patient’s illness), level 3 skills were advanced skills that were unlikely to accrue with experience alone (e.g., attending to emotions present during the meeting, asking about readiness to discuss prognosis). Faculty facilitators for the family meeting simulations were all attending physicians in either the Division of Critical Care Medicine (A.A.H., M.N.G., A.B.K.) or the Palliative Care Program (J.A.F., P.A.P.). Of the five faculty facilitators, three had previous fellowship training in palliative medicine and had been exposed to prior communication skills training (A.A.H., J.A.F., P.A.P.).
We recruited clinician volunteers (critical care nurses, physicians, and other care providers) to play the roles of the family members for the four cases. These volunteers were integrated when possible into the planning of the program (S.J.H., J.M.H.). Borrowing from sociodrama and psychodrama (12), each volunteer was assigned a particular role to play with specific attitudes, beliefs, feelings, and values. Our volunteer clinicians were encouraged to “own” the scenario through practice and reflection for 10 minutes before the afternoon of simulations and were provided some guidance on how to provide feedback to our fellows (13).
Implementation and Evaluation
At the beginning (and end) of a month-long curriculum, the fellows were excused from clinical services for an afternoon and led one to two simulated family meetings. Each simulation lasted about 25 minutes, leaving 5 to 10 minutes for feedback and reflection. During the afternoon of simulations, we aimed to create a safe, interpersonal, and nonjudgmental climate (see Table 1 for key strategies). Faculty facilitators were assigned to specific cases, were present throughout each simulation encounter, and were asked to observe and evaluate the encounter by (1) documenting the communication tasks that were completed during the simulation, and (2) rating the quality of the communication in four domains (nonverbal behavior, avoiding medical jargon, responding to emotions, clarity of the follow-up plan) using a rating scale from 1 “excellent” to 5 “poor.” At the end of each simulation, faculty facilitators used the specific tasks that they observed during the meeting to provide feedback directly to the fellow but were careful to only offer one or two suggestions for improvement. Fellows were asked to identify one thing that went well during the encounter and one thing that could have been improved. Input from the role-playing clinician was requested (13).
Table 1.
Key strategies to ensure a safe simulation environment for communication skills training
| Have dedicated faculty champion(s) whose focus is to develop a rapport with the learners, set the tone for the simulation encounters, debrief with faculty and with learners after the simulation encounters. |
| Ensure buy-in from the program director and other clinical leaders in the training program. |
| Ensure that the learners have space and time for reflection both before and after the simulation encounter (e.g., we used a conference room where instructions and schedules were written out, we minimized clinical interruptions during the simulation encounters by ensuring our fellows were excused from their clinical rotations). |
| Provide learners with ground rules to help to set expectations. |
| Emphasize that the simulation is learner-centered (e.g., the simulations were introduced to our learners as an opportunity for them to practice their communication skills; they were encouraged to invent any clinical details about the case they believed were appropriate). |
| Explain the role of the faculty evaluator (e.g., the faculty evaluator will not tell you what to do; they will provide you feedback and debrief with you at the end of the simulation). |
| Provide learners with mechanisms to respond to intrasimulation crisis (e.g., we instituted a Time Out option that the learners were encouraged to use to stop the simulation for any reason, including such things as anxiety, feeling beyond their comfort zone, etc.). |
| Provide faculty evaluators with ground rules about feedback and debriefing. |
| Feedback is learner centered (e.g., we asked the learner to name one or two things they did well, then asked them to name one or two things they could have done better). |
| Feedback is specific (e.g., we used the observable communication tasks developed for each case to ground feedback). |
| Encourage faculty evaluators to listen actively and to invite reflections from learners. |
One faculty champion (A.A.H.) closely supervised the month-long curriculum and was present for most of the month’s activities. Lectures and case discussion were scheduled throughout the month and included such topics as: basic communication skills for the critical care setting (14, 15), introduction to palliative care and end-of-life care in the ICU, cultural and spiritual aspects to end-of-life, brain death, chronic critical illness, and bioethics case discussion (see Table E3 for more details). The faculty champion for the program led a wrap-up session at the end of the month focused on repetition and reinforcement of key points made during the month. At the end of the month, fellows were again taken off their clinical services for an afternoon and provided an opportunity to lead up to two simulated family meetings; we ensured that the two cases were different from the cases they had done at the beginning of the month. At the end of the program, we asked the fellows to assess how much the course had changed their comfort level in several communication domains and provided space for comments and suggestions.
Statistical Analyses
We used descriptive statistics to describe the characteristics and attitudes of the fellows, their performance rates for key communication tasks, and the faculties’ quality ratings. We used the Chi-square test to compare simulations at the beginning of the month to those done at the end of the month; a two-sided P value less than 0.05 was our threshold for statistical significance. All analyses were done using Microsoft Excel 2010 (Microsoft, Redmond, WA).
Results
Over the course of three years (2012–2014), 31 fellows participated in the program, of whom 28 participated in at least one of the family meeting simulations; we conducted 51 and 50 simulated family meetings at the beginning and end of our month-long curriculum, respectively, with our critical care fellows (Figure 1). The average age of our fellows was 34.3 years; about 80% of them were men, and most had completed medical school outside of the United States. Table 2 shows some characteristics and attitudes of our participants from our precourse survey.
Table 2.
Fellow characteristics and attitudes
| Age, mean ± SD,
yr |
34.3 ± 3.2 |
| Female | 7 (22.6) |
| Medical school graduation year, median (interquartile range) | 2003 (2001–2006) |
| Career plan is to pursue primarily patient care at an academic hospital in the next 5–10 yr | 16 (53.3) |
| Completed medical school in the United States | 7 (22.6) |
| More inclined toward the social/emotional aspects of patient care or the technological and scientific aspects? | |
| A little more/much more inclined toward social/emotional | 12 (38.7) |
| A little/much more inclined toward technical | 18 (58.1) |
| Completely agree that breaking bad news is a teachable skill* | 20 (63.6) |
| Completely agree that it is possible to tell patients/proxies the truth and still maintain hope* | 14 (46.7) |
Data are presented as n (%) unless otherwise noted.
4-Point Likert scale that included completely agree, generally agree, generally disagree, and completely disagree.
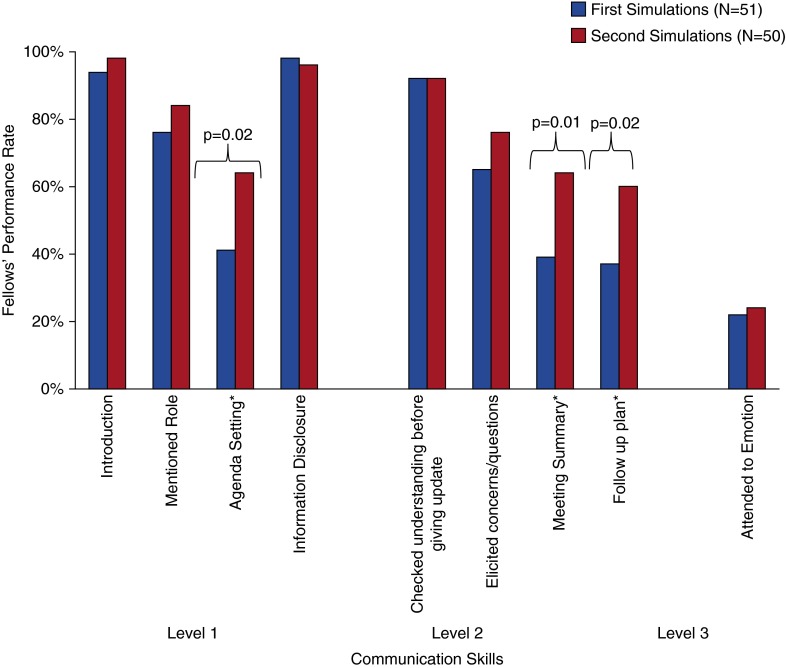
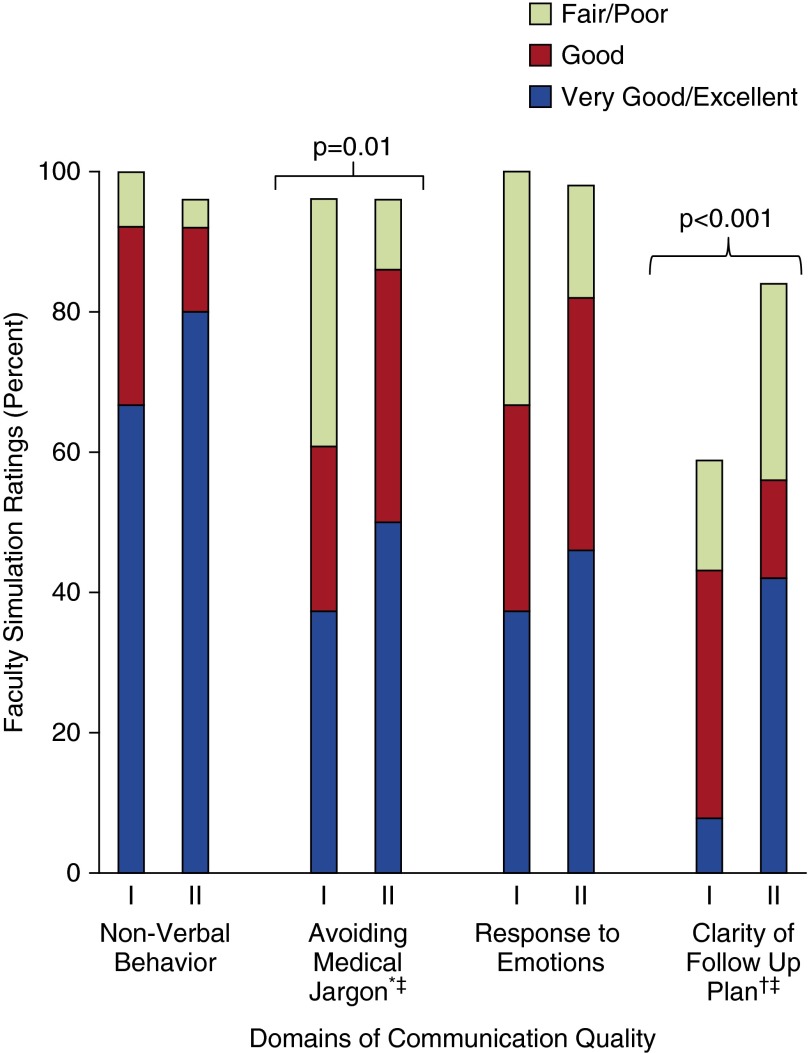
During the simulated family meetings, performance rates for skills like introductions, role identification, and information disclosure to family regarding illness were high (at or greater than 80%), regardless of when simulation occurred. The fellows were observed performing three skills at significantly higher rates in the simulations done at the end of the month compared with those done at the beginning of the month: verbalizing an agenda for the meeting (64 vs. 41%; Chi-square, 5.27; P = 0.02), summarizing what will be done for the patient (64 vs. 39%; Chi-square, 6.21; P = 0.01), and providing a follow-up plan (60 vs. 37%; Chi-square, 5.2; P = 0.02) (Figure 2). In general, our faculty evaluators rated the quality of the communication higher in the simulations that occurred at the end of the month, but only in two of the four quality domains was this statistically significant: in how they avoided medical jargon (50% rated very good/excellent during the second simulations vs. 37.5% in the first; Chi-square, 9.36; P = 0.01) and in the clarity of the follow-up plan provided (42% rated very good/excellent in the second simulation vs. 7.8% in the first; Chi-square, 16.5; P < 0.0001) (Figure 3).
Figure 2.
Fellows’ performance of communication tasks during family meeting simulations. Shows the performance rates for nine communication tasks that faculty facilitators were asked to document in all family meeting simulations. Explicitly attending to emotions refers to any of five strategies used to acknowledge emotions during a communication encounter (reflected in the mnemonic “NURSE” for Naming, Understanding, Respect, Supportive Statement, and Explore). First Simulations refers to family meeting simulations done at the beginning of the month-long curriculum, and Second Simulations refers to those done at the end of the month. Consensus was reached regarding the skill level of each task: level 1 skills were considered necessary for effective communication; level 2 skills were considered intermediate communication skills that could be used to enhance communication and rapport building; level 3 skills were advanced skills that were unlikely to accrue with experience alone. *Comparisons between the first and second simulations were not statistically significant except for the three that are highlighted in the figure.
Figure 3.
Faculty ratings of simulations across four quality domains. Shows the faculty quality ratings for the family meeting simulations across four quality domains. First Simulations refers to family meeting simulations done at the beginning of the month-long curriculum, and Second Simulations refers to those done at the end of the month. *Does not add up to 100% because of missing data. †Does not add up to 100% because of the many simulations where no follow-up plan was provided. ‡Comparisons between the first and second simulations were not statistically significant except for the two that are highlighted in the figure.
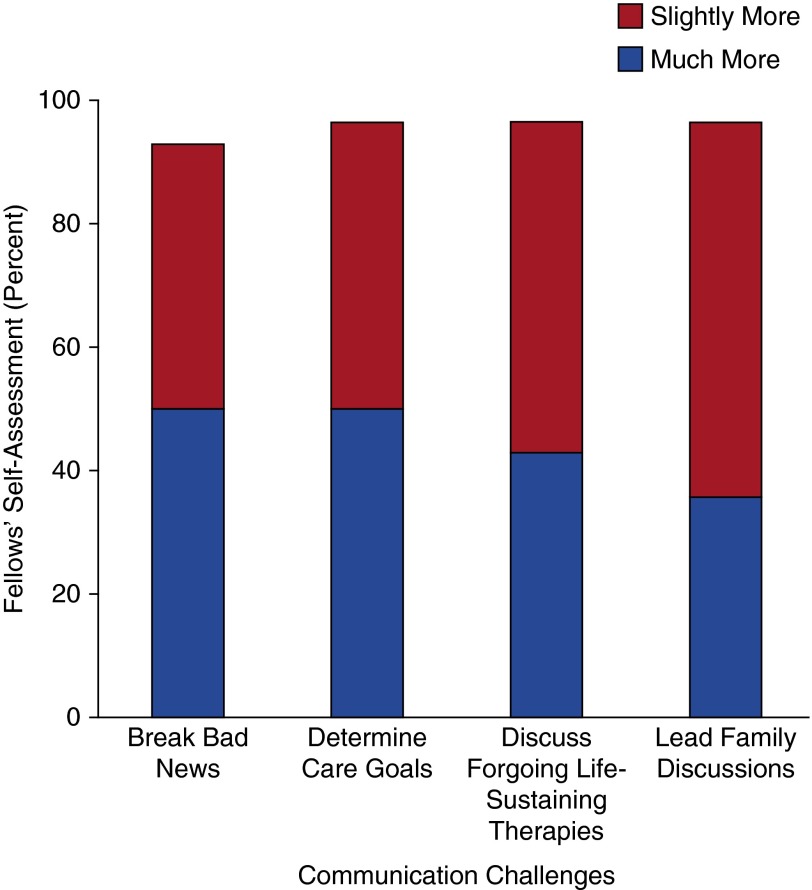
At the end of the program, 50 and 35.7% of the fellows rated themselves much more comfortable at breaking bad news and at leading family meetings, respectively; 42.9 and 60.7% rated themselves slightly more comfortable, respectively. In general, more than 90% of our fellows rated themselves much more or slightly more comfortable at breaking bad news, determining goals of care, discussing foregoing life-sustaining therapies, and leading family discussions in general (Figure 4). Formal and informal evaluations of the program were generally positive from the fellows: of the 28 who evaluated the program, we received written comments from 24 fellows. Several fellows commented that they wanted more case simulations available for practice; others wanted more opportunity for feedback from their Attendings in real-life clinical encounters. Several fellows lamented missing some of the lectures due to their clinical schedule during the month. Representative quotes from the fellows include the following:
Figure 4.
Fellows’ self-assessment at the end of the month-long curriculum. Shows the percent of program participants who felt that they were slightly more comfortable or much more comfortable performing the four communication challenges after the month-long curriculum.
“Was really good. Addressed the points which I probably would have missed during the family meeting.”
“I think the teaching was good...I could not attend all of the sessions, just attending first and last session due to the rotation I was on.”
“…want more scenarios…other conflict scenarios that occur.”
“Very good cases. They give you the option of a variety of scenarios.”
Discussion
Our objective was to improve the communication skills of our critical care fellows using a mixture of methods, including family meeting simulations, lectures, and case discussions. We have described a simulation-based month-long curriculum that can feasibly be integrated into a critical care fellowship, and we show that this program was associated with improvements in fellows’ comfort level in leading family meetings. In a setting with highly motivated faculty members without any specialized training or expertise in communication skills, we developed a program that could be executed with minimal interruption of the fellows’ clinical obligations. Our simulation cases were designed to be directly relevant to critical care clinicians, and our evaluation tools for each case allowed faculty facilitators to easily provide feedback to our fellows while also providing insight into the communication skills being used by our fellows. Data from more than 100 such simulations over the course of 3 years of sustaining this program highlight potentially modifiable communication skills that could be the focus of training for critical care fellows.
Communication skills programs such as Oncotalk and Geritalk have shown improvements in trainees’ communication skills by removing trainees out of their training environment for several days, focusing on communication skills practice, skills demonstrations, didactic overview, and small group reflection (9, 11). Recently, Arnold and colleagues show that a similar skills workshop model can improve self-assessed skills in 36 critical care fellows (16). The novelty of our program lies in its use of internal division resources to integrate a communication skill program into the training environment of our busy critical care fellowship with minimal interruption of the fellows’ clinical schedule. These modifications enhance the generalizability of our approach when compared with previously published programs.
We did this by using a faculty champion who choreographed a month of lectures/didactics with two afternoons dedicated to family meeting simulations where the fellows were able to practice their skills and receive feedback directly. The faculty champion, by being present throughout the month, could tailor case discussions and repetition around particular skills deficits in our fellows. Because we did not depend on trained communication experts to execute our program, we developed, instead, rigorous approaches to evaluate the family meeting simulations that focused on directly observable communication tasks for each simulation case (Table E2). This approach provided rich insight into the kinds of communication skills that trainees exhibit and what potential skills are likely to improve with brief interventions such as these.
In more than 100 family meeting simulations with critical care fellows over the course of 3 years, we found that our fellows’ content skills (what was actually said, the type of language that was used during the encounter) (17) was judged by faculty as good/very good or excellent in about 60% of the simulations at the beginning of the month, which improved to 86% at the end of the month. Our fellows also showed significant improvements in process skills such as agenda setting, summarizing, and establishing a follow-up plan (17). Performance rates for perceptual skills such as explicit attention to emotions during the simulations were low during the first simulations and remained low at the end of the month. Taken together, these results suggests that content and process skills may be easier to change during brief communication skills programs such as these and suggests that perceptual skills may be more difficult to change.
Teaching communication skills well requires trainees to have opportunities for skills practice with opportunities for direct feedback (18). In our program, each afternoon of simulation required 3 hours of faculty facilitation for each case (we offered four cases twice per year) plus the 3 hours of involvement from our clinician volunteers who role-played family members for the simulations. In addition, the availability of the faculty champion during the month’s activities may have been important to the success of the program. We believe that this model may be adaptable for many fellowship training programs in the United States because (1) the simulation cases were specifically tailored to the needs of critical care fellows, including cases that highlighted communication challenges for the critical care consultant as well as the critical care practitioner in the ICU; (2) the level of expertise required by faculty facilitators was significantly less than most previously published programs, because we focused on developing evaluation tools for each case that helped faculty facilitators to tailor their feedback to directly observable communication tasks. However, future innovation is needed to develop novel strategies to improve communication skills of fellows with less faculty time commitment.
The project has limitations. Due to feasibility, outcome measures were restricted to self-assessment and the faculty evaluations during the simulations, both of which may be subject to bias. We did not, a priori, test the reliability of faculty evaluation, but we had little turnover in faculty over the 3 years of the program, and our faculty facilitators in all cases facilitated the same simulation case throughout the years of the program. Also, our faculty evaluators were not blinded to the timing of the simulations. In addition, because we used clinicians to play the part of family members, our faculty evaluators had the advantage of looking for consensus with these volunteers when evaluating the family meeting simulations, which makes severe misclassification less likely. Although our sample size was small, our ability to sustain this program over 3 years is an important strength. We did not take attendance during the month of lectures/case discussion because all lectures/case discussions were taped and available online for months after the program completion. Participation was not mandatory; fellows who were working nights or on vacation during the month of the program would have missed several components of the program. Despite these limitations, the fact that our fellows’ comfort level in key communication domains improved after the month and the rates of several observable skills increased during the simulations at the end of the month suggest that this approach to improving communication skills is feasible and effective. Participants in our program had low rates of explicit attention to emotions and showed little improvement in these skills over the course of the month-long curriculum. Given the potential importance of these skills for effective communication with seriously ill patients and their families, future communication skills programs should test innovative ways to improve trainees’ ability to attend explicitly to emotions. We did not assess the impact of our program on patient or family outcomes.
In summary, we show that a communication skills program with opportunity for skills practice and feedback can be integrated into critical care training programs and may improve fellows’ skill and comfort in leading family meetings. More data are needed on what kinds of trainee skills improve during these short-term training programs, but data from our many simulations suggest that the type of language that is used in communication encounters and how the communication is structured may be responsive to change.
Acknowledgments
Acknowledgment
The authors thank the Division of Critical Care Medicine, including its faculty and fellows, for supporting this program. They also thank Mirian Martinez, Dr. Nida Qadir, and Dr. Hayley Gershengorn for acting as family members for our simulations.
Footnotes
Supported by the Division of Critical Care Medicine at Albert Einstein College of Medicine; NHLBI U01 HL10871203 (M.N.G.), R03AG040673 from the National Institute of Aging, and 8KL2TR0000088-05 from the Albert Einstein College of Medicine—Montefiore Medical Center Institute for Clinical and Translational Research (S.J.H.).
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
Author Contributions: Study conception and design, A.A.H., S.J.H., J.M.H., A.B.K., J.A.F., and M.N.G. Data acquisition, analysis, and interpretation, A.A.H., S.J.H., J.M.H., A.B.K., J.A.F., P.A.P., and M.N.G. Drafting the manuscript for important intellectual content, A.A.H., S.J.H., J.M.H., A.B.K., J.A.F., P.A.P., and M.N.G.
References
- 1.Nelson JE, Mulkerin CM, Adams LL, Pronovost PJ. Improving comfort and communication in the ICU: a practical new tool for palliative care performance measurement and feedback. Qual Saf Health Care. 2006;15:264–271. doi: 10.1136/qshc.2005.017707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scheunemann LP, McDevitt M, Carson SS, Hanson LC. Randomized, controlled trials of interventions to improve communication in intensive care: a systematic review. Chest. 2011;139:543–554. doi: 10.1378/chest.10-0595. [DOI] [PubMed] [Google Scholar]
- 3.Azoulay E, Chevret S, Leleu G, Pochard F, Barboteu M, Adrie C, Canoui P, Le Gall JR, Schlemmer B. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28:3044–3049. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 4.Curtis JR, Engelberg RA, Wenrich MD, Shannon SE, Treece PD, Rubenfeld GD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med. 2005;171:844–849. doi: 10.1164/rccm.200409-1267OC. [DOI] [PubMed] [Google Scholar]
- 5.DeVita MA, Arnold RM, Barnard D. Teaching palliative care to critical care medicine trainees. Crit Care Med. 2003;31:1257–1262. doi: 10.1097/01.CCM.0000060160.78227.35. [DOI] [PubMed] [Google Scholar]
- 6.Downar J, Knickle K, Granton JT, Hawryluck L. Using standardized family members to teach communication skills and ethical principles to critical care trainees. Crit Care Med. 2012;40:1814–1819. doi: 10.1097/CCM.0b013e31824e0fb7. [DOI] [PubMed] [Google Scholar]
- 7.Berkhof M, van Rijssen HJ, Schellart AJ, Anema JR, van der Beek AJ. Effective training strategies for teaching communication skills to physicians: an overview of systematic reviews. Patient Educ Couns. 2011;84:152–162. doi: 10.1016/j.pec.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Reed S, Shell R, Kassis K, Tartaglia K, Wallihan R, Smith K, Hurtubise L, Martin B, Ledford C, Bradbury S, et al. Applying adult learning practices in medical education. Curr Probl Pediatr Adolesc Health Care. 2014;44:170–181. doi: 10.1016/j.cppeds.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Back AL, Arnold RM, Tulsky JA, Baile WF, Fryer-Edwards KA. Teaching communication skills to medical oncology fellows. J Clin Oncol. 2003;21:2433–2436. doi: 10.1200/JCO.2003.09.073. [DOI] [PubMed] [Google Scholar]
- 10.Back AL, Arnold RM, Baile WF, Fryer-Edwards KA, Alexander SC, Barley GE, Gooley TA, Tulsky JA. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. 2007;167:453–460. doi: 10.1001/archinte.167.5.453. [DOI] [PubMed] [Google Scholar]
- 11.Kelley AS, Back AL, Arnold RM, Goldberg GR, Lim BB, Litrivis E, Smith CB, O’Neill LB. Geritalk: communication skills training for geriatric and palliative medicine fellows. J Am Geriatr Soc. 2012;60:332–337. doi: 10.1111/j.1532-5415.2011.03787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baile WF, De Panfilis L, Tanzi S, Moroni M, Walters R, Biasco G. Using sociodrama and psychodrama to teach communication in end-of-life care. J Palliat Med. 2012;15:1006–1010. doi: 10.1089/jpm.2012.0030. [DOI] [PubMed] [Google Scholar]
- 13.Thomas JD, Arnold RM. Giving feedback. J Palliat Med. 2011;14:233–239. doi: 10.1089/jpm.2010.0093. [DOI] [PubMed] [Google Scholar]
- 14.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES—a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302–311. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 15.Pollak KI, Arnold RM, Jeffreys AS, Alexander SC, Olsen MK, Abernethy AP, Sugg Skinner C, Rodriguez KL, Tulsky JA. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol. 2007;25:5748–5752. doi: 10.1200/JCO.2007.12.4180. [DOI] [PubMed] [Google Scholar]
- 16.Arnold RM, Back AL, Barnato AE, Prendergast TJ, Emlet LL, Karpov I, White PH, Nelson JE. The Critical Care Communication project: improving fellows’ communication skills. J Crit Care. 2015;30:250–254. doi: 10.1016/j.jcrc.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 17.Kurtz SM, Silverman J, Draper J. Abingdon, Oxon, UK: Radcliffe Medical Press; 1998. Teaching and learning communication skills in medicine. [Google Scholar]
- 18.Back AL, Arnold RM, Baile WF, Tulsky JA, Barley GE, Pea RD, Fryer-Edwards KA. Faculty development to change the paradigm of communication skills teaching in oncology. J Clin Oncol. 2009;27:1137–1141. doi: 10.1200/JCO.2008.20.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]