Abstract
The present study aimed to study the effects of exercise training (ET) performed by rats on a 10-week high-fructose diet on metabolic, hemodynamic, and autonomic changes, as well as intraocular pressure (IOP). Male Wistar rats receiving fructose overload in drinking water (100 g/L) were concomitantly trained on a treadmill for 10 weeks (FT group) or kept sedentary (F group), and a control group (C) was kept in normal laboratory conditions. The metabolic evaluation comprised the Lee index, glycemia, and insulin tolerance test (KITT). Arterial pressure (AP) was measured directly, and systolic AP variability was performed to determine peripheral autonomic modulation. ET attenuated impaired metabolic parameters, AP, IOP, and ocular perfusion pressure (OPP) induced by fructose overload (FT vs F). The increase in peripheral sympathetic modulation in F rats, demonstrated by systolic AP variance and low frequency (LF) band (F: 37±2, 6.6±0.3 vs C: 26±3, 3.6±0.5 mmHg2), was prevented by ET (FT: 29±3, 3.4±0.7 mmHg2). Positive correlations were found between the LF band and right IOP (r=0.57, P=0.01) and left IOP (r=0.64, P=0.003). Negative correlations were noted between KITT values and right IOP (r=-0.55, P=0.01) and left IOP (r=-0.62, P=0.005). ET in rats effectively prevented metabolic abnormalities and AP and IOP increases promoted by a high-fructose diet. In addition, ocular benefits triggered by exercise training were associated with peripheral autonomic improvement.
Keywords: Fructose, Exercise training, Intraocular pressure, Autonomic modulation
Introduction
Metabolic syndrome (MS) is defined by physiological, biochemical, clinical, and metabolic changes that directly increase the risk of diabetes and cardiovascular mortality (1,2). These include atherogenic dyslipidemia, hypertension, glucose intolerance, a proinflammatory state, and a prothrombotic state (3). Higher socioeconomic status, sedentary lifestyle, and high body mass index (BMI) are also strongly associated with the increasing prevalence of MS (4). Moreover, diet plays an important role in maintaining health and preventing cardiometabolic dysfunctions. Diets high in sugars, saturated fats, and with high ratios of polyunsaturated fatty acids are associated with MS development in humans and animal models; however, the causal relationship between diet and health remains elusive (5-9).
In fact, several studies have shown that the large increase in fructose consumption in the last several decades has paralleled the increase in obesity rates (10,11). In this context, fructose overload in drinking water or chow has been used to promote metabolic, hemodynamic, structural, and functional derangements in animals. This MS model has been used by our laboratory (12,13) and others (9,14-16) to elucidate the various aspects of obesity, dyslipidemia, and insulin resistance associated with autonomic changes.
Intraocular pressure (IOP) is the only known modifiable risk factor for primary open-angle glaucoma, and it has been associated with cardiometabolic risk factors such as type II diabetes, systemic hypertension, and concurrent atherosclerotic disease (17-19). In addition, MS and other insulin resistance-related features (e.g., hepatic steatosis), increased left ventricular mass, and proteinuria have all been strongly associated with high IOP (20). Although the relationship between cardiometabolic risk factors and increased IOP is now well established, IOP has not yet been studied in a model of fructose overload-induced MS.
Growing evidence demonstrates that exercise training (ET) promotes beneficial effects in cardiovascular and metabolic diseases, such as MS (21). Furthermore, evidence continues to accumulate that beginning an exercise regimen helps prevent open-angle glaucoma, most likely due to the IOP-lowering effects of ET in sedentary individuals. However, the effects of ET on IOP and the underlying mechanisms in a fructose overload-induced MS model remain poorly understood. Thus, the aim of this study was to investigate whether moderate ET performed during 10 weeks on a high-fructose diet can prevent metabolic, hemodynamic, and autonomic changes, as well as increased IOP in male Wistar rats. To our knowledge, this is the first study to address this issue.
Material and Methods
Animals
Experiments were performed in adult male Wistar rats (240-260 g) from the Animal House of the Faculdade de Medicina, Universidade de São Paulo, São Paulo, SP, Brazil. Prior to the study, rats were fed standard laboratory chow and water ad libitum. The animals were housed in collective polycarbonate cages in a temperature-controlled room (22-23°C) under 54-55% humidity with a 12-h dark-light cycle (light 7:00 am to 7:00 pm). The experimental protocol was approved by the Animal Care and Use Committee of the Faculdade de Medicina, Universidade de São Paulo, and this investigation was conducted in accordance with the 8th edn. of the National Research Council Guide for the Care and Use of Laboratory Animals. The rats were randomly assigned to three groups of 7 animals each: sedentary control (C), sedentary fructose (F), and trained fructose (FT).
ET and fructose drinking
All experimental groups were adapted to the treadmill (10 min/day, 0.3 km/h) for 1 week. The animals underwent a maximal treadmill exercise test to determine aerobic capacity and ET intensity at the beginning of the experiment (initial evaluation) and after completion of the ET protocol (final evaluation). ET was performed on a motorized treadmill at low intensity (50-70% of maximal running speed) by the FT group for 1 h a day beginning at 6:00 pm, 5 days a week for 10 weeks (12). At the beginning of the ET protocol, the F and FT groups received fructose overload via dilution of D-fructose in the drinking water (100 g/L) for 10 weeks. Control animals received regular water during this period (12).
Obesity parameter
The Lee index for each animal was calculated after 10 weeks of the ET protocol and fructose overload to obtain the obesity parameter. This index was calculated as the cube root of body weight (g) × 10/naso-anal length (mm), and a value equal to or less than 0.300 was classified as normal at the third month of life. Rats with values higher than 0.300 were classified as obese (12).
IOP measurements
A TonoPen XL (Mentor, USA) tonometer was used to assess IOP in conscious, non-sedated rats as described previously (22). IOP evaluation was performed 24 h after the last exercise session, and assessed by an operator who was blinded to the group. Animals were wrapped in a small towel and held gently, with one operator holding the animal and another taking the readings. In a single measurement, five IOP readings were obtained from each eye by using firm contact with the cornea and omitting readings obtained as the instrument was removed from the eye. The differences among readings were less than 10% (standard error). The mean of the five readings was recorded as the IOP for that eye.
Cardiovascular assessments
One day after IOP measurements, two catheters filled with 0.06 mL saline were implanted into the femoral artery and femoral vein of rats that were intraperitoneally (ip) anesthetized with ketamine and xylazine (80 and 12 mg/kg, respectively). Twenty-four hours later, an arterial cannula was connected to a strain-gauge transducer (Blood Pressure XDCR; Kent Scientific, USA), and arterial pressure (AP) signals were recorded over a 30-min period in conscious animals by a microcomputer equipped with an analog-to-digital converter board (WinDaq, 2 kHz, DAT-AQ, USA). The recorded data were analyzed on a beat-to-beat basis to quantify changes in mean AP (MAP) and heart rate (HR) (13).
Rate constant for blood glucose disappearance
One day after blood pressure recording, the blood glucose values of all animals were measured after a 4-h fast with a glucosimeter (ACCUCHEK Advantage, Roche, Switzerland). The rats also underwent an intravenous insulin tolerance test (ITT) after a 2-h fast. Animals were anesthetized with thiopental (40 mg/kg body weight, ip), and a drop of blood from the tail was collected to measure blood glucose. This procedure was performed at baseline and 4, 8, 12, and 16 min after insulin administration (0.75 U/kg). The rate constant for blood glucose disappearance (KITT) was calculated using the 0.693/t1/2 formula, and the blood glucose half-time (t1/2) was calculated from the least-squares regression slope of the blood glucose concentration during the linear phase of decline (12).
Systolic blood pressure variability
Systolic AP (SAP, systograms) was obtained from blood pressure records. Fluctuations in SAP were further assessed in the frequency domain by means of autoregressive spectral estimation. The theoretical and analytical procedures for autoregressive modeling of oscillatory components have been described previously (13). Briefly, the SAP series derived from each recording were divided into 300 beat segments with a 50% overlap. The spectra of each segment were calculated via Levinson-Durbin recursion, and the order of the model was selected according to Akaike's criterion, with the oscillatory components quantified in low-frequency (LF, 0.2-0.6 Hz) and high-frequency (HF, 0.6-3.0 Hz) ranges (13).
Statistical analysis
Data are reported as means±SE. After confirming that all continuous variables were normally distributed using the Kolmogorov-Smirnov test, statistical differences between groups were obtained by one-way analysis of variance (ANOVA) followed by Student-Newman-Keuls post-tests. Pearson's correlation was used to study the association between different parameters. All tests were 2-sided, and the significance level was established to be P<0.05. Statistical calculations were performed using SPSS version 20.0 (IBM Corp, USA).
Results
Exercise capacity and morphometric and metabolic evaluations
ET promoted an increase in exercise capacity as evaluated by maximal running speed; the mean value for the FT animals was higher (1.8±0.05 km/h) compared to the C (1.2±0.04 km/h) and F (1.2±0.03 km/h) groups.
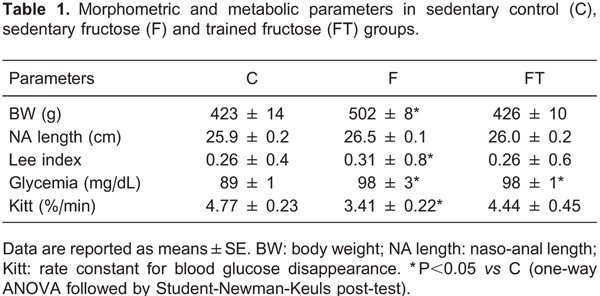
The morphometric and metabolic data are reported in Table 1. Body weight, Lee index, and KITT were impaired in F rats compared to C rats. It should be stressed that FT prevented these impairments; similar values were found compared to C animals. On the other hand, glycemia was increased in both the F and FT groups compared to the C group (Table 1).
IOP measurements
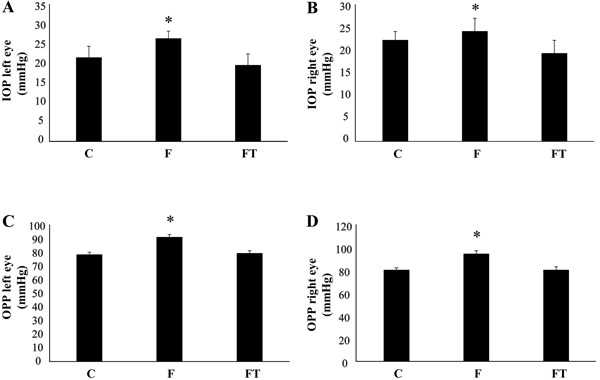
As shown in Figure 1, IOPs in the left (Figure 1A) and right (Figure 1B) eyes were higher in the F group than the C group. Similarly, ocular perfusion pressure (OPP) was increased in F rats compared to C rats for both the left (Figure 1C) and right (Figure 1D) eyes. Importantly, ET prevented IOP and OPP increases in FT rats.
Figure 1. Intraocular pressure (IOP) and ocular perfusion pressure (OPP) in the left (A and C) and right (B and D) eyes. Data are reported as means±SE. F: sedentary fructose; FT: trained fructose. *P<0.05 vs sedentary control (C) (one-way ANOVA followed by Student-Newman-Keuls post-test).
Cardiovascular and autonomic evaluations
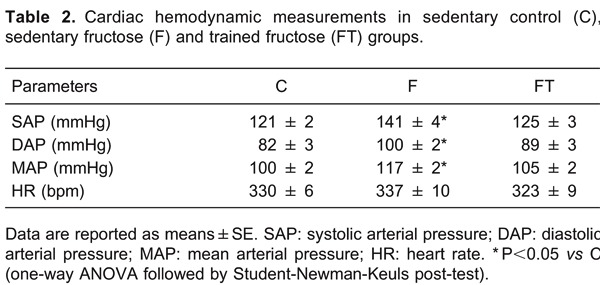
Direct measurements of AP demonstrated that the F group exhibited increased SAP, diastolic AP (DAP), and MAP compared to the C group. Ten weeks of ET were sufficient to attenuate the increases in these values in the FT group, which remained similar to those of the C animals. Resting HR values were similar among the groups (Table 2).
In addition to hemodynamic data, we evaluated SAP variability. F animals displayed increased SAP variance (Figure 2A) and LF band of SAP variability (Figure 2B) compared to C animals. Again, these impairments were prevented by ET.
Figure 2. Variance of systolic arterial pressure (VAR SAP) and low frequency (LF) band in experimental groups. Data are reported as means±SE. F: sedentary fructose; FT: trained fructose. *P<0.05 vs sedentary control (C) (one-way ANOVA followed by Student-Newman-Keuls post-test).

Correlation analysis
Positive correlations were found between SAP variance and right OPP (r=0.56, P=0.01) and left OPP (r=0.72, P=0.007). Correlations were also found between the LF band of SAP and the right IOP (r=0.57, P=0.01) and left IOP (r=0.64, P=0.003). MAP positively correlated with left IOP (r=0.79, P=0.001). Regarding metabolic parameters, a negative correlation was noted between KITT values and right IOP (r=-0.55, P=0.01) and left IOP (r=-0.62, P=0.005).
Discussion
The main finding of the present study lies in the fact that metabolic, IOP, AP, and peripheral autonomic alterations promoted by a high-fructose diet can be attenuated by simultaneous ET. Additionally, maintenance of IOP levels was associated with the preservation of peripheral autonomic modulation and metabolic parameters in experimental animals. To our knowledge, this is the first study to demonstrate the preventive effect of ET on the increase in IOP induced by fructose overload in rats.
MS induced by fructose overload in animals is characteristically accompanied by moderate hypertension and glucose intolerance and is associated with increased levels of plasma insulin, cholesterol, and triglycerides (12,13). In the present investigation, chronic fructose consumption promoted changes in body composition, as demonstrated by the increases in body weight and Lee index, and led to metabolic disturbances, as demonstrated by the decrease in insulin sensitivity and increased glycemia. These data corroborate previous findings published by our group (12,13).
ET has been considered a key component in the treatment of patients with MS because regular physical exercise can promote metabolic and cardiovascular adaptations. In fact, a recent meta-analysis demonstrated that dynamic ET is associated with favorable effects on most cardiovascular risk factors associated with MS (e.g., BMI, waist circumference, total cholesterol, and triglycerides) (23). Furthermore, it is known that regular exercise improves glycemia, lipid profile, and insulin sensitivity while promoting weight reduction and improving muscle glucose uptake (24). In the present study, ET was able to attenuate increases in body weight and Lee index and prevent insulin resistance in trained rats consuming high levels of fructose. The fact that ET was carried out during fructose overload might account for enhanced energetic demand and lipolysis, which could prevent weight gain and also contribute to improved insulin sensitivity.
Animal studies have shown strong associations between high fructose intake and the onset of arterial hypertension. In line with our previous findings (12,13), the present study demonstrated that 10 weeks of fructose overload led to increased SAP, DAP, and MAP in rats. Several candidate mechanisms have been suggested including the association between AP and insulin resistance. In this sense, our study emphasized the role of increased sympathetic nervous system activity as a possible factor leading to the observed changes (25,26).
In the present investigation, we observed increased peripheral sympathetic modulation in the F group compared to the C group. Bunnag et al. (14) previously demonstrated in vivo and in vitro that impaired vascular responses in fructose-fed rats may be associated with adaptation to increased sympathetic nervous activity, or be a compensatory response to other structural or functional changes that produce hypertension in this MS model. Data obtained by Kamide et al. (16) in fructose rats suggested that hyperinsulinemia may have an important role in promoting left ventricular hypertrophy by activating the local renin-angiotensin system and sympathetic activity. Additionally, high levels of fructose consumption exacerbated impairment of metabolic parameters and cardiac autonomic control, by reducing vagal tone and baroreflex sensitivity and increasing sympathetic nerve activity with additional insulin resistance in rats (12,13,27,28).
In addition to these hemodynamic and autonomic data, we also evaluated IOP and OPP in experimental animals. In the present study, 10 weeks of fructose overload induced an increase in intraocular pressure and OPP in F rats. The mechanism underlying the association between MS and IOP increase remains to be clarified. In humans, a recent study of 4875 men participating in the Korean National Health and Nutrition Examination Survey (2008-2010) demonstrated that increased IOP was positively correlated with BMI, systolic blood pressure, fasting blood glucose, triglycerides, low-density lipoprotein cholesterol, and insulin resistance after adjusting for all covariates (19).
In fact, it seems that each of the components of MS appears to contribute to increases in levels of IOP (29). Higher IOPs in obesity are likely due to excess intraorbital fat tissue, higher blood viscosity, and an increase in episcleral venous pressure, all of which consequently decrease the outflow facility (30). Systemic hypertension may trigger excessive production of aqueous humor, increasing the episcleral venous and ciliary arterial pressures (31). Additionally, elevated blood glucose can lead to autonomic dysfunction and a disturbed osmotic gradient, with subsequent fluid shift into the intraocular space, both of which are associated with elevated IOP (32).
Regarding these associations, we observed significant correlations between KITT values and OPP (in both eyes), as well as between parameters of SAP variability (VAR SAP and LF of SAP) and OPP (in both eyes). In fact, it was previously demonstrated that sympathetic acceleration of MAP by phenylephrine induced surges in IOP and ocular pulse amplitude (33).
On the other hand, clinical and experimental evidence has highlighted the blood pressure-lowering effects of aerobic endurance exercise in patients with hypertension. Indeed, a significant reduction in sympathetic neural activity has been reported as one of the main mechanisms accounting for the favorable effects of exercise on blood pressure control (34,35). The effects of physical activity on IOP have been reviewed by Risner et al. (36) and, more recently, by Roddy et al. (37). According to these reviews, a reduction in IOP occurs immediately or shortly after exercise, and patients with higher fitness levels have decreased IOPs and lower risk of glaucoma than patients with lower physical fitness levels (38).
The mechanisms underlying the exercise-induced lowering of IOP remain to be fully understood; however, some candidate mechanisms have been proposed including lower norepinephrine concentrations, increased colloid osmotic pressure, co-action of nitric oxide and endothelin after exercise, and the association with a β2-adrenergic receptor gene polymorphism (36,39,40). The present study provides the first evidence that ET is capable of preventing increases in IOP and OPP in rats on a high-fructose diet, and the potential underlying mechanisms include improved insulin sensitivity, reduced MAP, and diminished peripheral sympathetic modulation.
Although some limitations of the present study should be addressed (e.g., the lack of functional and molecular data for the cardiovascular and ocular systems and the absence of a control trained group), our observations led us to conclude that ET may be an effective tool in preventing metabolic abnormalities, as well as AP and IOP increases promoted by a high-fructose diet in rats. We also observed that ocular benefits in response to ET were associated with peripheral autonomic improvements despite the consumption of a high-fructose diet. Thus, by preventing an increase of peripheral sympathetic modulation, other structural and functional changes in the eyes of subjects with metabolic syndrome may be improved, highlighting the importance of autonomic benefits of ET in this pathological condition.
Acknowledgments
Research supported by FAPESP (#2007/58942-0; #2012/20141-5) and CNPq (#482520/2009-4; #306011/2010-7; #479766/2011-8). B. Rodrigues, K. De Angelis, and M.C. Irigoyen received financial support from CNPq-BPQ.
Footnotes
First published online.
References
- 1.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 2.Kaur J. A comprehensive review on metabolic syndrome. Cardiol Res Pract. 2014;2014:943162. doi: 10.1155/2014/943162. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 3.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome - a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23:469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 4.Kolovou GD, Anagnostopoulou KK, Salpea KD, Mikhailidis DP. The prevalence of metabolic syndrome in various populations. Am J Med Sci. 2007;333:362–371. doi: 10.1097/MAJ.0b013e318065c3a1. [DOI] [PubMed] [Google Scholar]
- 5.Moussavi N, Gavino V, Receveur O. Could the quality of dietary fat, and not just its quantity, be related to risk of obesity? Obesity. 2008;16:7–15. doi: 10.1038/oby.2007.14. [DOI] [PubMed] [Google Scholar]
- 6.Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr. 2010;91:535–546. doi: 10.3945/ajcn.2009.27725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tiniakos DG, Vos MB, Brunt EM. Nonalcoholic fatty liver disease: pathology and pathogenesis. Annu Rev Pathol. 2010;5:145–171. doi: 10.1146/annurev-pathol-121808-102132. [DOI] [PubMed] [Google Scholar]
- 8.Poudyal H, Panchal SK, Ward LC, Waanders J, Brown L. Chronic high-carbohydrate, high-fat feeding in rats induces reversible metabolic, cardiovascular, and liver changes. Am J Physiol Endocrinol Metab. 2012;302:E1472–E1482. doi: 10.1152/ajpendo.00102.2012. [DOI] [PubMed] [Google Scholar]
- 9.Renaud HJ, Cui JY, Lu H, Klaassen CD. Effect of diet on expression of genes involved in lipid metabolism, oxidative stress, and inflammation in mouse liver-insights into mechanisms of hepatic steatosis. PLoS One. 2014;9: doi: 10.1371/journal.pone.0088584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elliott SS, Keim NL, Stern JS, Teff K, Havel PJ. Fructose, weight gain, and the insulin resistance syndrome. Am J Clin Nutr. 2002;76:911–922. doi: 10.1093/ajcn/76.5.911. [DOI] [PubMed] [Google Scholar]
- 11.Basciano H, Federico L, Adeli K. Fructose, insulin resistance, and metabolic dyslipidemia. Nutr Metab. 2005;2:5. doi: 10.1186/1743-7075-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mostarda C, Moraes-Silva IC, Salemi VM, Machi JF, Rodrigues B, De Angelis K, et al. Exercise training prevents diastolic dysfunction induced by metabolic syndrome in rats. Clinics. 2012;67:815–820. doi: 10.6061/clinics/2012(07)18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morvan E, Lima NE, Machi JF, Mostarda C, De Angelis K, Irigoyen MC, et al. Metabolic, hemodynamic and structural adjustments to low intensity exercise training in a metabolic syndrome model. Cardiovasc Diabetol. 2013;12:89. doi: 10.1186/1475-2840-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bunnag P, Hori MT, Ormsby B, Berger ME, Golub MS, Tuck ML. Impaired in vivo adrenergic responses in diet-induced hypertensive rats. Hypertens Res. 1997;20:17–21. doi: 10.1291/hypres.20.17. [DOI] [PubMed] [Google Scholar]
- 15.Verma S, Bhanot S, McNeill JH. Sympathectomy prevents fructose-induced hyperinsulinemia and hypertension. Eur J Pharmacol. 1999;373:R1–R4. doi: 10.1016/S0014-2999(99)00301-5. [DOI] [PubMed] [Google Scholar]
- 16.Kamide K, Rakugi H, Higaki J, Okamura A, Nagai M, Moriguchi K, et al. The renin-angiotensin and adrenergic nervous system in cardiac hypertrophy in fructose-fed rats. Am J Hypertens. 2002;15:66–71. doi: 10.1016/S0895-7061(01)02232-4. [DOI] [PubMed] [Google Scholar]
- 17.Wu SY, Leske MC. Associations with intraocular pressure in the Barbados Eye Study. Arch Ophthalmol. 1997;115:1572–1576. doi: 10.1001/archopht.1997.01100160742012. [DOI] [PubMed] [Google Scholar]
- 18.Lazaro C, Garcia-Feijoo J, Castillo A, Perea J, Martinez-Casa JM, Garcia-Sanchez J. Impact of intraocular pressure after filtration surgery on visual field progression in primary open-angle glaucoma. Eur J Ophthalmol. 2007;17:357–362. doi: 10.1177/112067210701700313. [DOI] [PubMed] [Google Scholar]
- 19.Kim YH, Jung SW, Nam GE, Do Han K, Bok AR, Baek SJ, et al. High intraocular pressure is associated with cardiometabolic risk factors in South Korean men: Korean National Health and Nutrition Examination Survey, 2008-2010. Eye. 2014;28:672–679. doi: 10.1038/eye.2014.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang YC, Lin JW, Wang LC, Chen HM, Hwang JJ, Chuang LM. Association of intraocular pressure with the metabolic syndrome and novel cardiometabolic risk factors. Eye. 2010;24:1037–1043. doi: 10.1038/eye.2009.247. [DOI] [PubMed] [Google Scholar]
- 21.Roque FR, Hernanz R, Salaices M, Briones AM. Exercise training and cardiometabolic diseases: focus on the vascular system. Curr Hypertens Rep. 2013;15:204–214. doi: 10.1007/s11906-013-0336-5. [DOI] [PubMed] [Google Scholar]
- 22.Moore CG, Epley D, Milne ST, Morrison JC. Long-term non-invasive measurement of intraocular pressure in the rat eye. Curr Eye Res. 1995;14:711–717. doi: 10.3109/02713689508998499. [DOI] [PubMed] [Google Scholar]
- 23.Pattyn N, Cornelissen VA, Eshghi SR, Vanhees L. The effect of exercise on the cardiovascular risk factors constituting the metabolic syndrome: a meta-analysis of controlled trials. Sports Med. 2013;43:121–133. doi: 10.1007/s40279-012-0003-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malin SK, Niemi N, Solomon TP, Haus JM, Kelly KR, Filion J, et al. Exercise training with weight loss and either a high- or low-glycemic index diet reduces metabolic syndrome severity in older adults. Ann Nutr Metab. 2012;61:135–141. doi: 10.1159/000342084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tran LT, MacLeod KM, McNeill JH. Selective alpha(1)-adrenoceptor blockade prevents fructose-induced hypertension. Mol Cell Biochem. 2014;392:205–211. doi: 10.1007/s11010-014-2031-5. [DOI] [PubMed] [Google Scholar]
- 26.Schlaich M, Straznicky N, Lambert E, Lambert G. Metabolic syndrome: a sympathetic disease? Lancet Diabetes Endocrinol. 2014 doi: 10.1016/S2213-8587(14)70033-6. (in press) [DOI] [PubMed] [Google Scholar]
- 27.Huggett RJ, Hogarth AJ, Mackintosh AF, Mary DA. Sympathetic nerve hyperactivity in non-diabetic offspring of patients with type 2 diabetes mellitus. Diabetologia. 2006;49:2741–2744. doi: 10.1007/s00125-006-0399-9. [DOI] [PubMed] [Google Scholar]
- 28.Brito JO, Ponciano K, Figueroa D, Bernardes N, Sanches IC, Irigoyen MC, et al. Parasympathetic dysfunction is associated with insulin resistance in fructose-fed female rats. Braz J Med Biol Res. 2008;41:804–808. doi: 10.1590/S0100-879X2008005000030. [DOI] [PubMed] [Google Scholar]
- 29.Lee MK, Cho SI, Kim H, Song YM, Lee K, Kim JI, et al. Epidemiologic characteristics of intraocular pressure in the Korean and Mongolian populations: the Healthy Twin and the GENDISCAN study. Ophthalmology. 2012;119:450–457. doi: 10.1016/j.ophtha.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 30.Mori K, Ando F, Nomura H, Sato Y, Shimokata H. Relationship between intraocular pressure and obesity in Japan. Int J Epidemiol. 2000;29:661–666. doi: 10.1093/ije/29.4.661. [DOI] [PubMed] [Google Scholar]
- 31.Hennis A, Wu SY, Nemesure B, Leske MC. Hypertension, diabetes, and longitudinal changes in intraocular pressure. Ophthalmology. 2003;110:908–914. doi: 10.1016/S0161-6420(03)00075-7. [DOI] [PubMed] [Google Scholar]
- 32.Zhang X, Zeng H, Bao S, Wang N, Gillies MC. Diabetic macular edema: new concepts in patho-physiology and treatment. Cell Biosci. 2014;4:27. doi: 10.1186/2045-3701-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li JC, Gupta VK, You Y, Ng KW, Graham SL. The dynamic response of intraocular pressure and ocular pulse amplitude to acute hemodynamic changes in normal and glaucomatous eyes. Invest Ophthalmol Vis Sci. 2013;54:6960–6967. doi: 10.1167/iovs.13-12405. [DOI] [PubMed] [Google Scholar]
- 34.Kishi T, Hirooka Y, Katsuki M, Ogawa K, Shinohara K, Isegawa K, et al. Exercise training causes sympathoinhibition through antioxidant effect in the rostral ventrolateral medulla of hypertensive rats. Clin Exp Hypertens. 2012;34:278–283. doi: 10.3109/10641963.2012.681084. [DOI] [PubMed] [Google Scholar]
- 35.Leosco D, Parisi V, Femminella GD, Formisano R, Petraglia L, Allocca E, et al. Effects of exercise training on cardiovascular adrenergic system. Front Physiol. 2013;4:348. doi: 10.3389/fphys.2013.00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Risner D, Ehrlich R, Kheradiya NS, Siesky B, McCranor L, Harris A. Effects of exercise on intraocular pressure and ocular blood flow: a review. J Glaucoma. 2009;18:429–436. doi: 10.1097/IJG.0b013e31818fa5f3. [DOI] [PubMed] [Google Scholar]
- 37.Roddy G, Curnier D, Ellemberg D. Reductions in intraocular pressure after acute aerobic exercise: a meta-analysis. Clin J Sport Med. 2014;24:364–372. doi: 10.1097/JSM.0000000000000073. [DOI] [PubMed] [Google Scholar]
- 38.Yip JL, Broadway DC, Luben R, Garway-Heath DF, Hayat S, Dalzell N, et al. Physical activity and ocular perfusion pressure: the EPIC-Norfolk eye study. Invest Ophthalmol Vis Sci. 2011;52:8186–8192. doi: 10.1167/iovs.11-8267. [DOI] [PubMed] [Google Scholar]
- 39.Martin B, Harris A, Hammel T, Malinovsky V. Mechanism of exercise-induced ocular hypotension. Invest Ophthalmol Vis Sci. 1999;40:1011–1015. [PubMed] [Google Scholar]
- 40.Gale J, Wells AP, Wilson G. Effects of exercise on ocular physiology and disease. Surv Ophthalmol. 2009;54:349–355. doi: 10.1016/j.survophthal.2009.02.005. [DOI] [PubMed] [Google Scholar]


