Abstract
Introduction
Early acute antibody-mediated rejection (ABMR) occurs more frequently in ABO-incompatible (ABOi) than in ABO-compatible (ABOc) kidney transplantation. This could lead to increased inflammation/scarring in the ABOi grafts. Protocol biopsy data in ABOi kidney recipients are scarce.
Methods
A single-center retrospective matched cohort study was conducted. Eighty adult living donor (LD) renal transplant recipients without HLA donor-specific antibodies (DSA) transplanted between 2009 and 2012 were included; 20 ABOi and 60 ABOc controls matched for donor age and transplantation year. Protocol biopsies at one yr were scored according to the Banff classification. Three sums of scores were constructed: tubulointerstitial inflammation (t + i = 0 vs. >0), microvascular inflammation (g + ptc = 0 vs. >0), scarring/hyalinosis (ci + ct + cv + ah ≤ 1 vs. >1. Scores and presence of subclinical rejection (SCR) at one yr were compared.
Results
Protocol biopsy findings at one yr in the ABOi vs. ABOc matched control group were not statistically different: (t + i) > 0, 30% vs. 20%; (g + ptc) > 0, 5% vs. 8%; (ci + ct + cv + ah) > 1, 85% vs. 60%, respectively. No transplant glomerulopathy occurred. SCR rate at one yr was 30% vs. 18%, subclinical ABMR 5% vs. 7% (all with de novo HLA DSA).
Conclusion
One-year protocol biopsies of ABOi and ABOc LD recipients do not differ in chronic changes, inflammation, or SCRs.
Keywords: ABO incompatible, de novo donor-specific antibodies, kidney transplantation, protocol biopsy, subclinical rejection
Introduction of ABO-incompatible (ABOi) kidney transplantation has increased the possibility of finding suitable living donors (LDs) for patients with end stage renal disease. Historically, plasmapheresis and splenectomy were performed to remove circulating blood group antibodies and to minimize the risk of hyperacute humoral rejection (1–5).
Currently, immunoadsorption or (double-/single-filtration) plasmapheresis, intravenous immunoglobulin (IvIg) and anti-CD20 monoclonal antibody (rituximab) is the standard of care for ABOi kidney transplantation in most centers (6–9). This has lead to a reduction of early acute/active antibody-mediated rejection (ABMR) from 46% to 5–33% (10–16). However, compared to non-HLA-immunized ABO-compatible (ABOc) transplants, ABOi transplants still have an increased risk of acute ABMR during the first months post-transplantation (10,13,15). Antibody-mediated injury in the early phase after transplantation may induce subsequent transplant glomerulopathy (TG) and scarring (10). There is also a risk for development of de novo (dn) HLA donor-specific antibodies (DSA) and chronic ABMR post-transplantation in ABOi transplants (16–20). If ABOi recipients are transplanted with preformed HLA DSA, it is difficult to know whether antibody-mediated biopsy changes are due to blood group incompatibility or due to preformed HLA DSA.
There are few studies with protocol biopsies in ABOi recipients with current immunosuppressive regimes or in recipients without preformed HLA DSA. There is increasing evidence that subclinical rejection (SCR), detected by protocol biopsies, is an important entity. Studies have confirmed that findings in protocol biopsies correlate with later graft outcome (21–23).
No previous study has examined histological changes in biopsies from ABOi recipients compared to a matched group of ABOc controls. All recipients were transplanted without presence of HLA DSA. The ABOc patients were matched for donor age, an important contributor to chronic histological changes and year of transplantation. Protocol biopsies performed at one yr were evaluated for chronic changes including fibrosis, TG, presence of inflammation, and SCR.
Materials and methods
Study population
From January 2009 to December 2012, we performed 1156 renal transplantations, of which 341 were LD transplantations. Eighty adult recipients of LD kidney transplants without presence of preformed HLA DSA or panel-reactive antibodies (PRA) >20% at transplantation and with a valid one-yr protocol biopsy were included (ABOi study group [n = 20]/ABOc controls [n = 60]).
Twenty-five adult ABOi LD kidney transplantations were performed from 2009 to 2012. Five recipients were excluded from the final evaluation (two grafts lost in early acute ABMR, one at polyomavirus nephropathy to cause one-yr biopsy, and two refused biopsy). The ABOc group was randomly selected 3:1 from LD transplantations with a valid one-yr protocol biopsy. Recipients were matched for the period of transplantation, 2009–2010 or 2011–2012, and for donor age ± 5 yr. Children under the age of 16 yr were excluded. Demographic characteristics at baseline and one yr are given in Table1A,B.
Table 1.
Patient and transplant characteristics at (A) baseline and (B) one yr
| ABOi n = 20 | ABOc n = 60 | |
|---|---|---|
| (A) | ||
| Recipient age (yr), mean (±SD) | 47.9 ± 12.2 | 50.0 ± 13.7 |
| Recipient gender (men), n (%) | 15 (75) | 42 (70) |
| Donor age (yr), mean (±SD) | 48.7 ± 8.8 | 50.0 ± 10.1 |
| Donor gender (men), n (%) | 8 (40) | 27 (45) |
| Graft number ≥ 2, n (%) | 8 (40) | 1 (2) |
| HLA mismatches, n (%) | ||
| A + B mismatch ≥ 2 | 13 (65) | 34 (57) |
| DR mismatch ≥ 1 | 18 (90) | 35 (58) |
| Creatinine μmol/l at six wk, mean ± SD | 115.9 ± 24.3 | 115.3 ± 32.8 |
| CMV D+→R−, n (%) | 3 (15) | 5 (8) |
| Anti-A titer IgM, median (range) pre-treatmenta | 32 (4–512) | |
| Anti-A titer IgG, median (range) pre-treatment | 128 (4–1024) | |
| Anti-B titer IgM, median (range) pre-treatmentb | 4 (2–16) | |
| Anti-B titer IgG, median (range) pre-treatment | 4 (4–32) | |
| Anti-A titer IgM, median (range) at transplant | 1 (<1–4) | |
| Anti-A titer IgG, median (range) at transplant | 4 (1–8) | |
| Anti-B titer IgM, median (range) at transplant | <1 (<1–2) | |
| Anti-B titer IgG, median (range) at transplant | <1 (<1–2) | |
| Immunosuppression induction | ||
| Rituximab, n (%) | 12 (60) | 0 |
| IvIg, n (%) | 13 (65) | 0 |
| Basiliximab, n (%) | 20 (100) | 60 (100) |
| (B) | ||
| Hypertension, n (%)c | 13 (65) | 46 (77) |
| Creatinine μmol/L, mean ± SD | 116.4 ± 16.4 | 108.3 ± 24.8 |
| Protein/creatinine ratio, mean ± SD | 12.3 ± 22.7 | 10.0 ± 15.4 |
| De novo HLA DSA, n (%) | 1 (5) | 6 (10) |
| Anti-A titer IgM, median (range)d | 1 (<1–128) | |
| Anti-A titer IgG, median (range) | 4 (<1–64) | |
| Ant-B titer IgM, median (range)d | <1 | |
| Anti-B titer IgG, median (range) | 1 (<1–2) | |
| Calcineurin inhibitor, n (%) | 20 (100) | 58 (97) |
| Tacrolimus/Cyclosporine | 18/2 | 41/17 |
| Everolimus, n (%) | 0 | 2 (3) |
| MMF, n (%) | 19 (95) | 54 (90) |
| Tacrolimus trough, mean ± SD | 7.0 ± 1.8 | 6.1 ± 1.2 |
| Cyclosporine C0 trough, mean ± SD | 139 ± 65 | 115 ± 25 |
ABOi, ABO incompatible; ABOc, ABO compatible; SD, standard deviation; DSA, donor-specific antibody; MMF, mycophenolate mofetil/enteric-coated mycophenolate sodium; HLA, human leukocyte antigen; CMV, cytomegalovirus; D+, donor IgG CMV positive; R−, recipient CMV IgG negative; IvIg, intravenous immunoglobulin.
Anti-A, n = 15.
Anti-B, n = 5.
Hypertension defined by use of at least one antihypertensive drug at one yr.
n = 4, anti-A titer; and n = 1, anti-B titer missing at one yr.
Protocol biopsy
A protocol biopsy was taken 1 yr ± 2 months post-transplantation during a period of stable graft function without acute graft failure or recent immunological event. Two cores were obtained with ultrasound guidance using an 18-gauge spring-loaded biopsy gun, one for histology (hematoxylin and eosin, periodic acid–Schiff, and Masson's trichrome) and one for C4d indirect immunofluorescence staining (monoclonal antibody; Quidel, San Diego, CA, USA). On the frozen section C4d diffuse >50%/grade 3 was classified as positive. Only three ABOc one-yr protocol biopsies were scored for C4d in paraffin-embedded material, all negative (grade 0). Protocol biopsies were assessed and deemed adequate for interpretation by one of four dedicated pathologists and graded according to the revisited Banff 2007 classification and updates (24,25). Adequate biopsy was defined as a specimen with a minimum of seven glomeruli and one artery. Patients with protocol biopsies not fulfilling these criteria were excluded from the study.
Based on the Banff scoring system three sums of scores were constructed, representing tubulointerstitial inflammation (tubulitis [t] + interstitial inflammation [i] = 0, vs. >0), microvascular inflammation (peritubular capillaritis [ptc] + glomerulitis [g] = 0, vs. >0), scarring/hyalinosis (interstitial fibrosis [ci] + tubular atrophy [ct] + intima fibrosis [cv] + arteriolar hyalinosis [ah] ≤ 1, vs. >1). Sis et al. (26) proposed that pathological lesions are not independent, but members of groups, where microcirculation changes reflect stress of DSA and scarring, hyalinosis and arterial fibrosis cumulative burden of injury over time.
Data collection
Clinical data were obtained by chart reviews. The follow-up data were retrieved from the Norwegian Renal Registry. Follow-up time was defined as time from transplantation to death, graft loss (defined as need for dialysis or retransplantation) or to end of study December 31, 2013. No patient was lost to follow-up, and complete data for HLA dnDSA and Banff scoring at one yr were available. The study was conducted in accordance with the Helsinki Declaration and approved by the regional ethical committee and the institutional review board.
Definition and treatment of subclinical and clinical TCMR and ABMR in ABOi and ABOc patients
Subclinical borderline rejections, defined by a Banff score of at least i0t1, did not receive any additional treatment. The subclinical and clinical T-cell-mediated rejection (TCMR), defined as Banff IA (at least i2t2), received methylprednisolone i.v. The details of our protocol for treatment of clinical TCMR and ABMR are described earlier (27).
Clinical and subclinical ABMR/mixed rejection diagnosis in ABOi and ABOc were classified according to the Banff 2013 report (25). The treatment of subclinical ABMR was individualized.
Histocompatibility testing
Pre-transplantation donor and recipient HLA typing (A, B, DR, and DQ) was performed twice by a combination of serological and DNA-based techniques. HLA-C and DP typing was performed if the recipient had anti-HLA-C or HLA-DP antibodies. Cytotoxic T- and B-cell cross-matches were negative at transplantation in all recipients. Additional testing on the Luminex platform LX200, using the LSM12-screening kit (One Lambda, Canoga Park, CA, USA), for the identification of HLA class I and class II IgG antibody specificities was performed using single-antigen-coated flow beads provided by One Lambda at transplantation, indication biopsy and one yr post-transplant. We used 1000 mean fluorescence intensity as a cutoff value. As a negative control, we used serum (LS-NC) delivered by the kit producer (One Lambda). No patient had HLA DSA or PRA > 20% prior to or at transplantation.
Titration of ABO blood group antibodies and ABOi immunoadsorption protocol
Anti-A or anti-B titers of the recipient were determined using gel hemagglutination titration technique, both for immunoglobulin (Ig) M and IgG. Titrations were performed using microtubes of saline (NaCl) gel card (Micro Typing System; BioRad, Cressier sur Morat, Switzerland) and Liss/Coombs gel card (DiaMed ID), respectively. Recipients’ anti-A/anti-B titers were tested against donor erythrocytes by direct agglutination in NaCl for titration of IgM and the indirect agglutination using indirect antiglobulin test for IgG (28).
ABO antigen-specific immunoadsorption (GS, GlycosorbABO®; Glycorex Transplantation AB, Lund, Sweden) was performed preoperatively until ABO IgG/IgM titers were <1:8, routinely on four d, or as needed (29). Immunoadsorption post-transplant was performed on demand if a titer rise ≥1:32 appeared <3 wk post-transplantation or on indication due to rejection.
From June 2009, the number of pre-transplant immunoadsorptions was tailored according to the highest measured titer pre-transplantation. If the baseline anti-A or anti-B IgG/IgM titers were <1:1 no immunoadsorption was performed, <1:16 two, <1:128 four, 1:128 five, and 1:256 six to seven immunoadsorptions were scheduled. The level of anti-A/anti-B titers pretreatment at transplantation and at one yr is shown in Table1A,B.
Immunosuppression
Standard immunosuppression in all patients consisted of induction with basiliximab, calcineurin inhibitor (CNI), mycophenolate mofetil (MMF), and prednisolone. Due to participation in a clinical study, two patients in the ABOc group were switched to the mTOR-inhibitor everolimus seven wk post-transplantation. Table1A,B shows immunosuppression by group.
CNI, mostly tacrolimus 0.05 mg/kg, twice daily was started day 0. In the ABOi group, initial tacrolimus target was 8–12 μg/L at day 1–30, 6–10 μg/L at day 31–60, and after day 60 the same target as the ABOc patients. In the ABOc group, tacrolimus target was 3–7 μg/L from day of transplantation. Nineteen patients received cyclosporine (two ABOi/17 ABOc). In the ABOi recipients, the initial cyclosporine C2 target was 1400–1600 μg/L at day 1–30, 900–1100 μg/L at day 30–60, and tapered from week 9 to reach 500–700 μg/L at month 7. For ABOc recipients, the initial cyclosporine C2 target was 900–1100 μg/L (C0 150–250 μg/L) and tapered from week 5 to reach 500–700 μg/L (C0 75–125 μg/L) at month 7. One dose of methylprednisolone 250 mg intravenously (i.v.) was given at transplantation. Prednisolone was started at 20 mg/d and tapered to 15 mg by day 15, 10 mg from day 29, 7.5 mg from day 60, and 5 mg from month 7. All patients used steroids at one yr. MMF 0.75 g twice daily was administered with concomitant tacrolimus and 1 g twice daily with cyclosporine.
In ABOi transplantation, one intravenous dosage of anti-CD20 monoclonal antibody rituximab 375 mg/m2 was administered four wk prior to transplantation and oral immunosuppression with MMF 1 g × 2 and prednisolone 30 mg was started on day-14. On day 1, IvIg 500 mg/kg bodyweight was administered. From May 2011 until June 2012, rituximab and IvIg were not used for induction of ABOi patients, and five of 20 ABOi patients were transplanted by this protocol. In addition, three ABOi patients received only IvIg induction. Due to two early severe acute ABMR, not included in the study population, we returned to our previously used protocol.
Infectious disease prophylaxis, monitoring, and diagnosis
Our approach to infectious disease prophylaxis, monitoring, and diagnosis post-transplantation had already been described in detail elsewhere (27). From 2012, all cytomegalovirus D+→R− transplants received valganciclovir prophylaxis for six months. There were no biopsy-proven polyomavirus-associated nephropathies detected in the study population. Two vs. nine patients at 10 wk and 1 vs. 6 at one yr were polyomavirus PCR positive in blood, respectively in the ABOi and ABOc group.
Statistical analysis
Statistical analyses were performed using SPSS (SPSS 20.0, Chicago, IL, USA). Data are reported as mean (SD), median (total range), or frequencies (%). Protocol biopsy findings at one yr and categorical data of the two groups were compared using conditional logistic regression. Continuous data were analyzed with repeated measures ANOVA, if not normal distributed with Friedman's test. p-values < 0.05 were considered statistically significant.
Results
Protocol biopsy findings
At one yr, there were no statistically significant differences between the ABOi and ABOc groups concerning the combined scores for microvascular inflammation, tubulointerstitial inflammation, and scarring/hyalinosis (Table2). The detected inflammation in both the tubulointerstitial and the microvascular compartment was low grade. Chronic damage was also of low grade in the majority of cases (Table2, Fig.1A,B). There were three of 20 patients in the ABOi group and five of 60 patients in the ABOc group with a scarring/hyalinosis score higher than 4 of maximal 12.
Table 2.
Findings in protocol biopsies at one yr after transplantation
| ABOi n = 20 | ABOc n = 60 | p-value | |
|---|---|---|---|
| Interstitial inflammation, i | |||
| i score > 0, n (%) | 5 (25) | 7 (12) | 0.58 |
| Mean i score ± SD | 0.3 ± 0.57 | 0.18 ± 0.54 | |
| Tubulitis, t | |||
| t score > 0, n (%) | 5 (25) | 11 (18) | 0.77 |
| Mean t score ± SD | 0.3 ± 0.57 | 0.23 ± 0.53 | |
| Glomerulitis, g | |||
| g score > 0, n (%) | 1 (5) | 4 (7) | 0.95 |
| Mean g score ± SD | 0.05 ± 0.22 | 0.07 ± 0.25 | |
| Capillaritis, ptc | |||
| ptc score > 0, n (%) | 0 | 4 (7) | NA |
| Mean ptc score ± SD | 0 | 0.08 ± 0.33 | |
| Interstitial fibrosis, ci/IF | |||
| ci score > 0, n (%) | 17 (85) | 31 (58) | 0.054 |
| Mean ci score ± SD | 1.0 ± 0.56 | 0.53 ± 0.54 | |
| Tubulus atrophy, ct/TA | |||
| ct score > 0, n (%) | 18 (90) | 42 (70) | 0.14 |
| Mean ct score ± SD | 1.1 ± 0.64 | 0.72 ± 0.49 | |
| Intima fibrosis, cv | |||
| Score > 0, n (%) | 7 (35) | 18 (30) | 0.82 |
| Mean score ± SD | 0.7 ± 1.13 | 0.47 ± 0.85 | |
| Arteriolar hyalinosis, ah | |||
| Score > 0, n (%) | 6 (30) | 14 (23) | 0.76 |
| Mean score ± SD | 0.35 ± 0.59 | 0.25 ± 0.47 | |
| Transplant glomerulopathy, cg | 0 | 0 | NA |
| C4d > 50%, n (%) | 15 (75) | 3 (5) | 0.002 |
| C4d > 10%, n (%) | 17 (85) | 3 (5) | |
| t + i > 0, n (%) | 6 (30) | 12 (20) | 0.42 |
| g + ptc > 0, n (%) | 1 (5) | 5 (8) | 0.64 |
| ci + ct + cv + ah > 1, n (%) | 17 (85) | 36 (60) | 0.24 |
| ci + ct (IFTA) > 1 | 16 (80) | 28 (47) | 0.085 |
| Subclinical rejection at one yr, n (%) | 6 (30) | 11 (18) | 0.33 |
| ABMR, n (%) | 1 (5) | 0 | |
| ABMR + borderline, mixed, n (%) | 0 | 4 (7) | |
| Banff IA, n (%) | 0 | 2 (3) | |
| Borderline, n (%) | 5 (25) | 5 (8) | |
ABOi, ABO incompatible; ABOc, ABO compatible; NA, not applicable; SD, standard deviation; C4d, complement component 4d; ABMR, antibody-mediated rejection.
Fig 1.
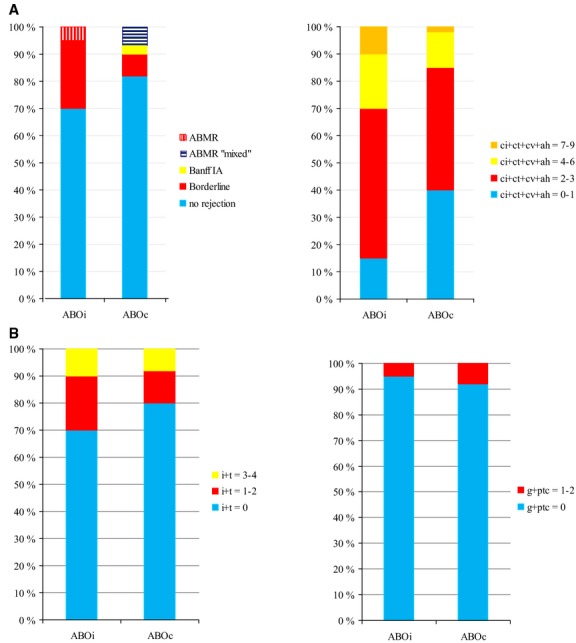
(A) Biopsy findings at one yr – subclinical rejections (SCRs) and Banff (scarring) scores: interstitial fibrosis (ci) + tubular atrophy (ct) + intima fibrosis (cv) + arteriolar hyalinosis (ah). (B) Biopsy findings at one yr – tubulointerstitial (i + t) and microvascular (g + ptc) inflammation. ABO incompatible (ABOi), n = 20; and ABO compatible (ABOc), n = 60 match/control.
The occurrence of SCR was similar in the two groups (Table2). Subclinical ABMR was diagnosed in one ABOi patient. Mixed ABMR/borderline changes were found in four patients, all in the ABOc group. The patient with subclinical ABMR in the ABOi group had low blood group antibody titer IgG 1/IgM < 1 at one yr. All five patients with subclinical ABMR/mixed ABMR received their first kidney transplant, had one DR-HLA mismatch, and developed dnDSA at one yr. Overall, one ABOi and six ABOc patients had developed dn HLA DSA at one yr; the difference was not statistically significant (details presented in Table3). By light microscopy, none of the patients in the study showed evidence of TG.
Table 3.
Patients with de novo HLA DSA at one yr post-transplant, de novo HLA DSA class, mean fluorescence intensity (MFI), and one-yr protocol biopsy characteristics
| Age, gender KTx no. HLA mm (A-B-DR) | dn DSA class, specificity (MFI) | ∑ MFI | Banff score | Banff classification | Immunosuppression at one yr |
|---|---|---|---|---|---|
| ABOi n = 1/20 | |||||
| Patient no. 1a 37 yr, male, 1.KTx (1-1-1) | Class I A2 (3500) B8 (2800) Class II DR17 (1170) DQ2 (5700) | 13 170 | i1t0v0 ptc0, g1 C4d3 pos. cv0, ah0, ci1, ct1 | ABMR | Standard |
| ABOc 6/60 | |||||
| Patient no. 2 22 yr, male 1.KTx (1-0-1) | Class I A68 (1500) | 1500 | i2t1v0, ptc1, g1 C4d3 pos. cv0, ah0, ci1, ct1 | ABMR + borderline | MMF reduced |
| Patient no. 3 29 yr, male 1.KTx (1-1-1) | Class II DQ7 (7700) | 7700 | i2t1v0, ptc2, g0 C4d0 neg. cv0, ah0, ci1, ct1 | ABMR + borderline | MMF reduced |
| Patient no. 4 42 yr, male 1.KTx (0-1-1) | Class II DQ7 (4300) | 4300 | i0t1v0 ptc0, g0 C4d3 pos. cv0, ah1, ci1, ct1 | Suspicious ABMR + borderline | Standard |
| Patient no. 5 55 yr, male 1.KTx (1-1-1) | Class II DQ7 (6000) | 6000 | i0t0v0 ptc0, g0 C4d0 neg. cv1, ah1 ci0, ct0 | No rejection | Standard |
| Patient no. 6 66 yr, male 1.KTx (1-1-1) | Class II DQ6 (2200) | 2200 | i0t1v0 ptc1, g1 C4d0 neg. cv0, ah0, ci1, ct1 | ABMR + borderline | Low tacrolimus trough level around 3 |
| Patient no. 7 27 yr, male 1.KTx (1-1-1) | Class II DR52 (1700) DR17 (3100) DQ2 (9500) | 14 300 | i0t0v0 ptc0, g0 C4d3 pos. cv0, ah0, ci0, ct1 | No rejection | Standard Comment Three months later-mixed ABMR i3t3v0, ptc3, g1, C4d3 pos. |
KTx no., kidney transplantation number; HLA mm, human leukocyte antigen mismatch; dn DSA, de novo donor-specific antibody; ABOi, ABO incompatible; ABOc, ABO compatible; ABMR, antibody-mediated rejection; MMF, mycophenolate mofetil/enteric-coated mycophenolate sodium; i, interstitial inflammation; t, tubulitis; v, vasculitis; ptc, peritubular capillaritis; g, glomerulitis; C4d, complement component 4d; pos, positive; neg, negative; cv, intima fibrosis; ah, arteriolar hyalinosis; ci, interstitial fibrosis; ct, tubulus atrophy.
Anti-blood group antibodies IgM/IgG < 1.
The median follow-up time was 2.3 yr (range 1.1–5 yr). There were no statistically significant differences between the groups neither in the use of ACE inhibitors/ARBs, calcium inhibitors, β-blockers, or statins at one yr nor in the demographic baseline and transplant characteristics at one yr (Table1A,B).
Acute clinical rejections prior to one yr post-transplantation
During the first six months post-transplantation, biopsy-verified acute clinical rejections were diagnosed in four of 20 ABOi patients compared to nine of 60 in ABOc patients. In the ABOi group, there were two mixed acute ABMR/TCMR episodes (one Banff IIA and one IB rejection), both occurring before postoperative day 15. In addition, one Banff IA was diagnosed on day 15, and one borderline rejection occurred four months post-transplant. The two ABOi patients with mixed rejection episodes received rituximab and IvIg induction. Only one of the ABOi patients with early mixed acute ABMR/TCMR experienced a marginal rise in blood type IgG 16/IgM 32 titer at clinical rejection, and the others did not show a rise in blood type IgG/IgM during clinical or SCR. The nine rejection episodes in the ABOc group were all TCMR (three Banff IIA, one IIB, two Banff IA/B, and three borderline rejections) occurring at median 34 d (range 3 d to 4.5 months) post-transplantation.
Patient mortality
Two patients in the ABOi and one in the ABOc group died with functioning grafts. Causes of death in the ABOi group were cardiovascular (n = 1) and septicemia (n = 1), time to death 1.5 and 2.8 yr, respectively; and in the ABOc group, cancer coli (n = 1), time to death 2.2 yr.
Kidney graft function
There were no statistically significant differences in kidney graft function at one yr post-transplantation as shown in Table1B. No graft was lost during follow-up.
Discussion
This is the first study reporting one-yr surveillance biopsy findings in ABOi kidney graft recipients compared to a matched group of ABOc controls, all HLA DSA negative pre-transplant. One-yr protocol biopsies showed a low rate of tubulointerstitial and microvascular inflammation, and there was no difference between the ABOi and the matched ABOc group. All recipients with subclinical ABMR had developed dn HLA DSA. Although scarring/hyalinosis scores were present in 85% and 60% and IFTA > 1 in 80% and 47% in ABOi and ABOc group, respectively, it was low grade and not significantly different between the groups. TG was not found in any biopsy at one yr.
The rate of early acute ABMR was 2/20 (10%) in ABOi patients in the present study, comparable to 5–32% in other reports (12,13,15). ABMR and the presence of DSA increase the risk for development of TG (10,13,15). A recent study on surveillance biopsy data from the Mayo Clinic presented TG in 3% and 8% in ABOc cross-match-negative recipients, 11% and 12% in ABOi recipients, and 29% and 58% in cross-match-positive recipients at one and five yr post-transplant (15). In ABOi recipients, the incidence of TG at one yr varies from 0% to 15% (10,12,13,15). In the present study, we found no TG, neither in the ABOi nor in the ABOc recipients. The study population was recruited 2009–2012 and thoroughly screened for HLA DSA before transplantation. The rate of early acute ABMR was low. This may explain the lack of TG in our study.
There was no difference in the rate of microinflammation or subclinical ABMR in the ABOi and ABOc groups. Seven patients (one of 20 ABOi patients and six of 60 ABOc patients) developed dn HLA DSA within one yr post-transplant. All patients with subclinical ABMR acquired dn HLA DSA. Recent publications in unselected low-risk populations demonstrate that 11–35% of patients develop dnDSA during the first years post-transplant (30–33) and that these patients experience a higher rate of acute rejections (32–34). We have shown that dn HLA DSA is prevalent in patients with late ABMR, and this represents a risk for inferior graft survival (27). Data on dn HLA DSA in ABOi recipients are scarce. In the present study, dn HLA DSA, and not blood group, antibodies appear to be a risk factor for development of microvascular inflammation and subclinical ABMR at one yr.
In one-yr protocol biopsies, we found positive C4d staining to be more frequent in the ABOi group than in the ABOc group, 15/20 vs. 3/60, respectively. The ABOi biopsies were characterized by a constellation of a low rate of microvascular inflammation and a high rate of complement activation. In ABOc allografts, C4d is a marker of antibody-mediated complement activation and ABMR (35,36). In ABOi grafts, C4d is often positive without histological features of ABMR (37,38), and an endothelial accommodation process has been proposed (39).
Eighty-five percent of biopsies in the ABOi and 60% in the ABOc group had a scarring score > 1. The scores were predominantly low grade. These findings are in accordance with other studies (10,13,15). Both inflammatory and scarring mean scores were low in ABOi recipients in our study. These findings imply encouraging outcomes for our patients, and in several reports, graft survival of ABOi LD transplantation equals ABOc transplantations (4,6,11,15). Using the Scientific Registry of Transplant Recipients, Montgomery et al. (40) found inferior graft survival in ABOi transplantation, the difference was mainly caused by early graft losses. During the study period, we lost two ABOi grafts due to early ABMR at our center.
Studies on outcome of ABOi transplants are difficult to compare. The studies vary by era, differences in methods for detection of blood group and HLA antibodies, and different immunosuppressive protocols. These factors may contribute to differences in findings. The strength of our study was the completeness of biopsy data, together with complete data on dn HLA DSA. Due to the retrospective design of most studies, data often are missing. Also the design of our study with a matched control group from a recent time period is a strength. In addition, no patients with preformed HLA DSA were included in any of the groups. Data on protocol biopsies together with dn HLA DSA in ABOi patients are rarely published (41). Some limitations in our study merit consideration. There were a limited number of ABOi patients with one-yr protocol biopsy data, which we share with other studies (10,12,13,15).
It should also be mentioned that we do not perform electron microscopy routinely and may have missed early ultrastructural changes (42).
In conclusion; one-yr biopsies of ABOi and ABOc controls matched for donor age and transplantation year did not differ in inflammation, SCR, and scarring. The chronic changes/scarring, although affecting the majority of patients, were low grade. Microvascular inflammation >0 was low grade and only found in 5% and 8%, respectively, mainly in patients with dn HLA DSA. No development of TG was found in any of the groups. If early graft losses caused by ABMR can be avoided, our findings suggest similar long-term results for ABOi and ABOc recipients. For both patient groups, strategies to avoid dn HLA DSA are warranted.
Acknowledgments
The authors acknowledge the team of the Immunology Laboratory Ullevål for their excellent and enthusiastic support in establishing the ABOi renal transplant program in Norway. CD was supported by a grant from the Norwegian Foundation for Health and Rehabilitation.
Authors’ contributions
Christina Dörje, Geir Mjøen, and Anna Varberg Reisæter: Initiated the study, and Christina Dörje collected data, wrote the first draft, and participated in design and data analysis; Geir Mjøen and Milada Cvancarova: Performed the statistical analysis; Geir Mjøen, Erik H. Strøm, Hallvard Holdaas, Trond Jenssen, Ole Øyen, Çigdem Akalin Akkök, Milada Cvancarova, Karsten Midtvedt, and Anna Varberg Reisæter: All participated in the design, data analysis, and writing of the manuscript.
References
- 1.Alexandre GP, Squifflet JP, De Bruyere M, et al. Present experiences in a series of 26 ABO-incompatible living donor renal allografts. Transplant Proc. 1987;19:4538. [PubMed] [Google Scholar]
- 2.Tanabe K, Takahashi K, Sonda K, et al. Long-term results of ABO-incompatible living kidney transplantation: a single-center experience. Transplantation. 1998;65:224. doi: 10.1097/00007890-199801270-00014. [DOI] [PubMed] [Google Scholar]
- 3.Gloor JM, Lager DJ, Moore SB, et al. ABO-incompatible kidney transplantation using both A2 and non-A2 living donors. Transplantation. 2003;75:971. doi: 10.1097/01.TP.0000058226.39732.32. [DOI] [PubMed] [Google Scholar]
- 4.Ichimaru N, Takahara S. Japan's experience with living-donor kidney transplantation across ABO barriers. Nat Clin Pract Nephrol. 2008;4:682. doi: 10.1038/ncpneph0967. [DOI] [PubMed] [Google Scholar]
- 5.Montgomery RA, Locke JE, King KE, et al. ABO incompatible renal transplantation: a paradigm ready for broad implementation. Transplantation. 2009;87:1246. doi: 10.1097/TP.0b013e31819f2024. [DOI] [PubMed] [Google Scholar]
- 6.Tyden G, Donauer J, Wadstrom J, et al. Implementation of a protocol for ABO-incompatible kidney transplantation–a three-center experience with 60 consecutive transplantations. Transplantation. 2007;83:1153. doi: 10.1097/01.tp.0000262570.18117.55. [DOI] [PubMed] [Google Scholar]
- 7.Morath C, Becker LE, Leo A, et al. ABO-incompatible kidney transplantation enabled by non-antigen-specific immunoadsorption. Transplantation. 2012;93:827. doi: 10.1097/TP.0b013e31824836ae. [DOI] [PubMed] [Google Scholar]
- 8.Fuchinoue S, Ishii Y, Sawada T, et al. The 5-year outcome of ABO-incompatible kidney transplantation with rituximab induction. Transplantation. 2011;91:853. doi: 10.1097/TP.0b013e31820f08e8. [DOI] [PubMed] [Google Scholar]
- 9.Muramatsu M, Gonzalez HD, Cacciola R, Aikawa A, Yaqoob MM, Puliatti C. ABO incompatible renal transplants: good or bad? World J Transplant. 2014;4:18. doi: 10.5500/wjt.v4.i1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gloor JM, Cosio FG, Rea DJ, et al. Histologic findings one year after positive crossmatch or ABO blood group incompatible living donor kidney transplantation. Am J Transplant. 1841;2006:6. doi: 10.1111/j.1600-6143.2006.01416.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilpert J, Fischer KG, Pisarski P, et al. Long-term outcome of ABO-incompatible living donor kidney transplantation based on antigen-specific desensitization. An observational comparative analysis. Nephrol Dial Transplant. 2010;25:3778. doi: 10.1093/ndt/gfq229. [DOI] [PubMed] [Google Scholar]
- 12.Flint SM, Walker RG, Hogan C, et al. Successful ABO-incompatible kidney transplantation with antibody removal and standard immunosuppression. Am J Transplant. 1016;2011:11. doi: 10.1111/j.1600-6143.2011.03464.x. [DOI] [PubMed] [Google Scholar]
- 13.Setoguchi K, Ishida H, Shimmura H, et al. Analysis of renal transplant protocol biopsies in ABO-incompatible kidney transplantation. Am J Transplant. 2008;8:86. doi: 10.1111/j.1600-6143.2007.02036.x. [DOI] [PubMed] [Google Scholar]
- 14.Tobian AA, Shirey RS, Montgomery RA, et al. ABO antibody titer and risk of antibody-mediated rejection in ABO-incompatible renal transplantation. Am J Transplant. 2010;10:1247. doi: 10.1111/j.1600-6143.2010.03103.x. [DOI] [PubMed] [Google Scholar]
- 15.Bentall A, Herrera LP, Cornell LD, et al. Differences in chronic intragraft inflammation between positive crossmatch and ABO-incompatible kidney transplantation. Transplantation. 2014;98:1089. doi: 10.1097/TP.0000000000000188. [DOI] [PubMed] [Google Scholar]
- 16.Toki D, Ishida H, Setoguchi K, et al. Acute antibody-mediated rejection in living ABO-incompatible kidney transplantation: long-term impact and risk factors. Am J Transplant. 2009;9:567. doi: 10.1111/j.1600-6143.2008.02538.x. [DOI] [PubMed] [Google Scholar]
- 17.Kohei N, Hirai T, Omoto K, Ishida H, Tanabe K. Chronic antibody-mediated rejection is reduced by targeting B-cell immunity during an introductory period. Am J Transplant. 2012;12:469. doi: 10.1111/j.1600-6143.2011.03830.x. [DOI] [PubMed] [Google Scholar]
- 18.Yamanaga S, Watarai Y, Yamamoto T, et al. Frequent development of subclinical chronic antibody-mediated rejection within 1 year after renal transplantation with pre-transplant positive donor-specific antibodies and negative CDC crossmatches. Hum Immunol. 2013;74:1111. doi: 10.1016/j.humimm.2013.06.022. [DOI] [PubMed] [Google Scholar]
- 19.Ashimine S, Watarai Y, Yamamoto T, et al. Neither pre-transplant rituximab nor splenectomy affects de novo HLA antibody production after renal transplantation. Kidney Int. 2014;85:425. doi: 10.1038/ki.2013.291. [DOI] [PubMed] [Google Scholar]
- 20.Hirai T, Furusawa M, Omoto K, Ishida H, Tanabe K. Analysis of predictive and preventive factors for de novo DSA in kidney transplant recipients. Transplantation. 2014;98:443. doi: 10.1097/TP.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 21.Loupy A, Suberbielle-Boissel C, Hill GS, et al. Outcome of subclinical antibody-mediated rejection in kidney transplant recipients with preformed donor-specific antibodies. Am J Transplant. 2009;9:2561. doi: 10.1111/j.1600-6143.2009.02813.x. [DOI] [PubMed] [Google Scholar]
- 22.Thierry A, Thervet E, Vuiblet V, et al. Long-term impact of subclinical inflammation diagnosed by protocol biopsy one year after renal transplantation. Am J Transplant. 2011;11:2153. doi: 10.1111/j.1600-6143.2011.03695.x. [DOI] [PubMed] [Google Scholar]
- 23.Heilman RL, Devarapalli Y, Chakkera HA, et al. Impact of subclinical inflammation on the development of interstitial fibrosis and tubular atrophy in kidney transplant recipients. Am J Transplant. 2010;10:563. doi: 10.1111/j.1600-6143.2009.02966.x. [DOI] [PubMed] [Google Scholar]
- 24.Solez K, Colvin RB, Racusen LC, et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant. 2008;8:753. doi: 10.1111/j.1600-6143.2008.02159.x. [DOI] [PubMed] [Google Scholar]
- 25.Haas M, Sis B, Racusen LC, et al. Banff 2013 meeting report: inclusion of c4d-negative antibody-mediated rejection and antibody-associated arterial lesions. Am J Transplant. 2014;14:272. doi: 10.1111/ajt.12590. [DOI] [PubMed] [Google Scholar]
- 26.Sis B, Einecke G, Chang J, et al. Cluster analysis of lesions in nonselected kidney transplant biopsies: microcirculation changes, tubulointerstitial inflammation and scarring. Am J Transplant. 2010;10:421. doi: 10.1111/j.1600-6143.2009.02938.x. [DOI] [PubMed] [Google Scholar]
- 27.Dorje C, Midtvedt K, Holdaas H, et al. Early versus late acute antibody-mediated rejection in renal transplant recipients. Transplantation. 2013;96:79. doi: 10.1097/TP.0b013e31829434d4. [DOI] [PubMed] [Google Scholar]
- 28.Kumlien G, Wilpert J, Safwenberg J, Tyden G. Comparing the tube and gel techniques for ABO antibody titration, as performed in three European centers. Transplantation. 2007;84(12 Suppl):S17. doi: 10.1097/01.tp.0000296019.85986.af. [DOI] [PubMed] [Google Scholar]
- 29.Kumlien G, Ullstrom L, Losvall A, Persson LG, Tyden G. Clinical experience with a new apheresis filter that specifically depletes ABO blood group antibodies. Transfusion. 2006;46:1568. doi: 10.1111/j.1537-2995.2006.00927.x. [DOI] [PubMed] [Google Scholar]
- 30.Gill JS, Landsberg D, Johnston O, et al. Screening for de novo anti-human leukocyte antigen antibodies in nonsensitized kidney transplant recipients does not predict acute rejection. Transplantation. 2010;89:178. doi: 10.1097/TP.0b013e3181c3503e. [DOI] [PubMed] [Google Scholar]
- 31.Wiebe C, Gibson IW, Blydt-Hansen TD, et al. Evolution and clinical pathologic correlations of de novo donor-specific HLA antibody post kidney transplant. Am J Transplant. 2012;12:1157. doi: 10.1111/j.1600-6143.2012.04013.x. [DOI] [PubMed] [Google Scholar]
- 32.Devos JM, Gaber AO, Teeter LD, et al. Intermediate-term graft loss after renal transplantation is associated with both donor-specific antibody and acute rejection. Transplantation. 2014;97:534. doi: 10.1097/01.TP.0000438196.30790.66. [DOI] [PubMed] [Google Scholar]
- 33.Dieplinger G, Ditt V, Arns W, et al. Impact of de novo donor-specific HLA antibodies detected by Luminex solid-phase assay after transplantation in a group of 88 consecutive living-donor renal transplantations. Transpl Int. 2014;27:60. doi: 10.1111/tri.12207. [DOI] [PubMed] [Google Scholar]
- 34.Cooper JE, Gralla J, Cagle L, Goldberg R, Chan L, Wiseman AC. Inferior kidney allograft outcomes in patients with de novo donor-specific antibodies are due to acute rejection episodes. Transplantation. 2011;91:1103. doi: 10.1097/TP.0b013e3182139da1. [DOI] [PubMed] [Google Scholar]
- 35.Feucht HE, Schneeberger H, Hillebrand G, et al. Capillary deposition of C4d complement fragment and early renal graft loss. Kidney Int. 1993;43:1333. doi: 10.1038/ki.1993.187. [DOI] [PubMed] [Google Scholar]
- 36.Collins AB, Schneeberger EE, Pascual MA, et al. Complement activation in acute humoral renal allograft rejection: diagnostic significance of C4d deposits in peritubular capillaries. J Am Soc Nephrol. 1999;10:2208. doi: 10.1681/ASN.V10102208. [DOI] [PubMed] [Google Scholar]
- 37.Haas M, Rahman MH, Racusen LC, et al. C4d and C3d staining in biopsies of ABO- and HLA-incompatible renal allografts: correlation with histologic findings. Am J Transplant. 1829;2006:6. doi: 10.1111/j.1600-6143.2006.01356.x. [DOI] [PubMed] [Google Scholar]
- 38.Haas M, Segev DL, Racusen LC, et al. C4d deposition without rejection correlates with reduced early scarring in ABO-incompatible renal allografts. J Am Soc Nephrol. 2009;20:197. doi: 10.1681/ASN.2008030279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Park WD, Grande JP, Ninova D, et al. Accommodation in ABO-incompatible kidney allografts, a novel mechanism of self-protection against antibody-mediated injury. Am J Transplant. 2003;3:952. doi: 10.1034/j.1600-6143.2003.00179.x. [DOI] [PubMed] [Google Scholar]
- 40.Montgomery JR, Berger JC, Warren DS, James NT, Montgomery RA, Segev DL. Outcomes of ABO-incompatible kidney transplantation in the United States. Transplantation. 2012;93:603. doi: 10.1097/TP.0b013e318245b2af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shirakawa H, Ishida H, Shimizu T, et al. The low dose of rituximab in ABO-incompatible kidney transplantation without a splenectomy: a single-center experience. Clin Transplant. 2011;25:878. doi: 10.1111/j.1399-0012.2010.01384.x. [DOI] [PubMed] [Google Scholar]
- 42.Haas M, Mirocha J. Early ultrastructural changes in renal allografts: correlation with antibody-mediated rejection and transplant glomerulopathy. Am J Transplant. 2011;11:2123. doi: 10.1111/j.1600-6143.2011.03647.x. [DOI] [PubMed] [Google Scholar]


