Abstract
OBJECTIVES:
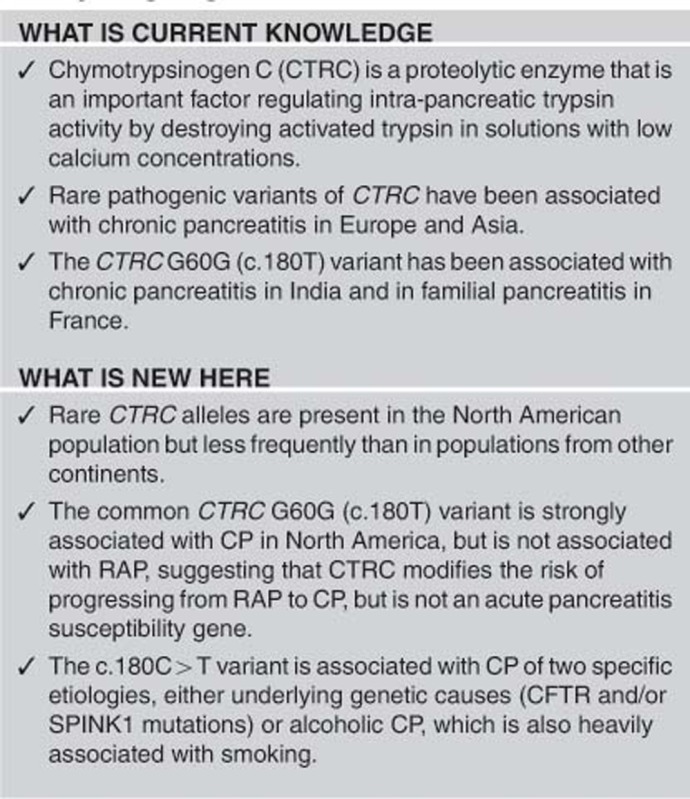
Recurrent acute pancreatitis (RAP) is a complex inflammatory disorder that may progress to fibrosis and other irreversible features recognized as chronic pancreatitis (CP). Chymotrypsinogen C (CTRC) protects the pancreas by degrading prematurely activated trypsinogen. Rare mutations are associated with CP in Europe and Asia. We evaluated the occurrence of CTRC variants in subjects with RAP, CP, and controls from the North American Pancreatitis Study II cohort.
METHODS:
CP (n=694), RAP (n=448), and controls (n=1017) of European ancestry were evaluated. Subgroup analysis included CFTR and SPINK1 variants, alcohol, and smoking.
RESULTS:
We identified previously reported rare pathogenic CTRC A73T, R254W, and K247_R254del variants, intronic variants, and G60G (c.180 C>T; rs497078). Compared with controls (minor allele frequency (MAF)=10.8%), c.180T was associated with CP (MAF=16.8%, P<0.00001) but not RAP (MAF=11.9% P=NS). Trend test indicated co-dominant risk for CP (CT odds ratio (OR)=1.36, 95% confidence interval (CI)=1.13–1.64, P=0.0014; TT OR=3.98, 95% CI=2.10–7.56, P<0.0001). The T allele was significantly more frequent with concurrent pathogenic CFTR variants and/or SPINK1 N34S (combined 22.9% vs. 16.1%, OR 1.92, 95% C.I. 1.26–2.94, P=0.0023) and with alcoholic vs. non-alcoholic CP etiologies (20.8% vs. 12.4%, OR=1.9, 95% CI=1.30–2.79, P=0.0009). Alcohol and smoking generally occurred together, but the frequency of CTRC c.180 T in CP, but not RAP, was higher among never drinkers–ever smokers (22.2%) than ever drinker–never smokers (10.8%), suggesting that smoking rather than alcohol may be the driving factor in this association.
CONCLUSIONS:
The common CTRC variant c.180T acts as disease modifier that promotes progression from RAP to CP, especially in patients with CFTR or SPINK1 variants, alcohol, or smoking.
INTRODUCTION
The chronic pancreatitis (CP) syndrome (ICD9 577.1, ICD10 K86.x) encompasses inflammatory disorders of the pancreas characterized by recurrent acute pancreatitis (RAP) or chronic pancreatic inflammation with variable fibrosis, calcifications, morphologic changes, and progressive loss of functional parenchyma, leading to endocrine and exocrine insufficiency, pain and risk of pancreatic adenocarcinoma.2 CP is responsible for some of the worst quality-of-life scores of any chronic disease.3 Based on the imaging criteria, the prevalence of CP in the United States is 41 cases per 100,000 people,4 and we estimate that the prevalence of cases with a history of RAP is about three times higher.4 Thus, the RAP and CP syndrome is not a rare disorder.
There are important distinctions between acute pancreatitis (AP), RAP, and CP. AP is a syndrome of sudden pancreatic injury followed by an acute inflammatory response. The diagnosis of AP is based on clinical criteria of pancreatic inflammation leading to typical pain, release of pancreatic digestive enzymes into the blood stream and/or detection of edema or other markers of inflammation of the pancreatic gland and surrounding tissue using abdominal imaging methods.5, 6, 7 AP can be a serious medical problem, because the magnitude of the inflammatory response is typically many times greater than is expected from similar amount of injury to other tissues because of the activation of trypsinogen to trypsin within the pancreas.5, 8
Trypsin is a serine protease of broad specificity that is normally activated in the duodenum to serve as a nutrient protease and as the primary activator of other pancreatic digestive enzymes. Premature activation of trypsin in the pancreatic acinar cell or within the pancreatic duct can lead to direct cell injury, indirect tissue injury through the effect of activating other pancreatic digestive enzymes, and cross-activation of the immune system. In addition to the acute inflammatory response, AP events initiate the activation, proliferation, and survival of pancreatic stellate cells, which are normally involved in pancreatic tissue healing, and under pathological conditions, fibrosis.9, 10
Patients with one episode of AP are susceptible to RAP. The risk of RAP can often be reduced if the proximal etiological factor is removed. Examples include removal of the gallbladder to reduce the risk of recurrent biliary AP11, 12 and stopping alcohol consumption to prevent recurrent alcoholic pancreatitis.13, 14 Effective treatments are not yet available for patients with genetic variants that increase susceptibility to AP such as cationic trypsinogen gene (PRSS1) mutations,15, 16 and therefore patients with genetic risk or idiopathic pancreatitis typically suffer from RAP. Patients with RAP from any etiology may, but will not always, develop CP. RAP typically precedes CP by 2–5 years, but the rate of progression is highly variable,17, 18, 19, 20 indicating both a sequenced process and the effect of modifying factors. About a quarter of patients with CP do not have clinically recognized AP prior to diagnosis (below), but the fact that the majority of CP patients do have such a history suggest that this is a major pathological pathway as envisioned in the Sentinel Acute Pancreatitis Event model.21, 22, 23
The paradigm of the RAP-to-CP sequence seen in genetic disorders such as hereditary pancreatitis has been replicated in population-based epidemiological studies of non-genetic etiologies, such as alcoholic AP and idiopathic AP. After an incident of AP, the risk of developing CP over the next 10 years is five times higher in patients with RAP then those without RAP,19 indicating that RAP is a major risk factor for the later development of CP.13, 18, 19, 24
Although there is no consensus definition of CP, recent practice guidelines25, 26, 27, 28 have adopted a pragmatic definition of CP based on signs of pancreatic fibrosis and gland distortion following recommendations proposed by the Pancreatic Society of Great Britain and Ireland, known as the Cambridge Classification.29 The Cambridge definition of CP is based on abdominal imaging criteria with identification of duct system distortion associated with fibrosis, supported by features of calcifications or atrophy, but not other complications of chronic injury and inflammation, such as gland dysfunction or pain. Fibrosis represents an abnormal immune response to injury mediated through macrophages and stellate cells, which are scarce in the native pancreas prior to an initial episode of AP.9, 10 Thus, in the majority of cases, clinical evidence of fibrosis follows two distinct steps, each with different risk factors. The first is recurrent injury, such as RAP, which is linked to trypsin activation in the pancreatic acinar and duct cells. The second step is an extreme or abnormal immune response to pancreatic injury30, 31 mediated through activated pancreatic stellate cells.
Based on a review of clinical studies, about a third of patients with AP will develop RAP and about a third of RAP patients will develop CP.4, 19, 32 The risk of progression is the highest in patients with hereditary pancreatitis and those with exposure to environmental factors, such as alcohol and tobacco. Thus RAP is a risk factor of future development of CP, but RAP alone is not sufficient to cause CP.
Within established academic clinical pancreas centers, two subgroups of patients can be identified, those with well-established RAP and no significant evidence of fibrosis on abdominal imaging studies such as CT scan (defined as RAP patients), and those with evidence of pancreatic fibrosis on abdominal imaging (defined as CP patients).1 Based on the known relationship between RAP and CP, the factors associated with susceptibility to RAP should also be associated with CP, but not all factors associated with CP are associated with RAP. Factors only associated with CP are linked to the second step, which involves the immune response and generation of fibrosis and presumed exposure to immune-modifying factors, whether environmental, genetic, or both. Although this is a dominant theme, there is clearly heterogeneity, which we believe is a function of both the severity and/or repetition of the injury and the individual's immune response to (recurrent) pancreatic injury. Thus, in the North American Pancreatitis Study II (NAPS2) study, we test for pancreatitis susceptibility using controls vs. RAP+CP and for susceptibility to fibrosis by comparing RAP and CP. If a potential risk factor is identified, then the nature of it being a protective factor or a CP risk factor can be explored by comparing RAP with controls (differences indicate protection from progression) and CP with controls (differences indicate risk of progression).
Alcohol and smoking are risk factors for CP, but other risk factors are also required as most people who smoke and drink do not develop CP. Most genetic factors associated with RAP/CP are also linked to mechanisms that normally protect the pancreas from intra-pancreatic trypsin activation. These include the cationic trypsinogen gene (PRSS1),15, 16 the cystic fibrosis transmembrane conductance regulator gene (CFTR),33, 34 and the serine protease inhibitor Kasal type 1 (SPINK1).35, 36 Other trypsin-regulating genes appear to be disease modifiers with a lower independent risk such as the calcium-sensing receptor gene (CaSR),37, 38 the gamma-glutamyltransferase 1 gene (GGT1),39 and the chymotrypsinogen C gene (CTRC)40, 41 as recently reviewed.23, 42, 43, 44 Exceptions to the trypsin activation pathway include the CLDN2 locus, which is a risk factor for progression from RAP to CP, especially in men with heavy alcohol use45 and rare carboxypeptidase A (CPA) variants, which appear to drive fibrosis through the unfolded protein response.46
Possible associations between CTRC variants and RAP/CP have not been reported in North American Populations. Genetic association studies from Europe and Asia have identified rare CTRC variants that are associated with CP, but they differ between populations, and associations with specific rare variants have been difficult to replicate.40, 41, 47, 48 The most commonly reported rare variants (minor allele frequency <5%) across all these studies have been R254W and K246_R254del, although multiple novel mutations have been identified.40, 41, 47, 48
The strongest evidence for a role of CTRC in pancreatitis is from functional studies. CTRC is a Ca2+-dependent serine protease that can rapidly degrade all three human trypsinogen and is likely the protective agent identified by Rinderknecht as enzyme Y.49 Functional studies on the CTRC protein by the Sahin-Tóth laboratory40, 50, 51 have shown convincingly that CTRC has a key role in a major mechanism of trypsin auto-digestion and that loss-of-function mutations in CTRC disrupt this mechanism. Thus the strong biological plausibility of a protective role for CTRC against trypsin-dependent pancreatic injury and pancreatitis is supported by both population genetic and functional studies.
The primary aim of this study was to replicate the association between pathogenic CTRC variants and pancreatitis in a North American population. An additional aim was to determine whether there were interactions between CTRC variants and other risk factors for RAP or CP, such as alcohol use or smoking.
METHODS
Study population
NAPS2 and NAPS2 validation (NAPS2-CV) cohorts have been described in detail.1, 45, 52 All NAPS2 subjects were recruited and consented by expert physicians using IRB (Institutional Review Board)-approved protocols. Prospectively collected demographic and phenotypic information included race, sex, family history, exposure to environmental risk factors (including alcohol and smoking history52), natural history of the disease (chronology of change in symptoms and status), and physician assessment of etiology. RAP was defined by more than one episode of documented AP (typical abdominal pain with elevation of pancreatic enzyme >3 × normal or imaging evidence of AP), and CP was defined using imaging criteria or histology.1 Alcohol and smoking histories were taken in detail and were categorized by both usage (non-user, ex-user, or current) and average threshold (smoking pack years 0, 1–12, 12–35, ≥35; average weekly alcohol intake (quantity–frequency criteria, i.e., average amount consumed on a drinking day and the number of days per month that this amount was consumed): abstainers: no alcohol use or <20 drinks in lifetime; light drinkers: ≤3 drinks/week; moderate drinkers: 4–7 drinks/week for females; 4–14 drinks/week for males; heavy drinkers: 8–34 drinks/week for females; 15–34 drinks/week for males; and very heavy drinkers: ≥35 drinks/week.) An additional 296 de-identified healthy control DNA samples were provided by SomaLogic, Inc. (Boulder, CO) and included demographic information (sex, age, ethnicity), drinking status, smoking status, and personal medical history (described in Whitcomb et al.45). Additional healthy controls were also obtained from an inflammatory bowel disease (IBD) case–control study (Dr Richard Duerr, University of Pittsburgh) (n=309 healthy non-IBD controls), variables included age, sex, race, and smoking data.
DNA preparation and mutations analysis
Peripheral blood leukocyte DNA was purified as described.1 PCR primers were designed for CTRC gene exons 2, 3, and 7 and the corresponding intronic regions that contain most of the commonly reported mutations reported in Germany, India, France, and Taiwan.40, 41, 47, 48, 53
PCR was performed in a total volume of 25 μl; 200 nmol of forward and reverse primers, 200 μmol of dNTP and 1 × PCR buffer II (ABI, Foster City, CA) with 20 ng of DNA. Amplification settings were 95 °C for 12 min × 1 cycle, 95 °C for 30 s, annealing temperature × 30 s and 72 °C × 20 s for 35 cycles, and 72 °C for 2 min × 1 cycle. Annealing temperatures and magnesium concentrations for different primers are available on request. PCR amplification products were treated with exonuclease I (NEB, Beverley, MA) and shrimp alkaline phosphatase (Roche Diagnostics, Indianapolis, IN) and then purified by ethanol EDTA precipitation, according to the manufacturer's recommendations. For restriction fragment length polymorphisms (RFLP) analysis, the 463-bp amplification product of exon 7 sequencing as described above was digested with SmaI (New England BioLabs, Frankfurt, Germany) at 37 °C for 2 h. The digestion products were analyzed by electrophoresis in 5% polyacrylamide gel (Bio-Rad, Hercules, CA) and visualized with ethidium bromide staining. For direct sequencing, the PCR products were run on an ABI Prism 3730 Genetic Analyzer, and the sequence was analyzed using Sequencher 4.7 (Gene Codes, Ann Arbor, MI; Cycle sequencing kit v3.1 diluted 1:8 (ABI) using the appropriate PCR primers).
Genotyping of CTRC was done using a multi-step process. An initial group of CP and unrelated controls enrolled sequentially in the NAPS2 cohort were selected for DNA sequencing of exons 2–3 and 7 of CTRC, with final genotypes obtained for 247 Caucasian samples (CP=148, controls=99). Based on the CTRC variants identified in this initial direct sequencing, we tested the remainder of the cohort for the most frequent variants, R254W and G60G. We genotyped the NAPS2 cohort and SomaLogic controls for p.G60G (rs497078) using Taqman single-nucleotide polymorphism genotyping assay (Life Technologies, Carlsbad CA; Assay ID C__2393026) and obtained final genotype data for 755 CP, 429 RAP, 1024 unrelated controls, and 183 family controls. We also extended the genotyping of R254W to all NAPS2 samples using RFLP, a technique that captured both the R254W and K247_R254del mutations, and confirmed all positive and random negative results by sequencing. In total, we collected final genotypes for the exon 7 region in a total of 1512 samples: 128 by sequencing alone, 961 by RFLP, and 423 by a combination of the two.
Genotyping of PRSS1, SPINK1, and CFTR
The NAPS2 cohort was genotyped for known variants in related pancreatitis risk genes PRSS1, SPINK1, and CFTR by a combination of direct sequencing and multiplex genotyping assays (Sequenom, San Diego CA) and individual taqman genotyping assays (Life Technologies) as previously described.54 SPINK1 N34S taqman and PRSS1 rs10273639 genotyping was completed in the NAPS2-CV cohort. PRSS1 rs10273639, CFTR and SPINK1 N34S taqman genotyping was completed in the NAPS2, IBD controls, and SomaLogic control cohorts.
Statistical analysis
STATA SE12.0 (STATAcorp LP, College station, TX) was used to analyze and generate summary statistics of the data set. We compared variation frequency between cases and controls using either the Chi Square test (χ2) or Fisher's exact test and used the Mann–Whitney test to compare age of onset. Odds ratios (ORs) and the corresponding 95% confidence intervals (95% CI) for CP risk were calculated using logistic regression. The Cochran–Armitage test for trend was used to investigate dose effects of c.180C>T. RAP and CP were modeled as having common susceptibilities, with CP occurring over time in the presence of additional disease-modifying factors to test whether associated risk were for pancreatic injury or fibrosis.45, 52 For all statistical comparisons, frequencies of CTRC variants in cases (CP and RAP) or CP or RAP were compared against unrelated controls only; family members genotyped were not included in this analysis. For all tests, P<0.05 was considered significant.
RESULTS
Study population
We compared the demographics, alcohol and smoking classification, and reported etiology of pancreatitis for cases and controls (Table 1). The prevalence of very heavy alcohol use, ever smoking, and current smoking was significantly higher among CP cases than among either RAP cases or unrelated controls; a higher percentage of RAP cases never used alcohol or smoked compared with CP cases and controls. Alcohol usage was not available for the SomaLogic and IBD study healthy control samples.
Table 1. Demographics, self-reported alcohol and smoking, and physician-defined etiology in the study cohort.
| Controls | CP | P value | RAP | P value | CP vs. RAP P value | |
|---|---|---|---|---|---|---|
| Total number | 1017 | 694 | 448 | |||
| Mean age—years (s.d.) | 52.3 (15.8) | 50.5 (16.1) | 0.026 | 46.1 (15.5) | <0.0001 | |
| Male—n (%) | 440 (43.2) | 364 (52.4) | 0.0002 | 201 (44.8) | 0.57 | 0.013 |
| Drinking and smoking | ||||||
| Ever drinker—n/N (%)a | 552/700 (78.9) | 544/683 (79.7) | 0.76 | 332/442 (75.1) | 0.14 | 0.078 |
| Very heavy drinker—n/N (%)b | 25/424 (5.9) | 104/471 (22.1) | <0.0001 | 39/394 (9.9) | 0.033 | <0.0001 |
| Ever smoker—n/N (%) | 468/1009 (46.4) | 491/684 (71.8) | <0.0001 | 246/441 (55.8) | 0.0010 | <0.0001 |
| Current smoker—n/N (%) | 149/1009 (14.8) | 306/684 (44.7) | <0.0001 | 99/441 (22.5) | 0.0003 | <0.0001 |
| Never smoke or drank—n/N (%)a | 100/697 (14.3) | 90/682 (13.2) | 0.54 | 85/438 (19.4) | 0.025 | 0.0068 |
| Alcohol etiology—n/N (%) | — | 284/694 (40.9) | 109/448 (24.3) | <0.0001 | ||
| Age of AP diagnosis, mean years (s.d.) | — | 40.5 (17.9) | 41.6 (16.2) | |||
| Age of CP diagnosis, mean years (s.d.) | — | 47.6 (16.5) | — | |||
AP, acute pancreatitis; CP, chronic pancreatitis; RAP, recurrent acute pancreatitis. Definitions: Ever drinker: consumption of ≥20 drinks during lifetime; very heavy drinker: ≥5 drinks/day during “the period of maximum drinking in life” ever smoker: smoked ≥100 cigarettes during lifetime; current smoker: smoking at the time of study enrollment. Alcohol etiology for RAP and CP is based on the enrolling physician's assessment, with or without additional factors. Reported P-values are on demographics when compared with the control group.
Alcohol status (current, ex, never) was not available for the Duerr controls.
Alcohol usage (light, moderate, heavy, very heavy drinker) was not available for the inflammatory bowel disease study and SomaLogic controls.
Within the NAPS2-CV cohort (n=521 CP cases) we found that a minority (n=134; 25.7%) did not have a history of AP. We could not determine if there were subclinical episodes of AP, but a slight majority of these subjects with CP reported either no pancreatitis pain (n=46; 34.3%) or only limited episodes of mild-to-moderate pain (n=25; 18.7%) so that episodes of AP, typically recognized by pain, may not have been brought to medical attention.
Initial CTRC sequencing and RFLP genotyping of R254W
We identified rare exonic genetic variants in CTRC among the RAP and CP cases (Table 2); genotyping of exon 7 in the expanded cohort identified additional carriers of the rare variant R254W for a final count of 8/677 (1.2%) CP, 3/444 (0.7%) RAP, and 2/404 (0.5%) unrelated controls. The previously reported microdeletion in exon7, K247_R254del was identified in one RAP and one CP patient and no controls (0.1% CP vs. 0.2% RAP vs. 0.0% ctrl). All of the rare variations were found in the heterozygous state, and none were significantly associated with CP or RAP when compared with unrelated controls (Table 2). The mutation carriers had variable age of onset, gender, etiology, and alcohol/tobacco use (detailed in Table 3). Combined, disease-associated CTRC mutations (R254W, A73T, or K247_R254del) were identified in 1.33% of cases (1.62% CP) and 0.50% controls (P=NS). Thus we were unable to confirm statistical association between these rare variants and RAP or CP in this cohort, either individually or in a group.
Table 2. Rare genetic variations in chymotrypsinogen C (CTRC) gene in cases and controls.
| DNA | Amino-acid change | Genotyping strategy | CP | RAP | Controls | P valuea | |
|---|---|---|---|---|---|---|---|
| Exon | |||||||
| 3 | c. 217 G>A | p.A73T | Sequencing | 1/148 (0.6%) | 0/99 (0.0%) | NS | |
| 7 | c.760 C>T | p.R254W | RFLP+Sequencing | 8/677 (1.2%) | 3/444 (0.7%) | 2/404 (0.5%) | NS |
| 7 | c.738_761del24 | p.K247_R254del | RFLP+Sequencing | 1/677 (0.1%) | 1/444 (0.2%) | 0/404 (0.0%) | NS |
| Intron | |||||||
| 6 | c.640-12G>A | Sequencing | 1/148 (0.7%) | 0/99 (0.0%) | NS | ||
| 6 | c.640-42G>C | Sequencing | 2/148 (1.4%) | 0/99 (0.0%) | NS | ||
CP, chronic pancreatitis; NS, not significant; RAP, recurrent acute pancreatitis; RFLP, restriction fragment length polymorphisms. NS, P>0.05. No homozygous or compound homozygous mutations above were identified.
Fisher's test between CP vs. controls.
Table 3. Demographics, alcohol consumption, smoking, etiology, and status of other genetic mutations (CFTR, SPINK1) in carriers of CTRC mutations in NAPS2 cohort.
| Diagnosis | Enrollment age | Sex | CTRC | SPINK1 | CFTR | Etiology | AP.dx age | CP.dx age | Smoker | Drinker | Drinker type |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CP | 53 | F | K247_R254DEL | wt | wt | Alcohol | 45 | 53 | Current | Ex | Heavy |
| CP | 61 | M | R254W | wt | R75Q | Alcohol | — | 51 | Current | Current | Very heavy |
| RAP | 42 | F | R254W | wt | wt | Alcohol | 39 | — | Ex | Current | Heavy |
| CP | 56 | M | R254W | wt | wt | Alcohol | 39 | 40 | Ex | Ex | Very heavy |
| CP | 31 | M | R254W | N34S | F508del | Alcohol | — | 20 | Ex | Ex | Mod |
| RAP | 32 | F | K247_R254DEL | wt | wt | Gallstones | 20 | — | Current | Ex | Heavy |
| RAP | NA | M | R254W | wt | wt | NA | NA | — | NA | NA | NA |
| CP | 46 | M | R254W | wt | wt | Idiopathic | 28 | 44 | Current | Current | Light |
| CP | 33 | M | R254W | wt | wt | Idiopathic | 27 | 28 | Current | No | — |
| CP | 66 | M | R254W | wt | wt | Idiopathic | 60 | 62 | Ex | Ex | NA |
| CP | 64 | F | R254W | wt | wt | Idiopathic | — | 61 | Ex | No | — |
| RAP | 43 | F | R254W | wt | F508del | Idiopathic | 42 | — | No | Current | Light |
| CP | 40 | F | A73T | wt | wt | Idiopathic | — | 40 | No | Ex | Mod |
| CP | 44 | M | R254W | wt | wt | Genetic | 42 | 44 | No | No | — |
| CP | 6 | F | R254W | N34S/N34S | wt | Genetic | 4 | 5 | No | No | — |
| Family | 37 | F | R254W | N34S | wt | — | — | — | Ex | Current | Heavy |
| Control | 47 | M | R254W | wt | wt | — | — | — | Ex | Ex | Very heavy |
| Control | 29 | F | R254W | wt | wt | — | — | — | No | Current | Light |
| CP | 51 | M | c.640-12G>A | wt | NA | Alcohol | 49 | 49 | Current | Current | Very heavy |
| CP | 56 | F | c.640-42G>C | wt | NA | Obstructive | 56 | 56 | Ex | Current | Light |
| CP | NA | M | c.640-42G>C | wt | R75Q | Alcohol | 51 | 51 | Current | Ex | Very heavy |
| Family | 60 | M | c.640-42G>C | wt | NA | — | — | — | Ex | Current | Light |
AP, acute pancreatitis; CP, chronic pancreatitis; CTRC, chymotrypsinogen C; F, female; M, male; NA, data not available; RAP, recurrent acute pancreatitis; wt, genotyping revealed no mutation.
Direct sequencing of exon 3 in the initial cohort of 148 CP and 99 controls identified the common variant CTRC c.180 C>T/A (G60G) with non-significant overrepresentation of the minor T allele in CP, (CP T=15.1%, A=0.4% unrelated controls T=11.1%, A=0%).
Analysis of CTRC c.180 C>T/A (G60G) among RAP and CP
In the expanded genotyping cohort, CTRC c.180T (G60G) was significantly overrepresented in CP (all etiologies) but not RAP patients as compared with unrelated controls (16.8% CP, 11.9% RAP, 10.8% controls) (Table 4). Comparing ORs indicated a dose effect of the minor allele with CT vs. CC OR 1.36, P=0.001 and TT vs. CC OR 3.98, P<0.0001.
Table 4. CTRC G60G genotype frequencies in the study cohort stratification for physician-defined etiology and the presence of PRSS1, CTRC, SPINK1, and CFTR mutations.
| Analysis |
TT vs. CC |
CT vs. CC |
TT/CT vs. CC |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G60G | TT | CT | CC | MAF% | OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value |
| Unrelated controls | 10 | 199 | 804 | 10.8% | |||||||||
| Controls with any known mutation | 0 | 12 | 56 | 8.8% | |||||||||
| All RAP | 7 | 92 | 345 | 11.9% | NS | NS | NS | ||||||
| All CP | 30 | 170 | 484 | 16.8% | 3.98 | 2.10–7.56 | <0.0001 | 1.36 | 1.13–1.64 | 0.0014 | 1.48 | 1.23–1.77 | <0.0001 |
| Known risk mutation (CFTR/SPINK1) | 4 | 42 | 63 | 22.9% | 4.32 | 1.45–12.92 | 0.0044 | 2.04 | 1.39–3.00 | 0.0002 | 2.15 | 1.48–3.12 | <0.0001 |
| Known HP mutation (CTRC/PRSS1) | 1 | 7 | 36 | 10.2% | NS | NS | NS | ||||||
| No known mutations | 25 | 123 | 390 | 16.1% | 5.15 | 2.45–10.84 | <0.0001 | NS | 1.46 | 1.15–1.86 | 0.0022 | ||
| Alcoholic no mutation | 16 | 66 | 154 | 20.8% | 8.35 | 3.72–18.75 | <0.0001 | 1.73 | 1.25–2.40 | 0.0009 | 2.05 | 1.51–2.78 | <0.0001 |
| Non-alcoholic no mutation | 9 | 57 | 236 | 12.4% | 3.066 | 1.23–7.63 | 0.011 | NS | NS | ||||
| Alcoholic CP vs. non-alcoholic CP | 2.72 | 1.17–6.32 | 0.016 | 1.77 | 1.18–2.67 | 0.0056 | 1.90 | 1.30–2.79 | 0.0009 | ||||
CI, confidence interval; CP, chronic pancreatitis; CTRC, chymotrypsinogen C; HP, hereditary pancreatitis; MAF, minor allele frequency; NS, not significant; OR, odds ratio; RAP, recurrent acute pancreatitis. CP patients with any CFTR or SPINK1 mutation (known risk) were investigated separately from those with HP causing mutations (either PRSS1 or CTRC rare alleles) and those with no identified mutations (which included both alcoholic and non-alcoholic etiologies).
Reported OR were made by comparing against all unrelated controls, except for the final. Bold values indicate statistically significant comparison (OR, P-value).
Because of the original report by Masson et al.41 linking c.180C>T with familial CP only, we analyzed the G60G CTRC variant specifically in the background of known genetic risk factors (disease-associated mutations in SPINK1 (N34S), CFTR, CTRC, and PRSS1) and alcohol-associated etiologies. CTRC G60G was in epistasis with CFTR and SPINK1 mutations as reflected by a higher frequency of the T allele among carriers (22.9%) but not with the limited number of PRSS1 or CTRC mutations (10.2%).
We removed the samples with any known genetic risk factors and assessed the impact of c.180C>T within different etiologies. The c.180T allele was most frequent among alcohol-associated CP etiologies either when alcohol was reported as the only cause or with some additional etiological factor (20.8%). The T allele was less frequent among non-alcoholic etiologies (idiopathic, obstructive, autoimmune, etc.) (12.4%) and not significantly overrepresented in this group when compared with controls. The CP cases diagnosed by physicians as having alcohol-related pancreatitis were significantly more likely to have a high-risk G60G T allele than non-alcohol-related CP cases (Table 4, P=0.0009).
To investigate whether alcohol and smoking modify the relationship between G60G and CP, we evaluated the risk of CP with and without alcohol and/or smoking by stratifying cases and controls with no mutations in SPINK1, CFTR, CTRC, and PRSS1 based on self-reported drinking and smoking status (Table 5). Among patients with no known genetic mutations, the association of CTRC G60G with CP was influenced by drinking and smoking status, with the highest frequency seen in the small group of smokers who were never drinkers (22.2%). Although the T allele was significantly overrepresented among CP subjects who both smoke and drank at some point compared with healthy controls with the same history (OR 1.71, P=0.0064), it was also significant among those with smoking only (OR 5.43, P=0.0022) but not with those who drank alcohol but never smoked. The association between CTRC G60G and CP in subjects classified by physicians as having an alcohol-related etiology could be driven by smoking, which is tightly correlated with drinking,24, 52 making further analysis difficult due to sample size. Indeed, 91.8% of CP patients with alcoholic etiology in our cohort were ever smokers and 71.3% were current smokers, in contrast to non-alcoholic CP composing of 57.8% ever smokers and 28.2% current smokers.
Table 5. CTRC G60G carrier frequencies in CP cases and controls (no genetic mutation) with and without smoking or drinking history.
| Drinking and smoking analysis G60G | TT | CT | CC | MAF% | OR TT/CC vs. CC | 95% CI | P value |
|---|---|---|---|---|---|---|---|
| +Ever drinkers+ever smokers | |||||||
| CP | 17 | 87 | 257 | 16.76% | 1.67 | 1.15–2.42 | 0.0064 |
| Controls | 3 | 53 | 231 | 10.28% | |||
| +Ever drinkers−never smokers | |||||||
| CP | 2 | 12 | 60 | 10.81% | NS | ||
| Controls | 4 | 37 | 178 | 10.27% | |||
| −Never drinkers+ever smokers | |||||||
| CP | 1 | 14 | 21 | 22.22% | 5.43 | 1.73–17.04 | 0.0022 |
| Controls | 1 | 4 | 38 | 6.98% | |||
| −Never drinkers−never smokers | |||||||
| CP | 5 | 7 | 44 | 15.18% | NS | ||
| Controls | 0 | 24 | 63 | 13.79% | |||
| Current smokers | |||||||
| CP | 16 | 68 | 163 | 20.24% | 2.08 | 1.27–3.40 | 0.0031 |
| Controls | 1 | 27 | 113 | 10.28% | |||
| Current drinkers | |||||||
| CP | 6 | 43 | 131 | 15.28% | 1.61 | 1.06–2.42 | 0.024 |
| Controls | 4 | 71 | 322 | 9.95% | |||
CI, confidence interval; CP, chronic pancreatitis; CTRC, chymotrypsinogen C; MAF, minor allele frequency; NS, not significant; OR, odds ratio.
Bold values indicate statistically significant comparison (RO, P-value).
DISCUSSION
In the current study, we demonstrate that the CTRC G60G (c.180C>T) variant significantly increases risk of alcohol/smoking or CFTR/SPINK1-associated CP, but not RAP. In addition, we found that the CTRC c.180C>T allele, in a dose-dependent way, significantly increased the risk of CP, but not RAP. These findings may be especially important to the field of medicine, because the high-risk CTRC G60G T allele is common, with a frequency of approximately 10% among Caucasians, and the effect is strong and associated with frequent risk factors such as smoking, alcohol, and SPINK1 or CFTR mutations. Following the Sentinel Acute Pancreatitis Event model,55 the pathogenic CTRC variants become important after an initial attack of AP, providing a window of opportunity for CP-preventing interventions.
The present study is the first from North America and provides several important observations. Our first aim was to replicate the European and South Asian findings of a statistical association between rare variants (A73T, R254W, and K247_R254del) and CP. Although there was a trend, the frequency of these variants in the NAPS2 cohort was too low to confirm statistical association with CP. Our second aim was to evaluate more complex genetic interactions. We attempted to replicate the findings of Masson et al.41 in reporting that CTRC G60G T allele is a risk factor for CP. An important new discovery was that the CTRC c.180C>T allele was not associated with RAP, suggesting that loss of CTRC function accelerates progression from RAP to CP. A second important discovery was demonstration of a strong association between CTRC c.180C>T and CP in subjects with trypsin-dysregulating genetic risks (SPINK1 and CFTR mutations). Finally, we demonstrated that CTRC c.180T allele increases risk of CP in patients with a history of alcohol use and smoking, with the primary effect potentially linked to smoking.
Several important differences were noted between the results of our North American cohort and previous reports. The primary reason appears to be differences in the population demographics and patient characteristics. Masson et al.41 first reported that the common polymorphism c.180 C>T CT genotype to be significantly overrepresented in a small European cohort of CP patients with a positive family history short of hereditary pancreatitis classification (n=42); however, there was no significant association found in idiopathic CP (n=216) or hereditary pancreatitis (n=29) patients in the same study or with the collective cohort or the TT genotype. Follow-up studies in tropical CP48, 56 confirmed the G60G impact in a larger Indian cohort, while a Japanese study57 reported no significance but very few carriers of the T allele (2/506 CP, 0/274 controls). Functionally deleterious CTRC mutations (i.e., R254W, K247_R254del and A73T) were collectively associated with CP in all previous studies, but we were unable to replicate this finding. Aside from the racial variability in c.180C>T frequency between Caucasian, South Asian, and Japanese populations, we note many other differences between the previous studies and ours.
CTRC is believed to provide protection from prematurely activated trypsin in the pancreas.50 Previous studies and reviews documented a high concordance of CTRC variants with CFTR or SPINK1 variants, suggesting that risk is conferred through complex genotypes.56, 58 In addition, alcohol and smoking are major risk factors for CP, but additional risk factors appear to be necessary to specifically target the pancreas.22, 45, 52
The mechanism underlying the pathology associated with CTRC G60G is unknown, but disruption of key regulator elements is likely. The CTRC G60G (c.180C>T, rs497078) variant disrupts a SP-1 nucleotide-binding site. In addition, this single-nucleotide polymorphism is in linkage disequilibrium (R2≥0.8) with other variants altering nucleotide-binding sites, including c.493+52G>A (rs545634) that disrupts an ATF3 site involved in the complex process of cellular stress response and (rs201599742) that disrupts a TATA box and other regulator motifs.59 A disease mechanism linked to disruption of SP-1 and ATF3-binding sites is biologically plausible, as nucleotide-binding factors linked to this site are associated with pancreatic injury responses, including inflammation and fibrosis.60
CTRC clearly has an important role in protecting the pancreas from injury, and the present study clarifies the role. First, the lack of association between pathogenic CTRC variants and RAP indicates that CTRC is not an AP susceptibility factor such as PRSS1 or CFTR but rather a disease modifier. Second, the pathogenic effects of CTRC variants are linked to pathogenic CFTR and SPINK variants resulting in multiple defects in regulating intra-pancreatic trypsin. Third, the higher prevalence of the CTRC G60G haplotype in smokers and alcoholics suggests that CTRC expression is positively regulated by stress. Finally, the high risk of CP in smokers with the CTRC G60G haplotype is provocative, because it suggests that chronic smoking increases stress and that smoking either causes injury through a trypsin-related process or that CTRC has broader functions than degrading trypsin in compartments with low calcium concentrations.
The study has some limitations. We have identified the well-known CTRC mutations R254W, K245_R254del and A73T in CP, but at a lower frequency than in other reported cohorts,40, 41, 48, 50, 56, 57 leading to a discrepancy in the impact of these mutations on North American CP as a whole. Our study was unable to demonstrate association of rare variants with disease despite being a larger cohort than other studies. In addition, we sequenced only three exonic regions in our initial screening study, thus a number of rare or common variants in the untested coding and regulatory regions would be missed. On the other hand, the detailed and mechanism-based phenotyping of the NAPS2 cohort allowed for simultaneous assessment of genetic and environmental factors in this cohort and provided new insights and hypotheses into the mechanism of a complex disorder. Future studies are needed to understand the dynamics of CTRC expression under stress, determining the specific single-nucleotide polymorphisms linked with altered expression, the mechanism of increased risk with alcohol and smoking, and modeling of genetic risk in the background of complex genomic data and environmental factors.
In conclusion, we found that the common synonymous variant CTRC c.180C>T (G60G) is associated with significant risk for CP, but not for RAP. We also demonstrated that the risk of CP in humans is associated with the presence of other genetic factors linked to disregulated intra-pancreatic trypsin activity and RAP and CP such as mutations in CFTR and SPINK1, alcohol, and smoking. As CTRC c.180C>T is in a genetic region that contains multiple nuclear-binding protein sites, we hypothesize that the risk of CP is enhanced by failed response to pancreatic stress, allowing trypsin-activating conditions to drive inflammation and rapid progression to CP.
Study Highlights
Acknowledgments
We thank Jyothsna Talluri, MD for critical review of the manuscript and the following individuals and sites for contributing samples to the NAPS2 programs: NAPS2-CV Sites (Directors). David C. Whitcomb, MD, PhD (Principal Investigator); Samer Alkaade, MD (Saint Louis University, St Louis, MO); Stephen T. Amann, MD (North Mississippi Medical Center, Tupelo, MS); Michelle A. Anderson, MD (Univeristy of Michigan, Ann Arbor, MI); Peter A. Banks, MD (Brigham and Women's Hospital, Boston, MA); Randall E. Brand, MD (Shadyside Medical Center, University of Pittsburgh, Pittsburgh, PA); Gregory Cote', MD (Indiana University, Indianapolis, IN); Timothy B. Gardner, MD (Dartmouth-Hitchcock Medical Center, Hanover, NH); Andres Gelrud, MD (University of Pittsburgh, Pittsburgh, PA and University of Chicago, Chicago, IL); Darwin Conwell, MD (Brigham and Women's Hospital, Boston, MA); Michele D. Lewis, MD (Mayo Clinic, Jacksonville, FL); Thiruvengadam Muniraj, MD, PhD, MRCP (Mercy Medical Center, University of Pittsburgh, Pittsburgh, PA); Joseph Romagnuolo, MD MScEpid (Medical University of South Carolina, Charlestown, SC); Bimaljit Sandhu, MD (Virginia Commonwealth University Medical Center, Richmond, VA); and Adam Slivka, MD, PhD (Presbyterian University Hospital, University of Pittsburgh, Pittsburgh, PA)
NAP2-CV Coordinating Center (Pittsburgh): Steven Wisniewski, PhD (Director); Emil Bauer; M. Michael Barmada, PhD; Bernie Devlin, PhD; Danielle Dwyer; Megan Hendricks; Michelle Kienholz; Jessica LaRusch; Michael O'Connell; Darina Protivak, PhD; Laurie Silfies; Kimberly Stello; Dhiraj Yadav, MD, MPH; and Tian “Mark” Ye, PhD
NAPS2 Sites: David C. Whitcomb, MD PhD (Principal Investigator). University of Pittsburgh, Pittsburgh, PA: Kenneth K. Lee, MD; Arthur James Moser, MD; Georgios Papachristou, MD; Adam Slivka, MD, PhD; and Dhiraj Yadav, MD, MPH. Medical University of South Carolina, Charleston, SC: Peter B. Cotton, MD; Robert H. Hawes, MD; Christopher Lawrence, MD; and Tammy Glen, RN, MSN. CCRC: Evanston Northwestern Healthcare, Evanston, IL: Randal Brand, MD; Nahla Hasabou, MD; and Michael Goldberg, MD. University of Michigan, Ann Arbor, MI: Michelle Anderson, MD; Meredith Korneffel, MD; Grace H. Elta, MD; Erik-Jan Wamsteker, MD; and James M. Scheiman, MD. Brigham and Women's Hospital, Boston, MA: Peter Banks, MD; Darwin Conwell, MD; and Martha Vander Vliet, RN. Duke University Medical Center, Durham, NC: John Baillie M.B., Ch.B; Helen Stiffler, RN, MSN; and Lisa Gray, RN. PC: Paul S. Jowell, MD; and Malcolm S. Branch, MD. Indiana University, Indianapolis, IN: SC: Lee McHenry, MD; Evan Fogel, MD; Glen Lehman, MD; Stuart Sherman, MD; and James Watkins, MD. Laura Lazzell-Pannell, RN, BSN; and Suzette Schmidt, RN, BSN. University of Utah, Salt Lake City, UT: James DiSario, MD; and Nicole Omer. St Louis University, St Louis, MO: Samer Alkaade, MD; Frank Burton, MD; Samer Alkaade, MD; and Kusal Mihindukulasuriya. Dartmouth-Hitchcock Medical Center, Lebanon, NH: Timothy B. Gardner, MD; Christina Engstrom, BS; and Virginia Kelly, RN. Cedars-Sinai Medical Center, University of California, Los Angeles, CA: Simon K. Lo, MD. North Mississippi Medical Center, Tupelo, MS: Stephen Amann, MD; and Melanie Benge, RN. University of Cincinnati, Cincinnati, OH: SC: Andres Gelrud, MD; Patricia Krotchen, PA; Nathan. Schmulewitz, MD; Syed Ahmad, MD; and Shailendra Chauhan, MD. Rush University Medical Center, Chicago, IL: Mark T. DeMeo, MD, Anita Runoweicki, RN; and Sri Komanduri, MD. Washington Hospital Center, Washington, DC: William M. Steinberg, MD. University of Pennsylvania, Philadelphia, PA: Michael L. Kochman, MD; and Gregory G. Ginsberg, MD. Ochsner Clinic, New Orleans, LA: Babak Etemad, MD, and Elizabeth Nix, LPN
NAPS2-Coordinating Center (Pittsburgh): M. Michael Barmada, PhD; Kathy Bauer, RN; Scott Cooper, MD; Beth Elinoff, RN, MPH; Erin Fink, MS; Megan Hendricks, RN; Daniel Mullady, MD; Michael O'Connell, PhD; Amit Raina, MD; Arun Sharma, MD; and Dhiraj Yadav, ME, MPH
Additional Phenotyped Control Samples: Richard Duerr, MD (University of Pittsburgh, Pittsburgh, PA) and Rachel Ostroff (SomaLogic, Boulder, CO). Meredith Goss and Jan Timm from SomaLogic prepared the samples.
Guarantor of the article: David C. Whitcomb, MD, PhD.
Specific Author Contributions: Concept and design: JL, VM, DW, and MO; analysis and interpretation: JL, AM, AL, MO, BD, and KS; drafting and editing of manuscript: JL, DY, DW, BD, and AL; final approval of manuscript: JL and DW.
Financial support: Funding was provided by NIH grants DK061451 (D.C.W.) and DK077906 (D.Y.). Dr LaRusch was supported by T32 DK063922. Dr Lozano was supported by a grant from the Conselleria de Industria e Innovación, Xunta de Galicia. Spain. This project used the UPCI Clinical Genomics Immunoproteomics and Sequencing Facility (NIH P30CA047904) and the University of Pittsburgh Genomics and Proteomics Core Laboratory that was possible, in part, by Grant Number UL1 RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NCRR or NIH.
Potential competing interests: None.
References
- Whitcomb DC, Yadav D, Adam S, et al. Multicenter approach to recurrent acute and chronic pancreatitis in the United States: the North American Pancreatitis Study 2 (NAPS2) Pancreatology. 2008;8:520–531. doi: 10.1159/000152001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etemad B, Whitcomb DC. Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterology. 2001;120:682–707. doi: 10.1053/gast.2001.22586. [DOI] [PubMed] [Google Scholar]
- Amann ST, Yadav D, Barmada MM, et al. Physical and mental quality of life in chronic pancreatitis: a case-control study from the North American Pancreatitis Study 2 Cohort. Pancreas. 2013;42:293–300. doi: 10.1097/MPA.0b013e31826532e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–1261. doi: 10.1053/j.gastro.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitcomb DC. Acute pancreatitis. N Engl J Med. 2006;354:2142–2150. doi: 10.1056/NEJMcp054958. [DOI] [PubMed] [Google Scholar]
- Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. doi: 10.1136/gutjnl-2012-302779. [DOI] [PubMed] [Google Scholar]
- Forsmark CE, Baillie J. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022–2044. doi: 10.1053/j.gastro.2007.03.065. [DOI] [PubMed] [Google Scholar]
- Bhatia M. Acute pancreatitis as a model of SIRS. Front Biosci. 2009;14:2042–2050. doi: 10.2741/3362. [DOI] [PubMed] [Google Scholar]
- Witt H, Apte MV, Keim V, et al. Chronic pancreatitis: challenges and advances in pathogenesis, genetics, diagnosis, and therapy. Gastroenterology. 2007;132:1557–1573. doi: 10.1053/j.gastro.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Bachem MG, Zhou Z, Zhou S, et al. Role of stellate cells in pancreatic fibrogenesis associated with acute and chronic pancreatitis. J Gastroenterol Hepatol. 2006;21 ((Suppl 3:S92–S96. doi: 10.1111/j.1440-1746.2006.04592.x. [DOI] [PubMed] [Google Scholar]
- van Baal MC, Besselink MG, Bakker OJ, et al. Timing of cholecystectomy after mild biliary pancreatitis: a systematic review. Ann Surg. 2012;255:860–866. doi: 10.1097/SLA.0b013e3182507646. [DOI] [PubMed] [Google Scholar]
- Gurusamy KS, Nagendran M, Davidson BR. Early versus delayed laparoscopic cholecystectomy for acute gallstone pancreatitis. Cochrane Database Syst Rev. 2013;9:CD010326. doi: 10.1002/14651858.CD010326.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeyama Y. Long-term prognosis of acute pancreatitis in Japan. Clin Gastroenterol Hepatol. 2009;7 ((11 Suppl:S15–S17. doi: 10.1016/j.cgh.2009.08.022. [DOI] [PubMed] [Google Scholar]
- Nordback I, Pelli H, Lappalainen-Lehto R, et al. The recurrence of acute alcohol-associated pancreatitis can be reduced: a randomized controlled trial. Gastroenterology. 2009;136:848–855. doi: 10.1053/j.gastro.2008.11.044. [DOI] [PubMed] [Google Scholar]
- Whitcomb DC, Gorry MC, Preston RA, et al. Hereditary pancreatitis is caused by a mutation in the cationic trypsinogen gene. Nat Genet. 1996;14:141–145. doi: 10.1038/ng1096-141. [DOI] [PubMed] [Google Scholar]
- Gorry MC, Gabbaizedeh D, Furey W, et al. Mutations in the cationic trypsinogen gene are associated with recurrent acute and chronic pancreatitis. Gastroenterology. 1997;113:1063–1068. doi: 10.1053/gast.1997.v113.pm9322498. [DOI] [PubMed] [Google Scholar]
- Ammann RW. A clinically based classification system for alcoholic chronic pancreatitis: summary of an international workshop on chronic pancreatitis [see comments] Pancreas. 1997;14:215–221. doi: 10.1097/00006676-199704000-00001. [DOI] [PubMed] [Google Scholar]
- Lankisch PG, Breuer N, Bruns A, et al. Natural history of acute pancreatitis: a long-term population-based study Am J Gastroenterol 20091042797–2805.quiz 2806. [DOI] [PubMed] [Google Scholar]
- Yadav D, O'Connell M, Papachristou GI. Natural history following the first attack of acute pancreatitis. Am J Gastroenterol. 2012;107:1096–1103. doi: 10.1038/ajg.2012.126. [DOI] [PubMed] [Google Scholar]
- Howes N, Lerch MM, Greenhalf W, et al. Clinical and genetic characteristics of hereditary pancreatitis in Europe. Clin Gastroenterol Hepatol. 2004;2:252–261. doi: 10.1016/s1542-3565(04)00013-8. [DOI] [PubMed] [Google Scholar]
- Whitcomb DC. Hereditary pancreatitis: new insights into acute and chronic pancreatitis. Gut. 1999;45:317–322. doi: 10.1136/gut.45.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav D, Whitcomb DC. The role of alcohol and smoking in pancreatitis. Nat Rev Gastroenterol Hepatol. 2010;7:131–145. doi: 10.1038/nrgastro.2010.6. [DOI] [PubMed] [Google Scholar]
- Whitcomb DC. Genetic risk factors for pancreatic disorders. Gastroenterology. 2013;144:1292–1302. doi: 10.1053/j.gastro.2013.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cote GA, Yadav D, Slivka A, et al. Alcohol and smoking as risk factors in an epidemiology study of patients with chronic pancreatitis. Clin Gastroenterol Hepatol. 2010;9:266–273. doi: 10.1016/j.cgh.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frulloni L, Falconi M, Gabbrielli A, et al. Italian consensus guidelines for chronic pancreatitis. Dig Liver Dis. 2010;42 (((Suppl 6):S381–S406. doi: 10.1016/S1590-8658(10)60682-2. [DOI] [PubMed] [Google Scholar]
- Martinez J, Abad-Gonzalez A, Aparicio JR, et al. The Spanish Pancreatic Club recommendations for the diagnosis and treatment of chronic pancreatitis: part 1 (diagnosis) Pancreatology. 2013;13:8–17. doi: 10.1016/j.pan.2012.11.309. [DOI] [PubMed] [Google Scholar]
- Mayerle J, Hoffmeister A, Werner J, et al. Chronic pancreatitis--definition, etiology, investigation and treatment. Dtsch Arztebl Int. 2013;110:387–393. doi: 10.3238/arztebl.2013.0387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delhaye M, Van Steenbergen W, Cesmeli E, et al. Belgian consensus on chronic pancreatitis in adults and children: statements on diagnosis and nutritional, medical, and surgical treatment. Acta Gastroenterol Belg. 2014;77:47–65. [PubMed] [Google Scholar]
- Sarner M, Cotton PB. Classification of pancreatitis. Gut. 1984;25:756–759. doi: 10.1136/gut.25.7.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng X, Wang L, Elm MS, et al. Chronic alcohol consumption accelerates fibrosis in response to cerulein-induced pancreatitis in rats. Am J Pathol. 2005;166:93–106. doi: 10.1016/S0002-9440(10)62235-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gukovsky I, Lugea A, Shahsahebi M, et al. A rat model reproducing key pathological responses of alcoholic chronic pancreatitis. Am J Physiol Gastrointest Liver Physiol. 2008;294:G68–G79. doi: 10.1152/ajpgi.00006.2007. [DOI] [PubMed] [Google Scholar]
- Yadav D. Recent advances in the epidemiology of alcoholic pancreatitis. Curr Gastroenterol Rep. 2011;13:157–165. doi: 10.1007/s11894-011-0177-9. [DOI] [PubMed] [Google Scholar]
- Cohn JA, Friedman KJ, Noone PG, et al. Relation between mutations of the cystic fibrosis gene and idiopathic pancreatitis. N Engl J Med. 1998;339:653–658. doi: 10.1056/NEJM199809033391002. [DOI] [PubMed] [Google Scholar]
- Sharer N, Schwarz M, Malone G, et al. Mutations of the cystic fibrosis gene in patients with chronic pancreatitis. N Engl J Med. 1998;339:645–652. doi: 10.1056/NEJM199809033391001. [DOI] [PubMed] [Google Scholar]
- Witt H, Luck W, Hennies HC, et al. Mutations in the gene encoding the serine protease inhibitor, Kazal type 1 are associated with chronic pancreatitis. Nat Genet. 2000;25:213–216. doi: 10.1038/76088. [DOI] [PubMed] [Google Scholar]
- Pfutzer RH, Barmada MM, Brunskill AP, et al. SPINK1/PSTI polymorphisms act as disease modifiers in familial and idiopathic chronic pancreatitis. Gastroenterology. 2000;119:615–623. doi: 10.1053/gast.2000.18017. [DOI] [PubMed] [Google Scholar]
- Felderbauer P, Hoffmann P, Einwachter H, et al. A novel mutation of the calcium sensing receptor gene is associated with chronic pancreatitis in a family with heterozygous SPINK1 mutations. BMC Gastroenterol. 2003;3:34. doi: 10.1186/1471-230X-3-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muddana V, Lamb J, Greer JB, et al. Association between calcium sensing receptor gene polymorphisms and chronic pancreatitis in a US population: Role of serine protease inhibitor Kazal 1type and alcohol. World J Gastroenterol. 2008;14:4486–4491. doi: 10.3748/wjg.14.4486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand H, Diergaarde B, O'Connell MR, et al. Variation in the gamma-glutamyltransferase 1 gene and risk of chronic pancreatitis. Pancreas. 2013;42:836–840. doi: 10.1097/MPA.0b013e318279f720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosendahl J, Witt H, Szmola R, et al. Chymotrypsin C (CTRC) variants that diminish activity or secretion are associated with chronic pancreatitis. Nat Genet. 2008;40:78–82. doi: 10.1038/ng.2007.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masson E, Chen JM, Scotet V, et al. Association of rare chymotrypsinogen C (CTRC) gene variations in patients with idiopathic chronic pancreatitis. Hum Genet. 2008;123:83–91. doi: 10.1007/s00439-007-0459-3. [DOI] [PubMed] [Google Scholar]
- Solomon S, Whitcomb DC. Genetics of pancreatitis: an update for clinicians and genetic counselors. Curr Gastroenterol Rep. 2012;14:112–117. doi: 10.1007/s11894-012-0240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitcomb DC. Genetics of alcoholic and nonalcoholic pancreatitis. Curr Opin Gastroenterol. 2012;28:501–506. doi: 10.1097/MOG.0b013e328356e7f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen JM, Ferec C. Genetics and pathogenesis of chronic pancreatitis: the 2012 update. Clin Res Hepatol Gastroenterol. 2012;36:334–340. doi: 10.1016/j.clinre.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Whitcomb DC, Larusch J, Krasinskas AM, et al. Common genetic variants in the CLDN2 and PRSS1-PRSS2 loci alter risk for alcohol-related and sporadic pancreatitis. Nat Genet. 2012;44:1349–1354. doi: 10.1038/ng.2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt H, Beer S, Rosendahl J, et al. Variants in CPA1 are strongly associated with early onset chronic pancreatitis. Nat Genet. 2013;45:1216–1220. doi: 10.1038/ng.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang MC, Chang YT, Wei SC, et al. Association of novel chymotrypsin C gene variations and haplotypes in patients with chronic pancreatitis in Chinese in Taiwan. Pancreatology. 2009;9:287–292. doi: 10.1159/000199437. [DOI] [PubMed] [Google Scholar]
- Derikx MH, Szmola R, te Morsche RH, et al. Tropical calcific pancreatitis and its association with CTRC and SPINK1 (p.N34S) variants. Eur J Gastroenterol Hepatol. 2009;21:889–894. doi: 10.1097/MEG.0b013e32832183cf. [DOI] [PubMed] [Google Scholar]
- Szmola R, Sahin-Toth M. Chymotrypsin C (caldecrin) promotes degradation of human cationic trypsin: identity with Rinderknecht's enzyme Y. Proc Natl Acad Sci USA. 2007;104:11227–11232. doi: 10.1073/pnas.0703714104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beer S, Zhou J, Szabo A, et al. Comprehensive functional analysis of chymotrypsin C (CTRC) variants reveals distinct loss-of-function mechanisms associated with pancreatitis risk. Gut. 2012;62:1616–1624. doi: 10.1136/gutjnl-2012-303090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo A, Sahin-Toth M. Determinants of chymotrypsin C cleavage specificity in the calcium binding loop of human cationic trypsinogen. FEBS J. 2012;279:4283–4292. doi: 10.1111/febs.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav D, Hawes RH, Brand RE, et al. Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis. Arch Intern Med. 2009;169:1035–1045. doi: 10.1001/archinternmed.2009.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitahara K, Kawa S, Katsuyama Y, et al. Microsatellite scan identifies new candidate genes for susceptibility to alcoholic chronic pancreatitis in Japanese patients. Dis Markers. 2008;25:175–180. doi: 10.1155/2008/426764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaRusch J, Jung J, General IJ, et al. Mechanisms of CFTR functional variants that impair regulated bicarbonate permeation and increase risk for pancreatitis but not for cystic fibrosis. PLoS Genet. 2014;10:e1004376. doi: 10.1371/journal.pgen.1004376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitcomb DC. Genetic polymorphisms in alcoholic pancreatitis. Dig Dis. 2005;23:247–254. doi: 10.1159/000090172. [DOI] [PubMed] [Google Scholar]
- Paliwal S, Bhaskar S, Mani KR, et al. Comprehensive screening of chymotrypsin C (CTRC) gene in tropical calcific pancreatitis identifies novel variants. Gut. 2012;62:1602–1606. doi: 10.1136/gutjnl-2012-302448. [DOI] [PubMed] [Google Scholar]
- Masamune A, Nakano E, Kume K, et al. Identification of novel missense CTRC variants in Japanese patients with chronic pancreatitis. Gut. 2013;62:653–654. doi: 10.1136/gutjnl-2012-303860. [DOI] [PubMed] [Google Scholar]
- Rosendahl J, Landt O, Bernadova J, et al. CFTR, SPINK1, CTRC and PRSS1 variants in chronic pancreatitis: is the role of mutated CFTR overestimated. Gut. 2013;62:582–592. doi: 10.1136/gutjnl-2011-300645. [DOI] [PubMed] [Google Scholar]
- Ward LD, Kellis M. HaploReg: a resource for exploring chromatin states, conservation, and regulatory motif alterations within sets of genetically linked variants. Nucleic Acids Res. 2012;40 ((Database issue:D930–D934. doi: 10.1093/nar/gkr917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandoval J, Pereda J, Rodriguez JL, et al. Ordered transcriptional factor recruitment and epigenetic regulation of tnf-alpha in necrotizing acute pancreatitis. Cell Mol Life Sci. 2010;67:1687–1697. doi: 10.1007/s00018-010-0272-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


