Abstract
Food insecurity is a considerable challenge in sub-Saharan Africa, disproportionately affecting persons living with HIV/AIDS. This study investigates the lived experience, determinants, and consequences of food insecurity and hunger among individuals living with HIV/AIDS on the shore of Lake Victoria in Suba District, Kenya. Parallel mixed methods included semi-structured interviews and administration of the Household Food Insecurity Access Scale among a systematic sampling of 67 persons living with HIV/AIDS (49 of whom were receiving antiretroviral therapy (ART)). All respondents were either severely (79.1%) or moderately (20.9%) food insecure; no respondents were mildly food insecure or food secure. Qualitative data and simple and multiple linear regression models indicated that significant determinants of food insecurity include increased age, a greater number of children, and not being married. A number of themes related to food insecurity and ART emerged, including: (1) an increase in hunger or appetite since initiating ART; (2) exacerbation of ART-related side effects; and (3) non-adherence to ART due to hunger, food insecurity, or agricultural work responsibilities. HIV interventions should address food insecurity and hunger, particularly among at-risk populations, to promote ART adherence and better health outcomes.
Keywords: food insecurity, hunger, HIV/AIDS, anti-retroviral agents, social determinants, Kenya, sub-Saharan Africa
Background
Food insecurity, characterized by insufficient quantity or quality of food, reductions of food intake, and feelings of uncertainty, anxiety, or shame over food (Coates, Swindale, & Bilinsky, 2007), is a leading cause of global mortality and morbidity and affects an estimated 239 million people in sub-Saharan Africa (FAO, 2010; Lartey, 2008). Food insecurity in sub-Saharan Africa stems from a host of social and structural factors and disproportionately affects the estimated 22.5 million persons living with HIV/AIDS in sub-Saharan Africa (Ivers et al., 2009; Mwaniki, 2006; UNAIDS, 2010).
At the household level, the presence of even one individual living with HIV/AIDS can jeopardize the food security of an entire household. For instance, an HIV-infected individual may experience a loss of income, which may lead to reduced food intake for an entire household (Bukusuba, Kikafunda, & Whitehead, 2007; Haddad & Gillespie, 2001). Lack of food can lead to risky coping strategies in the household which may increase economic vulnerability or exposure to HIV, including the redirection of wage labor or the exchange of sex for money or food (Fenton, 2005; Gillespie & Kadiyala, 2005; Weiser et al., 2007). Food insecurity is also associated with ARV non adherence, incomplete viral load suppression, worse physical health status and mortality among PLWHA (Ivers, et al., 2009; Weiser et al., 2009a; Weiser et al., 2010). Understanding the determinants of food insecurity is critical for guiding policies for integrating nutrition support and HIV/AIDS programming.
Determinants of food insecurity in the general population in both resource-rich and resource-poor countries include markers of low socio-economic status (lower education, income, assets, and unemployment, age, larger household size, and number of children (Foley et al., 2010; Knueppel, Demment, & Kaiser, 2010; Laraia, Siega-Riz, Gunderson, & Dole, 2006; Leyna, Mmbaga, Mnyika, Hussain, & Klepp, 2010; Mohammadzadeh, Dorosty, & Eshraghian, 2010; Vosoris & Tarasuk, 2003). Married men and women have reported higher levels of food security than their never married, cohabiting, separated, and divorced counterparts (Hanson, Sobal, & Frongillo, 2007).
Some studies have investigated determinants of food insecurity among persons living with HIV/AIDS (PLWHA) in the USA (Weiser et al., 2009b), but data are limited on correlates of food insecurity among PLWHA in sub-Saharan Africa. The objectives of this study were to determine the prevalence of food insecurity among PLWHA, to identify demographic and socio-economic correlates of food insecurity among PLWHA, and to explore the lived experience and consequences of food insecurity among PLWHA receiving antiretroviral therapy (ART). To our knowledge, this is the first study to examine household food insecurity among PLWHA in Kenya, and the first mixed methods investigation of the determinants and consequences of food insecurity among PLWHA in sub-Saharan Africa.
Methods
Study Community
This study was conducted in Mfangano Island, Suba District, Nyanza Province, Kenya. Mfangano Island is located between longitudes 33’55” E and 34’6” E and latitudes 0’25” S and 0’30” S. and is one of 16 islands in Suba District located in Lake Victoria. Approximately 19,000 people live on the island, most of whom belong to the Suba or Luo ethnic groups. In Suba District, 32.9% of residents are infected with HIV and 80% of hospital beds are occupied with AIDS-related illness (NASCOP, 2005). Subsistence farming and fishing are the major occupations for most residents. Wild plants and fruits are important in Luo diets and are commonly used for medicinal purposes (Johns & Kokwaro, 1991; Nagata et al., 2011).
Participants
Inclusion criteria for eligible study participants included being older than 18 and being HIV-infected. Eligible respondents also had to be a patient at the Family AIDS Care and Education Services (FACES) Sena Clinic in Mfangano Island. FACES supports the Kenyan Ministry of Health, and is affiliated with the Kenya Medical Research Institute and the University of California, San Francisco and is the only program that currently distributes ART on Mfangano Island.
Biomedical health care providers at the FACES-supported clinic conducted systematic sampling by asking every second man and every second woman meeting the inclusion criteria to participate in a research study about HIV/AIDS and hunger.
Ethics
Ethical approval for this research was provided by the Central University Research Ethics Committee at the University of Oxford and the Suba District Medical Officer of Health in Nyanza Province. Informed consent was obtained verbally.
Study Design and Data Collection
The study was cross-sectional and used parallel mixed methods, including surveys and interviews with quantitative and qualitative components (Creswell, Plano Clark, Gutmann, & Hanson, 2003). Interviews were conducted among PLWHA receiving care at the FACES-supported clinic using a semi-structured questionnaire that lasted approximately 30 minutes. The first and second authors conducted all interviews between 08:00 to 13:00, Monday through Thursday (clinic hours), in March and April 2009 at private offices on the premises of the FACES-supported clinic in the respondent’s preferred language (Luo or English). Luo responses were translated into English.
Food insecurity was measured using the Household Food Insecurity Access Scale (HFIAS) developed by the USAID Food and Nutrition Technical Assistance (FANTA) project (Coates, et al., 2007) and validated in both developed and developing regions (Coates et al., 2006; Frongillo & Nanama, 2006; Knueppel, et al., 2010; Melgar-Quinonez et al., 2006; Swindale & Bilinsky, 2006; Webb et al., 2006; Weiser et al., 2009b). Based on this scale, individuals were categorized into four levels of food insecurity: food secure, mildly food insecure, moderately food insecure, and severely food insecure in accordance with the HFIAS Indicator Guide (Coates, et al., 2007).
Qualitative data on the lived experience and consequences of hunger were collected among PLWHA on ART. A topic guide was created based on inputs from key informants, who were long-term residents of the island, including healthcare workers, community leaders, and host families. Demographic, socio-economic, and ART variables were selected based on previous food insecurity literature (Knueppel, et al., 2010; Laraia, et al., 2006; Leyna, et al., 2010; Mohammadzadeh, et al., 2010) and included age, gender, number of children, marital status, years of schooling, ART usage, and ever skipped a dose of ART.
Data Analysis
Given a power of 80%, significance level of p<0.05, and various estimates for standard deviation, we calculated a sample size of 66 participants in order to determine a regression slope of one. Quantitative statistical analyses were conducted with SPSS 12.0 for Windows (SPSS Inc., Chicago, IL). Simple linear regression was performed with the HFIAS score (continuous) as the dependent variable, and demographic, socio-economic, and health status measures as the independent variables. A backwards stepwise regression was utilized to determine significant variables in a multiple linear regression model.
Grounded theory was used to analyze qualitative data (Lingard, Albert, & Levinson, 2008; Strauss & Corbin, 1998). Open-ended interviews were initially hand coded to generate a master set of codes. Major themes related to food insecurity, ART, socio-demographics, and adherence were discerned utilizing coding and analytic memos. Frequencies of each theme were then tabulated using a computer spreadsheet. The emergent themes were then examined for commonalities, disagreements, and variations.
Results
Seventy patients were approached, 51 female and 19 male. Because the FACES patient population on the island is predominantly female, this proportion is representative of those in care. Sixty-seven (95.7% response rate) consented to participate, 49 who were receiving ART (stavudine, lamivudine, nevirapine or zidovudine, lamivudine, nevirapine) and 18 on supportive HIV/AIDS treatment (such as trimethoprim-sulfamethoxazole) but not receiving ART. The 49 patients receiving ART were also interviewed in depth for the qualitative analysis.
The average age of the sample was 34.7 years and a majority (73.1%) was female (Table 1). Respondents on average had 2.9 children and 6.9 years of schooling. Over three-quarters of the sample were married (77.6%) while a minority was widowed (16.4%) or single (6.0%).
Table 1.
Selected food security, demographic, socio-economic characteristics of study participants
| Variable | n | Percent | Mean | SD | Range |
|---|---|---|---|---|---|
| Household food insecurity | |||||
| Household Food Insecurity Access Scale score | 67 | 12.96 | 5.07 | 2 – 23 | |
| Household Food Insecurity Access prevalence | |||||
| Food secure | 0 | 0.0% | |||
| Mildly food insecure | 0 | 0.0% | |||
| Moderately food insecure | 14 | 20.9% | |||
| Severely food insecure | 53 | 79.1% | |||
| Demographic Characteristics | |||||
| Gender | |||||
| Female | 49 | 73.1% | |||
| Male | 18 | 26.8% | |||
| Age | 67 | 34.71 | 10.51 | 18 – 60 | |
| Marital status | |||||
| Single | 4 | 6.0% | |||
| Married | 52 | 77.6% | |||
| Widowed | 11 | 16.4% | |||
| Number of children | 67 | 2.85 | 1.90 | 0 – 9 | |
| Socio-economic status | |||||
| Schooling (years) | 67 | 6.93 | 3.62 | 0 – 14 | |
| Antiretroviral Therapy | |||||
| Current ART usage | |||||
| Yes | 49 | 73.1% | |||
| No | 18 | 26.8% |
Characterization of Food Insecurity
The average HFIAS score among PLWHA was 13.0 (Table 1). Overall, 79.1% of respondents were severely food insecure, 20.9% of respondents were moderately food insecure, and no respondents were mildly food insecure or food secure.
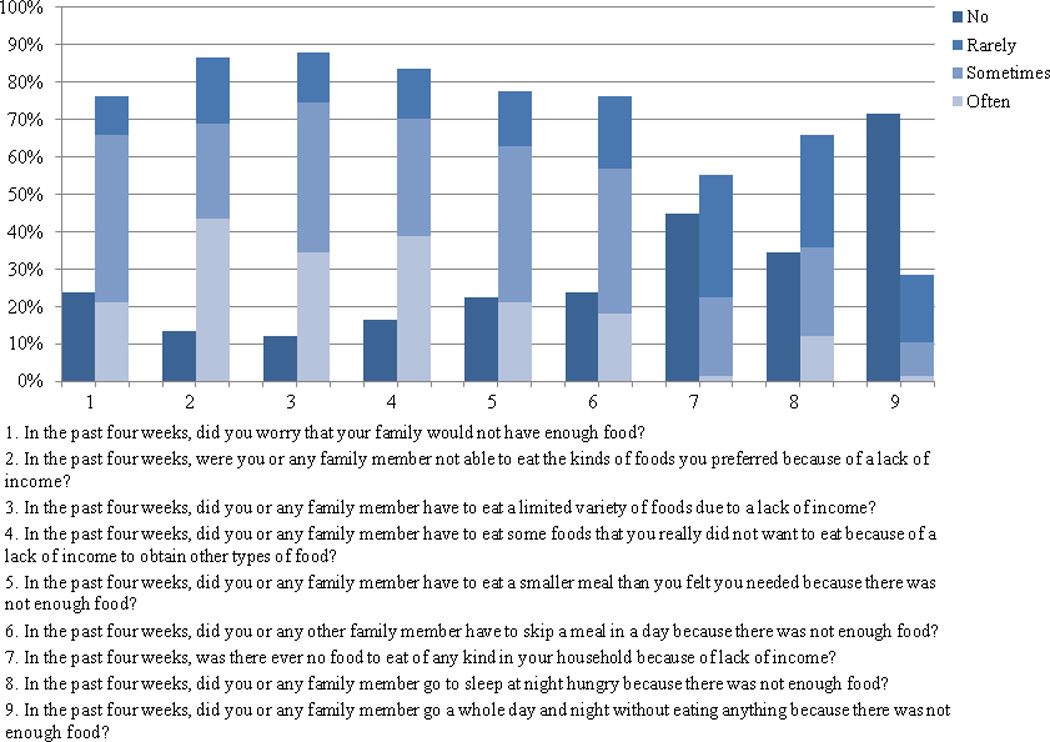
A majority of respondents reported experiencing each of the nine food insecurity conditions in the past month except for going a whole day and night without eating (Figure 1). Among the nine household food insecurity-related conditions, respondents most often experienced eating a limited variety of foods due to a lack of resources.
Figure 1.
Determinants of Food Insecurity
Qualitative data indicated that large family size, lack of a spouse, and old age contributed to food insecurity. In simple and multiple linear regression models of food insecurity, these three demographic variables were significantly associated with higher levels of food insecurity. Gender, education, and ART use were not found to be significantly associated with the HFIAS score (Table 2).
Table 2.
Results from simple and multiple linear regression with Household Food Insecurity Access Scale score (HFIAS Score) as the dependent variable, and various measures of socio-economic status and demographics as independent variables
| Simple Linear Regression | Multiple linear regressiona | |||||||
|---|---|---|---|---|---|---|---|---|
| B(SE) | Intercept | R2 | p | B(SE) | Intercept | R2 | p | |
| Determinants | ||||||||
| Socio-demographic | ||||||||
| Age | 0.17 (0.06)** | 7.16 | 0.11 | <0.01** | 0.10 (0.05)* | 9.62 | 0.40 | <0.01** |
| Gender | 1.23 (1.40) | 12.06 | 0.01 | 0.38 | ||||
| Childrenb | 1.10 (0.30)** | 9.82 | 0.17 | <0.01** | 1.16 (0.29)** | 9.62 | 0.40 | <0.01** |
| Married | −3.41 (1.44)* | 15.60 | 0.08 | 0.02* | −4.54 (1.25)** | 9.62 | 0.40 | <0.01** |
| Schoolingc | −0.28 (0.17) | 14.86 | 0.04 | 0.11 | ||||
| Antiretroviral therapy | ||||||||
| ART usage | 2.14 (1.38) | 11.40 | 0.04 | 0.13 | ||||
Multiple linear regression model included age, children, and marriage.
number of children in household
number of completed years of schooling
p<0.05
p<0.01
Family size
In the simple linear regression model, each additional child was associated with a 1.10 unit increase in the HFIAS score (p<0.01). In interviews, respondents described concern over feeding their children, particularly in families with many children. Some respondents reported sacrificing their own food intake so that their children could eat sufficiently.
“I have been taking ARV’s for one and a half years and they have been good. I even take ARV’s on an empty stomach sometimes so my kids can eat more. Kids don't understand why there is no food. Not knowing how to get food is very hard” (Female ART patient, married, age 34, 4 children).
“I skip lunch as a way of saving money and working longer during the day. It is worth it to be able to provide my children with a good supper” (Male ART patient, married, age 49, 5 children).
Marital Status
Being married was associated with a 3.41 decrease in the HFIAS score (p=0.02) in the simple linear regression model of food insecurity. Some respondents explained the additional challenge of acquiring food for a household without the support of a spouse. Women who were widowed, single, or not receiving financial support from a breadwinner discussed these challenges.
“My husband died. It has been tough; not because of HIV but because of income. Unless you have someone working for an income it is not easy to provide for your family. We sometimes go without eating anything” (Female ART patient, married, age 28).
Single women similarly relied on parents, particularly fathers, for food and financial support. “I had some differences in the house with my father so my sisters and I did not eat much for a week” (Female ART patient, single, age 23).
Older Age
A one-year increase in age was associated with a 0.17 unit increase in the HFIAS score in simple linear regression (p<0.01). This was borne out in qualitative data; PLWHA describe the increasing difficulty in completing agricultural labor and therefore producing food as they grow older.
“Work is hard; it is more difficult now than it has ever been before. At times, I’m too tired. I work slower on the farm than I did in the past so it takes me longer to harvest crops” (Female ART patient, married, age 59).
Multiple linear regression was performed to control for confounding and to find a combination of variables that best predicted the HFIAS score. In backwards stepwise linear regression age, number of children, and being married remained significantly associated with the HFIAS score (all p<0.01) (Table 2).
Consequences of Food Insecurity among Persons on Antiretroviral Therapy
In our qualitative data (n=49), three themes related to the consequences of food insecurity among PLWHA receiving ART emerged: (1) an increase in hunger or appetite since initiating ART (n=41); (2) exacerbation of ART gastrointestinal side-effects (n=15); and (3) skipping a dose of ART for any reason (n=20) or directly due to hunger, food insecurity, or agricultural work responsibilities (n=8) (Table 3).
Table 3.
Number of ART patients who identified hunger and food insecurity related themes
| Identified | Disagreed | Not addressed |
|
|---|---|---|---|
| Hunger and ART | |||
| Increased hunger while on ART | 41 (84%) | 4 (8%) | 4 (8%) |
| Immediate change in hunger when starting ART | 14 (29%) | 2 (4%) | 33 (67%) |
| Increased frequency of eating | 11 (22%) | 4 (8%) | 34 (69%) |
| ART side-effects | |||
| Nausea, vomitting, gastrointestinal side-effects | 15 (31%) | 4 (8%) | 30 (61%) |
| ART adherence | |||
| Ever skipped a dose of ART | 20 (41%) | 29 (59%) | 0 (0%) |
| Ever skipped ART due to hunger, food insecurity, agriculture | 8 (16%) | 36 (74%) | 5 (10%) |
1. Increased hunger and appetite after ART initiation
A majority of respondents (84%) described an increase in appetite or hunger since initiating ART, beyond hunger levels experienced before starting ART.
“I feel very hungry when it is the time to take meals. I feel the stomach is really burning” (Female ART patient, married, age 39).
“I experienced an increase in appetite, so I needed something to eat after every short time. I just felt hungry” (Female ART patient, married, age 28).
For many PLWHA on ART, the increased hunger was experienced as an immediate change after initiating ART (29%). The changes experienced on the first few days of ART were particularly memorable to respondents.
“On the day I started ARV's, I felt very hungry. On the second day, I felt very, very hungry” (Male ART patient, married, age 49).
In order to cope with increased appetite with ARVs, participants often increased the frequency of eating (22%). “When I started ARVs, I felt a lot of hunger. I needed to eat more frequently than usual. The hunger becomes difficult because I am not in a position to get the foods I want. But I just take the ARVs even if I don’t have food … since these are powerful drugs against HIV” (Female ART patient, widowed, age 48).
Others chose to give up the morning meal, since sensations of hunger were most bothersome at night and interfered with sleep. “It is better to skip the morning meals rather than the evening ones. During the day, you can ignore the hunger by eating with your eyes. You can talk to people, look at foods, swim, or work at the farm. But at night, I am telling you that you will not be able to sleep. You will have problems” (Male ART patient, married, 38).
Despite the hunger, some patients would continue take ART consistently, because they believed in its “power” to combat HIV.
In contrast, a minority of respondents (8%) reported decreased hunger after initiating ART, potentially explained by lamivudine’s side effect of loss of appetite. “I was tested one day, and immediately I found out that I was HIV positive. … Soon after, I was told to start taking ARV's. Since starting on ARV's, I have not felt any kind of sickness. When I take ARV's, I just feel like the hunger disappears” (Female ART patient, widowed, age 33).
2. ART side effects
Gastrointestinal side-effects of ART, which included the exacerbation of nausea, vomiting, and diarrhea symptoms after the initiation of ART, affected 31% of respondents.
“I had pangs in my lower abdomen. After three days, I was feeling very fatigued. My belly felt as if it was being constantly pumped. I felt a lot of pain. The following day I started diarrhea, which continued for two days. I had been instructed about these side effects” (Male ART patient, married, age 48). These side effects were also often exacerbated by the absence of food. As explained by one participant, “I usually take the pills before eating anything, so I will sometimes have a stomach ache or feel nausea” (Male ART patient, married, age 33).
3. Hunger and adherence
Nearly a third of respondents (31%) reported skipping at least one ART dose and 40% of these respondents cited reasons related to hunger, food insecurity, or food production work. Because some ARV’s should be taken with food, respondents without access to sufficient food reported occasionally skipping the drugs.
“When you take these drugs, you feel so hungry. They are so powerful. If you take them on an empty stomach they just burn. I found that sometimes I would just skip the drugs, but not tell anyone. These are some of the things that make it difficult to survive” (Male ART patient, married, age 33).
“There was a time when I defaulted. I slept hungry. The following morning, after just seeing the drugs I felt like vomiting on an empty stomach. I stopped for one month. When I came back to the clinic for another supply I was not treated well because I had skipped. I started again and defaulted again” (Female ART patient, married, age 28).
Discussion
Severe and moderate food insecurity was universal among PLWHA in this rural island community in Lake Victoria. To our knowledge, this is the first study to evaluate the experience of food insecurity and its correlates among PLWHA in Kenya. Food insecurity levels in this study among PLWHA were higher than food insecurity levels reported in other parts of sub-Saharan Africa (Knueppel, et al., 2010; Mamlin et al., 2009). Rural areas may have higher levels of food insecurity due to higher levels of poverty, smaller plots of land per family, and poor soil quality (Mamlin, et al., 2009).
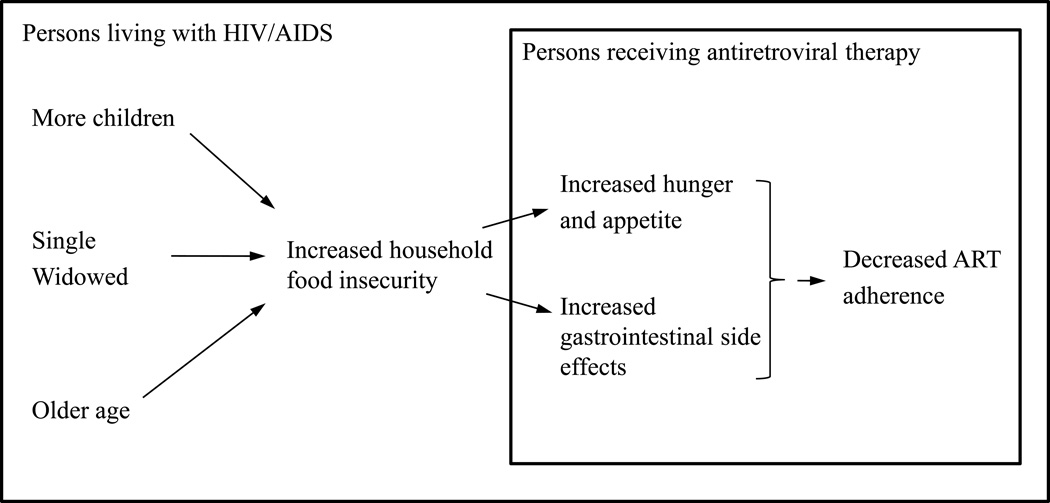
Having more children, being single or widowed, and being older may lead to increased household food insecurity (Figure 2). A larger number of children in a household may mean less food consumption for each family member (Chaput, Gilbert, & Tremblay, 2007; Mohammadzadeh, et al., 2010; Townsend, Peerson, Love, Achterberg, & Murphy, 2001). Marriage can enhance family income and wealth (Light, 2004; Waite, 1995), allow for the sharing of resources (Hanson, et al., 2007), and provide social support (Cutrona, 1996), which all may contribute to improved food security. Older adults living with HIV/AIDS may have higher food insecurity due to challenges in working on farms and dependence on others for food, as reported in other studies. (Knueppel, et al., 2010; Laraia, et al., 2006; Leyna, et al., 2010).
Figure 2.
Determinants and consequences of household food insecurity in SubaDistrict, Kenya
Household food insecurity contributed to increased hunger and appetite among PLWHA, as well as increased gastrointestinal side effects after the start of ART. Both of these factors likely contributed to decreased adherence to ART among participants interviewed, as was observed in Uganda (Weiser, et al., 2010). It should be noted that the recommendation to take some medicines, including zidovudine, with food in the setting of universal food insecurity may contribute to decreased ART adherence.
This study has several limitations and its cross-sectional design precludes any causal inferences. While the qualitative data alluded to a possible association between food insecurity and adherence, this needs to be confirmed in further studies. Although the three patients who declined to be interviewed reflected the gender proportion of the overall sample, it is unknown if they differed in other demographic characteristics. Data on body mass index, household wealth and consumption, and more comprehensive adherence or clinical data would have strengthened the study. In addition, the lack of variability in the sample may have made it difficult to detect correlates of food insecurity. Furthermore, we did not have a non-HIV infected group for comparison. As the study was conducted in a rural island community in western Kenya with a relatively small sample size, results may not be generalizable to other populations more urban or on the mainland, which may have improved transportation and access to markets. Despite these limitations, the food insecurity instrument (HFIAS) was designed for cross-cultural settings, has been validated in rural sub-Saharan Africa, and was pre-tested with key informants in Mfangano Island. In addition, the strengths of the study include mixed qualitative and quantitative methods, which allowed for statistical testing supported by qualitative analysis.
Conclusion
Severe and moderate food insecurity was universal among PLWHA in Suba District, and its severity was associated with increased age, greater number of children, and not being married. Our findings coupled with those of others support the assertion that combating food insecurity may be imperative to the success of HIV/AIDS support programs (Ivers, et al., 2009). Through partnerships between government agencies, non-governmental organizations, and communities, countries need to develop and expand nutritional, agricultural and structural interventions to radically improve food insecurity, reduce hunger, and improve the health of families, particularly those affected by HIV.
Acknowledgements
Thanks to Charles Salmen, Nadine Levin, and Caroline Potter for advice and comments. Insights into Luo and Suba culture and on-site guidance in Mfangano Island were greatly appreciated from the Family AIDS Care and Education Services (FACES), Ministry of Health, and Organic Health Response staff. This research was made possible by a grant from the E.O. James Bequest, All Souls College, University of Oxford.
References
- Bukusuba J, Kikafunda J, Whitehead R. Food security status in households of people living with HIV/AIDS (PLWHA) in a Ugandan urban setting. British Journal of Nutrition. 2007;98:211–217. doi: 10.1017/S0007114507691806. [DOI] [PubMed] [Google Scholar]
- Chaput S, Gilbert J, Tremblay A. Relationship between food insecurity and body composition in Ugandans living in urban Kampala. Journal of the American Dietetic Association. 2007;107:1978–1982. doi: 10.1016/j.jada.2007.08.005. [DOI] [PubMed] [Google Scholar]
- Coates J, Frongillo E, Rogers B, Webb P, Wilde P, Houser R. Commonalities in the experience of household food insecurity across cultures: what are measures missing? Journal of Nutrition. 2006;136(5):1438S–1448S. doi: 10.1093/jn/136.5.1438S. [DOI] [PubMed] [Google Scholar]
- Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Household Food Access: Indicator Guide (v. 3) Washington, DC: Food and Nutrition Technical Assistance Project, Academy for Educational Development; 2007. [Google Scholar]
- Creswell J, Plano Clark V, Gutmann M, Hanson W. Advanced mixed methods research designs. In: Tashakkori A, Teddlie C, editors. Handbook of Mixed Methods in Social and Behavioral Research. Thousand Oaks, CA: Sage; 2003. [Google Scholar]
- Cutrona C. Social support in couples: marriage as a resource in times of stress. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- FAO. The State of Food Insecurity in the World. Rome: Food and Agriculture Organization; 2010. [Google Scholar]
- Fenton L. Preventing HIV/AIDS through poverty reduction: the only sustainable solution. Lancet. 2005;364(9440):1186–1187. doi: 10.1016/S0140-6736(04)17109-2. [DOI] [PubMed] [Google Scholar]
- Foley W, Ward P, Carter P, Coveney J, Tsourtos G, Taylor A. An ecological analysis of factors associated with food insecurity in South Australia, 2002-7. Public Health Nutrition. 2010;13(2):215–221. doi: 10.1017/S1368980009990747. [DOI] [PubMed] [Google Scholar]
- Frongillo E, Nanama S. Development and validation of an experience-based measure of household food insecurity within and across seasons in Northern Burkina Faso. Journal of Nutrition. 2006;136(5):1409S–1419S. doi: 10.1093/jn/136.5.1409S. [DOI] [PubMed] [Google Scholar]
- Gillespie S, Kadiyala S. HIV/AIDS and food and nutrition security: from evidence to action. Washington, DC: International Food Policy Research Institute; 2005. [Google Scholar]
- Haddad L, Gillespie S. Effective food and nutrition policy responses to HIV/AIDS: what we know and what we need to know. Journal of International Development. 2001;13(4):487–511. [Google Scholar]
- Hanson K, Sobal J, Frongillo E. Gender and marital status clarify associations between food insecurity and body weight. Journal of Nutrition. 2007;137(6):1460–1465. doi: 10.1093/jn/137.6.1460. [DOI] [PubMed] [Google Scholar]
- Ivers L, Cullen K, Freedberg K, Block S, Coates J, Webb P. HIV/AIDS, undernutrition, and food insecurity. Clinical Infectious Diseases. 2009;49(7):1092–1102. doi: 10.1086/605573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns T, Kokwaro J. Food plants of the Luo of Siaya District, Kenya. Economic Botany. 1991;45(1):103–113. [Google Scholar]
- Knueppel D, Demment M, Kaiser L. Validation of the Household Food Insecurity Access Scale in rural Tanzania. Public Health Nutrition. 2010;13(3):360–367. doi: 10.1017/S1368980009991121. [DOI] [PubMed] [Google Scholar]
- Laraia B, Siega-Riz A, Gunderson C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. Journal of Nutrition. 2006;136(1):177–182. doi: 10.1093/jn/136.1.177. [DOI] [PubMed] [Google Scholar]
- Lartey A. Maternal and child nutrition in Sub-Saharan Africa: challenges and interventions. Proceedings of the Nutrition Society. 2008;67(1):105–108. doi: 10.1017/S0029665108006083. [DOI] [PubMed] [Google Scholar]
- Leyna G, Mmbaga E, Mnyika K, Hussain A, Klepp K. Food insecurity is associated with food consumption patterns and anthropometric measures but not serum micronutrient levels in adults in rural Tanzania. Public Health Nutrition. 2010;13(9):1438–1444. doi: 10.1017/S1368980010000327. [DOI] [PubMed] [Google Scholar]
- Light A. Gender differences in the marriage and cohabitation income premium. Demography. 2004;41(2):263–284. doi: 10.1353/dem.2004.0016. [DOI] [PubMed] [Google Scholar]
- Lingard L, Albert M, Levinson W. Grounded theory, mixed methods, and action research. British Medical Journal. 2008;337:a567. doi: 10.1136/bmj.39602.690162.47. [DOI] [PubMed] [Google Scholar]
- Mamlin J, Kimaiyo S, Lewis S, Tadayo H, Jerop F, Gichunge C, Einterz R. Integrating nutrition support for food-insecure patients and their dependents into an HIV care and treatment program in Western Kenya. American Journal of Public Health. 2009;99(2):215–221. doi: 10.2105/AJPH.2008.137174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melgar-Quinonez H, Zubieta A, MkNelly B, Nteziyaremye A, Gerardo M, Dunford C. Household food insecurity and food expenditure in Bolivia, Burkina Faso, and the Philippines. Journal of Nutrition. 2006;136(5):1420S–1430S. doi: 10.1093/jn/136.5.1431S. [DOI] [PubMed] [Google Scholar]
- Mohammadzadeh A, Dorosty A, Eshraghian M. Household food security status and associate factors among high-school students in Esfahan, Iran. Public Health Nutrition. 2010;13(10):1609–1613. doi: 10.1017/S1368980010000467. [DOI] [PubMed] [Google Scholar]
- Mwaniki A. Achieving food security in Africa – Challenges and Issues, from http://www.un.org/africa/osaa/reports/Achieving%20Food%20Security%20in%20Africa-Challenges%20and%20Issues.pdf>. (2006, 24 August 2010) [Google Scholar]
- Nagata J, Jew A, Kimeu J, Salmen C, Bukusi EC, Cohen CR. Medical pluralism on Mfangano Island: Use of medicinal plants among persons living with HIV/AIDS in Suba District, Kenya. Journal of Ethnopharmacology. 2011;135(2):501–509. doi: 10.1016/j.jep.2011.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NASCOP. National AIDS and STI Control Program. Nairobi: Ministry of Health; 2005. Sentinel Surveillance of HIV and STDs in Kenya. [Google Scholar]
- Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Swindale A, Bilinsky P. Development of a universally applicable household food insecurity measurement tool: process, current status, and outstanding issues. Journal of Nutrition. 2006;136(5):1449S–1452S. doi: 10.1093/jn/136.5.1449S. [DOI] [PubMed] [Google Scholar]
- Townsend M, Peerson J, Love B, Achterberg C, Murphy S. Food insecurity is positively related to overweight in women. Journal of Nutrition. 2001;131(6):1738–1745. doi: 10.1093/jn/131.6.1738. [DOI] [PubMed] [Google Scholar]
- UNAIDS. UNAIDS Report on the Global AIDS Epidemic 2010. Geneva: Joint United Nations Programme on HIV/AIDS; 2010. [Google Scholar]
- Vosoris N, Tarasuk V. Household food insufficiency is associated with poorer health. Journal of Nutrition. 2003;133(1):120–126. doi: 10.1093/jn/133.1.120. [DOI] [PubMed] [Google Scholar]
- Waite L. Does marriage matter? Demography. 1995;32:483–507. [PubMed] [Google Scholar]
- Webb P, Coates J, Frongilo E, Rogers B, Swindale A, Bilinsky P. Measuring household food insecurity: why it’s so important and yet so difficult to do. Journal of Nutrition. 2006:1404S–1408S. doi: 10.1093/jn/136.5.1404S. [DOI] [PubMed] [Google Scholar]
- Weiser S, Bangsberg D, Kegeles S, Ragland K, Kushel M, Frongillo E. Food insecurity among homeless and marginally housed individuals living with HIV/AIDS in San Francisco. AIDS and Behavior. 2009b;13(5):841–848. doi: 10.1007/s10461-009-9597-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser S, Frongillo E, Ragland K, Hogg R, Riley E, Bangsberg D. Food Insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. Journal of General Internal Medicine. 2009a;24(1):14–20. doi: 10.1007/s11606-008-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser S, Leiter K, Bangsberg D, Butler L, Pery-de Korte F, Phaladze N, Heisler M. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Medicine. 2007;4:1589–1597. doi: 10.1371/journal.pmed.0040260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser S, Tuller D, Frongillo E, Senkungu J, Mukiibi N, Bangsberg D. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PloS One. 2010;5(4):e10340. doi: 10.1371/journal.pone.0010340. [DOI] [PMC free article] [PubMed] [Google Scholar]